Abstract
Background
The Coronavirus disease (COVID-19) has caused 91,305 confirmed cases and 4746 deaths in China by 13:50 on October 11, 2020. We analyzed data on 69 infections in Wuxi to describe the disease’s characteristics, to analyze factors of cases clinical outcome and to evaluate the prevention and control measures.
Methods
The demographic characteristics, exposure history, time indicators and propagation dynamics in Wuxi were collected.
Results
The clinical severity of cases was mostly mild and normal (75.36 %). Aging (relative risk [RR] = 1.04, 95 % confidence interval [CI]: 1.001–1.08) and fever (RR = 10.33, 95 %CI: 2.75–38.78) were risk factors for disease severity. The mean incubation period was estimated to be 4.77 days (95 % CI: 3.61–5.94), with a mean serial interval of 6.31 days (95 % CI: 5.12–7.50). The controlled reproduction number was estimated to be 1.12 (95 %CI: 0.71–1.69).
Conclusions
The incidence of COVID-19 in Wuxi has turned into a lower level, suggesting the early prevention and control measures have achieved effectiveness. Aging and fever of initial symptom were risk factors for severe clinical outcome. The family clusters provided further clues of the risk factors for COVID-19 transmission.
Keywords: COVID-19, Characteristics, Time indicators, Propagation dynamics, Risk factors
1. Introduction
The Coronavirus disease (COVID-19) was first reported in December 2019 in Wuhan, China, and now has spread globally (Guan et al., 2020). On January 20, 2020, National Health Commission of the People's Republic of China announced that the COVID-19 should be included in the Category B infectious disease stipulated in the Law of the People's Republic of China on the Prevention and Treatment of Infectious Diseases, and prevention and control measures of Category A infectious disease should be adopted (National Health Commission of the People’s Republic of China, 2020). Wuhan was closed on January 23, 2020. These measures have undoubtedly slowed the growth of the number of COVID-19 cases and limited the scale of the epidemic in China, with studies suggesting that hundreds of thousands of cases were averted as of February 19 (Li, Pei et al., 2020; Munster, Koopmans, van Doremalen, van Riel, & de Wit, 2020). Meanwhile, containment measures such as quarantining suspected patients and their contacts, restricting travel and imposing social isolation on the population were adopted in Wuxi to minimize the spread of the disease. The epidemic situation of Wuxi decreased significantly through such a series of measures after a longest incubation period. Although the results have shown that to fully control COVID-19, the identification and isolation of currently unregistered infections needs to be greatly increased (Li, Pei et al., 2020), but it is uncertain which measures are most effective. The population is generally susceptible to the SARS-CoV-2, and the elderly over 65 years of age are more likely to develop severe illness (Sun & Zhai, 2020; Tian et al., 2020). Adolescents and young adults have more opportunities to be exposed because of frequent activities such as study, work, and travel (Liao et al., 2020). The patients under the age of 20 in Wuxi accounted for 14.49 % (10/69), so a more comprehensive understanding of the characteristics of the disease is very necessary. The manuscript was based on the data from patients with COVID-19 in Wuxi city to describe the characteristics of the disease, to dynamically assess the infectivity of the SARS-CoV-2 in Wuxi and to evaluate the effectiveness of the prevention and control measures.
2. Materials and methods
2.1. Sources of data
According to the updated version (version 7) of COVID-19 prevention and control program published by National Health Commission of the People's Republic of China, when a medical institution finds a suspected case, a confirmed case or an asymptomatic infected person of COVID-19, it should immediately report the case directly in China Information System for Disease Control and Prevention. The medical institutions should timely revise the information of case classification and clinical severity according to laboratory test results, disease progression.
Once a suspected case was identified and reported, the field epidemiological investigation team comprising members from Wuxi Center for Disease Control and Prevention (Wuxi CDC) together with prefecture CDCs would be informed to initiate detailed field investigations and to collect the respiratory specimens for centralized testing at the laboratory of Wuxi CDC. The field epidemiological investigation team should conduct detailed field investigations for all suspected and confirmed COVID-19 cases in 24 h.
Epidemiologic data were collected through interviews and field reports. Data were collected in standardized forms through interviews of infected persons, relatives, close contacts, and health care workers. All epidemiologic information such as the history of exposure 2 weeks before the onset of illness, timelines of events, and close contacts identification, were collected during the field investigations.
