Highlights
-
•
Barium oesophagram often shows features suggestive of achalasia: bird-beak appearance of the distal oesophagus, and a dilated oesophagus with food residue.
-
•
Characteristic symptoms and barium oesophagrams demonstrated features of achalasia, bearing a resemblance to those of a caged bird.
-
•
In the setting where manometry is not accessible, barium oesophagram plays an important role.
-
•
Recognition of easily identifiable features such as the “caged bird sign of achalasia” can assist in the diagnosis of this entity.
Keywords: Achalasia, Caged bird sign, Barium oesphagram
Abstract
Introduction
Achalasia is an uncommon oesophageal motility disorder caused by failed relaxation of a hypertensive lower oesophageal sphincter in response to swallowing. It often manifests clinically with symptoms such as dysphagia, regurgitation, and weight loss.
Manometry is considered the gold standard diagnostic test in diagnosing this condition. However, it is not always accessible, especially in the resource-limited setting. Other radiological adjuncts, such as barium oesophagram, often show features that are highly suggestive of achalasia: the bird-beak appearance of the distal oesophagus, and a dilated oesophagus (megaoesophagus) containing food residue, which may then progress to become tortuous (sigmoid) or aperistaltic. Thus, the use of these tests play a significant role in the identification of this condition.
Case presentation
Three patients were diagnosed with achalasia at the San Fernando General Hospital, Trinidad and Tobago. Together with characteristic symptoms, barium oesophagrams demonstrated features of achalasia, bearing a close resemblance to those of a caged bird. The barium oesophagrams were scrutinized by a fellowship trained, upper GI advanced laparoscopic surgeon, and the consistent features described were noted.
Conclusion
In the setting where manometry is not accessible, barium oesophagram plays an important role. We propose that recognition of easily identifiable features such as the “caged bird sign of achalasia” on this imaging modality can assist in the diagnosis of this entity.
1. Introduction
Achalasia was first described in 1672 by Sir Thomas Wills, where he treated a patient with cardiospasm by performing lower oesophageal dilation using a whale sponge attached to a whale bone. The actual name “achalasia” was given to the condition by Hurt and Rake in 1929 when they discovered that the disease process was as a result of failure of relaxation of the lower oesophageal sphincter [1]. With the improvement in technology, we are now able to easily make the diagnosis.
The diagnostic gold standard test for achalasia is oesophageal manometry; the American College of Gastroenterology guidelines suggest the use of oesophageal manometry once endoscopy excludes an anatomical cause for the patient’s symptoms [2]. In Trinidad and Tobago, a developing country, access to oesophageal manometry is extremely limited, and we therefore rely on the presentation of typical symptoms, together with characteristic features on other imaging modalities to aid in the diagnosis of achalasia. Barium oesophagram demonstrates easily recognisable features, such as a dilated oesophagus with distal narrowing (bird’s beak appearance), and delayed emptying into the stomach. However, there are other pathologies that are associated with the bird’s beak sign. For example, differentiation between a caecal volvulus and a caecal bascule seen on contrast enema, as well as incomplete obstruction of a sigmoid volvulus, also feature the bird’s beak sign [3,4].
Since this study is a retrospective look at one of the common tests used in the treatment protocol of achalasia, and no patients were denied the current gold standard care, ethical approval or registration of the study was not deemed to be required.
In this retrospective, single centre, non-consecutive study, three patients who were diagnosed with achalasia had the barium oesophagram reviewed by the same surgical consultant. This consultant is a fellowship trained, advanced laparoscopic, upper GI surgeon. The patients then underwent successful laparoscopic Heller’s myotomy with fundoplication. In an attempt to clarify the possible ambiguity of the bird’s beak sign, we wish to introduce the “caged bird sign of achalasia”, based on the appearances of their barium oesophagrams, which showed features of the abnormal oesophagus bearing semblance to that of a caged bird: a tapered lower oesophagus resembling a bird’s beak, dilated aperistaltic oesophagus resembling the head, body and tail of a bird, all enclosed by the thoracic cage. This case series was reported in accordance with the PROCESS guidelines [5].
2. Method
All confirmed cases of achalasia between January 2017 and December 2019 at a single tertiary hospital located in South Trinidad were included in this retrospective, observational study. The inclusion criteria were an oesophageal manometric diagnosis of achalasia and a barium meal. Three patients fulfilled the requirements.
The observation, description and analysis of the barium meal was done by a trained, minimally invasive, upper GI, laparoscopic surgeon. The study was registered with a research registry (UIN: researchregistry6015) and all required approvals were obtained [6].
Since this is an observational study, stills of the barium meal studies for each case were used to describe the sign, with the omission of all patient identifiers to maintain patient confidentiality.
3. Case 1
A patient with no previous comorbidities presented with a six month history of dysphagia to solids, regurgitation twenty minutes after eating, and associated weight loss of twenty pounds. Upper GI endoscopy showed a dilated oesophagus with delayed relaxation of the distal oesophagus.
