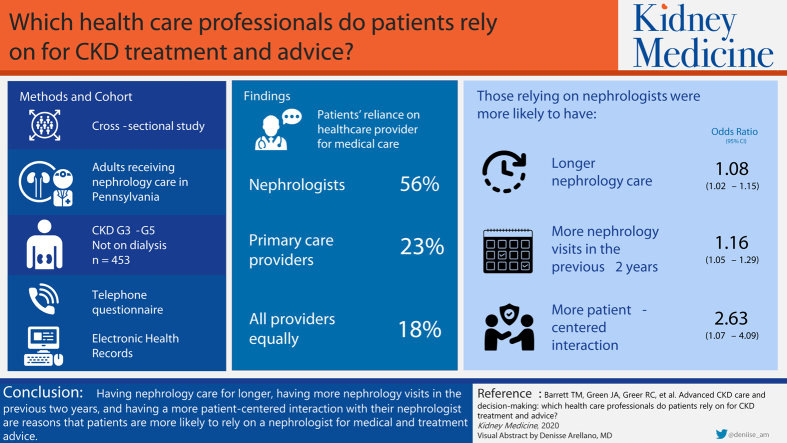
Graphical Abstract
Index Words: Chronic kidney disease, patient-centeredness, fragmented care, patient-provider communication, nephrology care
Abstract
Rationale & Objective
Chronic kidney disease (CKD) care is often fragmented across multiple health care providers. It is unclear whether patients rely mostly on their nephrologists or non-nephrologist providers for medical care, including CKD treatment and advice.
Study Design
Cross-sectional study.
Setting & Participants
Adults receiving nephrology care at CKD clinics in Pennsylvania.
Predictors
Frequency, duration, and patient-centeredness (range, 1 [least] to 4 [most]) of participants’ nephrology care.
Outcome
Participants’ reliance on nephrologists, primary care providers, or other specialists for medical care, including CKD treatment and advice.
Analytical Approach
Multivariable logistic regression to quantify associations between participants’ reliance on their nephrologists (vs other providers) and their demographics, comorbid conditions, kidney function, and nephrology care.
Results
Among 1,412 patients in clinics targeted for the study, 676 (48%) participated. Among these, 453 (67%) were eligible for this analysis. Mean age was 71 (SD, 12) years, 59% were women, 97% were white, and 65% were retired. Participants were in nephrology care for a median of 3.8 (IQR, 2.0-6.6) years and completed a median of 4 (IQR, 3-5) nephrology appointments in the past 2 years. Half (56%) the participants relied primarily on their nephrologists, while 23% relied on primary care providers, 18% relied on all providers equally, and 3% relied on other specialists. Participants’ adjusted odds of relying on their nephrologists were higher for those in nephrology care for longer (OR, 1.08 [95% CI, 1.02-1.15]; P = 0.02), those who completed more nephrology visits in the previous 2 years (OR, 1.16 [95% CI, 1.05-1.29]; P = 0.005), and those who perceived their last interaction with their nephrologists as more patient-centered (OR, 2.63 [95% CI, 1.70-4.09]; P < 0.001).
Limitations
Single health system study.
Conclusions
Many nephrology patients relied on non-nephrologist providers for medical care. Longitudinal patient-centered nephrology care may encourage more patients to follow nephrologists’ recommendations.
Plain-Language Summary.
Patients with chronic kidney disease (CKD) often see multiple health care providers, but little is known about how they prioritize the information they receive from these providers. We asked 453 patients with advanced CKD if they rely mostly on their nephrologists or other providers for their medical care, including CKD treatment and advice. Half the participants reported that they relied primarily on their nephrologists for medical care. Those who were in nephrology care for longer, completed more nephrology appointments in the past 2 years, and perceived their last nephrology visits as more patient-centered had higher odds of relying primarily on their nephrologists for medical care. Establishing long-term patient-centered nephrology care may help ensure that patients receive optimal CKD treatment and advice.
Editorial, p. 511
Patients with chronic kidney disease (CKD) often have multiple comorbid conditions,1 requiring them to interact with nephrologists and non-nephrologist health care providers. As a result, CKD care can be fragmented, and patients may receive conflicting treatment information.2,3 Previous studies show that non-nephrologist health care providers may have limited knowledge of CKD and may fail to follow CKD clinical practice guidelines.4, 5, 6, 7 However, non-nephrologists, especially primary care providers (PCPs), encounter barriers when they attempt to comanage patients alongside nephrologists, such as delays in delivery of nephrologists’ consultation notes.8
These communication barriers may affect patient outcomes. For example, patients’ adherence to recommended treatments for CKD risk factors, such as diabetes and hypertension, is often suboptimal.9, 10, 11, 12 Poor adherence may in part be attributable to communication challenges in which advice from multiple health care providers is not coordinated or synchronized. Recent evidence also suggests that nephrologists may be missing key discussions with their patients who have not yet started kidney replacement therapy, such as discussing their preferences for end-of-life care.13 When patients with CKD receive care from multiple health care providers, it is unclear how they prioritize multiple sources of information. Understanding how patients with CKD prioritize medical treatment and advice from multiple providers could inform efforts to improve health care providers’ coordination and elucidate mechanisms that could help optimize multidisciplinary care strategies.
We conducted a cross-sectional study among patients receiving longitudinal nephrology care in CKD clinics to better understand their reliance on nephrologists versus other health care providers for their medical care, including treatment and advice for CKD. We also sought to identify clinical factors and aspects of CKD care that could influence patients’ likelihood of relying on their nephrologists’ recommendations.
Methods
Study Design and Participants
We conducted a cross-sectional study using data collected in 2017 as part of the PREPARE NOW trial. PREPARE NOW (NCT 02722382) is an ongoing cluster randomized controlled trial examining the effectiveness of a multifaceted intervention to improve shared and informed decision making in the care of patients with CKD.14 Individuals were eligible for the PREPARE NOW trial if they had advanced kidney disease, according to the Kidney Disease: Improving Global Outcomes (KDIGO) guidelines (ie, those with stages G3aA3, G3bA2-A3, G4A1-A3, and G5A1-A3 based on estimated glomerular filtration rate and albuminuria),15 had not started kidney replacement therapy, were English speaking, and were older than 18 years.14 Study participants completed a standard telephone questionnaire administered by trained research staff that was not tied to a specific visit to the CKD clinic. They also provided consent to obtain their electronic health records (EHRs). All study protocols were approved by the Duke University Institutional Review Board (IRB), which serves as a Central IRB for PREPARE NOW (IRB approval number Pro00075488) .
Study Setting
The Geisinger Health System provides care for approximately 4.2 million people in 45 counties in Pennsylvania and 7 counties in southern New Jersey. Within the health system, 9 clinical practice sites provide outpatient nephrology care to approximately 4,000 patients with CKD. Each clinic has between 1 and 3 nephrology providers, with some providers practicing in multiple clinics. Seven nephrologists and 1 physician assistant were practicing at the PREPARE NOW study sites. Participants typically saw 1 nephrologist but may have occasionally visited a second. Study participants were under the care of approximately 235 PCPs, and PCPs do not receive system-wide CKD training at Geisinger other than best practice alerts and Anticipatory Management Program care gap reports. Geisinger Health Plan provides insurance coverage for approximately one-third of all patients receiving care in the Geisinger Health System and provides nurse care management for patients with complex chronic illnesses, including CKD.
