Abstract
Objectives
To present a comprehensive review of current literature available on Corona virus disease and dentistry, modifications required in dental and laboratory settings; and recommended disinfection protocols in current scenario. Special emphasis has been given to discuss guidelines for handling different prosthodontic procedures and implications of this pandemic on prosthodontic practice, education and research.
Materials and methods
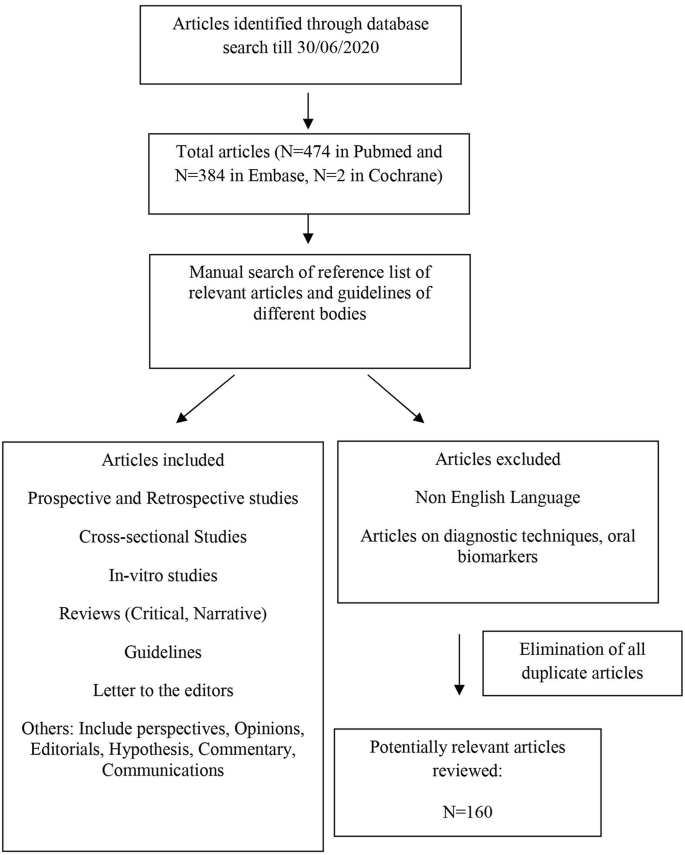
Relevant literature pertaining to COVID-19 and dentistry was scrutinized on electronic search engines including PubMed, EMBASE and Cochrane. Guidelines given by various organizations, institutions, national and international regulatory bodies and Indian Prosthodontic Society were also consulted to gather information pertaining to the objectives of our review.
Results
and observations: A total of 160 articles including cross-sectional studies, in vitro study, narrative reviews, letters to the editor and opinions were found to be relevant in accordance with our search strategy. Documented literature revealed that Covid-19 pandemic has culminated in serious clinical, financial and psychological implications in the field of dentistry. Certain steps such as adoption of teledentistry, judicious use of protective equipment, use of rubber dams, pre-procedural rinses have been suggested unanimously. However, there is a dearth of evidence-based recommendations in literature. Data regarding consequences of delaying prosthodontic procedures and patients’ perspectives is also sparse.
Conclusion
The COVID-19 necessitates the need to adopt a balanced approach while treating patients and safeguarding the dental professionals at the same time. Risk-benefit ratio has to be assessed along with stringent following of guidelines and disinfection protocols to combat this unprecedented situation.
Keywords: Covid-19, Dentistry, SARS-CoV-2, Prosthodontics, Guidelines, Recommendations
1. Introduction
Covid-19 (Corona virus disease 2019) is a RNA-based virus that came to light in December 2019 when China informed World Health Organization (WHO) of rampant spread of pneumonia-like cases.1 On March 11, 2020, Covid-19 was declared as a pandemic, a public health crisis that is still having a rippling effect in every sector.2 Due to its implications, dental healthcare has faced several clinical, psychological and financial repercussions, having unforeseen consequences on dental professionals, patients and lab personnels.3,4
Covid-19 virus, having diameter in the range of 100 nm, primarily transmits through person to person contact and direct contact with respiratory droplets.5 The word ‘corona’ is derived from its appearance as ‘crown-like’ while being observed under the electron microscope.6 It primarily transmits through person to person contact and direct contact with respiratory droplets. Spread through asymptomatic carriers has also been recently documented and is one of the major reasons for creating fear and dilemma in the minds of dental practitioners.7 The close proximity to oral fluids, aerosols and long incubation period of the virus, place the dental fraternity at a high risk of contracting and transmitting the virus.8 Ministry of health and family welfare (MOHFW), India has formulated specific guidelines and is playing a pivotal role to constantly update them with changing dynamics of disease. At present, only emergency and urgent procedures have been recommended to be taken up, with extreme focus on personal protective equipment and disinfection protocols.9 However, the fleeting nature of specialty-wise guidelines and overlap of recommendations given by various organizations; has convoluted its implementation in regular dental setup.10
The prosthodontic procedures especially need to be modified during the COVID times. The target population, comprising of the geriatric group with or without co-morbidities, post-cancer immune compromised patients or patients with extra-oral maxillofacial defects requiring prosthetic rehabilitation, makes it imperative to lay down guidelines which are versatile and compliant by the patients and doctors as well.11,12 The prosthodontist community has to deal with multiple saliva- and blood-contaminating articles which can serve as a potent source of viral transmission. The overwhelming dependence on the aerosol generating instruments during prosthodontic rehabilitation needs urgent and innovative strategies to combat the spread. Sudden lockdown world-wide has left many prosthodontic procedures pending at different steps. The indispensable role played by the laboratory in the prosthodontic reconstruction cannot be undermined and hence extra caution needs to be taken at every checkpoint: collection of the dental impression, pouring of the models, designing and fabrication of prosthesis, finishing and polishing using lathe-driven machines and delivery of the final work at the clinics. Additionally, the consequences can be financially and psychologically devastating for patients, the clinicians and; the lab personnel who have not received their payments owing to incomplete procedures.13
Thus, with a basic question in mind that how prosthodontics should be practiced during COVID-19 pandemic, an effort has been made to review the existent literature and guidelines from different national and international sources and suggest implementation of a systematic workflow by the dental professionals to ensure a safe practice.
