Abstract
Purpose
To report trends in real-world outcomes of anti-vascular endothelial growth factor (anti-VEGF) therapy for neovascular age-related macular degeneration (nAMD) in the United Kingdom (UK) over the last decade.
Design
Systematic review.
Methods
Medline, PubMed, and Embase databases were searched from 9 April 2010 to 8 April 2020 for publications that met the inclusion criteria: treatment-naïve eyes, UK-only data and ≥1 year of follow-up. ICHOM (International Consortium for Health Outcome Measures) outcomes and study quality were assessed. Visual acuity (VA) trends were assessed in studies with ≥100 eyes at baseline.
Results
Twenty-six studies (n=25,761 eyes) were included, meeting 14–17 out of 20 Institute of Health Economics Quality Appraisal of Case Series checklist domains. Only ranibizumab and aflibercept outcome data were available. The mean injection number in the first year of treatment was 5.9 in publications from 2010 to 2015 and 7.1 from 2015 to 2020. Average baseline VA and mean one-year, two-year and three-year VA gains gradually improved over the last decade. Longer-term studies reported that the visual gains achieved in the first year of treatment were rarely maintained, with under-treatment a likely contributing factor.
Conclusion
UK real-world outcomes have improved over the last decade with improved service delivery and the adoption of more proactive treatment regimens but are still not always as impressive as registration clinical trial results. Access to longer-acting anti-VEGF therapies would reduce the treatment burden for patients, carers, and the healthcare system, potentially making replication of clinical trial results possible in the NHS.
Keywords: anti-vascular endothelial growth factor, anti-VEGF, macular degeneration, treatment, systematic review, aflibercept, ranibizumab, intravitreal therapy
Introduction
Age-related macular degeneration (AMD) is a leading cause of blindness, accounting for approximately 7% of all cases worldwide,1,2 and in 2017, the European Society of Retina Specialists (EURETINA) estimated that around 4 million people were living with AMD in the United Kingdom (UK).3 Its prevalence is set to rise as the world’s population ages: it is estimated that 288 million people globally would have either an early or late manifestation of AMD by the year 2040.4 Late disease is characterized by a significant loss of central vision gradually due to geographic atrophy, or more rapidly from development of neovascular AMD (nAMD; also termed “exudative” or “wet” AMD).5 It is estimated that 40,000 new cases of nAMD develop each year in the UK. Unlike geographic atrophy, treatments are currently available for nAMD.6
The last 10–15 years have seen a transformation in how nAMD is managed. The introduction of intravitreally administered anti-VEGF drugs has transformed the treatment of nAMD, moving away from an era where laser photocoagulation and verteporfin photodynamic therapy were administered in an attempt to reduce the rate at which vision was lost, to a world where improved visual and morphologic outcomes are regularly achieved, with a corresponding fall in the rate of nAMD-related blindness.7–14
There is seldom a drug that performs better in clinical practice than in clinical trials. There are multiple reasons for this phenomenon. Patients tend to be carefully selected for inclusion in clinical trials and dosing regimens are strictly adhered to. Real-world clinical practice involves the treatment of many patients who would never have been included in these trials and the same treatment protocols are often not applied.15 Patients miss appointments for many reasons and therefore lose the opportunity to be treated with an effective drug on time, with the outcome that their vision suffers. Additionally, restrictions on public funding limit clinic capacity and availability of licensed drugs to patients often until visual acuity (VA) has deteriorated to less than the driving standard.16 These phenomena help explain the global gap in performance between clinical trials and real-world clinical practice for anti-VEGF drugs used for the treatment of nAMD.17,18
To better understand the real-world situation in the UK, we performed a systematic review to assess trends in outcomes over the last decade and identify whether registration clinical trial outcomes of intravitreal anti-VEGF therapy for neovascular AMD have been replicated in UK NHS practice.
Methods
A systematic literature search was conducted on studies published from 9 April 2010 to 8 April 2020, using Medline, PubMed, and Embase library databases. The following multipurpose (.mp) search terms and Medical Subject Headings (MeSH) terms where available were used: macular degeneration, age related macula degeneration, AMD, nAMD, neovascular, wet, VEGF, anti-VEGF, ranibizumab, Lucentis, aflibercept, Eylea, bevacizumab, Avastin, visual acuity, visual outcomes, vision, ocular, blindness, registry, database, long term study/studies, observational study/studies, Phase IV study/studies, real world, real-world, United Kingdom, UK, Scotland, Wales, Northern Ireland, England. Further references were identified by manually searching included articles and consulting experts in the field. Real-world studies of intravitreal ranibizumab, aflibercept and bevacizumab therapy for nAMD published before the search date were included.
Included studies were required to have at least 1 year of follow-up data, and eyes were required to be treatment naïve; switching studies were, therefore, excluded. Randomized clinical trial results and meeting abstracts were excluded. Only studies with UK data were included and, therefore, were all English language articles. The supplementary figure 1 summarises the selection of included studies. It was pre-specified that analysis of VA trends would be restricted to studies that contained ≥100 eyes at baseline. The year of publication of the study was recorded to enable comparison of outcomes published in the first half of the decade (9 April 2010 to 8 April 2015) and the second half of the decade (9 April 2015 to 8 April 2020).
Data extraction and quality assessment of the original studies were performed independently by two authors (LK, PZ). Outcome measures were cross-referenced against the ICHOM (International Consortium for Health Outcome Measures) checklist, and the quality of each study was assessed using the quality appraisal checklist for case series developed by the Institute of Health Economics (IHE)19 as this is preferred tool of the National Institute for Health and Care Excellence (NICE).20
Results
We identified 26 real-world published studies with 25,761 eyes meeting the inclusion criteria (Supplementary Table 1).21–47 There were 13 studies with ≥100 eyes at baseline and reporting relevant VA outcomes representing 23,464 eyes. Only ranibizumab and aflibercept outcome data was available.
Baseline Visual Acuity
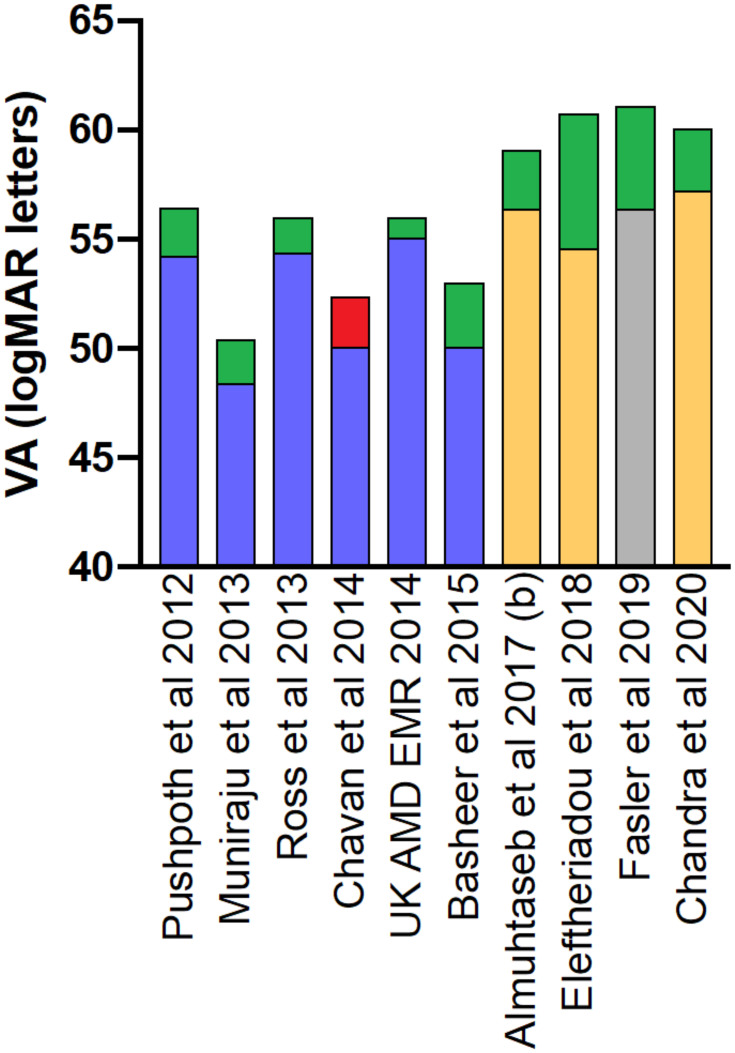
The mean baseline VA ranged from 48 to 57 letters in included studies. The mean baseline VA in general improved over the course of the decade (Figure 1). There does appear to be variation in baseline VA between centres even when data was collected and published at similar times.
