Abstract
Objectives
The United States has the highest number of coronavirus disease 2019 (COVID-19) in the world, with high variability in cases and mortality between communities. We aimed to quantify the associations between socio-economic status and COVID-19–related cases and mortality in the U.S.
Study design
The study design includes nationwide COVID-19 data at the county level that were paired with the Distressed Communities Index (DCI) and its component metrics of socio-economic status.
Methods
Severely distressed communities were classified by DCI>75 for univariate analyses. Adjusted rate ratios were calculated for cases and fatalities per 100,000 persons using hierarchical linear mixed models.
Results
This cohort included 1,089,999 cases and 62,298 deaths in 3127 counties for a case fatality rate of 5.7%. Severely distressed counties had significantly fewer deaths from COVID-19 but higher number of deaths per 100,000 persons. In risk-adjusted analysis, the two socio-economic determinants of health with the strongest association with both higher cases per 100,000 persons and higher fatalities per 100,000 persons were the percentage of adults without a high school degree (cases: RR 1.10; fatalities: RR 1.08) and proportion of black residents (cases and fatalities: Relative risk(RR) 1.03). The percentage of the population aged older than 65 years was also highly predictive for fatalities per 100,000 persons (RR 1.07).
Conclusion
Lower education levels and greater percentages of black residents are strongly associated with higher rates of both COVID-19 cases and fatalities. Socio-economic factors should be considered when implementing public health interventions to ameliorate the disparities in the impact of COVID-19 on distressed communities.
Keywords: Coronavirus, COVID-19, SARS-CoV-2, Socio-economic status, Race
Highlights
-
•
Socio-economic factors play an important role in coronavirus disease 2019 (COVID-19) prevalence and mortality.
-
•
Lower education level was the strongest association with both cases and fatalities.
-
•
The higher proportion of Black residents was also associated with cases and fatalities.
-
•
The poverty rate and median income were also associated with COVID-19 cases.
-
•
Median income and change in employment were also associated with COVID-19 fatalities.
Introduction
The coronavirus disease 2019 (COVID-19) pandemic is a worldwide public health crisis on a scale not witnessed in modern times. The United States has the highest number of COVID-19 cases and fatalities in the world.1 There is wide variability in COVID-19–related mortality across countries and between communities within the U.S. While research has identified a number of risk factors for mortality such as age and comorbid disease, there are new data suggesting social determinants of health also influence outcomes.2 , 3 Data from the Centers for Disease Control and Prevention suggest strong racial disparities in both COVID-19 prevalence and outcomes.4 This point has been highlighted by the U.S. Surgeon General, the lay press, and recent publications.4, 5, 6
Socio-economic factors impact all facets of human functioning, including health-related quality of life. While a few publications have speculated on the impact of socio-economic status on the COVID-19 pandemic, there is limited quantitative analysis available.7, 8, 9, 10 A unique opportunity for investigation lies with the Distressed Communities Index (DCI). This metric was developed by the Economic Innovation Group and is a comprehensive estimate of socio-economic status by geographic location.11 The DCI is a composite socio-economic ranking that accounts for unemployment, education level, poverty rate, median income, business growth, and housing vacancies. Previous studies have correlated a higher DCI score (lower socio-economic status) with worse health-related outcomes.12, 13, 14 The objective of this study was to quantify the association between socio-economic status, both the composite metric of DCI and its individual component measures, and COVID-19 outcomes, accounting for other risk factors such as age and chronic diseases. We hypothesized that communities with lower socio-economic status (higher DCI scores) would have disproportionately higher COVID-19 prevalence and mortality.
Methods
Data sources and definitions
COVID-19–related cases and mortality were extracted from a publicly available data set of aggregated county sources (USAFacts) on May 2, 2020.15 In addition, county-level estimates for chronic diseases were obtained from the Centers for Disease Control and Prevention. Specifically, the Centers for Disease Control and Prevention (CDC) COVID-19 response team used data from the 2018 Behavioral Risk Factor Surveillance System and U.S. Census population data to model prevalence of chronic diseases potentially associated with COVID-19 risk.16 The model estimates for chronic kidney disease, chronic obstructive pulmonary disease, heart disease, obesity, and diabetes at the county level were included for risk adjustment. The data for rates of uninsured individuals under age 65, percent of population black, and percent of population age over 65 were obtained from the American Communities Survey 5-year Estimates. The United States is geographically and governmentally organized into 50 states. The states are then subdivided into counties with their own local governance structures. There is wide variability in the population and size of the states and counties, with the number of counties per state ranging from 3 (Delaware) to 254 (Texas). There is a total of 3143 counties or county-equivalent areas (parishes in Louisiana and boroughs in Alaska). At the time of writing, the most granular COVID-19–related data for the United States were available at the county level.
