Abstract
Purpose
The majority of acute anterior shoulder dislocations are sustained during sports and wilderness activities. The management of acute dislocations in the pre-hospital setting is currently without guidelines based on the evidence. The study aims to assess the risk of acute complications in pre-hospital shoulder reduction and identify which pre-hospital reduction technique has the highest success rate in the published literature.
Methods
The involved databases were Allied and Complementary Medicine, CENTRAL, CINAHL, Cochrane Database of Systematic Reviews, Embase, Europe PMC, Ovid MEDLINE®, Pedro, Proquest, Trip, and World Health Organization International Clinical Trials Registry platform. Only original research of high methodological quality was included, which was defined by the recently developed assessment tool–assessing the methodological quality of published papers (AMQPP) and investigated the management of acute anterior shoulder dislocations in the pre-hospital setting.
Results
Two hundred and ninety-eight articles were identified and screened. A full text review was performed on 40 articles. Four articles published between 2015 and 2018 met the inclusion criteria. A total of 181 patients were included with the study duration ranging from 6 to 60 months. All studies reported zero immediate complication following pre-hospital reduction and there were no documented subsequent adverse events regardless of the technique used. Prompt resolution of neurological symptoms was observed following the early and successful pre-hospital reduction. First attempt success rate, when performed by skilled practitioners, ranged from 72.3% to 94.9%.
Conclusion
Pre-hospital shoulder reduction appears to be a safe and feasible option when carried out with the appropriate expertise. A novel reduction technique adapted from the mountain medicine diploma course at the University of Paris North was found to have the highest first attempt reduction success rate of 94.9%. Other techniques described in the literature included Hippocratic, Stimson's, Counter-traction and external rotation with the success rates ranging from 54% to 71.7%.
Keywords: Should dislocation, Pre-hospital reduction, Success rate, Imaging
Introduction
The glenohumeral joint is inherently one of the most unstable joints in the body. It allows for the varied range of motion required for daily activities at the expense of stability and is therefore at increased risk of dislocation. Anterior shoulder dislocations account for 90% of cases and primary acute dislocations have an incidence of 1.7% in the general population.1
Approximately 75% of acute primary dislocations are sustained during sports and wilderness activities, some of which may be appropriately managed by pre-hospital reduction.2 In this way athletes and members of the armed forces are at significantly higher risk of these injuries in comparison to the general population. Furthermore, sports activities often involve young, healthy individuals and as a result, this group forms the largest demographic for many studies assessing traumatic anterior shoulder dislocations.2,3
The majority of shoulder dislocations are treated in the emergency department. However, as these injuries occur commonly in remote and/or difficult-to-access environments, the importance of effective on-site management should not be overlooked, especially if a considerable delay to hospital transfer is anticipated.4 Less than 1% of young patients (<30 years) with anterior shoulder dislocations sustain a concomitant fracture.5 Therefore, many authors have suggested that reduction should be performed in time when trauma occurs to decrease the risk of developing neurovascular complications.2,4,6 It also has a potential to reduce the number of pre-reduction radiographs of young patients by 40%.5
The pre-hospital management of acute dislocations is currently without standards of care or best practice guidelines. There is no standardised protocol for the initial treatment of pre-hospital anterior shoulder dislocations, and thus medical expertise and clinical judgement may vary considerably.7 However, in the current literature no study has compared the pre-hospital and in-hospital reduction, the effect upon future complications and the long-term functional recovery.
The primary aim of this study was to determine the risk of acute complications when performing a pre-hospital reduction of anterior shoulder dislocations in the existing literature. The secondary aim was to identify which technique has the highest success rate and lowest complication rate in a pre-hospital environment.
Methods
A systematic literature review was performed in concordance with Preferred Reporting Items for Systematic Review and Meta-Analyses guidelines8 and was registered in the International Prospective Register of Systematic Reviews.9 The following databases were searched from inception to 19 October 2018 including Allied and Complementary Medicine, CENTRAL, CINAHL, Cochrane Database of Systematic Reviews, Embase, Europe PMC, Ovid MEDLINE®, Pedro, Proquest, Trip, and World Health Organization International Clinical Trials Registry platform. MeSH was devised using Healthcare Databases Advanced Search engine with search strategies adapted to the individual databases. Terms included shoulder, glenohumeral, subluxation, reduction, dislocation, reduction and pre-hospital.