Figure 1.
Visual acuity (VA) outcomes of intravitreal anti-VEGF therapy for nAMD at baseline and 1 year. Only real-world studies with ≥100 eyes at baseline are included. The year of publication is later than the date of acquisition of data for all studies. Blue indicates ranibizumab treated eyes. Orange indicates aflibercept treated eyes. Grey indicates that combined data for ranibizumab and aflibercept treated eyes was reported. Green indicates mean visual gain from baseline. Red indicates mean visual loss from baseline.
Visual Acuity Outcomes
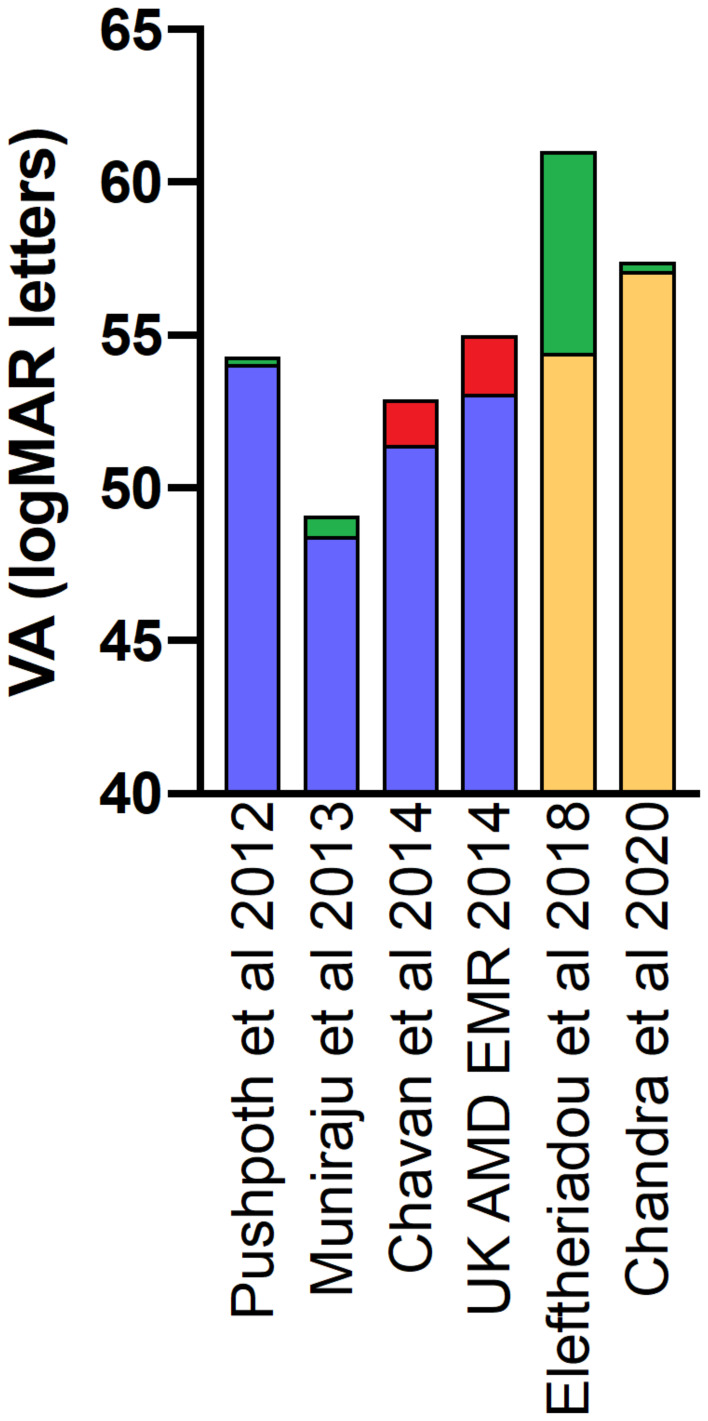
The mean visual gains from baseline levels to 1 year, where recorded, ranged from −1.3 to +8.0 logMAR letters, with more significant visual gains being observed in studies that reported outcomes in the latter half of the decade than the former (Figure 1). A similar trend was seen in the subset of studies that reported 2-year VA data (Figure 2).
Figure 2.
Visual acuity (VA) outcomes of intravitreal anti-VEGF therapy for nAMD at baseline and 2 years. Only real-world studies with ≥100 eyes at baseline are included. The year of publication is later than the date of acquisition of data for all studies. Blue indicates ranibizumab treated eyes. Orange indicates aflibercept treated eyes. Green indicates mean visual gain from baseline. Red indicates mean visual loss from baseline.
A number of included real-world studies stratified visual outcomes according to baseline VA. The UK AMD EMR study, with over 8000 eyes at baseline was the largest study to report on the impact of baseline VA on final VA. The included studies consistently reported that those eyes with worse baseline VA achieved greater gains in relative vision, but the final VA outcome was worse than those eyes that commenced treatment with good VA.46
The ICHOM recommended minimum dataset was only published in 2016.48 As well as baseline VA and mean VA gain, it is recommended 15-letter gain and loss from baseline and maintenance of driving-level vision (6/12 or better) are recorded. These parameters were not consistently reported even in studies published after 2016 (Supplementary Table 1). The percentage of treated eyes with >15-letter loss at 1 year ranged from between 5.6% to 10% in included UK real-world studies and by 2 years this ranged from 9.2% to 18% (Table 1). The percentage of treated eyes with VA >70 letters at baseline ranged from 3.3% to 32.2% in included studies with a clear trend for improvement over the decade. Similarly, the percentage of eyes with >70 letter at 1 and 2 years increased with improving baseline vision (Table 2).
Table 1.
Percentage of Eyes Losing >15 Letters from Baseline VA
| Study | >15 Letter Loss at End of Year 1 | >15 Letter Loss at End of Year 2 |
|---|---|---|
| Pushpoth et al 201244 | 9.5 | 14.6 |
| Ross et al 201345 | 9.9 | N/R |
| Muniraju et al 201332 | 9.8 | 14.4 |
| UK AMD EMR. 201446 | 10 | 18 |
| Basheer et al 201522 | 8.1 | 11.5 |
| Talks et al 201636 | 8 | N/A |
| Eleftheriadou et al 201826 | 6.8 | 9.2 |
| Chandra et al 202041 | 5.6 | 13.3 |
Notes: It should be noted that baseline characteristics will be different between real-world studies and compared with registration clinical trials. The percentage of eyes losing >15 letters at 2 years was approximately 9% in the MARINA registration trial for ranibizumab. In the integrated analysis of 2-year VIEW 1 and 2 data, 7.6% of eyes lost >15 letters from baseline.
Abbreviations: N/R, not reported; N/A, not applicable.
Table 2.
Percentage of Eyes with Driving Level VA at Baseline and 1 and 2-Year Follow-Up
| Study | >70 Letters at Baseline | >70 Letters at Year 1 | >70 Letters at Year 2 |
|---|---|---|---|
| Pushpoth et al 2013*44 | 6.4% | 31.3% | 17.2% |
| Ross et al 201345 | 11.3% | – | – |
| Chavan et al 2014** 25 | 3.3% | 6.7% | 7.9% |
| Buckle et al 2016 24 | 16.9% | 17.0% | 15.9% |
| Talk et al 2016 36 | 16.4% | 33.7% | – |
| Almuhtaseb et al 2017b 43 | – | – | 34% |
| Eleftheriadou et al 2018*** 26 | 10.8% | 30.4% | 38.9% |
| Fasler et al 2019 27 | 24% | 42% | 44% |
| Chandra et al 2020 41 | 32.2% | 54.4% | 50.3% |
Notes: It should be noted that baseline characteristics will be different between real-world studies and compared with registration clinical trials. There is significant loss to follow-up over time in included real-world studies. *Study recorded greater than 75 logMAR letters and may have included some pre-treated eyes. **Study recorded greater than 75 logMAR letters. ***Study recorded greater than 73 letters that is equated to 6/12 Snellen in some clinical trials.
