Abstract
The Coronavirus disease 2019 (COVID-19) pandemic, caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), is an international public health emergency. Although respiratory symptoms predominate the clinical manifestations of COVID-19, gastrointestinal symptoms have been observed in a subset of patients. Notably, some patients have nausea/vomiting as the first clinical manifestation of COVID-19, which is often overlooked by people. It is now clear that not only the lungs, the gastrointestinal tract could also be attacked by SARS-CoV-2. Its host receptor angiotensin-converting enzyme 2 (ACE2), which acts as a gateway to infection, has been found to be highly expressed in the gastrointestinal epithelium and may lead to the development of nausea/vomiting. Raise awareness of these symptoms and take timely intervention would help people combat the pandemic. This review discussed epidemiology, mechanisms, management, and prevention of COVID-19 related nausea and vomiting.
Keywords: COVID-19, Nausea, Vomiting, Epidemiology, Mechanism
Introduction
The Coronavirus disease 2019 (COVID-19) pandemic, caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has brought considerable morbidity and mortality since late December 2019 and continues threatening the whole world. As of September 6, 2020, more than 25 million confirmed cases and more than 876,616 deaths had been reported worldwide.1
SARS-CoV-2, an enveloped positive-sense, single-stranded RNA virus, belongs to the Sarbecovirus subgenus, along with SARS-CoV.2 The SARS-CoV-2 receptor is the angiotensin-converting enzyme 2 (ACE2) whose binding affinity for SARS-CoV-2 is 10–20 times higher than that for SARS-CoV.3 , 4 It is reported that ACE2 is abundantly expressed not only in lung alveolar type 2 cells and esophageal cells, but also on cells in gastrointestinal tract, including glandular cells of gastric, duodenal and rectal, absorptive enterocytes from the ileum and colon, making these tissues susceptible to infection by the virus.5 , 6 In the meantime, a growing number of studies have reported gastrointestinal symptoms in patients with COVID-19. Moreover, patients with gastrointestinal involvement had a higher prevalence of complications.7 Nausea and vomiting are the main gastrointestinal symptoms; nevertheless, the prevalence of nausea/vomiting is variable. The roles they play in COVID-19 are not entirely known. Here we review the epidemiology and possible mechanisms of nausea and vomiting in COVID-19 in order to better characterize these symptoms and to propose any effective measures for people in this public health crisis.
Epidemiology of COVID -19 associated nausea and vomiting
Many studies have shown that nausea and vomiting are not uncommon symptoms in COVID-19. One of the earliest studies analyzing gastrointestinal manifestations in 1141 patients hospitalized with COVID-19 in Wuhan reported that nausea was in 134 cases (11.7%) and vomiting was 119 (10.4%).8 In a multicenter cohort study enrolling 318 patients hospitalized with confirmed COVID-19 in the United States, nausea and vomiting occurred in 26.4% and 15.4% of patients respectively.9 Furthermore, the latest review and meta-analysis performed by the American Gastroenterological Association (AGA) institute showed that the pooled prevalence of nausea/vomiting was 7.8%.10 A similar result was observed in another systematic review and meta-analysis by Mao et al.7 They reported that the rate of nausea/vomiting was 7%. Compared with studies from China (5.2%), the pooled prevalence in studies from countries other than China was much higher: 14.9%.10 The frequency of nausea and vomiting being reported varies widely in different areas, indicating varied susceptibility of the individual digestive system. Of note, most of the studies were retrospective, which may have memory bias. Furthermore, many studies included inpatients but excluded the outpatients with perhaps milder symptoms, which makes it fail to estimate the actual prevalence of nausea and vomiting in COVID-19 patients.8 , 9 , 11, 12, 13
As for children with COVID-19, while most of them appeared to have a milder clinical course than sick adults, vomiting could also be seen in pediatric patients with a certain proportion (Table 1 ).14, 15, 16, 17, 18, 19, 20, 21, 22, 23 In a cohort of 171 infected children, vomiting and nausea were observed in 11 (6.4%) and 9 (5.3%) of the patients respectively.16 Analysis from the American Centers for Disease Control and Prevention suggested a higher rate of vomiting: 11% (31/291).14 In a systematic review of 62 studies, the prevalence of vomiting was 7.2%, which was similar to that of adults.7 , 24 Since children were less symptomatic than adults, the appearance of vomiting could be a warning of infection. In a case report article, Cai et al. described 5 cases of children with COVID-19 who showed non-respiratory symptoms as the first manifestation.25 Among them, two children showed vomiting before admission.