Socio-economic status was measured using the DCI and its components. A data use agreement is in place with the Economic Innovation Group.11 The DCI score is available for 99% of the United States population and is derived from the American Communities Survey 5-year Estimates and Census Bureau County and Zip Code Business Patterns. The score is composed from the following data points: ‘percentage adults with no high school degree, housing vacancy rate, percentage of adults not working, poverty rate, median income ratio, percentage change in employment, and percentage change in business establishments.’ Detailed data definitions are available in Supplemental Table 1. The score ranges from 0 (no distress) to 100 (most distress) and is available on the zip code, county and state level. Severely distressed communities were defined by a DCI score >75. This study conformed to the principles embodied in the Declaration of Helsinki and was exempt from review by the University of Virginia Institutional Review Board due to the deidentified nature of the publicly available data sets.
Counties were included for analysis if both COVID-19 data and DCI score were available. Individual cases and deaths were excluded from the analysis if they were not attributed to a specific county.
Statistical analysis
Categorical variables are presented as counts (%) and continuous variables as median [25th, 75th percentile]. Counties were stratified by severely distressed (DCI>75) versus less distressed (DCI ≤75) for univariate analysis using the Mann-Whitney U test. Adjusted effects of socio-economic status were approximated using hierarchical linear mixed models with Laplace approximation and a negative binomial distribution. Socio-economic effects were adjusted for county-level prevalence of elderly residents, uninsured adults, and the following comorbidities: chronic kidney disease, chronic obstructive pulmonary disease, heart disease, diabetes, and obesity. A random effect was used for clustering at the state level. Temporal bias was accounted for with a variable of days since first COVID-19 case. Regression results were exponentiated to construct adjusted rate ratios. Statistical analyses were carried out using SAS, version 9.4 (SAS Institute, Cary, NC), with some graphical representation performed with Prism 8 (GraphPad, San Diego, CA). A P-value <0.05 determined statistical significance.
Results
Cohort description
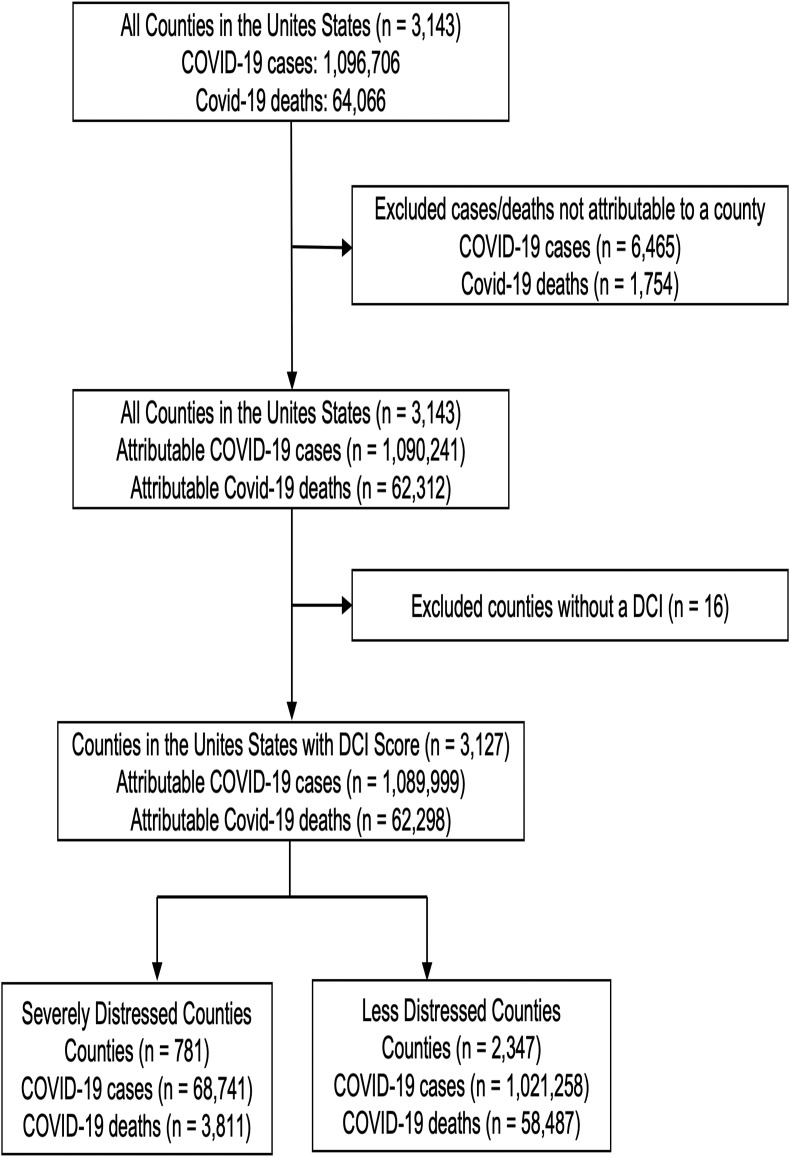
