Abstract
With covalently closed circular structures, circular RNAs (circRNAs) were once misinterpreted as by-products of mRNA splicing. Being abundant, stable, highly conserved, and tissue-specific, circRNAs are recently identified as a type of regulatory RNAs. CircRNAs bind to certain miRNAs or proteins to participate in gene transcription and translation. Emerging evidence has indicated that the dysregulation of circRNAs is closely linked to the tumorigenesis and treatment response of hematological malignancies. CircRNAs play critical roles in various biological processes, including tumorigenesis, drug resistance, tumor metabolism, autophagy, pyroptosis, and ferroptosis. The N6-methyladenosine modification of circRNAs and discovery of fusion-circRNAs provide novel insights into the functions of circRNAs. Targeting circRNAs in hematological malignancies will be an attractive treatment strategy. In this review, we systematically summarize recent advances toward the novel functions and molecular mechanisms of circRNAs in hematological malignancies, and highlight the potential clinical applications of circRNAs as novel biomarkers and therapeutic targets for future exploration.
Keywords: Circular RNAs, Hematological malignancies, Tumorigenesis, Drug-resistance, Biomarker
Background
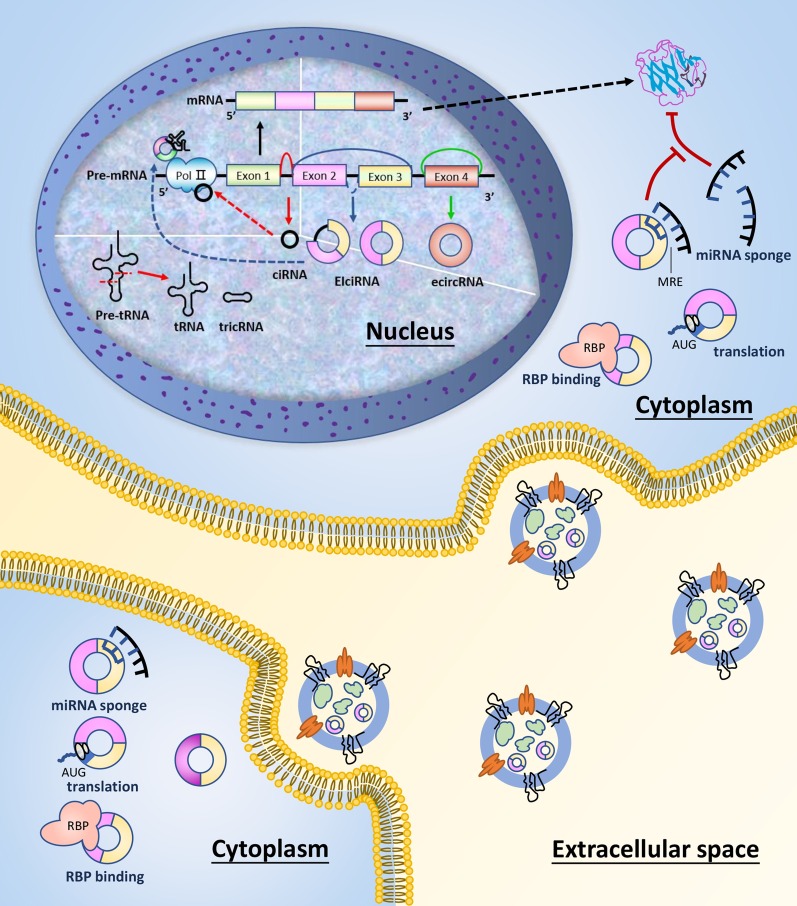
Circular RNAs (circRNAs) are a novel type of competing endogenous RNAs (ceRNAs) of the non-coding RNA (ncRNA) families. Without 5′ and 3′ ends, they are hallmarked by covalently closed continuous loops and are more stable than linear RNAs in vivo [1]. CircRNAs are abundant in biological cells, highly conserved, and expressed in a tissue-specific pattern [2]. CircRNAs are classified into four categories, including exon circRNAs (ecRNAs), circular intron RNAs (ciRNAs), exon-intron circRNAs (EIciRNAs), and tRNA intronic circular RNAs (tricRNAs) (Fig. 1). Accumulating evidence has revealed various biological functions of circRNAs, which have attracted widespread attention [3]. Localized in miRNA binding sites, circRNAs could directly sponge miRNAs through miRNA response elements (MREs), thereby negatively regulating the inhibition of target mRNAs [4]. CircRNAs also regulate gene expression and bind to RNA-binding proteins (RBPs), playing critical roles in gene transcription and translation [5, 6]. In addition, the translation potential of circRNAs as protein templates related to tumorigenesis and development has been proved [7]. Since circRNAs are abundant in human peripheral blood and tissues, making them easy to detect [8, 9]. CircRNAs have been illuminated to participate in various biological and physiological processes, containing cell growth, metastasis, stemness, tumor microenvironment, and immune evasion [10, 11], suggesting potential contributions to the pathogenesis of several human diseases.
Fig. 1.
The biogenesis and function of circRNAs. CircRNAs are classified into 4 types: ecircRNAs, ciRNAs, EIciRNAs, and tricRNAs. CircRNAs function as regulators of transcription and translation, which includes miRNA binding, protein binding, gene expression regulating, and acting as templates for translation
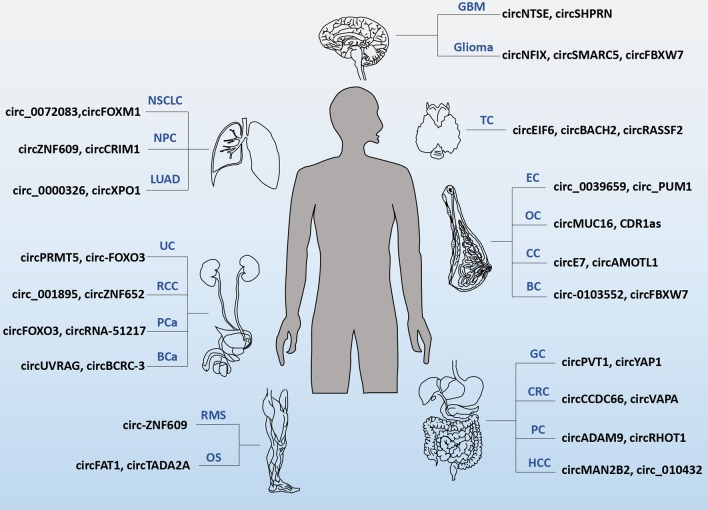
CircRNAs act as tumor suppressors or oncogenes to participate in the development of a variety of tumors and are becoming novel diagnostic and prognostic biomarkers [12]. The differential expression and function of circRNAs in a variety of cancers have been identified (Fig. 2) [13]. Recently, emerging evidence suggests that circRNAs play vital roles in the tumorigenesis and progression of hematological tumors [14, 15]. Moreover, circRNAs are affective in iron metabolism and N6-methyladenosine (m6A) modification [16, 17]. The artificial circRNAs molecules targeting miRNAs and nanoparticle-based delivery systems provide novel therapeutic prospects [18]. Given that emerging literature has summarized the expression patterns and classical functions of circRNAs in hematological malignancies, here, we focus on the current state of knowledge regarding the novel mechanisms and potential clinical applications of circRNAs among hematological tumors.
Fig. 2.
CircRNAs differentially expressed in cancers. GC: gastric cancer; CRC: colorectal cancer; PC: pancreatic cancer; HCC: hepatocellular carcinoma; BC: breast cancer; CC: cervical cancer; OC: ovarian cancer; EC: endometrial cancer; NSCLC: non-small cell lung cancer; LUAD: lung adenocarcinoma; NPC: nasopharyngeal carcinoma; BCa: bladder cancer; PCa: prostate cancer; RCC: renal cell carcinoma; UC: urothelial carcinoma; GBM: glioblastoma; TC: thyroid carcinoma; OS: osteosarcoma; RMS: rhabdomyosarcoma
Functions of circRNAs in hematological malignancies
Facilitating tumorigenesis of hematological malignancies
Through genome-wide studies of myeloid leukemia, aberrantly expressed circRNAs in acute myeloid leukemia (AML) and chronic myeloid leukemia (CML) were identified [19, 20]. A total of 569 differentially expression circRNAs (DECs) were screened by circRNA microarray in 6 bone marrow samples from pediatric AML patients, with 273 circRNAs upregulated and 296 downregulated. Functional investigation illustrated that circ-0004136 promoted the proliferation of AML cells by sponging miR-142 [21]. Moreover, circRNA-sequencing of bone marrow samples from AML patients identified the differentially expression of circ_0009910, which promoted the growth of AML cells by downregulating miR-20a-5p [19]. Han et al. found that circ_0001947 curbed cell proliferation by targeting the miR-329-5p/CREBRF axis in AML [22]. Circ_100290, highly expressed in AML, promoted proliferation and restrained apoptosis of AML cells by sponging miR-203 to regulate Rab10 expression [23].
In addition, recent studies have demonstrated that circRNAs could also modulate cell proliferation independent of their related linear RNAs [3]. Circ_0121582, a product of the reverse splicing of GSK3β exon 1 to exon 7, was confirmed to suppress the growth of AML cells [24]. Interestingly, different mechanisms were regulated by circ_0121582 in the cytoplasm and nucleus, respectively. Circ_0121582 formed a sponge with the miR-224/GSK3β axis in the cytoplasm, and bound to the promoter of GSK3β to recruit TET1 in the nucleus [24]. The occurrence of internal tandem duplication (ITD) mutations in the juxtamembrane domain of the FMS-like tyrosine kinase-3 (FLT3) gene (FLT3-ITD) is identified in up to 30% of AML patients, suggesting a significantly worse clinical outcome. Sun et al. reported that circMYBL2 promoted the proliferation of FLT3-ITD-positive AML cells by directly interacting with the RBP PTBP1 in vitro and in vivo [25]. Moreover, knocking down circMYBL2 decreased the phosphorylation of FLT3 kinase in ITD mutant cells, and further weakened the phosphorylation of STAT5, the downstream target of FLT3 critical for AML progression [25]. Another circRNA recently identified in FLT3-ITD-positive AML was circ_0000370, derived from the FLI-1 gene, which was associated with FLT3-ITD. Circ_0000370 facilitated the viability and suppressed apoptosis of FLT3-ITD-positive AML cells by modulation of miR-1299 and S100A7A [26].
In terms of lymphocytic leukemia, knockdown of circPVT1 accelerated the apoptosis of acute lymphocytic leukemia (ALL) cells by declining the expression of c-Myc and Bcl-2 [27]. Upregulation of circ-0000745 resulted in enhanced proliferation of ALL cells by activating ERK [28]. Transcriptomic sequencing of 21 de novo chronic lymphocytic leukemia (CLL) patients revealed differentially expression of 859 circRNAs distinguished CLL cells from normal B cells [29]. It was recently demonstrated that circ_0132266 participated in CLL tumorigenesis through interacting with miR-337-3p to modulate PML expression [30]. Xia and colleagues demonstrated that circ-CBFB contributed to CLL progression by modulation of the miR-607/FZD3/Wnt/β-catenin cascade [31].
