Key Points
Question
Are specific social risk factors associated with patients’ interest in receiving health care–based social risk assistance?
Findings
In this cross-sectional study of 1021 adult patients and adult caregivers of pediatric patients, 53% of participants who had positive screening results for social risks were interested in receiving social risk assistance compared with 9% of participants who had negative screening results. Among those with positive screening results, interest in receiving assistance was higher among participants who answered the question about their interest in receiving assistance before answering the questions about social risks and among participants who had positive results for multiple risks, reported lower household income, and self-identified as having non-Hispanic Black ancestry.
Meaning
The study’s findings suggest that understanding patients’ perspectives regarding their interest in receiving social risk assistance may be an important consideration in the implementation of patient-centered social care interventions.
Abstract
Importance
Health care organizations are increasingly incorporating social risk screening into patient care. Studies have reported wide variations in patients’ interest in receiving health care–based assistance for identified social risks. However, no study to date has examined the factors associated with patients’ interest in receiving assistance, including whether interest in receiving assistance varies based on specific patient demographic characteristics. Targeted research on this topic could improve the success of health care–based programs that offer social care services.
Objective
To identify participant characteristics associated with interest in receiving health care–based social risk assistance.
Design, Setting, and Participants
This cross-sectional study was conducted in 7 primary care clinics and 4 emergency departments in 9 US states between July 2, 2018, and February 13, 2019. A convenience sample of adult patients and adult caregivers of pediatric patients completed a screening survey that measured social risk factors and participants’ interest in receiving assistance for identified social risks. Participants were randomly selected to receive 1 of 2 versions of the survey, which differed based on the order in which questions about social risks and interest in receiving assistance were presented. Multivariable logistic regression analyses were used to evaluate the associations between covariates and participants’ interest in receiving assistance, stratified by social risk screening results. Data were analyzed from September 8, 2019, to July 30, 2020.
Exposures
Social risk screening questions assessed risk factors comprising housing, food, transportation, utilities, and exposure to interpersonal violence. Additional questions assessed participants’ interest in receiving assistance and their perspectives on health care–based social risk screening.
Main Outcomes and Measures
Participant interest in receiving health care–based social risk assistance.
Results
A total of 1021 adult participants with complete survey responses were included in the analysis. Of those, 709 of 1004 participants (70.6%) were female, and 544 of 1007 participants (54.0%) were aged 18 to 44 years. Overall, 353 of 662 participants (53.3%) with positive screening results for 1 or more social risk factors were interested in receiving assistance, whereas 31 of 359 participants (8.6%) with negative screening results for all social risks were interested in receiving assistance. Participants with positive screening results for 1 or more social risk factors had a higher likelihood of being interested in receiving assistance if they answered the question about interest in receiving assistance before they answered the questions about social risk factors (adjusted odds ratio [aOR], 1.48; 95% CI, 1.05-2.07), had positive screening results for a higher number of social risk factors (aOR, 2.40; 95% CI, 1.68-3.42), reported lower household income levels (aOR, 7.78; 95% CI, 2.96-20.44), or self-identified as having non-Hispanic Black ancestry (aOR, 2.22; 95% CI, 1.37-3.60). Among those with negative screening results for all social risk factors, the interest in receiving assistance was higher if the participants reported lower household income levels (aOR, 12.38; 95% CI, 2.94-52.15), previous exposure to health care–based social risk screening (aOR, 2.35; 95% CI, 1.47-3.74), higher perceived appropriateness of social risk screening (aOR, 3.69; 95% CI, 1.08-12.55), or worse health status (aOR, 4.22; 95% CI, 1.09-16.31).
Conclusions and Relevance
In this study, multiple factors were associated with participants’ interest in receiving social risk assistance. These findings may have implications for how and when social risk assistance is offered to patients. As the health care system’s role in addressing social risk factors evolves, an understanding of patients’ perspectives regarding screening and their interest in receiving assistance may be important to implementing patient-centered interventions.
This cross-sectional study assesses social risk factors and examines characteristics associated with interest in receiving health care–based social risk assistance among adult patients and adult caregivers of pediatric patients.
Introduction
Along with increasing recognition that patients’ social contexts may substantially impact their health, health care systems in the US are also increasing rates of screening patients for unmet social risk factors, such as food insecurity and housing instability,1,2,3,4,5,6,7,8,9 and are subsequently providing referrals to affiliated clinic or community social resources (ie, social risk assistance). This assistance may include the provision of food vouchers or help with the completion of applications for government benefits.6,7,9,10,11,12,13,14,15,16,17,18 As more organizations implement these types of social care initiatives across systems,19 variation has emerged regarding patients’ interest in receiving assistance from the health care system in response to identified social risks.6,7,9,11,12,13,14,15,16,17,18,20 For example, across previous studies, 25% to 94% of patients with positive screening results for food insecurity chose not to receive food assistance.6,9,10,11,12,13,15,17 In contrast, patients with negative screening results for social risks have sometimes expressed interest in receiving assistance.11 No study, to our knowledge, has examined the factors associated with patients’ interest in receiving assistance, including whether interest in receiving assistance varies based on specific demographic characteristics. Targeted research on this topic could improve the success of health care–based programs that offer social care services, with the goal of reducing health disparities and improving health outcomes.20
We aimed to identify factors associated with interest in receiving assistance among adult patients and adult caregivers of pediatric patients. We hypothesized that higher interest in receiving assistance would be associated with higher social risk burden,21,22 greater trust in clinicians,13,23,24,25,26,27 recruitment from safety-net settings, previous exposure to and perceived acceptability of social risk screening and social care activities,23,27 and fewer previous experiences with health care–based discrimination.27,28,29,30 We also hypothesized that the order in which survey questions were presented would be associated with participants’ interest in receiving assistance.
Methods
We conducted a multisite cross-sectional study among a convenience sample of English- and Spanish-speaking adult patients and adult caregivers of pediatric patients from 7 primary care clinics and 4 emergency departments (EDs) in 9 US states between July 2, 2018, and February 13, 2019. To assess the association of the order in which survey questions were presented with participant responses, participants were randomly selected to receive 1 of 2 versions of the survey, which differed based on whether participants were asked about social risks before they were asked about their interest in receiving assistance or vice versa. The study was approved by the institutional review board of the University of California, San Francisco; 8 study sites (University of Arkansas, Boston Medical Center [Massachusetts], University of Chicago [Illinois], University of Colorado, Dartmouth College [New Hampshire], Hennepin Health [Minnesota], New York University [New York], and Brigham and Women’s Hospital [Massachusetts]) obtained additional site-specific institutional review board approval. All participants provided verbal informed consent. This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline.31
Participants and Data Collection
Study participants were recruited from 11 clinical sites that provided health care services for a population in which at least 30% of patients were publicly insured or uninsured and that had not already implemented systematic social risk screening programs. The study sites included 4 family medicine clinics, 3 internal medicine clinics, 2 general EDs, and 2 pediatric EDs located in 9 states: Arkansas, California, Colorado, Illinois, Massachusetts, Minnesota, New Mexico, New York, and Vermont. Ten of 11 study sites recruited convenience samples of 100 adult patients or adult caregivers of pediatric patients; 1 internal medicine site recruited 50 participants because of limited time among staff members. Participants were eligible for inclusion if they (1) did not need immediate medical attention, (2) were 18 years or older, (3) were able to speak and read English and/or Spanish, (4) were comfortable using an electronic tablet, and (5) were able to provide informed consent. After providing verbal informed consent, participants completed a 32-item survey (eMethods in the Supplement) on their own (ie, without face-to-face or verbal interaction with survey administrators) using electronic tablets. Surveys took approximately 15 minutes to complete and were administered in private patient areas either before or after clinical visits. Participants were compensated $5.00 for their time. All patients and caregivers who were approached by research staff were offered information about local social services resources regardless of whether they decided to participate in the study.
Data were collected and managed using the REDCap online platform (REDCap Consortium and Vanderbilt University).27,32 Additional details regarding study site recruitment and eligibility criteria have been described in previous publications.27,29
Outcome Measures
The primary outcome measure was participants’ interest in receiving assistance; this outcome was assessed through the following question: “Would you like to receive assistance with any of the following issues? (Check all that apply).” Response options included (1) housing; (2) food access; (3) medical or nonmedical transportation; (4) electric, gas, oil, or water utility services; (5) your safety, or violence in your household; or (6) none of these. Social risks were assessed using the Accountable Health Communities Health-Related Social Needs screening tool developed by the Center for Medicare and Medicaid Innovation33 and the Housing Stability Vital Sign developed by Children’s HealthWatch at Boston Medical Center.34 The Health-Related Social Needs 10-item screening tool assesses 5 social risk domains: (1) housing-associated social risks (ie, current instability or problems with quality of housing), (2) food insecurity, (3) transportation problems, (4) difficulty paying for utilities, and (5) exposure to interpersonal violence. The Housing Stability Vital Sign includes 3 questions that assess housing instability.34 Positive screening results were defined using the screening instruments’ criteria.33 Participants were considered to have positive results for a housing-associated social risk if they received positive results on either the Health-Related Social Needs or the Housing Stability Vital Sign tool.
