Highlights
-
•
Child sexual abuse is a reality in black Africa.
-
•
Detection of anogenital lesions during a paediatric consultation must evoke the possibility of sexual abuse.
-
•
In such cases, it’s important to “listening to the child’s voice”.
Abbreviations: CSA, Child sexual abuse
Keywords: Child sexual abuse, Anogenital lesion, Surgery, Africa, Case series
Abstract
Introduction
Child sexual abuse (CSA) remains a big taboo in black Africa with an underestimated prevalence. In our context, the majority of cases are known by revelations of the child at least one year after the facts.
Presentation of cases
We report three cases of CSA revealed by an anal/anogenital lesion requiring surgery. All of these patients were female with ages ranging from 20 months to 8 years. The lesions encountered were: an anal abscess, a fissure-in-ano with permanent anal mucosal eversion and a complex perineal tear including partial anal sphincter rupture with partial section of the rectovaginal septum. The outcome was favorable in all cases after surgery. The abuser was subsequently able to be identified after the statements of two of these three children.
Discussion
Detection of anogenital lesions during a pediatric consultation should make practitioners aware of the possibility of sexual abuse. Surgical repair of these lesions can be simple or complex, requiring major reconstructions. In such cases, it’s important to listening to the child’s voice.
Conclusion
Anogenital lesions discovered during pediatric consultation must evoke sexual abuse. The silence and the taboo surrounding these abuses in Africa must be break down.
1. Background
According to WHO, child sexual abuse (CSA) is the involvement of a child in sexual activity that he/she does not fully understand and/or is unable to give informed consent [1,2]. Globally, the prevalence of genito-anal injuries after sexual abuse is estimated between 9% and 87% depending on the ages of the survivors in the sample, method of examination and the type of injuries included [[3], [4], [5]].
The earliest study of CSA in Africa dates back in 1984 by Westcott et al., who described 18 cases at a Cape Town hospital [6]. In Cameroon, several studies have been done on sexual abuse involving minors [[7], [8], [9], [10]]. These studies have estimated the prevalence ranging from 2.05 to 4.69% in hospitals [7], 9.5% in a judicial environment [8] and nearly 16% in schools [9]. Mbassa et al. [9] in 2012 further demonstrated, in a cohort study, that rape with vagina/anal penetration was the main type of CSA (81.5%) in Cameroon [9].
In both developing and developed countries, recognizing CSA is difficult, due to many hurdles among which the silence of the victims [1,11,12]. CSA remains a big taboo in black Africa. In Cameroon, 74.1% of the abuses are known after children purposefully disclosure, and 50% of them after at least one year [9]. To the best of our knowledge no study has described anal or anogenital injuries in children abused sexually in Cameroon. Herein, we report the management of three consecutive cases of CSA revealed by different anal pathologies in a black African setting, at the Yaoundé’ University Teaching Hospital (Cameroon) over a five-year period (from 2015 to 2019). This article complies with the SCARE 2018 guidelines for reporting surgical case series [13] and has been reported in line with the PROCESS criteria [14]. This study has been registered in Research Registry under the Unique Identifying number (UIN) 5940 [15].
2. Presentation of cases
2.1. Case 1
A 3 years 5 months old female was received, accompanied by her parents, with febrile anal pain persisting for 96 h. This was associated, several hours ago, with a purulent offensive anal discharge and a painful defecation. On examination, the child had a temperature of 38.5 °C with a tachycardia, right inflammatory and fluctuating perianal swelling, anal yawning and abrasions with preserved sphincters (Fig. 1A). The diagnosis of anal abscess was then retained. Biological investigations revealed a leucocytosis with a negative HIV serology. The treatment consisted of administration of intravenous antibiotics followed by an incision and drainage of the abscess. Postoperative course was uneventful with a discharge at postoperative day five and a total regression of anal lesions (Fig. 1B). On further postoperative inquiry, the child revealed that an “uncle’’ in school put “a stick in her buttocks” and judicial investigations identified the school guard as the abuser. A psychological follow-up of the child was initiated and the HIV serology was negative 3 months later.
Fig. 1.
Anal abscess following child sexual abuse. 1A: Right inflammatory perianal swelling with anal yawning. 1B: Regression of lesions at postoperative day 12.