At the time of data extraction on May 2, 2020, there were 1,096,706 cases and 64,066 deaths in the United States. There were 3143 counties with COVID-19 data available. Twenty-four states had cases not allocated to counties for a total of 6465 cases (0.6%), while 14 states had unallocated deaths for a total of 1754 deaths (2.7%), with 1445 being unallocated in Tennessee. A DCI score was available for 3127 counties with COVID-19 data. This cohort included 1,089,999 cases (99%) and 62,298 deaths (97%) for a case fatality rate of 5.7%. A consort diagram depicting the exclusions leading to the final cohort is shown in Fig. 1 .
Fig. 1.
Consort diagram of included and excluded counties, COVID-19 cases, and COVID-19 fatalities. COVID-19 = coronavirus disease 2019.
Differences by the DCI
A total of 781 counties were designated as severely distressed (DCI >75), accounting for 68,741 (6.3%) COVID-19 cases and 3811 (6.1%) COVID-19 fatalities. When compared with less distressed counties, those classified as severely distressed had significantly lower median COVID-19 cases (13 [3–39] vs 21 [4–117], P < 0.0001) and fatalities (0 [0–1] vs 0 [0–4], P < 0.0001). Owing to the rural nature of many distressed counties, after accounting for county population size, there was no difference in median cases per 100,000 persons and a reverse in the trend with higher median fatalities per 100,000 persons in severely distressed counties (Table 1 ). The median percentage of black Americans was significantly higher in severely distressed counties compared with less distressed counties (7.3% vs 1.8%, P < 0.0001). Other significant differences included severely distressed counties having higher rates of elderly residents, uninsured individuals, and individuals with chronic kidney disease, chronic obstructive pulmonary disease, heart disease, diabetes, and obesity. However, severely distressed communities were hit later in the pandemic with lower median days since first case (34 vs 38, P < 0.0001).
Table 1.
Univariate analysis by severely versus less distressed counties.
| Variable | Severely distressed | Less distressed | P-value |
|---|---|---|---|
| Cases per 100,000 persons | 61 [22–176] | 63 [27–145] | 0.813 |
| Deaths per 100,000 persons | 0 [0–7.1] | 0 [0–5.4] | 0.028 |
| % of population aged older than 65 years | 17.4% [15.4–19.5] | 16.8% [14.1–19.6] | <0.0001 |
| % of population Black | 7.3% [1.1–33.1] | 1.8% [0.6–6.7] | <0.0001 |
| % of uninsured population aged younger than 65 years | 14.9% [11.1–17.5] | 10.0% [7.0–14.0] | <0.0001 |
| Chronic kidney disease prevalence | 4.0% [3.7–4.3] | 3.3% [3.0–3.5] | <0.0001 |
| COPD prevalence | 11.0% [9.8–12.3] | 8.3% [7.0–9.8] | <0.0001 |
| Heart disease prevalence | 10.1% [9.3–11.0] | 8.2% [7.1–9.1] | <0.0001 |
| Diabetes prevalence | 15.8% [14.5–17.3] | 12.0% [10.8–13.5] | <0.0001 |
| Obesity prevalence | 38.1% [35.7–40.5] | 34.6% [31.7–36.9] | <0.0001 |
| Days since first case | 34 [25–39] | 38 [29–44] | <0.0001 |
All values expressed as median [interquartile range]; COPD = chronic obstructive pulmonary disease.