Participant Sociodemographic Characteristics
Participants reported their age, sex, race/ethnicity, education, employment, and household income by telephone questionnaire. We assessed participants’ insurance status using EHR data. We characterized participants’ education as less than high school, high school graduate/general equivalency diploma, or college graduate. We characterized employment as working/looking for work, unemployed, retired due to disability, or retired. We characterized yearly household income as <$30,000; $30,000 to $59,999; or ≥$60,000.
Participant Kidney Function and Comorbid Conditions
We assessed participants’ comorbid conditions and kidney function using EHR data. We ascertained their estimated glomerular filtration rates using the most recently available value in the EHR before administering the questionnaire. Estimated glomerular filtration rate values in the EHR were estimated based on the CKD Epidemiology Collaboration (CKD-EPI) equation.16 We also assessed whether participants had cardiovascular disease or diabetes diagnosed using EHR data. We assessed comorbid condition burden using the Charlson Comorbidity Index (ranging from 0 [lowest comorbidity] to 37 [highest comorbidity]).17
Participants’ Nephrology Care, Care by Other Providers, and Reliance on Nephrologists
We estimated the time that participants had been under the care of their nephrologists based on the date of their first nephrology visit at the Geisinger Health System that was recorded in the EHR. We also asked participants to report the frequency of their nephrology visits with the question, “How often do you see your kidney doctor?” (possible answers: “at least once a month,” “at least every 2 months,” “at least every 3 months,” “at least every 6 months,” “once a year,” “whenever you have a problem,” and “don’t know”). We ascertained participants’ number of completed appointments with both nephrology and primary care within the past 2 years from the EHR.
To assess participants’ care by non-nephrologist health care providers, we asked them, “Besides a kidney doctor, do you currently have a regular doctor or other primary care doctor (such as a physician assistant or nurse) who you see for check-ups, illnesses, and concerns about your health?” (possible answers: “yes” or “no”). We also asked them, “Are you currently seeing any other doctors besides a kidney doctor or primary care doctor? For example, this could be a doctor to treat heart disease, diabetes, your prostate, women’s health issues such as Pap smears, or a transplant surgeon.” (possible answers: “yes” or “no”).
To ascertain which of their health care providers that participants relied on most for medical care, including CKD treatment and advice, we asked, “Between your kidney doctor, your primary care doctor, and your other doctors, which doctor do you most heavily rely on for care of your medical problems and for medical advice about your kidney disease and kidney treatment? Would you say mostly your kidney doctor, mostly your primary care doctor, mostly another doctor, or that you rely on your doctors fairly equally?”
Participants’ Perceived Patient-Centeredness of Nephrology Care
We asked participants to assess the patient-centeredness of their last visit with their nephrologist using questions adapted from the Patient Perception of Patient Centeredness scale, which has been validated in primary care and deployed in other settings.18,19 Participants were asked to “Think back to your last visit with your kidney doctor” and answer the following 5 questions: (1) “To what extent was your main problem(s) discussed during your last visit with your kidney doctor?” (possible answers: “not at all,” “a little,” “mostly,” and “completely”), (2) “Would you say that your kidney doctor knew that this was one of your reasons for coming in during the visit? (possible answers: “no,” “don’t know,” “maybe,” and “yes”), (3) “To what extent did your kidney doctor understand the importance of your reason for the visit?” (possible answers: “not at all,” “a little,” “mostly,” and “completely”), (4) “How well do you think your kidney doctor understood you during the visit?” (possible answers: “not at all,” “a little,” “mostly,” and “completely”), and (5) “How much would you say that your kidney doctor cares about you as a person?” (possible answers: “not at all,” “a little,” “mostly,” and “completely”). We then assigned participants’ responses to each question a value ranging from 1 (“not at all” or “no”) to 4 (“completely” or “yes”) and averaged the values across all 5 questions to create a composite Patient Perception of Patient Centeredness score ranging from 1 to 4, with 4 representing the highest degree of perceived patient-centeredness.18
Statistical Analysis
Our analysis was limited to individuals who reported which provider they primarily rely on for medical care. We described participants’ sociodemographic, clinical, and nephrology care characteristics both among all study participants and according to their reported reliance on nephrologists versus other providers. We constructed a multivariable logistic regression model to assess associations of participants’ sociodemographic characteristics, CKD stage, Charlson Comorbidity Index score, number of completed nephrology and primary care appointments in the past 2 years, time in nephrology care, and perceived patient-centeredness with their reliance on nephrologists versus other providers for medical care, including CKD treatment and advice.
In post hoc analyses, we constructed 5 separate multivariable logistic regression models to assess the associations between participants’ scores on each Patient Perception of Patient Centeredness scale question and their reliance on nephrologists versus other providers for their medical care, including CKD treatment and advice. These models adjusted for participants’ sociodemographic, clinical, and nephrology care characteristics. All hypothesis tests were 2 sided at the 0.05 significance level, and all analyses were performed using SAS, version 9.4 (SAS Institute).
Results
Participant Sociodemographic and Clinical Characteristics
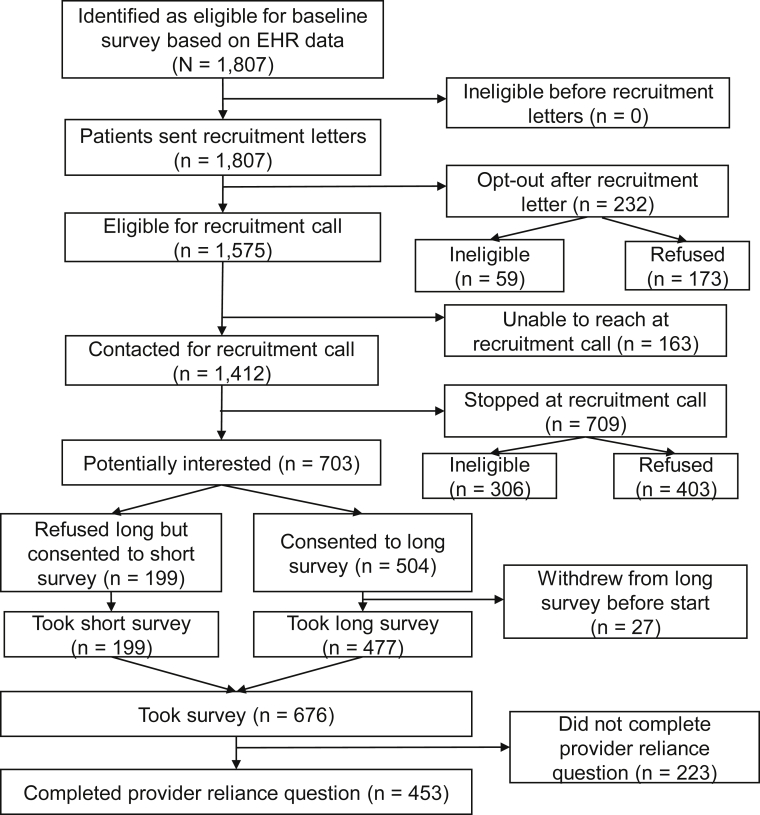
A total of 1,807 individuals were identified as potentially eligible for our study based on EHR data. Among these, we attempted to contact 1,412 individuals. Of these, 676 (48%) completed a questionnaire. Among all participants completing a questionnaire, 477 (71%) completed the long questionnaire, and 453 (67%) reported which provider they primarily rely on for medical care and were included in this analysis (Fig 1). Participants (n = 453) had a mean age of 71 (SD, 12) years. Most (59%) were women, white (97%), high school graduates (66%), retired (65%), and insured through Medicare (70%). Approximately one-third (32%) were low income (household income < $30,000 per year). Among all participants, most had stage 4 (35%), 3b (45%), or 3a (12%) CKD. Few participants had stage 5 (6%) or 2 (2%) CKD. Median Charlson Comorbidity Index score was 5 (interquartile range [IQR], 3-7). Nearly half of all participants had had cardiovascular disease (48%) and diabetes (57%; Table 1) diagnosed. Compared with participants who completed only the short questionnaire, those included in the analysis who completed the long questionnaire were younger, more educated, and more likely to have commercial insurance and had a higher prevalence of cardiovascular disease (Table S1).