2.2. Case 2
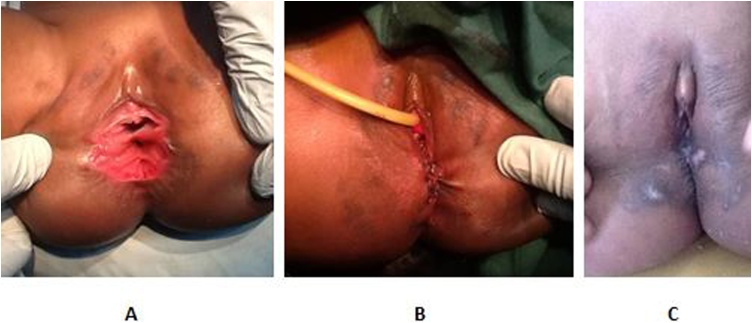
An 8 years old female was received in our consultation with constipation and painful defecation. She had been an orphan since the age of 5 and was then placed in a foster family, from where she ran away few months earlier. Placed in another family since few days, her new parents found that she had difficulties to pass stools normally, thus motivated a consultation in our hospital. The examination was remarkable of a permanent eversion of the anal mucosa with fissure (Fig. 2A). The diagnosis of fissure in ano was then advocated. On further inquiry, the patient declared that “My former father usually comes to my room in the night to inject me in the buttocks”. Laboratory investigations were normal with a negative HIV serology at the admission and 3 months later too. A surgical treatment was performed, consisting of a lateral sphincterotomy and an “U” mucosal anoplasty (Fig. 2B). The Patient was discharged on post-operative day 1. Further follow-up showed a good cosmetic (Fig. 2C) and functional evolution with normal defecation. A psychological follow-up was initiated. Arrested by the police, the former father recognized the facts.
Fig. 2.
Fissure-in-ano following child sexual abuse. 1A: pre-operative view fissure-in-ano (black arrow) and permanent mucosal eversion. 1B: Immediate postoperative view. 1C: Good cosmetic result at postoperative day 12.
2.3. Case 3
A 20 months old female infant was taken in our hospital by her mother for frequent stools and abnormal aspect of the perineum. The mother was 17 years old and had never been to school. Single mother, she had entrusted her daughter to her parents 4 months earlier, for a job in a neighboring town. On her return three months later, she notes that her child passes an average of 6 stools per day compared to 2 previously; moreover, she finds ” weird” the aspect of perineum. During the following 4 weeks, she administered to the child a traditional treatment without any improvement, and therefore decided to consult in our hospital. On examination we found signs of mild dehydration and normal vital signs. There was a complex perineal tear (Fig. 3A) including an anal yawning with partial sphincter rupture, a partial section of the rectovaginal septum, absence of hymen with vaginal yawning. The HIV serology was negative at the admission and 3 months later too. The treatment consisted of adequate rehydration protocol followed by surgery. We performed an anal sphincteroplasty with overlapping sutures, vaginoplasty with insertion of an urinary catheter and perineoplasty. The post-operative cosmetic result was good (Fig. 3A and B) as well as the functional one (2–3 stools per day). Questioned by the police, the grandfather confessed to having regularly raped the infant during the three months during which she had been entrusted to him.
Fig. 3.
Complex perineal tear after child sexual abuse. 1A: pre-operative view an anal yawning with partial sphincter rupture, a partial section of the rectovaginal septum and vaginal yawning. 1B: Immediate postoperative view. 1C: Postoperative view at day 90.
3. Discussion
Despite multiples studies highlighting its existence [[6], [7], [8], [9], [10]], CSA remains a big taboo in black Africa. Their prevalence in sub-Saharan countries is certainly under estimated; families often prefer an amicable settlement followed by traditional rites of purification to the dishonor of a public trial [16]; Poverty, with difficulties to bear the cost of legal proceedings or medical fees, could also be another explanation. Child sexual abuse in Africa is also hidden in plain sight under teenage pregnancy and child marriage [17]. All of this comes at the expense of children's mental and physical health.