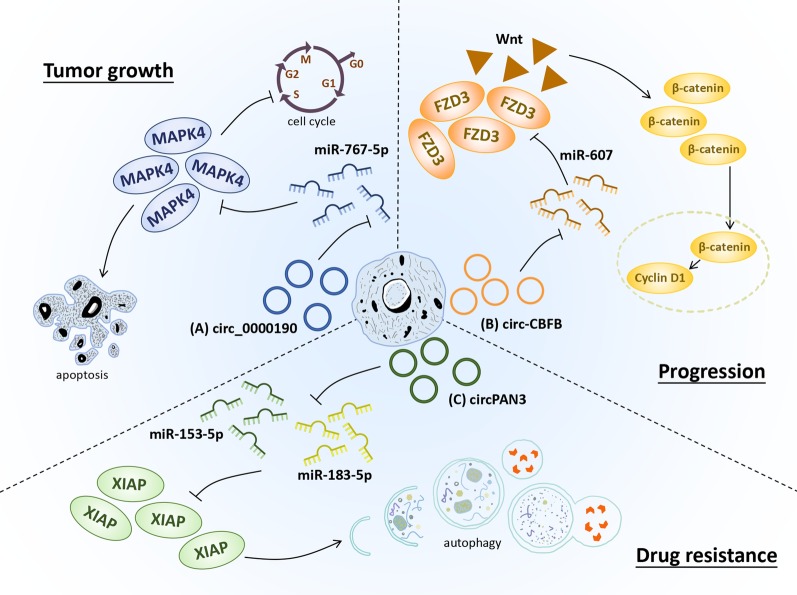
Currently, studies of circRNAs in lymphoma are relative rare, with only some subtypes reported. Ectopic expression of circ-LAMP1 was detected in T-cell lymphoblastic lymphoma (T-LBL) tissues, which promoted T-LBL progression by sponging miR-615-5p and activating DDR2 level [32]. Augmented expression of circ-APC inhibited the growth of diffuse large B-cell lymphoma (DLBCL) cells in vitro and in vivo by recruiting TET1 to the promoter of APC, subsequently resulted in the activation of canonical Wnt/β-catenin signaling pathway [33]. Remarkable overexpression of circ-CDYL was detected in the plasma of mantle cell lymphoma (MCL) and multiple myeloma (MM) patients [34, 35]. Knockdown of circCDYL could inhibit DNA synthesis rate and cell activities to stunt MM progression. Silencing circCDYL decreased the expression of YAP, the key effector of Hippo signaling, and upregulated miR-1180 in MM xenograft model [35, 36]. Circ_0000190, downregulated in the tissues and plasma of MM patients, restrained the proliferation of MM cells through modulating the miR-767-5p/MAPK4 axis [37]. The overexpressed circ_0000142 in MM targeted miR-610 to promote the level of AKT3 mRNA and enhance cell growth, migration and invasion [38]. Moreover, circ_0007841 directly interacted with miR-338-3p to accelerate MM progression [39]. All these results provide evidence that circRNAs mainly function as sponges of miRNAs and form circRNA/miRNA/mRNA axes to participate in the tumorigenesis of hematological cancers (Fig. 3). Nevertheless, further investigations are still needed to explore the detailed mechanism and potential clinical application.
Fig. 3.
CircRNA-miRNA-mRNA networks in hematological malignancies. Selected samples of circRNAs and their genomic targets are exhibited for tumor growth, progression and drug resistance. (A) Circ_0000190 was downregulated in MM and inhibited proliferation as well as induced apoptosis of MM cells through negatively regulating the suppression of miR-767-5p to MAPK4, which led to tumor growth. (B) Circ-CBFB, overexpressed in CLL, was identified as a sponge of miR-607 that targeted FZD3. Circ-CBFB promoted FZD3 expression, resulting in activation of the Wnt/β-catenin pathway and consequent progression of CLL. (C) CircPAN3 could inhibit both miR-153-5p and miR-183-5p, thereby upregulating the expression of XIAP. CircPAN3 was also responsible for AML drug resistance via regulating the level of autophagy-associated proteins
Participating in drug resistance
With the clinical application of novel anti-tumor drugs, the efficacy of hematological tumors has been remarkably improved. However, drug resistance is still a bottleneck that hinders better prognosis of patients. CircRNAs are proved to perform pivotal parts in chemoresistance by reducing drug concentration, activating downstream signaling pathways, and modulating DNA repair ability [40, 41]. Li et al. constructed a doxorubicin (ADM)-resistant cell line (HL-60/ADM) and screened differentially expressed ncRNAs using high-throughput sequencing, 1824 circRNAs included. Targets of DECs were enriched in ribonucleoside and purine ribonucleoside triphosphate catabolic process, intracellular, adenyl ribonucleotide binding, and several classical signaling pathways through Gene Ontology (GO) and Kyoto Encyclopedia of Genes and Genomes (KEGG) enrichment analyses, indicating that circRNAs may participate in drug resistance in AML via modulating multiple biological processes [42]. Moreover, circPAN3 was validated to mediate ADM-resistance of AML cells via targeting the miR-153-5p/miR-183-5p/XIAP axis as well as enhancing autophagy activity, and to promote the expression of apoptosis-marked proteins [14, 43]. Knockdown of circMYBL2 accelerated apoptosis and inhibited proliferation of AML cells resistant to quizartinib, a selective and efficient FLT3 inhibitor, indicating circMYBL2 inducing quizartinib resistance in AML [25].
The application of tyrosine kinase inhibitors (TKIs), represented by imatinib (IM), has doubled the 5-year overall survival (OS) of CML patients [44]. Nevertheless, TKI resistance is gradually being common in clinical practice. Several studies have demonstrated the participation of circRNAs in drug resistance of CML cells. Knocking down circ_0080145 in IM-resistant CML cell lines (K562/IM, KU812/IM) suppressed the glycolysis process and cell growth and induced apoptosis through circ_0080145/miR-326/PPFIA1 axis [15]. Besides, the expression of circBA9.3 was positively related to the BCR-ABL level among TKI-resistant CML patients. Mechanistically, circBA9.3 strengthened the antiapoptotic properties of K562 cells and upregulated the levels of both ABL1 and BCR-ABL1 proteins to reduce the sensitivity of leukemia cells to TKIs, thereby promoting resistance against TKI therapy [45]. Circ_100053 was overexpressed in IM-resistant CML patients and K562/IM cells and was associated with advanced clinical stages and the mutation status of BCR-ABL, indicating the contribution to IM resistance of CML, nevertheless, with the unclear mechanism [46]. As a miR-34a-5p sponge, circ_0009910 could promote cell proliferation, block apoptosis in K562/R cells, and activate ULK1-induced autophagy, leading to increased resistance of CML cells to IM [47].
As sponges of different miRNAs, circRNAs may participate in different mechanisms to induce drug resistance in the same disease. Circ_0007841 was involved in the bortezomib (BTZ) tolerance [48] and ADM-resistance in MM cells, and induced chemoresistance by activating ABCG2 [49]. Taken together, circRNAs mediate chemoresistance by regulating signaling transduction pathways or forming ceRNA regulatory networks, and may act as novel therapeutic targets to improve the efficacy of refractory/relapsed patients.
Regulation of tumor metabolism
Represented by glycolysis, fatty acid oxidation, and amino acid metabolism, metabolic reprogramming is a typical hallmark in cancer cells [50]. Tumor cells are featured by the strong dependence on glycolysis to provide energy despite sufficient oxygen availability [51]. Targeting glycolysis has been revealed to be a promising therapeutic strategy for hematological malignancies [52]. Hexokinase-2 (HK2) and glucose transporters (GLUT) act as critical modulators of glycolysis progress [53]. A recent study confirmed that silencing circ_0080145 suppressed the glucose consumption, lactic acid content, and the HK2 levels in IM-resistant CML cell lines, indicating the regulatory effect of circ_0080145 on glycolysis in IM-resistance [15]. Aberrant high expression of circ_100290 upregulated GLUT1 by targeting miR-378a to promote the glycolysis in oral squamous cell carcinoma (OSCC) cells [54]. Circ_100290 was also overexpressed in AML, co-expressed with Rab10 [23]. As a target of miR-432-5p, Rab10 participated in the decreased glycolysis induced by miR-432-5p in glioma [55]. Knockdown of circ-PVT1 reduced the glycolytic metabolism of OSCC cells by targeting the miR-106a-5p/HK2 axis [56]. Although circ-PVT1 has been found to be involved in the occurrence of ALL, its regulation on the glucose metabolism of hematological malignancies has not yet been reported. In addition, further investigations on the specific function of circRNAs and glycolysis in hematological tumors are warranted.
Increased de novo synthesis of fatty acids and fat accumulation present in diverse tumors are responsible for tumor development [57]. The content of lipoproteins is tightly connected with the phenotypic and clinical characteristics of hematological malignancies [58]. Recent studies have clarified that circRNAs maintained the global adipocyte transcriptional program of lipid biosynthesis and metabolism [59]. Moreover, circFASN enhanced the promotion of tacrolimus on triglyceride accumulation [60]. Nevertheless, the mechanism of circRNAs in lipid metabolism of malignancies is still unclear, which is expected to become a novel field in the study of circRNAs in hematological tumors.
Novel functions of circRNAs
Inducing autophagy
Autophagy is a primary intracellular degradation process regulating tumorigenesis and associated with the sensitivity of tumor cells to chemotherapeutic drugs [61]. Emerging discoveries indicated that circRNAs played significant roles in tumor autophagy [62]. Enhanced autophagic activity was found in ADM-resistant AML cell lines, THP1/ADM and K562/ADM. Silencing circPAN3 reduced the levels of autophagy markers, including the LC3-II/LC3I ratio and Beclin-1. The targeted miRNAs of circPAN3, analyzed by target prediction database, were related to AMPK signaling pathway and downregulated in THP-1 cells with circPAN3 overexpression. Taken together, circPAN3 may activate MAPK pathway to enhance autophagy to induce chemo-resistance in AML [14].
Silencing circ_0009910 resulted in downregulation of ULK1, an autophagy promoter overexpressed in IM-resistant K562 cells. It was further confirmed that circ_0009910 could activate ULK1-induced autophagy via sponging miR-34a-5p, thereby promoting the IM resistance of CML cells [47]. CircCDYL was demonstrated to enhance the autophagic level in breast cancer through miR-1275/ATG7/ULK1 axis [63]. It is worth noting that upregulated levels of circCDYL were also detected in MCL and MM and might serve as potential biomarkers for diagnosis [34, 35]. However, the involvement of circCDYL in the autophagy of hematological malignancies still needs further investigation. Although investigations on circRNAs in tumor autophagy are still in infancy, it will bring new opportunities for future diagnosis and treatment of hematological malignancies.
Regulating pyroptosis
Pyroptosis is an inflammasome-activated programmed cell death pathway, characterized by the immediate formation of pores in cell membrane and increased permeability [64]. Induction of pyroptosis represents a novel potential therapeutic strategy for hematological malignancies [65]. The latest studies have illuminated the regulation of circRNAs on pyroptosis in human diseases. CircACTR2, upregulated in high-glucose-treated HK-2 cells, was proved to increase pyroptosis by evaluating propidium iodide (PI) uptake and lactate dehydrogenase (LDH) level [66]. Besides, circ_0076631, overexpressed in glucose-stressed cardiomyocytes and serum of diabetic patients, was validated to activate pyroptosis via circ_0076631/miR-214-3p/caspase-1 axis in diabetic cardiomyopathy [67]. High-throughput sequencing analysis showed the high expression of miR-214-3p in primary cutaneous follicle center lymphoma (PCFCL), suggesting the potential of circRNA/miRNA axis in pyroptosis of lymphoma [68]. The participation of circHIPK3 in pyroptosis was recently reported. CircHIPK3 could downregulate miR-421, leading to the increased FOXO3a expression, thereby inhibiting pyroptosis and releasing IL-1β and IL-18 [69]. Previous studies have found that the high expression of circHIPK3 in CML was significantly associated with poor prognosis [70]. Besides, AKT/FOXO3a pathway was involved in the apoptosis of AML [71]. Genetic polymorphisms of IL-18 and IL-1β were confirmed related to the prognosis of AML [72]. However, whether circHIPK3 could influence the pyroptosis level in leukemia remains further investigations. Overall, the regulation of circRNAs on pyroptosis is a hopeful therapeutic target, but its role in hematological malignancies is yet to be fully understood.