Treatment Burden
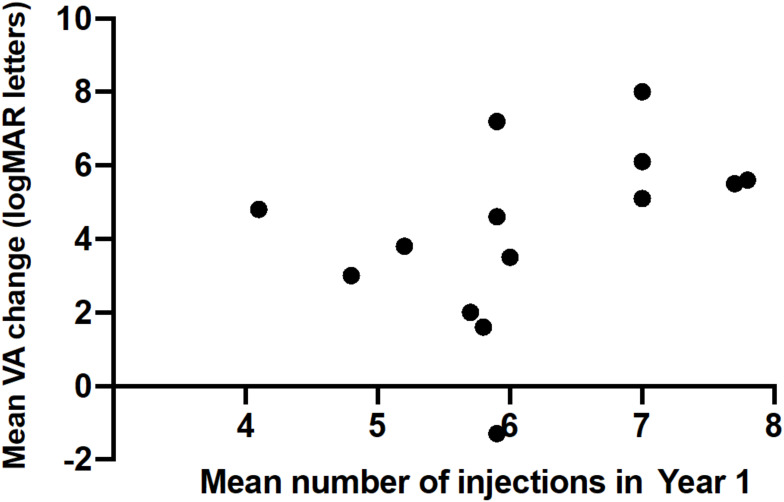
The mean number of intravitreal injections over 12 months ranged from 4.5 to 11.4 in included studies, and the median number of intravitreal injections in the first year of treatment was 5.9 in studies published in the first half of the decade and 7.1 in the latter half. Mean VA gain at 1 year positively correlated with the mean number of intravitreal anti-VEGF injections received (Figure 3, Pearson correlation coefficient, r=0.66, p=0.0095). The treatment regimen reported in the included studies changed from predominantly as required (PRN) injections in the first half of the decade (9 April 2010 to 8 April 2015) to predominantly fixed interval dosing and treat-and-extend (T&E) in the second half of the decade (9 April 2015 to 8 April 2020) (Supplementary Table 1).
Figure 3.
Mean VA gain at 1 year correlated with mean number of intravitreal anti-VEGF injections received. Only real-world studies with ≥100 eyes at baseline were included. It should be noted that a limitation is that there will be variation in baseline characteristics of included studies. Pearson correlation coefficient, r = 0.66 (p = 0.0095) indicating moderate positive correlation that is statistically significant.
Another aspect of treatment burden relates to the average number of clinic visits, with PRN regimens requiring between 12–14 visits in year 1, whereas fixed interval regimens required 9 visits in year 1. Chandra et al41 reported a T&E approach after the initial year of fixed dosing with aflibercept. They reported better maintenance of driving-level vision in those eyes receiving 5 or more injections (and therefore, by implication, clinic visits) from years 2–5.
In terms of time spent in the clinic, the TERRA study reported that one-stop clinics used less staff resources and were likely to be shorter in duration than the cumulative time spent for two-stop clinics.40
Anatomical Outcomes
There were two real-world studies reporting drying of intraretinal and subretinal fluid at the macula as recorded by the treating clinician. Both studies investigated aflibercept treatment for nAMD. Almuhtesab et al21 reported that by the eleventh month of treatment, 53% of eyes were dry and 47% of eyes remained wet. Eleftheriadou et al26 reported 67% of eyes were dry by the end of the first year of treatment with a similar proportion at the end of years 2 and 3. There was not comparative data available on the anatomical outcomes of ranibizumab versus aflibercept treated eyes in the included UK studies.
Adverse Events
Few studies reported adverse event rates (Supplementary Table 1). Gupta et al49 reported that one patient developed acute anterior uveitis (and that they observed no episodes of endophthalmitis); Kumar et al30 reported one patient experienced elevated intraocular pressure (IOP), and Shona et al35 stated that no cases of endophthalmitis, retinal detachment or acute inflammation were observed. Borooah et al23 reported no incidents of endophthalmitis from 994 intravitreal injections. Pushpoth et al44 reported 4 cases of endophthalmitis out of 1086 eyes (0.4%). Ross et al45 reported 3657 injections were administered to 406 eyes. There were 2 cases of endophthalmitis during the study period, a rate of 1 in every 1828 injections and of 1 in every 203 eyes (0.5%). Buckle et al24 reported 8 cases of endophthalmitis out of 1483 eyes (0.5%), which arose from 16,993 injections (a rate of 1 per 2124 injections), and also that 31 eyes (2.1%) experienced subconjunctival haemorrhage, 26 eyes experienced corneal epithelial cell abrasion (1.8%) and 40 eyes (2.7%) experienced IOP elevations above 21 mmHg. Vardarinos et al38 reported no serious ocular or systemic adverse events. Systemic adverse events were not consistently reported in the included studies.
Excluded Studies
Where it was clear that data from the same eyes had been published more than once, then the largest dataset was included, and the smaller dataset excluded. This applied to the 2 and 3 year data published by Eleftheriadou et al.26 They stated in their 2017 publication, “eyes receiving their first aflibercept treatment between October 1, 2013 and December 31, 2013 were included in this analysis” and in their 2018 publication, “… eyes, receiving intravitreal aflibercept injections from 1 September 2013 to 31 February 2014, were included and analysed in this study”. Therefore, the 2018 publication data only was included. The first36 and subsequently second-year43 data of the Aflibercept Users Group was published. So as not to double count eyes, only the larger sample size from the 2017 publication was included when calculating the total number of eyes in this systematic review. Williams and Blyth39 published an interesting article primarily focused on eyes with better than 6/12 vision at presentation. Although an important topic, and a patient group likely to benefit from early treatment, that particular subset of the population with nAMD was not the focus of this review. Although Buckle et al24 had well over 100 eyes, mean VA changes of individual eyes were not presented and so could not be included in the summary graphs. Where it was reported that eyes were not treatment naïve, this subset of eyes were excluded from the overall analysis.40,44
Quality of Life
Quality of life indices such as patient-reported outcome measures were not reported in the included real-world studies.
Quality of Included Studies
The quality of the included studies varied, with 14–17 out of 20 domains of the IHE Quality Appraisal of Case Series checklist satisfied (Supplementary Table 2).
Discussion
Many UK NHS services have developed a culture of auditing their real-world outcomes of intravitreal anti-VEGF therapy for nAMD over the last decade, a practice that should be commended. Over 25,000 eyes were included in this systematic review and visual outcome trends were assessed in over 23,000 eyes. Although representing a lower level on the evidence hierarchy, these real-world studies dwarf the size of randomized clinical trials in this field.
Baseline Visual Acuity
Baseline VA in published studies has gradually improved over the last decade. Worse baseline VA might be a reflection of the delay in a patient receiving initial anti-VEGF therapy, and therefore a surrogate marker of the effectiveness of local referral pathways and capacity of local macular services, rather than as a measure of the intrinsic efficacy of the drug being used. It can be implied that referral pathways have become more streamlined and capacity of local macular services has improved over the last decade. Further measures involving home monitoring, strong community links, human or artificial intelligence referral refinement pathways, and adequate resources will support this trend in the future. Baseline VA is a strong predictor of long-term visual outcomes and restricting treatment until VA declines below the driving standard is likely to be counterproductive.
Similar to the MARINA50 and ANCHOR51 ranibizumab and VIEW 1 and 2 aflibercept registration clinical trials,52 better baseline VA is associated with lower VA gains but a greater likelihood of achieving driving-level vision.53,54 Older age and larger lesion size at baseline were also associated with worse visual outcomes in these registration clinical trials. The mean age of patients enrolled in real-world studies ranged from 76.5 to 83.0 years. This was not dissimilar to the 77 and 76 years reported, respectively, in the MARINA50 and ANCHOR51 clinical trials and 78 years reported in the VIEW 1 cohort; the VIEW 2 cohort was on average younger with a mean age of 74 years.52 Characterizing nAMD lesions on fundus fluorescein angiography has become less common in routine UK NHS practice in recent years (Supplementary Table 1).
Short Term Visual Acuity Outcomes (≤2 Years)
Encouragingly, mean VA gains in UK real-world studies have improved over the last decade. Of note, the number of intravitreal injections received in the first year of treatment significantly and positively correlated with vision gain, despite differing baseline characteristics in the included studies.