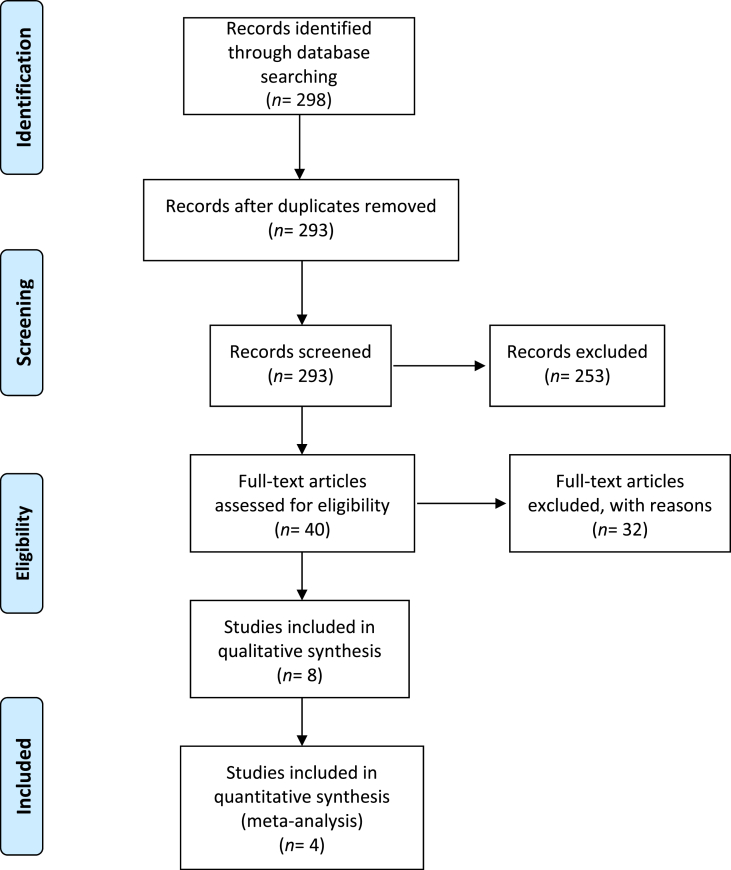
All article titles and abstracts were screened independently by two reviewers for eligibility. Forty articles underwent a full text review to assess eligibility according to our inclusion criteria (Fig. 1). Reference list of relevant reviews and selected papers were screened for further studies.
Fig. 1.
Flow diagram of article selection for the systematic review according to Preferred Reporting Items for Systematic Review and Meta-Analyses guidelines.
Inclusion and exclusion criteria
The articles included the original research investigating the management of acute anterior shoulder dislocations in the pre-hospital setting, and the outcomes related to the primary and secondary aims. Studies relating to patients with intrinsic shoulder instability were excluded. In agreement with Eljabu et al.,3 only studies considered to be of high methodological quality, defined by a minimum score of 4 out of 6 in the tool of assessing the methodological quality of published papers (AMQPP) were included.
Data collection process/calculation
Data were extracted onto an excel document in order to aid interpretation of study findings. The collected data included study design, demographics, location of reduction, reduction technique, success rates, complications, analgesic use, time to return to sport, recurrence rates and surgical intervention rates. Data extraction was validated by a second reviewer. The lead author of the relevant paper would be contacted to seek further information if the data have been collected but not reported in a study. The methodological quality of each study was evaluated using the AMQPP tool as described by Eljabu et al.3 (Table 1).
Table 1.
AMQPP assessment tool.
| AMQPP assessment | Helfen et al.10 (2015) | Ditty et al.11 (2010) | Siebenbürger et al.12 (2018) | Bokor-Billman et al.13 (2015) |
|---|---|---|---|---|
|
Yes | Yes | Yes | Yes |
|
Yes | Yes | Yes | Yes |
|
Yes | Yes | Yes | Yes |
|
Yes | Yes | Yes | Yes |
|
No | No | No | No |
|
No | No | No | No |
| Total score | 4 | 4 | 4 | 4 |
Yes = 1 point. No/Not sure = 0 point.
AMQPP: assessing the methodological quality of published papers.
Results
The literature search identified 298 articles. Of these, five duplicates were removed and 253 were rejected based upon titles. Forty articles underwent a full-text review. The final qualitative review consisted of four articles that met the inclusion criteria (Fig. 1), all of which were published between 2015 and 2018.10, 11, 12, 13 The AMQPP tool revealed that all the four articles scored 4 out of the total 6 marks available (Table 1). No study clearly identified an implementation to avoid bias. Assessor blinding was not relevant to those studies included.
A total of 181 patients were included in the four studies with an age ranging from (40.1 ± 21.3) years to (42.0 ± 16.3) years. Although no mean age was reported by Ditty et al.,11 activities performed by patients included climbing, kayaking, mountain biking and skiing, thus which implied a certain element of health and fitness within the study population. A summary of the characteristics of each study is presented in Table 2, Table 3. All studies constitute level 4 evidences according to the Oxford Centre for Evidence-Based Medicine.14
Table 2.
