Abstract
Objectives:
Biological behavior of pancreatic neuroendocrine tumors (Pan NETs) is difficult to predict on morphology alone. The assessment of proliferation by the Ki-67 proliferation index (PI) is considered to be an important prognostic parameter in these tumors and has been endorsed by the 2017 World Health Organization (WHO) grading system for Pan NETs. Although widely accepted on surgical specimens, there is varied opinion on grading of these tumors on cytology samples. This study aimed at classification and grading of Pan NETs on endoscopic ultrasound-guided fine-needle aspiration (EUS-FNA) using the recent 2017 WHO criteria and assess the reliability of Ki-67 grading by comparing it with histology samples wherever available.
Material and Methods:
Search of cytopathology lab records over a 3-year period (June 2015–May 2018) revealed 33 cases of pancreatic NETs diagnosed on EUS-FNA specimens. Using the guidelines of 2017 WHO classification and grading of Pan NETs, retrospective grading of these Pan NETs was done. They were graded as Grades 1, 2, and 3 well differentiated Pan NETs and poorly differentiated Grade 3 neoplasms based on Ki-67 PI and cytomorphology. Cytomorphological features were compared across the three grades. The cytological grading was then compared with the histological grading where available.
Results:
Ki-67 grading on cytology was done in 32 cases (22 on cell block and 10 on smears), of which 19 (59.4%) were Grade 1, 8 (25%) were Grade 2, and 5 (15.6%) were Grade 3 tumors. The most common cytomorphological features observed in Grade 1 tumors were small round uniform cells with granular chromatin and prominent plasmacytoid morphology. As the grade increased, tumor cells showed increased pleomorphism, angulated nuclei, and less frequent plasmacytoid cells. Histopathology (biopsy/resected specimens) was available in 11 of the 32 cases. Comparison of grading on cytology and histology showed concordance in ten of the 11 cases (k value = 0.862).
Conclusion:
Our data suggest that grading of Pan NETs by assessing Ki-67 PI on cytology samples collected by EUS-FNA shows good agreement with that measured on histology samples.
Keywords: Pancreatic neuroendocrine tumor, Ki-67 proliferation index, Cytological Ki-67 grading, Endoscopic ultrasound-guided fine-needle aspiration
INTRODUCTION
Pancreatic neuroendocrine tumors (Pan NETs) are uncommon and comprise approximately 2% of all pancreatic tumors.[1] Endoscopic ultrasound (EUS) has emerged as a useful diagnostic tool in evaluation of pancreatic masses and several authors have shown sensitivity and accuracy rates >80% in diagnosing Pan NETs by EUS guided fine-needle aspiration (EUS-FNA).[2,3] Morphology alone cannot be used to predict the prognosis in these tumors. It is currently stated that grading and staging of these tumors are the strongest predictors of outcome.[4]
The recent World Health Organization (WHO) classification and grading of Pan NETs (2017) have categorized them on basis of morphology and Ki-67 proliferation index (PI) into well differentiated Pan NETs (WD Pan NETs), poorly differentiated pancreatic neuroendocrine carcinomas (PD Pan NECs), and mixed neuroendocrine-non neuroendocrine neoplasms (Mi NENs).[5] WD Pan NETs are further divided based on the proliferative activity assessed by mitotic count and/or Ki-67 PI into Grades 1, 2, and 3 while all PD Pan NECs are categorized as Grade 3 tumors.[5] Thus, Grade 3 Pan NETs now include well differentiated and poorly differentiated types based on morphological and molecular characteristics. WD Grade 3 Pan NETs need to be separated from PD Grade 3 Pan NEC because of the differences in their prognosis, behavior, and treatment response.[6] WD Grade 3 Pan NETs are usually locally advanced disease. These tumors show an increased proliferation rate over the course of disease progression.[7] In contrast, PD Grade 3 Pan NEC invariably presents at advanced stage, is aggressive in nature, and has poor survival.[8] Many studies have validated Ki-67 PI as an important prognostic indicator and emphasized its role in grading of these tumors. Grading by Ki-67 PI is widely accepted on histology samples. On the other hand, there is no consensus on accuracy of grading on FNA cytology samples.[9] Hence, this study was planned to assess the feasibility and reliability of grading of Pan NETs using morphology and Ki-67 PI (as per the 2017 WHO classification and grading guidelines) on cytology samples obtained by EUS-FNA in comparison to that on histological samples (biopsies and/or resection specimens).
MATERIAL AND METHODS
Patient selection
Analysis of records of cytopathology laboratory over a 3-year period (June 2015–May 2018) was done (retrospective study). A total of 450 patients with EUS-FNA of pancreatic masses were retrieved and of these 33 cases (7.3%) had been diagnosed as Pan NETs. EUS-FNA was performed by gastroenterologists using Olympus GF UCT 180 curvilinear scope and 22- gauge needle after obtaining a written informed consent from the patient. Smears and cell block were prepared from FNA material. Cytomorphological diagnosis was based on Papanicolaou+ and May-Grunwald Giemsa stained smears and immunohistochemistry (IHC) for synaptophysin and/or chromogranin on cell block/ smears. Demographic profile and presenting symptoms of the patients were retrieved from the records.