Mean VA gains in included studies ranged from −1.3 to +8.0 logMAR letters. The VIEW 1 and 2 registration clinical trials for aflibercept enrolled 2457 study eyes.52,55 In the first year, patients received either aflibercept 0.5 mg every 4 weeks (0.5Q4), aflibercept 2 mg every 4 weeks (2Q4), aflibercept every 8 weeks after three monthly loading injections (2Q8), or 0.5 mg intravitreal ranibizumab every 4 weeks (RQ4). The three fixed interval aflibercept groups had similar VA gains compared with fixed interval ranibizumab at 52 weeks, with mean best-corrected visual acuity (BCVA) gains ranging from 8.3 to 9.3 letters. In the second year of the trial, a PRN approach was followed in all treatment arms with the maximum treatment interval capped at 12 weeks. The VA gains at 52 weeks in all treatment arms were not fully maintained at week 96 with the mean BCVA gain ranging from 6.6 to 7.9 letters, with the most likely cause being the reduced frequency of intravitreal injections in year 2. The 2q8 aflibercept group had similar mean VA outcomes to the q4 aflibercept and q4 ranibizumab groups over 96 weeks, but with an average of 5 fewer injections. There was no 2q8 ranibizumab arm in this trial.
The proportion of treated eyes with 15-letter loss at 1 year was reported to range from 5.6% to 10% when reported in included UK real-world studies. These numbers almost doubled by 2 years, ranging from 9.2% to 18%. Table 1 highlights that over the last decade, the proportion of eyes with 15-letter loss at 1 and 2 years has reduced. The MARINA trial randomized patients to ranibizumab 0.3 mg, 0.5 mg and sham injections for a period of 24 months.50 After one year, approximately 5% of the groups treated with ranibizumab lost greater than 15 letters from baseline compared with 38% receiving sham injections. At 2 years, approximately 9% of eyes of the groups treated with ranibizumab lost >15 letters from baseline compared with 47% receiving sham injections. The ANCHOR trial randomized patients into treatment groups with intravitreal ranibizumab (0.3 mg or 0.5 mg) and photodynamic therapy with verteporfin.51 At one year, groups treated with ranibizumab lost greater than 15 letters from baseline in 6% and 4% of cases, respectively, compared with 36% receiving verteporfin. In the integrated analysis of 2-year VIEW 1 and 2 data, 7.6% of eyes lost greater than 15 letters from baseline.
Some of the more recent UK real-world studies reported comparable mean VA gains to the registration clinical trials at 1 and 2 years; the extent of 15-letter loss is not so favourable, especially in the second year of treatment (ranging from 9.2% to 13.3% in publications in the last 5 years versus 7.6% in the integrated VIEW 1 and 2 clinical trials).26,41 A possible reason for this significant visual loss may be under-treatment as eyes move beyond the first year of fixed interval treatment every 8 weeks.
Long-Term Visual Outcomes (>2 Years)
Only six UK real-world included studies with ≥100 eyes at baseline reported mean VA outcomes beyond 2 years,25,26,32,41,44,46 Five of these out to 3 years, and Chandra et al41 reporting outcomes data out to 5 years. Chandra et al41 reported the best long-term visual outcomes in the UK with long-term proactive treatment. Horner et al42 had just less than 100 eyes but is worthy of mention as outcomes were reported out to 8 years – they reported using a PRN approach that mean VA could be maintained into the third year of treatment, but by year 7 there was a mean 6.4 letter loss. The third year of treatment represents the last year where mean vision gains from baseline were still reported in the included UK studies. This is in contrast with other healthcare systems, where the Fight Retinal Blindness! Registry reported56 they were able to maintain the VA gains for 5 years, but beyond that there was a mean loss of 2.6 letter loss by year 7 – a phenomenon that is likely related to the use of a more proactive T&E treatment approach throughout the disease course.
Most clinical trials do not provide outcomes data beyond 3 years. The SEVEN-UP extension study56,57 of patients who had participated in MARINA50 or ANCHOR51 then HORIZON58 clinical trials and were subsequently treated in routine clinical practice with mainly a PRN regimen and with chronic under-treatment from the third year of treatment had a mean loss of 8.6 letters over 7 years.56,57 Sadda et al reported that it is important to recognize that adequately treating nAMD remains the best option to optimize visual outcomes in patients, particularly given the risk of vision loss with under-treatment observed in the real-world.59 Mones et al60 suggest that better long-term visual outcomes could be achieved by changing the community mindset that contributes to under-treatment of this chronic disease. Other reasons initial gains may wane over time include loss of patient enthusiasm for frequent treatment and also the progressive onset of atrophic AMD.
Inter-Centre and Intra-Centre Variation in Visual Outcomes
There was considerable variation in baseline VA and visual outcomes between centres even when looking at published data from similar time-points in the included real-world studies. The UK AMD EMR Users group published an analysis of anonymized inter-centre variation in VA outcomes in 2016.61 A total of 5811 treatment-naïve eyes of 5205 patients from 13 UK centres were assessed. There was considerable variation in mean baseline VA between centres ranging from 48.9 to 59.9 logMAR letters. Mean inter-centre VA change from baseline to 12 months varied from +6.9 letters to −0.6 letters (mean of +2.5 letters). The authors reported these differences are influenced, but not completely explained, by factors such as patient age, starting VA, number of injections, and visits. Additional factors include socio-economic status and resource allocation with deprivation being related to worse ocular health outcomes.62,63
Choosing the right parameters to judge the quality of a good service is an important consideration. Looking just at mean VA gain could penalize services that have good referral mechanisms in place and start with better baseline VA. Therefore, the proportion of eyes achieving 6/12 vision might be a better comparator. Maintenance of vision after 3 loading injections is another way to assess an intravitreal service. The Retinal Outcomes Group and other expert panels have suggested parameters to record to enable both patient outcomes and service delivery to be audited and compared.64,65
Three recent publications from the same institution had slightly different visual outcomes.26,27,41 Some of this relates to the time-point when eyes were included, consistent with a national trend for better outcomes over time. Inclusion and exclusion criteria varied and the way in which missing data was treated was different between the analyses. This highlights the importance of trying to standardize the methodological approach as well as outcomes measured in real-world studies of nAMD.
Treatment Burden
The mean number of injections in the first year of treatment was 5.9 in publications from the first half of the decade and 7.1 from the latter half. The increase in average first-year injection numbers corresponded with the transition from PRN to T&E ranibizumab treatment regimens and the introduction of aflibercept with a fixed treatment interval for the initial 12 months in UK clinical practice.
The advantage of fixed interval and T&E dosing over a PRN regimen is that each clinic visit is likely to also be a treatment visit. In the analysis by Lee et al,31 the mean number of visits in year 1 for PRN treatment was 10.8 versus 8.9 for fixed dose-treatment, with an average of 5.8 injections versus 7.0 respectively. A global meta-analysis of ranibizumab nAMD real-world outcomes identified that the mean change in VA for patients on a T&E regimen was better than PRN regimens out to 3 years.18 T&E patients received on average more injections (6.9 vs. 4.7) but had fewer visits (7.6 vs. 9.2) in the first year of treatment.
Lee et al31 compared PRN ranibizumab and continuous aflibercept UK real-world treatment outcomes of treatment-naïve nAMD. After 1 year, the vision gains in the aflibercept arm were greater than those achieved in the ranibizumab arm with similar baseline vision in both treatment groups. However, the authors noted that “the observed VA differences are small and likely to be related to more frequent treatment with aflibercept”. Ozturk et al33 identified that VIEW 1 and 2 visual gains could be achieved in year 1 in UK NHS practice when patients received 7–8 injections. However, VA outcomes were less good when patients received 6 or fewer injections in year 1. A French observational study also highlighted the importance of regular and frequent aflibercept therapy to achieving better visual outcomes out to 2 years.66 Fixed interval regimens for year 1 transitioning into T&E longer-term or T&E regimens after loading injections are now preferred to PRN treatment approaches in the UK.64,67,68
Anatomical Outcomes
Two included studies reported that between a third and a half of aflibercept treated eyes continued to have intraretinal or subretinal fluid at the end of the first year of treatment. In the VIEW 2 clinical trial, 28% of eyes in the 2Q8 arm were not dry at the end of 12 months.52 The long-term visual implications of persistent intraretinal or subretinal fluid are not fully understood.