Function of circRNAs in ferroptosis
Different from autophagy and apoptosis, ferroptosis is an iron- and reactive oxygen species (ROS)-dependent form of programmed cell death activated by iron oxidation [73, 74]. Accumulating studies have reported the regulatory mechanisms of ncRNAs in ferroptosis of tumors, but few of them focused on circRNAs [75]. Xu et al. reported that circIL4R accelerated tumorigenesis and refrained ferroptosis by regulating the miR-541-3p/GPX4 axis in HCC [76]. Circ-TTBK2 knockdown delayed proliferation and invasion, as well as promoted ferroptosis of glioma cells by regulating the miR-761/ITGB8 axis [77]. GPX4, a key regulator of ferroptosis, was overexpressed in primary MM cells [78]. However, both the circRNA/miRNA/GPX4 axis and its function in ferroptosis in MM have not been revealed. Although the relationship between circRNAs and ferroptosis in hematological malignancies has not been reported before, emerging evidence suggests that the changes in iron metabolism are central characters of leukemia [79]. Typhaneoside (TYP) was proved to prevent AML progression through triggering autophagy and ferroptosis. Therefore, targeting iron metabolism, such as ferroptosis, is likely to provide promising therapeutic options for individualized treatment of leukemia.
circRNAs and m6A modification
m6A methylation has emerged recently as the novel mechanism of RNA modification, which executes important functions in malignant hematopoiesis, including AML [80]. The interplay between m6A modification and circRNAs provides novel insights into the therapeutic strategy of malignancies [81, 82]. Zhou et al. demonstrated that the written and read complexes of m6A modification in circRNAs were the same as those of mRNAs, but the modification patterns were distinct [83]. A growing body of evidence indicates that m6A modification could modulate the production and function of circRNAs. The m6A circRNAs expressed in a cell-type-specific pattern, indicating that m6A modification of circRNAs may exert different biological functions in different cell types [83, 84].
m6A modification of circRNA inhibits innate immunity by blocking RIG-I activation. Moreover, the m6A reader YTHDF2 could bind to m6A-circRNA, thereby suppressing the innate immunity [17]. Chen et al. identified that circNSUN2 could form a circNSUN2/IGF2BP2/HMGA2 RNA-protein ternary complex to enhance the stability of HMGA2 mRNA in colorectal carcinoma [85]. Microarray analysis of DECs in poorly differentiated gastric adenocarcinoma revealed that most DECs had m6A modification, and the trend of m6A modification changes was consistent with the expression level of circRNAs [86]. Circ_0001105 suppressed the progression of osteosarcoma through sponging miR-766 to enhance the expression of YTHDF2 [87]. Interestingly, the inhibition of YTHDF2 selectively targeted leukemic stem cells (LSCs) in AML, indicating the potential functions of circRNA regulated YTHDF2 in the progression of AML [88]. In addition, circ_KIAA1429 could promote the progression of HCC by regulating the m6A-YTHDF3-Zeb1 [89]. It was confirmed that SNHG14/miR-5590-3p/Zeb1 axis enhanced the progression and immune evasion through regulating PD-1/PD-L1 checkpoint in DLBCL, which provide an innovative perspective for circRNA mediated immunotherapy of lymphoma [90]. Nevertheless, the m6A modification of circRNAs in hematological malignancies has rarely been reported yet. Further studies on how m6A modification modulates the production and function of circRNAs in hematological malignancies will improve our understating of the biological function of circRNAs.
Function of fusion circRNAs
Gene fusion is a central class of somatic mutational events in hematological malignancies through chromosomal rearrangements triggered by DNA double-strand breaks. As high-risk factors of AML, cytogenetic abnormalities are featured by fusion proteins, including AML1-ETO, PML-RARα, and MLL/AF9, originated from chromosomal translocations, which have been acknowledged as specific biomarkers for prognosis [91]. Additionally, translocations produce not only fusion mRNAs but also fusion circRNAs (f-circRNAs) [92]. Despite the lack of specific mechanisms, f-circRNAs are oncogenic in in vitro and in vivo models [93]. Human mixed lineage leukemia (MLL) gene is involved in chromosome translocations with a multitude of partners, such as AF9 (MLLT3) [94]. Several f-circRNAs have been identified from MLL fusion genes, including MLL-AF9, MLL-AF4, and MLL-ENL [95]. The MLL-AF9 fusion gene is predominantly expressed in AML. Sanger sequencing revealed the existence of f-circM9_1 and f-circM9_2 in THP1 cells. F-circM9 overexpression suppressed apoptosis induced by cytarabine (Ara-C) and arsenic trioxide (ATO) in K562 cells. Moreover, the spleens of mice transplanted with f-circM9 overexpressed leukemia cells were relatively bigger with more leukemia cells, and decreased apoptosis in bone marrow when treated with Ara-C [93]. AF4 is another partner of MLL fusion genes. Four circRNAs were detected from AF4 gene, including circAF4 (EX3-4), circAF4 (EX3-5), circAF4 (EX5-6), and circAF4 (EX12). CircAF4 was upregulated in leukemia patients and cells with MLL-AF4 translocation. CircAF4 enhanced proliferation and blocked apoptosis through circAF4/miR-128-3p/MLL-AF4 axis. Knockdown of circAF4 extended survival times of mice [96].
Potential clinical application of circRNAs
Promising biomarkers for diagnosis and prognosis
CircRNAs are widely and conservatively expressed in hematopoietic cells [97]. As a result of their abundancy and accessibility, circRNAs are expected to be ideal biomarkers in the diagnosis and prognosis of hematological malignancies. Among all the circRNAs, PVT1 has been considered to participate in the pathogenesis of hematological malignancies [98, 99]. CircPVT1 showed increased expression in ALL, pediatric B-precursor ALL and AML cases harboring MYC amplifications in the form of dmin, hsr, or ring chromosomes (AML-Amp) [27, 100, 101]. Silencing circPVT1 was validated to inhibit cell proliferation and induce apoptosis in ALL [27]. Additionally, circPVT1 was overexpressed in AML-Amp cases leading to the identification between various karyotypes of AML [101].
Due to the high heterogeneity of hematological malignancies and the cell-type specificity of circRNAs, there are specific expressions of circRNA in different types of hematological diseases (Table 1). At present, a variety of circRNAs have performed promising function for evaluating prognostic model, such as circ_0003602, circ_0005571, circ_0074371, circ_0007609, circ_0012152, hsa_circ_0001857 and circ_0001247 [102, 103]. Circ-Foxo3, Circ-RPS6KB1, circ-CSMD2, circ-ANXA2, circ-PWP2, circ-RBM5, circ-ZZEF1, circ-GSK3B and circ-FOXP1 could potentially identify AML patients from healthy groups [104, 105]. Among them, circ-ANXA2 overexpression was related to shorter event-free survival (EFS) and OS of AML patients. Meanwhile, AML patients achieved complete remission (CR) presented lower level of circ-ANAX2 than those did not reach CR, accompanied by longer EFS and OS [105]. Receiver operating characteristic (ROC) curve analysis revealed that the expression of circ-VIM could distinguish AML patients from healthy groups. Highly expressed circ-VIM acted as an independent prognostic factor for OS and leukemia-free survival (LFS) in AML [106]. Interestingly, the expression level of the same circRNA differs in subtypes of the same disease, highlighting the specificity of circRNAs as biomarkers. Circ_0075001 was overexpressed in M0 or M1 subtype of AML patients and significantly downregulated in M2, M4 and M5 subgroups, showing the potential to distinguish the differentiation degree of the AML [107].
Table 1.
Circular RNAs implicated in hematological malignancies
| Disease | CircRNA | Expression | Phenotype | Clinical significance | Possible target/mechanism | Ref. |
|---|---|---|---|---|---|---|
| AML | circRNA-DLEU2 | Up | proliferation ( +), apoptosis (−), tumor formation ( +) | / | miR-496/PRKACB | [125] |
| circ_100290 | Up | proliferation ( +), apoptosis (−) | / | miR-203/Rab10 | [23] | |
| circPAN3 | Up | autophagy ( +), apoptosis (−), ADM-resistance ( +) | / | miR-153-5p/miR-183-5p/XIAP | [14, 43] | |
| circ-ANXA2 | Up | proliferation ( +), apoptosis (−) | high disease risk, poor risk stratification, low CR level, short EFS and OS | miR-23a-5p/miR-503-3p | [105] | |
| circ_0009910 | Up | proliferation ( +), apoptosis (−) | poor risk, short OS | miR-20a-5p | [19] | |
| circ_0000370 | Up | proliferation ( +), apoptosis (−), cell cycle ( +) | FLT3-ITD + | miR-1299/S100A7A | [26] | |
| circMYBL2 | Up | proliferation ( +), quizartinib resistance ( +) | FLT3-ITD + | PTBP1, FLT3 kinase translational ( +) | [25] | |
| circ-VIM | Up | / | distribution of WBC count, FAB subtypes, short OS and LFS | / | [106] | |
| circ-0004136 | Up | proliferation ( +) | / | miR-142 | [21] | |
| circ-HIPK2 | Down | differentiation ( +) | ATRA-induced differentiation | miR-124-3p | [111] | |
| circ_0001947 | Down | proliferation (−), apoptosis ( +) | white blood cell, hemoglobin, diagnosis, prognosis | miR-329-5p/CREBRF | [22] | |
| circ_0121582 | Down | proliferation (−) | / | miR-224/GSK3β, TET1/GSK3β/Wnt/β-catenin | [24] | |
| CML | circ_0080145 | Up | proliferation ( +) | / | sponge miR-29b | [20] |
| circ_0009910 | Up | proliferation ( +), autophagy ( +), apoptosis (−) | imatinib resistance, short OS | miR-34a-5p/UKL1 | [47] | |
| circBA9.3 | Up | proliferation ( +), apoptosis (−) | TKI-resistance | c-ABL1 & BCR-ABL1 level ( +) | [45] | |
| circ_100053 | Up | / | clinical stage, BCR/ABL mutant status, short OS, imatinib resistance | / | [46] | |
| circ_0080145 | Up | proliferation ( +), glycolysis ( +), apoptosis (−) | IM-resistance | miR-326/PPFIA1 | [15] | |
| ALL | circPVT1 | Up | proliferation ( +), apoptosis (−) | / | c-Myc & Bcl-2 expression ( +) | [27] |
| circAF4 | Up | apoptosis (−), leukemogenesis ( +) | risk stratification | miR-128-3p/MLL-AF4 | [96] | |
| CLL | circ-CBFB | Up | progression ( +), apoptosis (−) | diagnosis, low survival time, independent predictor of prognosis | miR-607/FZD3/Wnt/β-catenin pathway | [31] |
| circ-RPL15 | Up | proliferation ( +) | IGHV mutation status | miR-146b-3p/RAS/RAF1/MEK/ERK pathway | [108] | |
| circ_0132266 | Down | proliferation (−), apoptosis ( +) | / | miR-337-3p/PML | [30] | |
| DLBCL | circ-APC | Down | proliferation (−), cell cycle (−) | Ann Arbor stage, CHOP-like and rituximab resistance, short OS, independent prognostic factor | miR-888/APC, TET1/APC, inactivate Wnt/β-catenin pathway | [33] |
| MCL | circCDYL | Up | proliferation ( +) | diagnosis | [34] | |
| T-LBL | circ-LAMP1 | Up | proliferation ( +), apoptosis (−) | / | miR-615-5p/DDR2 | [32] |
| MM | circ_0007841 | Up | proliferation ( +) | clinical type, cytogenetic mutation, bone destruction, R-ISS staging, DOX resistance | ABCG2 level ( +) | [49] |
| circCDYL | Up | DNA synthesis ( +), apoptosis (-) | ISS and DS stage, diagnosis, short OS | miR-1180/YAP | [35] | |
| circ_0000190 | Down | proliferation (−), apoptosis ( +), tumor growth (−) | ISS and DS stage, high risk, short PFS, OS | miR-767-5p/MAPK pathway | [37] | |
| circ-SMARCA5 | Down | proliferation (−), apoptosis ( +) | β2-MG level, ISS stage, short PFS and OS | miR-767-5p | [126] |
Note: (+) means promotion and (−) means suppression
The high expression of circHIPK3 in serum of CML patients was related to Sokal relative risk, an independent factor of CML prognosis, and shorter OS, indicating poor clinical outcome [70]. The level of circ-RPL15 was negatively correlated to the mutation state of immunoglobulin heavy chain (IGHV) gene, predicting poorer OS [108]. In DLBCL, downregulating plasma circ-APC presented diagnostic potential and was related to advanced Ann Arbor stage, low International Prognostic Index, rituximab resistance, and shorter OS [33]. The high expression of circRNA_101237 was associated with shorter OS and PFS in MM patients [109]. What is more, the expression of circRNAs in several diseases exhibited temporal specificity, which indicated that circRNAs were likely to predict clinical outcome [110]. A total of 508 circRNAs expressed dynamically throughout the treatment of all-trans retinoic acid (ATRA) in NB4 cells, and independently from the parent genes [111]. The low expression state of circ_0004277 in AML patients was diminished after chemotherapy, while the level of circ_0004277 decreased again when patients relapsed after CR, demonstrating the relationship between the increasing expression and good curative effect [112]. As consequence, the expression of circRNAs is dynamic during disease progression, which provides new aspects for therapeutic efficacy and prognosis evaluation.