In our context, the abuse is known in the majority of cases (74.1%) after revelations of the child at least one year after the facts and only 3.7% after anogenital lesions [9]. Thus, receiving three consecutive cases of anogenital lesions revealing sexual abuse is unusual in an African hospital environment. Anal sexual abuse in children may present acutely as bleeding or bruising and chronically as chronic stellate lacerations of the anus with lymphoedema but also as anal fissures [3,18,19]. In our report, we had three different presentations: anal abscess, fissure-in-ano with permanent mucosa eversion, complex perineal tear with both anal and vagina lesions. Detection of anogenital lesions during a pediatric consultation should make practitioners aware of the possibility of sexual abuse; These signs may be used in court to provide corroboration for proceedings [18].
Surgical repair of anogenital lesions after CSA can be simple or complex, requiring major reconstructions. Our three observations highlight this fact, with gestures ranging from abscess drainage to a perineal reconstruction. The medical follow-up of these patients will be done over the long term; in addition to the anal sphincter function, the obstetric prognosis can be degraded by certain lesions.
Unlike a previous Cameroonian study which found that 37.5% of CSA victims had been infected with HIV [10], our three patients remained HIV negative. They were however received beyond the 72-h period following the exposure, enabling the initiation of preventive antiretroviral therapy. HIV infection remains one of the challenges in case of CSA.
Our cases also highlight the importance listening to the child's voice. Indeed, the statements of two of them, one aged less than 4 years old, made possible to know who their assailant was.
4. Conclusion
CSA is a reality in Africa. If in the majority of cases the child reveals its assault at least one year later, these abuses may be revealed by anal or anogenital injuries. Thus, detection of anogenital lesions during pediatric consultation must evoke sexual abuse. Although surgery occupies a preponderant place in the treatment of such lesions, the management of CSA must be part of a multidisciplinary approach.
Declaration of Competing Interest
The authors report no declarations of interest.
Funding
No funding sources.
Ethical approval
The study was submitted to and approved by the ethics committee of the Faculty and Medicine and Biomedical Sciences of the University of Yaoundé I.
Consent
Written informed consent was obtained from the patient’s guardian for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contribution
Patients was admitted and operated under the care of GAB and GBM. GAB concepted the study. PT, EPS and GBM collected and analyzed the data. GAB wrote the paper. MAS revised the work and give the final approval.
Registration of research studies
-
1.
Name of the registry: Research Registry
-
2.
Unique identifying number or registration ID: 5940
-
3.
Hyperlink to your specific registration (must be publicly accessible and will be checked): https://www.researchregistry.com/browse-theregistry#home/registrationdetails/5f43f6374b3d600016361089/.
Guarantor
Maurice Aurélien SOSSO, Professor of general surgery at the Faculty of medicine and Biomedical Sciences of the university of Yaoundé I (Cameroon).
Provenance and peer review
Not commissioned, externally peer-reviewed.
Acknowledgments
The authors wish to acknowledge the help provided for this study by Pierre René BINYOM, Yannick Mahamat EKANI BOUKAR and Arthur ESSOMBA especially in the management of these cases and in manuscript reviewing.
Contributor Information
Guy Aristide Bang, Email: guyaristidebang@yahoo.fr.
Paul Tolefac, Email: ptolefac15@gmail.com.
Eric Patrick Savom, Email: esavom@yahoo.fr.
Georges Bwelle Moto, Email: gbwelle@gmail.com.
Maurice Aurélien Sosso, Email: sossomaurice@yahoo.fr.