Risk adjusted analyses of socio-economic status
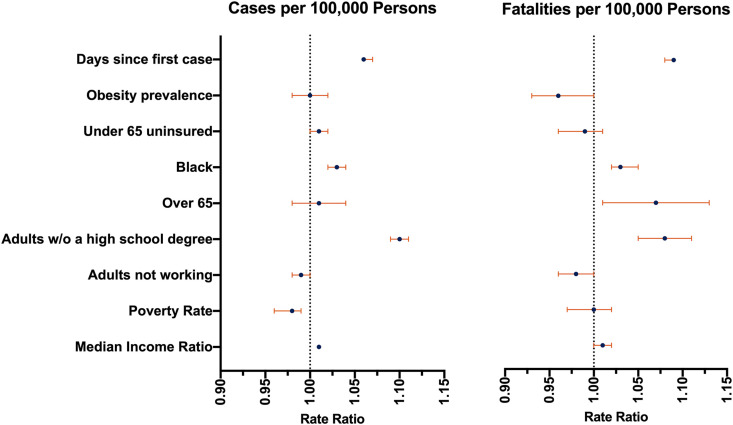
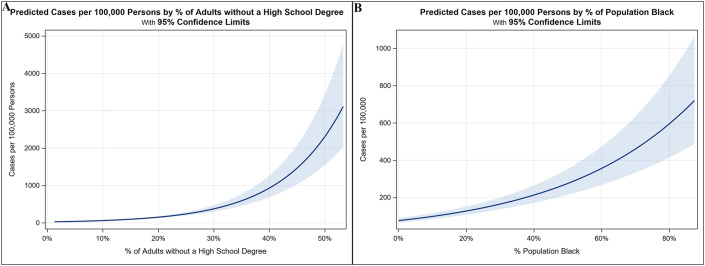
Cases of COVID-19 by county were associated with multiple socio-economic factors and days since first infection but not health-related comorbidities. The adjusted risk ratios can be visualized in Fig. 2 , with complete model results in Table 2 . A higher number of cases were associated with lower education level, higher proportion of black Americans, higher income, and lower poverty rate. The specific covariates with significant associations with cases per 100,000 persons were the percentage of adults without a high school degree (RR 1.10), proportion of black residents (RR 1.03), median income ratio (RR 1.01), and poverty rate (RR 0.98). Fig. 3 shows risk-adjusted predicted cases per 100,000 persons for the two strongest associations, the percentage of adults without a high school degree and proportion of black residents. No comorbid medical conditions were associated with COVID-19 cases at the county level.
Fig. 2.
Forrest plot of adjusted rate ratio for covariates significantly associated with either COVID-19 cases or fatalities per 100,000 persons. COVID-19 = coronavirus disease 2019.
Table 2.
Adjusted rate ratios for COVID-19–related cases and fatalities per 100,000 persons.