Adverse Event Reporting
Three cases of endophthalmitis were reported in each of the Q4 ranibizumab and Q4 aflibercept arms of the VIEW 1 clinical trial, giving a rate of endophthalmitis of 1% of patients in those treatment arms but no cases of endophthalmitis were reported in the VIEW 2 clinical trial.52,55 The endophthalmitis rates in MARINA and ANCHOR were 1% and 1.1%, respectively.50,51 In real-world studies, it is more common to report rates of endophthalmitis per injection rather than per patient, although both provide useful information. The reported rate of endophthalmitis in a global meta-analysis of real-world outcomes of nAMD was 17 of 66,176 intravitreal injections (0.026%),18 with possible under-reporting. The number of reported endophthalmitis cases in the UK real-world studies was considerably lower than would have been expected based on reported rates in the literature.69,70 Buckle et al24 reported 8 cases in total, with an endophthalmitis rate of 1 in 2124 injections (0.047%). Ross et al45 which also recorded data from Gloucestershire, reported 2 cases of endophthalmitis, a rate of 1 in 1828 injections (0.055%). It is likely other UK real-world studies under-reported ocular safety outcomes. It will be important to accurately record ocular safety as new longer-acting drugs become available. Prospective studies, which made up only 6 of 26 included studies, have greater potential to accurately capture ocular safety data.
Systemic adverse event rates were not recorded in many of these real-world studies. Systemic anti-VEGF drug use is associated with thromboembolic events like stroke and heart attack. Although the systemic exposure to intravitreally injected anti-VEGF agents is very small, it is not clear from reports in the literature if there is an increased risk of these adverse events when these drugs are used to treat nAMD, especially in high-risk groups that would have been excluded from clinical trials.13 The incidence of Antiplatelet Trialists’ Collaboration-defined arterial thromboembolic events from baseline to week 96 in the VIEW 1 and 2 clinical trials were similar amongst the aflibercept and ranibizumab groups (2.4–3.8%). Capturing systemic safety data can be challenging in an ophthalmology clinic setting. It may be that history of systemic adverse events is not sought most of the time. In the future, cross-referencing a comprehensive prospective UK nAMD registry with a comprehensive UK stroke registry in a well-defined region might help generate a more definitive answer. A similar approach has been used in Singapore.71
Quality of Life Measurement
It is clear that maintaining patients’ vision for longer, or improving their VA has quality of life benefits. However, quality of life assessments and patient-reported outcomes were not available in the included UK real-world studies.
Study Limitations
This study had a number of limitations. As the IHE study quality assessment identified, the study design, methodology, baseline patient characteristics and outcomes assessments were heterogeneous, making it challenging to compare studies. A meta-analysis was not carried out here, but if that is considered in a future analysis, the real-world studies would need to be weighted by number of study eyes and baseline characteristics adjusted for. Some studies were prospective, but most were retrospective where there is a greater chance of selection bias, especially as loss to follow-up rates tend to be high in real-world studies.15 It is possible UK real-world studies that did not meet the search criteria were not included in this analysis; however, if that is the case, they are likely to represent small studies that would not change the overall conclusions of this study. The real-world studies were not randomized or controlled. VA measurements are usually not performed with full refraction in routine clinical practice in contrast to that in clinical trial protocols. There are potential causes for visual decline other than macular degeneration. There may be a publication bias, with the UK centres that reported real-world outcomes potentially having outcomes that were better than the national average. There is a likelihood that some data is duplicated as some study centres may have contributed eyes to more than one publication. Nevertheless, the size of the study dataset was large enough to help minimize the impact of some of these limitations. This was the reason that VA trends were only assessed in studies with ≥100 eyes at baseline.
It is also worth addressing the fact that there is a time lag between what is recorded in clinical practice and when the study is published. The included studies typically reflect what was prevailing clinical practice in the preceding 1–3 years of publication, rather than what was the clinical practice on the publication date. A better approach would be to have prospectively designed registries, which have the benefit of being able to identify and report contemporary real-world practice patterns in a far timelier manner.72,73
International Consortium for Health Outcome Measures (ICHOM)
A minimum set of standardized patient-centred outcomes have been specified by ICHOM to allow easy comparison between different units nationally and internationally.48 When future real-world studies are planned, it would be helpful to record the ICHOM visual outcomes including baseline VA, VA gain, 15-letter gain and loss from baseline, and maintenance of driving-level vision (Snellen VA of 6/12 or better). Such practice would allow future real-world studies to be more easily compared.
Maintenance of driving-level of vision is a useful big-picture statistic to identify if patients are being referred in a timely manner to nAMD services, and whether they are receiving adequate long-term treatment. Maintaining patients’ independence clearly has profound economic benefits for the individual, carers and wider society. It is important that the NICE health economic modelling reflects this.
Additional parameters that are recommended by ICHOM include: patient-reported outcome measures such as the Brief Impact of Vision Impairment (IVI) questionnaire, ocular safety, and treatment burden including clinic visit numbers as well as injection numbers.74
Emerging Challenges
There was a significant reduction in referrals of nAMD to NHS eye services at the outset of the COVID-19 pandemic. In the first month of the lockdown, there was an approximately 72% reduction in referrals in 4 large NHS Trusts.75 If these figures are extrapolated to the whole of the UK, a conservative estimate is that a treatment delay of 3 months could lead to a >50% relative increase in the number of eyes with vision ≤6/60 and 25% relative decrease in the number of eyes with driving vision at one year.75
The COVID-19 pandemic has also meant that many patients are either unable or unwilling to attend routine hospital appointments during periods of quarantine. The nAMD treatment population largely includes elderly patients with multiple co-morbidities who are at higher risk of death from COVID-19 than the general population, explaining the reluctance of patients to visit eye clinics. A short to medium term solution may be establishing fully equipped and staffed community nAMD treatment facilities where practical. Longer treatment intervals and infrequent clinical visits can facilitate better uptake by patients and maintenance of vision for the majority. The observed difference in UK real-world visual outcomes in studies pre and post 2015 supports the role of proactive treatment regimens (e.g. T&E and fixed interval dosing). This emphasizes the need for longer-acting agents that do not require regular treatment visits for patients to maintain their vision. This would not only reduce the burden on patients and their families under normal circumstances but would be of value in reducing visual impact on patients during periods of quarantine.
Another challenge is to continue to optimize real-world UK NHS treatment outcomes as the population ages and demand for services increases. This will require long-term use of proactive treatment regimens and avoidance of under-treatment, patient education, staff training and governance, greater use of virtual clinics, telemedicine and information technology infrastructure, key performance indicators and adequate resources.76,77
Conclusion
UK real-world outcomes have improved over the last decade with the adoption of more proactive treatment regimens and service improvements but are still not consistently as impressive as those from registration clinical trials or some international observational cohorts with long-term data. The adoption of prospective registries can inform key stakeholders of important changes in clinical practice outcomes in a more timely manner.72 Access to longer-acting intravitreal anti-VEGF therapies can reduce the treatment burden for patients and carers and potentially make replication of clinical trial results possible in the NHS.
Funding Statement
Editorial assistance was provided to the authors by Dr Mark Hillen, BSc, PhD, through unrestricted grant funding by Allergan International plc, Dublin, Ireland. Open Access publication costs were also provided through an unrestricted education grant from Allergan International at the request of the first author. Allergan plc had no role in the design or conduct of this research. All authors met the ICMJE authorship criteria. Neither honoraria nor payments were made for authorship and authors retained full control over the manuscript.
Disclosure
HM has received research grants, educational travel grants and honoraria from Allergan/AbbVie, Bayer, Novartis and Roche outside the submitted work. TM is a consultant for Allergan, Bayer and Novartis; and reports grants, personal fees, non-financialsupport from Novartis and non-financial support from Bayer outside the submitted work. FG has received honoraria for consultancy-advisory boards from Alimera, Allergan, Bayer, Novartis, Oxford BioElectronics, Roche; educational travel grants from Allergan, Bayer, Novartis and departmental research grants from Allergan, Bayer, Boehringer Ingelheim, Chengdu Pharma, Novartis, PanOptica and Roche; and reports grants, personal fees from Allergan, grants from Bayer, personal fees from Novartis, outside the submitted work. WMA has received honoraria for advisory board memberships from AbbVie, Alcon, Alimera, Allergan, Bayer, Bausch and Lomb, Novartis and Pfizer, speaker Fees from Alimera, Allergan, Bayer, Novartis and Pfizer, and educational travel grants from Alimera, Allergan, Bayer, Novartis and Pfizer; and reports grants and personal fees from Novartis, Bayer and Allergan, personal fees from Roche, AbbVie, and Alimera, and grants from Boehringer Ingelheim, outside the submitted work. WMA has undertaken clinical research sponsored by Allergan, Bayer, Gyroscope, and Novartis and his institution has received research funding from Allergan, Bayer, Boehringer Ingelheim, CenterVue, Novartis, and Optos plc. LK is a consultant for AbbVie, Alcon, Allergan, Bayer, Kris, Novartis and Théa laboratories; and reports personal fees from Bayer, grants from Allergan, outside the submitted work. LNK and PZ have no disclosures and the authors report no other potential conflicts of interest for this work.