Table 1.
Vomiting in pediatric patients with COVID-19.
| Study | Country | Age | N | N (%) of vomiting | N (%) of family contact |
|---|---|---|---|---|---|
| CDC14 | USA | Median 11 years (0–17 years) | 291 | 31 (11%) | 168 (58%) |
| Xiong et al.15 | China | 0–18 years | 244 | 23 (9%) | 208 (85%) |
| Lu et al.16 | China | Median 6.7 year (1 day–15 years) | 171 | 11 (6%) | 154 (90%) |
| Parri et al.17 | Italy | Median 3.3 years (0–17.5 years) | 100 | 10 (10%) | 45 (45%) |
| de Ceano-Vivas et al.18 | Spain | Median 35.5 months (3.3 months–146 months) | 58 | 9 (15%) | 30 (51%) |
| Qiu et al.19 | China | Mean 8.3 years (1–16 years) | 36 | 2 (5%) | 32 (89%) |
| Zhang et al.20 | China | Median 33 months (10–94 months) | 34 | 4 (12%) | 13 (38%) |
| Zheng et al.21 | China | Median 3 years (3 months–14 years) | 25 | 2 (8%) | 21 (84%) |
| Xia et al.22 | China | Median 2.1 (0–14 years) | 20 | 2 (10%) | 13 (65%) |
| Tan et al.23 | China | Median 7.5 years (13 months–12 years) | 10 | 1 (10%) | 9 (90%) |
a: Single case reports and small case series (<10 cases)are not included in this table.
N: Number.
It is worth mentioning that nausea and vomiting might be the initial symptoms in COVID-19. A case report showed that a 68-year-old male was admitted to the hospital for “paroxysmal vomiting for seven days, fever for one day”. After admission, he still had vomiting without diarrhea or other respiratory symptoms. Later on, he was diagnosed with SARS-CoV-2 infection.26 Similarly, according to the first confirmed case of SARS-CoV-2 infection in the United States, the patient reported a 2-day history of nausea and vomiting on admission.27 Furthermore, regardless of hospitalization status, the prevalence of nausea/vomiting as one of the initial symptoms was estimated to 7.6% by AGA.10 Among 1141 patients with COVID-19 in Hubei, 183 (16%) patients presented with gastrointestinal symptoms only without respiratory features of which nausea and vomiting accounted for about two thirds.8 Conversely, in a study regarding 116 American patients with confirmed COVID-19, none of the patients showed isolated gastrointestinal symptoms or had gastrointestinal symptoms as an initial symptom.28 However, in a retrospective study by Lin et al., nausea was one of the main symptoms occurring in 17/95 patients (17.9%) with three (3.2%) cases occurred on the illness onset.29 Among these 17 patients, 2 cases did not have any CT imaging features of COVID-19 pneumonia. These findings indicate that the symptoms of COVID-19 can be atypical. Meanwhile, nausea and vomiting should not be overlooked, especially for those who live in high-risk areas.