Cell-block preparation and fixative used
One dedicated pass of EUS- FNA with a wider gauge needle was used to prepare one cell block for each case. The de novo clotted specimen method was used, i.e., the aspirate was allowed to clot with the aspirated blood and then the clot was carefully expelled into a filter paper moistened with 10% formalin. The filter paper was folded and put into a cassette which was then immersed in a container with 10% formalin and sent to the laboratory. This was further processed as formalin fixed paraffin embedded (FFPE) blocks similar to surgical pathology specimens.
Number of cell-blocks prepared: 25. Specimen collected in: 10% formalin
Duration of specimen in the collection media and temperature: 3–4 h, room temperature
Any processing before making the cell-block: No
Fixation time in 10% formalin (before start of actual tissue processing): 5–6 h.
Ki-67 grading
Ki-67 IHC staining was done on 2 μm deparaffinised cell block sections using Biogenex mouse monoclonal Ki-67 antibody-clone BGX-297 in Biogenex X-matrix autostainer. A minimum of at least 200 tumor cells for manual counting of Ki-67 was considered as adequate. Distinct nuclear staining of the tumor cells was regarded as positive. As per the WHO recommendation, areas of highest density of Ki-67 immunoreactivity called hotspots were selected for counting of Ki-67 PI. One cell block was available for each case of which 22 cell blocks showed adequate number of tumor cells (>200) for IHC with Ki-67. In ten cases, IHC was done on alcohol fixed destained smears. One case was excluded because of scant material. A scan of the entire cell block section was done with ×4 objective and areas of hot spots (areas with highest Ki67 nuclear labeling) were identified. Total number of tumor cells counted in these areas ranged from 500 to 2000. In three cases, counting could be done in 200 cells.
Manual eye counting method under a microscope was used for counting Ki-67 positive tumor cells, i.e., tumor cells showing crisp dark brown nuclear staining.[10] Morphologically identifiable non tumor or stromal cells were excluded from the count.
Ki-67 PI was calculated as percentage of positive cells (positive cells per 100 tumor nuclei).
Tumors were graded as G1, G2, and G3 based on Ki-67 PI as per the WHO criteria. In 11/32 cases, corresponding surgical resected specimens or biopsies were available and Ki-67 grading was done.
Cytomorphology evaluation
The cytology smears and cell blocks of 32 Pan NETs included were re-evaluated for morphological features independently by three cytologists. They were blinded to clinical history and grading of the tumors. The cytomorphological features assessed were: Shape of nuclei (round/angulated), nuclear contour, presence of plasmacytoid morphology, nuclear pleomorphism, nuclear chromatin, nucleoli, presence of rosettes, perivascular arrangement of tumor cells, abundant cytoplasm, presence of nuclear tangles, apoptotic debris, and molding and necrosis [Table 1]. Tumors were classified as well differentiated and poorly differentiated using WHO criteria. Similarly hematoxylin and eosin sections from 11 cases were also studied and graded into well differentiated and poorly differentiated.
Table 1:
Comparison of cytomorphological features in G1, G2, and G3-WD Pan NETs and G3-PD Pan NEC.
| Cytological features | WD-Pan NET | PD-Pan NEC | ||
|---|---|---|---|---|
| G1 (n=19) | G2 (n=8) | G3-WD (n=2) | G3-PD (n=3) | |
| Ki-67 index range | 1–<3% | 3–10% | 21–27% | 29–90% |
| Architecture | ||||
| Perivascular arrangement of tumor cells | 6 | 2 | 1 | 0 |
| Rosettes | 9 | 2 | 2 | 2 |
| Molding | 5 | 3 | 1 | 2 |
| Plasmacytoid | 15 | 6 | 1 | 1 |
| Nuclear features | ||||
| Shape | Round (17) Angulated (2) | Round (6) Angulated (2) | Round (1) Angulated (1) | Round (1) Angulated (3) |
| Smooth nuclear contour | 18 | 7 | 2 | 2 |
| Chromatin (salt and pepper) | 16 | 4 | 1 | 1 |
| Nuclear tangles | 4 | 3 | 1 | 3 |
| Prominent nucleoli | 1 | 2 | 1 | 2 |
| Nuclear pleomorphism | 2 | 2 | 1 | 2 |
| Cytoplasm | ||||
| Abundant cytoplasm | 14 | 5 | 1 | 0 |
| Background | ||||
| Apoptosis | 2 | 4 | 1 | 3 |
| Necrosis | 0 | 2 | 1 | 2 |
WD: Well differentiated, PD: Poorly differentiated
Statistical analysis
The agreement between cytological and histological grade was evaluated using percent agreement and Kappa statistics. All statistical analysis was performed with SAS 9.2, SPSS 15.0, Stata 10.1.
