In several case series the sphenopalatine ganglion (SPG) block has been reported to effectively treat postdural puncture headache (PDPH).1, 2, 3 To understand the proposed mechanism behind the SPG block, the cerebrovascular dynamics of PDPH must be understood. Boezaart measured the increase in cerebral blood flow (CBF) due to vasodilation associated with cerebral spinal fluid loss and reported the decrease in CBF due to vasoconstriction that occurred immediately following blood being introduced into the epidural space.4 The pain associated with PDPH is due to meningeal nociceptive stimulation from cerebral vasodilation, which is carried via the trigeminal nerve. This trigemino-vascular network mediates the parasympathetic autonomic vasomotor system and includes the SPG as an essential component.5 The SPG has a parasympathetic root, therefore blocking the SPG decreases vasodilatory parasympathetic autonomic activity and vasoconstriction ensues. This mechanism for PDPH relief is shared by the SPG block and epidural blood patch.
The transnasal SPG block uses a long cotton tip applicator, soaked in local anesthetic, advanced into the nasal cavity.2 The only randomized controlled trial to date demonstrated no difference in efficacy when the transnasal block was performed with local anesthetics versus saline.6 We believe the efficacy of the transnasal route SPG block is inconsistent due to requiring precise placement of the applicator, as well as absorption of the local anesthetic across multiple barriers, including the nasal mucosa, sphenopalatine foramen, and fat space within the pterygopalatine fossa (PPF). Additionally, in the current COVID-19 pandemic, recommendations from the Society for Obstetric Anesthesia and Perinatology (SOAP) suggest that this technique is inadvisable in known or suspected COVID-19 patients because the transnasal route risks aerosolization.7 Due to significant discomfort reported by patients, the lack of efficacy of the transnasal approach, and risk of aerosolization, we do not endorse the transnasal route. Rather, we propose a percutaneous approach, which in our experience has a higher success rate and is well tolerated by patients.
A suprazygomatic, percutaneous, needle-based approach to blocking the SPG is an alternative to the transnasal technique. This approach can be performed using real-time ultrasound guidance to place a 25-gauge spinal needle into the PPF, delivering 5 mL of 0.5% ropivacaine bilaterally (Fig. 1 ).8 A high-frequency linear ultrasound probe is positioned inferior to the zygomatic arch and angled approximately 45° cephalad to image the PPF between the maxilla anteriorly and the ramus of the mandible and pterygoid process of the sphenoid bone posteriorly. The needle is inserted superior to the zygomatic arch and posterior to the posterior orbital rim. It is directed approximately 45° caudad, 10° anterior, and advanced 50 mm into the PPF, where the ropivacaine can be deposited. This approach to the SPG block is highly effective because it delivers local anesthetic directly into the PPF and around the nerves of interest. It is also a low-risk approach because the needle is directed at 90° apposition to all the bony foramina connecting the PPF to other spaces. As such, it is anatomically impossible to direct the needle to unsafe locations without passing it through bone. Serious complications have only been described in conjunction with either intra-oral approaches or infrazygomatic approaches. The intra-oral approach involves inserting the needle through the greater palatine foramen and palatine canal, widely regarded as the highest risk approach to the PPF.9 The infrazygomatic approach is performed either directly medial or using a posterior-to-anterior approach, transiting the infratemporal fossa, which contains all five terminal branches of the maxillary artery.10 The posterior-to-anterior approach also directs the needle toward the infra-orbital fissure, risking needle entry into the orbit. To date, there have been no descriptions in the literature of any complications associated with the suprazygomatic approach except minor skin bleeding at the needle insertion site. We have chosen the suprazygomatic approach in our practice specifically because of its safety profile. Data extracted from the electronic medical records at the University of Florida revealed over 1500 of these procedures have been safely performed for various indications.
Fig. 1.