2.2. Related definitions
The case definitions according to the updated version (version 7) of COVID-19 diagnosis and treatment program published by National Health Commission of the People's Republic of China. (1) A suspected COVID-19 case was defined as a pneumonia that either fulfilled all the following three criteria -fever, with or without recorded temperature; radiographic evidence of pneumonia; low or normal white-cell count or low lymphocyte count, following standard clinical guidelines or meeting the above mentioned two criteria and had an epidemiologic history. The epidemiologic four criteria were the following: a travel or residence history to Wuhan and surrounding areas or other communities with reported cases within 14 days before illness onset; a history of exposure to people infected with SARS-CoV-2; direct contact with patients from Wuhan and surrounding areas who had fever or respiratory symptoms. (2) A confirmed case was defined as a case with respiratory specimens that tested positive for SARS-CoV-2 by at least one of the following three methods: isolation of SARS-CoV-2 or at least two positive results by real-time reverse-transcription–polymerase chain-reaction (RT-PCR) assay for SARS-CoV-2 or a genetic sequence that matched SARS-CoV-2. (3) Asymptomatic infection was referred to those who had no clinical symptoms and respiratory tract or other specimens were positive in the detection of SARS-CoV-2. It was mainly found by means of cluster epidemic investigation and infection source tracking investigation. Cluster outbreak was defined as the detection of 2 or more confirmed cases or asymptomatic infection within 14 days in a small area (such as a family, a construction site, a unit, etc.), and the possibility of human-to-human transmission due to close contact, or the possibility of infection caused by joint exposure.
Close contacts referred to persons who had not effective protection and had close contact (within 1 m) with suspected or confirmed cases from 2 days before symptom onset or 2 days before sampling of samples of asymptomatic infected persons. Close contacts of the cases were monitored in intensive isolation for 14 days, and nasopharyngeal swabs and serum samples were collected for testing on the first day of observation and on the day before the released or when any symptoms of discomfort not limited to the respiratory system. At the same time, we also performed CT tests on close contacts.
Clinical subtypes included asymptomatic infection, mild-type (mild clinical symptoms, no pneumonia on imaging), normal-type (with fever, respiratory tract and other symptoms, imaging evidence of pneumonia), severe-type (i.e., dyspnea, respiratory frequency 30/min, blood oxygen saturation 93 %, partial pressure of arterial oxygen to fraction of inspired oxygen ratio <300, and/or lung infiltrates >50 % within 24–48 hours) and critical-type (i.e., respiratory failure, septic shock, and/or multiple organ dysfunction or failure).
2.3. Laboratory testing
The medical institutions that accepted and treated the cases should collect the relevant clinical specimens in time, including upper respiratory tract specimens (e.g. nasopharyngeal swabs, pharyngeal swabs, etc.), lower respiratory tract specimens (e.g. deep cough sputum, alveolar lavage fluid, bronchial lavage fluid, respiratory tract aspiration, etc.), fecal/anal swabs, anticoagulant and serum specimens, etc. The samples were sent to the virus laboratory of Wuxi CDC for testing as soon as possible. The positive results were reviewed by Jiangsu provincial CDC. MagNa Pure 96 DNA and Viral NA Small Volume Kit (Roche) was used to extract viral nucleic acid. The real-time fluorescent quantitative reverse transcription polymerase chain reaction (Real time RTPCR method, Real time PCR instrument, Light Cycler Ⅱ 480) was applied to identify the virus. SARS-CoV-2 was detected using the SARS-CoV-2 (ORF1ab/N) nucleic acid detection kit produced by DAAN Gene Co., Ltd. Of Sun Yat-sen University.
2.4. Statistical analysis
The epidemic curve was constructed by date of illness onset. The general characteristics of the cases were described, including demographic characteristics, exposure history and clinical information. The incubation period distribution (the time delay from infection to illness onset) was estimated by fitting a log-normal distribution to data on exposure history and onset dates in a subset of cases with detailed information available. Onset-first-medical visit and onset-to-admission distributions were estimated by fitting a Weibull distribution on the dates of illness onset, first medical visit, and hospital admission in a subset of cases with detailed information available. We fitted a gamma distribution to data from cluster investigations to estimate the serial interval distribution, which defined as the delay between illness onset dates in successive cases in chains of transmission.
The basic reproductive number (R0) was defined as the expected number of additional cases that one case would generate, on average, over the course of the infectious period in an otherwise uninfected population (Anderson & May, 1992). The controlled reproduction number (Rc), which was used to describe the ability of disease spreading after taking the interventions (such as quarantine, isolation, or traffic control), should be used instead of R0. A good measure of any intervention was to reduce Rc and the disease would decline and eventually died out if Rc≤1. We used an informative prior distribution for the serial interval based on the serial interval of SARS with a mean of 8.4 and a standard deviation of 3.8. We used the Exponential growth rate-based (EGR) model to calculate Rc (Wallinga & Lipsitch, 2007). Analyses of the incubation period, serial interval and Rc were performed with the use of R software (R Foundation for Statistical Computing).