RESULTS
Clinical and imaging characteristics
The patient population consisted of 19 (57.6%) males and 14 (42.4 %) females, with age ranging from 17 to 70 years. The commonest clinical presentation was abdominal pain (48.5%), followed by recurrent diarrhea. Majority of tumors were located in head of pancreas (73%) with size ranging from 1.1 × 1 cm to 7 × 5.5 cm.
Classification on cytomorphology
Based on cytomorphology, Pan NETs were categorized as WD and PD tumors [Table 1]. WD tumors tended to have more of round nuclei, smooth nuclear contours, minimal pleomorphism, and plasmacytoid cells with abundant cytoplasm [Figure 1a-c]. In contrast, PD Pan NET demonstrated pleomorphic angulated nuclei, nuclear molding, nucleoli, more prominent nuclear tangles, apoptosis, and necrosis [Figure 1d]. Of all the 32 cases, only three were considered as PD based on cytomorphology and all three were small cell type.
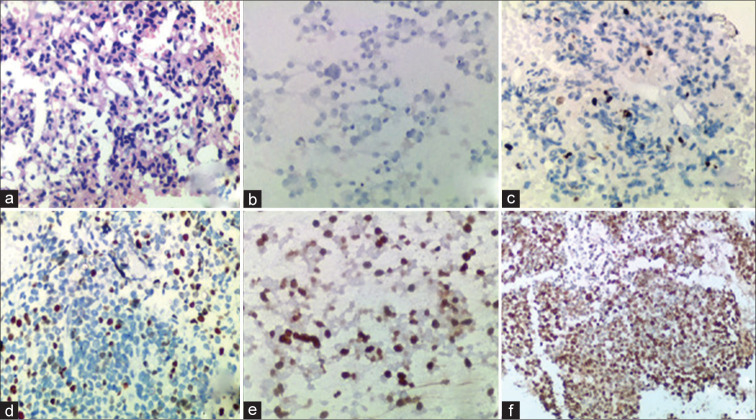
Figure 1:
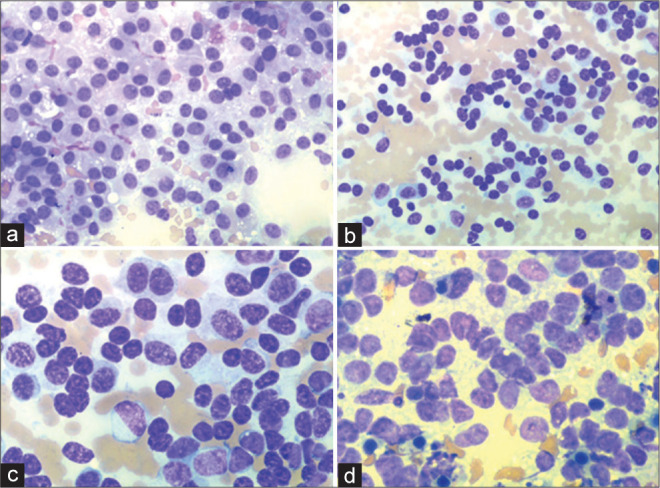
(a) G1WD pancreatic neuroendocrine tumor (Pan NET) with classical plasmacytoid morphology and smooth nuclear contours (May-Grunwald Giemsa stain, ×20), (b) G2 WD Pan NET showing uniform round nuclei and smooth nuclear contours (×20), (c) G3 WD Pan NET with mild nuclear pleomorpism, few cells with abundant cytoplasm and focal nuclear molding (×40), (d) G3 PD Pan NEC (small cell type) showing nuclear molding, angulated nuclei, rosettes, scant cytoplasm, and few nuclear tangles (×40).
Histologic classification
Histological features were reviewed in 11 cases and classified as WD and PD based on morphology. WD tumors have organoid architecture, plasmacytoid cells, and fine granular chromatin. PD tumors have patternless architecture with cells showing nuclear molding. These cells were small with scant cytoplasm and hyperchromatic nuclei. Apoptotic debris and mitotic figures were also noted. Tumors were categorized as WD and PD in 6 and 1 cases, respectively [Table 2]. Four tumors were intermediate in morphology showing predominantly well differentiated features but with focal areas showing nuclear atypia, overlapping, and coarse chromatin.