Conflicting results about nausea and vomiting in severe and non-severe cases have been reported. Yan et al. found that there was no significant difference in nausea/vomiting between severe and non-severe patients (nausea 8.3% vs 4.5%; vomiting 2.3% vs 11.1%).30 Another study reported similar results: the incidence rates of nausea/vomiting between ICU patients and non-ICU patients were not statistically different.13 On the contrary, Chen et al. reported that nausea and vomiting were more common in mild group.31 Similarly, Zhang et al. reported that the proportion of nausea in non-severe patients (23.2%) was significantly higher than that in severe patients (8.8%).32
Of note, it is quite challenging to compare the rates of nausea and vomiting between studies. The definitions of nausea and vomiting are relatively vague and subjective.33 There are no objective data or images to confirm the judgment. Since we lack precise diagnostic criteria for nausea and vomiting, it mainly depends on the patients’ subjective feelings to judge and to evaluate these symptoms, which may be inaccurate due to memory bias and individual tolerance.34 Moreover, criteria for diagnosing nausea and vomiting may be inconsistent among hospitals, which may affect the final diagnosis by clinicians.35 In summary, the differences in the incidence of nausea and vomiting between studies were partly attributable to subjective factors.
Pathogenesis of COVID -19 associated nausea and vomiting
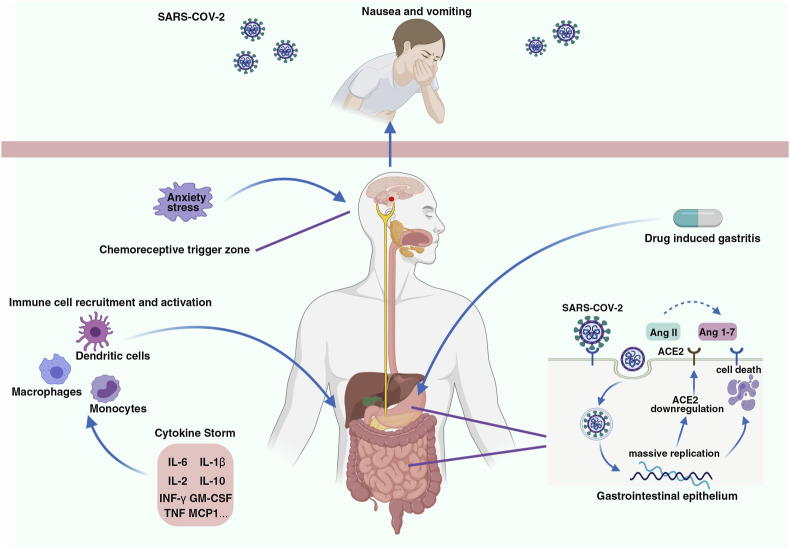
Although the specific mechanisms involved in COVID -19 associated nausea and vomiting are not entirely known, some theories of the viral infection could explain this phenomenon (Fig. 1 ).
Figure 1.
Possible reasons for COVID -19 associated nausea and vomiting. Many reasons can probably cause nausea and vomiting in COVID-19, including ACE2-mediated SARS-CoV-2 invasion of gastrointestinal epithelium, systemic inflammatory response, drug side effects and psychological distress. Afferent pathways arise from the gastrointestinal tract, as well as signals from the chemoreceptor trigger zone and cerebral cortex, stimulating the emetic center and triggering nausea and vomiting. Abbreviations: Ang II: Angiotensin II; Ang 1–7: Angiotensin-(1–7), Created with Biorender.com.
ACE2-mediated direct SARS-CoV-2 invasion of gastrointestinal epithelium
ACE2, the functional receptor of SARS-CoV-2, facilitates viral entry into the host's cells.36 Meanwhile, as a vital metalloproteinase, ACE2 could convert angiotensin II (Ang II) to angiotensin-(1–7), leading to protective effects on tissues such as anti-inflammation, anti-oxidant, and so on.37
SARS-CoV-2 spike (S) protein binds to ACE2 and in concert with host cell proteases transmembrane serine protease 2 (TMPRSS2), which plays a crucial role cleaving S protein, to invade the cells.36 In a single-cell transcriptomic analysis, ACE2 and TMPRSS2 were highly expressed in gastrointestinal tract epithelium.6 Using confocal- and electron-microscopy, Lamers et al. observed that SARS-CoV-2 could productively infect human gut enterocytes.3 They also found that low levels of ACE2 may be sufficient for viral entry. It is reported that SARS-CoV-2 was localized in the cytoplasm of gastric, duodenal, and rectum glandular epithelial cells.5 These findings suggest that SARS-CoV-2 can actively invade the gastrointestinal tract, which highly expresses ACE2.