2. Methods and methodology
Extensive search of literature was performed on electronic database PUBMED, EMBASE and Cochrane by three authors (VB, RJ and GP). Fig. 1 depicts the sequential steps involved in procuring the data and analyzing the shortlisted articles. The keywords/medical subject headings (MeSH) terms used for the search strategies were (“Covid-19” OR “coronavirus”) AND (“prosthodontics” OR “dentistry”) AND (“guidelines” OR “review”). Cross sectional surveys and studies, in vitro studies, retrospective studies, literature reviews and letter to Editor, opinions, editorials published in English language till June 30, 2020 were included. Duplicate articles and articles in language other than English were excluded. Several guidelines recommended by various international and national organizations such as World Health organization (WHO), Centers for disease control and prevention (CDC), Ministry of health and welfare, India and Indian Prosthodontic society (IPS) were also referred to. Certain opinions expressed in the review are on the basis of clinical and academic experience of the authors. Statistical analysis was not performed because of the heterogeneity of the data and lack of clinical trials published so far.
Fig. 1.
Flowchart of search strategy and results.
3. Observations and discussion
Distribution of types of publications and their country wise representation have been given in Fig. 4, Fig. 5. Various reviews on guidelines and recommendations have been published in literature based on current scenario of pandemic in different countries. It is proposed to follow these guidelines to ensure a safe practice; which are hereby discussed as general (applicable to all dental professionals) and prosthodontic specific considerations.
Fig. 4.
Country wise distribution of the shortlisted articles.
Fig. 5.
Categorisation of the articles based on the publication types.
3.1. General considerations
3.1.1. Recommendations for designing of existent clinics and new clinic set up
As per the need of the hour, entire clinical setup has been recommended to have separate areas for donning/doffing, a separate sterilization room along with the segregation of areas into different zones (Fig. 2).14 Its feasibility depends upon basic infrastructure, total area available, number of auxiliary health workers and number of patients reporting per day; all these vary substantially in Government hospitals and private set ups.
Fig. 2.
Suggested blueprint for an operational clinic.
3.1.1.1. ZONE A: reception and waiting area
This area is dedicated to gaining basic information about the patient using individual clinic or institution-based protocol. Non-contact temperature recording, sensor taps, contactless sanitizer dispensers are essential additions in this zone. Here the patient is requested to remove accessories like jewellery, watch etc. and sanitize their hands thoroughly.15 One attendant per needy patient is preferable owing to the norm of maintaining physical distancing.16 Patient should be provided with triple layer facemask, disposable shoe-covers, head cap and gloves. A glass barrier can be installed at the reception counter to avoid transmission of droplets between patient and the staff.17 A screening form (in local and national languages) (Fig. 3) and an informed consent should be duly filled by the patient in the language of his or her preference. Online consent before physical attendance of the patient is advisable, keeping the online signature on record. Posters can be designed and displayed to educate patients regarding hand hygiene, respiratory etiquettes etc using one's creativity. A pulse oximeter is a noninvasive, wireless finger tool recommended in screening area for monitoring of significant changes in arterial oxygen saturation in considerably less time, especially in asymptomatic individuals.18 If the oxygen saturation is less than 93%, referral to a physician for detailed screening is advisable.19
Fig. 3.
Suggested screening form.
In India, the use of the indigenous “Aarogya setu application” facilitates COVID-19 contact tracing, and self-assessment.20, 21 “Namastey campaign” was also started to minimize the transmission of the virus.22 Non-overlapping appointments with a gap of at least 15 min, physical distancing, digital payments are few other recommendations to be followed.14 Levels of Personal Protective Equipment (PPE) which includes gloves, impervious body suit, mask, visor/hood and linen/disposable gown and their indications have been tabulated in Table 1, Table 2.
Table 1.
Level of PPE based on the type of procedure and zone classification.
| LEVEL OF PERSONAL PROTECTION EQUIPMENT | RECOMMENDED CATEGORY |
ITEMS INCLUDED |
|---|---|---|
| PRIMARY LEVEL | RECEPTION AREA AND SCREENING AREA (Zone A and B) |
|
| SECONDARY LEVEL | NON- AEROSOL GENERATING PROCEDURE (Zone C) |
|
| TERTIARY LEVEL | AEROSOL GENERATING PROCEDURE (Zone D) |
|
Table 2.