Table 2:
Comparison of morphology and grading of neuroendocrine tumors. Cytology versus histology.
| Case No. | Cytology | Histology | ||||
|---|---|---|---|---|---|---|
| Morphology | Ki-67% | Grade | Morphology | Ki-67% | Grade | |
| 1 | WD + nuclear tangles and molding | 21 | 3 | WD + poorly differentiated areas | 25 (R) | 3 |
| 2 | WD | <3 | 1 | WD | 2 (R) | 1 |
| 3 | WD | <3 | 1 | WD | <2 (B) | 1 |
| 4 | WD + focal anisonucleosis | 27* | 3 | WD + poorly differentiated areas | 24 (B) | 3 |
| 5 | WD | <2* | 1 | WD + nuclear pleomorphism | 1 (R) | 1 |
| 6 | PD | 29* | 3 | PD | 25 (B) | 3 |
| 7 | WD | 3 | 2 | WD | 6–7 (B) | 2 |
| 8 | WD + nuclear pleomorphism | 6 | 2 | Intermediate | 3 (R) | 2 |
| 9 | WD | <2 | 1 | WD | 2 (R) | 1 |
| 10 | WD | 7-8 | 2 | WD | 3–4 (R) | 2 |
| 11 | WD | <2* | 1 | WD | 4 (B) | 2 |
Cytological Ki-67 grading done on alcohol fixed Pap stained smears=Four cases. R: Resection (six cases), B: Biopsy (five cases), WD: Well differentiated, PD: Poorly differentiated
Ki-67 grading
Ki-67 counting in all the cases was done blindly by one pathologist using the same microscope. In 29 cases, total number of tumor cells counted ranged from 500 to 2000. In three cases, counting could be done in 200 cells. WD- Pan NET were graded as G1, G2, and G3 in 19, 8, and 2 cases, respectively [Table 1], while PD-Pan NEC was all G3. Ki-67 PI ranges were 1–<3% (G1), 3–10% (G2), and 21–90% (G3). Median values were 2%, 6%, and 50% for G1, G2, and G3 tumors [Figure 2].
Figure 2:
(a) Cell block section of pancreatic neuroendocrine tumor (Pan NET) derived from EUS-FNA material (hematoxylin and eosin stain, ×20) (b) Pan NET G1 with Ki-67 positivity <3%, cell block (c) G2 with Ki-67 positivity between 3-20%, cell block (d) G3 WD Pan NET with Ki-67 positivity >20%, cell block (e) G3 WD Pan NET with Ki-67 positivity >20%, smear and (f) G3 PD Pan NEC with Ki-67 positivity >20%, cell block.
Comparison of cytology and histology grades using Ki-67 PI
Comparison of grading on cytology samples with histology could be done in 11 of 32 cases (six resected and five biopsies). There was agreement in grading in ten of the 11 (90.9%) cases. Of these 11 cases, the cytological grading based on Ki-67 PI was assessed on cell blocks in seven cases and on smears in four cases. One case demonstrated discordance between the cytological (done on smear) and histological grade. It was interpreted as G1 on cytological smears (Ki-67 PI <2%) but was scored as G2 by histological evaluation (Ki-67 PI 4%). No cases of G1 and G2 Pan NETs were upgraded to G3 Pan NETs on histological grading. The Kappa statistics was 0.862 suggesting a very good agreement. Results of the Ki-67 PI on cytology and histology are summarized in Table 2.
DISCUSSION
Pan NET is uncommon tumors. They are being diagnosed more often in cytopathology laboratories in past two decades due to emergence of EUS-FNA as a sensitive and accurate tool in evaluation of pancreatic masses and availability of IHC on FNA material. Some of these tumors are incidental findings on imaging, while others can present with abdominal pain, recurrent diarrhea and reflux.[11]
In the present study, the age of patients with Pan NET ranged from 17 to 70 years with a male to female ratio of 1.3:1. Majority presented as a well-defined mass in the pancreatic head on imaging. EUS-FNA established the diagnosis by cytomorphology, supplemented by IHC using one or more neuroendocrine markers.
Ki-67 PI is widely used to determine proliferative index for grading; however, vast majority of available data on grading of these tumors using Ki-67 PI are based on examination of surgical specimens. Only few studies have analyzed grading of Pan NETs using Ki-67 PI on EUS-FNA material.[9,11,12] Prognosis of these tumors is variable and is difficult to predict on morphology alone. The WHO has classified Pan NET into WD, PD, and mixed. Grading of these tumors is based on proliferative index for planning therapy. In the few studies available, the concordance rate of cytology and histology grading varied from 39%[13] to as high as 89.5%.[4] Further, as the current WHO classification and grading of Pan NETs are very recent (2017), only a handful of studies have applied the new criteria of classifying and grading on cytology samples.