References
- 1.Bourne RR, Stevens GA, White RA, et al. Causes of vision loss worldwide, 1990–2010: a systematic analysis. Lancet Glob Health. 2013;1(6):e339–e349. doi: 10.1016/S2214-109X(13)70113-X [DOI] [PubMed] [Google Scholar]
- 2.Bressler NM. Age-related macular degeneration is the leading cause of blindness. JAMA. 2004;291(15):1900–1901. doi: 10.1001/jama.291.15.1900 [DOI] [PubMed] [Google Scholar]
- 3.Li JQW, Schmid M, Letow J, Wolpers AC, Holz FG, Finger RP. EURETINA. Retinal Diseases in Europe: Prevalence. Incidence and Healthcare Needs. Bonn, Germany; 2017. Available from: https://www.euretina.org/downloads/EURETINA_Retinal_Diseases.pdf. Accessed September30, 2020. [Google Scholar]
- 4.Wong WL, Su X, Li X, et al. Global prevalence of age-related macular degeneration and disease burden projection for 2020 and 2040: a systematic review and meta-analysis. Lancet Glob Health. 2014;2(2):e106–e116. doi: 10.1016/S2214-109X(13)70145-1 [DOI] [PubMed] [Google Scholar]
- 5.Gass JD, Agarwal A, Lavina AM, Tawansy KA. Focal inner retinal hemorrhages in patients with drusen: an early sign of occult choroidal neovascularization and chorioretinal anastomosis. Retina. 2003;23(6):741–751. doi: 10.1097/00006982-200312000-00001 [DOI] [PubMed] [Google Scholar]
- 6.Owen CG, Jarrar Z, Wormald R, Cook DG, Fletcher AE, Rudnicka AR. The estimated prevalence and incidence of late stage age related macular degeneration in the UK. Br J Ophthalmol. 2012;96(5):752–756. doi: 10.1136/bjophthalmol-2011-301109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Macular Photocoagulation Study Group. Laser photocoagulation of subfoveal recurrent neovascular lesions in age-related macular degeneration. Results of a randomized clinical trial. Arch Ophthalmol. 1991;109(9):1232–1241. doi: 10.1001/archopht.1991.01080090056026 [DOI] [PubMed] [Google Scholar]
- 8.Gillies MC, Simpson JM, Luo W, et al. A randomized clinical trial of a single dose of intravitreal triamcinolone acetonide for neovascular age-related macular degeneration: one-year results. Arch Ophthalmol. 2003;121(5):667–673. doi: 10.1001/archopht.121.5.667 [DOI] [PubMed] [Google Scholar]
- 9.Rosenfeld PJ, Moshfeghi AA, Puliafito CA. Optical coherence tomography findings after an intravitreal injection of bevacizumab (Avastin) for neovascular age-related macular degeneration. Ophthalmic Surg Lasers Imaging. 2005;36(4):331–335. doi: 10.3928/1542-8877-20050701-14 [DOI] [PubMed] [Google Scholar]
- 10.Spaide RF, Laud K, Fine HF, et al. Intravitreal bevacizumab treatment of choroidal neovascularization secondary to age-related macular degeneration. Retina. 2006;26(4):383–390. [DOI] [PubMed] [Google Scholar]
- 11.Avery RL, Pieramici DJ, Rabena MD, Castellarin AA, Nasir MA, Giust MJ. Intravitreal bevacizumab (Avastin) for neovascular age-related macular degeneration. Ophthalmology. 2006;113(3):363–372.e365. doi: 10.1016/j.ophtha.2005.11.019 [DOI] [PubMed] [Google Scholar]
- 12.Macular Photocoagulation Study Group. Argon laser photocoagulation for senile macular degeneration. Results of a randomized clinical trial. Arch Ophthalmol. 1982;100(6):912–918. doi: 10.1001/archopht.1982.01030030920003 [DOI] [PubMed] [Google Scholar]
- 13.Solomon SD, Lindsley K, Vedula SS, Krzystolik MG, Hawkins BS. Anti‐vascular endothelial growth factor for neovascular age‐related macular degeneration. Cochrane Database Syst Rev. 2019;4(3):CD005139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rahman F, Zekite A, Bunce C, Jayaram H, Flanagan D. Recent trends in vision impairment certifications in England and Wales. Eye (Lond). 2020;34(7):1271–1278. doi: 10.1038/s41433-020-0864-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mehta H, Tufail A, Daien V, et al. Real-world outcomes in patients with neovascular age-related macular degeneration treated with intravitreal vascular endothelial growth factor inhibitors. Prog Retin Eye Res. 2018;65:127–146. doi: 10.1016/j.preteyeres.2017.12.002 [DOI] [PubMed] [Google Scholar]
- 16.Lee AY, Lee CS, Butt T, et al. UK AMD EMR USERS GROUP REPORT V: benefits of initiating ranibizumab therapy for neovascular AMD in eyes with vision better than 6/12. Br J Ophthalmol. 2015;99(8):1045–1050. doi: 10.1136/bjophthalmol-2014-306229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Holz FG, Tadayoni R, Beatty S, et al. Multi-country real-life experience of anti-vascular endothelial growth factor therapy for wet age-related macular degeneration. Br J Ophthalmol. 2015;99(2):220–226. doi: 10.1136/bjophthalmol-2014-305327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kim LN, Mehta H, Barthelmes D, Nguyen V, Gillies MC. Metaanalysis of real-world outcomes of intravitreal ranibizumab for the treatment of neovascular age-related macular degeneration. Retina. 2016;36(8):1418–1431. doi: 10.1097/IAE.0000000000001142 [DOI] [PubMed] [Google Scholar]
- 19.Guo B, Moga C, Harstall C, Schopflocher D. A principal component analysis is conducted for a case series quality appraisal checklist. J Clin Epidemiol. 2016;69:199–207.e2. doi: 10.1016/j.jclinepi.2015.07.010 [DOI] [PubMed] [Google Scholar]
- 20.National Institute for Health and Care Excellence. Developing NICE Guidelines: The Manual. Manchester, UK; 2014. Available from: https://www.nice.org.uk/process/pmg20/. Accessed September30, 2020. [PubMed] [Google Scholar]
- 21.Almuhtaseb H, Kanavati S, Rufai SR, Lotery AJ. One-year real-world outcomes in patients receiving fixed-dosing aflibercept for neovascular age-related macular degeneration. Eye (Lond). 2017;31(6):878–883. doi: 10.1038/eye.2017.6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Basheer K, Mensah E, Khanam T, Minakaran N. Visual outcomes of age-related macular degeneration patients undergoing intravitreal ranibizumab monotherapy in an urban population. Clin Ophthalmol. 2015;9:959–965. doi: 10.2147/OPTH.S76754 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Borooah S, Jeganathan VS, Ambrecht AM, et al. Long-term visual outcomes of intravitreal ranibizumab treatment for wet age-related macular degeneration and effect on blindness rates in south-east Scotland. Eye (Lond). 2015;29(9):1156–1161. doi: 10.1038/eye.2015.83 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Buckle M, Donachie PH, Johnston RL. Long-term outcomes of intravitreal ranibizumab for neovascular age-related macular degeneration in a well defined region of the UK. Br J Ophthalmol. 2016;100(2):240–245. doi: 10.1136/bjophthalmol-2014-306423 [DOI] [PubMed] [Google Scholar]
- 25.Chavan R, Panneerselvam S, Adhana P, Narendran N, Yang Y. Bilateral visual outcomes and service utilization of patients treated for 3 years with ranibizumab for neovascular age-related macular degeneration. Clin Ophthalmol. 2014;8:717–723. doi: 10.2147/OPTH.S60763 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Eleftheriadou M, Vazquez-Alfageme C, Citu CM, et al. Long-term outcomes of aflibercept treatment for neovascular age-related macular degeneration in a clinical setting. Am J Ophthalmol. 2017;174:160–168. doi: 10.1016/j.ajo.2016.09.038 [DOI] [PubMed] [Google Scholar]
