Highlights
-
•
Retropharyngeal pseudomeningocele is a rare condition, which is usually detected weeks after trauma.
-
•
Early recognition and accurate diagnosis might help avoiding management delay and late intervention.
-
•
As surgical management is considered to be the definitive management, multidisciplinary management involving a team of Otolaryngology and Neurosurgery skull base surgeons is essential to achieve optimal outcomes.
Keywords: Case report, Pseudomeningocele, Atlanto-occipital dislocation, Retropharyngeal pseudomeningocele, Retropharyngeal cyst, Cervical trauma
Abstract
Introduction
Retropharyngeal pseudomeningocele is a very rare form of pseudomeningocele, that is known to be associated with cervical trauma. Identifying such pathology can be challenging leading to delayed management.
Case presentation
We report a case of post-traumatic retropharyngeal pseudomeningocele that was managed surgically in a 21-year-old gentleman with poly-trauma injuries due to a motor vehicle accident. After 10 weeks since the traumatic event, magnetic resonance imaging (MRI) and computerised tomography (CT) scan showed evidence of bilateral atlanto-occipital dislocation and a fluid collection of 8 × 4 × 2 cm in the retropharyngeal space. The patient was found to have dysphagia and muffled voice with difficult visualisation of the vocal cords upon examination. After a multidisciplinary team decision, the patient underwent cerebrospinal fluid (CSF) leak management, pseudomeningocele resection and dural defect repair with shunting conducted by the Neurosurgery and Otolaryngology. Postoperative assessments and patient's symptoms, at 9 months follow-up, were satisfactory and reassuring.
Discussion
It’s believed that conservative management with bed rest, elevation of bed head and acetazolamide is the initial step in management. As an alternative measure, shunting of the CSF had led to resolution of the collection. However, surgical removal of the collection and direct dural defect repair have been suggested in the literature but needed to be properly studied.
Conclusion
Early recognition of this condition is important to avoid management delay. With a multidisciplinary approach, surgical management can be safe and an acceptable option for retropharyngeal pseudomeningocele.
1. Introduction
Pseudomeningocele is an extremely rare condition of cerebrospinal fluid (CSF) collection, due to leakage of CSF through a dural defect or tear into an extradural sac [1]. It is believed that a tear in the dura with an intact arachnoid will lead to herniation of an arachnoid-like sac, while a dural-arachnoid tear will lead to leakage of CSF into the surrounding soft tissue, which might be encapsulated with a fibrous capsule [2,3]. The dural defect can form a ball-valve way for the outflow of CSF, leading to the development of a pseudomeningocele [4]. Pseudomeningoceles, if occurred, are seen mostly in the lumbar region and rarely in the cervical spine region [5]. The most common cause of pseudomeningocele is iatrogenic due to the violation of the dura’s integrity after spine surgery [[6], [7], [8]]. Less frequently, it can be secondary to traumatic causes [3]. While post-trauma pseudomeningocele is rare, a retropharyngeal pseudomeningocele is extremely rare and is strongly, if not exclusively, associated with cervical trauma [1,9]. Its management might be delayed as its recognition can be challenging [1]. This case report has been written in line with the SCARE criteria [10].
2. Case report
We report the case of a 21-year-old gentleman with poly-trauma injuries due to a motor vehicle accident, including skull base fracture with cistern hemorrhage, subdural hemorrhage, bilateral atlanto-occipital dislocation and a splenic laceration. He was managed by a different healthcare provider before his presentation to our institution. At 10 weeks after the traumatic event, a retropharyngeal cyst like mass was detected by magnetic resonance imaging (MRI) prior to occipitocervical fixation. It was diagnosed as a retropharyngeal abscess and managed accordingly with incision and drainage (I&D).
The Otolaryngology service was consulted at day 7 post-op due to recurrence of the retropharyngeal mass despite previous medical and surgical management including antibiotic therapy. Decannulation was attempted but failed, and visualisation of the larynx was not possible due to a large cystic mass in the posterior wall of oropharynx.
Computerised tomography (CT) scan and MRI showed a fluid collection of 8 × 4 × 2 cm in the retropharyngeal space, extending from the skull base (atlanto-occiptal joint) to the level of the base of the tongue, also pneumocephalus secondary defect at skull base (Fig. 1).
Fig. 1.
Retropharyngeal cyst.
Sagittal T2-weighted MRI image showing torn tectorial ligament with CSF leak forming a collection of 8 × 3 × 2 cm in the retropharyngeal space. The cyst shows smooth and regular wall enhancement.
The patient was reevaluated at 6 months since the traumatic event and was found to have dysphagia, muffled voice and signs of recollection and more symptomatic as stated by the patient and with difficult visualisation of the vocal cords. After a multidisciplinary team decision, the patient underwent CSF leak management, pseudomeningocele resection and dural defect repair with shunting conducted by the Neurosurgery and Otolaryngology.