Figure 1.
Study flow diagram describes steps to analytical sample. Abbreviation: EHR, electronic health record.
Table 1.
Participant Characteristics Stratified by the Provider They Primarily Relied on for Medical Care, Including CKD Treatment and Advice
| Characteristics | Overall (n = 453) | Nephrologist (n = 253) | PCP (n = 104) | Other Specialist (n = 14) | All Providers Equally (n = 82) |
|---|---|---|---|---|---|
| Sociodemographic Characteristics | |||||
| Age, y | 71 (12) | 70 (12) | 73 (11) | 75 (10) | 71 (13) |
| Sex | |||||
| Women | 266 (59%) | 148 (59%) | 63 (61%) | 4 (29%) | 51 (62%) |
| Men | 187 (41%) | 105 (41%) | 41 (39%) | 10 (71%) | 31 (38%) |
| Race/ethnicity | |||||
| White | 438 (97%) | 242 (96%) | 102 (98%) | 14 (100%) | 80 (98%) |
| Other race/ethnicity | 13 (3%) | 11 (4%) | 1 (1%) | 0 (0%) | 1 (1%) |
| Do not know | 2 (0.4%) | 0 (0%) | 1 (1%) | 0 (0%) | 1 (1%) |
| Income | |||||
| <$30,000 | 146 (32%) | 73 (29%) | 37 (36%) | 7 (50%) | 29 (35%) |
| $30,000-$59,999 | 114 (25%) | 64 (25%) | 27 (26%) | 4 (27%) | 19 (23%) |
| ≥$60,000 | 82 (18%) | 58 (23%) | 10 (10%) | 1 (7%) | 13 (16%) |
| Missing/refused/do not know | 111 (25%) | 58 (23%) | 30 (29%) | 2 (14%) | 21 (26%) |
| Education | |||||
| <High school | 58 (13%) | 26 (10%) | 15 (14%) | 4 (29%) | 13 (16%) |
| High school graduate/GED | 301 (66%) | 164 (65%) | 74 (71%) | 8 (57%) | 55 (67%) |
| College graduate | 90 (20%) | 62 (25%) | 15 (14%) | 1 (7%) | 12 (15%) |
| Missing/refused/do not know | 4 (0.9%) | 1 (0.4%) | 0 (0%) | 1 (7%) | 2 (2%) |
| Employment | |||||
| Working/looking for work | 85 (19%) | 56 (22%) | 15 (14%) | 1 (7%) | 13 (16%) |
| Unemployed | 4 (0.9%) | 3 (1%) | 1 (1%) | 0 (0%) | 0 (0%) |
| Retired due to disability | 59 (13%) | 24 (10%) | 17 (16%) | 2 (14%) | 16 (20%) |
| Retired | 295 (65%) | 164 (65%) | 68 (65%) | 11 (79%) | 52 (63%) |
| Missing/refused/do not know | 10 (2%) | 6 (2%) | 3 (3%) | 0 (0%) | 1 (1%) |
| Insurance | |||||
| Commercial | 98 (22%) | 59 (23%) | 21 (20%) | 2 (14%) | 16 (20%) |
| Government/other | 4 (0.9%) | 4 (2%) | 0 (0%) | 0 (0%) | 0 (0%) |
| Medicaid | 35 (8%) | 17 (7%) | 9 (9%) | 1 (7%) | 8 (10%) |
| Medicare | 316 (70%) | 173 (68%) | 74 (71%) | 11 (79%) | 58 (71%) |
| Clinical Characteristics | |||||
| eGFR, mL/min/1.73 m2 | 33 (12) | 33 (12) | 33 (11) | 33 (10) | 35 (12) |
| CKD stage | |||||
| Stage 2 (eGFR = 60) | 9 (2%) | 5 (2%) | 1 (1%) | 0 (0%) | 3 (4%) |
| Stage 3a (60 > eGFR ≥ 45) | 56 (12%) | 30 (12%) | 14 (14%) | 1 (7%) | 11 (13%) |
| Stage 3b (45 > eGFR ≥ 30) | 205 (45%) | 110 (44%) | 49 (47%) | 7 (50%) | 39 (48%) |
| Stage 4 (30 > eGFR ≥ 15) | 157 (35%) | 89 (35%) | 36 (35%) | 6 (43%) | 26 (32%) |
| Stage 5 (eGFR < 15) | 26 (6%) | 19 (8%) | 4 (4%) | 0 (0%) | 3 (4%) |
| Charlson Comorbidity Index score | 5 [3-7] | 5 [3-7] | 5 [3-7] | 6 [5-9] | 5 [3-6] |
| Cardiovascular disease | |||||
| Yes | 216 (48%) | 116 (46%) | 53 (51%) | 10 (71%) | 37 (45%) |
| Diabetes | |||||
| Yes | 258 (57%) | 130 (51%) | 69 (66%) | 12 (86%) | 47 (57%) |
Note: Values expressed as mean (standard deviation), median [interquartile range], or number (percent).
Abbreviations: CKD, chronic kidney disease; eGFR, estimated glomerular filtration rate; GED, general equivalency diploma; PCP, primary care provider;
Participants’ Nephrology Care, Care From Other Providers, and Reliance on Nephrologists
Participants had been in nephrology care for a median of 3.8 (IQR, 2.0-6.6) years, and half (50%) reported seeing their nephrologist at least every 6 months. Overall, they had completed a median of 4 (IQR, 3-5) nephrology appointments and 9 (IQR, 6-13) primary care appointments in the previous 2 years. Nearly all participants reported having a PCP (99%) and a specialist provider other than their PCP or nephrologist (85%). Approximately half (56%) reported that they relied primarily on their nephrologist for medical care, including CKD treatment and advice, while 23% reported that they relied primarily on their PCP, 18% relied on all providers equally, and 3% relied on another specialist provider.