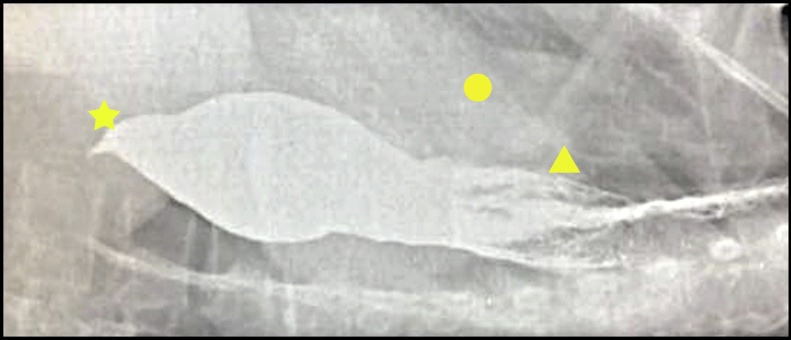
Barium oesophagram (Fig. 1) showed tapering of the distal oesophagus, a dilated oesophagus with diminished peristalsis, and delayed flow of contrast into the stomach.
Fig. 1.
Comparison between a bird and the Caged bird sign of achalasia.
The star shows the birds head and neck which is where the distal oesophagus tappers off. The triangle is in the area of the body and tail of the bird which is representative of the dilated portion of the oesophagus with food debris. The circle shows one rib of the thoracic cage encircling the bird.
4. Case 2
A patient presented with a two year history of dysphagia to solids. Upper GI endoscopy reported resistance to passage of the scope at the gastro-oesophageal junction, an akinetic, dilated oesophagus, and significant residual food debris within.
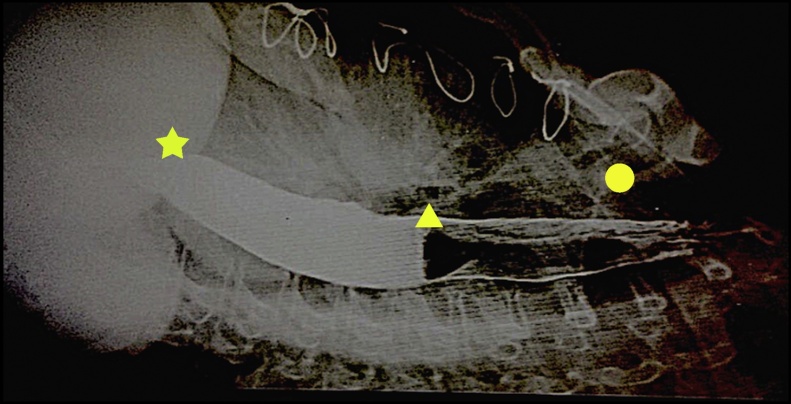
Barium oesophagram (Fig. 2) showed persistent dilation of the distal oesophagus with smooth tapering at the gastro-oesophageal junction.
Fig. 2.
The star shows the birds head and neck which is where the distal oesophagus tappers off. The triangle is in the area of the body and tail of the bird which is representative of the dilated portion of the oesophagus with food debris. The circle shows one rib of the thoracic cage encircling the bird.
5. Case 3
A 46 year old who had had a previous thymectomy, presented with a history of dysphagia to solids. Upper GI endoscopy reported delayed relaxation at the gastro-oesophageal junction, with a dilated and akinetic esophagus.
Barium oesophagram (Fig. 3) showed tapering at the gastro-oesophageal junction, a mildly dilated, aperistaltic oesophagus, and delayed passage of contrast into the stomach.
Fig. 3.
The star shows the birds head and neck which is where the distal oesophagus tappers off. The triangle is in the area of the body and tail of the bird which is representative of the dilated portion of the oesophagus with food debris. The circle shows one rib of the thoracic cage encircling the bird.
6. Discussion
Achalasia is characterised manometrically, by insufficient relaxation of the lower oesophageal sphincter (LOS) and a reduction in or absence of oesophageal peristalsis; radiographically by the “bird-beak” appearance suggesting poor emptying of barium, and endoscopically by a dilated oesophagus with retained saliva, liquid, and undigested food particles, in the absence of mucosal stricturing or tumour.
Typical findings for achalasia on oesophageal manometry include aperistalsis of the distal oesophagus, LOS resting pressure more than 45 mmHg, and incomplete LOS relaxation on swallowing. Although manometry is considered the gold standard, other radiological studies may be useful adjuncts, particularly in settings where manometry is not available [7].
Vantrappen et al. initially used the barium swallow while investigating patients being treated for achalasia. Features on barium oesophagram such as aperistalsis and dilation, narrowed gastroesophageal junction, and poor emptying into the stomach, can be used to support a diagnosis of achalasia when coupled with characteristic clinical symptoms [8,9]. These features are consistent with the typical bird’s beak sign. The caged bird sign localizes pathology to the thoracic cavity by identification an additional feature, viz. the rib cage, as opposed to the relative non-specificity of the rat-tail sign, which describes only the tapering of the viscus.