Summary of the included papers.
| Articles | Sample size n, age (year)a | Study duration (month) | Study design | Study location | Study aim | Study conclusion |
|---|---|---|---|---|---|---|
| Helfen et al.10 (2015) | 70, (40.2 ± 19.3) | 12 | Prospective cohort study | 16 pre-hospital rescue stations in Germany and Austria | To evaluate the feasibility of shoulder reduction in daily pre-hospital practice | There is no obvious contraindication for emergency physicians to reduce dislocated shoulders in the pre-hospital setting, as reduction is independent of pathological, neurological or vascular findings. |
| Ditty et al.11 (2010) | 39, (−) | 6 | Retrospective cohort study | Online wilderness sports forum; patients had endured injury during wilderness sports | To evaluate the success rate and complication rate for shoulder reduction attempts by non-medical personnel in the wilderness setting. | Successful shoulder reductions were reported at a rate of 71.8% despite no sedation and/or trained medical professionals on scene. |
| Siebenbürger et al.12 (2018) | 33, (40.1 ± 21.3) | 36 | Prospective cohort study | 16 pre-hospital rescue stations in Germany and Austria | To analyse the key factors associated with successful ankle, shoulder and patella joint reduction in pre-hospital emergency medicine. | The skill level and specialty type of the physician in charge determines a successful shoulder joint reduction. Overall there is a successful pre-hospital reduction rate but multiple attempts should be avoided. |
| Bokor-Billman et al.13 (2015) | 39, (42.3 ± 16.3) | 60 | Prospective cohort study | Remote areas of the Black Forest (Germany) and Vosges Mountains (France) | To present and compare a novel anterior shoulder luxation technique to the previously published series in the literature. | The novel reduction technique proposed in this study was proved effective for acute shoulder dislocation in the remote environment. |
: Mean ± SD, -: no data available.
Table 3.
A summary of technique, analgesic use and associated complications.
| Articles | Techniques | Success rate on first reduction attempt | Rate of analgesia use | Acute complication rate following reduction | Associated neurological deficit | Neurological deficit reported to improve following reduction |
|---|---|---|---|---|---|---|
| Helfen et al.10 (2015) | Hippocratic; scapula manipulation; self-reduction; and other | 54% | 95.8% | 0% | 10% | 100% |
| Ditty et al.11 (2010) | External rotation manoeuvre; Stimsons's; and Traction/Countertraction | 71.8% | – | 0% | – | – |
| Siebenbürger et al.12 (2018) | Hippocratic and other | 70% | 65% | 0% | 9% | 66% or 100%a |
| Bokor-Billman et al.13 (2015) | Unnamed technique adapted from the mountain medicine diploma course at the University of Paris North | 94.9% | 0% | 0% | – | – |
-: no data available.
: Value is a range as article data is incomplete and includes both shoulder and ankle joint dislocations. Of the eight dislocations reduced three were of the shoulder. Post reduction by Siebenbürger et al.12 stated that neurological deficit resolved in all but one of the cases however did not specify if this was at the ankle or shoulder joint.
Each study reported pre-hospital reduction techniques for anterior shoulder dislocations, and evaluated the initial success rate in reduction attempts and the associated rates of acute complications. Shoulder dislocations were sustained during a range of activities including alpine climbing, skiing, kayaking, trail running, mountain biking, rafting and hiking. Overall first attempt success rate for shoulder reduction in the pre-hospital setting ranged from 54% to 94.9%. All authors were in favour of the pre-hospital reduction manoeuvres provided by personnel with the appropriate level of skill and knowledge.
