Abstract
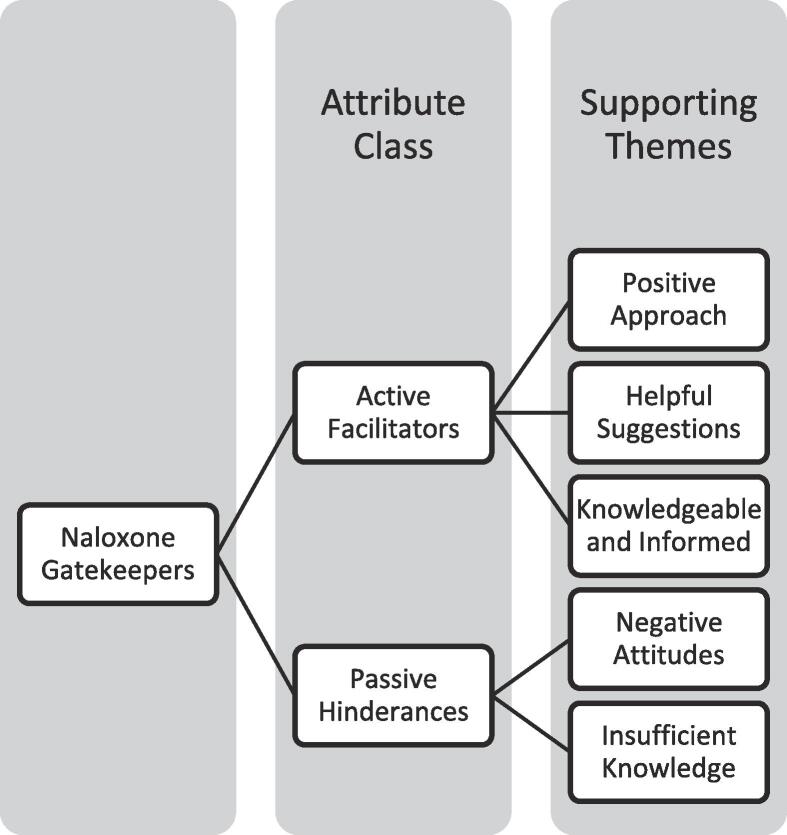
Given their critical gatekeeper function regarding naloxone access in rural areas, the purpose of the current study was to examine rural pharmacists’ knowledge and attitudes regarding naloxone use and access (Georgia, 2019), all 364 rural community pharmacies in Georgia were contacted using “secret shopper” methodology and asked about the availability, accessibility, and use of naloxone. A script provided specific questions for data collection. Callers recorded general notes about the call, including the dispositions and impressions of the pharmacists. Thematic analysis was conducted to identify key themes. Rural pharmacists exhibited two classes of attributes: Active Facilitators and Passive Hindrances. Active facilitators supported callers in their search for naloxone, but passive hindrances discouraged callers in a way that was not perceived to be malicious or intentional. Three types of active facilitators emerged: positive approach, helpful suggestions, and knowledgeable and informed. Two types of passive hindrances emerged: negative attitudes and insufficient knowledge. Community pharmacies are sometimes the only formal healthcare access point in rural communities. It is vital for pharmacists to be active facilitators of naloxone access for maximized public health impact. Specific interventions are needed to increase the ability of rural pharmacists to support access to naloxone.
Keywords: Rural, Opioid, Naloxone, Pharmacists, Standing orders
1. Introduction
The ongoing opioid crisis in the United States has become more apparent to the public, and for good reason. It is estimated that every day more than 128 people in the United States die from opioid overdose (CDC/NCHS, 2018). The epidemic has hit rural America exceedingly hard, especially in Appalachia. Appalachian counties have a near unbelievable opioid prescription rate of 84 prescriptions per 100 residents and an opioid overdose rate that is over 70% higher than that seen in non-Appalachian counties (National Association of Counties and the Appalachian Regional Commission, 2019). Georgia, a state with 37 Appalachian counties, has seen the crisis unfold in striking fashion. From 1999 to 2017, the opioid overdose mortality rate in rural counties increased from 0.5 deaths per 100,000 people to 9.5 per 100,000 people, representing a staggering 19-fold increase (Georgia, 2019).