Intraoperatively, through transpalatal (palatal split) approach, the dural defect at the level of C1 was identified. The defect was adequately dissected and exposed, the edges were freed and refreshed till oozing was seen to enhance the healing process and avoid residual tract as the site of CSF leak was evident with a gush of watery fluid. The defect was repaired with a muscle graft placement, and TISSEEL fibrin sealant was applied to achieve hemostasis and sealing. Then, with a transoral approach, the retropharyngeal space was exposed by a vertical incision of the posterior wall of the oropharynx. CSF collection was drained, and the fibrous layer formed on the retropharyngeal space wall was excised using a scalpel blade to enhance healing and closure (Fig. 2). An external ventricular drain (EVD) was inserted to prevent secondary leak, enhance the healing process and reduce the intracranial pressure. After achieving satisfactory hemostasis, wounds were closed using a 4-0 vicryl suture.
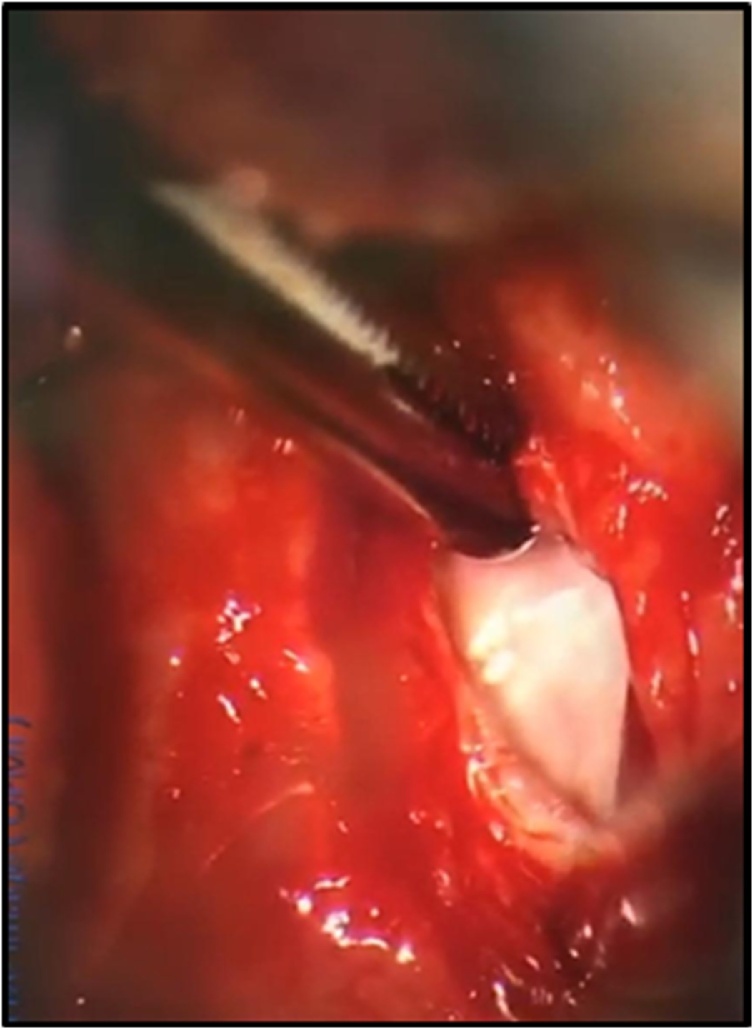
Fig. 2.
Intraoperative image of oropharynx area.
Fibrous layer formed on the retropharyngeal space wall, was clear during the surgery after drainage of CSF collection.
At 9 months follow up, MRI imaging findings, which showed total resolution of the pouch and complete resolution of pneumocephalus (Fig. 3), were reassuring and the patient showed improved symptoms with satisfactory speech and swallowing functions.
Fig. 3.
Post-resection of the pseudomeningocele.
Sagittal T2-weighted MRI image showing complete resolution of the retropharyngeal collection and patent upper airway.
3. Discussion
Pseudomeningocele is a rare condition of cerebrospinal fluid (CSF) collection, due to leakage of CSF through a dural defect or tear into an extradural sac [1]. The most common cause is iatrogenic due to violation of the dura’s integrity after spine surgery [[6], [7], [8]]. While post-trauma pseudomeningocele is rare, a retropharyngeal pseudomeningocele is believed to be extremely rare and is strongly, if not exclusively, associated with cervical trauma [1,9]. In the English literature, we found only 9 reported cases of retropharyngeal pseudomeningocele [1,5,[9], [10], [11], [12], [13], [14], [15]]. The incidence of the presented pathology is not yet clear due to its rarity [16]. Majority of the reported cases were victims of motor vehicle accidents [1,5,9,[11], [12], [13]]. Two of them were pedestrians [9,12]. While all reported cases were associated with a witnessed traumatic event, there is one reported case of an intoxicated patient who was found unconscious with cervical vertebrae dislocation, yet the authors could not rule out the possibility of trauma [14].