Acute complications
No acute complications following the reduction were observed in the included studies. None of the studies reported on subsequent operative intervention, long-term complications or return-to-sport phase. One study reported the frequency of subsequent transfer to hospital (97%), which was a part of the routine management.10
There were no documented neurological injuries observed by Ditty et al.11 or Bokor-Billman et al.13 Siebenbürger et al.12 found that 9% of patients suffering acute shoulder dislocation experienced a neuropraxia. Concerning the 7 cases (10%) with associated neurological complications reported by Helfen et al.,10 the reduction was performed in 4 patients, while in 3 of them no reduction was performed in the pre-hospital setting. All injury-associated neurological deficits were improved following the shoulder reduction.10
Choice of techniques
Techniques used in the pre-hospital environment over the four studies included: (1) Hippocratic manoeuvre; (2) self-reduction; (3) external rotation manoeuvre; (4) stimson's technique; (5) traction/counter-traction; (6) a novel 5-step technique described by Bokor-Billman et al.13; and (7) other unnamed techniques. The Hippocratic manoeuvre was the most commonly used technique in the patients of Helfen et al.’s research10 (60%) and Siebenbürger et al.’s research12 (65%). The highest success rate for first reduction attempts (94.9%) was observed in the study of Bokor-Billman et al.13 using their unnamed technique adapted from the mountain medicine diploma course at the University of Paris North. Both Helfen et al.10 and Siebenbürger et al.12 reported that physicians of different medical specialties have performed the reduction. Helfen et al.10 found no significant difference in the number of pre-hospital reduction attempts among different medical specialties. However, they did report that the success rate of first reduction attempts performed by surgeons (72.3%) was significantly greater than anaesthetists (35.3%) (p < 0.002). Siebenbürger et al.12 also found that compared to anaesthetists (31.1%) and other medical specialties (25%), surgeons (73.2%) have a greater success rate of first attempt reduction of the shoulder joint. Reduction techniques reported by Ditty et al.11 were all performed without the presence of trained medical professionals, including external rotation manoeuvre, Stimsons's, longitudinal traction and countertraction, which was self-reported by patients.
Analgesic use
Analgesia was used in the majority of patients in the studies of Helfen et al.10 (95%) and Siebenbürger et al.12 (65%). Three different types of analgesic therapy were observed: a 1-drug therapy (single use of Fentanyl), a 2-drug therapy (Midazolam as sedative, Ketamine or Fentanyl as anaesthetic) and a 3-drug therapy (Midazolam as sedative, Ketamine and Fentanyl as anaesthetic). There was no significant correlation between pain (p = 0.161) and success of reduction (p = 0.09), with the choice of analgesic medication.12 There was no documentation of analgesia use reported by Ditty et al.11 Bokor-Billman et al.13 actively excluded the use of analgesia, because of patient's report of a low pain score (visual analog scale, 1.7 ± 1.4).
Discussion
This systematic review has identified that based on current available literature, pre-hospital reduction of acute anterior dislocation of the shoulder in the active population resulted in no adverse outcomes. Studies meeting the inclusion criteria for this review were situated in pre-hospital environments, and therefore all inferences are made in relation to this environment.
Acute complications
When performing a reduction of an anterior shoulder dislocation in the pre-hospital environment, no acute complications were reported in the current literature. All studies reported zero immediate complication following the reduction and no subsequent adverse events regardless of the technique used. In comparison, a recent Cochrane review by Hanchard et al.15 featuring 4 randomised controlled trials using in-hospital reduction techniques reported an incidence of adverse events ranging from 1% to 8%.15, 16, 17, 18 In-hospital reduction techniques observed in the review comprised the Hippocratic method, the external rotation method, Kocher method, the Stimson method and elevation method. Reported adverse events included hyperaesthesia, axillary rash and limited range of movement. The overall age range of patients in the review was 12–90 years. It included patients from both active and sedentary backgrounds and excluded non-traumatic injuries.15 Although there is the limited evidence, it is impossible to conclude superior safety of reduction in one environment over another, until further evidence from randomised controlled trials. The findings of the current review suggest that pre-hospital reduction does not result in an increased risk of acute complications in the active population, which merits further researches.