Recommended Personal protection equipment for health care workers.
| Health care worker | Gloves | Impervious body suit | Mask | Visor/Hood | Linen/Disposable gown |
|---|---|---|---|---|---|
| Security guard | ✓ | ✗ | N-95 | ✓ | ✗ |
| Registration counter/(behind glass curtain | ✓ | ✗ | Surgical | ✗ | ✗ |
| Registration counter/(without glass curtain) | ✓ | ✗ | Surgical | ✓ | ✗ |
| Screening room/oral examination | ✓ | ✗ | Surgical/N95 | ✓ | ✓ |
| Dental procedures (non AGP) | ✓ | ✗ | N-95 | ✓ | ✓ |
| Dental procedures (AGP)/minor OT | ✓ | ✓ | N-95 | ✓ | ✓ |
| Sanitation staff | ✓ | ✗ (Thick boots) |
N-95 | ✗ | ✓ |
3.1.1.2. ZONE B: Screening area
Initial screening and diagnosis, using sterilized instruments is to be done in this zone. Maximum viral load is present at disease onset, mainly in the upper respiratory tract.23 According to Bidra et al., pre-procedural mouth rinse using oral preparation of Povidone-Iodine (PVP-I) in a concentration as low as 0.5% for at least 15 s can completely deactivate the virus.24 The strong virucidal activity of povidone iodine can be effectively exploited by employing it as mouth gargle against COVID-19.25 However lack of evidence-based research including randomized controlled trials warrants discretion before any final recommendation. Other chemical based mouth rinses advocated to disrupt the viral lipid membrane include ethanol, chlorhexidine, cetylperidinium chloride and hydrogen peroxide. However, their efficacy specifically against coronaviruses needs to be confirmed.26
During this phase, an Orthopantomogram (OPG) and cone-beam computed tomography (CBCT) are recommended rather than the intraoral radiographs to prevent salivary contamination.27,28 But OPG lacks diagnostic precision and CBCT exposes the patient to a higher radiation dose as compared to an intraoral radiograph.29 In house facility of taking digital radiographs is preferred rather than sending patients outside for this purpose.
3.1.1.3. ZONE C: Non-aerosol generating area
This section involves dentist performing those procedures where the use of airotor handpieces and ultrasonic scalers is not incorporated. Hence, priority is given to hand instruments such as spoon excavators and chemical-based caries removal agents. PPE is the sole effective method within the limit of administrative, environmental controls to prevent the spread of infection.30 The donning and doffing should be done in the specified dedicated areas following sequential steps as lay down by CDC.31 Four-hand dentistry with involvement of digital workflow is suggested.32
3.1.1.4. ZONE D: aerosol generating area
The use of high-speed hand pieces generates aerosols that are defined as particles which are less than 50 μm in diameter.33 It has been postulated that aerosols have a tendency to remain suspended for at least 30 min even after the completion of the procedure and can reach up to 2 feet from the dental chair.34 As the risk of transmission is high in this area and even the false negative rate of Covid Antigen test is around 30%, it becomes imperative to adopt universal precautions/OSHA guidelines.35,36 Only essential items should be kept in open while maximum material and instruments should be kept in closed cabinets.
MoHFW has suggested avoiding switching on ceiling fans during such procedures; frequent servicing of air conditioners and; blocking the return air vents in centrally air conditioned operatories.9 Use of carpets should be discontinued. However, in clinics that are already established and have a limitation due to lack of space and ventilation, it is advisable to filter the contaminated room-air using high volume evacuator and high efficiency particulate arrestor (HEPA) filters.37 Although expensive option, the HEPA filters have been documented to remove 99% of particles measuring 0.3 μm in diameter.8 According to the filtration efficiency, HEPA-13 or H-14 are recommended and the size depends on the total area of the clinic. However, it must be emphasized that these filters are an adjunct to the core strategies needed to combat the transmission. There is paucity in evidence-based research highlighting their role in COVID-19 era. Another recommendation, is the incorporation of the negative pressure rooms to treat the suspected or confirmed cases of COVID-19.38 Sufficient ventilation, both mechanical and natural with the help of exhaust fans, is suggested to ensure dilution of viral load and expulsion of infected air.39
In addition to the above precautions, a prior COVID test for patients undergoing aerosol generating procedures is advisable depending upon the feasibility and resources available.40 It is generally preferred to conduct such procedures during the latter part of the day or keeping a gap of 2 h before taking up the next patient. Eight o'clock chair position should be avoided completely to avoid direct contact with the splatter.6 Rubber dams, low-speed anti-retraction hand piece and high-volume suctions rather than chair side suctions are highly recommended.39 According to Peng et al., rubber dams are capable of reducing airborne particles by 70% within three feet wide operatory.32
3.1.2. Teleconsultation/teledentistry/videoconferencing
Teledentistry must be encouraged as the first mode of interaction between a dentist and a patient during the COVID era.41 It serves as an effective means to evaluate the intensity of the patient's complaint, thereby categorizing the procedure into an emergency or urgent one.42 Lending a patient ear to someone ensures ease in anxiety and fear amongst the distressed population.43 It helps the practitioner to record a detailed case history without coming in actual contact with the patient. Education posters regarding hygiene or respiratory etiquettes, screenshots of updated Aarogya setu App can be shared between dentist and patient on the phone itself. Video call with the patient can also help to understand the situation better and guide them as required.44 However, in view of difficult access and understanding in lower socioeconomic groups in India, this facility has limited significance. Other limitations include undue prescription of antibiotics and analgesics instead of treating etiology may sometime worsen the situation and expose the patient to a higher risk and side effects.