The survey also included questions about participants’ perspectives on social risk screening (eg, whether they believed it was appropriate to screen for social risks in their health care setting), previous experiences with social risk screening and assistance (eg, whether they had been screened for social risks in a health care setting within the past year), previous experience with discrimination in a health care setting (eg, whether they had ever been treated differently by a physician or nurse because of their race, ethnicity, or socioeconomic status), trust in their clinician, and demographic characteristics (including age, sex, race, ethnicity, and household income). The full survey is available in eMethods in the Supplement.
Study sites were characterized by type of site (primary care vs ED). A site was considered a safety-net setting if at least 80% of patients who received services at the site were publicly insured or uninsured (based on self-reporting from each site).
Statistical Analyses
The main outcome variable was participants’ interest in receiving assistance for any of the 5 social risk domains, dichotomized as any interest vs no interest. Because we assumed that interest in receiving assistance would differ based on whether participants received positive screening results for social risks, we stratified all analyses based on social risk endorsement (ie, positive results for any risk vs no risks). We used univariable analyses (2-sided Fisher exact χ2 tests) to assess bivariate associations with participants’ interest in receiving assistance. Associations between reported social risks and interest in receiving assistance for each risk domain were evaluated using Pearson correlation coefficients. Univariable and multivariable logistic regression analyses were used to identify factors independently associated with interest in receiving assistance. Robust SEs accounted for clustering by site. The multivariable analyses included variables that were associated with interest in receiving assistance at the P = .20 significance level in the univariable logistic regression analyses as well as variables that were hypothesized a priori to be associated with participants’ interest in receiving assistance.35 All independent variables were treated as categorical, with the exception of the burden of social risks, which was treated as ordinal (based on number of reported risks on a scale of 1-5).
For all regression models, we included participants with complete data after listwise deletion, with 1 exception for the household income variable, which had the most missing data (168 participants [16.5%]). For this variable, we included a separate category, defined as missing, to preserve the overall sample size and examine patterns of interest in receiving assistance among participants who did not respond to the income question.36 Because we assumed that missing data, such as household income and race/ethnicity (the variable with the second highest level of missing data, comprising 56 participants [5.5%]), were not missing at random, we did not conduct multiple imputations.37,38,39,40 Results were considered statistically significant at α < .05. We evaluated the impact of nonstratification based on social risk screening results through a pooled analysis. All analyses were conducted using Stata/SE software, version 15.1 (StataCorp). Data were analyzed from September 8, 2019, to July 30, 2020.
Results
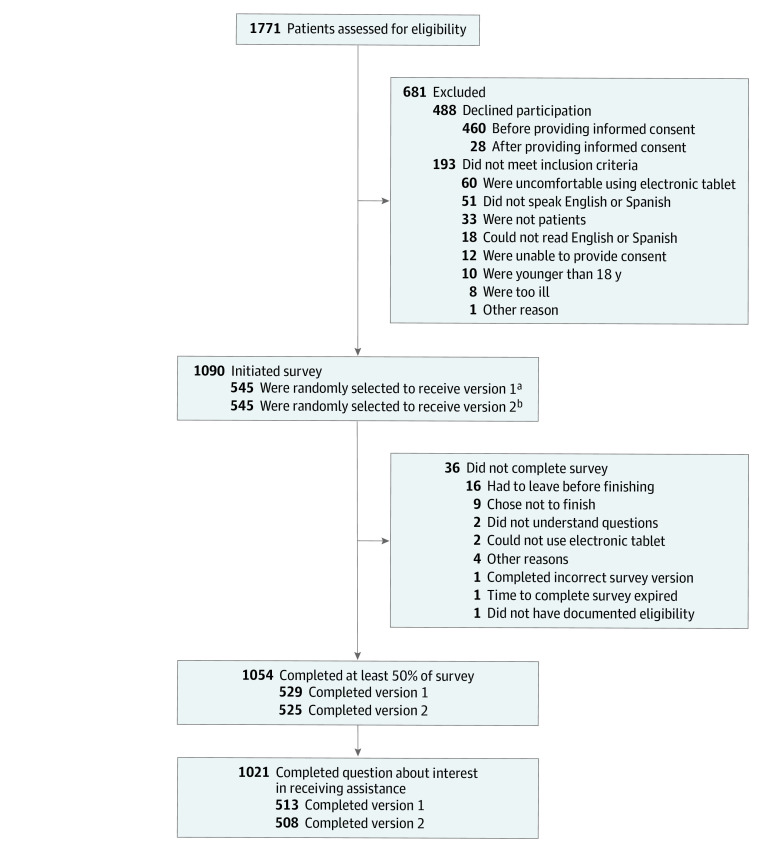
Overall, 1771 adult patients and adult caregivers of pediatric patients were invited to participate in the study (Figure). Among the 1054 participants (59.5%) who provided informed consent and responded to the survey, 1021 participants (96.9%) answered the question about interest in receiving assistance and were included in the final analysis. Most participants in the final sample were women (709 of 1004 participants [70.6%]) and aged 18 to 44 years (544 of 1007 participants [54.0%]) (Table 1).
Figure. Flowchart of Participant Recruitment and Survey Completion.
aParticipants who received version 1 completed the social risk screening questions first.
bParticipants who received version 2 completed the question regarding interest in receiving social risk assistance first.
Table 1. Participant Characteristics by Social Risk Screening Results and Interest in Receiving Assistancea.
| Characteristic | Participants, No./total No. (%) | ||||
|---|---|---|---|---|---|
| With complete survey responsesb | With positive screening results for ≥1 social risk factorc | With negative screening results for all social risk factorsd | |||
| Interested in assistance | Not interested in assistance | Interested in assistance | Not interested in assistance | ||
| Participants | 1021 | 353/662 (53.3) | 309/662 (46.7) | 31/359 (8.6) | 328/359 (91.4) |
| Participant characteristics | |||||
| Age range, y | |||||
| 18-44 | 544/1007 (54.0) | 209/381 (54.9) | 172/381 (45.1) | 14/163 (8.6) | 149/163 (91.4) |
| 45-64 | 299/1007 (29.7) | 105/194 (54.1) | 89/194 (45.9) | 10/105 (9.5) | 95/105 (90.5) |
| ≥65 | 164/1007 (16.3) | 33/77 (42.9) | 44/77 (57.1) | 7/87 (8.0) | 80/87 (92.0) |
| Sex | |||||
| Female | 709/1004 (70.6) | 251/466 (53.9) | 215/466 (46.1) | 17/243 (7.0) | 226/243 (93.0) |
| Male | 295/1004 (29.4) | 96/184 (52.2) | 88/184 (47.8) | 13/111 (11.7) | 98/111 (88.3) |
| Race/ethnicity | |||||
| Non-Hispanic White | 359/965 (37.2) | 68/185 (36.8) | 117/185 (63.2) | 10/174 (5.7) | 164/174 (94.3) |
| Non-Hispanic Black | 211/965 (21.9) | 103/150 (68.7) | 47/150 (31.3) | 6/61 (9.8) | 55/61 (90.2) |
| Hispanic | 311/965 (32.2) | 131/233 (56.2) | 102/233 (43.8) | 10/78 (12.8) | 68/78 (87.2) |
| Non-Hispanic other race or multiple races | 84/965 (8.7) | 28/52 (53.8) | 24/52 (46.2) | 4/32 (12.5) | 28/32 (87.5) |
| Preferred language | |||||
| English | 848/1021 (83.1) | 261/521 (50.1) | 260/521 (49.9) | 26/327 (8.0) | 301/327 (92.0) |
| Spanish | 173/1021 (16.9) | 92/141 (65.2) | 49/141 (34.8) | 5/32 (15.6) | 27/32 (84.4) |
| Educational level, y | |||||
| <12 | 181/1009 (17.9) | 100/146 (68.5) | 46/146 (31.5) | 3/35 (8.6) | 32/35 (91.4) |