In the present study, out of 32 cases of Pan NETs, 19 (59.4%) were Grade 1 tumors, eight (25%) were Grade 2 tumors, and five (15.6%) were Grade 3 tumors. Of the five cases of Grade 3 Pan NETs, two (6.25%) were WD and three (9.4%) were PD Grade 3 Pan NECs showing morphology of a small cell carcinoma. Similarly in a recent study, Grosse et al. graded Pan NETs using Ki-67 PI and WHO (2017) classification on EUS-FNA cytology samples. In their study, which included 15 cases of Pan NETs, two (13%) cases were scored as Grade 1 tumors, nine (60%) cases were scored as Grade 2 tumors and four (27%) cases were scored as Grade 3 tumors on EUS-FNA cytology sample. Further all the Grade 3 Pan NETs were classified as well differentiated Grade 3 based on morphology and molecular analysis.[5]
The results of present study showed a very good agreement between Ki-67 expression measured on EUS-FNA cytology samples when corelated with the Ki-67 expression measured on histology samples ascertaining the good reproducibility of this test when performed on EUS-FNA specimens. Grosse et al. found 100% concordance between cytology and histology grading using Ki-67 PI.[5] Weynand et al. in a study population of 46 Pan NETs, 33 of which had corresponding surgical specimens showed a good agreement of Ki-67 PI in EUS-FNA samples and surgical samples. Discrepancy between cytological and histological grade in present study was observed in only one G2 tumor where cytology underestimated the grading. Similarly, Weynand et al. found discrepancies in G2 tumors where cytology underestimated the grading.[9] In the present study, no case of cytological G1- G2 Pan NET was upgraded to G3 Pan NET on histological grading which has therapeutic implications. Carlinfante et al. demonstrated cytological and histological grading concordance in 46 out of 53 (86.8%) Pan NET cases and no case of G1-G2 Pan NET graded on cytology was upgraded to G3 on histological grading.[12] In contrast to our study, Weiss et al. reported a poor concordance of grading of 39% between FNA cell blocks and resection specimens. The discordant grading in their study was related to the larger size of the tumor.[13] Unno et al.[14] and Rebours et al.[15] similarly demonstrated that the concordance varied as per the tumor pattern and size with solid and small tumors having good correlation while cystic and larger tumors having poor correlation concluding that solid and small tumors are more homogenous showing a more consistent Ki-67 grading.
Various methods have been advocated for preparation of cell blocks from cytology material. A detailed review of cell block preparation and effect of fixatives used especially on IHC and molecular analysis has been done by Shidham. Cell-blocks prepared using formalin as fixative and processed as FFPE tissue show histomorphology and IHC results comparable to that of formalin-fixed biopsies and resections. Chemical fixatives such as acidic solutions (Picric acid, and Bouin’s fixative) and fixatives with heavy metal (B5, and Zenker’s fixative) although show comparable histomorphology, the immunostaining results may not be comparable to FFPE and may show aberrant immunoprofile. Alcohol based fixatives such as methanol (PreservCyt, CytoLyt of LBC) and ethanol (SurePath LBC) can show cell shrinkage and interference with IHC integrity giving fallacious immunoprofiles which are especially applicable to nuclear immunomarkers like Ki-67.[16]
The WHO (2010 and 2017) has recommended that for estimation of Ki-67 PI in tissue samples, a manual count of Ki-67 positive tumor cells in a minimum of 500–2000 tumor cells in areas of highest Ki-67 nuclear labeling or hot spots should be done.[17] In cytology samples, the Ki-67 PI index should be calculated in tumor hot spots.[11,18] In the present study, in the majority of cases (n = 29), 500–2000 cell were counted for Ki-67 index except in three cases where only 200 cells could be counted. Weynand et al. did not notice any increase in the cytology histology Ki-67 concordance rate by excluding samples with <200 tumor cells in EUS-FNA samples.[9] However, Hasegawa et al. showed an improved concordance rate of 90% when cytological samples with <200 tumor cells were excluded from the analysis.[19]
In the present study, manual counting through microscopic evaluation was used to estimate Ki-67 PI. Reid et al. analyzed different approaches to estimate Ki-67 PI in 68 surgically resected Pan NETs. These included eye-balling, automated counting by digital image analyzer, manual eye-counting, and manual counting of camera-captured/printed image.[10] At present, 2017 WHO recommends manual counting of printed or camera- captured images of hot spot for calculating the Ki-67 PI.[17]
In the present study, grading was done on the basis of Ki-67 PI as per criteria defined by the WHO 2017. Evaluation of mitotic figures morphologically was not done. Ki-67 PI is considered to be a preferable approach for grading Pan NETs than parameters based only on the number of mitotic figures with/without necrosis. It is superior and more reproducible than mitotic count. Furthermore, focal necrosis may not be sampled on FNA. Morphological evaluation for various features was done across the three grades in the present study with the aim of classifying into well differentiated and poorly differentiated. The presence of extensive necrosis was observed in two cases of G3-PD Pan NEC while focal necrosis was seen in one case of G3-WD Pan NET and two cases of G2-WD Pan NET.[20]
In the current study, all the concordant cases of cytology and histology grading had Ki-67 PI estimation done on cell block sections. The one case which demonstrated discordance had Ki-67 PI estimation on FNA alcohol fixed smear. To the best of our knowledge, the majority of studies of Pan NETs have demonstrated good agreement on EUS-FNA cell blocks using Ki-67 PI when compared with histological grading, while grading on smears have shown variable results. Carlinfante et al. did not observe any difference when Ki-67 PI was measured on alcohol-fixed smears or cell block sections.[12] Piani et al. estimated Ki-67 PI only on cytological smears and they showed an agreement rate of 78% between cytological grading and histological grading.[21] However, further studies are needed to establish feasibility of Ki-67 estimation on FNA smears only without cell blocks.