This review also identified, in a small sample size, that following early pre-hospital shoulder reduction there was prompt resolutions of neurological symptoms. Siebenbürger et al.12 and Helfen et al.10 identified 9 cases of neurological compromise, of which 8 were resolved within 24 h following the successful pre-hospital reduction. In comparison, Finestone et al.16 reported a recovery time of up to 10 weeks in 51 patients sustaining a neuropraxia associated with a shoulder dislocation that was subsequently reduced in-hospital. Prolonged neurological compromise increases the risk of long-term nerve damage, and therefore an early pre-hospital reduction by trained individuals may be more favourable than delaying for hospital transfer. However, in the event of severe neurovascular damage noted by a pulseless distal limb, inability to activate muscle fibres, and complete loss of sensation in the limb, immediate transportation to an emergency facility is recommended.6
Although acute fractures do not frequently occur as a result of correctly performed reduction attempts, they can be associated with the initial trauma to the shoulder.10,12, 13, 14, 15 Concomitant fractures result in a lower first attempt success rate for shoulder reduction and may require special consideration in order to prevent distraction of previously minimally displaced fragments.19 The most common predisposing factor for such bony pathology is the age of patient.20 Less than 1% of patients in their second and third decade of life with shoulder dislocations have an associated fracture.21 In patients over 40, the incidence of humeral fractures is significantly higher.20,22 Such fractures have been described as making it both impossible and dangerous to manipulate the humeral head by holding the humeral shaft.23 For example a surgical neck fracture of the humeral head would contraindicate closed reduction attempts due to the increased likelihood of displacing the fracture and causing neurovascular damage. Conversely, as these fractures are less common in younger age groups, a number of authors described that pre-reduction radiographs was unnecessary for patients less than 40 years.19
Solovyova et al.24 recently performed a retrospective study of 150 anterior shoulder dislocations across two level 1 trauma centres concluding that closed-reduction was safe even in the setting of fracture-dislocation. It supports the notion that pre-reduction radiographs are of little therapeutic benefit in the presence of a firm clinical diagnosis and should not be considered as a prerequisite for all patients. It should be noted that not all lesions seen on radiographs will be of concern nor should impede attempts at reduction. For example, Hill-Sachs lesions and bony Bankart lesions occur in 90% and 24% of the population respectively, which do not impact on the decision to reduce the shoulder in the acute setting.25,26
Choice of techniques
Several pre-hospital reduction techniques are reported in the literature. Overall first attempt success rate observed across the four studies, irrespective of technique, range from 54% to 94.9%. Not all patients included however underwent a pre-hospital reduction attempt. It was based on clinician judgement, considering the type of sport,11 mechanism of injury and associated injuries.12
The Hippocratic method was utilised in the researches of Helfen et al.10 and Siebenberger et al.,12 in 60% and 65% of cases respectively. It correlates with the high usage rate (61%) in hospital settings.18 Despite there are advances in radiological imaging and shoulder surgery, potential dangers to traditionally approaches are shown, such as the Hippocratic and Kocher methods.27 The Hippocratic method involves traction applied to the arm in 45° of abduction, with a sheet or foot placed in the axilla to provide counter traction, which puts the brachial plexus, axillary vessels and humeral head at a significant risk of injury.28, 29, 30, 31, 32
In contrast alternative techniques such as the Stimson method and the novel technique described by Bokor-Billman et al.13 have some advantages. The Stimson method is simple with few documented complications, which has been recommended for use in off-field and pitch-side management.2,6 The patient is lying prone with the affected arm hanging down in forward flexion and a weight applied to the wrist.33 It was reported a 72% success rate used by non-medical personnel in Ditty et al.’s study.11 Meanwhile, Bokor-Billman et al.13 described a technique adapted from the Mountain Medicine University that had a 94.9% first reduction attempt success rate and no associated acute complications despite using no sedation. Three trained rescue physicians who had no prior experience of the technique performed this manoeuvre. The head of the humerus is rotated into a position to maximise the chance of sliding over the scapula border, while the patient remains in a seated straight-back position.13
Shoulder injuries are complex, and thus multiple reduction techniques exist. Confidence and familiarity are important determinants of reduction success.34 Surgeons were noted to have a higher success rate compared with other specialties in two studies.10,12 The variation in first attempt success rate was described by Helfen et al.10 due to the different “level of skill” in those performing the manoeuvre. It is supported by Siebenbürger et al.12 that upon self-assessment of skill using a Likert scale, surgeons were scored higher than anaesthetists and other medical professionals. When only considering the reduction attempts performed by the skilled practitioners in the reduction technique, the first attempt success rate ranges from 72.3% to 94.9% in the pre-hospital setting.
Analgesic use
Success in reducing a dislocated shoulder can be significantly improved by overcoming pain-related muscle spasm.2,21,34 The longer the muscle is left in spasm, the more difficult it can be to provide adequate relaxation for the successful reduction. Most patients undergoing in-hospital reduction will therefore receive a combination of analgesia and sedation. This was replicated in the reports of Siebenberger et al.12 and Helfen et al.10, in which combinations of midazolam, fentanyl and ketamine were administered in most patients. Shoulder reduction rates were found to be equal between the different regimens. Midazolam, fentanyl and ketamine, however, come with significant risks such as airway and respiratory compromise. In the limited resource pre-hospital setting, it may be impossible to administer these drugs safely. This may impact on the safety profile that Siebenberger et al.12 and Helfen et al.10 reported for pre-hospital reduction. However, it has previously been shown that early shoulder reduction can be performed successfully without analgesia partly due to avoiding muscle spasm developing.27,35 The current review has identified that patients treated without analgesia had comparable success rates to those treated with analgesia.12,36 Further to this, Bokor-Billman et al.13 used no analgesia and reported the highest first attempt success rate. This suggests pre-hospital shoulder reduction without sedation is a viable option.