3.1.3. Guidelines for using facemasks and respirators
The selection of right mask in a “proper fit-checked” manner is an absolute necessity measure for the frontline workers while screening and treating the patient. The updated WHO guidelines (dated 6th June, 2020) calls for “targeted continuous medical mask use, which refers to the practice of wearing a medical mask by all health workers and caregivers working in clinical areas during all routine activities throughout the entire shift.45
According to United States based National Institute for Occupational Safety and Health (NIOSH), the respirators are of three categories: R, P and N. According to the European standard, the respirators are divided into FFP1, FFP2, and FFP3 where FFP is an abbreviation for filtering face piece. The FFP2 is similar to N95 in its filtration capacity and it provides two-way protection.46 Respirators with valves protect only the wearer while triple layer masks protect the people in surroundings not the wearer. Considering the high transmission rate of the virus, health workers should wear a respirator (N95 or FFP2 or FFP3 standard; or equivalent) especially during aerosol generating procedures.47 Reuse of N95 and respirators with valve should be avoided as it has no evidence based recommendation.48
3.1.4. Disinfection protocols for dental clinics and laboratories
Prevention of cross infection and disinfection of the clinic and laboratory as well are essential steps to maintain a pristine environment by preventing the transmission. Chairside assistants, support staff and laboratory technicians should be trained and recruited on rotational basis with an aim to keep minimum workforce at a particular time.6 Constant monitoring of staff involved in disinfection and waste disposal should be done to avoid any lapses in the protocol. COVID waste should be disposed in double layer bags, used PPEs should be disposed of in yellow bin, biomedical waste management (BMW) should be done in accordance with latest guidelines given in the year 2016 and amended in 2018.49 BMW generated during the screening, treatment, management and immunization from COVID-19 patients and healthcare staff working in wards should be segregated effectively.50 Sodium hypochlorite solution in various concentrations (0.1%–1%), Ethanol (70–90%) and vaporized hydrogen are commonly recommended solutions for surface disinfection.51,52 Additionally, the role of UV-C (wavelength = 200–280 nm) has been suggested as a method of terminal disinfection for dental clinics and laboratories.53 The advantages of ultraviolet radiation is that it is safe, does not leave any residues, an effective alternative to dangerous carcinogenic chemical disinfectants, has a wide spectrum of germicidal activity and can be used in presence of human beings.54,55 But still it has to be used on individual discretion as it lacks evidence for its specific action against corona virus.
3.1.5. Fumigation versus fogging
Fumigation and fogging are two methods used for disinfection of clinics and laboratory. In fumigation, formaldehyde solution is mixed with potassium permanganate in a fixed proportion. This combination gives rise to fumes, which are very effective in killing bacteria, fungus and their spores but formaldehyde is a known carcinogen, hence fumigation is obsolete now. Fogging can be done with the mixture of hydrogen peroxide and silver ion solution or third generation quaternary ammonium compounds (QACs).56 It is a rapid, effective and residual-free method making it a more preferred protocol for clinic disinfection. This method of “no-touch surface disinfection” usually takes 45 min followed by contact time/dwell time of an hour. It is recommended to carry out these procedures where circulation of clean and natural air is possible post procedure.9
3.2. Prosthodontic considerations during covid 19 era
Dentists are bound by ethical obligation of treating patients even in times of emergency and personal obligation to keep their families and staff safe. MOHFW recommended postponing all elective procedures indefinitely and to manage only emergency procedures in red zones while urgent procedures can be done in orange and green zones (Table 3).9 The implications of Covid in different sectors of dentistry have been depicted in Table 4.
Table 3.
Management of Urgent Prosthodontic procedures.
| Presentation/Condition | Consequences/risk | Intervention required |
|---|---|---|
| Mobile/Faulty prosthesis | Risk of aspiration | Removal with a crown remover |
| Fixed faulty prosthesis | Pain/Continued inflammation of underlying tissues/food impaction/source of infection | Removal with airotor/crown remover |
| Infection around prosthesis | Pain/Spread of infection | Removal of prosthesis |
| Perimplantitis | Pain/Spread of infection/Implat failure | Antibiotics/Currettage |
| Sensitivity/caries of abutment underneath fixed prosthesis | Pain/pulp exposure | Endodontic intervention |
| Fabrication of surgical and interim obturators | Problems in speech and deglutition | Impressions and delivery of prosthesis |
| Dislodged prosthesis needing recementation | Compromise in esthetics and function, pulpal sensitivity, Supraeruption of teeth | Recementation |
Table 4.
The implications of COVID 19 on different sectors in dentistry.
| Clinical Implications |
|
| Psychological implications |
|
| Financial implications |
|
| Academic implications66 |
|
3.2.1. Removable prosthodontics
This includes fabrication of complete and partial dentures. Age has been documented as primary risk factor for increasing COVID-19 mortality rate, compounded with the presence of co-morbidities.57 Hence, a thorough medical case history is a must before starting any geriatric patient to evaluate risk versus need benefit. Completion of pending procedures must be given preference in comparison to starting of new cases to avoid unnecessary implications.
3.2.1.1. Chair-side protocol
Fractured prosthesis should be repaired by first disinfecting it thoroughly. Ulcerations or mucosal erosions can be handled through tele consultation by advising some analgesic and antiseptic gels for local application and discontinuation of the prosthesis for the time being. Mild smoothening of sharp borders can be advised with sandpaper if patient can't come to the clinic. Patients should be recalled in the clinic on strict appointment schedule if any further adjustment of the prosthesis is mandatory to restore its function. Denture adjustment should be done using a low speed micro motor. New prosthesis should be fabricated if it is affecting the systemic health of the patient. Primary impressions should be made in well-fitting stock trays and secondary impressions should be made in custom trays which can be discarded after obtaining the master cast. One step border molding can be done to minimize chair side time.
3.2.1.2. Laboratory protocol
Record bases and wax rims should be adjusted on prior basis in order to avoid any modifications after insertion in the mouth. Care should be taken to minimize processing errors in lab and dentures should be remounted to adjust occlusion. This will ensure lesser follow up visits of the patient.