The detection of retropharyngeal pseudomeningocele is usually made days to weeks after the traumatic event [11]. As in this case, symptoms are usually attributed to the mass effect, disturbing the swallowing and obstructing the airway [1]. Failure to wean off mechanical ventilation and the development of respiratory failure during extubation are the most common presentations [1,5]. Moreover, dysphagia, difficulty in intubation and even incidental finding on imaging studies have also been reported [1,5,9,13]. The need for tracheostomy tube insertion and enteral feeding have been reported frequently in these cases [1,9,13]. In this case, the patient suffered multiple traumatic injuries from a high-speed motor vehicle accident. And, he required multiple interventions for these injuries, including tracheostomy. Ten weeks after the traumatic event, a retropharyngeal mass was detected incidentally on a preoperative MRI for the preparation of an occipito-cervical fixation. The patient was found to have atlantooccipital dislocation and atlanto-axial ligaments tear before the appearance of the retropharyngeal collection. These findings were suggested in the literature to predispose the development of retropharyngeal pseudomeningocele [16]. MRI is the mainstay diagnostic modality in detecting retropharyngeal pseudomeningocele [1]. The extradural collection represents the radiological characteristics of CSF on MRI, as low signal intensity on T1 and high signal intensity on T2 [3]. A dural defect and level of communication may be identified on MRI; however, CT myelography may have better utilisation in visualizing the location of the defect [3]. Head CT is recommended upon the confirmation of the presence of retropharyngeal pseudomeningocele to rule out concomitant hydrocephalus [12], as half of the reported cases in the literature had developed hydrocephalus in association with the presented pathology [9,11,13].
Surgical treatment is generally considered as the definitive management of pseudomeningoceles [3]. Conservative management with bed rest, elevation of bed head and acetazolamide is the initial step for the management of retropharyngeal pseudomeningocele [1,5]. As an alternative measure, shunting of the CSF had led to resolution of the collection, and it succeeded in majority of the survived patients regardless of morbidity [1,9,11,14]. It is suggested that ventriculo-peritoneal shunt is indicated in the presence of hydrocephalus [5]. In the absence of hydrocephalus, a lumbo-peritoneal shunt is the procedure of choice [5]. However, in our case, surgical removal of the collection and direct dural defect repair have been suggested but needed to be properly studied and reported in the literature. The outcome in the reported cases was greatly determined by the other associated injuries and the consequences of the traumatic force rather than being related solely to the pseudomeningocele [1]. However, surgical repair of retropharyngeal pseudomeningocele was challenging for some cases because of the following: difficulty in approaching the site of the defect, increased risk of developing meningitis, or severe morbidity such as poor neurological function [1,5,16]. Indications for surgical management were proposed as failure of conservative management or the presence of progressive signs and symptoms of neurological injury [3].
4. Conclusion
Post-trauma pseudomeningocele is a rare complication. Recognition and accurate diagnosis are important to avoid management delay or avoidable complications. Surgical technique might be challenging; therefore, multiple disciplinary management involving a team of Otolaryngology and Neurosurgery skull base surgeons is essential to achieve optimal outcomes.
Declaration of Competing Interest
None.
Funding
None.
Ethical approval
The study has been approved by our research centre and IRB committee at Dr Suliman Al Habib Medical Group.
Consent
Written informed consent for the publication of this study has been obtained from the patient.
Author contribution
Naif H. Alotaibi MD: First author, treating physician, data collection, and writing – supervision, review and editing.
Abdullah J. AlShehri: First author, writing and editing – original draft, data collection and finalized the manuscript.
Osamah H. Alshankiti MD: Second author, contributed at treating the patient, revised manuscript.
Ibrahim AlThubaiti MD: Last author, the primary physician – treating and following up the patient, revised manuscript.
All authors approved the final version of the manuscript
Registration of research studies
Name of the registry: Dr Suliman Al Habib Medical Group, Al Habib Research Centre, Institutional Review Board (IRB) committee, 3rd project 29/04/2020.
Guarantor
Naif H. Alotaibi MD, Associate professor, College of Medicine, Alfaisal University, Department of Otolaryngology, Dr. Suliman Al Habib Medical Group, Riyadh, Saudi Arabia.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Acknowledgement
None.