In response to the opioid crisis, every state has increased naloxone access through expanded prescribing methods. Naloxone, a pure opioid antagonist, reverses opioid overdoses, which can help prevent opioid-related deaths and disabilities. Providing naloxone to individuals, friends, and family members of people at risk of overdose can reduce the time to overdose rescue and improve outcomes (Guy et al., 2019). The most popular mechanism is statewide standing protocols/orders, which allow community pharmacists to dispense naloxone to patients who seek the medication without a prescription (Davis and Carr, 2017). However, prior research showed slow adoption of stocking and dispensing the medication under standing orders (Correal, 2018, Meyerson et al., 2018). A recent report has shown an increase in naloxone dispensing from retail pharmacies from 2012 to 2018, although rural counties had a higher likelihood of having low rates of naloxone dispensing (Guy et al., 2019).
As frontline healthcare providers (particularly in rural areas), pharmacists are crucial gatekeepers and have a critical hand in decreasing overdose mortality. Pharmacists have previously been referred to as gatekeepers, noting their ability to “label client’s behavior and subsequently grant or withhold access to resources” (Chiarello, 2013) and highlighting their unique positions to prevent medication abuse and dependence (Shimane, 2013). While the law does not require naloxone to be stocked, pharmacists are expected to be knowledgeable about the relevant laws in their state. It is unclear, however, the extent to which rural pharmacists are aware of and support standing orders. A previous study explored the availability of naloxone at rural Georgia pharmacies, and found that just over half of the pharmacies carried naloxone, but 47.1% of pharmacists gave incorrect information regarding the need for a prescription to obtain naloxone (Nguyễn et al., 2020). This qualitative study conducted a thematic analysis of rural pharmacist knowledge and attitudes regarding naloxone access in all rural pharmacies in Georgia during those calls.
2. Methods
This project focuses on pharmacies in legislatively designated rural counties in Georgia, where the state-wide standing order allows individuals to obtain naloxone without a prescription (Standing order for prescription of naloxone for overdose prevention, 2017, Georgia Department of Community Health. Georgia Rural County Map, 2008). A list of pharmacies was provided by the state’s Board of Pharmacy (Georgia, 2019). The research team also conducted a secondary check to ensure the list’s comprehensiveness. There were 2,453 total pharmacies, 374 of which met eligibility criteria: rural, in service, retail (chain and independent) community pharmacy (not a compounding or mail-order pharmacy). Trained researchers called pharmacies seeking information about the availability and accessibility of the name brand naloxone (i.e. Narcan). Researchers asked each location to speak to the pharmacist only. The “secret shopper method” has been used for previous research regarding pharmacy accessibility of birth control (Bullock et al., 2016, French and Kaunitz, 2007). Pharmacists were not informed the calls were part of a research study, the calls were not recorded, and no identifying information was recorded. The list verification and phone calls were completed within a three-month time frame. This research was exempted by the university’s institutional review board.
Researchers posed as patients calling to get information regarding naloxone. A phone script provided specific questions for data collection, which included a decision tree based on responses. The data collection tool was developed in consultation with pharmacy practice faculty who had extensive pharmacy expertise and practicing retail pharmacists (Nguyễn et al., 2020). Callers also recorded general notes about the call, including the dispositions and impressions of the pharmacists. Multiple norming sessions were conducted with research assistants to discuss the data collection process, including the tone and demeanor of pharmacists answering the questions. The data collection tool provided research assistants with an open ended “notes” field to record their impressions of the call, also known as memoing.