3.2.2. Fixed prosthodontics
The fixed prosthodontics includes fabrication of crowns and bridges, inlays, onlays, smile designing, veneers, full mouth rehabilitation, post and cores etc. These are elective and aerosol generating procedures. So, adherence to strict precautions and disinfection protocols is mandatory. Digital impressions using intraoral scanners is safe alternative but the cost-benefit ratio needs to be taken care of. Papi et al. have compared digital workflow with conventional workflow and concluded that digital method reduces human contact at multiple steps thereby decreasing risk of transmission of virus, saves time and improves efficacy.58
3.2.2.1. Chair side protocol
Use of rubber dam and high vacuum suction are recommended during tooth preparations where supragingival margins are planned.59 This effectively wipes out most of the blood and saliva contaminants; also keeping the viral load to a minimum.60 Clinicians should avoid any undercuts and under-reduction in their tooth preparations. Shade matching should be done by digital spectrophotometers and consent of patient should be taken. Intraoral photographs can be sent online to the laboratory to avoid any shade mismatch. Removal of fractured and faulty prosthesis using crown removers is advisable. Recementation of the dislodged prosthesis can be done, whereas adjustment of the temporary crowns should be done extra-orally using a micromotor. The dental tools such as air rotor and burs should be autoclaved as per manufacturer's instructions. Additional steps include working position of dentist at 11–12 o’ clock, reduced air pressure in 3-way syringes, full protection PPE for both doctor and assistant, use of anti-retraction hand pieces and disposable burs.6 Frequent rinsing and spitting should be prohibited.
3.2.2.2. Laboratory protocol
Fomites can also lead to the spread of the virus.60 Hence, impressions, which can act as route of spreading cross contamination between clinic and lab, should be disinfected (sodium hypochlorite 1% for ten minutes) and stored in disposable pouches.61 If an external laboratory is involved, each work item must be separately stored in a sealed pouch and collected by the delivery boy. The delivery boy should also be provided with basic protective equipment. The prosthesis should be immersed in disinfectant before sending back to the clinic. Dentist can wash and store the prosthesis in a mouthwash before insertion in patient's mouth. Restorations should be fabricated on mounted models on an articulator. This will reduce the probability of repeating the procedure, time required for chairside adjustment, and use of micro motors or airotors. Consent for the final anterior restorations can be taken by sending the pictures to the patient before finalizing them.
Lab personnel and technician should practice physical distancing, hand hygiene and optimal disinfection. Computer aided designed and milled restorations should be preferred over conventional casting. Casting metal invariably involves generation of fumes and splatter. Also, digital workflow is proposed to minimize the salivary contact between different materials.58
3.2.3. Implant surgery & prosthodontics
3.2.3.1. Chair side protocol
Implant dentistry is the most fascinating and earning division for Prosthodontists these days. Deferring patients for placement of implants can lead to big financial and mental trauma to the dental and lab personnel. But implant treatment planning involves multiple dental visits which along with use of surgical aerosol generating hand pieces call for extreme precaution in regard to disinfection and infection control. Following recommendations are suggested by authors though personal discretion is a must. Healthy patients with no other co-morbidities can be taken up based on CBCT and virtual planning. During surgery, slow speed drilling with sharp drills is preferable. Intermittent external irrigation along with high volume suction should be done. Use of ultrasonic devices and piezoelectric surgery should be minimized; whereas use of osteotomes should be encouraged in order to reduce aerosol formation.62 Immediate implants with immediate loading should be taken up wherever indicated as they require lesser time number of visits. It is advisable to avoid complex full mouth procedures. Digital impression with scan bodies is suggested as an alternative to conventional impression making.
3.2.3.2. Laboratory protocol
Implant impressions and components need to be carefully disinfected/autoclaved before reusing them. Careful impression making using resin jig and precise pouring of the impressions are a must in order to prevent repetition of any chair-side step.
3.2.4. Intraoral and extra oral maxillofacial prostheses
Fabrication of surgical and interim obturators must be done at this time in order to restore the function of patients with intraoral defects. But owing to immune compromised status of post-operative carcinoma patients, they should be deferred for definitive obturator fabrication. Facial defects may act as esthetic urgencies for the patients who are going out of homes for their daily routines and have to interact with people. So, fabrication of extra oral prosthesis should be considered after assessing the risk benefit ratio. Additionally, psychological counseling and motivation for the maintenance of the prosthesis can be done through Teledentistry.63
3.2.5. Handling dental impressions
Dental impressions are a high risk source of infection transmission. Autoclaved stock trays should be used and material should be loaded carefully to avoid gag reflex. Impression should be kept under running water avoiding direct flow over tissue surface to avoid losing surface details. Spray disinfectant can be used for chair side disinfection followed by packing in zip lock bags before sending the impressions to laboratory for pouring. Recommendations given in Table 5 should be followed in the lab for disinfection as per the material.64 Work authorization forms should be sent in separate zip lock bag.
Table 5.