The existing modalities of disease diagnosis and efficacy evaluation are invasive. Liquid biopsy, being non-invasive and repeatable, is becoming a new diagnostic tool. Accumulating evidence discovers the enrichment of circRNAs in exosomes. Exosomes protect inner circRNAs from influences of extracellular substances, making it more possible for detecting the existence of exosomal circRNAs [113]. Exosomal circRNAs act a significant part mainly in proliferation and tumor metastasis [114]. Mc-COX2, a mitochondrial genome-derived circRNA, was significantly enriched in exosomes of plasma from CLL patients, and was positively correlated with worse OS [115]. Associated with deletion 17p, t (4; 14), Durie-Salmon staging and international staging system, the level of exosomal circMYC was higher in bortezomib-resistant patients than non-resistant groups [116]. Additionally, the exosomal circ_0007841 was validated to enhance proliferation and metastasis and suppress apoptosis via activating PI3K/AKT pathway in MM cell lines [39]. Although a large number of circRNAs with biomarker value have been discovered by high-throughput sequencing, the targets and mechanisms are still unclear. The constantly emerging circRNA databases provide great convenience for target prediction and expression visualization. Here, we summarize 10 representative circRNA databases (Table 2).
Table 2.
CircRNA databases
| Name | Website address | Description | Ref. |
|---|---|---|---|
| circBase | https://circbase.org/ | A public dataset of thousands of circRNAs in eukaryotic cells | [127] |
| circInteractome | https://circinteractome.nia.nih.gov/ | A computational tool enabling the prediction and mapping of binding sites for RBPs and miRNAs on reported circRNAs | [128] |
| CIRCpedia V2 | https://www.picb.ac.cn/rnomics/circpedia/ | An updated comprehensive database containing circRNA annotations from over 180 RNA-seq datasets across six different species | [129] |
| circRNADb | https://reprod.njmu.edu.cn/cgi-bin/circrnadb/circRNADb.php | A comprehensive database of circular RNA molecules in humans | [130] |
| CSCD | https://gb.whu.edu.cn/CSCD | An integrated interactional database of cancer-specific circRNAs | [131] |
| exoRBase | https://www.exoRBase.org | A repository of circRNA, lncRNA and mRNA derived from RNA-seq data analyses of human blood exosomes | [132] |
| MiOncoCirc | https://mioncocirc.github.io/ | A compendium of circular RNAs compiled from cancer clinical samples | [133] |
| CircAtlas 2.0 | https://circatlas.biols.ac.cn/ | A database of over one million of circRNAs across 6 species (human, macaca, mouse, rat, pig, chicken) and tissues | [134] |
| CircBank | https://www.circbank.cn/index.html | A comprehensive database of human circRNA including more than 140,000 human annotated circRNA from different source | [135] |
| NoncoRNA | https://www.ncdtcdb.cn:8080/NoncoRNA/ | A database for experimentally supported ncRNA and drug target associations in cancer | [136] |
circRNA-related therapeutic strategies
The circRNA-miRNA-mRNA axis has become a vital mechanism in hematological tumorigenesis. As circRNAs contain multiple miRNA binding sites, targeted inhibition of circRNAs exerts more therapeutic advantages and potential than targeted inhibition of single miRNA/gene. RNA interference (RNAi) is one of the most common methods to determine the function of circRNA through loss-of-function approach. Transcripts of circRNAs could be packaged into viral vectors or oligonucleotide and then delivered to target cells to mediate their therapeutic effects [96]. Inhibiting the expression of specific circRNA could enhance the protective function of the relevant miRNAs in inhibiting oncogenes, such as XIAP, β-catenin, GSK3β and YAP [24, 31, 35, 43]. Recently, the CRISPR/Cas9-mediated genetic engineering technology provides a robust tool for circRNAs investigation. The CRISPR/Cas-assisted homologous recombination method can replace circRNA gene with a marker gene, thereby consuming circRNAs without affecting the existing gene [117]. Future investigations fueled by the well-defined guide RNA (gRNA) libraries designed for circRNA will promote the targeted therapy based on circRNA screening.
At present, a practical artificial circRNA sponge could be synthesized using simple enzymatic ligation approach. The artificial circRNA molecule is applied as an exogenous miRNA inhibitor to effectively bind and block mature miRNA, providing a promising strategy for cancer therapy [18]. Jost et al. engineered the artificial circRNA sponges into customized miRNA to isolate miR-122 from hepatitis C virus (HCV). In addition, circRNAs can also be used as protein sponges, and the binding sites obtained from SELEX or CLIP data can be used for many RBPs [118]. The anti-HCV circular miRNA-122 RNA sponge can be used in combination with the sequence of host factors necessary to isolate the propagation of HCV, such as hnRNP L and HuR [118]. Therefore, the artificial circRNA sponge is a promising tool in circRNA-based anti-tumor therapy, which has potential value in clinical application.
In addition, emerging evidence indicated the potential therapeutic value of tumor-related functional peptides encoded by circRNAs, especially cancer-inhibiting peptides/proteins, such as β-catenin-370aa encoded by circβ-catenin, circPPP1R12A-73aa by circPPP1R12A, and AKT3-174aa by circ-AKT3 [119]. These functional peptides can play important roles in tumorigenesis, which made them potential novel targets for drug development [119]. Due to the potential development value and clinical utility of functional peptides encoded by circRNAs, the functional peptides may be used in the research and treatment of hematological malignancies in the future.
Both the artificial circRNA and functional peptides need to be transported to the cell through an appropriate delivery system. Nanoparticles could be used to treat tumor in a variety of ways, such as intravenous injection and tail vein injection, and have become promising tools for cancer treatment. Recently, Wang et al. established a new plasmid delivery system, Micropoly-transfecter, which can deliver circ-1073 plasmid through intratumoral injection, thereby inhibiting tumor progression [120]. Moreover, accumulating evidence has indicated the potential value of exosomal circRNAs in clinical application [121]. Exosomes could carry circ-0051443 from normal cells to HCC cells, and inhibit the malignant biological behaviors through inducing apoptosis and cell cycle arrest [122].
CircRNAs play vital roles in the tumor microenvironment (TME) by regulating the immune surveillance and remodeling the extracellular matrix [9, 123]. CircRNA-002178 was indicated to promote the expression of PD-L1 in tumor cells through the ceRNA mechanism. Meanwhile, circRNA-002178 in tumor cells was delivered from exosomes to CD8 + T cells to achieve immune evasion of tumor cells by promoting PD-1 expression [124]. The regulation of PDL-1/PD-1 pathway by circRNA-002178 may also provide a new direction for the development of tumor-targeted drugs. Currently, the circRNA-based targeted therapy in hematological malignancies is still in its infancy. Therefore, regulation of PD-1/PD-L1 by targeting relevant circRNA may be a promising direction of future immune therapy.
Conclusion and future perspectives
Emerging studies have revealed that the expression of circRNAs is strongly associated with tumorigenesis and prognosis of hematological malignancies. However, most of them were limited in the abnormal expression and ceRNA functions, rarely in clinical significance. Due to the convenience of circRNAs detection form peripheral blood, circRNAs may act as ideal biomarkers with the potential of clinical application. The expression of circRNAs is dynamic throughout the whole process of chemotherapy, suggesting that detecting the level of circRNAs may reflect the disease status in real time, so as to estimate the therapeutic efficacy in time. Nevertheless, such biomarkers are not specific enough for clinical appliance, which could constitute one of the focuses for future study. Current studies have confirmed that circRNAs regulate cell activity and tumor growth mainly by sponging to miRNAs and RBPs. The development of bioinformatics technology has greatly promoted the investigation of circRNA-miRNA axis. However, the specific content and mechanism of ceRNA network in hematological malignancies are still unclear. There remain a large number of circRNAs with unknown functions, and the involved mechanism is yet to be validated. Whether circRNAs participate in hematological cancers through other manners such as encoding peptides needs further investigation.
In this review, we not only summarize the contributions of circRNAs to the pathogenesis, diagnosis, chemo-resistance, and prognosis of hematological malignancies, but also put up novel biological functions and perspectives for the future clinical significances of circRNAs as therapeutic targets as well as novel treatment strategies. CircRNAs have great potential in targeted therapy due to its known regulatory functions, and the stability of circRNAs may be conducive to identify hematological malignancies by body fluids. Nevertheless, the mechanism involved in the interaction between circRNAs and hematological tumors is not fully understood yet. What’s more, although it is confirmed that circRNAs can act as potential diagnosis and prognosis biomarkers, most of the available circRNA-biomarkers are still not specific and sensitive enough to apply in clinical practice. Further studies on large-cohort prospective clinical trials will verify and promote the clinical application of circRNA biomarker candidates. Irrespective of these defects, circRNAs may still be utilized for targeted therapy in the future.
Acknowledgements
Not applicable.