Participants who stated that they primarily relied on their nephrologists for medical care had been in nephrology care for a longer time (median, 4.4 [IQR, 2.2-6.9] years) than those who primarily relied on their PCP (median, 4.0 [IQR, 1.9-6.2] years), another specialist provider (median, 3.6 [IQR, 1.8-6.6] years), or all providers equally (median, 3.1 [IQR, 1.9-5.5] years). More participants who relied on their nephrologists reported visiting their nephrologist at least every 6 months (53%) than those who relied on their PCP (46%), all providers equally (46%), or another specialist provider (43%). Participants who relied on their nephrologists and on all providers equally completed a similar number of nephrology appointments in the previous 2 years (median, 4 [IQR, 3-6] and 4 [IQR, 3-5], respectively) and completed more appointments than those who relied on their PCP (median, 3 [IQR, 2-5]) or another specialist provider (median, 3 [IQR, 3-5]). Participants who relied on their nephrologists completed fewer primary care appointments in the previous 2 years (median, 8 [IQR, 4-12]) than those who relied on their PCP (median, 10 [IQR, 6-14]), another specialist (median, 12 [IQR, 8-19]), or all providers equally (median, 10 [IQR, 6-13]; Table 2).
Table 2.
Characteristics of Participants’ Nephrology Care Stratified by the Provider They Primarily Relied on for Medical Care, Including Chronic Kidney Disease Treatment and Advice
| Characteristics | Overall (n = 453) | Nephrologist (n = 253) | PCP (n = 104) | Other Specialist (n = 14) | All Providers Equally (n = 82) | P |
|---|---|---|---|---|---|---|
| Years in nephrology care | 3.8 [2.0-6.6] | 4.4 [2.2-6.9] | 4.0 [1.9-6.2] | 3.6 [1.8-6.6] | 3.1 [1.9-5.46] | 0.06 |
| Self-reported frequency of nephrology visits | ||||||
| At least 1×/mo | 19 (4%) | 14 (6%) | 3 (3%) | 0 (0%) | 2 (2%) | |
| At least every 2 mo | 9 (2%) | 4 (2%) | 2 (2%) | 1 (7%) | 2 (2%) | |
| At least every 3 mo | 109 (24%) | 71 (28%) | 13 (13%) | 2 (14%) | 23 (28%) | <0.001 |
| At least every 6 mo | 225 (50%) | 133 (53%) | 48 (46%) | 6 (43%) | 38 (46%) | |
| 1×/y | 66 (15%) | 27 (11%) | 20 (19%) | 4 (29%) | 15 (18%) | |
| When there is a problem | 20 (4%) | 3 (1%) | 15 (14%) | 0 (0%) | 2 (2%) | |
| Do not know | 5 (1%) | 1 (0.4%) | 3 (3%) | 1 (7%) | 0 (0%) | |
| Participant sees PCP | ||||||
| Yes | 450 (99%) | 250 (99%) | 104 (100%) | 14 (100%) | 82 (100%) | 0.50 |
| Participant sees other specialist provider | ||||||
| Yes | 387 (85%) | 227 (90%) | 82 (79%) | 14 (100%) | 64 (78%) | 0.004 |
| No. of completed appointments in past 2 y | ||||||
| Nephrology | 4 [3-5] | 4 [3-6] | 3 [2-5] | 3 [3-5] | 4 [3-5] | <0.001 |
| Primary care | 9 [6-13] | 8 [4-12] | 10 [6-14] | 12 [8-19] | 10 [6-13] | 0.01 |
Note: Values for categorical variables are given as number (percent); values for continuous variables are given as median [interquartile range].
Abbreviation: PCP, primary care provider.
Participants’ Perceived Patient-Centeredness of Nephrology Care
Participants’ perceived patient-centeredness of their most recent nephrology visit was high (median, 3.8 [IQR, 3.4-4.0] of a highest possible score of 4). Scores on the Patient Perception of Patient Centeredness scale were higher among those who relied primarily on their nephrologists for medical care (median, 4.0 [IQR, 3.6-4.0]) than among those who relied primarily on non-nephrologist providers (median, 3.6 [IQR, 3.2-4.0]). Participants who relied primarily on their nephrologists were more likely to report that their main problem was “completely” discussed during their last visit (64% vs 45%), that their nephrologist “completely” understood the importance of the reason for their visit (87% vs 67%), “completely” understood them during the visit (87% vs 65%), and “completely” cares about them as a person (83% vs 62%; Table 3).
Table 3.
Participants’ Perceived Patient-Centeredness of Their Most Recent Nephrology Visit
| Perceived Patient-Centeredness Questions and Responses | Overall | Relied Primarily on Nephrologist | Did Not Rely Primarily on Nephrologist | P |
|---|---|---|---|---|
| Composite score | 3.8 [3.4-4.0] | 4.0 [3.6-4.0] | 3.6 [3.2-4.0] | <0.001 |
| To what extent was your main problem(s) discussed during your last visit with your kidney doctor? | ||||
| Not at all | 28 (6%) | 13 (5%) | 15 (8%) | |
| A little | 61 (14%) | 23 (9%) | 38 (19%) | |
| Mostly | 100 (22%) | 51 (20%) | 49 (25%) | |
| Completely | 252 (56%) | 163 (64%) | 89 (45%) | <0.001 |
| Refused | 1 (0.2%) | 0 (0%) | 1 (0.5%) | |
| Do not know | 11 (2%) | 3 (1%) | 8 (4%) | |
| Would you say that your kidney doctor knew that this was one of your reasons for coming in during the visit? | ||||
| No | 28 (6%) | 18 (7%) | 10 (5%) | |
| Do not know | 15 (3%) | 7 (3%) | 8 (4%) | |
| Maybe | 16 (4%) | 5 (2%) | 11 (6%) | 0.15 |
| Yes | 394 (87%) | 223 (88%) | 171 (86%) | |
| To what extent did your kidney doctor understand the importance of your reason for the visit? | ||||
| Not at all | 7 (2%) | 2 (0.8%) | 5 (2%) | |
| A little | 19 (4%) | 4 (2%) | 15 (7%) | |
| Mostly | 64 (14%) | 25 (10%) | 39 (20%) | <0.001 |
| Completely | 353 (78%) | 220 (87%) | 133 (67%) | |
| Refused | 1 (0.2%) | 0 (0%) | 1 (0.5%) | |
| Do not know | 9 (2%) | 2 (0.8%) | 7 (3%) | |
| How well do you think your kidney doctor understood you during the visit? | ||||
| Not at all | 8 (2%) | 0 (0%) | 8 (4%) | |
| A little | 18 (4%) | 3 (1%) | 15 (7%) | |
| Mostly | 73 (16%) | 30 (12%) | 43 (21%) | <0.001 |
| Completely | 348 (77%) | 219 (87%) | 129 (65%) | |
| Refused | 1 (0.2%) | 0 (0%) | 1 (0.5%) | |
| Do not know | 5 (1%) | 1 (0.4%) | 4 (2%) | |
| How much would you say that your kidney doctor cares about you as a person? | ||||
| Not at all | 7 (2%) | 0 (0%) | 7 (4%) | |
| A little | 21 (5%) | 5 (2%) | 16 (8%) | |
| Mostly | 78 (17%) | 35 (14%) | 43 (22%) | |
| Completely | 334 (74%) | 211 (83%) | 123 (62%) | <0.001 |
| Missing | 1 (< 0.1%) | 0 (0%) | 1 (0.1%) | |
| Do not know | 12 (3%) | 2 (0.8%) | 10 (5%) | |
Note: Values expressed as median [interquartile range] or number (percent).
