Abstract
Background:
Cough is frequent symptom in sarcoidosis and its impact on patient’s quality of life (QoL) has not been adequately addressed so far.
Objectives:
The goal of this study was to determine the significant predictors of cough-specific and generic QoL in sarcoidosis patients.
Methods:
In the prospective study 275 sarcoidosis patients administered Patient Reported Outcomes instruments for measurement of dyspnea (Borg and MRC scales) and fatigue (Fatigue Assessment Scale (FAS) and Daily Activity List (DAL)), as well as patients’ QoL (cough-specific Leicester Cough Questionnaire (LCQ) and generic tool – 15D). The LCQ contains 3 domains covering physical, psychological and social aspects of chronic cough. Pulmonary function tests (spirometry and diffusing capacity for carbon monoxide) and serum angiotensin converting enzyme (sACE) were also measured.
Results:
Dyspnea measured by Borg scale and impairment of daily activities determined by DAL instrument as well as sACE were the strongest predictors of all cough-specific QoL domains. Mental aspect of patients’ fatigue was significantly correlated with all domains except with psychological LCQ domain. Regarding the generic QoL, the following significant predictors were: dyspnea measured by MRC scale, overall fatigue determined by FAS and physical domain of the LCQ.
Conclusion:
It is important to measure both cough-specific and generic QoL in sarcoidosis patients since they measure different health aspects and their predictors can be different. We demonstrated that physical domain of cough-specific QoL is significant predictor of generic QoL. (Sarcoidosis Vasc Diffuse Lung Dis 2020; 37 (2): 158-168)
Keywords: Sarcoidosis, Quality of life, Cough, Dyspnea, Fatigue, sACE
Introduction
Sarcoidosis is a chronic multisystem granulomatous disease of unknown origin that most commonly affects the lungs but may also involve any other organ [1].
Patients with pulmonary sarcoidosis may have symptoms related directly to the chest such as dyspnea, chest pain and discomfort, cough, and wheeze. Patients may also develop symptoms related to extrapulmonary organ involvement. In addition, sarcoidosis may cause constitutional symptoms such as fatigue, fever, anorexia, weight loss, generalized weakness, and pain that are not related to involvement of any specific organ [2, 3]. Both organ-related and nonspecific sarcoidosis symptoms may significantly adversely influence patients’ qulity of life (QoL).
Nowadays many tools for measurement of Patient-Reported Outcomes (PROs) as study endpoints have been developed in sarcoidosis [4]. PROs measure different aspects of a patient’s health status that comes directly from the patient, without interpretation of the patient’s responses by a physician or anyone else [5]. PROs encompass symptoms and signs of disease, treatment satisfaction and QoL of patients. This is increasingly observed as the regulatory authorities’ requirement due to several limitations of the objective disease outcomes, like pulmonary function tests or radiographic findings.
Numerous studies showed that correlations between PROs as subjective outcomes and objective outcomes are rather mild or moderate or even do not exist at all [6]. QoL and ‘functionality’ are two most highly-rated outcomes for treatment and care by sarcoidosis patients [7,8]. The outcomes that are most important to patients should be considered to make sure that the recommendations in the international guidelines take into account aspects of treatment which matter to patients. They should participate in treatment decision making. For example, physician might prescribe steroids to improve patient’s cough. The patient may choose not to take the steroids because the side effects (possible nausea, sleep problems, mood swings etc.) are worse for them than the cough. In that situation, the patients might rate what is more important for them.
Recently, more attention has been paid to the cough in patients with sarcoidosis. The mechanism of cough is unknown but airway inflammation, mechanical distortion from pulmonary fibrosis and disruption of the vagus nerve from mediastinal lymphadenopathy are possible [9]. However, the influence of cough on sarcoidosis patients’ QoL has not been adequately addressed so far. There is a validated tool – Leicester Cough Questionnaire (LCQ) for measuring this important symptom [10]. The literature on LCQ use in sarcoidosis is limited – currently only a few studies used LCQ for assessing cough in sarcoidosis patients [11-13].