In the current study, only one case showed discordance between the cytological and histological grading as it had been undergraded on cytology as G1 while on histology it was G2. There are certain challenges in estimation of Ki67 PI. Undergrading on cytology can be attributed to tumor heterogeneity in Pan NETs and it is plausible that EUS-FNA may not always sample the most proliferative area of the tumor. Tumor size may be one of the causes as discordant cases reported in some studies had significantly larger tumor size. Overestimation of Ki-67 PI can be due to lymphocytic infiltration in tumor or proliferating stromal cells including endothelial cells which can be wrongly interpreted as Ki-67 positivity leading to upgrading of the tumor.[13,20] Stromal cells (endothelial cells, fibroblasts) can be differentiated morphologically. Stromal cells when compared to tumor cells are few in number, more scattered, and usually spindle shaped.
Dual-color Ki-67 protocol (Shidham’s dual-color immunostaining – Ki-67: Brown nuclear with LCA: red cytoplasmic) has shown to help differentiate Ki-67 positive tumor cells (without red cytoplasmic immunostaining) from lymphocytes (cells with both nuclear brown and red cytoplasmic immunostaining). This has been shown to increase the precision of quantifying Ki-67 PI especially in borderline cases and in differentiating WHO Grade 1 and Grade 2 tumors.[20]
Mejías-Badillo et al. in their study of 23 surgical specimens of WD G1 and WD G2 Pan NETs reported higher precision of classifying cases into Grades 1 and 2 with dual color immunostaining protocol.[20]
Basturk et al. determined that WD G3 Pan NETs are significantly less aggressive than PD G3 Pan NECs suggesting that the G3 category is heterogeneous and can be further divided into WD G3 Pan NET and PD G3 Pan NEC.[7] Recently, 2017 WHO has divided G3 Pan NETs into WD and PD. In the present study, G3 Pan NETs were divided into WD and PD based on cytomorphology highlighting the significance in segregating these two groups as both have different prognosis and management. Of five cases of G3 Pan NETs, two were WD, and three were PD. Prominent cytomorphological feature of G3 WD Pan NETs when compared with G3 PD Pan NETs was a predominant plasmacytoid appearance of tumor cells, round nuclei with smooth nuclear contours, and minimal pleomorphism whereas, the G3 PD Pan NETs demonstrated pleomorphic and angulated nuclei, apoptosis, nuclear tangles, and lack of plasmacytoid morphology.
Pancreatic neuroendocrine neoplasms with a Ki-67 labeling index >20% were reclassified in 2017 by the WHO into well differentiated and poorly differentiated Grade 3 neuroendocrine carcinoma. At present, differentiation is based on subjective morphologic assessment. However, recent advances in molecular analysis of Pan NET have shown ability to separate WD NETs from NEC. WD NET grading is supported by either loss of death domain- associated protein (DAXX) or α thalassemia/mental retardation syndrome X (ATRX) protein expression by IHC or by presence of DAXX, ATRX, or menin (MEN1) mutation. PD NEC grading is supported by either loss of retinoblastoma 1 (RB1) protein expression by IHC, protein overexpression of tumor protein (TP53) by IHC, or presence of RB1, TP53, or Kirsten rat sarcoma oncogene homolog (KRAS) mutation. However, these tests are not yet universally available and may not be applicable currently in most centers.[6]
Patients with Pan NETs need to have a multidisciplinary therapeutic approach. Surgery is the treatment of choice for most of the cases of Pan NETs. However, for small non- functional tumors (<2 cm in diameter) and in unresectable tumors or metastatic disease, evaluation on cytological specimens can play a major role in tumor classification and determination of treatment strategies.[22]
The current study is limited by small sample size and included only five Grade 3 tumors. Corelation of Ki-67 grading on cytology with histology was limited to eleven cases only. High grade Pan NETs are rare tumors and are often treated with chemotherapy without undergoing surgical resection of the tumor. Overall, the present study has shown good agreement of cytological grading of Pan NETs when compared with histological grading as per the WHO 2017 classification. However, it is advisable to have larger multicenter studies to evaluate the reproducibility of Ki-67 PI on cytology samples when compared to histology.
CONCLUSION
Our study demonstrates an overall good agreement between Ki-67 grading done on cytology samples when collected by EUS-FNA with that measured on histology samples. In addition, cytomorphological features based on 2017 WHO classification of NETs can give a clue to the grading of these tumors. Hence, a pre-operative classification of Pan NETs based on Ki-67 grading on cytology samples is feasible and can guide clinical and therapeutic decisions.