References
- 1.Badoe E. A critical review of child abuse and its management in Africa. Afr. J. Emerg. Med. 2017;7:32–35. doi: 10.1016/j.afjem.2017.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wolfe D.A., Pierre J.S. Child abuse and neglect. In: Ollendick T.H., Hersen M., editors. Handbook of Child Psychopathology. Springer US; Boston: 1989. pp. 377–398. [DOI] [Google Scholar]
- 3.Jina R., Jewkes R., Vetten L., Christofides N., Sigsworth R., Loots L. Genito-anal injury patterns and associated factors in rape survivors in an urban province of South Africa: a cross-sectional study. BMC Womens Health. 2015;15:29. doi: 10.1186/s12905-015-0187-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Astrup B.S., Ravn P., Thomsen J.L., Lauritsen J. Patterned genital injury in cases of rape—a case-control study. J. Forensic Leg. Med. 2013;20(5):525–529. doi: 10.1016/j.jflm.2013.03.003. [DOI] [PubMed] [Google Scholar]
- 5.Lincoln C., Perera R., Jacobs I., Ward A. Macroscopically detected female genital injury after consensual and non-consensual vaginal penetration: a prospective comparison study. J. Forensic Leg. Med. 2013;20(7):884–901. doi: 10.1016/j.jflm.2013.06.025. [DOI] [PubMed] [Google Scholar]
- 6.Westcott D.L. Sexual abuse of children - a hospital-based study. S. Afr. Med. J. 1984;65(22):895–897. [PubMed] [Google Scholar]
- 7.Mbassa Menick D. Les abus sexuels en milieu scolaire au Cameroun résultats d’une recherche-action à Yaoundé. Med. Trop. 2002;62:1–58. [PubMed] [Google Scholar]
- 8.Mbassa Menick D. La problématique des enfants victimes d’abus sexuels en Afrique ou l’imbroglio d’un double paradoxe: l’exemple du Cameroun. Child Abuse Negl. 2001;25(1):109–121. doi: 10.1016/s0145-2134(00)00220-9. [DOI] [PubMed] [Google Scholar]
- 9.Mbassa Menick D., Bang G.A., Abanda Ngon G. Mineurs (inces)-tués, parents complices? Approche épidémiologique des violences sexuelles intrafamiliales en Afrique. Perspect. Psychol. 2012;51(2):124–133. [Google Scholar]
- 10.Mbassa Menick D., Ngoh F. Séroprévalence de l’infection à VIH chez les enfants victimes d’abus sexuels au Cameroun. Med Trop. 2003;63(2):155–158. [PubMed] [Google Scholar]
- 11.Acharya P.N., Gill D.S. The physical signs of child sexual abuse. An evidence-based review and guidance for best practice. Br. Dent. J. 2008;205:55. [Google Scholar]
- 12.Madu S.N., Peltzer K. Prevalence and patterns of child sexual abuse and victim–perpetrator relationship among secondary school students in the Northern Province (South Africa) Arch. Sex. Behav. 2001;30(3):311–321. doi: 10.1023/a:1002704331364. [DOI] [PubMed] [Google Scholar]
- 13.Agha R.A., Borrelli M.R., Farwana R., Koshy K., Fowler A., Orgill D.P., SCARE Group The SCARE 2018 statement: updating consensus surgical case report (SCARE) guidelines. Int. J. Surg. 2018;(60):132–136. doi: 10.1016/j.ijsu.2018.10.028. [DOI] [PubMed] [Google Scholar]
- 14.Agha R.A., Borrelli M.R., Farwana R., Koshy K., Fowler A., Orgill D.P., PROCESS Group The PROCESS 2018 statement: updating consensus preferred reporting of case series in surgery (PROCESS) guidelines. Int. J. Surg. 2018;(60):279–282. doi: 10.1016/j.ijsu.2018.10.031. [DOI] [PubMed] [Google Scholar]
- 15.Research Registry. https://www.researchregistry.com/browse-theregistry#home/registrationdetails/5f43f6374b3d600016361089/. (Accessed 23 September 2020).
- 16.Mbassa Menick D., Ngoh F. Réconciliation et/ou médiation comme voies de recours en cas d’abus sexuels sur mineurs au Cameroun. Med Trop. 1999;59:161–164. [PubMed] [Google Scholar]
- 17.Ramabu N.M. The extent of child sexual abuse in Botwana: hidden in plain sight. Heliyon. 2020;6(4):e03815. doi: 10.1016/j.heliyon.2020.e03815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hobbs C.J., Wright C.M. Anal signs of child sexual abuse: a case–control study. BMC Pediatr. 2014;14:128. doi: 10.1186/1471-2431-14-128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ameh E.A. Anal injury and fissure-in-ano from sexual abuse in children. Ann. Trop. Paediatr. 2001;21(3):273–275. doi: 10.1080/02724930120077871. [DOI] [PubMed] [Google Scholar]