Using Nvivo, Thematic analysis was conducted by a single researcher in an immersive, iterative process to reflect on and extract insights from the call data (Chapman et al., 2015). A grounded theory approach allowed for an inductive strategy for coding to generate insights from the data. First, the coding researcher familiarized themselves with the data and searched for inconsistencies or potential errors. After data cleaning, salient elements served as initial codes, such as perceived attitudes of the pharmacists and accuracy of the information given. These codes were then categorized into larger themes. The lead qualitative researchers then discussed and finalized the themes. Through the thematic lens, data were reviewed to ensure credibility and verify that the themes were supported by the data (Chiarello, 2013).
3. Results
A total of 364 rural pharmacies responded to the calls. Rural pharmacists presented discrete attributes of naloxone gatekeepers (Fig. 1). These attributes were not dependent on whether the pharmacy had naloxone stocked. “Active facilitators” supported patients in the search for naloxone. When pharmacists had a positive approach, informed knowledge levels, and supportive suggestions, they became positive catalysts for patients to obtain naloxone, even if their pharmacy did not stock the drug. “Passive hindrances” discouraged callers, but were not perceived to be malicious. Negative attitudes and insufficient knowledge were not helpful and potentially blocked access to naloxone.
Fig. 1.
Naloxone gatekeepers.
Five themes emerged within these two classes of attributes:
Positive Approach These pharmacists communicated the correct basic information about naloxone, had a “helpful”, “nice”, and “friendly” demeanor, and instilled a sense of willingness to help. Another positive approach included offering to show the patient how to use naloxone. Some pharmacists even mentioned having samples to demonstrate how to use the nasal spray. While there were varying levels of confidence in how to use naloxone, several pharmacists took a collaborative approach, telling callers that they would “explain how to use it” or “walk through it together.”
Helpful suggestions. Some helpful suggestions were ways to alleviate high prices. Pharmacists were able to suggest the use of cheaper options, coupons, and applying insurance to decrease naloxone’s price. Other pharmacists offered to order naloxone to their location and have it ready in a few days. Several pharmacists even offered other means of obtaining naloxone, such as asking a doctor for a sample, or going to a clinic. Suggestions of going to larger, chain pharmacies were common when the pharmacy did not have naloxone in stock or if the price was prohibitive (“Walmart may be a cheaper option”).
Knowledgeable and Informed. “Knowledgeable and informed” pharmacists were able to give correct information about naloxone and prescription requirements. Some of the pharmacists were perceived to be well-educated and “knew the information right away”, while others had to consult with other pharmacists or staff but eventually gave correct information. Other pharmacists took the time to check to ensure naloxone was in stock. Furthermore, several pharmacists offered to call back with more detailed information.
Negative Attitudes. Some pharmacists were viewed as “not very helpful”. These individuals often did not supply additional information, would answer questions with “I don’t know” or “no idea”, were “short” or “rushed”, and were “passive”. Furthermore, these pharmacists “did not seem interested or willing to help at all”, while others seemed “reluctant” and “hesitant”. Some pharmacists even took a more accusatory stance, asking for “who it was for” or “is it an emergency situation?”
Insufficient Knowledge. These pharmacists provided incorrect information about naloxone, such as incorrect formulations (“there is a tablet”), or stating wrong information about the need for a prescription. Also, not all pharmacists were knowledgeable about naloxone in general, were “unsure” without further investigating for the patient, or just “not clear” in the answers they were giving. A few pharmacists even gave contradicting information during the call. For instance, they would start by saying they had naloxone in stock, and then saying later in the call they do not have it. Another pharmacist gave the following contradicting information to a caller: “No [you don’t need a prescription], not in an emergency situation…Only if you are having an overdose in the pharmacy.”
These themes are not mutually exclusive. A pharmacist could have been very positive, but still given the wrong information. Conversely, some pharmacists had negative attitudes (answered in a terse manner) but were able to offer helpful suggestions (pricing, availability without a prescription, etc.).