If the immune system cannot defeat the infection, then SARS-CoV-2 will actively replicate. The massive replication of the virus will decrease the level of ACE2 and destroy the host's cells. In the meantime, downregulation of ACE2 leads to decreased organ protection.38 As a result, the gastrointestinal function is ruined and inflammation is accelerated.
Therefore, nausea and vomiting may be caused by the virus attacking the gastrointestinal tract.
Injury of gastrointestinal system through immune response and inflammatory reactions
The antiviral responses of human immune system, including the production of proinflammatory cytokines and chemokines, the activation of CD4+ Th1 and CD8+ T cells cellular response, results in viral clearance in mild cases.39 However, in severe cases, the tissue injury caused by the virus could activate monocytes, macrophages and dendritic cells with excessive amounts of proinflammatory cytokines (including IL-6, IL-8I, IL-1β, IL-2, IL-17, G-CSF, GM-CSF, IP10, MCP1, MIP1α, TNF), leading to cytokine storm syndrome.39, 40, 41 The systemic inflammatory response could damage many organs and systems in the body, including the digestive system.40 , 41 Although no studies have reported the levels of cytokines in the gastrointestinal tract of nausea/vomiting patients with COVID-19, several studies have suggested that the digestive system is very likely to be injured by the chain reactions of inflammatory factors. A retrospective analysis of 409 severe patients with COVID-19 found that peripheral cytokine levels of IL-6, IL-10 and TNF-α were significantly increased in patients with diarrhea.42 Xiao et al. also found that occasional lymphocyte infiltration in the esophageal squamous epithelium and a large number of infiltrating plasma cells and lymphocytes, interstitial edema could be seen in the lamina propria of the stomach, duodenum and rectum.5
Other possible impact factors of nausea and vomiting
Adverse effects of COVID-19 treatments
Some patients with COVID-19 presented with nausea and vomiting during hospitalization, which may be related to the adverse effects of treatments. After receiving remdesivir, 2 of the first 7 patients hospitalized with COVID-19 showed nausea, which had not been observed before the application.43 One randomized, controlled trial conducted by Cao et al. included 199 hospitalized patients with severe COVID-19, of which 99 received treatment to lopinavir/ritonavir and 100 to the standard-care group for 14 days.44 There were 9.5% (9/99) with nausea and 6.3% (6/99) with vomiting, while there was no one who had nausea/vomiting in the standard-care group. Gastrointestinal adverse events were the most common ones and were the primary reason for discontinuing the full 14-day course.
Stress and pressure
Anxiety and stress, psychological distress brought by COVID-19, are of concern worldwide lately, which are also common causes of nausea and vomiting.33 Underneath the medical crisis, long-term social isolation and the economic burden, people remain at high risk of having mental health problems, especially for the vulnerable ones such as healthcare workers, children and the elderly.45 National surveys reveal a high prevalence of distress in the population during COVID-19, which is 35%–60%.45 A study including 1210 respondents from 194 cities in China showed that 28.8% reported moderate to severe anxiety symptoms.46 A prospective case–control study from the United States showed that among the outpatients during the COVID-19 pandemic, nausea and vomiting are common in outpatients who tested negative for COVID-19:26% and 12% respectively.47 While there is yet no specific data of nausea and vomiting in people with anxiety, psychological factors do play an important role in people's illness and should be regarded with certain care during the COVID-19 pandemic.