In Trinidad and Tobago, a developing country with very limited resources, our case series of barium oesophagram demonstrates features likened to those of a caged bird: the head of the bird representing tapering of the distal oesophagus due to failed relaxation of the LOS, the body and tail of the bird representing an aperistaltic, dilated oesophagus, and the bird’s cage representing the thoracic cage. This sign can be distinguished from other described bird’s beak signs as previously mentioned, and can possibly be diagnostic of achalasia for resource poor settings.
The cost of an upper GI endoscopic study and conventional manometry ranges between $600–$700 USD, and this facility is not available in our public setting, versus a barium oesophagram which is readily available to the patient from the public health care system. As such, many of our patients may have a barium oesophagram as the only available investigation. During this observational study, all radiographs were scrutinized by a specialist advanced, upper GI laparoscopic surgeon.We therefore propose that in a resource limited center, the caged bird sign would be a good diagnostic tool.
This study is limited by the small number of cases, as well as the small population studied, and the incidence of the disease is described as low in the quoted literature. Thus, a retrospective look at a larger, high flow center, with access to more scans can further substantiate these findings. Thus, a prospective study should be conducted with more institutions and as such an increase in the number of patients.
7. Conclusion
The features of achalasia can be easily demonstrated as closely resembling the appearance of a caged bird on barium oesophagram. In resource-limited settings, we propose that the recognition of this “caged bird sign” on barium oesophagram should be included as an easily recognisable, and possibly a diagnostic sign of achalasia.
Declaration of Competing Interest
There was no conflict of interest in this case series.
Funding
No funding was received for this case series.
Ethical approval
In light of this case series being a retrospective, observational study with no patient identifiers, no ethical approval was required at our institution.
Consent
Written informed consent was obtained from the patient for publication of this case series and accompanying images.
A copy of the written consent is available for review by the Editor-in-Chief of this journal on request
Author contribution
Yardesh Singh: Conceptualization, Methodology, Review and Editing, Supervision.
Aneela Shah: Writing original draft, Formal analysis, Methodology.
Sidiyq Mohammed: Writing original draft, Formal analysis, Methodology.
Narendra Samlal: Writing original draft, Review and Editing, Formal analysis.
Vijay Naryansingh: Review and Editing, Supervision.
Registration of research studies
-
1.
Name of the registry: Research Registry
-
2.
Unique identifying number or registration ID: UIN: researchregistry6015
-
3.
Hyperlink to your specific registration (must be publicly accessible and will be checked): Browse the Registry, (n.d.). https://www.researchregistry.com/browse-the-registry (accessed September 14, 2020).
Guarantor
Dr. Yardesh Singh is the guarantor of this case series.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Contributor Information
Yardesh Singh, Email: yardesh_singh@hotmail.com.
Sidiyq Mohammed, Email: sidiyq@gmail.com.
References
- 1.M.M. Achalasia Foundation [Internet]. All About Achalasia. Martin Muller IV Achalasia Awareness Foundation. [cited 2018Dec8]. Available from: http://achalasia.us/index.html.
- 2.Townsend . 20th ed. Elsevier; Philadelphia: 2017. Sabiston Textbook of Surgery; pp. 1016–1019. [Google Scholar]
- 3.Gaillard F. Bird Beak Sign (disambiguation) | Radiology Reference Article [Internet] https://radiopaedia.org/articles/bird-beak-sign-disambiguation Radiopaedia.org. [cited 2018Dec12]. Available from:
- 4.Mehmet Yigit K. Coffee bean sign, whirl sign and bird’s beak sign in the diagnosis of sigmoid volvulus [Internet] PubMed Central (PMC) 2018 doi: 10.11604/pamj.2014.19.56.5142. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4317068/ [cited 12 December 2018]. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Agha R.A., Borrelli M.R., Farwana R., Koshy K., Fowler A., Orgill D.P., SCARE Group The PROCESS 2018 statement: updating consensus preferred reporting of CasE series in surgery (PROCESS) guidelines. Int. J. Surg. 2018;60:279–282. doi: 10.1016/j.ijsu.2018.10.031. [DOI] [PubMed] [Google Scholar]
- 6.Browse the Registry, (n.d.). https://www.researchregistry.com/browse-the-registry (Accessed September 14, 2020).
- 7.El Kafsi Management of achalasia in the UK: do we need new guidelines? Ann. Med. Surg. 2016;12:32–36. doi: 10.1016/j.amsu.2016.10.009. [cited 2018 June 3] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Medscape [Internet] 2017. place unknown]: Medscape;c2005-2018. Achalasia Imaging. Feb 11 [cited 2018 June 3] [Google Scholar]
- 9.Kahrilas P., Boeckxstaens G. The spectrum of achalasia: lessons from studies of pathophysiology and high-resolution manometry. Gastroenterology. 2013;145(5):954–965. doi: 10.1053/j.gastro.2013.08.038. [DOI] [PMC free article] [PubMed] [Google Scholar]