Abbreviations
- circRNA
Circular RNA
- ceRNA
Competing endogenous RNA
- ncRNA
Non-coding RNA
- ecRNA
Exon circRNA
- ciRNA
Circular intron RNA
- EIciRNA
Exon-intron circRNA
- tricRNA
TRNA intronic circular RNA
- MRE
MiRNA response element
- RBP
RNA-binding protein
- m6A
N6-methyladenosine
- AML
Acute myeloid leukemia
- CML
Chronic myeloid leukemia
- DEC
Differentially expression circRNA
- ITD
Internal tandem duplication
- FLT3
FMS-like tyrosine kinase-3
- ALL
Acute lymphocytic leukemia
- CLL
Chronic lymphocytic leukemia
- T-LBL
T-cell lymphoblastic lymphoma
- DLBCL
Diffuse large B-cell lymphoma
- MCL
Mantle cell lymphoma
- MM
Multiple myeloma
- ADM
Doxorubicin
- GO
Gene ontology
- KEGG
Kyoto Encyclopedia of Genes and Genomes
- TKI
Tyrosine kinase inhibitor
- IM
Imatinib
- OS
Overall survival
- BTZ
Bortezomib
- HK2
Hexokinase-2
- GLUT
Glucose transporters
- OSCC
Oral squamous cell carcinoma
- PI
Propidium iodide
- LDH
Lactate dehydrogenase
- PCFCL
Primary cutaneous follicle center lymphoma
- ROS
Reactive oxygen species
- TYP
Typhaneoside
- LSC
Leukemic stem cell
- f-circRNA
Fusion circRNA
- MLL
Mixed lineage leukemia
- Ara-C
Cytarabine
- ATO
Arsenic trioxide
- AML-Amp
AML cases harboring MYC amplifications in the form of dmin, hsr, or ring chromosomes
- EFS
Event-free survival
- CR
Complete remission
- ROC
Receiver operating characteristic
- LFS
Leukemia-free survival
- IGHV
Immunoglobulin heavy chain
- NHL
Non-Hodgkin lymphoma
- ATRA
All-trans retinoic acid
- RNAi
RNA interference
- gRNA
Guide RNA
- HCV
Hepatitis C virus
- TME
Tumor microenvironment
Authors’ contributions
X.Z. and L.Z. wrote and edited this manuscript and created figures and tables. X.Z., X.W. and K.H. reviewed and revised the manuscript. X.W. provided direction and guidance throughout the preparation of the manuscript. All authors read and approved the final manuscript.
Funding
This work was supported by National Natural Science Foundation of China (No. 81800194, No.81770210, and No.81473486); Translational Research Grant of National Clinical Research Center for Hematologic Diseases (NCRCH) (No.2020ZKMB01); Key Research and Development Program of Shandong Province (No.2018CXGC1213); Technology Development Projects of Shandong Province (No.2017GSF18189); Shandong Provincial Natural Science Foundation (No.ZR2018BH011); China Postdoctoral Science Foundation (No.2020M672103); Development Project of Youth Innovation Teams in Colleges and Universities of Shandong Province (No.2020KJL006); Technology Development Project of Jinan City (No.201805065); Taishan Scholars Program of Shandong Province; Academic promotion programme of Shandong First Medical University; Key Laboratory for Kidney Regeneration of Shandong Province; Shandong Provincial Engineering Research Center of Lymphoma.
Availability of data and materials
Not applicable.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Xiangxiang Zhou and Linquan Zhan have contributed equally to this work
Contributor Information
Xiangxiang Zhou, Email: zhouxiangxiang90@163.com.
Xin Wang, Email: xinw007@126.com.
References
- 1.Jeck WR, Sorrentino JA, Wang K, Slevin MK, Burd CE, Liu J, Marzluff WF, Sharpless NE. Circular RNAs are abundant, conserved, and associated with ALU repeats. RNA. 2013;19:141–157. doi: 10.1261/rna.035667.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhang Q, Wang W, Zhou Q, Chen C, Yuan W, Liu J, Li X, Sun Z. Roles of circRNAs in the tumour microenvironment. Mol Cancer. 2020;19:14. doi: 10.1186/s12943-019-1125-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chen LL. The expanding regulatory mechanisms and cellular functions of circular RNAs. Nat Rev Mol Cell Biol. 2020;21:475–490. doi: 10.1038/s41580-020-0243-y. [DOI] [PubMed] [Google Scholar]
- 4.Shen T, Han M, Wei G, Ni T. An intriguing RNA species–perspectives of circularized RNA. Protein Cell. 2015;6:871–880. doi: 10.1007/s13238-015-0202-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yang ZG, Awan FM, Du WW, Zeng Y, Lyu J, Wu D, Gupta S, Yang W, Yang BB. The circular RNA interacts with STAT3, increasing its nuclear translocation and wound repair by modulating Dnmt3a and miR-17 function. Mol Ther. 2017;25:2062–2074. doi: 10.1016/j.ymthe.2017.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Du WW, Yang W, Chen Y, Wu ZK, Foster FS, Yang Z, Li X, Yang BB. Foxo3 circular RNA promotes cardiac senescence by modulating multiple factors associated with stress and senescence responses. Eur Heart J. 2017;38:1402–1412. doi: 10.1093/eurheartj/ehx501.P440. [DOI] [PubMed] [Google Scholar]
- 7.Zheng X, Chen L, Zhou Y, Wang Q, Zheng Z, Xu B, Wu C, Zhou Q, Hu W, Wu C, Jiang J. A novel protein encoded by a circular RNA circPPP1R12A promotes tumor pathogenesis and metastasis of colon cancer via Hippo-YAP signaling. Mol Cancer. 2019;18:47. doi: 10.1186/s12943-019-1010-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Koh W, Pan W, Gawad C, Fan HC, Kerchner GA, Wyss-Coray T, Blumenfeld YJ, El-Sayed YY, Quake SR. Noninvasive in vivo monitoring of tissue-specific global gene expression in humans. Proc Natl Acad Sci USA. 2014;111:7361–7366. doi: 10.1073/pnas.1405528111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Li Z, Cheng Y, Wu F, Wu L, Cao H, Wang Q, Tang W. The emerging landscape of circular RNAs in immunity: breakthroughs and challenges. Biomark Res. 2020;8:25. doi: 10.1186/s40364-020-00204-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yang H, Zhang H, Yang Y, Wang X, Deng T, Liu R, Ning T, Bai M, Li H, Zhu K, et al. Hypoxia induced exosomal circRNA promotes metastasis of Colorectal Cancer via targeting GEF-H1/RhoA axis. Theranostics. 2020;10:8211–8226. doi: 10.7150/thno.44419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hong W, Xue M, Jiang J, Zhang Y, Gao X. Circular RNA circ-CPA4/ let-7 miRNA/PD-L1 axis regulates cell growth, stemness, drug resistance and immune evasion in non-small cell lung cancer (NSCLC) J Exp Clin Cancer Res. 2020;39:149. doi: 10.1186/s13046-020-01648-1. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 12.Chen B, Huang S. Circular RNA: an emerging non-coding RNA as a regulator and biomarker in cancer. Cancer Lett. 2018;418:41–50. doi: 10.1016/j.canlet.2018.01.011. [DOI] [PubMed] [Google Scholar]
- 13.Chen Y, Li C, Tan C, Liu X. Circular RNAs: a new frontier in the study of human diseases. J Med Genet. 2016;53:359–365. doi: 10.1136/jmedgenet-2016-103758. [DOI] [PubMed] [Google Scholar]
- 14.Shang J, Chen WM, Liu S, Wang ZH, Wei TN, Chen ZZ, Wu WB. CircPAN3 contributes to drug resistance in acute myeloid leukemia through regulation of autophagy. Leuk Res. 2019;85:106198. doi: 10.1016/j.leukres.2019.106198. [DOI] [PubMed] [Google Scholar]
- 15.Che H, Ding H, Jia X. circ_0080145 Enhances imatinib resistance of chronic myeloid leukemia by regulating miR-326/PPFIA1 axis. Cancer Biother Radiopharm 2020. [DOI] [PubMed]
- 16.Liu Z, Wang Q, Wang X, Xu Z, Wei X, Li J. Circular RNA cIARS regulates ferroptosis in HCC cells through interacting with RNA binding protein ALKBH5. Cell Death Discov. 2020;6:72. doi: 10.1038/s41420-020-00306-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chen YG, Chen R, Ahmad S, Verma R, Kasturi SP, Amaya L, Broughton JP, Kim J, Cadena C, Pulendran B, et al. N6-methyladenosine modification controls circular RNA immunity. Mol Cell. 2019;76:96–109. doi: 10.1016/j.molcel.2019.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Liu X, Abraham JM, Cheng Y, Wang Z, Wang Z, Zhang G, Ashktorab H, Smoot DT, Cole RN, Boronina TN, et al. Synthetic circular RNA functions as a miR-21 sponge to suppress gastric carcinoma cell proliferation. Mol Ther Nucleic Acids. 2018;13:312–321. doi: 10.1016/j.omtn.2018.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ping L, Jian-Jun C, Chu-Shu L, Guang-Hua L, Ming Z. Silencing of circ_0009910 inhibits acute myeloid leukemia cell growth through increasing miR-20a-5p. Blood Cells Mol Dis. 2019;75:41–47. doi: 10.1016/j.bcmd.2018.12.006. [DOI] [PubMed] [Google Scholar]
- 20.Liu J, Kong F, Lou S, Yang D, Gu L. Global identification of circular RNAs in chronic myeloid leukemia reveals hsa_circ_0080145 regulates cell proliferation by sponging miR-29b. Biochem Biophys Res Commun. 2018;504:660–665. doi: 10.1016/j.bbrc.2018.08.154. [DOI] [PubMed] [Google Scholar]
- 21.Yuan DM, Ma J, Fang WB. Identification of non-coding RNA regulatory networks in pediatric acute myeloid leukemia reveals circ-0004136 could promote cell proliferation by sponging miR-142. Eur Rev Med Pharmacol Sci. 2019;23:9251–9258. doi: 10.26355/eurrev_201911_19417. [DOI] [PubMed] [Google Scholar]
- 22.Han F, Zhong C, Li W, Wang R, Zhang C, Yang X, Ji C, Ma D. hsa_circ_0001947 suppresses acute myeloid leukemia progression via targeting hsa-miR-329-5p/CREBRF axis. Epigenomics. 2020;12:935–953. doi: 10.2217/epi-2019-0352. [DOI] [PubMed] [Google Scholar]
- 23.Fan H, Li Y, Liu C, Liu Y, Bai J, Li W. Circular RNA-100290 promotes cell proliferation and inhibits apoptosis in acute myeloid leukemia cells via sponging miR-203. Biochem Biophys Res Commun. 2018;507:178–184. doi: 10.1016/j.bbrc.2018.11.002. [DOI] [PubMed] [Google Scholar]
- 24.Chen JJ, Lei P, Zhou M. hsa_circ_0121582 inhibits leukemia growth by dampening Wnt/beta-catenin signaling. Clin Transl Oncol 2020. [DOI] [PubMed]
- 25.Sun YM, Wang WT, Zeng ZC, Chen TQ, Han C, Pan Q, Huang W, Fang K, Sun LY, Zhou YF, et al. circMYBL2, a circRNA from MYBL2, regulates FLT3 translation by recruiting PTBP1 to promote FLT3-ITD AML progression. Blood. 2019;134:1533–1546. doi: 10.1182/blood.2019000802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zhang L, Bu Z, Shen J, Shang L, Chen Y, Wang Y. A novel circular RNA (hsa_circ_0000370) increases cell viability and inhibits apoptosis of FLT3-ITD-positive acute myeloid leukemia cells by regulating miR-1299 and S100A7A. Biomed Pharmacother. 2020;122:109619. doi: 10.1016/j.biopha.2019.109619. [DOI] [PubMed] [Google Scholar]