Disinfection of various materials and equipment in a dental setting.
| IMPRESSION MATERIAL | METHOD AND MATERIAL OF DISNFECTION |
|---|---|
| Alginate and Polyether (hydrophilic) |
0.5–1% Sodium Hypochlorite (1:10 dilution) or 1:213 iodophors (Spray) |
| Zinc-oxide eugenol impression paste | 2% Glutaraldehyde or 1:213 Iodophors (immersion) for 10 min |
| Impression Compound | Sodium hypochlorite (1:10 dilution) (immersion) |
| Rubber-base impression materials | 2% Glutaraldehyde or Cidex |
| Wax rims | Iodophor disinfection sprays |
| Acrylic appliance | Povidone iodine/1% Sodium hypochlorite, store in mouthwash before use |
| Fixed prosthesis | Immersion in cidex, or 1% Sod. Hypochlorite |
| Gypsum casts | Microwave irradiation for 5 min at 100 W |
| Tips of intraoral scanners | Rubbing with alcohol based disinfectants |
4. Conclusion
The intent of this paper was to discuss the effect of COVID-19 on dental practice as it is a matter of global concern. Still dentists across the world are struggling with a plethora of questions, fear, dilemma and financial crisis. On one hand, it is affecting the mental health of the dentists while on the other hand; dental health and needs of the patients are at stake. Moreover, evidence-based recommendations are still lacking. Authors have attempted to consolidate the information available so far on this issue so that we can offer safe services to our patients and protect ourselves too from this deadly corona virus. The guidelines have been summarized in Table 6.
Table 6.
Summary.
| For the Clinician |
|
|
|
|
| For the Patient |
|
|
|
| For the Clinic |
|
|
|
|
|
| For the Laboratory |
|
|
|
Declaration of competing interest
None.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jobcr.2020.10.010.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Lu H., Stratton C.W., Tang Y.W. Outbreak of pneumonia of unknown etiology in Wuhan, China: the mystery and the miracle. J Med Virol. 2020;92:401. doi: 10.1002/jmv.25678. 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Balkhair A.A. COVID-19 pandemic. A new chapter in the history of infectious diseases. Oman Med J. 2020;35:e123. doi: 10.5001/omj.2020.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.José G.O.M., Raquel O.M.A., Bendición D.R., Martín R.M., María C.D. Perceived vulnerability to coronavirus infection: impact on dental practice. Braz Oral Res. 2020;34:e044. doi: 10.1590/1807-3107bor-2020.vol34.0044. [DOI] [PubMed] [Google Scholar]
- 4.Ghani F. Covid-19 Outbreak - immediate and long-term impacts on the dental profession. Pak J Med Sci. 2020;36:S126–S129. doi: 10.12669/pjms.36.COVID19-S4.2698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Boopathi S., Poma A.B., Kolandaivel P. Novel 2019 coronavirus structure, mechanism of action, antiviral drug promises and rule out against its treatment. J Biomol Struct Dyn. 2020:1–10. doi: 10.1080/07391102.2020.1758788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bhanushali P., Katge F., Deshpande S., Chimata V.K., Shetty S., Pradhan D. COVID-19: changing trends and its impact on future of dentistry. Int J Dent. 2020;2020 doi: 10.1155/2020/8817424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yu X., Yang R. COVID-19 transmission through asymptomatic carriers is a challenge to containment. Influenza Other Respir Viruses. 2020;14:474–475. doi: 10.1111/irv.12743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ge Z.Y., Yang L.M., Xia J.J., Fu X.H., Zhang Y.Z. Possible aerosol transmission of COVID-19 and special precautions in dentistry. J Zhejiang Univ - Sci B. 2020;21:361–368. doi: 10.1631/jzus.B2010010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ministry of Health and Family Welfare, Government of India . Ministry of Health and Family Welfare, Government of India; New Delhi, India: 2019. Guidelines for Dental Professionals in Covid-19 Pandemic Situation.https://www.mohfw.gov.in/pdf/DentalAdvisoryF.pdf [Google Scholar]
- 10.Alharbi A., Alharbi S., Alqaidi S. Guidelines for dental care provision during the COVID-19 pandemic. Saudi Dent J. 2020;32:181–186. doi: 10.1016/j.sdentj.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Marchini L., Ettinger R.L. COVID-19 pandemics and oral health care for older adults. Spec Care Dent. 2020;40:329–331. doi: 10.1111/scd.12465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Martins-chaves R.R., Gomes C.C., Gomez R.S. Immunocompromised patients and coronavirus disease 2019: a review and recommendations for dental health care. Braz Oral Res. 2020;34:e048. doi: 10.1590/1807-3107bor-2020.vol34.0048. [DOI] [PubMed] [Google Scholar]
- 13.Farooq I., Ali S. COVID-19 outbreak and its monetary implications for dental practices, hospitals and healthcare workers. Postgrad Med. 2020 doi: 10.1136/postgradmedj-2020-137781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Clarkson J., Ramsay C., Aceves M. Recommendations for the re-opening of dental services: a rapid review of international sources. Cochrane Oral Health. 2020:1–36. version 1.2. [Google Scholar]
- 15.Villani F.A., Aiuto R., Paglia L., Re D. COVID-19 and dentistry: prevention in dental practice, a literature review. Int J Environ Res Publ Health. 2020;17:4609. doi: 10.3390/ijerph17124609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Abramovitz I., Palmon A., Levy D. Dental care during the coronavirus disease 2019 (COVID-19) outbreak: operatory considerations and clinical aspects. Quintessence Int. 2020;51:418–429. doi: 10.3290/j.qi.a44392. [DOI] [PubMed] [Google Scholar]
- 17.Pan Y., Liu H., Chu C., Li X., Liu S., Lu S. Transmission routes of SARS-CoV-2 and protective measures in dental clinics during the COVID-19 pandemic. Am J Dent. 2020;33:129–134. [PubMed] [Google Scholar]