Footnotes
How to cite this article: Kalantri S, Bakshi P, Verma K. Grading of pancreatic neuroendocrine tumors on endoscopic ultrasound-guided fine- needle aspiration using Ki-67 index and 2017 World Health Organization criteria: An analysis of 32 cases. CytoJournal 2020;17:21.
HTML of this article is available FREE at: https://dx.doi.org/10.25259/Cytojournal_4_2020
COMPETING INTERESTS STATEMENT BY ALL AUTHORS
The authors declare that they have no competing interests.
AUTHORSHIP STATEMENT BY ALL AUTHORS
All authors of this article declare that we qualify for authorship as defined by ICMJE http://www.icmje.org/#author. Each author has participated adequately in the work and takes public responsibility for appropriate portions of the content of this article. SK, PB and KV conceptualized and designed the study. SK, PB and KV contributed in data collection, analysis and interpretation of data. SK, PB and KV drafted and critically analyzed the article. All authors read and approved the final manuscript. Each author acknowledges that this final version was read and approved.
ETHICS STATEMENT BY ALL AUTHORS
This was a retrospective analysis of the data and all the procedures were done after obtaining informed consents from patients.
LIST OF ABBREVIATIONS (In alphabetic order)
EUS – Endoscopic ultrasound
EUS – FNA-Endoscopic ultrasound guided fine needle aspiration
FFPE – Formalin fixed paraffin embedded
G – Grade
H&E – Hematoxylin and eosin
IHC – Immunohistochemistry
MGG – May-Grunwald Giemsa
NEC – Neuroendocrine carcinoma
NET – Neuroendocrine tumors
Pan NETs – Pancreatic neuroendocrine tumors
PD – Poorly differentiated
PI – Proliferation index
WD – Well differentiated
WHO – World Health Organization.
EDITORIAL/PEER-REVIEW STATEMENT
To ensure the integrity and highest quality of CytoJournal publications, the review process of this manuscript was conducted under a double-blind model (authors are blinded for reviewers and vice versa) through automatic online system.
References
- 1.Fitzgerald TL, Hickner ZJ, Schmitz M, Kort EJ. Changing incidence of pancreatic neoplasms: A 16-year review of statewide tumor registry. Pancreas. 2008;37:134–8. doi: 10.1097/MPA.0b013e318163a329. [DOI] [PubMed] [Google Scholar]
- 2.Ardengh JC, de Paulo GA, Ferrari AP. EUS-guided FNA in the diagnosis of pancreatic neuroendocrine tumors before surgery. Gastrointest Endosc. 2004;60:378–84. doi: 10.1016/S0016-5107(04)01807-3. [DOI] [PubMed] [Google Scholar]
- 3.Pais SA, Al-Haddad M, Mohamadnejad M, Leblanc JK, Sherman S, McHenry L, et al. EUS for pancreatic neuroendocrine tumors: A single-center, 11-year experience. Gastrointest Endosc. 2010;71:1185–93. doi: 10.1016/j.gie.2009.12.006. [DOI] [PubMed] [Google Scholar]
- 4.Jin M, Roth R, Gayetsky V, Niederberger N, Niederberger N, Lehman A, et al. Grading pancreatic neuroendocrine neoplasms by Ki-67 staining on cytology cell blocks: Manual count and digital image analysis of 58 cases. J Am Soc Cytopathol. 2016;5:286–95. doi: 10.1016/j.jasc.2016.03.002. [DOI] [PubMed] [Google Scholar]
- 5.Grosse C, Noack P, Silye R. Accuracy of grading pancreatic neuroendocrine neoplasms with Ki-67 index in fine-needle aspiration cellblock material. Cytopathology. 2019;30:187–93. doi: 10.1111/cyt.12643. [DOI] [PubMed] [Google Scholar]
- 6.Sigel CS, Silva VW, Reid MD, Chhieng D, Basturk O, Sigel KM, et al. Well differentiated grade 3 pancreatic neuroendocrine tumors compared with related neoplasms: A morphologic study. Cancer Cytopathol. 2018;126:326–35. doi: 10.1002/cncy.21982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Basturk O, Yang Z, Tang LH, Hruban RH, Adsay V, McCall CM, et al. The high-grade (WHO G3) pancreatic neuroendocrine tumor category is morphologically and biologically heterogenous and includes both well differentiated and poorly differentiated neoplasms. Am J Surg Pathol. 2015;39:683–90. doi: 10.1097/PAS.0000000000000408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Heetfeld M, Chougnet CN, Olsen IH, Rinke A, Borbath I, Crespo G, et al. Characteristics and treatment of patients with G3 gastroenteropancreatic neuroendocrine neoplasms. Endocr Relat Cancer. 2015;22:657–64. doi: 10.1530/ERC-15-0119. [DOI] [PubMed] [Google Scholar]