| Variable | Cases per 100,000 persons |
Fatalities per 100,000 persons |
||||
|---|---|---|---|---|---|---|
| Rate ratio | 95% CI | P-value | Rate ratio | 95% CI | P-value | |
| Housing vacancy rate | 1.01 | 1.00–1.02 | 0.1382 | 0.98 | 0.95–1.01 | 0.1274 |
| Median income ratio | 1.01 | 1.01–1.01 | <0.0001 | 1.01 | 1.00–1.02 | 0.0094 |
| Poverty rate | 0.98 | 0.96–0.99 | 0.0019 | 1.00 | 0.97–1.02 | 0.8511 |
| % change in employment | 1.00 | 1.00–1.00 | 0.2358 | 0.99 | 0.99–1.00 | 0.0521 |
| % change in establishments | 1.00 | 0.99–1.01 | 0.7611 | 1.00 | 0.99–1.02 | 0.7516 |
| % of adults not working | 0.99 | 0.98–1.00 | 0.1496 | 0.98 | 0.96–1.00 | 0.0266 |
| % of adults w/o a high school degree | 1.10 | 1.09–1.11 | <0.0001 | 1.08 | 1.05–1.11 | <0.0001 |
| % population in distressed zip codes | 1.00 | 1.00–1.00 | 0.7609 | 1.00 | 0.99–1.00 | 0.2284 |
| % of population aged older than 65 years | 1.01 | 0.98–1.04 | 0.410 | 1.07 | 1.01–1.13 | 0.0216 |
| % of population Black | 1.03 | 1.02–1.04 | <0.0001 | 1.03 | 1.02–1.05 | <0.0001 |
| % of uninsured population aged younger than 65 years | 1.01 | 1.00–1.02 | 0.1665 | 0.99 | 0.96–1.01 | 0.2239 |
| Chronic kidney disease prevalence | 0.81 | 0.47–1.37 | 0.4266 | 0.84 | 0.34–2.09 | 0.7136 |
| COPD prevalence | 1.00 | 0.89–1.13 | 0.967 | 1.15 | 0.95–1.41 | 0.1576 |
| Heart disease prevalence | 1.03 | 0.81–1.32 | 0.7833 | 0.89 | 0.58–1.37 | 0.5919 |
| Obesity prevalence | 1.00 | 0.98–1.02 | 0.7464 | 0.96 | 0.93–1.00 | 0.0358 |
| Diabetes prevalence | 0.98 | 0.89–1.09 | 0.7132 | 1.06 | 0.89–1.26 | 0.5221 |
| Days since first case | 1.06 | 1.06–1.07 | <0.0001 | 1.09 | 1.08–1.09 | <0.0001 |
CI = confidence interval; COPD = chronic obstructive pulmonary disease; COVID-19 = coronavirus disease 2019.
Fig. 3.
Adjusted predicted COVID-19 cases per 100,000 persons for the two strongest socio-economic factors. (A) Percentage of adults without a high school degree and (B) percentage of population Black. Estimates are shown holding all other predictors at mean values (Supplemental Table 1). COVID-19 = coronavirus disease 2019.
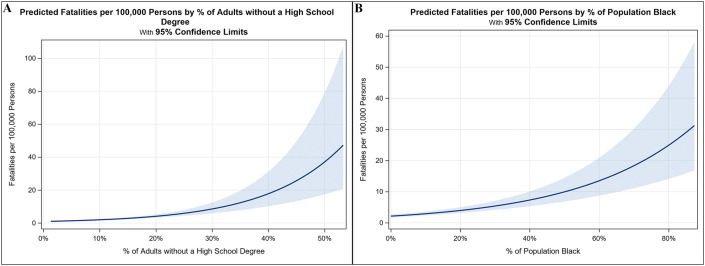
Higher COVID-19 mortality was associated with higher income but lower education, higher employment rate, higher proportion of black Americans, older residents, and less obesity (Table 2). The significant socio-economic associations were the percentage of adults without a high school degree (RR 1.08), median income ratio (RR 1.01), and percentage of adults not working (RR 0.98). Significant demographic and health-related associations included the percentage of population aged older than 65 years (RR 1.07), proportion of black residents (RR 1.03), and obesity prevalence (RR 0.96). Fig. 4 shows the risk-adjusted predicted fatalities per 100,000 persons for the two strongest socio-economic associations, the percentage of adults without a high school degree and proportion of black residents.
Fig. 4.
Adjusted predicted COVID-19 fatalities per 100,000 persons for the three strongest socio-economic factors. (A) Percentage of adults without a high school degree and (B) percentage of population Black. Estimates are shown holding all other predictors at mean values (Supplemental Table 1). COVID-19 = coronavirus disease 2019.
Discussion
The present study highlights community-level socio-economic disparities in COVID-19 prevalence and mortality within the United States. Severely distressed communities account for a disproportionately higher number of deaths per 100,000 persons. However, poverty and unemployment were protective against contracting COVID-19, highlighting the unique risks of a pandemic and limitations of composite metrics of socio-economic status. Risk-adjusted analysis identified two socio-economic determinants of health as having the strongest association with both population-adjusted cases and fatalities: lower education level and higher proportion of black residents. Although age, comorbidities, and overall health status also appear to impact COVID-19 prevalence and outcomes, socio-economic factors have higher risk ratios and represent the strongest associated factors with both number of cases and fatalities.