| ≥12 | 828/1009 (82.1) | 248/508 (48.8) | 260/508 (51.2) | 28/320 (8.8) | 292/320 (91.3) |
| Household income, $ | |||||
| 0-10 000 | 225/1021 (22.0) | 142/195 (72.8) | 53/195 (27.2) | 6/30 (20.0) | 24/30 (80.0) |
| 10 001-25 000 | 189/1021 (18.5) | 78/146 (53.4) | 68/146 (46.6) | 10/43 (23.3) | 33/43 (76.7) |
| 25 001-50 000 | 182/1021 (17.8) | 61/126 (48.4) | 65/126 (51.6) | 4/56 (7.1) | 52/56 (92.9) |
| 50 001-75 000 | 80/1021 (7.8) | 8/35 (22.9) | 27/35 (77.1) | 2/45 (4.4) | 43/45 (95.6) |
| ≥75 001 | 177/1021 (17.3) | 5/56 (8.9) | 51/56 (91.1) | 3/121 (2.5) | 118/121 (97.5) |
| Missing | 168/1021 (16.5) | 59/104 (56.7) | 45/104 (43.3) | 6/64 (9.4) | 58/64 (90.6) |
| Self-reported health or caregiver-reported child’s health41 | |||||
| Excellent, very good, or good | 748/986 (75.9) | 225/454 (49.6) | 229/454 (50.4) | 10/294 (6.8) | 274/294 (93.2) |
| Fair or poor | 238/986 (24.1) | 112/182 (61.5) | 70/182 (38.5) | 10/56 (17.9) | 46/56 (82.1) |
| Participant type | |||||
| Adult patient | 793/1021 (77.7) | 249/498 (50.0) | 249/498 (50.0) | 24/295 (8.14) | 271/295 (91.9) |
| Adult caregiver of pediatric patient | 228/1021 (22.3) | 104/164 (63.4) | 60/164 (36.6) | 7/64 (10.9) | 57/64 (89.1) |
| Trust in clinician42 | |||||
| Complete (rating of 10) | 504/981 (51.4) | 163/313 (52.1) | 150/313 (47.9) | 13/191 (6.8) | 178/191 (93.2) |
| High (rating of 8-9) | 285/981 (29.1) | 86/178 (48.3) | 92/178 (51.7) | 9/107 (8.4) | 98/107 (91.6) |
| Medium to low (rating of 1-7) | 192/981 (19.6) | 86/144 (59.7) | 58/144 (40.3) | 7/48 (14.6) | 41/48 (85.4) |
| Any previous experience with discrimination in a health care setting43,44 | |||||
| Yes | 274/1005 (27.3) | 110/211 (52.1) | 101/211 (47.9) | 7/63 (11.1) | 56/63 (88.9) |
| No | 731/1005 (72.7) | 235/440 (53.4) | 205/440 (46.6) | 22/291 (7.6) | 269/291 (92.4) |
| Order of response to survey questions | |||||
| Answered questions about social risk factors first | 513/1021 (50.2) | 162/330 (49.1) | 168/330 (50.9) | 14/183 (7.7) | 169/183 (92.3) |
| Answered question about interest in receiving assistance first | 508/1021 (49.8) | 191/332 (57.5) | 141/332 (42.5) | 17/176 (9.7) | 159/176 (90.3) |
| Social risk screening33,45 | |||||
| Risk factors, No. | |||||
| 0 | 359/1021 (35.2) | 0 | 0 | 31/359 (8.6) | 328/359 (91.4) |
| 1 | 257/1021 (25.2) | 81/257 (31.5) | 176/257 (68.5) | NA | NA |
| 2 | 227/1021 (22.2) | 128/227 (56.4) | 99/227 (43.6) | NA | NA |
| 3 | 135/1021 (13.2) | 104/135 (77.0) | 31/135 (23.0) | NA | NA |
| 4 | 40/1021 (3.9) | 37/40 (92.5) | 3/40 (7.5) | NA | NA |
| 5 | 3/1021 (0.3) | 3/3 (100.0) | 0 | NA | NA |
| Any exposure to social risk screening in health care setting within past 12 mo | |||||
| Yes | 313/1002 (31.2) | 150/243 (61.7) | 93/243 (38.3) | 7/70 (10.0) | 63/70 (90.0) |
| No | 689/1002 (68.7) | 194/409 (47.4) | 215/409 (52.6) | 22/279 (7.9) | 258/280 (92.1) |
| Any social risk assistance in health care setting within past 12 mo | |||||
| Yes | 182/1002 (18.2) | 123/163 (75.5) | 40/163 (24.5) | 5/19 (26.3) | 14/19 (73.7) |
| No | 820/1002 (81.8) | 219/487 (45.0) | 268/487 (55.0) | 25/333 (7.5) | 308/333 (92.5) |
| Any discomfort with questions in any screening domain | |||||
| Yes | 69/998 (6.9) | 42/62 (67.7) | 20/62 (32.3) | 2/7 (28.6) | 5/7 (71.4) |
| No | 929/998 (93.1) | 301/586 (51.4) | 285/586 (48.6) | 28/343 (8.2) | 315/343 (91.8) |
| Perceptions of appropriateness of health care–based social risk screening | |||||
| Very appropriate or somewhat appropriate | 782/982 (79.6) | 276/515 (53.6) | 239/515 (46.4) | 26/267 (9.7) | 241/267 (90.3) |
| Neither, very inappropriate, or somewhat inappropriate | 200/982 (20.4) | 60/122 (49.2) | 62/122 (50.8) | 3/78 (3.8) | 75/78 (96.2) |
| Comfort with integrating social risk data into EHR | |||||
| Completely comfortable or somewhat comfortable | 632/982 (64.4) | 229/403 (56.8) | 174/403 (43.2) | 18/229 (7.9) | 211/229 (92.1) |
| Neither, completely uncomfortable, or somewhat uncomfortable | 350/982 (35.6) | 107/234 (45.7) | 127/234 (54.3) | 11/116 (9.5) | 105/116 (90.5) |
| Health care setting | |||||
| Primary care | 628/1021 (61.5) | 199/398 (50.0) | 199/398 (50.0) | 15/230 (6.5) | 215/230 (93.5) |
| Emergency department | 393/1021 (38.5) | 154/264 (58.3) | 110/264 (41.7) | 16/129 (12.4) | 113/129 (87.6) |
| Individual study sites | |||||
| 1 | 101/1021 (9.9) | 56/75 (74.7) | 19/75 (25.3) | 5/26 (19.2) | 21/26 (80.8) |
| 2 | 100/1021 (9.8) | 24/59 (40.7) | 35/59 (59.3) | 6/41 (14.6) | 35/41 (85.4) |
| 3 | 98/1021 (9.6) | 58/81 (71.6) | 23/81 (28.4) | 4/17 (23.5) | 13/17 (76.5) |
| 4 | 98/1021 (9.6) | 34/58 (58.6) | 24/58 (41.4) | 3/40 (7.5) | 37/40 (92.5) |
| 5 | 95/1021 (9.3) | 40/75 (53.3) | 35/75 (46.7) | 1/20 (5.0) | 19/20 (95.0) |
| 6 | 97/1021 (9.5) | 38/66 (57.6) | 28/66 (42.4) | 3/31 (9.7) | 28/31 (90.3) |
| 7 | 99/1021 (9.7) | 23/50 (46.0) | 27/50 (54.0) | 2/49 (4.1) | 47/49 (95.9) |
| 8 | 89/1021 (8.7) | 17/41 (41.5) | 24/41 (58.5) | 3/48 (6.3) | 45/48 (93.8) |
| 9 | 96/1021 (9.4) | 35/71 (49.3) | 36/71 (50.7) | 1/25 (4.0) | 24/25 (96.0) |
| 10 | 100/1021 (9.8) | 21/67 (31.3) | 46/67 (68.7) | 0 | 33/33 (100.0) |
| 11 | 48/1021 (4.7) | 7/19 (36.8) | 12/19 (63.2) | 3/29 (10.3) | 26/29 (89.7) |
| Participants with public insurance or no insurance, % | |||||
| <80 | 726/1021 (71.1) | 204/435 (46.9) | 231/435 (53.1) | 21/292 (7.2) | 270/291 (92.8) |
| ≥80 | 295/1021 (28.9) | 149/227 (65.6) | 78/227 (34.4) | 10/68 (14.7) | 58/68 (85.3) |
Abbreviations: EHR, electronic health record; NA, not applicable.
A total of 33 of 1054 participants (3.1%) completed at least 50% of the survey (the study’s threshold for completion) but did not answer the question about interest in receiving assistance. These participants were more likely to be Hispanic, to speak Spanish, to report better health, and to have been recruited from a primary care setting compared with other participants (eTable 1 in the Supplement).
Denominators are based on the total number of participants with complete responses for each specific characteristic.
Denominators are based on the total number of participants with positive screening results for 1 or more risk factors.