- 9.Weynand B, Borbath I, Bernard V, Sempoux C, Gigot JF, Hubert C, et al. Pancreatic neuroendocrine tumour grading on endoscopic ultrasound-guided fine needle aspiration: High reproducibility and inter-observer agreement of the Ki-67 labelling index. Cytopathology. 2014;25:389–95. doi: 10.1111/cyt.12111. [DOI] [PubMed] [Google Scholar]
- 10.Reid MD, Bagci P, Ohike N, Saka B, Seven IE, Dursun N, et al. Calculation of the Ki67 index in pancreatic neuroendocrine tumors: A comparative analysis of four counting methodologies. Mod Pathol. 2015;28:686–94. doi: 10.1038/modpathol.2014.156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Farrell JM, Pang JC, Kim GE, Tabatabai ZL. Pancreatic neuroendocrine tumors: Accurate grading with Ki-67 index on fine-needle aspiration specimens using the WHO 2010/ENETS criteria. Cancer Cytopathol. 2014;122:770–8. doi: 10.1002/cncy.21457. [DOI] [PubMed] [Google Scholar]
- 12.Carlinfante G, Baccarini P, Berretti D, Cassetti T, Cavina M, Conigliaro R, et al. Ki-67 cytological index can distinguish well-differentiated from poorly differentiated pancreatic neuroendocrine tumors: A comparative cytohistological study of 53 cases. Virchows Arch. 2014;465:49–55. doi: 10.1007/s00428-014-1585-7. [DOI] [PubMed] [Google Scholar]
- 13.Weiss VL, Kiernan C, Wright J, Merchant NB, Coogan AC, Shi C. Fine-needle aspiration-based grading of pancreatic neuroendocrine neoplasms using Ki-67: Is accurate WHO grading possible on cytologic material? J Am Soc Cytopathol. 2018;7:154–459. doi: 10.1016/j.jasc.2018.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Unno J, Kanno A, Masamune A, Kasajima A, Fujishima F, Ishida K, et al. The usefulness of endoscopic ultrasound-guided fine-needle aspiration for the diagnosis of pancreatic neuroendocrine tumors based on the World Health Organization classification. Scand J Gastroenterol. 2014;49:1367–74. doi: 10.3109/00365521.2014.934909. [DOI] [PubMed] [Google Scholar]
- 15.Rebours V, Cordova J, Couvelard A, Fabre M, Palazzo L, Vullierme MP, et al. Can pancreatic neuroendocrine tumour biopsy accurately determine pathological characteristics? Dig Liver Dis. 2015;47:973–7. doi: 10.1016/j.dld.2015.06.005. [DOI] [PubMed] [Google Scholar]
- 16.Shidham VB. CellBlockistry: Chemistry and art of cell-block making-a detailed review of various historical options with recent advances. Cytojournal. 2019;16:12. doi: 10.4103/cytojournal.cytojournal_20_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lloyd RV, Osamura RY, Klöppel G, Rosai J, editors. 4th ed. Vol. 10. Lyon: International Agency for Research on Cancer; 2017. WHO Classification of Tumours of Endocrine Organs; pp. 209–39. [Google Scholar]
- 18.Arco CD, Pérez JÁ, Medina LO, Valera JS, Aceñero MJ. Reliability of Ki-67 determination in FNA samples for grading pancreatic neuroendocrine tumors. Endocr Pathol. 2016;27:276–83. doi: 10.1007/s12022-016-9455-2. [DOI] [PubMed] [Google Scholar]
- 19.Hasegawa T, Yamao K, Hijioka S, Bhatia V, Mizuno N, Hara K, et al. Evaluation of Ki-67 in EUSFNA specimens for the assessment of malignancy risk in pancreatic neuroendocrine tumors. Endoscopy. 2014;46:32–8. doi: 10.1055/s-0033-1344958. [DOI] [PubMed] [Google Scholar]
- 20.Mejías-Badillo L, Jeanty J, Khalid K, Bhalla A, Salem N, Thomas S, et al. Dual-color immunocytochemistry (Ki-67 with LCA) for precise grading of pancreatic neuroendocrine tumors with applicability to small biopsies and cell blocks. Cytojournal. 2020;17:6. doi: 10.25259/Cytojournal_92_2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Piani C, Franchi GM, Cappelletti C, Scavini M, Albarello L, Zerbi A, et al. Cytological Ki-67 in pancreatic neuroendocrine tumors: An opportunity for pre-operative grading. Endocr Relat Cancer. 2008;15:175–81. doi: 10.1677/ERC-07-0126. [DOI] [PubMed] [Google Scholar]
- 22.Alexiev BA, Darwin PE, Goloubeva O, Loffe OB. Proliferative rate in endoscopic ultrasound fine-needle aspiration of pancreatic endocrine tumors: Correlation with clinical behavior. Cancer. 2009;117:40–5. doi: 10.1002/cncy.20014. [DOI] [PubMed] [Google Scholar]