Using the composite DCI metric, which includes seven different socio-economic factors, we found that counties with lower socio-economic status (higher DCI score) have higher COVID-19 death rates per 100,000 persons compared with non-distressed counties. Rates of high mortality in distressed communities are multifactorial, likely accounting for differences in age, number of chronic medical conditions per person, and socio-economic status. One of the strongest predictors of mortality from COVID-19 is age, where in Italy the case fatality rate in octogenarians was more than 20%.3 , 17 Distressed communities are rapidly aging and have a greater proportion of elderly residents.18 In addition, lower socio-economic status has been associated with a higher burden of chronic medical conditions and comorbidities.13 These underlying medical comorbidities have also been shown to increase COVID-19–related mortality.2 However, in the present data, we demonstrate a stronger association between socio-economic factors than underlying medical conditions with only obesity inversely associated with COVID-19 mortality. Obesity has traditionally been considered protective against acute respiratory distress syndrome–related mortality, but preliminary data on COVID-19 suggest possible increased risk.19 , 20 There are significant overlaps in socio-economic status and obesity that were not accounted for in other studies, and the independent effect of obesity of COVID-19–related cases and mortality requires further study.
Distressed communities tend to be disproportionately comprising black Americans, and these individuals have higher COVID-19 mortality rates.4, 5, 6 , 21 A study not yet published found that communities with a higher proportion of black residents had increased COVID-19 cases (relative risk 1.24) and deaths (relative risk 1.18).22 Our study corroborates these findings where a higher proportion of black residents were associated with both increased cases and fatalities per 100,000 persons. The exact reasons to explain these associations cannot be determined from the current data sets and analysis, and a more thorough understanding of racial inequities requires nationwide disaggregated data. The underlying etiology for the racial inequity likely reflects trends of economic, geographic, and health disparities seen with socioeconomically disadvantaged populations. In addition, the impact of systemic flaws in the structural organization of American society with racism, access to health care, and community-level resources should not be underestimated.
The COVID-19 pandemic in America is becoming increasingly a story of economics. Significant attention has focused on how public health measures to save lives (social distancing, closure of all non-essential business, stopping the delivery of all non-urgent/emergent health care) have resulted in one of the largest increases in unemployment in American history. However, our data focus on the opposite relationship, how economics is affecting who contracts and dies from COVID-19.23 Those individuals in frontline jobs who maintain employment are at increased risk of contracting coronavirus, particularly with concerns related to asymptomatic spread in the setting of inadequate testing.24 Our data are supportive of this theory in two ways. First, higher income and less poverty both were associated with higher rates of COVID-19 cases while higher unemployment was associated with fewer COVID-19 fatalities. These findings suggesting a significant amount of transmission is through the workplace. Second, lower education levels were also associated with contracting COVID-19. This could be due to frontline jobs being disproportionately low paying and without a requirement of an advanced degree.23 The education relationship is relatively strong (RR 1.10) compared with other metrics, which may be due to the highest paying jobs being more amenable to remote working, making employment and income imperfect markers of risk.
This public health trope of economics underpinning health inequalities is true not only in America but also was highlighted in 1980 in Britain with the Black Report.25 One of the expectations of establishing the National Health Service with universal healthcare coverage was to eliminate health disparities. However, thirty years after, it was made clear that economic divisions (employment, income, education, housing, and so on) were only widening health disparities in the United Kingdom. The next few decades saw focused efforts to identify the causes of morbidity and mortality differences, develop better metrics to gauge true health disparities, and quantify those differences.26, 27, 28 COVID-19 represents a rare disruptive opportunity to refocus our efforts on using this knowledge to reverse health disparities.