Multivariate logistic regression analysis was used to analyze the factors affecting the outcome of the disease with SPSS version 16.0 (SPSS, Chicago, IL, USA). All testing was two-sided, and a p value < 0.05 was considered statistically significant.
3. Results
3.1. General characteristics
We identified suspected patients through enhancing surveillance in the fever clinics and collected their nasopharyngeal swabs for testing SARS-CoV-2. From January 18 to March 2, a total of 9023 nasopharyngeal swabs from suspected patients were sent to Wuxi CDC laboratory, 21(0.23 %) patients were detected positive of SARS-CoV-2. While screening suspected patients, we also quarantined and tested 1326 close contacts of the 21 confirmed cases. Through testing these close contacts, we detected 48(3.62 %) positive infections. All the 69 positive cases were reported from Jan 18, 2020 to Mar 2, 2020 in Wuxi city.
The median age of the patients was 45 years (range from 7 to 86), and 50.72 % patients (35/69) were male. Children and adolescents aged 0–19, young people aged 20–59 and elderly persons aged 60 and above accounted for 14.49 %, 65.22 % and 20.29 % respectively. The underlying diseases and clinical severity were significantly different across age groups (P < 0.05). Among the 69 infected patients, mild and normal types accounted for 75.36 % (52/69) and asymptomatic infections accounted for 14.49 % (10/69). Forty-six(66.67 %) cases were imported cases, including 24 cases from Hubei and 22 cases from other regions outside Hubei. The general characteristics of the imported cases and locally transmitted secondary cases were shown in Table 1 .
Table 1.
Characteristics of the patients with COVID-19 in Wuxi, China.
| General characteristics | Total cases n (%) |
Imported cases n (%) | Secondary cases n (%) |
|---|---|---|---|
| Total | 69 | 46 | 23 |
| Sex | |||
| Male | 35(50.72 %) | 26(56.52 %) | 9(39.13 %) |
| Female | 34(49.28 %) | 20(43.48 %) | 14(60.87 %) |
| Age group(year) | |||
| 0- | 3(4.35 %) | 1(2.17 %) | 2(8.70 %) |
| 10- | 7(10.14 %) | 7(15.22 %) | 0(0) |
| 20- | 9(13.04 %) | 8(17.39 %) | 1(4.35 %) |
| 30- | 10(14.49 %) | 7(15.22 %) | 3(13.04 %) |
| 40- | 10(14.49 %) | 7(15.22 %) | 3(13.04 %) |
| 50- | 16(23.19 %) | 8(17.39 %) | 8(34.78 %) |
| 60- | 7(10.14 %) | 4(8.70 %) | 3(13.04 %) |
| 70- | 5(7.25 %) | 3(6.52 %) | 2(8.70 %) |
| ≥80 | 2(2.90 %) | 1(2.17 %) | 1(4.35 %) |
| Exposure history | |||
| Travel or residence history in Hubei | 24(34.78 %) | 24(52.17 %) | – |
| Travel or residence history in other regions except Hubei | 22(31.88 %) | 22(47.83 %) | – |
| Contact with other people with a history of travelling or residence history in Hubei or other regions | 14(20.29 %) | – | 14(60.87 %) |
| History of exposure to locally confirmed cases or asymptomatic infections | 9(13.04 %) | – | 9(39.13 %) |
| Underlying diseases | |||
| Yes | 27(39.13 %) | 15(32.61 %) | 12(52.17 %) |
| No | 42(60.87 %) | 31(67.39 %) | 11(47.83 %) |
| Clinical severity* | |||
| Asymptomatic | 10(14.49 %) | 4(8.70 %) | 6(26.10 %) |
| Mild | 17(24.64 %) | 10(21.74 %) | 7(30.43 %) |
| Normal | 35(50.72 %) | 26(56.50 %) | 9(39.10 %) |
| Severe | 5(7.25 %) | 4(8.70 %) | 1(4.35 %) |
| Critical | 2(2.90 %) | 2(4.35 %) | 0(0) |
Patients were classified by their most severe status as of March 2, 2020. There may be cases where the composition ratio is not 1 due to rounding.