The aim of this study was to assess the significant predictors of both cough-specific and generic Qol in patients with pulmonary sarcoidosis.
Methods
In this prospective observational study in the period from April to December 2018 we enrolled 275 biopsy positive patients with pulmonary sarcoidosis diagnosed at the Clinic for Pulmonary Diseases of the Clinical Centre of Serbia in Belgrade, Serbia. All subjects were ≥ 18 years old and they did not have any associated ilnesses that could influence their health status (those with significant comorbidity, like cardiac or respiratory disorders other than sarcoidosis, were excluded). These patients were examined during regular clinical visits and the patients voluntarily completed the self-administered PROs, provided lab samples for sACE and performed pulmonary function testing. This study was approved by the institution’s ethics committee and all patients consented to participation.
Following PROs were administered: 1) dyspnea instruments: Modified Medical Research Council (MRC) Dyspnea Scale [14] and Borg dyspnea category-ratio-10 scale (CR-10) [15], 2) fatigue questionnaires: Fatigue Assessment Scale (FAS) [16] and Daily Activity List (DAL) [17], and 3) QoL scales: Leicester Cough Questionnaire (LCQ) [10] and generic quality of life questionnaire 15D [18].
Modified Medical Research Council (MRC) Dyspnea Scale classifies subjects into one of five categories according to their degree of dyspnea when performing certain activities [14]. Scores range from the 0 to 4, with the higher scores indicating more severe dyspnea. We previously used it in patients with sarcoidosis [19,20].
Borg dyspnea category-ratio-10 scale (CR-10) [15] is an 11-point scale on which dyspnea is graded from 0 (nothing at all) to 10 (maximum). It is widely used in clinical practice and trials in different respiratory and cardiovascular diseases.
The Fatigue Assessment Scale (FAS) is a 10-item self-report fatigue questionnaire. Its five items represent physical and other five items indicate mental fatigue domains. The response scale is a 5-point Likert scale (1 never to 5 always). Total scores on the FAS can range from 10 to 50, with high scores indicating more fatigue. FAS total score < 22 indicates no fatigue. The psychometric properties (reliability and validity) of the FAS are good, and it was also shown in sarcoidosis patients [21,22,23]. The Serbian version proved to be valid in rheumatoid arthritis [24] and sarcoidosis [25].
The degree of limitation in daily life activities was evaluated with the Daily Activity List (DAL), a scale that was originally designed by Stewart and coworkers [17]. It has 11 items that are related to the usual activities that persons with good health can perform without particular effort. The number of positive responses comprises the DAL score and indicates the degree of impairment. The scale has been used in several studies in patients with chronic pulmonary diseases [19,26,27,28].
LCQ is a 19-item validated specific QoL measure of cough over the period of previous two weeks [10]. Its scores can be calculated in 3 domains covering physical (8 items), psychological (7 items), and social (4 items) aspect of chronic cough, in addition to the total score. It evaluates the impact of cough on patients’ QoL. It takes 5 to 10 minutes to complete. Scores are calculated by domain (range from 1 to 7) and then added to obtain the total score (range from 3 to 21), with higher scores indicating a better QoL. Our study group recently validated the Serbian version of the LCQ in sarcoidosis patients [29].
We measured QoL by standardized generic questionnaire – The fifteen-dimensional measure scale of health-related quality of life (15D) [18]. 15D is a multiatributive instrument for measurement of QoL that consists of 15 different and mutually exclusive health dimensions, each represented by one item. The total questionnaire score ranges between 0 and 1, where 1 signifies the highest level of QoL. 15D was used in different diseases in many different countries. The Serbian version of 15D was previously used in patients with sarcoidosis where it demonstrated good psychometric measurement properties [19,30].