- 27.Fasler K, Moraes G, Wagner S, et al. One- and two-year visual outcomes from the moorfields age-related macular degeneration database: a retrospective cohort study and an open science resource. BMJ Open. 2019;9(6):e027441. doi: 10.1136/bmjopen-2018-027441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fulcher C, Hazel CA, Pacey I, Ali H, Ghanchi FD. Predicting visual outcomes in patients treated with aflibercept for neovascular age-related macular degeneration: data from a real-world clinical setting. Eur J Ophthalmol. 2020;30(3):543–549. [DOI] [PubMed] [Google Scholar]
- 29.Gupta B, Adewoyin T, Patel SK, Sivaprasad S. Comparison of two intravitreal ranibizumab treatment schedules for neovascular age-related macular degeneration. Br J Ophthalmol. 2011;95(3):386–390. doi: 10.1136/bjo.2010.179499 [DOI] [PubMed] [Google Scholar]
- 30.Kumar A, Sahni JN, Stangos AN, Campa C, Harding SP. Effectiveness of ranibizumab for neovascular age-related macular degeneration using clinician-determined retreatment strategy. Br J Ophthalmol. 2011;95(4):530–533. doi: 10.1136/bjo.2009.171868 [DOI] [PubMed] [Google Scholar]
- 31.Lee AY, Lee CS, Egan CA, et al. UK AMD/DR EMR REPORT IX: comparative effectiveness of predominantly as needed (PRN) ranibizumab versus continuous aflibercept in UK clinical practice. Br J Ophthalmol. 2017;101(12):1683–1688. doi: 10.1136/bjophthalmol-2016-309818 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Muniraju R, Ramu J, Sivaprasad S. Three-year visual outcome and injection frequency of intravitreal ranibizumab therapy for neovascular age-related macular degeneration. Ophthalmologica. 2013;230(1):27–33. doi: 10.1159/000350238 [DOI] [PubMed] [Google Scholar]
- 33.Ozturk M, Harris ML, Nguyen V, Barthelmes D, Gillies MC, Mehta H. Real-world visual outcomes in patients with neovascular age-related macular degeneration receiving aflibercept at fixed intervals as per UK licence. Clin Exp Ophthalmol. 2018;46(4):407–411. doi: 10.1111/ceo.13085 [DOI] [PubMed] [Google Scholar]
- 34.Razi F, Haq A, Tonne P, Logendran M. Three-year follow-up of ranibizumab treatment of wet age-related macular degeneration: influence of baseline visual acuity and injection frequency on visual outcomes. Clin Ophthalmol. 2016;10:313–319. doi: 10.2147/OPTH.S97775 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Shona O, Gupta B, Vemala R, Sivaprasad S. Visual acuity outcomes in ranibizumab-treated neovascular age-related macular degeneration; stratified by baseline vision. Clin Exp Ophthalmol. 2011;39(1):5–8. [DOI] [PubMed] [Google Scholar]
- 36.Talks JS, Lotery AJ, Ghanchi F, et al. First-year visual acuity outcomes of providing aflibercept according to the VIEW Study Protocol for age-related macular degeneration. Ophthalmology. 2016;123(2):337–343. doi: 10.1016/j.ophtha.2015.09.039 [DOI] [PubMed] [Google Scholar]
- 37.Tufail A, Patel PJ, Egan C, et al. Bevacizumab for neovascular age related macular degeneration (ABC trial): multicentre randomised double masked study. BMJ. 2010;340:c2459. doi: 10.1136/bmj.c2459 [DOI] [PubMed] [Google Scholar]
- 38.Vardarinos A, Gupta N, Janjua R, Iron A, Empeslidis T, Tsaousis KT. 24-month clinical outcomes of a treat-and-extend regimen with ranibizumab for wet age-related macular degeneration in a real life setting. BMC Ophthalmol. 2017;17(1):58. doi: 10.1186/s12886-017-0451-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Williams GS, Seow E, Evans H, Owoniyi M, Evans S, Blyth C. Factors affecting visual acuity after one year of follow up after repeated intravitreal ranibizumab for macular degeneration. Saudi J Ophthalmol. 2015;29(3):187–191. doi: 10.1016/j.sjopt.2015.02.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Yang Y, Downey L, Mehta H, et al. Resource use and real-world outcomes for ranibizumab treat and extend for neovascular age-related macular degeneration in the UK: interim results from TERRA. Ophthalmol Ther. 2017;6(1):175–186. doi: 10.1007/s40123-017-0091-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chandra S, Rasheed R, Menon D, et al. Impact of injection frequency on 5-year real-world visual acuity outcomes of aflibercept therapy for neovascular age-related macular degeneration. Eye (Lond). 2020:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Horner F, Lip PL, Clark H, Chavan R, Sarmad A, Mushtaq B. Real-world visual and clinical outcomes for patients with neovascular age-related macular degeneration treated with intravitreal ranibizumab: an 8-year observational cohort (AMD8). Clin Ophthalmol. 2019;13:2461–2467. doi: 10.2147/OPTH.S218378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Almuhtaseb H, Johnston RL, Talks JS, Lotery AJ. Second-year visual acuity outcomes of nAMD patients treated with aflibercept: data analysis from the UK Aflibercept Users Group. Eye (Lond). 2017;31(11):1582–1588. doi: 10.1038/eye.2017.108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Pushpoth S, Sykakis E, Merchant K, Browning AC, Gupta R, Talks SJ. Measuring the benefit of 4 years of intravitreal ranibizumab treatment for neovascular age-related macular degeneration. Br J Ophthalmol. 2012;96(12):1469–1473. doi: 10.1136/bjophthalmol-2012-302167 [DOI] [PubMed] [Google Scholar]
- 45.Ross AH, Donachie PH, Sallam A, et al. Which visual acuity measurements define high-quality care for patients with neovascular age-related macular degeneration treated with ranibizumab? Eye (Lond). 2013;27(1):56–64. doi: 10.1038/eye.2012.225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tufail A, Xing W, Johnston R, et al. The neovascular age-related macular degeneration database: multicenter study of 92 976 ranibizumab injections: report 1: visual acuity. Ophthalmology. 2014;121(5):1092–1101. [DOI] [PubMed] [Google Scholar]
- 47.Tan SZ, Laude A, Aspinall PA, Ambrecht AM, Vani A, Dhillon B. Decisional answer tree analysis of exudative age-related macular degeneration treatment outcomes. Int Ophthalmol. 2013;33(5):467–474. doi: 10.1007/s10792-013-9717-7 [DOI] [PubMed] [Google Scholar]
- 48.Rodrigues IA, Sprinkhuizen SM, Barthelmes D, et al. Defining a minimum set of standardized patient-centered outcome measures for macular degeneration. Am J Ophthalmol. 2016;168:1–12. doi: 10.1016/j.ajo.2016.04.012 [DOI] [PubMed] [Google Scholar]
- 49.Gupta OP, Shienbaum G, Patel AH, Fecarotta C, Kaiser RS, Regillo CD. A treat and extend regimen using ranibizumab for neovascular age-related macular degeneration clinical and economic impact. Ophthalmology. 2010;117(11):2134–2140. doi: 10.1016/j.ophtha.2010.02.032 [DOI] [PubMed] [Google Scholar]
- 50.Rosenfeld PJ, Brown DM, Heier JS, et al. Ranibizumab for neovascular age-related macular degeneration. N Engl J Med. 2006;355(14):1419–1431. doi: 10.1056/NEJMoa054481 [DOI] [PubMed] [Google Scholar]
- 51.Brown DM, Kaiser PK, Michels M, et al. Ranibizumab versus verteporfin for neovascular age-related macular degeneration. N Engl J Med. 2006;355(14):1432–1444. doi: 10.1056/NEJMoa062655 [DOI] [PubMed] [Google Scholar]
- 52.Heier JS, Brown DM, Chong V, et al. Intravitreal aflibercept (VEGF trap-eye) in wet age-related macular degeneration. Ophthalmology. 2012;119(12):2537–2548. doi: 10.1016/j.ophtha.2012.09.006 [DOI] [PubMed] [Google Scholar]