- 18.Michard F., Shelley K., L'Her E. COVID-19: pulse oximeters in the spotlight. J Clin Monit Comput. 2020:1–4. doi: 10.1007/s10877-020-00550-7. N/A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wang X., Fang J., Zhu Y. Clinical characteristics of non-critically ill patients with novel coronavirus infection (COVID-19) in a Fangcang Hospital. Clin Microbiol Infect. 2020;26:1063–1068. doi: 10.1016/j.cmi.2020.03.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Centre Makes Aarogya Setu App Must for All Central govt Employees". India Today. 2020. [Google Scholar]
- 21.Kinariwala N., Samaranayake L.P., Perera I., Patel Z. Concerns and fears of Indian dentists on professional practice during the coronavirus disease 2019 (COVID-19) pandemic [published online ahead of print, 2020 Jun 7] Oral Dis. 2020 doi: 10.1111/odi.13459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Namaste campaign. http://www.xinhuanet.com/english/2020-03/12/c_138869387.html
- 23.Kelly N., Nic Íomhair A., McKenna G. Can oral rinses play a role in preventing transmission of Covid 19 infection? Evid Base Dent. 2020;21:42–43. doi: 10.1038/s41432-020-0099-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bidra A.S., Pelletier J.S., Westover J.B., Frank S., Brown S.M., Tessema B. Rapid in-vitro inactivation of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) using povidone-iodine oral antiseptic rinse [published online ahead of print, 2020 Jun 8] J Prosthodont. 2020 doi: 10.1111/jopr.13209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kariwa H., Fujii N., Takashima I. Inactivation of SARS coronavirus by means of povidone-iodine, physical conditions and chemical reagents. Dermatol. 2006;212:119–123. doi: 10.1159/000089211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kampf G., Todt D., Pfaender S., Steinmann E. Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. J Hosp Infect. 2020;104:246–251. doi: 10.1016/j.jhin.2020.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ilhan B., Bayrakdar İ.S., Orhan K. Dental radiographic procedures during COVID-19 outbreak and normalization period: recommendations on infection control. Oral Radiol. 2020:1–5. doi: 10.1007/s11282-020-00460-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Doriguêtto P., Americano J., Devito K. Challenges for the dental radiology clinic in times of the COVID-19 pandemic. Oral Radiol. 2020;36:404–405. doi: 10.1007/s11282-020-00456-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dave M., Coulthard P., Patel N., Seoudi N., Horner K. Use of dental radiography in the COVID-19 pandemic. J Dent Res. 2020;99:1112. doi: 10.1177/0022034520923323. [DOI] [PubMed] [Google Scholar]
- 30.World Health Organization . 2020. Rational Use of Personal Protective Equipment for Coronavirus Disease (COVID-19) and Considerations during Severe Shortages: Interim Guidance.https://apps.who.int/iris/handle/10665/331695 Available from: URL. [Google Scholar]
- 31.https://www.cdc.gov/coronavirus/2019-ncov/hcp/using-ppe.html
- 32.Peng X., Xu X., Li Y., Cheng L., Zhou X., Ren B. Transmission routes of 2019-nCoV and controls in dental practice. Internal J Oral Sci. 2020;12:1–6. doi: 10.1038/s41368-020-0075-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Micik R.E., Miller R.L., Mazzarella M.A., Ryge G. Studies on dental aerobiology, I: bacterial aerosols generated during dental procedures. J Dent Res. 1969;48:49–56. doi: 10.1177/00220345690480012401. [DOI] [PubMed] [Google Scholar]
- 34.Turkistani K.A. Precautions and recommendations for orthodontic settings during the COVID-19 outbreak: a review [published online ahead of print, 2020 May 13] Am J Orthod Dentofacial Orthop. 2020 doi: 10.1016/j.ajodo.2020.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jacofsky D., Jacofsky E.M., Jacofsky M. Understanding antibody testing for COVID-19. J Arthroplasty. 2020;35:S74–S81. doi: 10.1016/j.arth.2020.04.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Occupational Safety and Health Act OSHA 3990-03 2020. Guidance on preparing workplaces for COVID-19. https://www.osha.gov/Publications/OSHA3990.pdf24
- 37.Jamal M., Shah M., Almarzooqi S.H. Overview of transnational recommendations for COVID-19 transmission control in dental care settings [published online ahead of print, 2020 May 19] Oral Dis. 2020 doi: 10.1111/odi.13431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zeng L., Su T., Huang L. Strategic plan for management in oral and maxillofacial surgery during COVID-19 epidemic. Oral Oncol. 2020;105 doi: 10.1016/j.oraloncology.2020.104715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Volgenant C., Persoon I., Ruijter R., Soet J. Infection control in dental health care during and after the SARS‐CoV‐2 outbreak. Oral Dis. 2020 doi: 10.1111/odi.13408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zhang X.H., Ling J.Q. Guidelines on the prevention and control of disease in dental practice during the coronavirus outbreak. Chin J Dent Res. 2020;23:89–94. doi: 10.3290/j.cjdr.a44743. [DOI] [PubMed] [Google Scholar]
- 41.Estai M., Kanagasingam Y., Mehdizadeh M. Teledentistry as a novel pathway to improve dental health in school children: a research protocol for a randomised controlled trial. BMC Oral Health. 2020;20:1–9. doi: 10.1186/s12903-019-0992-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Giudice A., Barone S., Muraca D. Can teledentistry improve the monitoring of patients during the Covid-19 dissemination? A descriptive pilot study. Int J Environ Res Publ Health. 2020;17:3399. doi: 10.3390/ijerph17103399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Telles-Araujo G., Caminha R., Kallás M., Santos P. Teledentistry support in COVID-19 oral care. Clinics. 2020:75. doi: 10.6061/clinics/2020/e2030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ghai S. Teledentistry during COVID-19 pandemic [published online ahead of print, 2020 Jun 16] Diabetes Metab Syndr. 2020;14:933–935. doi: 10.1016/j.dsx.2020.06.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Advice on the Use of Masks in the Context of COVID-19: Interim Guidance. World Health Organization.