Denominators are based on the total number of participants with negative screening results for all risk factors.
Interest in Receiving Assistance
A total of 384 participants (37.6% of the study sample) expressed interest in receiving assistance with at least 1 social risk. Interest in receiving assistance was higher among the 662 participants who had a positive screening result for at least 1 social risk (353 participants [53.3%] were interested in receiving assistance) than among the 359 participants who had negative screening results (31 participants [8.6%] were interested in receiving assistance). Across the 11 study sites, interest in receiving assistance among those who received a positive screening result for 1 or more social risk factors ranged from 21 of 67 participants (31.3%) to 56 of 75 participants (74.7%) (P < .001). Table 1 shows the unadjusted associations between independent variables and interest in receiving assistance, stratified by social risk status.
Among 1021 participants, the interest in risk-specific assistance was highest for housing (232 participants [22.7%]), followed by food (167 participants [16.4%]), transportation (121 participants [11.8%]), utilities (114 participants [11.2%]), and safety (19 participants [1.9%]). Interest in receiving social risk–specific assistance among those with a positive screening result for any single risk factor was consistent across most social risk domains, ranging from 144 of 417 participants (34.5%) who were interested in receiving food assistance to 79 of 200 participants (39.5%) who were interested in receiving transportation assistance. The sole exception was interpersonal violence, for which only 2 of 18 participants (11.1%) who had a positive screening result were interested in receiving assistance. Interest in receiving risk-specific assistance among those with a negative screening result for any single risk factor ranged from 16 of 966 participants (1.7%) who were interested in receiving assistance for interpersonal violence to 39 of 494 participants (7.9%) who were interested in receiving assistance for housing (Table 2). Bivariate associations with risk-specific interest in receiving assistance are available in eTable 2 through eTable 6 in the Supplement. Interest in receiving assistance with food was associated with interest in receiving assistance with transportation (Pearson r = 0.37; P < .001), housing (Pearson r = 0.37; P < .001), and utilities (Pearson r = 0.32; P < .001).
Table 2. Participant Interest in Receiving Risk-Specific Assistance, Stratified by Response to Specific Social Risk Screening Questions.
| Specified risk domain | Participants, No./total No. (%) | P valued | ||||||
|---|---|---|---|---|---|---|---|---|
| With complete survey responses, No. | With positive screening results | With negative screening results | ||||||
| Totala | Interested in assistanceb | Not interested in assistanceb | Totala | Interested in assistancec | Not interested in assistancec | |||
| Housing | 1021 | 527/1021 (51.6) | 193/527 (36.6) | 334/527 (63.4) | 494/1021 (48.4) | 39/494 (7.9) | 455/494 (92.1) | <.001 |
| Food | 1011 | 417/1011 (41.2) | 144/417 (34.5) | 273/417 (65.5) | 594/1011 (58.8) | 22/594 (3.7) | 572/594 (96.3) | <.001 |
| Utilities | 1001 | 129/1001 (12.9) | 45/129 (34.9) | 84/129 (65.1) | 872/1001 (87.1) | 66/872 (7.6) | 806/872 (92.4) | <.001 |
| Transportation | 998 | 200/998 (20.0) | 79/200 (39.5) | 121/200 (60.5) | 798/998 (80.0) | 39/798 (4.9) | 759/798 (95.1) | <.001 |
| Interpersonal violence | 984 | 18/984 (1.8) | 2/18 (11.1) | 16/18 (88.9) | 966/984 (98.2) | 16/966 (1.7) | 950/966 (98.3) | .04 |
| Any risks | 1021 | 662/1021 (64.8) | 353/662 (53.3) | 309/662 (46.7) | 359/1021 (35.2) | 31/359 (8.6) | 328/359 (91.4) | <.001 |
Denominators are based on the total number of participants with complete responses (column 1).
Denominators are based on the total number of participants with a positive screening result for each specified risk domain (column 2).
Denominators are based on the total number of participants with a negative screening result for each specified risk domain (column 5).
P value for Fisher exact χ2 analysis evaluating differences in participants’ levels of interest in receiving assistance by social risk screening result.
Multivariable and Pooled Analyses
Participants with a positive screening result for 1 or more social risk factors had a significantly higher likelihood of being interested in receiving assistance if they were asked the question about interest in receiving assistance before they were asked the questions about social risk (adjusted odds ratio [aOR], 1.48; 95% CI, 1.05-2.07; P = .02), had positive screening results for a higher number of social risks (aOR, 2.40; 95% CI, 1.68-3.42; P < .001), reported lower household income (aOR, 7.78; 95% CI, 2.96-20.44; P < .001), or self-identified as having non-Hispanic Black ancestry (aOR, 2.22; 95% CI, 1.37-3.60; P = .001). Participants who received negative screening results had a significantly higher likelihood of being interested in assistance if they reported lower household income (aOR, 12.38; 95% CI, 2.94-52.15; P = .001), reported previous exposure to health care–based social risk screening (aOR, 2.35; 95% CI, 1.47-3.74; P < .001), reported higher perceived appropriateness of health care–based social risk screening (aOR, 3.69; 95% CI, 1.08-12.55; P = .04), reported worse health (aOR, 4.22; 95% CI, 1.09-16.31; P = .04), or were recruited from an ED setting (aOR, 4.27; 95% CI, 1.59-11.45; P = .004).
Regardless of social risk screening results, participants’ interest in receiving assistance was not associated with trust in clinicians, recruitment from a safety-net setting, or previous experiences of health care–based discrimination. Stratified unadjusted and adjusted ORs for interest in receiving assistance are shown in Table 3, and stratified adjusted predicted probabilities for interest in receiving assistance are shown in Table 4. Comparison of independent variables for the 851 participants included in the multivariable models and the 170 participants excluded from the analysis owing to missing data are available in eTable 7 in the Supplement.
Table 3. Unadjusted and Adjusted Associations Between Social Risk Factors and Interest in Receiving Assistance, Stratified by Response to Social Risk Screening Questionsa.
| Variable | Participants with positive screening results for ≥1 social risk factor (n = 550) | Participants with negative screening results for all social risk factors (n = 301) | ||||||
|---|---|---|---|---|---|---|---|---|
| Unadjusted OR (95% CI) | P value | Adjusted OR (95% CI) | P value | Unadjusted OR (95% CI) | P value | Adjusted OR (95% CI) | P value | |
| Participant characteristics | ||||||||
| Age range, y | ||||||||
| 18-44 | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA |
| 45-64 | 0.79 (0.50-1.26) | .32 | 1.03 (0.67-1.58) | .91 | 1.22 (0.48-3.09) | .68 | 3.88 (0.67-22.35) | .13 |
| ≥65 | 0.61 (0.37-1.00) | .05 | 1.20 (0.70-2.05) | .51 | 0.92 (0.40-2.11) | .85 | 2.10 (0.42-10.43) | .36 |
| Race/ethnicity | ||||||||
| Non-Hispanic White | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA |
| Non-Hispanic Black | 3.78 (2.00-7.17) | <.001 | 2.22 (1.37-3.60) | .001 | 1.94 (1.08-3.49) | .03 | 0.57 (0.18-1.88) | .36 |
| Hispanic | 1.95 (1.34-2.85) | .001 | 0.74 (0.29-1.91) | .53 | 2.99 (1.02-8.81) | .05 | 1.51 (0.27-8.51) | .64 |
| Non-Hispanic other race or multiple races | 2.05 (1.10-3.80) | .02 | 1.36 (0.76-2.44) | .30 | 3.39 (0.80-14.28) | .10 | 1.43 (0.27-7.58) | .67 |
| Preferred language | ||||||||
| English | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA |
| Spanish | 1.55 (0.90-2.66) | .12 | 2.20 (0.97-4.97) | .06 | 2.45 (1.24-4.82) | .01 | 2.58 (0.49-4.70) | .17 |
| Educational level, y | ||||||||
| <12 | 1.84 (1.20-2.82) | .005 | 1.46 (0.81-2.65) | .21 | 1.01 (0.29-3.54) | .99 | 0.21 (0.02-2.18) | .19 |
| ≥12 | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA |
| Household income, $ | ||||||||
| Missing | 10.74 (3.89-29.70) | <.001 | 3.93 (1.06-14.57) | .04 | 2.67 (0.49-14.61) | .26 | 2.23 (0.22-22.06) | .49 |
| 0-10 000 | 34.13 (17.2-67.58) | <.001 | 7.78 (2.96-20.44) | <.001 | 10.40 (3.91-27.65) | <.001 | 12.38 (2.94-52.15) | .001 |