3.2. Date of symptoms onset
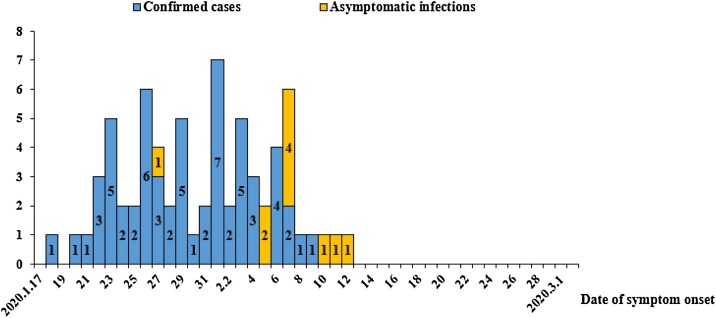
The epidemic curve of 69 patients (including 10 cases of asymptomatic infection) was shown in Fig. 1 . On January 23, Wuhan sealed the city. On January 25, Wuxi responded with a first-level response. After a maximum incubation period of 14 days, the number of cases decreased significantly. As of March 2, the onset of the last symptomatic case was on February 9.
Fig. 1.
Onset of illness among the cases of COVID-19 in Wuxi, China.
Our first case was identified when he returned Wuxi from Wuhan on January 15 (Wuhan city was closed on January 23), and developed symptoms on January 18. From January 18 to March 2, most of early cases came from Wuhan before the city was closed. During the middle and late of this period, Wuxi city began to discover cases from other provinces outside Hubei and other areas in our province (Jiangsu). The last asymptomatic infected person was tested positive for nucleic acid on 12 February (Fig. 1).
Analysis of time indicators and propagation dynamics
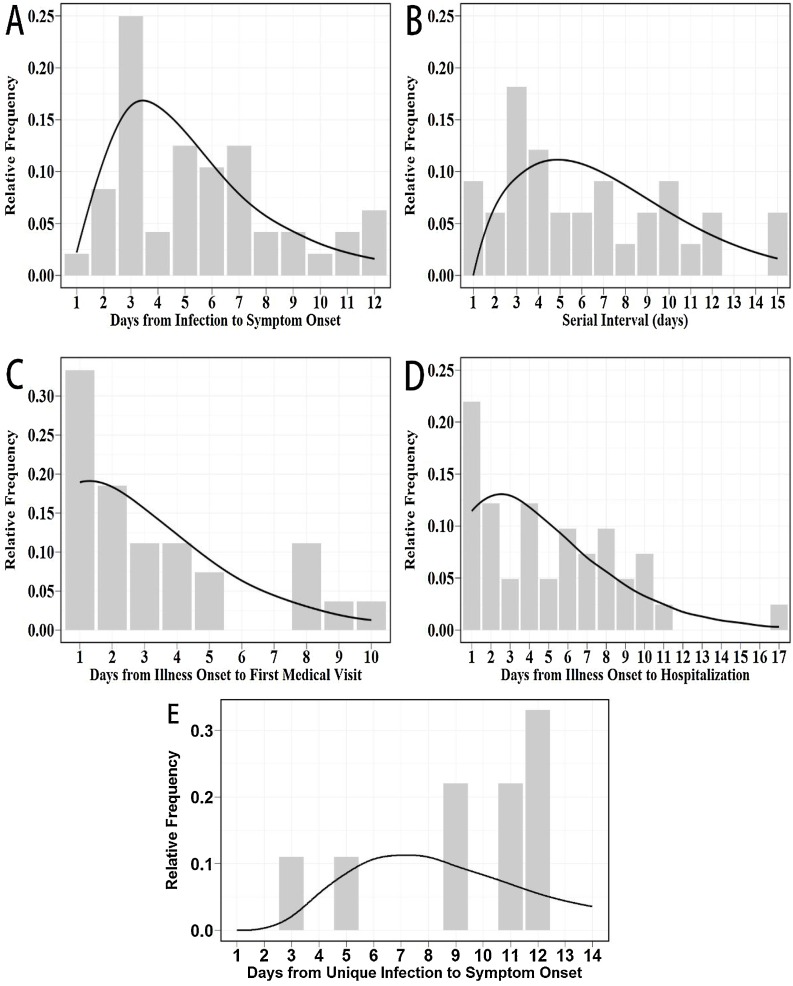
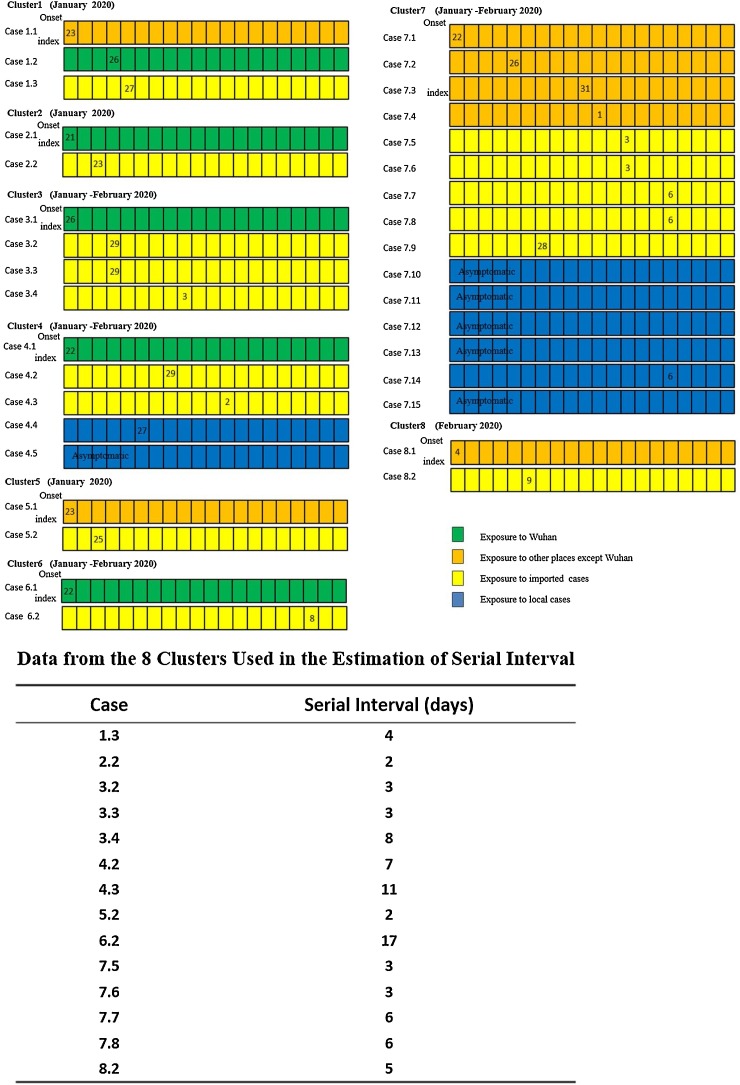
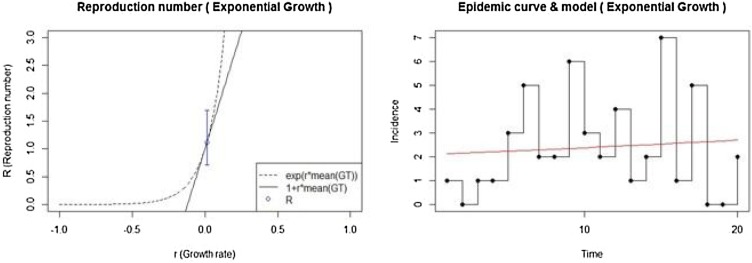