Management and prevention of COVID -19 associated nausea and vomiting
Clinicians should pay particular attention to nausea and vomiting during the COVID-19 pandemic. For people who already showed nausea and vomiting, physicians should acquire detailed information about the history of high-risk contact and symptoms associated with COVID-19, including cough, shortness of breath, difficulty breathing, fever, chills, muscle pain, sore throat, and new loss of taste or smell. If outpatients only present with nausea/vomiting or other gastrointestinal symptoms, a few days of monitoring will be necessary, as nausea and vomiting might be the initial symptoms of COVID-19. For those who only presented with nausea/vomiting but are at high-risk areas or with high-risk factors of COVID-19 such as advanced age and heart or lung disease, COVID-19 testing should be considered.10 Besides, in the face of patients with a history of nausea/vomiting, treatment with drugs having potential gastrointestinal adverse effects should be taken into more consideration.44
To date, safe and effective vaccines for COVID-19 are not available; however, at least 176 candidates are in clinical and preclinical evaluation, with nine new coronal vaccines in phase III clinical trials.48 Recently, three early-phase trials of adenovirus-vectored COVID-19 vaccine candidates have been reported in The Lancet, showing satisfactory immunogenicity, which is encouraging, whereas the clinical efficacy and safety still awaits for large scale clinical trials to confirm.49, 50, 51 Therefore, the current key measures lie in prevention, monitoring and timely intervention.52 The best way to protect people from infection is to avoid being exposed to SARS-CoV-2. Moreover, during COVID-19, for those who are under great pressure, for example, workers in health and long-term care, timely psychological support is essential.45
Conclusions
The ongoing COVID-19 pandemic requires long-term vigilance and strategies for fighting the virus. Nausea and vomiting are not uncommon symptoms for both adults and children during the COVID-19 and they can be the initial symptoms for SARS-CoV-2 infection. Many reasons can probably cause nausea and vomiting, including virus infection, systemic inflammatory response, drug side effects and psychological distress. To date, effective vaccines or treatments for SARS-CoV-2 are not available. Thus timely intervention and precautions are the key measures to control the COVID-19 pandemic. Also, psychological support is quite essential. Recognizing characteristics of nausea and vomiting can raise the suspicion of COVID-19, leading to early testing and diagnosis of the disease, and help people fight the virus in the long run.
Acknowledgments
Research was supported by grants from the National Key Research and Development Program of China 2018YFC1312103 (L.X.), National Natural Science Foundation of China No. 81972237 (L.X.), and No. 81772623 (L.X.).
References
- 1.WHO WHO coronavirus disease (COVID-19) dashboard. https://covid19.who.int/
- 2.Zhu N., Zhang D., Wang W., Li X., Yang B., Song J. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382(8):727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lamers M.M., Beumer J., van der Vaart J., Knoops K., Puschhof J., Breugem T.I. SARS-CoV-2 productively infects human gut enterocytes. Science. 2020:eabc1669. doi: 10.1126/science.abc1669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wrapp D., Wang N., Corbett K.S., Goldsmith J.A., Hsieh C.-L., Abiona O. Cryo-EM structure of the 2019-nCoV spike in the prefusion conformation. Science. 2020;367(6483):1260–1263. doi: 10.1126/science.abb2507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Xiao F., Tang M., Zheng X., Liu Y., Li X., Shan H. Evidence for gastrointestinal infection of SARS-CoV-2. Gastroenterology. 2020;158(6) doi: 10.1053/j.gastro.2020.02.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhang H., Kang Z., Gong H., Xu D., Wang J., Li Z. Digestive system is a potential route of COVID-19: an analysis of single-cell coexpression pattern of key proteins in viral entry process. Gut. 2020;69(6):1010–1018. doi: 10.1136/gutjnl-2020-320953. [DOI] [Google Scholar]