Characteristics Associated With Participants’ Reliance on Nephrologists
After adjustment, participants who perceived their last nephrology visit as more patient-centered had higher odds of reporting that they relied mostly on their nephrologists (vs other providers) for medical care, including CKD treatment and advice (odds ratio [OR], 2.63 [95% CI, 1.70-4.09] per 1-point increase in patient-centeredness score; P < 0.001). Participants’ odds of relying on their nephrologists (vs other providers) were also higher among those who had been in nephrology care for more (vs fewer) years (OR, 1.08 [95% CI, 1.02-1.15] per 1-year increase; P = 0.02) and those who completed more (vs fewer) nephrology appointments in the previous 2 years (OR, 1.16 [95% CI, 1.05-1.29] per 1 additional appointment; P = 0.005). In contrast, participants who completed more (vs fewer) primary care appointments in the previous 2 years had lower odds of relying on their nephrologists (vs other providers; OR, 0.96 [95% CI, 0.93-0.99] per 1 additional appointment; P = 0.01). Participants’ sociodemographic and clinical characteristics were not associated with their reported reliance on nephrologists for medical care (Table 4).
Table 4.
Odds of Participants Relying Primarily on Their Nephrologists (vs other providers) for Medical Care, Including CKD Treatment and Advice
| Characteristics | Overall (N = 453) | Unadjusted |
Adjusteda |
||
|---|---|---|---|---|---|
| OR (95% CI) | P | OR (95% CI) | P | ||
| Age | |||||
| 1-y increase | 0.99 (0.97-1.00) | 0.07 | 0.99 (0.96-1.01) | 0.19 | |
| Sex | |||||
| Male | 187 (41%) | Reference | 0.91 | Reference | 0.25 |
| Female | 266 (59%) | 0.98 (0.67-1.43) | 1.30 (0.83-2.02) | ||
| Income | |||||
| <$30,000 | 146 (32%) | 0.41 (0.23-0.74) | 0.02 | 0.81 (0.41-1.63) | 0.53 |
| $30,000-$59,999 | 114 (25%) | 0.53 (0.29-0.97) | 0.81 (0.41-1.58) | ||
| ≥$60,000 | 82 (18%) | Reference | Reference | ||
| Missing/refused/don’t know | 111 (25%) | 0.45 (0.25-0.83) | 0.61 (0.30-1.22) | ||
| Education | |||||
| <High school | 58 (13%) | Reference | 0.02 | Reference | 0.37 |
| High school graduate/GED | 301 (66%) | 1.47 (0.84-2.59) | 1.11 (0.59-2.09) | ||
| College graduate | 90 (20%) | 2.73 (1.38-5.40) | 1.76 (0.79-3.92) | ||
| Missing/refused/do not know | 4 (1%) | 0.41 (0.04-4.18) | 0.59 (0.05-7.01) | ||
| Employment | |||||
| Working/looking for work | 85 (19%) | Reference | 0.05 | Reference | 0.13 |
| Unemployed | 4 (1%) | 1.55 (0.16-15.6) | 1.26 (0.11-14.3) | ||
| Retired due to disability | 59 (13%) | 0.36 (0.18-0.71) | 0.38 (0.17-0.84) | ||
| Retired | 295 (65%) | 0.65 (0.39-1.07) | 0.84 (0.45-1.56) | ||
| Missing/refused/do not know | 10 (2%) | 0.78 (0.20-2.97) | 1.53 (0.32-7.18) | ||
| Time seeing a nephrologist | |||||
| 1-y increase | 1.10 (1.04-1.16) | 0.002 | 1.08 (1.02-1.15) | 0.02 | |
| No. of nephrology visits in past 2 y | |||||
| 1-visit increase | 1.21 (1.11-1.33) | <0.001 | 1.16 (1.05-1.29) | 0.005 | |
| No. of primary care visits in past 2 y | |||||
| 1-visit increase | 0.96 (0.93-0.98) | 0.002 | 0.96 (0.93-0.99) | 0.01 | |
| CKD stage | |||||
| Stage 2 or 3 (eGFR ≥ 30) | 270 (59%) | Reference | 0.17 | Reference | 0.24 |
| Stage 4 (30 > eGFR ≥ 15) | 157 (35%) | 1.13 (0.76-1.68) | 0.83 (0.53-1.32) | ||
| Stage 5 (eGFR < 15) | 26 (6%) | 2.34 (0.95-5.75) | 2.11 (0.71-6.28) | ||
| Comorbidity index score | |||||
| 1-unit increase | 0.97 (0.90-1.05) | 0.47 | 1.04 (0.94-1.14) | 0.47 | |
| Perceived patient centeredness | |||||
| 1-unit increase | 2.91 (1.95-4.34) | <0.001 | 2.63 (1.70-4.09) | <0.001 | |
Abbreviations: CI, confidence interval; CKD, chronic kidney disease; eGFR, estimated glomerular filtration rate; GED, general equivalency diploma; OR, odds ratio.
Mutually adjusted for age, sex, income, education, employment, years in nephrology care, number of nephrology visits in the past 2 years, number of primary care visits in the past 2 years, CKD stage, comorbidity index score, and perceived patient-centeredness.