We examined data on exposures among 46 confirmed cases who had the last exposure time, and we estimated the mean incubation period to be 4.77 days (95 % CI: 3.61–5.94); the 95th percentile of the distribution was 12 days (95 %CI: 10.09–13.91) (Fig. 2 A). We obtained information from 8 clusters of cases, which was showed in Fig. 3 . On the basis of the dates of illness onset of 14 pairs of cases in these clusters, we estimated that the serial interval distribution had a mean (±SD) of 6.31(±3.88) days (95 % CI: 5.12–7.50) (Fig. 2B). The duration from illness onset to first medical visit for 52 patients was estimated to have a mean of 3.47 days (95 % CI: 2.68–4.26) (Fig. 2C). The mean duration from onset to hospital admission was estimated to be 4.43 days (95 % CI: 3.45–5.40) among 51 cases with illness (Fig. 2D). Of the 69 infections, 12 cases had a unique history of exposure, and 3 cases were asymptomatic at discharge, so we analyzed 9 cases of them and estimated another mean incubation period of 8.59 days (95 % CI: 7.56–9.62) (Fig. 2E). We calculated Rc to evaluate the transmission dynamics of the disease using the Exponential growth rate-based (EGR) model. From January 18th to February 9th, the mean Rc value was 1.12 (95 % CI: 0.71–1.69), meaning that each patient could spread infection to 1.12 other people on average (Fig. 4 ).
Fig. 2.
Key time-to-event distributions.
Fig. 3.
Detailed information on exposures and dates of illness onset in 8 clusters including 35 cases.
Fig. 4.
Estimate of the reproduction number with the EGR model from January 18th to February 9th.