- 27.Hu J, Han Q, Gu Y, Ma J, McGrath M, Qiao F, Chen B, Song C, Ge Z. Circular RNA PVT1 expression and its roles in acute lymphoblastic leukemia. Epigenomics. 2018;10:723–732. doi: 10.2217/epi-2017-0142. [DOI] [PubMed] [Google Scholar]
- 28.Liu X, Zhou C, Li Y, Deng Y, Lu W, Li J. Upregulation of circ-0000745 in acute lymphoblastic leukemia enhanced cell proliferation by activating ERK pathway. Gene. 2020;751:144726. doi: 10.1016/j.gene.2020.144726. [DOI] [PubMed] [Google Scholar]
- 29.Raz O, Granot G, Pasmanik-Chor M, Raanani P, Rozovski U. Profiling and bioinformatics analyses reveal chronic lymphocytic leukemia cells share a unique circular RNA expression pattern. Exp Hematol. 2020;85:8–12. doi: 10.1016/j.exphem.2020.04.001. [DOI] [PubMed] [Google Scholar]
- 30.Wu W, Wu Z, Xia Y, Qin S, Li Y, Wu J, Liang J, Wang L, Zhu H, Fan L, et al. Downregulation of circ_0132266 in chronic lymphocytic leukemia promoted cell viability through miR-337-3p/PML axis. Aging (Albany NY) 2019;11:3561–3573. doi: 10.18632/aging.101997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Xia L, Wu L, Bao J, Li Q, Chen X, Xia H, Xia R. Circular RNA circ-CBFB promotes proliferation and inhibits apoptosis in chronic lymphocytic leukemia through regulating miR-607/FZD3/Wnt/beta-catenin pathway. Biochem Biophys Res Commun. 2018;503:385–390. doi: 10.1016/j.bbrc.2018.06.045. [DOI] [PubMed] [Google Scholar]
- 32.Deng L, Liu G, Zheng C, Zhang L, Kang Y, Yang F. Circ-LAMP1 promotes T-cell lymphoblastic lymphoma progression via acting as a ceRNA for miR-615-5p to regulate DDR2 expression. Gene. 2019;701:146–151. doi: 10.1016/j.gene.2019.03.052. [DOI] [PubMed] [Google Scholar]
- 33.Hu Y, Zhao Y, Shi C, Ren P, Wei B, Guo Y, Ma J. A circular RNA from APC inhibits the proliferation of diffuse large B-cell lymphoma by inactivating Wnt/beta-catenin signaling via interacting with TET1 and miR-888. Aging (Albany NY) 2019;11:8068–8084. doi: 10.18632/aging.102122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mei M, Wang Y, Wang Q, Liu Y, Song W, Zhang M. CircCDYL serves as a new biomarker in mantle cell lymphoma and promotes cell proliferation. Cancer Manag Res. 2019;11:10215–10221. doi: 10.2147/CMAR.S232075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chen F, Wang X, Fu S, Wang S, Fu Y, Zhang J, Liu Z. Circular RNA circ-CDYL sponges miR-1180 to elevate yes-associated protein in multiple myeloma. Exp Biol Med (Maywood) 2020;245:925–932. doi: 10.1177/1535370220918191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zhou X, Chen N, Xu H, Zhou X, Wang J, Fang X, Zhang Y, Li Y, Yang J, Wang X. Regulation of Hippo-YAP signaling by insulin-like growth factor-1 receptor in the tumorigenesis of diffuse large B-cell lymphoma. J Hematol Oncol. 2020;13:77. doi: 10.1186/s13045-020-00906-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Feng Y, Zhang L, Wu J, Khadka B, Fang Z, Gu J, Tang B, Xiao R, Pan G, Liu J. CircRNA circ_0000190 inhibits the progression of multiple myeloma through modulating miR-767-5p/MAPK4 pathway. J Exp Clin Cancer Res. 2019;38:54. doi: 10.1186/s13046-019-1071-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Liu F, Wang YL, Wei JM, Huang ZD. Upregulation of circ_0000142 promotes multiple myeloma progression by adsorbing miR-610 and upregulating AKT3 expression. J Biochem. 2020 [DOI] [PubMed]
- 39.Wang Y, Lin Q, Song C, Ma R, Li X. Circ_0007841 promotes the progression of multiple myeloma through targeting miR-338-3p/BRD4 signaling cascade. Cancer Cell Int. 2020;20:383. doi: 10.1186/s12935-020-01475-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Xia X, Li X, Li F, Wu X, Zhang M, Zhou H, Huang N, Yang X, Xiao F, Liu D, et al. A novel tumor suppressor protein encoded by circular AKT3 RNA inhibits glioblastoma tumorigenicity by competing with active phosphoinositide-dependent Kinase-1. Mol Cancer. 2019;18:131. doi: 10.1186/s12943-019-1056-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Huang X, Li Z, Zhang Q, Wang W, Li B, Wang L, Xu Z, Zeng A, Zhang X, Zhang X, et al. Circular RNA AKT3 upregulates PIK3R1 to enhance cisplatin resistance in gastric cancer via miR-198 suppression. Mol Cancer. 2019;18:71. doi: 10.1186/s12943-019-0969-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Li M, Meng F, Lu Q. Expression profile screening and bioinformatics analysis of circRNA, LncRNA, and mRNA in acute myeloid leukemia drug-resistant cells. Turk J Haematol. 2020;37:104–110. doi: 10.4274/tjh.galenos.2019.2019.0312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Shang J, Chen WM, Wang ZH, Wei TN, Chen ZZ, Wu WB. CircPAN3 mediates drug resistance in acute myeloid leukemia through the miR-153-5p/miR-183-5p-XIAP axis. Exp Hematol. 2019;70:42–54. doi: 10.1016/j.exphem.2018.10.011. [DOI] [PubMed] [Google Scholar]
- 44.Ferdinand R, Mitchell SA, Batson S, Tumur I. Treatments for chronic myeloid leukemia: a qualitative systematic review. J Blood Med. 2012;3:51–76. doi: 10.2147/JBM.S33380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Pan Y, Lou J, Wang H, An N, Chen H, Zhang Q, Du X. CircBA9.3 supports the survival of leukaemic cells by up-regulating c-ABL1 or BCR-ABL1 protein levels. Blood Cells Mol Dis. 2018;73:38–44. doi: 10.1016/j.bcmd.2018.09.002. [DOI] [PubMed] [Google Scholar]
- 46.Ping L, Jian-Jun C, Chu-Shu L, Guang-Hua L, Ming Z: High circ_100053 predicts a poor outcome for chronic myeloid leukemia and is involved in imatinib resistance. Oncol Res. 2019. [DOI] [PubMed]
- 47.Cao HX, Miao CF, Sang LN, Huang YM, Zhang R, Sun L, Jiang ZX. Circ_0009910 promotes imatinib resistance through ULK1-induced autophagy by sponging miR-34a-5p in chronic myeloid leukemia. Life Sci. 2020;243:117255. doi: 10.1016/j.lfs.2020.117255. [DOI] [PubMed] [Google Scholar]
- 48.Gao M, Li C, Xiao H, Dong H, Jiang S, Fu Y, Gong L. hsa_circ_0007841: A novel potential biomarker and drug resistance for multiple myeloma. Front Oncol. 2019;9:1261. doi: 10.3389/fonc.2019.01261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Song Y, Hu N, Song X, Yang J. Hsa_Circ_0007841 Enhances multiple myeloma chemotherapy resistance through upregulating ABCG2. Technol Cancer Res Treat. 2020;19:1533033820928371. doi: 10.1177/1533033820928371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Zhu YP, Zheng Z, Xiang Y, Zhang Y. Glucose starvation-induced rapid death of Nrf1alpha-deficient, but not Nrf2-deficient, hepatoma cells results from its fatal defects in the redox metabolism reprogramming. Oxid Med Cell Longev. 2020;2020:4959821. doi: 10.1155/2020/4959821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Warburg O. On the origin of cancer cells. Science. 1956;123:309–314. doi: 10.1126/science.123.3191.309. [DOI] [PubMed] [Google Scholar]
- 52.Lapa B, Goncalves AC, Jorge J, Alves R, Pires AS, Abrantes AM, Coucelo M, Abrunhosa A, Botelho MF, Nascimento-Costa JM, Sarmento-Ribeiro AB. Acute myeloid leukemia sensitivity to metabolic inhibitors: glycolysis showed to be a better therapeutic target. Med Oncol. 2020;37:72. doi: 10.1007/s12032-020-01394-6. [DOI] [PubMed] [Google Scholar]
- 53.Xu Y, Zhou Y, Cao W, Liu H. Improved production of malic acid in aspergillus niger by abolishing citric acid accumulation and enhancing glycolytic flux. ACS Synth Biol. 2020;9:1418–1425. doi: 10.1021/acssynbio.0c00096. [DOI] [PubMed] [Google Scholar]
- 54.Chen X, Yu J, Tian H, Shan Z, Liu W, Pan Z, Ren J. Circle RNA hsa_circRNA_100290 serves as a ceRNA for miR-378a to regulate oral squamous cell carcinoma cells growth via Glucose transporter-1 (GLUT1) and glycolysis. J Cell Physiol. 2019;234:19130–19140. doi: 10.1002/jcp.28692. [DOI] [PubMed] [Google Scholar]
- 55.Zhang X, Wang S, Lin G, Wang D. Down-regulation of circ-PTN suppresses cell proliferation, invasion and glycolysis in glioma by regulating miR-432-5p/RAB10 axis. Neurosci Lett. 2020;735:135153. doi: 10.1016/j.neulet.2020.135153. [DOI] [PubMed] [Google Scholar]
- 56.Zhu X, Du J, Gu Z. Circ-PVT1/miR-106a-5p/HK2 axis regulates cell growth, metastasis and glycolytic metabolism of oral squamous cell carcinoma. Mol Cell Biochem. 2020;474:147–158. doi: 10.1007/s11010-020-03840-5. [DOI] [PubMed] [Google Scholar]
- 57.Yu T, Wang Y, Fan Y, Fang N, Wang T, Xu T, Shu Y. CircRNAs in cancer metabolism: a review. J Hematol Oncol. 2019;12:90. doi: 10.1186/s13045-019-0776-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Andersen CJ, Dupree L, Murray K, Ragonesi N, McMullen K, Cintron-Rivera L, Doerr A. Low-density lipoproteins, high-density lipoproteins (HDL), and HDL-associated proteins differentially modulate chronic myelogenous leukemia cell viability. Lipids 2020. [DOI] [PubMed]
- 59.Arcinas C, Tan W, Fang W, Desai TP, Teh DCS, Degirmenci U, Xu D, Foo R, Sun L. Adipose circular RNAs exhibit dynamic regulation in obesity and functional role in adipogenesis. Nat Metab. 2019;1:688–703. doi: 10.1038/s42255-019-0078-z. [DOI] [PubMed] [Google Scholar]
- 60.Zhang C, Chen K, Wei R, Fan G, Cai X, Xu L, Cen B, Wang J, Xie H, Zheng S, Xu X. The circFASN/miR-33a pathway participates in tacrolimus-induced dysregulation of hepatic triglyceride homeostasis. Signal Transduct Target Ther. 2020;5:23. doi: 10.1038/s41392-020-0105-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ji MM, Wang L, Zhan Q, Xue W, Zhao Y, Zhao X, Xu PP, Shen Y, Liu H, Janin A, et al. Induction of autophagy by valproic acid enhanced lymphoma cell chemosensitivity through HDAC-independent and IP3-mediated PRKAA activation. Autophagy. 2015;11:2160–2171. doi: 10.1080/15548627.2015.1082024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Yao H, Han B, Zhang Y, Shen L, Huang R. Non-coding RNAs and autophagy. Adv Exp Med Biol. 2019;1206:199–220. doi: 10.1007/978-981-15-0602-4_10. [DOI] [PubMed] [Google Scholar]
- 63.Liang G, Ling Y, Mehrpour M, Saw PE, Liu Z, Tan W, Tian Z, Zhong W, Lin W, Luo Q, et al. Autophagy-associated circRNA circCDYL augments autophagy and promotes breast cancer progression. Mol Cancer. 2020;19:65. doi: 10.1186/s12943-020-01152-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.He D, Zheng J, Hu J, Chen J, Wei X. Long non-coding RNAs and pyroptosis. Clin Chim Acta. 2020;504:201–208. doi: 10.1016/j.cca.2019.11.035. [DOI] [PubMed] [Google Scholar]