Patient functional outcome
Unfortunately there was no documented data on the rates of recurrence, surgical requirement or return to sport in any of the four studies. In a recent systematic review by Norte et al.,7 early reduction was to decrease the stress on neurovascular structures and the muscle spasm, and thereby minimise humeral head defects in locked dislocations. This is supported by Kanji et al.37 who reported that every interval delay of 710 min between injury and intravenous sedation increased the odds of a failed reduction by 7%. It has also been suggested that an earlier successful shoulder reduction reduces the risk of an unstable joint, and thus the likelihood of requiring later operative management will be decreased.13,19 In this way it is possible that early pre-hospital reduction may decrease the recurrence rates and have a positive impact on the return of strength and joint movement by limiting the development of muscle spasm. It should be considered alongside other risk factors for recurrence, including the age at initial dislocation.,3,7,19 high energy trauma3 and bony involvement.13 There is level 4 case series evidence and level 5 expert opinion to suggest that a return to sport is permissible when the range of motion and strength are near normal.3 This would support the idea that early pre-hospital pitch-side reduction could be favourable to athletes aiming to accelerate their return to sport.
Financial implications
Reduction in the emergency department has impact on costs of clinician time, use of imaging, conscious sedation and possibility of hospital admission.23 Increasing time to reduction is likely to result in higher analgesia requirements to overcome muscle spasm and a greater number of attempts to achieve a closed reduction. Multiple unsuccessful attempts may necessitate surgical intervention, and therefore impose additional theatre costs as well as the cost for further follow-up appointments and prolonged physiotherapy.19 Furthermore, if pre-reduction radiographs for patients in the second and third decades of life were omitted, the total number of radiographs may be reduced by 40% in this population, which has beneficial impact on the health as well as cost.24 It is therefore important for clinicians to consider these factors during the process of making decisions.
Despite having the comprehensive literature search, very few eligible studies were identified. No randomised controlled trials have been conducted investigating pre-hospital shoulder reduction relative to in-hospital reduction methods. Where information was missing from studies, no additional data was obtained from trial authors after being contacted directly. The studies primarily included young active adults, and therefore the findings should not be applied to an elderly or sedentary population. It was also not possible to directly compare the acute complication rates of in-hospital reduction techniques and pre-hospital techniques due to a lack of existing evidence. Lack of data may explain why recognised protocols and guidelines for shoulder reduction in a pre-hospital environment are not commonplace.30
Conclusion
With an appropriate clinical judgement and correct expertise, the reduction of an anterior shoulder dislocation in a young, active patient is a safe and viable option in the pre-hospital environment. This review has identified that the presence of acute neurological deficit does not preclude safe reduction and is associated with early symptom resolution. The technique outlined by Bokor-Billman et al.13 is noted to have a high first-attempt success rate with no recorded complications despite being performed without analgesia. Further research into the benefits of pre-hospital versus in-hospital reduction of anterior shoulder dislocations and the long-term outcomes, would add the evidence and guide the development of reduction protocols aimed at improving patient care.
Funding
Nil.
Acknowledgements
Gill Rose BSc (Econ) MCLIP for the extensive literature search performed at Stoke Mandeville Hospital, Buckinghamshire NHS Trust. We would also like to acknowledge Mr Venkat Gade for his support.
Ethical Statement
Nil.
Declaration of Competing Interest
There are no conflicts of interest associated with this article.
Footnotes
Peer review under responsibility of Chinese Medical Association.