The estimated incubation period distribution (i.e., the time from infection to illness onset, the time infection was defined as the latest exposure to epidemic areas or infectious persons) was shown in Panel A. The estimated serial interval distribution (i.e., the time interval between the onset of successive cases in a transmission chain) was shown in Panel B. The estimated distribution of time from illness onset to first medical visit was shown in Panel C. The estimated distribution of time from illness onset to hospital admission was shown in Panel D. The estimated incubation period distribution (i.e., the time from unique infection to illness onset, the unique infection was defined as once exposure to infectious persons) was shown in Panel E.
Numbers in boxes were calendar dates in January and February 2020. Data from the 14 secondary cases (patients who had clear exposure to only one index case and had no other potential source of infection) were used to estimate the serial interval distribution.
3.3. Multi-factors analysis of cases clinical outcome
In the study of 59 symptomatic patients, the most common symptoms were fever (66.10 %), cough (dry cough or expectoration) (49.15 %), fatigue (15.25 %), headache (13.56 %), muscle aches (11.86 %), sore throat (10.17 %), and diarrhea (6.78 %). Thirty-six percent (21/59) of the patients had underlying diseases, including diabetes (9 patients), hypertension (11 patients), and cardiovascular disease (4 patients). We divided the infected patients into the non-pneumonia group (asymptomatic and mild) and the pneumonia group (common, severe and critical), and found that elder people (RR = 1.04, 95 %CI: 1.001–1.08) and people with fever (RR = 10.33, 95 %CI: 2.75–38.78) were more likely to develop pneumonia and severe illness (Table 2 ).
Table 2.
Risk factors analysis of clinical outcome of the 59 infected patients.
| Factors | B | S.E. | Wald | df | Sig | Exp(B) | 95 %CI for Exp(B) |
|
|---|---|---|---|---|---|---|---|---|
| Lower | Upper | |||||||
| Sex | 0.06 | 0.60 | 0.01 | 1 | 0.91 | 1.07 | 0.33 | 3.43 |
| Age | 0.04 | 0.02 | 4.10 | 1 | 0.04 | 1.04 | 1.001 | 1.08 |
| Fever | 2.34 | 0.68 | 11.98 | 1 | 0.00 | 10.33 | 2.75 | 38.78 |
| Underlying diseases | 0.59 | 0.81 | 0.53 | 1 | 0.47 | 1.80 | 0.37 | 8.83 |
*CI: confidence interval.
4. Discussion
On January 23, 2020, Wuhan was closed. On January 25, 2020, the prevention and control strategy of “external defense input and internal non-proliferation” was adopted in Wuxi (Wuxi Municipal People’s Government, 2020). After a maximum incubation period of 14 days (from January 23, 2020), the number of cases decreased significantly, proving that the blockade of Wuhan was effective (Liu, Liao et al., 2020; Munster et al., 2020). COVID-19 was susceptible to infection in all age groups, and we found that most (80 %) of the 10 cases under 20 years old were mild and asymptomatic, whereas the critical cases were all over 60 years old, which was similar to the national situation reported earlier (Wu & McGoogan, 2020). The analysis of the characteristics of different age groups showed that the early imported cases in Wuxi were young and middle-aged, and the clinical severity was mainly normal type. All children cases, who were mainly asymptomatic infections and mild cases, were found in close contacts. All of them were the secondary cases of clusters in families, indicating that parents and family members were the main source of infection in children. Most cases aged 60 years or above were associated with underlying diseases, as well as the deterioration of immune function, resulting in relatively rapid disease progression and more severe clinical symptoms. Analysis of the risk factors for clinical outcomes of cases also confirmed that people with older age and fever were prone to cause pneumonia and severe illness, which was consistent with the previous studies (Deng et al., 2020; Liu, Tao et al., 2020).
Here we provided an assessment of time indicators and propagation dynamics to prove the effectiveness of our prevention and control measures. In our study, the mean time of the serial interval distribution was 6.31 day, which was similar to the previous study (7.5 day) (Li, Guan et al., 2020). The delays between the onset of illness and seeking medical attention in our city were generally shorter than that of Wuhan, with 65 % of patients seeking attention within 1 day after onset, and the delays to hospitalization were 50 % of patients being hospitalized 3 days after illness, which indicated that our measures of early detection of cases and asymptomatic infections through close screening were effective. In our study, we calculated two incubation periods. We estimated a mean incubation period of 4.77 days, which was slightly lower than previous studies (5.2 days and 5.1 days) (Lauer et al., 2020; Li, Guan et al., 2020), when the last exposure date was used as the first infection date. We also selected 9 patients infected after single exposure and calculated the mean incubation period to be much higher than that of the former, which might be more accurate. Although the sample size is small, these results might provide a clue for future research. The value of Rc was 1.12 in our manuscript, which was lower than the previously published estimates, ranging from 2.2 (95 % CI: 1.4–3.9) to 3.58 (95 %CI: 2.89–4.39) (Li, Guan et al., 2020; Tang et al., 2020; Zhao et al., 2020). In general, an epidemic would increase as long as Rc was greater than 1, and the control measures should reduce it to less than 1.