- 65.Johnson DC, Taabazuing CY, Okondo MC, Chui AJ, Rao SD, Brown FC, Reed C, Peguero E, de Stanchina E, Kentsis A, Bachovchin DA. DPP8/DPP9 inhibitor-induced pyroptosis for treatment of acute myeloid leukemia. Nat Med. 2018;24:1151–1156. doi: 10.1038/s41591-018-0082-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Wen S, Li S, Li L, Fan Q. circACTR2: a novel mechanism regulating high glucose-induced fibrosis in renal tubular cells via pyroptosis. Biol Pharm Bull. 2020;43:558–564. doi: 10.1248/bpb.b19-00901. [DOI] [PubMed] [Google Scholar]
- 67.Yang F, Li A, Qin Y, Che H, Wang Y, Lv J, Li Y, Li H, Yue E, Ding X, et al. A novel circular RNA mediates pyroptosis of diabetic cardiomyopathy by functioning as a competing endogenous RNA. Mol Ther Nucleic Acids. 2019;17:636–643. doi: 10.1016/j.omtn.2019.06.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Koens L, Qin Y, Leung WY, Corver WE, Jansen PM, Willemze R, Vermeer MH, Tensen CP. MicroRNA profiling of primary cutaneous large B-cell lymphomas. PLoS ONE. 2013;8:e82471. doi: 10.1371/journal.pone.0082471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Yan B, Zhang Y, Liang C, Liu B, Ding F, Wang Y, Zhu B, Zhao R, Yu XY, Li Y. Stem cell-derived exosomes prevent pyroptosis and repair ischemic muscle injury through a novel exosome/circHIPK3/ FOXO3a pathway. Theranostics. 2020;10:6728–6742. doi: 10.7150/thno.42259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Feng XQ, Nie SM, Huang JX, Li TL, Zhou JJ, Wang W, Zhuang LK, Meng FJ. Circular RNA circHIPK3 serves as a prognostic marker to promote chronic myeloid leukemia progression. Neoplasma. 2020;67:171–177. doi: 10.4149/neo_2018_181129N908. [DOI] [PubMed] [Google Scholar]
- 71.Li JX, Zhang ZF, Wang XB, Yang EQ, Dong L, Meng J. PLZF regulates apoptosis of leukemia cells by regulating AKT/Foxo3a pathway. Eur Rev Med Pharmacol Sci. 2019;23:6411–6418. doi: 10.26355/eurrev_201908_18522. [DOI] [PubMed] [Google Scholar]
- 72.Wang H, Hua M, Wang S, Yu J, Chen C, Zhao X, Zhang C, Zhong C, Wang R, He N, et al. Genetic polymorphisms of IL-18 rs1946518 and IL-1beta rs16944 are associated with prognosis and survival of acute myeloid leukemia. Inflamm Res. 2017;66:249–258. doi: 10.1007/s00011-016-1012-4. [DOI] [PubMed] [Google Scholar]
- 73.Mou Y, Wang J, Wu J, He D, Zhang C, Duan C, Li B. Ferroptosis, a new form of cell death: opportunities and challenges in cancer. J Hematol Oncol. 2019;12:34. doi: 10.1186/s13045-019-0720-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Tang R, Xu J, Zhang B, Liu J, Liang C, Hua J, Meng Q, Yu X, Shi S. Ferroptosis, necroptosis, and pyroptosis in anticancer immunity. J Hematol Oncol. 2020;13:110. doi: 10.1186/s13045-020-00946-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Zhang X, Wang L, Li H, Zhang L, Zheng X, Cheng W. Crosstalk between noncoding RNAs and ferroptosis: new dawn for overcoming cancer progression. Cell Death Dis. 2020;11:580. doi: 10.1038/s41419-020-02772-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Xu Q, Zhou L, Yang G, Meng F, Wan Y, Wang L, Zhang L. CircIL4R facilitates the tumorigenesis and inhibits ferroptosis in hepatocellular carcinoma by regulating the miR-541–3p/GPX4 axis. Cell Biol Int. 2020. [DOI] [PubMed]
- 77.Zhang HY, Zhang BW, Zhang ZB, Deng QJ. Circular RNA TTBK2 regulates cell proliferation, invasion and ferroptosis via miR-761/ITGB8 axis in glioma. Eur Rev Med Pharmacol Sci. 2020;24:2585–2600. doi: 10.26355/eurrev_202003_20528. [DOI] [PubMed] [Google Scholar]
- 78.Zhong Y, Tian F, Ma H, Wang H, Yang W, Liu Z, Liao A. FTY720 induces ferroptosis and autophagy via PP2A/AMPK pathway in multiple myeloma cells. Life Sci. 2020;260:118077. doi: 10.1016/j.lfs.2020.118077. [DOI] [PubMed] [Google Scholar]
- 79.Wang F, Lv H, Zhao B, Zhou L, Wang S, Luo J, Liu J, Shang P. Iron and leukemia: new insights for future treatments. J Exp Clin Cancer Res. 2019;38:406. doi: 10.1186/s13046-019-1397-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Vu LP, Cheng Y, Kharas MG. The biology of m(6)A RNA methylation in normal and malignant hematopoiesis. Cancer Discov. 2019;9:25–33. doi: 10.1158/2159-8290.CD-18-0959. [DOI] [PubMed] [Google Scholar]
- 81.Huang H, Weng H, Chen J. m(6)A modification in coding and non-coding RNAs: roles and therapeutic implications in cancer. Cancer Cell. 2020;37:270–288. doi: 10.1016/j.ccell.2020.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Ma S, Chen C, Ji X, Liu J, Zhou Q, Wang G, Yuan W, Kan Q, Sun Z. The interplay between m6A RNA methylation and noncoding RNA in cancer. J Hematol Oncol. 2019;12:121. doi: 10.1186/s13045-019-0805-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Zhou C, Molinie B, Daneshvar K, Pondick JV, Wang J, Van Wittenberghe N, Xing Y, Giallourakis CC, Mullen AC. Genome-wide maps of m6A circRNAs identify widespread and cell-type-specific methylation patterns that are distinct from mRNAs. Cell Rep. 2017;20:2262–2276. doi: 10.1016/j.celrep.2017.08.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Paramasivam A, Vijayashree Priyadharsini J. Novel insights into m6A modification in circular RNA and implications for immunity. Cell Mol Immunol. 2020;17:668–669. doi: 10.1038/s41423-020-0387-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Chen RX, Chen X, Xia LP, Zhang JX, Pan ZZ, Ma XD, Han K, Chen JW, Judde JG, Deas O, et al. N(6)-methyladenosine modification of circNSUN2 facilitates cytoplasmic export and stabilizes HMGA2 to promote colorectal liver metastasis. Nat Commun. 2019;10:4695. doi: 10.1038/s41467-019-12651-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Zhang C, Wang J, Geng X, Tu J, Gao H, Li L, Zhou X, Wu H, Jing J, Pan W, Mou Y. Circular RNA expression profile and m6A modification analysis in poorly differentiated adenocarcinoma of the stomach. Epigenomics 2020. [DOI] [PubMed]
- 87.Yang J, Han Q, Li C, Yang H, Chen X, Wang X. Circular RNA circ_0001105 inhibits progression and metastasis of osteosarcoma by sponging miR-766 and activating YTHDF2 expression. Onco Targets Ther. 2020;13:1723–1736. doi: 10.2147/OTT.S234668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Paris J, Morgan M, Campos J, Spencer GJ, Shmakova A, Ivanova I, Mapperley C, Lawson H, Wotherspoon DA, Sepulveda C, et al. Targeting the RNA m(6)A reader YTHDF2 selectively compromises cancer stem cells in acute myeloid leukemia. Cell Stem Cell. 2019;25:137–148. doi: 10.1016/j.stem.2019.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Wang M, Yang Y, Yang J, Yang J, Han S. circ_KIAA1429 accelerates hepatocellular carcinoma advancement through the mechanism of m(6)A-YTHDF3-Zeb1. Life Sci. 2020;257:118082. doi: 10.1016/j.lfs.2020.118082. [DOI] [PubMed] [Google Scholar]
- 90.Zhao L, Liu Y, Zhang J, Liu Y, Qi Q. LncRNA SNHG14/miR-5590-3p/ZEB1 positive feedback loop promoted diffuse large B cell lymphoma progression and immune evasion through regulating PD-1/PD-L1 checkpoint. Cell Death Dis. 2019;10:731. doi: 10.1038/s41419-019-1886-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Chen SJ, Zhou GB. Targeted therapy: the new lease on life for acute promyelocytic leukemia, and beyond. IUBMB Life. 2012;64:671–675. doi: 10.1002/iub.1055. [DOI] [PubMed] [Google Scholar]
- 92.Wang WT, Han C, Sun YM, Chen TQ, Chen YQ. Noncoding RNAs in cancer therapy resistance and targeted drug development. J Hematol Oncol. 2019;12:55. doi: 10.1186/s13045-019-0748-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Guarnerio J, Bezzi M, Jeong JC, Paffenholz SV, Berry K, Naldini MM, Lo-Coco F, Tay Y, Beck AH, Pandolfi PP. Oncogenic role of fusion-circRNAs derived from cancer-associated chromosomal translocations. Cell. 2016;165:289–302. doi: 10.1016/j.cell.2016.03.020. [DOI] [PubMed] [Google Scholar]
- 94.Zhao X, Chen A, Yan X, Zhang Y, He F, Hayashi Y, Dong Y, Rao Y, Li B, Conway RM, et al. Downregulation of RUNX1/CBFbeta by MLL fusion proteins enhances hematopoietic stem cell self-renewal. Blood. 2014;123:1729–1738. doi: 10.1182/blood-2013-03-489575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Dal Molin A, Bresolin S, Gaffo E, Tretti C, Boldrin E, Meyer LH, Guglielmelli P, Vannucchi AM, Te Kronnie G, Bortoluzzi S. CircRNAs are here to stay: a perspective on the MLL recombinome. Front Genet. 2019;10:88. doi: 10.3389/fgene.2019.00088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Huang W, Fang K, Chen TQ, Zeng ZC, Sun YM, Han C, Sun LY, Chen ZH, Yang QQ, Pan Q, et al. circRNA circAF4 functions as an oncogene to regulate MLL-AF4 fusion protein expression and inhibit MLL leukemia progression. J Hematol Oncol. 2019;12:103. doi: 10.1186/s13045-019-0800-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Papaioannou D, Volinia S, Nicolet D, Swierniak M, Petri A, Mrozek K, Bill M, Pepe F, Walker CJ, Walker AE, et al. Clinical and functional significance of circular RNAs in cytogenetically normal AML. Blood Adv. 2020;4:239–251. doi: 10.1182/bloodadvances.2019000568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Nagoshi H, Taki T, Hanamura I, Nitta M, Otsuki T, Nishida K, Okuda K, Sakamoto N, Kobayashi S, Yamamoto-Sugitani M, et al. Frequent PVT1 rearrangement and novel chimeric genes PVT1-NBEA and PVT1-WWOX occur in multiple myeloma with 8q24 abnormality. Cancer Res. 2012;72:4954–4962. doi: 10.1158/0008-5472.CAN-12-0213. [DOI] [PubMed] [Google Scholar]
- 99.Tsutsumi Y, Chinen Y, Sakamoto N, Nagoshi H, Nishida K, Kobayashi S, Yokokawa Y, Taki T, Sasaki N, Yamamoto-Sugitani M, et al. Deletion or methylation of CDKN2A/2B and PVT1 rearrangement occur frequently in highly aggressive B-cell lymphomas harboring 8q24 abnormality. Leuk Lymphoma. 2013;54:2760–2764. doi: 10.3109/10428194.2013.790543. [DOI] [PubMed] [Google Scholar]