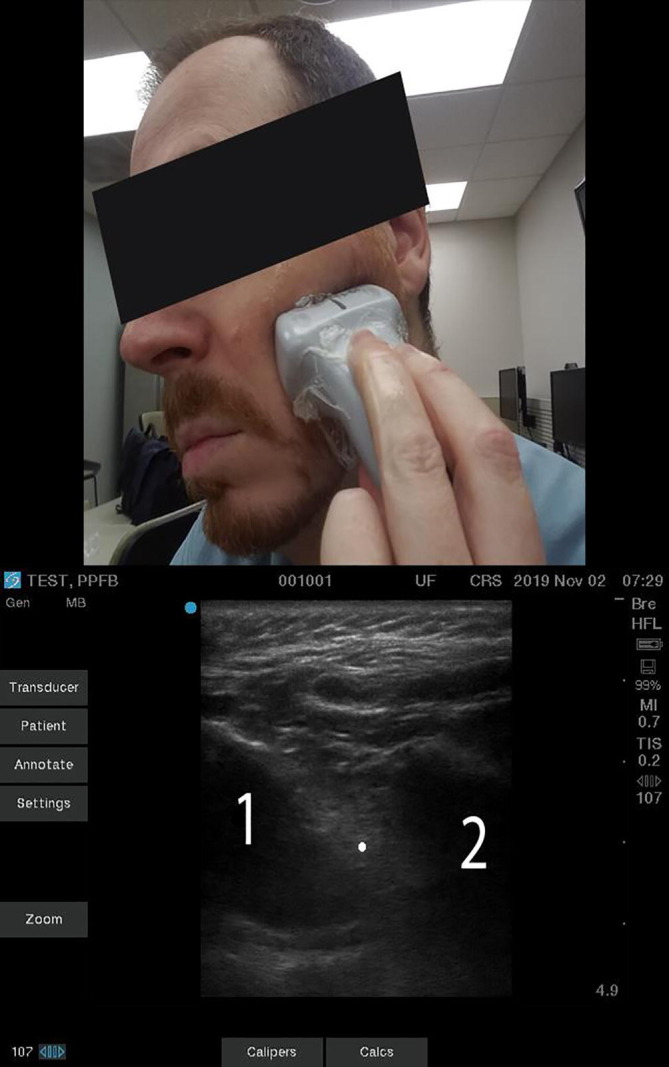
Top: A photograph of correct ultrasound placement on the face to image the pterygopalatine fossa. Below: An ultrasound image of the pterygopalatine fossa. (1) The bone shadow of the maxilla anteriorly. (2) The combined bone shadow of the mandibular ramus superficially and the pterygoid process of the sphenoid bone deep. The dot represents the position of the needle tip in the pterygopalatine fossa between the maxilla and the pterygoid process. Needle insertion site and angle of entry are described in the body of the text.
The current evidence does not support the transnasal SPG block for the treatment of PDPH. The suprazygomatic, percutaneous approach has shown efficacy in treating other vascular-mediated headaches and we are exploring this approach for the treatment of PDPH. We propose that this technique is worthy of further study.
Financial disclosures
None.
Declaration of interests
None.
References
- 1.Cohen S., Sakr A., Katyal S., Chopra D. Sphenopalatine ganglion block for postdural puncture headache. Anaesthesia. 2009;64:574–575. doi: 10.1111/j.1365-2044.2009.05925.x. [DOI] [PubMed] [Google Scholar]
- 2.Kent S., Mehaffey G. Transnasal sphenopalatine ganglion block for the treatment of postdural puncture headache in obstetric patients. J Clin Anesth. 2016;34:194–196. doi: 10.1016/j.jclinane.2016.04.009. [DOI] [PubMed] [Google Scholar]
- 3.Cohen S., Levin D., Mellender S. Topical sphenopalatine ganglion block compared with epidural blood patch for postdural puncture headache management in postpartum patients: a retrospective review. Reg Anesth Pain Med. 2018;43:880–884. doi: 10.1097/AAP.0000000000000840. [DOI] [PubMed] [Google Scholar]
- 4.Boezaart A.P. Effects of cerebrospinal fluid loss and epidural blood patch on cerebral blood flow in swine. Reg Anesth Pain Med. 2001;26:401–406. doi: 10.1053/rapm.2001.25916. [DOI] [PubMed] [Google Scholar]
- 5.Boezaart A.P., Smith C.R., Reyneke J.P. RAEducation.com LLC Publications; Gainesville, FL: 2018. Pterygopalatine ganglion block: for effective treatment of migraine, cluster headache, postdural puncture headache & postoperative pain. [Google Scholar]
- 6.Jespersen M.S., Jaeger P., Ægidius K.L. Sphenopalatine ganglion block for the treatment of postdural puncture headache: a randomised, blinded, clinical trial. Br J Anaesth. 2020;124:739–747. doi: 10.1016/j.bja.2020.02.025. [DOI] [PubMed] [Google Scholar]
- 7.COVID-19 FAQs for Providers. Society for Obstetric Anesthesia and Perinatology. Available at: https://soap.org/education/provider-education/expert-summaries/interim-considerations-for-obstetric-anesthesia-care-related-to-covid19/covid-19-faqs-for-providers/. Accessed August 21, 2020.
- 8.Olsen KR, Cometa MA, Zasimovich Y. Pterygopalatine ganglion block as a rescue technique for failed epidural blood patch. Turk J Anaesthesiol Reanim 2020;48:502–4. [DOI] [PMC free article] [PubMed]
- 9.Piagkou M., Demesticha T., Troupis T. The pterygopalatine ganglion and its role in various pain syndromes: from anatomy to clinical practice. Pain Pract. 2012;12:399–412. doi: 10.1111/j.1533-2500.2011.00507.x. [DOI] [PubMed] [Google Scholar]
- 10.Suresh S, Jagannathan N. Somatic blockade of the head and neck. In: Cousins MJ, Bridenbaugh PO, Carr DB, Horlocker TT, editors. Cousins and Bridenbaugh’s Neural Blockade in Clinical Anesthesia and Pain Medicine. 4th ed. Philadelphia: Elsevier; 2009:414.