4. Discussion
Even if pharmacists do not stock naloxone in their pharmacies, these healthcare providers should be able to share information regarding how to obtain naloxone, price of naloxone, how to use naloxone, etc. All patient encounters should be compassionate and consist of empathetic communication. However, if a pharmacist has a negative perception regarding individuals seeking naloxone, there will be negative impacts. Previous work has shown that perceived discrimination is linked to delay of care, resulting in more negative health consequences (Knox et al., 2014, Trivedi and Ayanian, 2006, Van Houtven et al., 2005, Ullrich et al., 2017). This shunning process will lead to further stigmatization, which contributes to poor outcomes, including preventable opioid overdose deaths. This is particularly acute in rural areas, where there may only be one community pharmacy available.
Limitations of this study include the lack of generalizability. While all rural community pharmacies in Georgia were included, other states may have different outcomes. Future work could also include a comparison with urban pharmacies. Additionally, these calls only give a snapshot of the information and the pharmacist who spoke to the researchers. Other pharmacists may have given different answers or displayed different attributes. Also, because of the secret shopper design, researchers did not correct pharmacists or ask why they were unfamiliar with the drug. Future work could continue to explore the attitudes and beliefs of rural community pharmacists regarding naloxone and patients who use opioids.
5. Conclusion
While there have been efforts to increase naloxone access in communities, especially via first responders and the police force, expanding access to rural community pharmacies is extremely important – in rural areas, community pharmacies may serve as the sole formal access point for health care (Georgia Department of Community Health. Georgia Rural County Map, 2008). In order to address the high rural mortality rates from opioid overdoses, naloxone access and availability are integral. There is a clear need to understand how, as gatekeepers, pharmacists can act not only as barriers to but also facilitators of secondary prevention efforts to address this crisis, and to develop educational interventions to increase the ability of rural pharmacists to adequately and affirmingly support access to naloxone.
CRediT authorship contribution statement
Lauren Gilbert: Conceptualization, Methodology, Formal analysis, Writing - original draft. Jacob Warren: Writing - review & editing. Kirby Smalley: Writing - review & editing. Jennifer Elliott: Conceptualization, Investigation, Writing - review & editing. Jennifer Nguyen: Conceptualization, Methodology, Formal analysis, Writing - original draft, Supervision, Project administration.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
We would like to thank Lauren Beasley, John J. Brooks, Jr., Ekene Oranu, and Olubukunola G. Onajin (PharmD candidates from Mercer University College of Pharmacy) for their assistance with data collection. We would also like to thank Kathryn Momary, PharmD for her guidance.
References
- CDC/NCHS, National Vital Statistics System, Mortality. CDC WONDER, Atlanta, GA: US Department of Health and Human Services, CDC; 2018. https://wonder.cdc.gov.
- National Association of Counties and the Appalachian Regional Commission. Opioids in Appalachia: The Role of Counties in Reversing a Regional Epidemic, 2019. https://www.naco.org/sites/default/files/documents/Opioids-Full.pdf.
- Georgia Department of Public Health. Online Analytical Statistical Information System (OASIS) [Internet]. 2019 [cited 8 August 2019]. Available from: https://oasis.state.ga.us/.
- G.P. Guy Jr. T.M. Haegerich M.E. Evans J.L. Losby R. Young C.M. Jones Vital Signs: Pharmacy-Based Naloxone Dispensing — United States, 2012–2018 MMWR Morb Mortal Wkly Rep 68 2019 679 686 http://dx.doi.org/10.15585/mmwr.mm6831e1external icon. [DOI] [PMC free article] [PubMed]
- Davis C., Carr D. State legal innovations to encourage naloxone dispensing. J. Am. Pharm. Assoc. 2017;57(2):S180–S184. doi: 10.1016/j.japh.2016.11.007. [DOI] [PubMed] [Google Scholar]
- Correal A. Overdose Antidote Is Supposed to Be Easy to Get. It’s Not. The New York Times. https://www.nytimes.com/2018/04/12/nyregion/overdose-antidote-naloxone-investigation-hard-to-buy.html. Published April 12, 2018. Accessed December 12, 2019.