| 10 001-25 000 | 12.16 (4.70-31.43) | <.001 | 3.90 (1.19-12.75) | .03 | 10.76 (5.06-22.86) | <.001 | 11.48 (2.44-53.94) | .002 |
| 25 001-50 000 | 12.16 (6.06-24.43) | <.001 | 5.45 (2.49-11.96) | <.001 | 2.36 (0.36-15.34) | .37 | 3.40 (0.41-28.37) | .26 |
| 50 001-75 000 | 3.62 (1.00-13.01) | .05 | 2.37 (0.59-9.51) | .22 | 1.78 (0.41-7.74) | .44 | 1.37 (0.28-6.77) | .70 |
| ≥75 001 | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA |
| Self-reported health or caregiver-reported child’s health | ||||||||
| Excellent, very good, or good | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA |
| Fair or poor | 1.66 (1.03-2.69) | .04 | 1.50 (0.92-2.46) | .11 | 2.95 (1.53-5.71) | .001 | 4.22 (1.09-16.31) | .04 |
| Participant type | ||||||||
| Adult patient | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA |
| Adult caregiver of pediatric patient | 2.03 (1.12-3.68) | .02 | 1.35 (0.52-3.50) | .53 | 1.51 (0.53-4.25) | .44 | 2.60 (0.66-10.32) | .17 |
| Trust in clinician | ||||||||
| Complete (rating of 10) | 0.76 (0.48-1.19) | .23 | 1.13 (0.64-1.99) | .66 | 0.43 (0.12-1.55) | .20 | 0.56 (0.08-4.11) | .57 |
| High (rating of 8-9) | 0.72 (0.44-1.17) | .19 | 1.31 (0.77-2.23) | .31 | 0.49 (0.20-1.17) | .11 | 0.70 (0.18-2.69) | .60 |
| Medium to low (rating of 1-7) | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA |
| Any previous experience with discrimination in a health care setting | ||||||||
| Yes | 0.98 (0.71-1.35) | .89 | 0.71 (0.48-1.05) | .09 | 1.58 (0.57-4.38) | .38 | 1.37 (0.25-7.55) | .71 |
| No | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA |
| Order of response to survey questions | ||||||||
| Answered questions about social risk factors first | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA |
| Answered question about interest in receiving assistance first | 1.22 (0.85-1.76) | .27 | 1.48 (1.05-2.07) | .02 | 1.76 (0.66-4.67) | .26 | 1.52 (0.49-4.70) | .47 |
| Social risk screening | ||||||||
| No. of risk factorsb | 2.86 (2.15-3.82) | <.001 | 2.40 (1.68-3.42) | <.001 | NA | NA | NA | NA |
| Any exposure to social risk screening in health care setting within past 12 mo | ||||||||
| Yes | 1.78 (1.01-3.14) | .05 | 1.42 (0.90-2.26) | .14 | 1.26 (0.50-3.16) | .63 | 2.35 (1.47-3.74) | <.001 |
| No | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA |
| Any social risk assistance in health care setting within past 12 mo | ||||||||
| Yes | 3.98 (2.57-6.15) | <.001 | 1.66 (0.97-2.82) | .06 | 4.36 (0.99-19.29) | .05 | 2.00 (0.42-9.45) | .38 |
| No | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA |
| Any discomfort with questions in any screening domain | ||||||||
| Yes | 2.54 (1.26-5.10) | .009 | 1.43 (0.54-3.75) | .47 | 3.63 (0.81-16.20) | .09 | 5.75 (0.64-51.58) | .12 |
| No | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA |
| Perceptions of appropriateness of health care–based social risk screening | ||||||||
| Very appropriate or somewhat appropriate | 1.04 (0.73-1.50) | .81 | 0.74 (0.44-1.25) | .26 | 2.19 (0.74-6.43) | .16 | 3.69 (1.08-12.55) | .04 |
| Neither, very inappropriate, or somewhat inappropriate | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA |
| Comfort with integrating social risk data into EHR | ||||||||
| Completely comfortable or somewhat comfortable | 1.49 (0.92-2.42) | .11 | 1.48 (0.90-2.45) | .13 | 0.70 (0.29-1.69) | .43 | 0.42 (0.08-2.22) | .31 |
| Neither, completely uncomfortable, or somewhat uncomfortable | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA |
| Health care setting | ||||||||
| Primary care | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA |
| Emergency department | 1.47 (0.72-3.02) | .30 | 1.39 (0.69-2.79) | .35 | 2.55 (1.03-6.32) | .04 | 4.27 (1.59-11.45) | .004 |
| Participants with public insurance or no insurance, % | ||||||||
| <80 | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA |
| ≥80 | 2.23 (1.15-4.34) | .02 | 1.62 (0.73-3.57) | .24 | 2.50 (0.91-6.86) | .07 | 1.91 (0.74-4.90) | .18 |
Abbreviations: EHR, electronic health record; NA, not applicable; OR, odds ratio.
The table shows all variables included in the adjusted analyses. Models were run as logistic regressions with clustered SEs that were categorized by clinical site. Sample size presented is the size after listwise deletion. Among participants interested in assistance, those excluded from the regression model were older and more likely to be Hispanic, to speak Spanish, to have lower educational levels and household income, and to report discomfort with answering the social risk screening questions (eTable 7 in the Supplement). Among participants not interested in assistance, those excluded from the regression model were older and more likely to be adult patients (vs adult caregivers), to have lower educational levels, to have been recruited from a primary care setting, and to report that health care–based social risk screening was less appropriate (eTable 7 in the Supplement).
The number of risk factors ranged from 0 to 5.
Table 4. Adjusted Predicted Probabilities of Interest in Receiving Assistance for Social Risks, Stratified by Response to Social Risk Screening Questions.
| Variable | Adjusted probability, % (95% CI) | |
|---|---|---|
| Participants with positive screening results for ≥1 social risk factor (n = 550) | Participants with negative screening results for all social risk factors (n = 301) | |
| Participant characteristics | ||
| Age range, y | ||
| 18-44 | 51.4 (47.1 to 55.6) | 6.1 (2.9 to 9.2) |
| 45-64 | 51.8 (44.7 to 58.9) | 15.1 (4.6 to 25.5) |
| ≥65 | 54.4 (45.1 to 63.7) | 10.2 (2.7 to 17.8) |
| Race/ethnicity | ||
| Non-Hispanic White | 49.8 (40.7 to 58.9) | 8.4 (3.5 to 13.3) |
| Non-Hispanic Black | 63.4 (58.1 to 68.8) | 5.6 (1.9 to 9.2) |
| Hispanic | 44.5 (33.9 to 55.1) | 11.1 (1.1 to 21.1) |
| Non-Hispanic other race or multiple races | 55.2 (42.6 to 67.7) | 10.7 (1.5 to 19.9) |
| Preferred language | ||
| English | 49.0 (44.4 to 53.6) | 8.0 (6.1 to 9.9) |
| Spanish | 62.3 (50.7 to 74.0) | 15.1 (4.3 to 25.9) |
| Educational level, y | ||
| <12 | 57.1 (48.2 to 66.0) | 3.0 (−1.5 to 7.5) |
| ≥12 | 50.6 (45.8 to 55.4) | 10.0 (6.9 to 13.1) |
| Household income, $ | ||
| Missing | 48.9 (38.2 to 59.7) | 6.2 (−2.9 to 15.3) |
| 0-10 000 | 61.8 (54.2 to 69.5) | 21.4 (8.9 to 33.9) |
| 10 001-25 000 | 48.8 (38.0 to 59.5) | 20.4 (4.8 to 36.1) |
| 25 001-50 000 | 55.2 (48.1 to 62.2) | 8.7 (−3.4 to 20.7) |
| 50 001-75 000 | 39.6 (24.7 to 54.4) | 4.1 (−1.5 to 9.7) |
| ≥75 001 | 25.5 (9.9 to 41.0) | 3.1 (1.0 to 5.2) |
| Self-reported health or caregiver-reported child's health | ||
| Excellent, very good, or good | 49.8 (45.2 to 54.5) | 6.8 (5.1 to 8.7) |
| Fair or poor | 56.8 (49.3 to 64.4) | 17.8 (7.3 to 28.4) |
| Participant type | ||
| Adult patient | 50.5 (43.7 to 57.2) | 7.4 (5.4 to 9.4) |
| Adult caregiver of pediatric patient | 55.7 (44.3 to 67.1) | 13.9 (5.3 to 22.6) |
| Trust in clinician | ||
| Complete (rating of 10) | 51.6 (46.2 to 57.0) | 7.6 (2.8 to 12.5) |
| High (rating of 8-9) | 54.1 (48.9 to 59.4) | 8.9 (5.1 to 12.7) |
| Medium to low (rating of 1-7) | 49.5 (41.3 to 57.6) | 11.4 (2.2 to 20.5) |
| Any previous experience with discrimination in a health care setting | ||
| Yes | 47.8 (41.2 to 54.4) | 10.3 (0.4 to 20.2) |
| No | 53.7 (49.5 to 57.9) | 8.3 (5.8 to 10.7) |
| Order of response to survey questions | ||
| Answered questions about social risk factors first | 48.4 (41.7 to 55.2) | 7.3 (3.2 to 11.5) |
| Answered question about interest in receiving assistance first | 55.1 (53.0 to 57.3) | 9.8 (6.5 to 13.2) |
| Social risk screening | ||
| Risk factors, No. | ||
| 1 | 36.2 (27.5 to 44.8) | NA |
| 2 | 53.2 (48.6 to 57.9) | NA |
| 3 | 69.6 (63.5 to 75.6) | NA |
| 4 | 82.3 (73.9 to 90.8) | NA |
| 5 | 90.8 (82.9 to 98.7) | NA |
| Any exposure to social risk screening in health care setting within past 12 mo | ||
| Yes | 49.8 (45.6 to 54.0) | 13.7 (9.3 to 18.2) |
| No | 55.9 (48.0 to 63.7) | 7.7 (6.2 to 9.3) |
| Any social risk assistance in health care setting within past 12 mo | ||
| Yes | 58.7 (51.3 to 66.0) | 13.1 (2.5 to 23.7) |
| No | 49.8 (44.8 to 54.9) | 8.2 (6.0 to 10.4) |
| Any discomfort with questions in any screening domain | ||
| Yes | 57.4 (41.0 to 73.9) | 24.5 (−2.5 to 51.4) |
