Abstract
The first wave of COVID-19 epidemic began in late January in Malaysia and ended with a very small final size. The second wave of infections broke out in late February and grew rapidly in the first 3 weeks. Authorities in the country responded quickly with a series of control strategies collectively known as the Movement Control Order (MCO) with different levels of intensity matching the progression of the epidemic. We examined the characteristics of the second wave and discussed the key control strategies implemented in the country. In the second wave, the epidemic doubled in size every 3.8 days (95% confidence interval [CI]: 3.3, 4.5) in the first month and decayed slowly after that with a halving time of approximately 3 weeks. The time-varying reproduction number Rt peaked at 3.1 (95% credible interval: 2.7, 3.5) in the 3rd week, declined sharply thereafter and stayed below 1 in the last 3 weeks of April, indicating low transmissibility approximately 3 weeks after the MCO. Experience of the country suggests that adaptive triggering of distancing policies combined with a population-wide movement control measure can be effective in suppressing transmission and preventing a rebound.
Keywords: COVID-19, Coronavirus, Prevention and control, Transmission, Reproduction number
Introduction
The first case of coronavirus disease 2019 (COVID-19) was confirmed in Malaysia on January 25, 2020, marking the first wave of infection in the country that lasted for about 3 weeks (Ministry of Health Malaysia (MOH), 2020). The total number of cases was low, with 22 confirmed infections, 20 of which were imported, and no fatality.
A second wave broke out on February 27 after 11 days of no new cases. On March 11, a neighboring country, Brunei, traced its first infection to a large religious gathering in Kuala Lumpur, Malaysia, between February 27 and March 1 attended by about 14,500 participants. Approximately 2 weeks after the gathering on March 15, Malaysia recorded the first 3-digit jump in a day with 190 new cases. Authorities announced the next day a nationwide Movement Control Order (MCO), a soft cordon sanitaire or partial lockdown that went into effect on March 18 to reduce social mixing (Ministry of Health Malaysia (MOH), 2020). This is followed by a stricter version called the enhanced MCO, an adaptive policy implemented indefinitely since March 27 to contain large epidemic clusters. Following the decline of cases, MCO was subsequently relaxed and replaced by Conditional Movement Control Order (CMCO) on May 4, and further relaxed under the Recovery Movement Control Order (RMCO) on June 10.
Here, we describe the characteristics of the second wave of COVID-19 epidemic in the country and recount the major control strategies.
Methods
Refer to the supplementary material.
Results
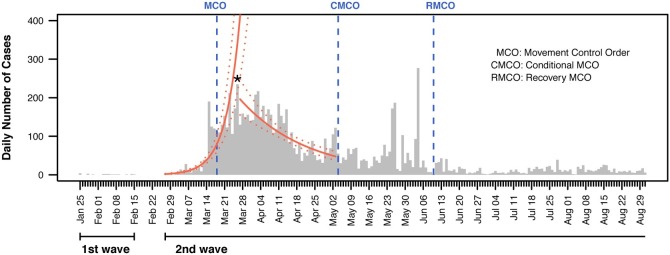
By the end of August, there were 9340 confirmed cases with a recovery rate of 96.9%. Imported cases made up 8.8% (826), while a total of 127 deaths were reported. The nationwide 14-day delay-adjusted case fatality rate is 1.4% (95% confidence interval: 1.2%, 1.6%) for the current study period. The second wave of the epidemic began on February 27 and grew at a rate of 18% (95% confidence interval: 15%, 21%) per day, with a doubling time of 3.8 (3.3, 4.5) days in the first month (Fig. 1 ). If there had been no intervention, daily cases would have exceeded 400 after March 26 and escalated thereafter. The epidemic decayed slowly at a rate of -4% (-5%, -3%) after March 26, with a halving time of 18.1 (14.1, 25.2) days. Transmissibility, represented by Rt, peaked at 3.1 (95% credible interval: 2.7, 3.5) on March 15 and declined sharply afterwards, reaching 1 in approximately 3 weeks after the national MCO (2 weeks after the enhanced version of the measure), and staying below 1 for the rest of April (Fig. 2 ).
Fig. 1.
Daily COVID-19 cases from January 25 to August 31, 2020, shown as vertical bars. Vertical dashed lines indicate the start of control measures. Solid curved lines represent the predicted number of daily cases for the second wave based on two exponential models, one for the growth phase starting from February 27 to March 26 (asterisk), and another for the decay phase starting from March 27 to May 3, a day before the CMCO. Dotted lines represent the corresponding 95% confidence interval.
Fig. 2.
Instantaneous reproduction number (Rt) estimated over weekly sliding windows for the second wave, shown as a solid line. The shaded area along the solid line represents the corresponding 95% credible interval. Background shading denotes the different periods under Movement Control Order (MCO), Conditional Movement Control Order (CMCO) and Recovery Movement Control Order (RMCO).