On the same day subjects completed the questionnaires and performed pulmonary function tests – spirometry and the transfer factor of the lung for carbon monoxide (DLCO). Spirometry parameters included pre-bronchodilator forced expiratory vital capacity (FVC) and forced expiratory volume in one second (FEV1), and it was measured with a pneumotachograph (Masterlab, Jaeger, Wurzburg, Germany). DLCO was measured using the single-breath method (Masterlab, Jaeger, Wurzburg, Germany). The European Respiratory Society criteria for lung function impairments was used [31].
Statistical methodology
Continuous variables are described by arithmetic mean and standard deviation, while nominal variables are presented by frequencies and percentages per respective outcomes. Chi-square test or the Exact probability test were used as univariate methods for testing the significance of difference between groups. The assessment of the relationship of sACE and other subjective characteristics of the health condition with cough-specific as well as generic QoL has been done by multivariate multiple linear regression (stepwise method). Stepping method criteria were based on the probability of F statistic, where variables with a probability less than 0.05 were retained, while variables with a probability greater than 0.10 were excluded from the model. The linearity assumption was checked by constructing a scatter plot for each independent variable. The diagnosis of collinearity between the predictors in the linear regression model was done by the arbitrary assessment of the conditional index and the variance inflation factor (VIF). The absence of the collinearity was defined by a conditional index less than 30 and VIF value less than 3 [32]. The Durbin-Watson statistic was used to arbitrarily evaluate the independence of the residuals. Homoscedasticity was graphically estimated based on the layout of the plot of standardized residuals vs. standardized predicted values. In the case of heteroscedasticity, a natural logarithm transformation of predictor variables was performed in order to homogenize the variance of the residuals. In order to normalize the distribution of residuals, all dependent variables were expressed by their squares. The normality of the distribution of residuals was verified by the Kolmogorov-Smirnov test. Outliers were detected and removed in each case where Cook’s distance statistic was greater than 1.
The accepted level of significance was 0.05. The statistical analysis was conducted using IBM SPSS Statistics 20.
Results
Our study population consists of 275 patients with pulmonary sarcoidosis. The majority of them were females (65.5%). Tables 1 and 2 contain descriptive statistics for the total study population.
Table 1.
Descriptive statistics for continuous variables for the total study population (N = 275)
| Mean ± SD | Range | |
| Age, years | 50.13 ± 11.07 | 28 – 76 |
| Height (cm) | 168.85 ± 10.08 | 148 – 199 |
| Weight (kg) | 82.07 ± 16.46 | 42 – 145 |
| Body-mass index (BMI, kg/m2) | 28.79 ± 5.33 | 16.00 – 55.25 |
| Disease duration, years | 15.62 ± 8.56 | 1 – 40 |
| sACE (8 – 52 U/L) | 47.35 ± 28.06 | 5.0 – 151.0 |
| Dyspnea scores | ||
| MRC | 0.89 ± 0.69 | 0 – 3 |
| Borg | 1.45 ± 1.54 | 0 – 9 |
| FAS Scores | ||
| Total score | 24.55 ± 6.23 | 15.00 – 42.00 |
| Physical score | 14.75 ± 3.08 | 8.00 – 22.00 |
| Mental score | 9.80 ± 4.06 | 5.00 – 23.00 |
| DAL | 3.00 ± 2.50 | 0 – 10 |
| LCQ Scores | ||
| Total score | 16.94 ± 3.68 | 5.48 – 21.00 |
| Physical domain score | 5.48 ± 1.18 | 1.88 – 7.00 |
| Psychological domain score | 5.64 ± 1.29 | 1.86 – 7.00 |
| Social domain score | 5.82 ± 1.33 | 1.75 – 7.00 |
| 15D | 0.85 ± 0.11 | 0.49 – 1.00 |
| FEV1 (% predicted) | 99.60 ± 20.02 | 34 – 150 |
| FVC (% predicted) | 108.52 ± 17.40 | 41 – 156 |
| FEV1/FVC | 76.57 ± 8.51 | 31.63 – 91.36 |
| DLCO (% predicted) | 81.55 ± 17.46 | 37 – 111 |
N = Numnber of patients; SD = standard deviation; sACE = Serum Angiotensin Converting Enzyme; MRC = Modified Medical Research Council Dyspnea Scale; Borg = Borg dyspnea category-ratio-10 scale; FAS = Fatigue Assessment Scale; DAL = List of Daily Activities; LCQ = Leicester Cough Questionnaire; 15D = Fifteen-dimensional measure of health-related quality of life; FEV1 = Forced expiratory volume in one second; FVC = Forced expiratory vital capacity; PEF = Peak Expiratory Flow; DLCO = transfer factor of the lung for carbon monoxide
Table 2.