| No | 51.4 (47.4 to 55.4) | 8.4 (6.7 to 10.1) |
| Perceptions of appropriateness of health care–based social risk screening | ||
| Very appropriate or somewhat appropriate | 50.8 (45.7 to 56.0) | 10.4 (7.8 to 12.9) |
| Neither, very inappropriate, or somewhat inappropriate | 55.9 (49.8 to 62.0) | 3.8 (0.4 to 7.3) |
| Comfort with integrating social risk data in EHR | ||
| Completely comfortable or somewhat comfortable | 54.4 (49.0 to 59.8) | 7.1 (3.5 to 10.7) |
| Neither, completely uncomfortable, or somewhat uncomfortable | 47.6 (41.3 to 54.0) | 12.7 (5.0 to 20.3) |
| Health care setting | ||
| Primary care | 49.5 (43.4 to 55.4) | 5.1 (2.4 to 7.7) |
| Emergency department | 55.2 (46.4 to 64.0) | 14.2 (9.9 to 18.5) |
| Participants with public insurance or no insurance, % | ||
| <80 | 49.2 (45.0 to 53.2) | 7.6 (5.2 to 10.0) |
| ≥80 | 57.4 (45.3 to 69.6) | 11.9 (6.0 to 17.7) |
Abbreviations: EHR, electronic health record; NA, not applicable.
In the pooled analysis of the full sample, variables associated with greater interest in receiving assistance included having positive screening results for a greater number of risks, answering the question about interest in receiving assistance before answering the questions about social risk, and reporting lower income, worse health, non-Hispanic Black ancestry, and Spanish (vs English) language preference (eTable 8 in the Supplement). Language preference was the only variable that was not associated with interest in receiving assistance in the stratified models. In the pooled model of participants without social risks, the 3 variables that were associated with interest in receiving assistance in the stratified models (previous exposure to health care–based social risk screening, higher perceived appropriateness of health care–based social risk screening, and recruitment from an ED setting) were no longer associated.
Discussion
In this multisite cross-sectional study of factors associated with patients’ interest in receiving social risk assistance in health care settings, we found that 53.3% of participants with a positive screening result for a social risk were interested in receiving assistance, and 8.6% of those with negative screening results were also interested in receiving assistance. Among participants with a positive screening result for at least 1 social risk, interest in receiving assistance was higher in those who answered the question about interest in receiving assistance before answering the questions about specific social risks; interest in receiving assistance was also higher in those who had a higher cumulative number of social risks, reported lower household income, and self-identified as having non-Hispanic Black ancestry. Among those with negative screening results for all 5 social risks, interest in receiving assistance was also associated with lower household income. In this group, interest in receiving assistance was also associated with worse self-rated health, previous exposure to health care–based social risk screening, higher perceived appropriateness of health care–based social risk screening, and recruitment from an ED setting; interest in receiving assistance was not associated with race/ethnicity, or the order in which questions were presented. Participants’ interest in receiving assistance, regardless of social risk screening results, was not associated with trust in clinicians, recruitment from a safety-net setting, or previous experiences of health care–based discrimination.
The proportion of patients interested in social risk assistance has varied in previous studies.6,7,9,10,11,12,13,14,15,16,17,18,20 In the present study, we found that 53.3% of those with positive screening results were interested in receiving assistance, although results varied by study site. Our finding that 8.6% of participants were interested in assistance despite receiving negative screening results is consistent with previous research.10,11,20 In the context of gaps in the data regarding the psychometric properties of social risk screening tools,46 the interest in receiving assistance among those with negative screening results might indicate that assistance initiatives should not be limited to those with positive screening results. Among those with negative screening results, higher interest in receiving assistance was associated with previous exposure to and higher acceptability of social risk screening, which suggests that as social care activities become more common in health care settings, interest in receiving assistance may increase.47
To our knowledge, this study is the first to examine the association between the order in which survey questions are presented and participant-reported interest in receiving social risk assistance. We found that interest in receiving assistance may increase when interest is assessed before specific social risks. It is possible that reviewing the risks first may have implications for individuals’ perspectives about whether they qualify for assistance, while asking about assistance first could help to convey that the reason for asking about risks is to provide assistance. Future studies are warranted to explore how the order in which survey questions are presented is associated with respondents’ interest in receiving assistance or the benefits of screening in comparison with more universal provision of assistance.11,48,49,50
Contrary to our a priori hypotheses, interest in receiving assistance was not associated with trust in clinicians, recruitment from a safety-net setting, or previous experiences with health care–based discrimination. Trust in clinicians was high at baseline, which may account for the lack of association between trust in clinicians and interest in receiving assistance in our sample. A previous analysis of this sample found that previous experience with discrimination was associated with lower perceived acceptability of social risk screening.27 In the present analyses, previous experience with discrimination was associated with lower interest in receiving assistance among those reporting social risk but higher interest in receiving assistance among those not reporting social risk; however, neither finding was statistically significant.
We found similar levels of interest in receiving assistance for housing, food, utilities, and transportation among participants with positive screening results for those risk factors. Lower levels of interest in receiving assistance were observed among participants with positive screening results for interpersonal safety. These findings, along with the low rates of reported interpersonal violence, are consistent with the literature12,51,52,53,54 and highlight the challenges in providing intervention services for individuals experiencing interpersonal violence.
Limitations
This study has several limitations. First, as a cross-sectional study, the analyses cannot indicate causation. Second, the study excluded patients and caregivers who did not speak or read English or Spanish. Third, although a diverse set of study sites was included, the sites are not representative of all health care settings. Fourth, the survey question about participants’ interest in receiving assistance was asked theoretically, as part of a research study rather than an intervention. Fifth, our analyses are limited by the variables included in the survey. Additional reasons that those with positive screening results may not be interested in receiving assistance include the receipt of false-positive results,46 the perception among patients that they are already familiar with available resources, and the ways in which assistance is offered.6,7,8,13,14,15,20,29,55 Among those with negative screening results, the additional reasons that patients may be interested in receiving assistance are similar and include the low sensitivity of the screening tools,46 concerns among patients about the consequences of endorsing social needs,23 and the likelihood that social needs are associated with one another.56,57 Sixth, the study relied on participant-reported information that could not be validated. Despite these limitations, this study has a number of strengths, including its randomized survey design and its diverse study sites and participant sample.