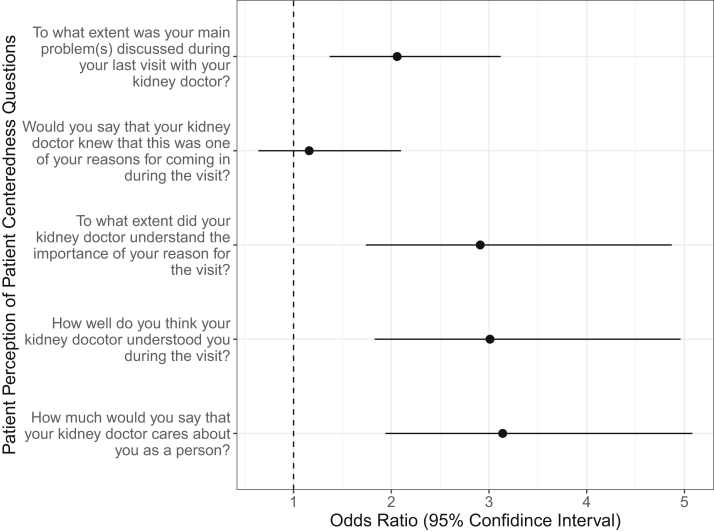
In adjusted post hoc analyses examining associations between the component questions of the Patient Perception of Patient Centeredness scale and participants’ reliance on nephrologists for medical care, 4 of the 5 questions had a statistically significant association with nephrologist reliance. Participants’ odds of relying on their nephrologists (vs other providers) were higher among those who more completely (vs less completely) agreed that their nephrologists discussed their main problem during their last visit (OR, 2.06 [95% CI, 1.37-3.12] per 1-point increase in patient-centeredness score; P < 0.001), that their nephrologists understood the importance of their reason for the visit (OR, 2.91 [95% CI, 1.74-4.87] per 1-point increase in patient-centeredness score; P < 0.001), that their nephrologists understood them during the visit (OR, 3.01 [95% CI, 1.83-4.96] per 1-point increase in patient-centeredness score; P < 0.001), and that their nephrologists care about them as a person (OR, 3.14 [95% CI, 1.94-5.08] per 1-point increase in patient-centeredness score; P < 0.001; Fig 2).
Figure 2.
Adjusted odds of participants relying on their nephrologists (vs other providers) for medical care, including chronic kidney disease treatment and advice, by component Patient Perception of Patient Centeredness questions. Adjusted for age, sex, income, education, employment, years in nephrology care, number of nephrology visits in the past 2 years, number of primary care visits in the past 2 years, chronic kidney disease stage, and comorbidity index score.
Discussion
In this cross-sectional study among patients receiving longitudinal nephrology care in CKD clinics, only half the participants reported that they primarily relied on their nephrologists for medical care, including CKD treatment and advice. Participants who had been in nephrology care for longer, completed more nephrology visits in the past 2 years, and perceived their last nephrology visit as more patient-centered had higher odds of reporting that they primarily relied on their nephrologists. These findings lend insight into how patients with CKD prioritize the medical care and advice they receive when under the care of multiple providers, highlighting factors that may inform strategies to improve care coordination.
To our knowledge, this study is among the first to examine how CKD patients prioritize medical care provided by their nephrologists versus non-nephrologist providers. Prior studies have examined different models of comanagement between nephrologists and non-nephrologists20 but they have not asked patients directly about how they prioritize information from the multiple providers involved in managing their medical care. A recent systematic review studying patterns of primary care delivery among patients receiving dialysis found that a majority of dialysis patients regarded their nephrologists as the primary source of their health care.21 Additionally, studies of dialysis modality choice suggest that patients place a high value on nephrologists’ treatment recommendations.22, 23, 24 In contrast, our findings in patients with less advanced CKD suggest that patients who have not yet initiated kidney replacement therapy still rely heavily on their non-nephrologist providers for medical care and CKD treatment and advice.
In this study, participants who were in nephrology care longer and who completed more nephrology visits in the previous 2 years were more likely to rely on their nephrologists for medical care. Given the often long-term relationships that patients establish with their PCPs,25 differences in patients’ reliance on nephrologists versus other health care providers may reflect the extent to which they had time to form trusting relationships with their nephrologists compared with their PCPs. PCPs play a critical role in supporting the complex care needs of patients with CKD, especially earlier in the CKD trajectory when primary care efforts are focused on managing risk factors such as hypertension and diabetes and when care may be less exclusively focused on nephrology.26 However, PCPs have identified several barriers to comanaging patients alongside nephrologists, including suboptimal PCP-nephrologist communication.8
Given the shortage of nephrologists available to care for the growing population of patients with CKD,26 efforts to optimize CKD comanagement are needed to ensure that all patients receive guideline-concordant care. Previous studies demonstrated the effectiveness of multidisciplinary team care that incorporates both nephrology and primary care in CKD management.27, 28, 29 Although both PCPs and nephrologists seem to desire this comanagement, they may lack alignment on goals of care,30 potentially contributing to the delivery of conflicting or inconsistent advice to patients. It may take time for patients to cultivate the type of trusting relationship with their nephrologists that they may already have with their PCPs, and our findings suggest that efforts to establish this relationship earlier may help patients prioritize the CKD treatment and advice they receive from their nephrologists.
Participants perceived their most recent nephrology visits to be highly patient-centered, and those who rated their visits as more patient-centered were more likely to rely on their nephrologists for medical care. Specific aspects of patient-centeredness that differed between participants who did and did not rely on their nephrologists included their perceptions that their nephrologists cared about them as a person, understood the importance of their reason for the visit, understood them during the visit, and discussed their main problem during the visit.
Previous studies in other areas have found that patients who perceived their visits with health care providers as patient-centered were less likely to avoid treatment, avoid visits, and discontinue visits.31, 32, 33, 34 Person-centered care, which expands on the concept of patient-centered care by recognizing that patients’ preferences and care needs change over time and invites patients to codesign and coproduce their health services alongside their care team, may also be an important aspect of care to capture in future studies to better understand how a more collaborative approach to kidney care could improve patients’ engagement with their nephrologists’ treatment recommendations.35 Still, our findings reinforce the importance of patient-centeredness as a key element of nephrologist-patient communication that affects how patients prioritize information in the context of complex chronic disease care.
Limitations of our study deserve mention. First, we studied patients within a single health system in Pennsylvania. The Geisinger population is largely white and rural, and perspectives in other populations may differ. Second, participants who opted to complete the long questionnaire were younger, more educated, and more commercially insured and had a higher prevalence of cardiovascular disease than those who completed only the short questionnaire, and this self-selection may affect the generalizability of our findings. Third, although we assessed participants’ number of completed primary care visits in the previous 2 years, we did not include more comprehensive assessments of participants’ relationships with their PCPs, such as perceived patient-centeredness. It is possible that participants’ interactions with their other providers, PCPs in particular, could contribute to our findings. We also did not ask participants about their reliance on other health care professionals, such as nurses or dieticians. Fourth, participants perceived an overall high degree of patient-centeredness, which leaves a marginal amount of room for improvement. However, our findings indicate that a small improvement would still meaningfully benefit the patient-nephrologist relationship. Further, interviews were not routinely conducted immediately after participants’ visits with their nephrologists, so participant recall bias may have also influenced our patient-centeredness findings. Finally, the cross-sectional nature of our study precludes causal inferences. Nonetheless, our findings provide new insight into patients’ prioritization of nephrologist-recommended CKD care.
In summary, although many patients with CKD relied on their nephrologists for medical care, including CKD treatment and advice, many did not. Those who received longer and more frequent nephrology care and those who perceived their nephrology visits to be more patient-centered were more likely to rely on their nephrologists. Efforts to improve comanagement with patients’ other trusted providers, particularly in primary care, and efforts to establish trusted and patient-centered nephrology care could help optimize multidisciplinary care strategies that promote patients’ adherence to nephrologists’ treatment recommendations.