To date, we have reported 13 clusters with a number of cases ranging from 2 to 15, and 59 cases were involved, with an average of 4.38 reported cases per cluster. Of the 13 clusters, 11 were in families, 1 in the office and 1 in the same tour group. There were 23 secondary cases of local transmission, with an average secondary infection rate of 4.34 % (23/530). These positive individuals were mainly family members who lived and ate with each other, and we also found a super-spreading event at a family dinner party. During the Chinese New Year, people usually have many entertainment activities, such as attending cocktail parties, banquets, playing MahJong, traveling, etc. It suggested that eating and talking in closed spaces such as family rooms, hotel rooms and cabins might be risk factors for transmission through droplets and close contact (Jin et al., 2020). We found that 26 infections, who were the close contacts of the cases, were asymptomatic at the beginning, and 16 of them appeared symptoms after an average of 2.25 days (between 0–6 days), and 4 of them developed CT abnormalities first, and the rest developed symptom such as fever and cough. We isolated positive infections and further screened their close contacts to stop the infection chain. It showed that early concentrated isolation and screening of close contacts could effectively detect potential sources of infection, cut off transmission and effectively avoid community transmission. We also found that 85.71 % (6/7) of the third-generation cases were asymptomatic. It indicates that the virulence of the SARS-CoV-2 might decrease as it spreads.
In conclusion, our data supported the effectiveness of prevention and control measures. Through epidemiological investigations, we quarantined and tested all those exposed and in close contact with the infected persons, which could effectively prevent community transmission. Our study of family clusters provided further clues to the path of COVID-19 transmission, such as single exposure to meals in the family, playing cards in confined spaces, and eating and living together in the family. At the same time, we found that the third-generation cases had a higher proportion of asymptomatic cases. Our manuscript could provide some suggestions for policy adjustments in the prevention and control process of COVID-19, which was conducive to reduce the burden of disease and promote the healthy development of cities. However, to reduce panic and economic loss, and to manage and save the infected, much remains to be done. The goal is to break the transmission chain of COVID-19.
5. Conclusions
The COVID-19 epidemic in Wuxi city was mainly imported cases. The cases were mainly 20–60 years old. The clinical severity was mostly mild and normal, and asymptomatic infection accounted for 14.49 %. We found that aging and fever were risk factors for severe clinical outcome. Our study of family clusters provided further clues of the risk factors for COVID-19 transmission. Our data supported the effectiveness of prevention and control measures. The two results of incubation period were useful for current proposals of the length of quarantine, although longer monitoring periods might be justified.
Funding
This research was supported by Wuxi Project of Health Commission (No. Z201718, No. Z202019, No. Q202018, No. Z202007), Wuxi Key Medical Disciplines (No. ZDXK009), Wuxi Project of Youth Talent (No. QNRC008), Wuxi Suitable Technical Project of Health and Family Planning (No. T201819) and Wuxi Municipal Bureau on Science and Technology (No. N2020×001).
Availability of data and materials
All datasets used and analyzed during the study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
Data collection and analysis of cases and close contacts were determined by the National Health Commission of the People’s Republic of China to be part of a continuing public health outbreak investigation and were thus considered exempt from institutional review board approval.
Consent for publication
Not applicable.
Authors’ contributions
PS and YMG analyzed the data and wrote the manuscript. YS, EPC, JL and KWW conducted field investigation and data collection. HC and YJC conducted data analysis. YX was in charge of lab testing. CS and BL were the project coordinator, responsible for the project design and implementation, and supervised all aspects of fieldwork, laboratory activities and data analysis. All authors approved the final version of the paper. All authors have read and agreed to the published version of the manuscript.
Declaration of Competing Interest
The authors report no declarations of interest.
Acknowledgements
We thank seven Districts Center for Disease Control and Prevention and Wuxi No.5 People's Hospital for their help and contributions to this study.