Now is the time to be proactive in the management of this pandemic and focus allocation of federal and state-level resources to these distressed communities. As society attempts to safely reverse restrictive public health measures such as stay at home orders, other more resource-intensive tools including testing and contact tracing will be required. The DCI may help to guide public health interventions to areas most in need. Clear and decisive actions are needed to help safeguard vulnerable populations who are at the highest risk for complications and death.29
This study is limited by the lack of epidemiologic data available at the zip code level or widespread detailed demographic information, representing systemic failures of the healthcare system which limits our ability to adequately respond in an equitable manner. Socio-economic factors are interrelated, and collinearity limits the utility of an epidemiologic study design such as this. Individual-level SES analyses are required to better understand the interaction of all aspects of Socioeconomic status on COVID-19. In addition, the delay in testing availability and narrow testing criteria vastly overestimate the case fatality rate, but it is unclear how this varies across the United States. Better racial data are needed regarding COVID-19 to truly understand the disparities by race beyond a rough estimation for black Americans. Finally, the DCI only accounts for a small portion of variability in case fatality rates, suggesting social determinants of health are only one factor in determining COVID-19–related outcomes.
In summary, socio-economic determinants of health are associated with COVID-19 prevalence and mortality. Severely distressed counties with low socio-economic status have higher rates of both COVID-19 cases and fatalities than communities with higher socio-economic status. The socio-economic influence is broad, with many components of the DCI (education level, income, and poverty rates) being associated with COVID-19 cases. However, due to the transmission patterns of COVID-19 in the United States, higher income but lower education levels were associated with COVID-19 cases and fatalities. A higher proportion of black residents were also one of the strongest associations with COVID-19 cases and fatalities. Socio-economic factors and the DCI could help allocate appropriate public health resources in areas with lower socio-economic status, a critical step toward an equitable fight against COVID-19.
Author statements
Ethical approval
This study is exempt from IRB review.
Funding
No funding was utilized for this research.
Competing interests
The authors report no conflicts of interest.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.puhe.2020.09.016.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Johns Hopkins Coronavirus Resource Center 2020. https://coronavirus.jhu.edu/map.htmlhttps://coronavirus.jhu.edu/map.html Available from:
- 2.Grasselli G., Zangrillo A., Zanella A., Antonelli M., Cabrini L., Castelli A. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the lombardy region, Italy. JAMA. 2020;323(16):1574–1581. doi: 10.1001/jama.2020.5394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Onder G., Rezza G., Brusaferro S. Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. J Am Med Assoc. 2020;323(18):1775–1776. doi: 10.1001/jama.2020.4683. [DOI] [PubMed] [Google Scholar]
- 4.Garg S., Kim L., Whitaker M., O'Halloran A., Cummings C., Holstein R. Hospitalization rates and characteristics of patients hospitalized with laboratory-confirmed coronavirus disease 2019 - COVID-NET, 14 states, March 1-30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:458–464. doi: 10.15585/mmwr.mm6915e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Summers J.U.S. National Public Radio; 2020. Surgeon general: people of color 'socially predisposed' to coronavirus exposure.https://www.npr.org/sections/coronavirus-live-updates/2020/04/10/832026070/u-s-surgeon-general-people-of-color-socially-predisposed-to-coronavirus-exposure [serial on the Internet] Available from: [Google Scholar]
- 6.Breslow J. National Public Radio; 2020. Why misinformation and distrust are making COVID-19 more dangerous for black America.https://www.npr.org/sections/coronavirus-live-updates/2020/04/10/832039813/why-misinformation-and-distrust-is-making-covid-19-more-dangerous-for-black-amer [serial on the Internet] Available from: [Google Scholar]
- 7.Choo E.K. COVID-19 fault lines. Lancet. 2020;395:1333. doi: 10.1016/S0140-6736(20)30812-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang Z., Tang K. Combating COVID-19: health equity matters. Nat Med. 2020;26:458. doi: 10.1038/s41591-020-0823-6. [DOI] [PubMed] [Google Scholar]
- 9.Armitage R., Nellums L.B. Considering inequalities in the school closure response to COVID-19. Lancet Glob Health. 2020;8:e644. doi: 10.1016/S2214-109X(20)30116-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dorn A.V., Cooney R.E., Sabin M.L. COVID-19 exacerbating inequalities in the US. Lancet. 2020;395:1243–1244. doi: 10.1016/S0140-6736(20)30893-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.The 2016 distressed communities Index. Economic Innovation Group; 2016. http://eig.org/dci Available from: [Google Scholar]
- 12.Mehaffey J.H., Hawkins R.B., Charles E.J., Turrentine F.E., Hallowell P.T., Friel C. Socioeconomic "distressed communities index" improves surgical risk-adjustment. Ann Surg. 2020;271:470–474. doi: 10.1097/SLA.0000000000002997. [DOI] [PubMed] [Google Scholar]
- 13.Hawkins R.B., Mehaffey J.H., Charles E.J., Kern J.A., Schneider E.B., Tracci M.C. Socioeconomically Distressed Communities Index independently predicts major adverse limb events after infrainguinal bypass in a national cohort. J Vasc Surg. 2019;70:1985–19893 e8. doi: 10.1016/j.jvs.2019.03.060. [DOI] [PubMed] [Google Scholar]
- 14.Charles E.J., Mehaffey J.H., Hawkins R.B., Fonner C.E., Yarboro L.T., Quader M.A. Socioeconomic distressed communities index predicts risk-adjusted mortality after cardiac surgery. Ann Thorac Surg. 2019;107:1706–1712. doi: 10.1016/j.athoracsur.2018.12.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Coronavirus Locations: COVID-19 Map by County and State. USAFacts; USAFacts [May 2, 2020]; Available from: https://usafacts.org/visualizations/coronavirus-covid-19-spread-map/.