Discussion
Our results suggest that the COVID-19 epidemic in Malaysia appears to be under control. Analyses show that approximately 3 weeks after the MCO, disease transmissibility has reduced substantially and remained low for the remaining time period, except for two upswings that occurred in late May and early June due to transmissions among foreigners in detention centers (Fig. 2) (Ministry of Health Malaysia (MOH), 2020). Decline in transmissibility started a few days before the official MCO measure, likely because of more public awareness and reduced social mixing because of earlier reports of increases in confirmed cases.
A mixture of interventions was implemented to curb spread. In the early stages of the second wave, authorities responded with MCO, a strict nationwide order to limit movement and border travel, in addition to ongoing contact tracing and proactive surveillance among individuals with influenza-like illness and severe acute respiratory infection. Community-targeted mass testing was also implemented selectively to contain epidemic hotspots. Exit strategy was executed in a few stages. The national MCO was replaced by CMCO and eventually by RMCO, while numerous new social distancing measures were introduced to suppress spread and prevent resurgence (Petersen et al., 2020). For example, restriction on the number of worshipers to the size of the buildings, staggered reopening of schools prioritizing students who will be taking school leaving examinations, a limitation of 250 people in public events, and access to digital technology to aid contact tracing, interstate travel, and self-evaluation which is useful for those under surveillance or quarantines. These strategies are consistent with the suggestions of some early reports that noted combining multiple measures might offer effective options to minimize the risk of further lockdowns (Chen et al., 2020; Colbourn, 2020; Cowling et al., 2020, Giordano et al., 2020, Prem et al., 2020).
Our observations suggest that intermittent triggering of adaptive measures coupled with population-wide distancing policies and proactive surveillance have provided effective control against the epidemic in the country. Until viable pharmaceutical options become available, the continuous evaluation of non-pharmaceutical strategies and the support for those disproportionately affected will be important.
Contributions
CFSN and XS conceived the study with input from MS, MLM, LM and MABAT. CFSN extracted the data which was validated by MABAT. CFSN led the analysis with inputs from XS and MS. All authors contributed to the interpretation and writing of the final draft.
Conflicts of interest
None.
Funding source
None.
Ethical approval
None.
Declaration of interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
.
Armitage and Nellums, 2020, Chung et al., 2020, Coulbourn, 2020 and Dorn et al. (2020).
Footnotes
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.ijid.2020.10.027.
Appendix A. Supplementary data
The following are Supplementary data to this article:
References
- Armitage R, Nellums LB. COVID-19 and the consequences of isolating the elderly. Lancet Public Health. 2020 doi: 10.1016/S2468-2667(20)30061-X. epub ahead of print. https://doi.org/10.1016/s2468-2667(20)30061-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen S., Yang J., Yang W. COVID-19 control in China during mass population movements at New Year. Lancet. 2020;395:764–766. doi: 10.1016/S0140-6736(20)30421-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chung R.Y., Dong D., Li M.M. Socioeconomic gradient in health and the covid-19 outbreak. BMJ. 2020;369:m1329. doi: 10.1136/bmj.m1329. [DOI] [PubMed] [Google Scholar]
- Coulbourn T. COVID-19: extending or relaxing distancing control measures. Lancet Public Health. 2020 doi: 10.1016/S2468-2667(20)30072-4. epub ahead of print. https://doi.org/10.1016/S2468-2667(20)30073-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cowling B.J., Ali S.T., Ng T.W.Y. Impact assessment of non-pharmaceutical interventions against coronavirus disease 2019 and influenza in Hong Kong: an observational study. Lancet Public Health. 2020 doi: 10.1016/S2468-2667(20)30090-6. epub ahead of print. https://doi.org/10.1016/s2468-2667(20)30090-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dorn A.V., Cooney R.E., Sabin M.L. COVID-19 exacerbating inequalities in the US. Lancet. 2020;395:1243–1244. doi: 10.1016/S0140-6736(20)30893-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giordano G., Blanchini F., Bruno R. Modelling the COVID-19 epidemic and implementation of population-wide interventions in Italy. Nature Medicine. 2020 doi: 10.1038/s41591-020-0883-7. epub ahead of print. https://doi.org/10.1038/s41591-020-0883-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ministry of Health Malaysia (MOH) 2020. COVID-19 Media Centre: Press Release. Available from: http://moh.gov.my/index.php/pages/view/2019-ncov-wuhan-kenyataan-akhbar. [Accessed 30 April 2020] [Google Scholar]
- Petersen E., Wasserman S., Lee S.-S. COVID-19–We urgently need to start developing an exit strategy. International Journal of Infectious Diseases. 2020 doi: 10.1016/j.ijid.2020.04.035. epub ahead of print. https://doi.org/10.1016/j.ijid.2020.04.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prem K., Liu Y., Russell T.W. The effect of control strategies to reduce social mixing on outcome of the COVID-19 epidemic in Wuhan, China: a modelling study. Lancet Public Health. 2020 doi: 10.1016/S2468-2667(20)30073-6. epub ahead of print. https://doi.org/10.1016/s2468-2667(20)30073-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.