- 7.Mao R., Qiu Y., He J.-S., Tan J.-Y., Li X.-H., Liang J. Manifestations and prognosis of gastrointestinal and liver involvement in patients with COVID-19: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2020 doi: 10.1016/S2468-1253(20)30126-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Luo S., Zhang X., Xu H. Don't overlook digestive symptoms in patients with 2019 novel coronavirus disease (COVID-19) Clin Gastroenterol Hepatol. 2020 doi: 10.1016/j.cgh.2020.03.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Redd W.D., Zhou J.C., Hathorn K.E., McCarty T.R., Bazarbashi A.N., Thompson C.C. Prevalence and characteristics of gastrointestinal symptoms in patients with SARS-CoV-2 infection in the United States: a multicenter cohort study. Gastroenterology. 2020 doi: 10.1053/j.gastro.2020.04.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sultan S., Altayar O., Siddique S.M., Davitkov P., Feuerstein J.D., Lim J.K. AGA institute rapid review of the GI and liver manifestations of COVID-19, meta-analysis of international data, and recommendations for the consultative management of patients with COVID-19. Gastroenterology. 2020 doi: 10.1053/j.gastro.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Guan W.-J., Ni Z.-Y., Hu Y., Liang W.-H., Ou C.-Q., He J.-X. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ai J., Chen J., Wang Y., Liu X., Fan W., Qu G. The cross-sectional study of hospitalized coronavirus disease 2019 patients in Xiangyang, Hubei province. medRxiv. 2020 doi: 10.1101/2020.02.19.20025023. 2020.2002.2019.20025023. [DOI] [Google Scholar]
- 13.Wang D., Hu B., Hu C., Zhu F., Liu X., Zhang J. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. J Am Med Assoc. 2020 doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Coronavirus disease 2019 in children - United States, February 12-April 2, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(14):422–426. doi: 10.15585/mmwr.mm6914e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Xiong X.-l., Wong K.K.-y., Chi S.-q., Zhou A.-f., Tang J.-q., Zhou L.-s. Comparative study of the clinical characteristics and epidemiological trend of 244 COVID-19 infected children with or without GI symptoms. Gut. 2020 doi: 10.1136/gutjnl-2020-321486. gutjnl-2020-321486. [DOI] [PubMed] [Google Scholar]
- 16.Lu X., Zhang L., Du H., Zhang J., Li Y.Y., Qu J. SARS-CoV-2 infection in children. N Engl J Med. 2020;382(17):1663–1665. doi: 10.1056/NEJMc2005073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Parri N., Lenge M., Buonsenso D. Children with covid-19 in pediatric emergency departments in Italy. N Engl J Med. 2020 doi: 10.1056/NEJMc2007617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.de Ceano-Vivas M., Martín-Espín I., Del Rosal T., Bueno-Barriocanal M., Plata-Gallardo M., Ruiz-Domínguez J.A. SARS-CoV-2 infection in ambulatory and hospitalised Spanish children. Arch Dis Child. 2020 doi: 10.1136/archdischild-2020-319366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Qiu H., Wu J., Hong L., Luo Y., Song Q., Chen D. Clinical and epidemiological features of 36 children with coronavirus disease 2019 (COVID-19) in Zhejiang, China: an observational cohort study. Lancet Infect Dis. 2020 doi: 10.1016/S1473-3099(20)30198-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhang C., Gu J., Chen Q., Deng N., Li J., Huang L. Clinical and epidemiological characteristics of pediatric SARS-CoV-2 infections in China: a multicenter case series. PLoS Med. 2020;17(6) doi: 10.1371/journal.pmed.1003130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zheng F., Liao C., Fan Q.