Article Information
PREPARE NOW Study Team members
Duke University, Durham, NC (L. Ebony Boulware, Clarissa Diamantidis, Clare Il’Giovine, George Jackson, Jane Pendergast, Sarah Peskoe, Tara Strigo); Geisinger Health System, Danville, PA (Jon Billet, Jason Browne, Ion Bucaloiu, Charlotte Collins, Daniel Davis, Sherri Fulmer, Jamie Green, Chelsie Hauer, Evan Norfolk, Michelle Richner, Cory Siegrist, Wendy Smeal, Rebecca Stametz, Mary Solomon, Christina Yule); Johns Hopkins University, Baltimore, MD (Patti Ephraim, Raquel Greer, Felicia Hill-Briggs); University of South Carolina, Columbia, SC (Teri Browne); University of Manitoba, Winnipeg, Manitoba (Navdeep Tangri); members of the Patient and Family Caregiver Stakeholder Group (Brian Bankes, Shakur Bolden, Patricia Danielson, Katina Lang-Lindsey, Suzanne Ruff, Lana Schmidt, Amy Swoboda, Peter Woods); American Association of Kidney Patients (Diana Clynes); Council of Nephrology Social Workers (Stephanie Stewart); Medical Education Institute (Dori Schatell, Kristi Klicko); Mid-Atlantic Renal Coalition (Brandi Vinson); National Kidney Foundation (Jennifer St. Clair Russell, Kelli Collins, Jennifer Martin); Renal Physicians Association (Dale Singer); and Pennsylvania Medical Society (Diane Littlewood).
Authors’ Full Names and Academic Degrees
Tyler M. Barrett, MA, Jamie A. Green, MD, MS, Raquel C. Greer, MD, MHS, Patti L. Ephraim, MPH, Sarah Peskoe, PhD, Jane F. Pendergast, PhD, Chelsie L. Hauer, MPH, Tara S. Strigo, MPH, Evan Norfolk, MD, Ion Dan Bucaloiu, MD, Clarissa J. Diamantidis, MD, MHS, Felicia F. Hill-Briggs, PhD, Teri Browne, PhD, MSW, George L. Jackson, PhD, and L. Ebony Boulware, MD, MPH.
Authors’ Contributions
Research idea and study design: TMB, JAG, PLE, LEB; data analysis: TMB, SP, JFP, LEB; intellectual contributions/interpretation: TMB, JAG, RCG, PLE, CLH, TSS, EN, IDB, CJD, FFH-B, TB, GLJ, LEB; supervision and mentorship: LEB, JAG. Each author contributed important intellectual content during manuscript drafting or revision, accepts personal accountability for the author’s own contributions, and agrees to ensure that questions pertaining to the accuracy or integrity of any portion of the work are appropriately investigated and resolved.
Support
This work was supported through a Patient-Centered Outcomes Research Institute (PCORI) Project Program Award (IHS-1409-20967).
Financial Disclosure
The authors declare that they have no relevant financial interests.
Acknowledgements
The authors express their gratitude to the physicians, nurses, medical assistants, staff, and patients of the Geisinger Health System, Danville, PA.
Disclaimer
All statements in this report, including its findings and conclusions, are solely those of the authors and do not necessarily represent the views of PCORI, its Board of Governors, or Methodology Committee.
Peer Review
Received January 26, 2020. Evaluated by 3 external peer reviewers, with direct editorial input from the Statistical Editor and the Editor-in-Chief. Accepted in revised form May 3, 2020.
Footnotes
Complete author and article information provided before references.
Table S1: Comparison of sociodemographic and clinical characteristics between PREPARE NOW participants who did and did not complete the ‘long’ questionnaire and the provider reliance question
Contributor Information
L. Ebony Boulware, Email: ebony.boulware@duke.edu.
PREPARE NOW study investigators:
L. Ebony Boulware, Clarissa Diamantidis, Clare Il’Giovine, George Jackson, Jane Pendergast, Sarah Peskoe, Tara Strigo, Jon Billet, Jason Browne, Ion Bucaloiu, Charlotte Collins, Daniel Davis, Sherri Fulmer, Jamie Green, Chelsie Hauer, Evan Norfolk, Michelle Richner, Cory Siegrist, Wendy Smeal, Rebecca Stametz, Mary Solomon, Christina Yule, Patti Ephraim, Raquel Greer, Felicia Hill-Briggs, Teri Browne, Navdeep Tangri, Brian Bankes, Shakur Bolden, Patricia Danielson, Katina Lang-Lindsey, Suzanne Ruff, Lana Schmidt, Amy Swoboda, Peter Woods, Diana Clynes, Stephanie Stewart, Dori Schatell, Kristi Klicko, Brandi Vinson, Jennifer St. Clair Russell, Kelli Collins, Jennifer Martin, Dale Singer, and Diane Littlewood
Supplementary Material
Table S1.
References
- 1.Tonelli M., Wiebe N., Guthrie B. Comorbidity as a driver of adverse outcomes in people with chronic kidney disease. Kidney Int. 2015;88(4):859–866. doi: 10.1038/ki.2015.228. [DOI] [PubMed] [Google Scholar]
- 2.Bowling C.B., Vandenberg A.E., Phillips L.S., McClellan W.M., Johnson T.M., 2nd, Echt K.V. Older patients’ perspectives on managing complexity in CKD self-management. Clin J Am Soc Nephrol. 2017;12(4):635–643. doi: 10.2215/CJN.06850616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sinnott C., Mc Hugh S., Browne J., Bradley C. GPs’ perspectives on the management of patients with multimorbidity: systematic review and synthesis of qualitative research. BMJ Open. 2013;3(9) doi: 10.1136/bmjopen-2013-003610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Patwardhan M.B., Samsa G.P., Matchar D.B., Haley W.E. Advanced chronic kidney disease practice patterns among nephrologists and non-nephrologists: a database analysis. Clin J Am Soc Nephrol. 2007;2(2):277–283. doi: 10.2215/CJN.02600706. [DOI] [PubMed] [Google Scholar]
- 5.Greer R.C., Cooper L.A., Crews D.C., Powe N.R., Boulware L.E. Quality of patient-physician discussions about CKD in primary care: a cross-sectional study. Am J Kidney Dis. 2011;57(4):583–591. doi: 10.1053/j.ajkd.2010.08.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Boulware L.E., Troll M.U., Jaar B.G., Myers D.I., Powe N.R. Identification and referral of patients with progressive CKD: a national study. Am J Kidney Dis. 2006;48(2):192–204. doi: 10.1053/j.ajkd.2006.04.073. [DOI] [PubMed] [Google Scholar]
- 7.Israni R.K., Shea J.A., Joffe M.M., Feldman H.I. Physician characteristics and knowledge of CKD management. Am J Kidney Dis. 2009;54(2):238–247. doi: 10.1053/j.ajkd.2009.01.258. [DOI] [PubMed] [Google Scholar]
- 8.Greer R.C., Liu Y., Cavanaugh K. Primary care physicians’ perceived barriers to nephrology referral and co-management of patients with CKD: a qualitative study. J Gen Intern Med. 2019;34(7):1228–1235. doi: 10.1007/s11606-019-04975-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tonelli M., Bohm C., Pandeya S., Gill J., Levin A., Kiberd B.A. Cardiac risk factors and the use of cardioprotective medications in patients with chronic renal insufficiency. Am J Kidney Dis. 2001;37(3):484–489. [PubMed] [Google Scholar]