References
- 1.Gutiérrez-González R., Boto G.R., Pérez-Zamarrón A., Rivero-Garvía M. Retropharyngeal pseudomeningocele formation as a traumatic atlanto-occipital dislocation complication: case report and review. Eur. Spine J. 2008;17(Suppl 2):S253–S256. doi: 10.1007/s00586-007-0531-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Couture D., Branch C.L., Jr. Spinal pseudomeningoceles and cerebrospinal fluid fistulas. Neurosurg. Focus. 2003;15(6):E6. doi: 10.3171/foc.2003.15.6.6. [DOI] [PubMed] [Google Scholar]
- 3.Hawk M.W., Kim K.D. Review of spinal pseudomeningoceles and cerebrospinal fluid fistulas. Neurosurg. Focus. 2000;9(1) doi: 10.3171/foc.2000.9.1.5. e5. [DOI] [PubMed] [Google Scholar]
- 4.Natale M., Bocchetti A., Scuotto A., Rotondo M., Cioffi F.A. Post traumatic retropharyngeal pseudomeningocele. Acta Neurochir. 2004;146(7):735–739. doi: 10.1007/s00701-004-0272-x. [DOI] [PubMed] [Google Scholar]
- 5.Cobb C., 3rd, Ehni G. Herniation of the spinal cord into an iatrogenic meningocele. Case report. J. Neurosurg. 1973;39(4):533–536. doi: 10.3171/jns.1973.39.4.0533. [DOI] [PubMed] [Google Scholar]
- 6.Jones A.A., Stambough J.L., Balderston R.A., Rothman R.H., Booth R.E., Jr Long-term results of lumbar spine surgery complicated by unintended incidental durotomy. Spine. 1989;14(4):443–446. doi: 10.1097/00007632-198904000-00021. [DOI] [PubMed] [Google Scholar]
- 7.Lee K.S., Hardy I.M., 2nd Postlaminectomy lumbar pseudomeningocele: report of four cases. Neurosurgery. 1992;30(1):111–114. doi: 10.1227/00006123-199201000-00020. [DOI] [PubMed] [Google Scholar]
- 8.O’Connor D., Maskery N., Griffiths W.E. Pseudomeningocele nerve root entrapment after lumbar discectomy. Spine. 1998;23(13):1501–1502. doi: 10.1097/00007632-199807010-00014. [DOI] [PubMed] [Google Scholar]
- 9.Reed C.M., Campbell S.E., Beall D.P., Bui J.S., Stefko R.M. Atlanto-occipital dislocation with traumatic pseudomeningocele formation and post-traumatic syringomyelia. Spine. 2005;30(5):E128–E133. doi: 10.1097/01.brs.0000154654.37815.01. [DOI] [PubMed] [Google Scholar]
- 10.Agha R.A., Borrelli M.R., Farwana R., Koshy K., Fowler A.J., Orgill D.P., SCARE Group The SCARE 2018 statement: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2018;60:132–136. doi: 10.1016/j.ijsu.2018.10.028. [DOI] [PubMed] [Google Scholar]
- 11.Cognetti D.M., Enochs W.S., Willcox T.O. Retropharyngeal pseudomeningocele presenting as dysphagia after atlantooccipital dislocation. Laryngoscope. 2006;116(9):1697–1699. doi: 10.1097/01.mlg.0000231737.67781.df. [DOI] [PubMed] [Google Scholar]
- 12.Naso W.B., Cure J., Cuddy B.G. Retropharyngeal pseudomeningocele after atlanto-occipital dislocation: report of two cases. Neurosurgery. 1997;40(6):1288–1291. doi: 10.1097/00006123-199706000-00033. [DOI] [PubMed] [Google Scholar]
- 13.Williams M.J., Elliott J.L., Nichols J. Atlantooccipital dislocation: a case report. J. Clin. Anesth. 1995;7(2):156–159. doi: 10.1016/0952-8180(94)00031-x. [DOI] [PubMed] [Google Scholar]
- 14.Achawal S., Casey A., Etherington G. Retropharyngeal pseudomeningocele. Br. J. Neurosurg. 2006;20(4):259–260. doi: 10.1080/02688690600875341. [DOI] [PubMed] [Google Scholar]
- 15.Louati A., Hadhri K., Tebourbi A., Kooli M. Traumatic retropharyngeal pseudomeningocele following C5-C6 subluxation. Neurol. India. 2017;65(1):226–227. doi: 10.4103/0028-3886.198216. [DOI] [PubMed] [Google Scholar]
- 16.Qiu R.S., Safain M.G., Shutran M., Hernandez A.M., Hwang S.W., Riesenburger R.I. Early identification of traumatic durotomy associated with atlantooccipital dislocation may prevent retropharyngeal pseudomeningocele development. Case Rep. Surg. 2015;2015 doi: 10.1155/2015/361764. [DOI] [PMC free article] [PubMed] [Google Scholar]