References
- Anderson R.M., May R.M. Infectious diseases of humans: Dynamics and control. Oxford University Press. 1992;14(12):616. [Google Scholar]
- Deng Y., Liu W., Liu K., Fang Y.Y., Shang J., Zhou L.…Liu H.G. Clinical characteristics of fatal and recovered cases of coronavirus disease 2019 in Wuhan, China: A retrospective study. Chinese Medical Journal. 2020;133(11):1261–1267. doi: 10.1097/CM9.0000000000000824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guan W.J., Ni Z.Y., Hu Y., Liang W.H., Ou C.Q., He J.X.…Zhong N.S. Clinical characteristics of coronavirus disease 2019 in China. The New England Journal of Medicine. 2020;382(18):1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jin T., Li J., Yang J., Li J., Hong F., Long H.…Luo P. SARS-CoV-2 presented in the air of an intensive care unit (ICU) Sustainable Cities and Society. 2020 doi: 10.1016/j.scs.2020.102446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lauer S.A., Grantz K.H., Bi Q., Jones F.K., Zheng Q., Meredith H.R.…Lessler J. The incubation period of coronavirus disease 2019 (COVID-19) from publicly reported confirmed cases: Estimation and application. Annals of Internal Medicine. 2020;172(9):577–582. doi: 10.7326/M20-0504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Q., Guan X., Wu P., Wang X., Zhou L., Tong Y.…Feng Z. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. The New England Journal of Medicine. 2020;382(13):1199–1207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li R., Pei S., Chen B., Song Y., Zhang T., Yang W.…Shaman J. Substantial undocumented infection facilitates the rapid dissemination of novel coronavirus (SARS-CoV-2) Science (New York, NY) 2020;368(6490):489–493. doi: 10.1126/science.abb3221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liao J.Q., Fan S.B., Chen J., Wu J.L., Xu S.Q., Guo Y.M.…Liang C.H. Epidemiological and clinical characteristics of COVID-19 in adolescents and young adults. The Innovation. 2020;1(1) doi: 10.1016/j.xinn.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu J., Liao X., Qian S., Yuan J., Wang F., Liu Y.…Zhang Z. Community transmission of severe acute respiratory syndrome coronavirus 2, Shenzhen, China, 2020. Emerging Infectious Diseases. 2020;26(6):1320–1323. doi: 10.3201/eid2606.200239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu W., Tao Z.W., Wang L., Yuan M.L., Liu K., Zhou L.…Hu Y. Analysis of factors associated with disease outcomes in hospitalized patients with 2019 novel coronavirus disease. Chinese Medical Journal. 2020;133(9):1032–1038. doi: 10.1097/CM9.0000000000000775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munster V.J., Koopmans M., van Doremalen N., van Riel D., de Wit E. A novel coronavirus emerging in China - key questions for impact assessment. The New England Journal of Medicine. 2020;382(8):692–694. doi: 10.1056/NEJMp2000929. [DOI] [PubMed] [Google Scholar]
- National Health Commission of the People’s Republic of China . 2020. Law of the People’s Republic of China on the prevention and treatment of infectious diseases.http://www.nhc.gov.cn/xcs/zhengcwj/202001/44a3b8245e8049d2837a4f27529cd386.shtml/ (Accessed 11 October 2020) [Google Scholar]
- Sun C., Zhai Z. The efficacy of social distance and ventilation effectiveness in preventing COVID-19 transmission. Sustainable Cities and Society. 2020;62 doi: 10.1016/j.scs.2020.102390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang B., Wang X., Li Q., Bragazzi N.L., Tang S., Xiao Y.…Wu J. Estimation of the transmission risk of the 2019-nCoV and its implication for public health interventions. Journal of Clinical Medicine. 2020;9(2) doi: 10.3390/jcm9020462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tian H., Liu Y., Li Y., Wu C.H., Chen B., Kraemer M.U.G.…Dye C. An investigation of transmission control measures during the first 50 days of the COVID-19 epidemic in China. Science (New York, NY) 2020;368(6491):638–642. doi: 10.1126/science.abb6105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallinga J., Lipsitch M. How generation intervals shape the relationship between growth rates and reproductive numbers. Proceedings Biological Sciences. 2007;274(1609):599–604. doi: 10.1098/rspb.2006.3754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu Z., McGoogan J.M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: Summary of a report of 72 314 cases from the Chinese center for disease control and prevention. JAMA. 2020 doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- Wuxi Municipal People’s Government. (2020). http://www.wuxi.gov.cn/doc/2020/01/26/2769109.shtml/. (Accessed 11 October 2020).
- Zhao S., Lin Q., Ran J., Musa S.S., Yang G., Wang W.…Wang M.H. Preliminary estimation of the basic reproduction number of novel coronavirus (2019-nCoV) in China, from 2019 to 2020: A data-driven analysis in the early phase of the outbreak. International Journal of Infectious Diseases: IJID: Official Publication of the International Society for Infectious Diseases. 2020;92:214–217. doi: 10.1016/j.ijid.2020.01.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All datasets used and analyzed during the study are available from the corresponding author on reasonable request.