Conclusions
In this multisite cross-sectional study, we found multiple factors that were associated with participants’ interest in receiving social risk assistance in health care settings. For participants with positive screening results for social risks, these factors included answering survey questions about assistance before answering questions about social risks, receiving positive results for a higher number of social risks, and reporting lower household income. Interest in receiving assistance was also expressed by those with negative screening results for social risks, especially those with lower income and worse self-reported health. These findings may have implications for how and when social risk assistance is offered to patients. For example, health care organizations might opt to first offer or describe assistive services before conducting social risk screening. As the health care system’s role in addressing social risk factors evolves, more work is needed to understand patients’ perspectives on social risk screening, and patients’ interest in receiving assistance can be used to augment efforts to implement patient-centered social care interventions.
eMethods. Study Survey Tool
eTable 1. Differences in Participant and Health Center Characteristics Between Study Sample and Respondents Excluded From Sample
eTable 2. Participant Characteristics by Interest in Housing Assistance and Housing-Related Social Risk Screening Results
eTable 3. Participant Characteristics by Interest in Food Assistance and Food Insecurity Screening Results
eTable 4. Participant Characteristics by Interest in Utilities Assistance and Utilities Screening Results
eTable 5. Participant Characteristics by Interest in Transportation Assistance and Transportation Problems Screening Results
eTable 6. Participant Characteristics by Interest in Safety Assistance and Interpersonal Violence Screening Results
eTable 7. Differences in Participant Characteristics, Stratified by Social Risk Screening Results, Between Respondents Included in Multivariable Model and Respondents Excluded Owing to Missingness
eTable 8. Pooled Analyses: Unadjusted and Adjusted Associations Between Interest in Assistance Among All Participants
References
- 1.McGinnis JM, Williams-Russo P, Knickman JR. The case for more active policy attention to health promotion. Health Aff (Millwood). 2002;21(2):78-93. doi: 10.1377/hlthaff.21.2.78 [DOI] [PubMed] [Google Scholar]
- 2.Alderwick H, Gottlieb LM. Meanings and misunderstandings: a social determinants of health lexicon for health care systems. Milbank Q. 2019;97(2):407-419. doi: 10.1111/1468-0009.12390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kangovi S, Mitra N, Grande D, Long JA, Asch DA. Evidence-based community health worker program addresses unmet social needs and generates positive return on investment. Health Aff (Millwood). 2020;39(2):207-213. doi: 10.1377/hlthaff.2019.00981 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Horwitz LI, Chang C, Arcilla HN, Knickman JR. Quantifying health systems’ investment in social determinants of health, by sector, 2017-19. Health Aff (Millwood). 2020;39(2):192-198. doi: 10.1377/hlthaff.2019.01246 [DOI] [PubMed] [Google Scholar]
- 5.Murray GF, Rodriguez HP, Lewis VA. Upstream with a small paddle: how ACOs are working against the current to meet patients’ social needs. Health Aff (Millwood). 2020;39(2):199-206. doi: 10.1377/hlthaff.2019.01266 [DOI] [PubMed] [Google Scholar]
- 6.Swavely D, Whyte V, Steiner JF, Freeman SL. Complexities of addressing food insecurity in an urban population. Popul Health Manag. 2019;22(4):300-307. doi: 10.1089/pop.2018.0126 [DOI] [PubMed] [Google Scholar]
- 7.Gold R, Bunce A, Cowburn S, et al. . Adoption of social determinants of health EHR tools by community health centers. Ann Fam Med. 2018;16(5):399-407. doi: 10.1370/afm.2275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stenmark SH, Steiner JF, Marpadga S, Debor M, Underhill K, Seligman H. Lessons learned from implementation of the food insecurity screening and referral program at Kaiser Permanente Colorado. Perm J. 2018;22(18):18-093. doi: 10.7812/TPP/18-093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tong ST, Liaw WR, Kashiri PL, et al. . Clinician experiences with screening for social needs in primary care. J Am Board Fam Med. 2018;31(3):351-363. doi: 10.3122/jabfm.2018.03.170419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fox CK, Cairns N, Sunni M, Turnberg GL, Gross AC. Addressing food insecurity in a pediatric weight management clinic: a pilot intervention. J Pediatr Health Care. 2016;30(5):e11-e15. doi: 10.1016/j.pedhc.2016.05.003 [DOI] [PubMed] [Google Scholar]
- 11.Bottino CJ, Rhodes ET, Kreatsoulas C, Cox JE, Fleegler EW. Food insecurity screening in pediatric primary care: can offering referrals help identify families in need? Acad Pediatr. 2017;17(5):497-503. doi: 10.1016/j.acap.2016.10.006 [DOI] [PubMed] [Google Scholar]
- 12.Hassan A, Scherer EA, Pikcilingis A, et al. . Improving social determinants of health: effectiveness of a web-based intervention. Am J Prev Med. 2015;49(6):822-831. doi: 10.1016/j.amepre.2015.04.023 [DOI] [PubMed] [Google Scholar]
- 13.Knowles M, Khan S, Palakshappa D, et al. . Successes, challenges, and considerations for integrating referral into food insecurity screening in pediatric settings. J Health Care Poor Underserved. 2018;29(1):181-191. doi: 10.1353/hpu.2018.0012 [DOI] [PubMed] [Google Scholar]
- 14.Uwemedimo OT, May H. Disparities in utilization of social determinants of health referrals among children in immigrant families. Front Pediatr. 2018;6:207. doi: 10.3389/fped.2018.00207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Eismann EA, Theuerling J, Maguire S, Hente EA, Shapiro RA. Integration of the Safe Environment for Every Kid (SEEK) model across primary care settings. Clin Pediatr (Phila). 2019;58(2):166-176. doi: 10.1177/0009922818809481 [DOI] [PubMed] [Google Scholar]
- 16.Schickedanz A, Sharp A, Hu YR, et al. . Impact of social needs navigation on utilization among high utilizers in a large integrated health system: a quasi-experimental study. J Gen Intern Med. 2019;34(11):2382-2389. doi: 10.1007/s11606-019-05123-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Martel ML, Klein LR, Hager KA, Cutts DB. Emergency department experience with novel electronic medical record order for referral to food resources. West J Emerg Med. 2018;19(2):232-237. doi: 10.5811/westjem.2017.12.35211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Buitron de la Vega P, Losi S, Sprague Martinez L, et al. . Implementing an EHR-based screening and referral system to address social determinants of health in primary care. Med Care. 2019;57(6)(Suppl 6 Suppl 2):S133-S139. doi: 10.1097/MLR.0000000000001029 [DOI] [PubMed] [Google Scholar]
- 19.National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Board on Health Care Services; Committee on Integrating Social Needs Care into the Delivery of Health Care to Improve the Nation's Health. Integrating Social Care into the Delivery of Health Care: Moving Upstream to Improve the Nation's Health National Academies Press; 2019. Accessed December 2, 2019. https://www.ncbi.nlm.nih.gov/books/NBK552597/ doi: 10.17226/25467 [DOI] [PubMed]
- 20.De Marchis EH, Alderwick H, Gottlieb LM. Do patients want help addressing social risks? J Am Board Fam Med. 2020;33(2):170-175. doi: 10.3122/jabfm.2020.02.190309 [DOI] [PubMed] [Google Scholar]
- 21.Barnidge E, LaBarge G, Krupsky K, Arthur J. Screening for food insecurity in pediatric clinical settings: opportunities and barriers. J Community Health. 2017;42(1):51-57. doi: 10.1007/s10900-016-0229-z [DOI] [PubMed] [Google Scholar]
- 22.Rogers AJ, Hamity C, Sharp AL, Jackson AH, Schickedanz AB. Patients’ attitudes and perceptions regarding social needs screening and navigation: multi-site survey in a large integrated health system. J Gen Intern Med. 2020;35(5):1389-1395. doi: 10.1007/s11606-019-05588-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Palakshappa D, Doupnik S, Vasan A, et al. . Suburban families’ experience with food insecurity screening in primary care practices. Pediatrics. 2017;140(1):e20170320. doi: 10.1542/peds.2017-0320 [DOI] [PubMed] [Google Scholar]
- 24.Hamity C, Jackson A, Peralta L, Bellows J. Perceptions and experience of patients, staff, and clinicians with social needs assessment. Perm J. 2018;22:18-105. doi: 10.7812/TPP/18-105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Klein MD, Schumacher DJ, Sandel M. Assessing and managing the social determinants of health: defining an entrustable professional activity to assess residents’ ability to meet societal needs. Acad Pediatr. 2014;14(1):10-13. doi: 10.1016/j.acap.2013.11.001 [DOI] [PubMed] [Google Scholar]