-H., Chen H.-B., Zhao X.-G., Xie Z.-G. Clinical characteristics of children with coronavirus disease 2019 in Hubei, China. Curr Med Sci. 2020;40(2):275–280. doi: 10.1007/s11596-020-2172-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Xia W., Shao J., Guo Y., Peng X., Li Z., Hu D. Clinical and CT features in pediatric patients with COVID-19 infection: different points from adults. Pediatr Pulmonol. 2020;55(5):1169–1174. doi: 10.1002/ppul.24718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tan Y.-P., Tan B.-Y., Pan J., Wu J., Zeng S.-Z., Wei H.-Y. Epidemiologic and clinical characteristics of 10 children with coronavirus disease 2019 in Changsha, China. J Clin Virol. 2020;127:104353. doi: 10.1016/j.jcv.2020.104353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Liguoro I., Pilotto C., Bonanni M., Ferrari M.E., Pusiol A., Nocerino A. SARS-COV-2 infection in children and newborns: a systematic review. Eur J Pediatr. 2020 doi: 10.1007/s00431-020-03684-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cai X., Ma Y., Li S., Chen Y., Rong Z., Li W. Clinical characteristics of 5 COVID-19 cases with non-respiratory symptoms as the first manifestation in children. Front Pediat. 2020;8(258) doi: 10.3389/fped.2020.00258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fu B., Qian K., Fu X. SARS-CoV-2-Induced vomiting as onset symptom in a patient with COVID-19. Dig Dis Sci. 2020;65(6):1568–1570. doi: 10.1007/s10620-020-06285-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Holshue M.L., DeBolt C., Lindquist S., Lofy K.H., Wiesman J., Bruce H. First case of 2019 novel coronavirus in the United States. N Engl J Med. 2020;382(10):929–936. doi: 10.1056/NEJMoa2001191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cholankeril G., Podboy A., Aivaliotis V.I., Tarlow B., Pham E.A., Spencer S. High prevalence of concurrent gastrointestinal manifestations in patients with SARS-CoV-2: early experience from California. Gastroenterology. 2020 doi: 10.1053/j.gastro.2020.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lin L., Jiang X., Zhang Z., Huang S., Zhang Z., Fang Z. Gastrointestinal symptoms of 95 cases with SARS-CoV-2 infection. Gut. 2020;69(6):997–1001. doi: 10.1136/gutjnl-2020-321013. [DOI] [PubMed] [Google Scholar]
- 30.Yan S., Song X., Lin F., Zhu H., Wang X., Li M. medRxiv; 2020. Clinical characteristics of coronavirus disease 2019 in Hainan, China. 2020.2003.2019.20038539. [DOI] [Google Scholar]
- 31.Chen X., Zheng F., Qing Y., Ding S., Yang D., Lei C. Epidemiological and clinical features of 291 cases with coronavirus disease 2019 in areas adjacent to Hubei, China: a double-center observational study. medRxiv. 2020 doi: 10.1101/2020.03.03.20030353. 2020.2003.2003.20030353. [DOI] [Google Scholar]
- 32.Zhang J.-J., Dong X., Cao Y.-Y., Yuan Y.-D., Yang Y.-B., Yan Y.-Q. Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China. Allergy. 2020 doi: 10.1111/all.14238. [DOI] [PubMed] [Google Scholar]
- 33.Quigley E.M., Hasler W.L., Parkman H.P. AGA technical review on nausea and vomiting. Gastroenterology. 2001;120(1):263–286. doi: 10.1053/gast.2001.20516. [DOI] [PubMed] [Google Scholar]
- 34.Klopfenstein T., Kadiane-Oussou N.d.J., Royer P.-Y., Toko L., Gendrin V., Diarrhea S. Zayet. An underestimated symptom in Coronavirus disease 2019. Clin Res Hepatol Gastroenterol. 2020 doi: 10.1016/j.clinre.2020.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Liu Y., Xiang L., Deng K. Focusing on gastrointestinal symptoms in COVID-19 is far from enough. Gastroenterology. 2020 doi: 10.1053/j.gastro.2020.05.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hoffmann M., Kleine-Weber H., Schroeder S., Krüger N., Herrler T., Erichsen S. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020;181(2) doi: 10.1016/j.cell.2020.02.