- 46.Salvi S.S. In this pandemic and panic of COVID-19 what should doctors know about masks and respirators? http://apiindia.org/wp-content/uploads/pdf/coronavirus/review-article-on-mask.pdf
- 47.Wang J., Pan L., Tang S., Ji J., Shi X. Mask use during COVID-19: a risk adjusted strategy. Environ Pollut. 2020;266 doi: 10.1016/j.envpol.2020.115099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Umer F., Haji Z., Zafar K. Role of respirators in controlling the spread of novel coronavirus (COVID-19) amongst dental healthcare providers: a review. Int Endod J. 2020;53:1062–1067. doi: 10.1111/iej.13313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Water, Sanitation, Hygiene, and Waste Management for the COVID-19 Virus: Interim Guidance. WHO; 2019. nCoV/IPC_WASH/2020.3. [Google Scholar]
- 50.Datta P., Mohi G.K., Chander J. Biomedical waste management in India: critical appraisal. J Lab Physicians. 2018;10:6–14. doi: 10.4103/JLP.JLP_89_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Cleaning and Disinfection of Environmental Surfaces in the Context of COVID-19. Interim Guidance 15 May 2020. WHO; 2019. nCoV/Disinfection/2020.1. [Google Scholar]
- 52.Baghizadeh Fini M. What dentists need to know about COVID-19. Oral Oncol. 2020;105 doi: 10.1016/j.oraloncology.2020.104741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Malateaux G., Gamarra R.S., Dib L.L. UV irradiation as a disinfection method to reduce Covid-19 cross-contamination in dentistry: a scoping review. J Dent Oral Hyg. 2020;3:2020. [Google Scholar]
- 54.Li J.J., Wang S.N., Qiao J.J. Portable pulsed xenon ultraviolet light disinfection in a teaching hospital animal laboratory in China. J Photochem Photobiol, B. 2020;207 doi: 10.1016/j.jphotobiol.2020.111869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Bizzoca M.E., Campisi G., Muzio L.L. Covid-19 pandemic: what changes for dentists and oral medicine experts? A narrative review and novel approaches to infection containment. Int J Environ Res Publ Health. 2020;17:3793. doi: 10.3390/ijerph17113793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Mishra P., Ramalakshmi K., Verma S., Shrivastava V. Comparative efficacy of 3rd generation quaternary ammonium compounds and formaldehyde for fumigation of operation theatres. J Clin Experiment Res. 2013;1:47. [Google Scholar]
- 57.Guan W.J., Liang W.H., Zhao Y. Comorbidity and its impact on 1590 patients with COVID-19 in China: a nationwide analysis. Eur Respir J. 2020;55 doi: 10.1183/13993003.00547-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Papi P., Di Murro B., Penna D., Pompa G. Digital prosthetic workflow during COVID-19 pandemic to limit infection risk in dental practice [published online ahead of print, 2020 May 27] Oral Dis. 2020 doi: 10.1111/odi.13442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Samaranayake L.P., Reid J., Evans D. The efficacy of rubber dam isolation in reducing atmospheric bacterial contamination. ASDC (Am Soc Dent Child) J Dent Child. 1989;56:442–444. [PubMed] [Google Scholar]
- 60.Van Doremalen N., Bushmaker T., Morris D. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020;382:1564–1567. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Parhizkar A., Shamszadeh S., Mardani M., Asgary S. Dental considerations after the outbreak of 2019 novel coronavirus disease: a review of literature. Arch Clin Infect Dis. 2020;15(2) [Google Scholar]
- 62.Zimmermann M., Nkenke E. Approaches to the management of patients in oral and maxillofacial surgery during COVID-19 pandemic. J Cranio-Maxillo-Fac Surg. 2020;48:521–526. doi: 10.1016/j.jcms.2020.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kochhar A., Bhasin R., Kochhar G., Dadlani H. Provision of continuous dental care for oral oncology patients during & after COVID-19 pandemic. Oral Oncol. 2020;106 doi: 10.1016/j.oraloncology.2020.104785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Bhat V.S., Shetty M.S., Shenoy K.K. Infection control in the prosthodontic laboratory. J Indian Prosthodont Soc. 2007;7:62–65. [Google Scholar]
- 65.Walton M., Murray E., Christian M.D. Mental health care for medical staff and affiliated healthcare workers during the COVID-19 pandemic. Eur Heart J Acute Cardiovasc Care. 2020;9:241–247. doi: 10.1177/2048872620922795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Machado R.A., Bonan P.R.F., Perez D.E.D.C., Martelli Junior H. COVID-19 pandemic and the impact on dental education: discussing current and future perspective. Braz Oral Res. 2020;34:e083. doi: 10.1590/1807-3107bor-2020.vol34.0083. [DOI] [PubMed] [Google Scholar]
- 67.Deery C. The COVID-19 pandemic: implications for dental education. Evid Base Dent. 2020;21:46–47. doi: 10.1038/s41432-020-0089-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Barabari P., Moharamzadeh K. Novel coronavirus (COVID-19) and dentistry–A comprehensive review of literature. Dent J. 2020;8:53. doi: 10.3390/dj8020053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Wu K., Wu D., Nguyen T., Tran S. COVID‐19's impact on private practice and academic dentistry in North America. Oral Dis. 2020:1–4. doi: 10.1111/odi.13444. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.