References
- 1.Romeo A.A., Cohen B.S., Carreira D.S. Traumatic anterior shoulder instability. Orthop Clin N Am. 2001;32:399–409. doi: 10.1016/s0030-5898(05)70209-1. [DOI] [PubMed] [Google Scholar]
- 2.Shah R., Chhaniyara P., Wallace W.A. Pitch-side management of acute shoulder dislocations: a conceptual review. BMJ Open Sport Exerc Med. 2017;2 doi: 10.1136/bmjsem-2016-000116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Eljabu W., Klinger H.M., Knoch Mvon. The natural course of shoulder instability and treatment trends: a systematic review. J Orthop Traumatol. 2017;18:1–8. doi: 10.1007/s10195-016-0424-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Longo U.G., Loppini M., Rizzello G. Management of primary acute anterior shoulder dislocation: systematic review and quantitative synthesis of the literature. Arthroscopy. 2014;30:506–522. doi: 10.1016/j.arthro.2014.01.003. [DOI] [PubMed] [Google Scholar]
- 5.DeVries J.G., Berlet G.C. Understanding levels of evidence for scientific communication. Foot Ankle Spec. 2010;3:205–209. doi: 10.1177/1938640010375184. [DOI] [PubMed] [Google Scholar]
- 6.Orloski J., Eskin B., Allegra P.C. Do all patients with shoulder dislocations need prereduction x-rays? Am J Emerg Med. 2011;29:609–612. doi: 10.1016/j.ajem.2010.01.005. [DOI] [PubMed] [Google Scholar]
- 7.Norte G.E., West A., Gnacinski M. On-field management of the acute anterior glenohumeral dislocation. Physician Sportsmed. 2011;39:151–162. doi: 10.3810/psm.2011.09.1931. [DOI] [PubMed] [Google Scholar]
- 8.Moher D., Liberati A., Tetzlaff J. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8:336–341. doi: 10.1016/j.ijsu.2010.02.007. [DOI] [PubMed] [Google Scholar]
- 9.Gourbault L., Fennelly J., Neal-Smith G. A systematic review of prehospital relocation techniques for anterior shoulder dislocations and the effect on patient return to function. http://www.crd.york.ac.uk/PROSPERO/display_record.php?ID=CRD42019120247 [DOI] [PMC free article] [PubMed]
- 10.Helfen T., Ockert B., Pozder P. Management of prehospital shoulder dislocation: feasibility and need of reduction. Eur J Trauma Emerg Surg. 2016;42:357–362. doi: 10.1007/s00068-015-0545-5. [DOI] [PubMed] [Google Scholar]
- 11.Ditty J., Chisholm D., Davis S.M. Safety and efficacy of attempts to reduce shoulder dislocations by non-medical personnel in the wilderness setting. Wilderness Environ Med. 2010;21:357–361. doi: 10.1016/j.wem.2010.06.010. e2. [DOI] [PubMed] [Google Scholar]
- 12.Siebenbürger G., Zeckey C., Fürmetz J. Medical speciality, medication or skills: key factors of prehospital joint reduction. A prospective, multicenter cohort study. Eur J Trauma Emerg Surg. 2018;44:637–642. doi: 10.1007/s00068-018-0933-8. [DOI] [PubMed] [Google Scholar]
- 13.Bokor-Billmann T., Lapshyn H., Kiffner E. Reduction of acute shoulder dislocations in a remote environment: a prospective multicenter observational study. Wilderness Environ Med. 2015;26:395–400. doi: 10.1016/j.wem.2014.12.027. [DOI] [PubMed] [Google Scholar]
- 14.Lebus G.F., Raynor M.B., Nwosu S.K. Predictors for surgery in shoulder instability: a retrospective cohort study using the FEDS system. Orthop J Sports Med. 2015;3 doi: 10.1177/2325967115607434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hanchard N.C.A., Goodchild L.M., Kottam L. Conservative management following closed reduction of traumatic anterior dislocation of the shoulder. Cochrane Database Syst Rev. 2014;4 doi: 10.1002/14651858.CD004962.pub3. [DOI] [PubMed] [Google Scholar]
- 16.Finestone A., Milgrom C., Radeva-Petrova D.R. Bracing in external rotation for traumatic anterior dislocation of the shoulder. J Bone Joint Surg Br. 2009;91:918–921. doi: 10.1302/0301-620X.91B7.22263. [DOI] [PubMed] [Google Scholar]
- 17.Itoi E., Hatakeyama Y., Sato T. Immobilization in external rotation after shoulder dislocation reduces the risk of recurrence. A randomized controlled trial. J Bone Joint Surg Am. 2007;89:2124–2131. doi: 10.2106/JBJS.F.00654. [DOI] [PubMed] [Google Scholar]
- 18.Taşkoparan H., Kılınçoğlu V., Tunay S. Immobilization of the shoulder in external rotation for prevention of recurrence in acute anterior dislocation. Acta Orthop Traumatol Turcica. 2010;44:278–284. doi: 10.3944/AOTT.2010.2274. [DOI] [PubMed] [Google Scholar]