- 16.Razzaghi H., Wang Y., Lu H., Marshall K.E., Dowling N.F., Paz-Bailey G. Estimated county-level prevalence of selected underlying medical conditions associated with increased risk for severe COVID-19 illness - United States, 2018. MMWR Morb Mortal Wkly Rep. 2020;69:945–950. doi: 10.15585/mmwr.mm6929a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Verity R., Okell L.C., Dorigatti I., Winskill P., Whittaker C., Imai N. Estimates of the severity of coronavirus disease 2019: a model-based analysis. Lancet Infect Dis. 2020;20(6):669–677. doi: 10.1016/S1473-3099(20)30243-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fikri K., Lettieri J. 2018. From great recession to great reshuffling: charting A decade of change across American communities: the economic innovation group. [Google Scholar]
- 19.Popkin B.M., Du S., Green W.D., Beck M.A., Algaith T., Herbst C.H. Individuals with obesity and COVID-19: a global perspective on the epidemiology and biological relationships. Obes Rev. 2020;21(11):e13128. doi: 10.1111/obr.13128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ni Y.N., Luo J., Yu H., Wang Y.W., Hu Y.H., Liu D. Can body mass index predict clinical outcomes for patients with acute lung injury/acute respiratory distress syndrome? A meta-analysis. Crit Care. 2017;21:36. doi: 10.1186/s13054-017-1615-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ozimek A., Fikri K., Lettieri J. 2019. From managing decline to building the future: could A Heartland Visa help struggling regions?: Economic innovation Group. [Google Scholar]
- 22.Millett G.A., Jones A.T., Benkeser D., Baral S., Mercer L., Beyrer C. Foundation for AIDS Research; 2020. Assessing differential impacts of COVID-19 on black communities. Pre-print on amfAR. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gamio L. The New York Times; 2020. The workers who face the greatest coronavirus risk. [Google Scholar]
- 24.Furukawa N.W., Brooks J.T., Sobel J. Evidence supporting transmission of severe acute respiratory syndrome coronavirus 2 while presymptomatic or asymptomatic. Emerg Infect Dis. 2020;26 doi: 10.3201/eid2607.201595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Black S.D. Department of Health and Social Security; 1980. Inequalities in health: report of a research working group. [Google Scholar]
- 26.Marmot M. Social determinants of health inequalities. Lancet. 2005;365:1099–1104. doi: 10.1016/S0140-6736(05)71146-6. [DOI] [PubMed] [Google Scholar]
- 27.Acheson D. hMso; London: 1998. Inequalities in health: report of an independent inquiry. [Google Scholar]
- 28.Smith G.D., Bartley M., Blane D. The Black report on socioeconomic inequalities in health 10 years on. BMJ. 1990;301:373–377. doi: 10.1136/bmj.301.6748.373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pan A., Liu L., Wang C., Guo H., Hao X., Wang Q. Association of public health interventions with the epidemiology of the COVID-19 outbreak in Wuhan, China. J Am Med Assoc. 2020;323(19):1915–1923. doi: 10.1001/jama.2020.6130. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.