- 53.Tufail A, Margaron P, Guerin T, Larsen M. Visual benefit versus visual gain: what is the effect of baseline covariants in the treatment arm relative to the control arm? A pooled analysis of ANCHOR and MARINA. Br J Ophthalmol. 2020;104(5):672–677. doi: 10.1136/bjophthalmol-2018-313682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ho AC, Saroj N, Baker K, et al. Impact of baseline characteristics on treatment response to intravitreal aflibercept injection for wet age-related macular degeneration. Ophthalmol Retina. 2018;2(7):676–683. doi: 10.1016/j.oret.2017.10.017 [DOI] [PubMed] [Google Scholar]
- 55.Schmidt-Erfurth U, Kaiser PK, Korobelnik J-F, et al. Intravitreal aflibercept injection for neovascular age-related macular degeneration: ninety-six-week results of the VIEW studies. Ophthalmology. 2014;121(1):193–201. doi: 10.1016/j.ophtha.2013.08.011 [DOI] [PubMed] [Google Scholar]
- 56.Rofagha S, Bhisitkul RB, Boyer DS, Sadda SR, Zhang K. Seven-year outcomes in ranibizumab-treated patients in ANCHOR, MARINA, and HORIZON: a multicenter cohort study (SEVEN-UP). Ophthalmology. 2013;120(11):2292–2299. doi: 10.1016/j.ophtha.2013.03.046 [DOI] [PubMed] [Google Scholar]
- 57.Gillies MC, Campain A, Barthelmes D, et al. Long-term outcomes of treatment of neovascular age-related macular degeneration: data from an observational study. Ophthalmology. 2015;122(9):1837–1845. doi: 10.1016/j.ophtha.2015.05.010 [DOI] [PubMed] [Google Scholar]
- 58.Singer MA, Awh CC, Sadda S, et al. HORIZON: an open-label extension trial of ranibizumab for choroidal neovascularization secondary to age-related macular degeneration. Ophthalmology. 2012;119(6):1175–1183. doi: 10.1016/j.ophtha.2011.12.016 [DOI] [PubMed] [Google Scholar]
- 59.Sadda SR, Guymer R, Mones JM, Tufail A, Jaffe GJ. Anti-vascular endothelial growth factor use and atrophy in neovascular age-related macular degeneration: systematic literature review and expert opinion. Ophthalmology. 2020;127(5):648–659. doi: 10.1016/j.ophtha.2019.11.010 [DOI] [PubMed] [Google Scholar]
- 60.Mones J, Singh RP, Bandello F, Souied E, Liu X, Gale R. Undertreatment of neovascular age-related macular degeneration after 10 years of anti-vascular endothelial growth factor therapy in the real world: the need for a change of mindset. Ophthalmologica. 2020;243(1):1–8. doi: 10.1159/000502747 [DOI] [PubMed] [Google Scholar]
- 61.Liew G, Lee AY, Zarranz-Ventura J, et al. The UK neovascular AMD database report 3: inter-centre variation in visual acuity outcomes and establishing real-world measures of care. Eye (Lond). 2016;30(11):1462–1468. doi: 10.1038/eye.2016.149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Nguyen V, Daien V, Guymer RH, et al. Clinical and social characteristics associated with reduced visual acuity at presentation in Australian patients with neovascular age-related macular degeneration: a prospective study from a long-term observational data set. The Fight Retinal Blindness! Project. Clin Exp Ophthalmol. 2018;46(3):266–274. [DOI] [PubMed] [Google Scholar]
- 63.Denniston AK, Lee AY, Lee CS, et al. United Kingdom Diabetic Retinopathy Electronic Medical Record (UK DR EMR) Users Group: report 4, real-world data on the impact of deprivation on the presentation of diabetic eye disease at hospital services. Br J Ophthalmol. 2019;103(6):837–843. doi: 10.1136/bjophthalmol-2018-312568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Amoaku W, Balaskas K, Cudrnak T, et al. Initiation and maintenance of a treat-and-extend regimen for ranibizumab therapy in wet age-related macular degeneration: recommendations from the UK Retinal Outcomes Group. Clin Ophthalmol. 2018;12:1731–1740. doi: 10.2147/OPTH.S174560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Gale RP, Mahmood S, Devonport H, et al. Action on neovascular age-related macular degeneration (nAMD): recommendations for management and service provision in the UK hospital eye service. Eye (Lond). 2019;33(Suppl 1):1–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Weber M, Dominguez M, Coscas F, et al. Impact of intravitreal aflibercept dosing regimens in treatment-naive patients with neovascular age-related macular degeneration: 2-year results of RAINBOW. BMC Ophthalmol. 2020;20(1):206. doi: 10.1186/s12886-020-01468-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Patel PJ, Devonport H, Sivaprasad S, et al. Aflibercept treatment for neovascular AMD beyond the first year: consensus recommendations by a UK expert roundtable panel, 2017 update. Clin Ophthalmol. 2017;11:1957–1966. doi: 10.2147/OPTH.S145732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Ross AH, Downey L, Devonport H, et al. Recommendations by a UK expert panel on an aflibercept treat-and-extend pathway for the treatment of neovascular age-related macular degeneration. Eye (Lond). 2020;34(10):1825–1834. doi: 10.1038/s41433-019-0747-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Fileta JB, Scott IU, Flynn HW Jr. Meta-analysis of infectious endophthalmitis after intravitreal injection of anti-vascular endothelial growth factor agents. Ophthalmic Surg Lasers Imaging Retina. 2014;45(2):143–149. doi: 10.3928/23258160-20140306-08 [DOI] [PubMed] [Google Scholar]
- 70.Daien V, Nguyen V, Essex RW, et al. Incidence and outcomes of infectious and noninfectious endophthalmitis after intravitreal injections for age-related macular degeneration. Ophthalmology. 2018;125(1):66–74. doi: 10.1016/j.ophtha.2017.07.005 [DOI] [PubMed] [Google Scholar]
- 71.Ng WY, Tan GS, Ong PG, et al. Incidence of myocardial infarction, stroke, and death in patients with age-related macular degeneration treated with intravitreal anti-vascular endothelial growth factor therapy. Am J Ophthalmol. 2015;159(3):557–564.e551. doi: 10.1016/j.ajo.2014.12.005 [DOI] [PubMed] [Google Scholar]
- 72.Gillies MC, Walton R, Liong J, et al. Efficient capture of high-quality data on outcomes of treatment for macular diseases: the fight retinal blindness! Project. Retina. 2014;34(1):188–195. doi: 10.1097/IAE.0b013e318296b271 [DOI] [PubMed] [Google Scholar]
- 73.Keenan TD, Kelly SP, Sallam A, Mohamed Q, Tufail A, Johnston RL. Incidence and baseline clinical characteristics of treated neovascular age-related macular degeneration in a well-defined region of the UK. Br J Ophthalmol. 2013;97(9):1168–1172. doi: 10.1136/bjophthalmol-2013-303233 [DOI] [PubMed] [Google Scholar]
- 74.Hassell JB, Weih LM, Keeffe JE. A measure of handicap for low vision rehabilitation: the impact of vision impairment profile. Clin Exp Ophthalmol. 2000;28(3):156–161. doi: 10.1046/j.1442-9071.2000.00312.x [DOI] [PubMed] [Google Scholar]
- 75.Thomas DS, Warwick A, Olvera-Barrios A, et al. Estimating excess visual loss in people with neovascular age-related macular degeneration during the COVID-19 pandemic. medRxiv. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Amoaku W, Bailey C, Downey L, et al. Providing a safe and effective intravitreal treatment service: strategies for service delivery. Clin Ophthalmol. 2020;14:1315–1328. doi: 10.2147/OPTH.S233061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Royal College of Ophthalmologists. The Way Forward. Options to Help Meet Demand for the Current and Future Care of Patients with Eye Disease —age-Related Macular Degeneration and Diabetic Retinopathy. London, UK; 2017. Available from: https://www.rcophth.ac.uk/wp-content/uploads/2015/10/RCOphth-The-Way-Forward-AMD-300117.pdf . Accessed September30, 2020. [Google Scholar]