- 19.Vermeiren J., Handelberg F., Casteleyn P.P. The rate of recurrence of traumatic anterior dislocation of the shoulder. Int Orthop. 1993;17:337–341. doi: 10.1007/BF00180449. [DOI] [PubMed] [Google Scholar]
- 20.Emond M., Le Sage N., Lavoie A. Clinical factors predicting fractures associated with an anterior shoulder dislocation. Acad Emerg Med. 2004;11:853–858. doi: 10.1111/j.1553-2712.2004.tb00768.x. [DOI] [PubMed] [Google Scholar]
- 21.Aronson P.L., Mistry R.D. Intra-articular lidocaine for reduction of shoulder dislocation. Pediatr Emerg Care. 2014;30:358–362. doi: 10.1097/PEC.0000000000000131. quiz 363-365. [DOI] [PubMed] [Google Scholar]
- 22.Perron A.D., Ingerski M.S., Brady W.J. Acute complications associated with shoulder dislocation at an academic emergency department. J Emerg Med. 2003;24:141–145. doi: 10.1016/s0736-4679(02)00717-5. [DOI] [PubMed] [Google Scholar]
- 23.Cutts S., Prempeh M., Drew S. Anterior shoulder dislocation. Ann R Coll Surg Engl. 2009;91:2–7. doi: 10.1308/003588409X359123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Solovyova O., Shakked R., Tejwani N.C. Should all shoulder dislocations be closed reduced? assessment of risk of iatrogenic injury in 150 patients. Iowa Orthop J. 2017;37:47–52. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5508270/ [PMC free article] [PubMed] [Google Scholar]
- 25.Kim D.-S., Yoon Y.-S., Yi C.H. Prevalence comparison of accompanying lesions between primary and recurrent anterior dislocation in the shoulder. Am J Sports Med. 2010;38:2071–2076. doi: 10.1177/0363546510371607. [DOI] [PubMed] [Google Scholar]
- 26.Taylor D.C., Arciero R.A. Pathologic changes associated with shoulder dislocations. Arthroscopic and physical examination findings in first-time, traumatic anterior dislocations. Am J Sports Med. 1997;25:306–311. doi: 10.1177/036354659702500306. [DOI] [PubMed] [Google Scholar]
- 27.Dala-Ali B., Penna M., McConnell J. Management of acute anterior shoulder dislocation. Br J Sports Med. 2014;48:1209–1215. doi: 10.1136/bjsports-2012-091300. [DOI] [PubMed] [Google Scholar]
- 28.Maliński B., Palka J., Rykowski H. Rupture of axillary artery during reduction of a dislocated shoulder joint. Chir Narzadow Ruchu Ortop Pol. 1975;40:433–435. [PubMed] [Google Scholar]
- 29.Regauer M., Polzer H., Mutschler W. Neurovascular complications due to the Hippocrates method for reducing anterior shoulder dislocations. World J Orthoped. 2014;5:57–61. doi: 10.5312/wjo.v5.i1.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schmal H., Strohm P.C., Rosahl S.K. Rupture of the arteria subscapularis following reduction of an anterior shoulder dislocation. Unfallchirurg. 2006;109:153–155. doi: 10.1007/s00113-005-0983-3. [DOI] [PubMed] [Google Scholar]
- 31.te Slaa R.L., Wijffels M.P.J.M., Marti R.K. Questionnaire reveals variations in the management of acute first time shoulder dislocations in The Netherlands. Eur J Emerg Med. 2003;10:58–61. doi: 10.1097/00063110-200303000-00015. [DOI] [PubMed] [Google Scholar]
- 32.Zanchetta M., Rigatelli G., Dimopoulos K. Endoluminal repair of axillary artery and vein rupture after reduction of shoulder dislocation. A case report. Minerva Cardioangiol. 2002;50:69–73. [PubMed] [Google Scholar]
- 33.Riebel G.D., McCabe J.B. Anterior shoulder dislocation: a review of reduction techniques. Am J Emerg Med. 1991;9:180–188. doi: 10.1016/0735-6757(91)90187-o. [DOI] [PubMed] [Google Scholar]
- 34.Kuhn J.E. Treating the initial anterior shoulder dislocation–an evidence-based medicine approach. Sports Med Arthrosc Rev. 2006;14:192–198. doi: 10.1097/01.jsa.0000212328.25345.de. [DOI] [PubMed] [Google Scholar]
- 35.Tajima K., Nishida Y., Shimizu C. Double traction method–an easy and safe reduction method for anterior shoulder dislocations, even for non-orthopedic surgeons. Acute Med Surg. 2015;3:272–275. doi: 10.1002/ams2.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hovelius L., Augustini B.G., Fredin H. Primary anterior dislocation of the shoulder in young patients. A ten-year prospective study. J Bone Joint Surg Am. 1996;78:1677–1684. doi: 10.2106/00004623-199611000-00006. [DOI] [PubMed] [Google Scholar]
- 37.Kanji A., Atkinson P., Fraser J. Delays to initial reduction attempt are associated with higher failure rates in anterior shoulder dislocation: a retrospective analysis of factors affecting reduction failure. Emerg Med J. 2016;33:130–133. doi: 10.1136/emermed-2015-204746. [DOI] [PubMed] [Google Scholar]