- 100.Gaffo E, Boldrin E, Dal Molin A, Bresolin S, Bonizzato A, Trentin L, Frasson C, Debatin KM, Meyer LH, Te Kronnie G, Bortoluzzi S. Circular RNA differential expression in blood cell populations and exploration of circRNA deregulation in pediatric acute lymphoblastic leukemia. Sci Rep. 2019;9:14670. doi: 10.1038/s41598-019-50864-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Alberto L, Tolomeo D, Cifola I, Severgnini M, Turchiano A, Augello B, Squeo G, Pietro D, Traversa D, Daniele G, et al. MYC-containing amplicons in acute myeloid leukemia: genomic structures, evolution, and transcriptional consequences. Leukemia. 2018;32:2152–2166. doi: 10.1038/s41375-018-0033-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Cheng Y, Su Y, Wang S, Liu Y, Jin L, Wan Q, Liu Y, Li C, Sang X, Yang L, et al: Identification of circRNA-lncRNA-miRNA-mRNA competitive endogenous RNA network as novel prognostic markers for acute myeloid leukemia. Genes (Basel) 2020, 11. [DOI] [PMC free article] [PubMed]
- 103.Guo S, Li B, Chen Y, Zou D, Yang S, Zhang Y, Wu N, Sheng L, Huang H, Ouyang G, Mu Q. Hsa_circ_0012152 and Hsa_circ_0001857 accurately discriminate acute lymphoblastic leukemia from acute myeloid leukemia. Front Oncol. 2020;10:1655. doi: 10.3389/fonc.2020.01655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Zhou J, Zhou LY, Tang X, Zhang J, Zhai LL, Yi YY, Yi J, Lin J, Qian J, Deng ZQ. Circ-Foxo3 is positively associated with the Foxo3 gene and leads to better prognosis of acute myeloid leukemia patients. BMC Cancer. 2019;19:930. doi: 10.1186/s12885-019-5967-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Ding Y, Dong Y, Lu H, Luo X, Fu J, Xiu B, Liang A, Zhang W. Circular RNA profile of acute myeloid leukaemia indicates circular RNA annexin A2 as a potential biomarker and therapeutic target for acute myeloid leukaemia. Am J Transl Res. 2020;12:1683–1699. [PMC free article] [PubMed] [Google Scholar]
- 106.Yi YY, Yi J, Zhu X, Zhang J, Zhou J, Tang X, Lin J, Wang P, Deng ZQ. Circular RNA of vimentin expression as a valuable predictor for acute myeloid leukemia development and prognosis. J Cell Physiol. 2019;234:3711–3719. doi: 10.1002/jcp.27145. [DOI] [PubMed] [Google Scholar]
- 107.Hirsch S, Blatte TJ, Grasedieck S, Cocciardi S, Rouhi A, Jongen-Lavrencic M, Paschka P, Kronke J, Gaidzik VI, Dohner H, et al. Circular RNAs of the nucleophosmin (NPM1) gene in acute myeloid leukemia. Haematologica. 2017;102:2039–2047. doi: 10.3324/haematol.2017.172866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Wu Z, Sun H, Liu W, Zhu H, Fu J, Yang C, Fan L, Wang L, Liu Y, Xu W, et al. Circ-RPL15: a plasma circular RNA as novel oncogenic driver to promote progression of chronic lymphocytic leukemia. Leukemia. 2020;34:919–923. doi: 10.1038/s41375-019-0594-6. [DOI] [PubMed] [Google Scholar]
- 109.Liu X, Tang H, Liu J, Wang X. hsa_circRNA_101237: a novel diagnostic and prognostic biomarker and potential therapeutic target for multiple myeloma. Cancer Manag Res. 2020;12:2109–2118. doi: 10.2147/CMAR.S241089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Rybak-Wolf A, Stottmeister C, Glazar P, Jens M, Pino N, Giusti S, Hanan M, Behm M, Bartok O, Ashwal-Fluss R, et al. Circular RNAs in the mammalian brain are highly abundant, conserved, and dynamically expressed. Mol Cell. 2015;58:870–885. doi: 10.1016/j.molcel.2015.03.027. [DOI] [PubMed] [Google Scholar]
- 111.Li S, Ma Y, Tan Y, Ma X, Zhao M, Chen B, Zhang R, Chen Z, Wang K. Profiling and functional analysis of circular RNAs in acute promyelocytic leukemia and their dynamic regulation during all-trans retinoic acid treatment. Cell Death Dis. 2018;9:651. doi: 10.1038/s41419-018-0699-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Li W, Zhong C, Jiao J, Li P, Cui B, Ji C, Ma D: Characterization of hsa_circ_0004277 as a new biomarker for acute myeloid leukemia via circular RNA profile and bioinformatics analysis. Int J Mol Sci. 2017 18. [DOI] [PMC free article] [PubMed]
- 113.Fanale D, Taverna S, Russo A, Bazan V. Circular RNA in exosomes. Adv Exp Med Biol. 2018;1087:109–117. doi: 10.1007/978-981-13-1426-1_9. [DOI] [PubMed] [Google Scholar]
- 114.Wang G, Liu W, Zou Y, Wang G, Deng Y, Luo J, Zhang Y, Li H, Zhang Q, Yang Y, Chen G. Three isoforms of exosomal circPTGR1 promote hepatocellular carcinoma metastasis via the miR449a-MET pathway. EBioMedicine. 2019;40:432–445. doi: 10.1016/j.ebiom.2018.12.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Wu Z, Sun H, Wang C, Liu W, Liu M, Zhu Y, Xu W, Jin H, Li J. Mitochondrial genome-derived circRNA mc-COX2 functions as an oncogene in chronic lymphocytic leukemia. Mol Ther Nucleic Acids. 2020;20:801–811. doi: 10.1016/j.omtn.2020.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Luo Y, Gui R: Circulating Exosomal circMYC is Associated with the recurrence and Bortezomib resistance in patients with multiple myeloma. Turk J Haematol. 2020. [DOI] [PMC free article] [PubMed]
- 117.Ho TT, Zhou N, Huang J, Koirala P, Xu M, Fung R, Wu F, Mo YY. Targeting non-coding RNAs with the CRISPR/Cas9 system in human cell lines. Nucleic Acids Res. 2015;43:e17. doi: 10.1093/nar/gku1198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Jost I, Shalamova LA, Gerresheim GK, Niepmann M, Bindereif A, Rossbach O. Functional sequestration of microRNA-122 from Hepatitis C Virus by circular RNA sponges. RNA Biol. 2018;15:1032–1039. doi: 10.1080/15476286.2018.1435248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Wu P, Mo Y, Peng M, Tang T, Zhong Y, Deng X, Xiong F, Guo C, Wu X, Li Y, et al. Emerging role of tumor-related functional peptides encoded by lncRNA and circRNA. Mol Cancer. 2020;19:22. doi: 10.1186/s12943-020-1147-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Yi Z, Li Y, Wu Y, Zeng B, Li H, Ren G, Wang X. Circular RNA 0001073 attenuates malignant biological behaviours in breast cancer cell and is delivered by nanoparticles to inhibit mice tumour growth. Onco Targets Ther. 2020;13:6157–6169. doi: 10.2147/OTT.S248822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Wang W, Han Y, Jo HA, Lee J, Song YS. Non-coding RNAs shuttled via exosomes reshape the hypoxic tumor microenvironment. J Hematol Oncol. 2020;13:67. doi: 10.1186/s13045-020-00893-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Chen W, Quan Y, Fan S, Wang H, Liang J, Huang L, Chen L, Liu Q, He P, Ye Y. Exosome-transmitted circular RNA hsa_circ_0051443 suppresses hepatocellular carcinoma progression. Cancer Lett. 2020;475:119–128. doi: 10.1016/j.canlet.2020.01.022. [DOI] [PubMed] [Google Scholar]
- 123.Song H, Liu Q, Liao Q. Circular RNA and tumor microenvironment. Cancer Cell Int. 2020;20:211. doi: 10.1186/s12935-020-01301-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Wang J, Zhao X, Wang Y, Ren F, Sun D, Yan Y, Kong X, Bu J, Liu M, Xu S. circRNA-002178 act as a ceRNA to promote PDL1/PD1 expression in lung adenocarcinoma. Cell Death Dis. 2020;11:32. doi: 10.1038/s41419-020-2230-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Wu DM, Wen X, Han XR, Wang S, Wang YJ, Shen M, Fan SH, Zhang ZF, Shan Q, Li MQ, et al: Role of Circular RNA DLEU2 in Human Acute Myeloid Leukemia. Mol Cell Biol. 2018. 38. [DOI] [PMC free article] [PubMed]
- 126.Liu H, Wu Y, Wang S, Jiang J, Zhang C, Jiang Y, Wang X, Hong L, Huang H. Circ-SMARCA5 suppresses progression of multiple myeloma by targeting miR-767-5p. BMC Cancer. 2019;19:937. doi: 10.1186/s12885-019-6088-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Glazar P, Papavasileiou P, Rajewsky N. circBase: a database for circular RNAs. RNA. 2014;20:1666–1670. doi: 10.1261/rna.043687.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Dudekula DB, Panda AC, Grammatikakis I, De S, Abdelmohsen K, Gorospe M. CircInteractome: a web tool for exploring circular RNAs and their interacting proteins and microRNAs. RNA Biol. 2016;13:34–42. doi: 10.1080/15476286.2015.1128065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Dong R, Ma XK, Li GW, Yang L. CIRCpedia v2: an updated database for comprehensive circular RNA annotation and expression comparison. Genom Proteomics Bioinform. 2018;16:226–233. doi: 10.1016/j.gpb.2018.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Chen X, Han P, Zhou T, Guo X, Song X, Li Y. circRNADb: A comprehensive database for human circular RNAs with protein-coding annotations. Sci Rep. 2016;6:34985. doi: 10.1038/srep34985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Xia S, Feng J, Chen K, Ma Y, Gong J, Cai F, Jin Y, Gao Y, Xia L, Chang H, et al. CSCD: a database for cancer-specific circular RNAs. Nucleic Acids Res. 2018;46:D925–D929. doi: 10.1093/nar/gkx863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Li S, Li Y, Chen B, Zhao J, Yu S, Tang Y, Zheng Q, Li Y, Wang P, He X, Huang S. exoRBase: a database of circRNA, lncRNA and mRNA in human blood exosomes. Nucleic Acids Res. 2018;46:D106–D112. doi: 10.1093/nar/gkx891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Vo JN, Cieslik M, Zhang Y, Shukla S, Xiao L, Zhang Y, Wu YM, Dhanasekaran SM, Engelke CG, Cao X, et al. The landscape of circular RNA in cancer. Cell. 2019;176(869–881):e813. doi: 10.1016/j.cell.2018.12.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Ji P, Wu W, Chen S, Zheng Y, Zhou L, Zhang J, Cheng H, Yan J, Zhang S, Yang P, Zhao F. Expanded expression landscape and prioritization of circular RNAs in mammals. Cell Rep. 2019;26:3444–3460. doi: 10.1016/j.celrep.2019.02.078. [DOI] [PubMed] [Google Scholar]
- 135.Liu M, Wang Q, Shen J, Yang BB, Ding X. Circbank: a comprehensive database for circRNA with standard nomenclature. RNA Biol. 2019;16:899–905. doi: 10.1080/15476286.2019.1600395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Li L, Wu P, Wang Z, Meng X, Zha C, Li Z, Qi T, Zhang Y, Han B, Li S, et al. NoncoRNA: a database of experimentally supported non-coding RNAs and drug targets in cancer. J Hematol Oncol. 2020;13:15. doi: 10.1186/s13045-020-00849-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.