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Renu K., Prasanna P.L., Valsala Gopalakrishnan A. Coronaviruses pathogenesis, comorbidities and multi-organ damage - a review. Life Sci. 2020;255:117839. doi: 10.1016/j.lfs.2020.117839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Xiao L., Sakagami H., Miwa N. ACE2: the key molecule for understanding the pathophysiology of severe and critical conditions of COVID-19: demon or angel? Viruses. 2020;12(5) doi: 10.3390/v12050491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Oberfeld B., Achanta A., Carpenter K., Chen P., Gilette N.M., Langat P. SnapShot: COVID-19. Cell. 2020;181(4) doi: 10.1016/j.cell.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Shimabukuro-Vornhagen A., Gödel P., Subklewe M., Stemmler H.J., Schlößer H.A., Schlaak M. Cytokine release syndrome. J Immunother Cancer. 2018;6(1):56. doi: 10.1186/s40425-018-0343-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Respiratory virus infections: Understanding COVID-19. Immunity. 2020 doi: 10.1016/j.immuni.2020.05.004. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zhang L., Han C., Zhang S., Duan C., Shang H., Bai T. Diarrhea and altered inflammatory cytokine pattern in severe coronavirus disease 2019: impact on disease course and in-hospital mortality. J Gastroenterol Hepatol. 2020 doi: 10.1111/jgh.15166. [DOI] [PubMed] [Google Scholar]
- 43.Kujawski S.A., Wong K.K., Collins J.P., Epstein L., Killerby M.E., Midgley C.M. First 12 patients with coronavirus disease 2019 (COVID-19) in the United States. medRxiv. 2020 doi: 10.1101/2020.03.09.20032896. 2020.2003.2009.20032896. [DOI] [PubMed] [Google Scholar]
- 44.Cao B., Wang Y., Wen D., Liu W., Wang J., Fan G. A trial of lopinavir-ritonavir in adults hospitalized with severe covid-19. N Engl J Med. 2020;382(19):1787–1799. doi: 10.1056/NEJMoa2001282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Nations U., UNITED Nations Policy B.R.I.E.F. COVID-19 and the need for action ON mental health. https://www.un.org/sites/un2.un.org/files/un_policy_brief-covid_and_mental_health_final.pdf
- 46.Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Publ Health. 2020;17(5) doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Chen A., Agarwal A., Ravindran N., To C., Zhang T., Thuluvath P.J. Are gastrointestinal symptoms specific for COVID-19 infection? A prospective case-control study from the United States. Gastroenterology. 2020 doi: 10.1053/j.gastro.2020.05.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.WHO. Draft landscape of COVID-19 candidate vaccines. https://www.who.int/publications/m/item/draft-landscape-of-covid-19-candidate-vaccines
- 49.Folegatti P.M., Ewer K.J., Aley P.K., Angus B., Becker S., Belij-Rammerstorfer S. Safety and immunogenicity of the ChAdOx1 nCoV-19 vaccine against SARS-CoV-2: a preliminary report of a phase 1/2, single-blind, randomised controlled trial. Lancet. 2020;396(10249):467–478. doi: 10.1016/S0140-6736(20)31604-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Zhu F.-C., Li Y.-H., Guan X.-H., Hou L.-H., Wang W.-J., Li J.-X. Safety, tolerability, and immunogenicity of a recombinant adenovirus type-5 vectored COVID-19 vaccine: a dose-escalation, open-label, non-randomised, first-in-human trial. Lancet. 2020;395(10240):1845–1854. doi: 10.1016/S0140-6736(20)31208-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Logunov D.Y., Dolzhikova I.V., Zubkova O.V., Tukhvatullin A.I., Shcheblyakov D.V., Dzharullaeva A.S. Safety and immunogenicity of an rAd26 and rAd5 vector-based heterologous prime-boost COVID-19 vaccine in two formulations: two open, non-randomised phase 1/2 studies from Russia. Lancet. 2020;396(10255):887–897. doi: 10.1016/S0140-6736(20)31866-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Cao W., Li T. COVID-19: towards understanding of pathogenesis. Cell Res. 2020;30(5):367–369. doi: 10.1038/s41422-020-0327-4. [DOI] [PMC free article] [PubMed] [Google Scholar]