- 10.Parikh N.I., Hwang S.J., Larson M.G., Meigs J.B., Levy D., Fox C.S. Cardiovascular disease risk factors in chronic kidney disease: overall burden and rates of treatment and control. Arch Intern Med. 2006;166(17):1884–1891. doi: 10.1001/archinte.166.17.1884. [DOI] [PubMed] [Google Scholar]
- 11.Kerr E.A., Heisler M., Krein S.L. Beyond comorbidity counts: how do comorbidity type and severity influence diabetes patients’ treatment priorities and self-management? J Gen Intern Med. 2007;22(12):1635–1640. doi: 10.1007/s11606-007-0313-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Muntner P., Anderson A., Charleston J. Hypertension awareness, treatment, and control in adults with CKD: results from the Chronic Renal Insufficiency Cohort (CRIC) Study. Am J Kidney Dis. 2010;55(3):441–451. doi: 10.1053/j.ajkd.2009.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Oskoui T., Pandya R., Weiner D.E., Wong J.B., Koch-Weser S., Ladin K. Advance care planning among older adults with advanced non–dialysis-dependent CKD and their care partners: perceptions versus reality? Kidney Med. 2020;2:116–124. doi: 10.1016/j.xkme.2019.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Green J.A., Ephraim P.L., Hill-Briggs F.F. Putting patients at the center of kidney care transitions: PREPARE NOW, a cluster randomized controlled trial. Contemp Clin Trials. 2018;73:98–110. doi: 10.1016/j.cct.2018.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kidney Disease: Improving Global Outcomes (KDIGO) CKD Working Group KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl. 2013;3:1–150. [Google Scholar]
- 16.Levey A.S., Stevens L.A., Schmid C.H. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150(9):604–612. doi: 10.7326/0003-4819-150-9-200905050-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Charlson M., Szatrowski T.P., Peterson J., Gold J. Validation of a combined comorbidity index. J Clin Epidemiol. 1994;47(11):1245–1251. doi: 10.1016/0895-4356(94)90129-5. [DOI] [PubMed] [Google Scholar]
- 18.Stewart M., Meredith L., Ryan B., Brown J. Canada Centre for Studies in Family Medicine; Ontario, Canada: 2004. The Patient Perception of Patient Centeredness Questionnaire (PPPC) #04-1. [Google Scholar]
- 19.Stewart M., Brown J.B., Donner A. The impact of patient-centered care on outcomes. J Fam Pract. 2000;49(9):796–804. [PubMed] [Google Scholar]
- 20.Nicoll R., Robertson L., Gemmell E., Sharma P., Black C., Marks A. Models of care for chronic kidney disease: a systematic review. Nephrology (Carlton) 2018;23(5):389–396. doi: 10.1111/nep.13198. [DOI] [PubMed] [Google Scholar]
- 21.Wang V., Diamantidis C.J., Wylie J., Greer R.C. Minding the gap and overlap: a literature review of fragmentation of primary care for chronic dialysis patients. BMC Nephrol. 2017;18(1):274. doi: 10.1186/s12882-017-0689-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wuerth D.B., Finkelstein S.H., Schwetz O., Carey H., Kliger A.S., Finkelstein F.O. Patients’ descriptions of specific factors leading to modality selection of chronic peritoneal dialysis or hemodialysis. Perit Dial Int. 2002;22(2):184–190. [PubMed] [Google Scholar]
- 23.Fortnum D., Grennan K., Ludlow M. Kidney Health Australia; 2015. Dialysis Consumer Perspectives Survey Two: Complete Dataset Report. [Google Scholar]
- 24.Walker R.C., Marshall R., Howard K., Morton R.L., Marshall M.R. “Who matters most?”: clinician perspectives of influence and recommendation on home dialysis uptake. Nephrology (Carlton) 2017;22(12):977–984. doi: 10.1111/nep.12920. [DOI] [PubMed] [Google Scholar]
- 25.Haggerty J.L., Reid R.J., Freeman G.K., Starfield B.H., Adair C.E., McKendry R. Continuity of care: a multidisciplinary review. BMJ. 2003;327(7425):1219–1221. doi: 10.1136/bmj.327.7425.1219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shahinian V.B., Saran R. The role of primary care in the management of the chronic kidney disease population. Adv Chronic Kidney Dis. 2010;17(3):246–253. doi: 10.1053/j.ackd.2010.02.003. [DOI] [PubMed] [Google Scholar]
- 27.Goldstein M., Yassa T., Dacouris N., McFarlane P. Multidisciplinary predialysis care and morbidity and mortality of patients on dialysis. Am J Kidney Dis. 2004;44(4):706–714. [PubMed] [Google Scholar]
- 28.Hemmelgarn B.R., Manns B.J., Zhang J. Association between multidisciplinary care and survival for elderly patients with chronic kidney disease. J Am Soc Nephrol. 2007;18(3):993–999. doi: 10.1681/ASN.2006080860. [DOI] [PubMed] [Google Scholar]
- 29.Bayliss E.A., Bhardwaja B., Ross C., Beck A., Lanese D.M. Multidisciplinary team care may slow the rate of decline in renal function. Clin J Am Soc Nephrol. 2011;6(4):704–710. doi: 10.2215/CJN.06610810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Diamantidis C.J., Powe N.R., Jaar B.G., Greer R.C., Troll M.U., Boulware L.E. Primary care-specialist collaboration in the care of patients with chronic kidney disease. Clin J Am Soc Nephrol. 2011;6(2):334–343. doi: 10.2215/CJN.06240710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Moore P.J., Sickel A.E., Malat J., Williams D., Jackson J., Adler N.E. Psychosocial factors in medical and psychological treatment avoidance: the role of the doctor-patient relationship. J Health Psychol. 2004;9(3):421–433. doi: 10.1177/1359105304042351. [DOI] [PubMed] [Google Scholar]
- 32.Federman A.D., Cook E.F., Phillips R.S. Intention to discontinue care among primary care patients: influence of physician behavior and process of care. J Gen Intern Med. 2001;16(10):668–674. doi: 10.1111/j.1525-1497.2001.01028.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Phibbs S.C., Faith J., Thorburn S. Patient-centred communication and provider avoidance: does body mass index modify the relationship? Health Educ J. 2016;76(1):120–127. [Google Scholar]
- 34.Kannan V.D., Veazie P.J. Predictors of avoiding medical care and reasons for avoidance behavior. Med Care. 2014;52(4):336–345. doi: 10.1097/MLR.0000000000000100. [DOI] [PubMed] [Google Scholar]
- 35.Morton R.L., Sellars M. From patient-centered to person-centered care for kidney diseases. Clin J Am Soc Nephrol. 2019;14(4):623–625. doi: 10.2215/CJN.10380818. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1.