- 26.Feder GS, Hutson M, Ramsay J, Taket AR. Women exposed to intimate partner violence: expectations and experiences when they encounter health care professionals: a meta-analysis of qualitative studies. Arch Intern Med. 2006;166(1):22-37. doi: 10.1001/archinte.166.1.22 [DOI] [PubMed] [Google Scholar]
- 27.De Marchis EH, Hessler D, Fichtenberg C, et al. . Part I: a quantitative study of social risk screening acceptability in patients and caregivers. Am J Prev Med. 2019;57(6)(suppl 1):S25-S37. doi: 10.1016/j.amepre.2019.07.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mattocks KM, Sullivan JC, Bertrand C, Kinney RL, Sherman MD, Gustason C. Perceived stigma, discrimination, and disclosure of sexual orientation among a sample of lesbian veterans receiving care in the Department of Veterans Affairs. LGBT Health. 2015;2(2):147-153. doi: 10.1089/lgbt.2014.0131 [DOI] [PubMed] [Google Scholar]
- 29.Byhoff E, De Marchis EH, Hessler D, et al. . Part II: a qualitative study of social risk screening acceptability in patients and caregivers. Am J Prev Med. 2019;57(6)(suppl 1):S38-S46. doi: 10.1016/j.amepre.2019.07.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bjarnadottir RI, Bockting W, Dowding DW. Patient perspectives on answering questions about sexual orientation and gender identity: an integrative review. J Clin Nurs. 2017;26(13-14):1814-1833. doi: 10.1111/jocn.13612 [DOI] [PubMed] [Google Scholar]
- 31.von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. Equator Network. October 22, 2019. Accessed December 2, 2019. https://www.equator-network.org/reporting-guidelines/strobe/
- 32.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377-381. doi: 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Center for Medicare and Medicaid Innovation The Accountable Health Communities Health-Related Social Needs screening tool. Centers for Medicare and Medicaid Services; 2018. Accessed March 18, 2019. https://innovation.cms.gov/files/worksheets/ahcm-screeningtool.pdf
- 34.Sandel M, Sheward R, de Cuba SE, et al. . Unstable housing and caregiver and child health in renter families. Pediatrics. 2018;141(2):e20172199. doi: 10.1542/peds.2017-2199 [DOI] [PubMed] [Google Scholar]
- 35.Mickey RM, Greenland S. The impact of confounder selection criteria on effect estimation. Am J Epidemiol. 1989;129(1):125-137. doi: 10.1093/oxfordjournals.aje.a115101 [DOI] [PubMed] [Google Scholar]
- 36.Park S, Pan L, Sherry B, Blanck HM. Consumption of sugar-sweetened beverages among US adults in 6 states: Behavioral Risk Factor Surveillance System, 2011. Prev Chronic Dis. 2014;11:E65. doi: 10.5888/pcd11.130304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Giusti C, Little RJ. An analysis of nonignorable nonresponse to income in a survey with a rotating panel design. J Off Stat. 2011;27(2):211-229. [Google Scholar]
- 38.King G, Honaker J, Joseph A, Scheve K. Analyzing incomplete political science data: an alternative algorithm for multiple imputation. Am Political Sci Rev. 2001;95(1):49-69. doi: 10.1017/S0003055401000235 [DOI] [Google Scholar]
- 39.Adjaye-Gbewonyo D, Bednarczyk RA, Davis RL, Omer SB. Using the bayesian improved surname geocoding method (BISG) to create a working classification of race and ethnicity in a diverse managed care population: a validation study. Health Serv Res. 2014;49(1):268-283. doi: 10.1111/1475-6773.12089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Grundmeier RW, Song L, Ramos MJ, et al. . Imputing missing race/ethnicity in pediatric electronic health records: reducing bias with use of US census location and surname data. Health Serv Res. 2015;50(4):946-960. doi: 10.1111/1475-6773.12295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.DeSalvo KB, Fan VS, McDonell MB, Fihn SD. Predicting mortality and healthcare utilization with a single question. Health Serv Res. 2005;40(4):1234-1246. doi: 10.1111/j.1475-6773.2005.00404.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Agency for Healthcare Research and Quality Patient Experience Measures From the CAHPS Clinician & Group Survey Document No. 2309. Updated June 1, 2017. Accessed April 19, 2018. https://www.ahrq.gov/sites/default/files/wysiwyg/cahps/surveys-guidance/cg/about/measures-cg30-2309.pdf
- 43.Hausmann LRM, Kressin NR, Hanusa BH, Ibrahim SA. Perceived racial discrimination in health care and its association with patients’ healthcare experiences: does the measure matter? Ethn Dis. 2010;20(1):40-47. [PubMed] [Google Scholar]
- 44.Bird ST, Bogart LM. Perceived race-based and socioeconomic status (SES)–based discrimination in interactions with health care providers. Ethn Dis. 2001;11(3):554-563. [PubMed] [Google Scholar]
- 45.Sandel M, Sheward R The Housing Stability Vital Sign: how health care can screen and intervene to address housing instability. Children’s HealthWatch. Accessed September 15, 2020. http://www.rootcausecoalition.org/wp-content/uploads/2017/10/Childrens-HealthWatch-Root-Cause-Presentation-1.pdf
- 46.Henrikson NB, Blasi PR, Dorsey CN, et al. . Psychometric and pragmatic properties of social risk screening tools: a systematic review. Am J Prev Med. 2019;57(6)(suppl 1):S13-S24. doi: 10.1016/j.amepre.2019.07.012 [DOI] [PubMed] [Google Scholar]
- 47.Wylie SA, Hassan A, Krull EG, et al. . Assessing and referring adolescents’ health-related social problems: qualitative evaluation of a novel web-based approach. J Telemed Telecare. 2012;18(7):392-398. doi: 10.1258/jtt.2012.120214 [DOI] [PubMed] [Google Scholar]
- 48.Makelarski JA, Thorngren D, Lindau ST. Feed first, ask questions later: alleviating and understanding caregiver food insecurity in an urban children’s hospital. Am J Public Health. 2015;105(8):e98-e104. doi: 10.2105/AJPH.2015.302719 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Beck AF, Cohen AJ, Colvin JD, et al. . Perspectives from the Society for Pediatric Research: interventions targeting social needs in pediatric clinical care. Pediatr Res. 2018;84(1):10-21. doi: 10.1038/s41390-018-0012-1 [DOI] [PubMed] [Google Scholar]
- 50.Garg A, Boynton-Jarrett R, Dworkin PH. Avoiding the unintended consequences of screening for social determinants of health. JAMA. 2016;316(8):813-814. doi: 10.1001/jama.2016.9282 [DOI] [PubMed] [Google Scholar]
- 51.O’Doherty L, Hegarty K, Ramsay J, Davidson LL, Feder G, Taft A. Screening women for intimate partner violence in healthcare settings. Cochrane Database Syst Rev. 2015;2015(7):CD007007. doi: 10.1002/14651858.CD007007.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ogunsiji O, Clisdell E. Intimate partner violence prevention and reduction: a review of literature. Health Care Women Int. 2017;38(5):439-462. doi: 10.1080/07399332.2017.1289212 [DOI] [PubMed] [Google Scholar]
- 53.Zink T, Putnam F. Intimate partner violence research in the health care setting: what are appropriate and feasible methodological standards? J Interpers Violence. 2005;20(4):365-372. doi: 10.1177/0886260504267548 [DOI] [PubMed] [Google Scholar]
- 54.Othman S, Goddard C, Piterman L. Victims’ barriers to discussing domestic violence in clinical consultations: a qualitative enquiry. J Interpers Violence. 2014;29(8):1497-1513. doi: 10.1177/0886260513507136 [DOI] [PubMed] [Google Scholar]
- 55.Marpadga S, Fernandez A, Leung J, Tang A, Seligman H, Murphy EJ. Challenges and successes with food resource referrals for food-insecure patients with diabetes. Perm J. 2019;23:18-097. doi: 10.7812/TPP/18-097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lindau ST, Makelarski JA, Abramsohn EM, et al. . CommunityRx: a real-world controlled clinical trial of a scalable, low-intensity community resource referral intervention. Am J Public Health. 2019;109(4):600-606. doi: 10.2105/AJPH.2018.304905 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lindau ST, Makelarski J, Abramsohn E, et al. . CommunityRx: a population health improvement innovation that connects clinics to communities. Health Aff (Millwood). 2016;35(11):2020-2029. doi: 10.1377/hlthaff.2016.0694 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods. Study Survey Tool
eTable 1. Differences in Participant and Health Center Characteristics Between Study Sample and Respondents Excluded From Sample
eTable 2. Participant Characteristics by Interest in Housing Assistance and Housing-Related Social Risk Screening Results
eTable 3. Participant Characteristics by Interest in Food Assistance and Food Insecurity Screening Results
eTable 4. Participant Characteristics by Interest in Utilities Assistance and Utilities Screening Results
eTable 5. Participant Characteristics by Interest in Transportation Assistance and Transportation Problems Screening Results
eTable 6. Participant Characteristics by Interest in Safety Assistance and Interpersonal Violence Screening Results
eTable 7. Differences in Participant Characteristics, Stratified by Social Risk Screening Results, Between Respondents Included in Multivariable Model and Respondents Excluded Owing to Missingness
eTable 8. Pooled Analyses: Unadjusted and Adjusted Associations Between Interest in Assistance Among All Participants