- Meyerson B.E., Agley J.D., Davis A., Jayawardene W., Hoss A., Shannon D.J., Ryder P.T., Ritchie K., Gassman R. Predicting pharmacy naloxone stocking and dispensing following a statewide standing order, Indiana 2016. Drug Alcohol. Dependence. 2018;188:187–192. doi: 10.1016/j.drugalcdep.2018.03.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiarello E. How organizational context affects bioethical decision-making: Pharmacists' management of gatekeeping processes in retail and hospital settings. Soc. Sci. Med. 2013;98:319–329. doi: 10.1016/j.socscimed.2012.11.041. [DOI] [PubMed] [Google Scholar]
- Shimane T. Pharmacist as gatekeeper: combating medication abuse and dependence. Yakugaku zasshi: J. Pharm. Soc. Jpn. 2013;133(6):617–630. doi: 10.1248/yakushi.13-00056-2. [DOI] [PubMed] [Google Scholar]
- Nguyễn, J., Gilbert, R., *Beasley, L., *Brooks, J., Elliott, J., Smalley, K., & Warren. Availability of Naloxone at Rural Georgia Pharmacies. JAMA Network Open, 2020; 3(2), e1921227. doi:10.1001/jamanetworkopen.2019.21227. [DOI] [PubMed]
- Standing order for prescription of naloxone for overdose prevention. Vol HB249. 2017. https://gbp.georgia.gov/document/standing-order-naloxone-june-29-2018/download.
- Georgia Department of Community Health. Georgia Rural County Map. Published 2008. https://dch.georgia.gov/documents/georgia-rural-county-map. Accessed December 1, 2019.
- Bullock Holly, Steele Sarah, Kurata Nicole, Tschann Mary, Elia Jennifer, Kaneshiro Bliss, Salcedo Jennifer. Pharmacy access to ulipristal acetate in Hawaii: is a prescription enough? Contraception. 2016;93(5):452–454. doi: 10.1016/j.contraception.2015.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- French Amy C., Kaunitz Andrew M. Pharmacy access to emergency hormonal contraception in Jacksonville, FL: a secret shopper survey. Contraception. 2007;75(2):126–130. doi: 10.1016/j.contraception.2006.09.004. [DOI] [PubMed] [Google Scholar]
- Chapman AL, Hadfield M, Chapman CJ. Qualitative research in healthcare: an introduction to grounded theory using thematic analysis. J R Coll Physicians Edinb. 2015;45(3):201–205. doi: 10.4997/JRCPE.2015.305. [DOI] [PubMed] [Google Scholar]
- Knox Kathy, Fejzic Jasmina, Mey Amary, Fowler Jane L, Kelly Fiona, McConnell Denise, Hattingh Laetitia, Wheeler Amanda J. Mental health consumer and caregiver perceptions of stigma in Australian community pharmacies. Int. J. Soc. Psychiatry. 2014;60(6):533–543. doi: 10.1177/0020764013503149. [DOI] [PubMed] [Google Scholar]
- Trivedi Amal N., Ayanian John Z. Perceived discrimination and use of preventive health services. J. Gen. Intern. Med. 2006;21(6):553–558. doi: 10.1111/j.1525-1497.2006.00413.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Houtven Courtney Harold, Voils Corrine I., Oddone Eugene Z., Weinfurt Kevin P., Friedman Joëlle Y., Schulman Kevin A., Bosworth Hayden B. Perceived discrimination and reported delay of pharmacy prescriptions and medical tests. J. Gen Int. Med. 2005;20(7):578–583. doi: 10.1111/j.1525-1497.2005.0123.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ullrich F, Salako A, Mueller K. Issues Confronting Rural Pharmacies after a Decade of Medicare Part D. Rural Policy Brief. 2017;(2017 3):1-5. [PubMed]