Descriptive statistics for nominal variables for the total study population (N = 275)
| Variable | F | % |
| Gender | ||
| Men | 95 | 34.5 |
| Women | 180 | 65.5 |
| Age > 55 years | ||
| Yes | 173 | 62.9 |
| No | 102 | 37.1 |
| Ro stage of lung disease | ||
| 0 | 68 | 24.7 |
| 1 | 148 | 53.8 |
| 2 | 47 | 17.1 |
| 3 | 12 | 4.3 |
| Course of the sarcoidosis | ||
| Acute | 102 | 27.1 |
| Chronic | 173 | 62.9 |
| Extrapulmonary sarcoidosis | ||
| Yes | 191 | 69.5 |
| No | 84 | 30.5 |
| Treatment | ||
| No treatment | 17 | 6.2 |
| Prednisone | 98 | 35.6 |
| Methotrexate | 146 | 53.1 |
| Chloroquine | 5 | 1.8 |
| Prednisone + Methotrexate | 9 | 3.3 |
| Smoking status | ||
| Active smoker | 25 | 9.1 |
| Non-smoker | 204 | 74.2 |
| Ex-smoker | 46 | 16.8 |
| Total FAS score ≥ 22 | ||
| Yes | 172 | 62.5 |
| No | 103 | 37.5 |
F = frequency; FAS = Fatigue Assessment Scale.
The total time required to complete all PRO questionnaires ranged from 30 to 40 minutes.
Multivariate multiple linear regression models for predictors of square transformed LCQ – Total and Domains Scores are presented in Table 3. There are four indipendent predictors of total cough-specific QoL. Natural logarithm of Borg and natural logarithm of DAL scores as well as natural logarithm of sACE values showed the strongest correlations with all square transformed LCQ scores. It was also the case with natural logarithm of Mental score of FAS that was not correlated only with LCQ Psychological domain score squared. All multivariate regression models obtained were linear and showed a good adequacy with respect to Durbin-Watson statistics (all individually were close to value of 2) – Table 3. Obtained plots of standardised residuals vs. standardised predicted values showed no obvious signs of funnelling, suggesting the assumption of homoscedasticity has been met (Figure 1). In the mentioned models, the Kolmogorov-Smirnov test showed that the values of the residuals were normally distributed (p > 0.05).
Table 3.
Parametres of multivariate multiple linear regressions for predictors of LCQ – Total and Domains Scores
| Model 1 – Dependent variable: LCQ - Total Score Square | |||||||
| The total R2 = 0.397 Durbin-Watson = 1.847 |
Unstandardized Coefficients | Standardized Coefficients | t | p | Change Statistics | ||
| B | SE | Beta | R2 Change | p (F Change) | |||
| Constant | 302.689 | 7.661 | 39.508 | 0.000 | 0.296 | 0.000 (78.865) |
|
| Ln (Borg Scale score) | -78.386 | 8.941 | -0.544 | -8.767 | 0.000 | ||
| Constant | 353.819 | 15.158 | 23.342 | 0.000 | 0.053 | 0.000 (14.920) |
|
| Ln (Borg Scale score) | -58.229 | 10.076 | -0.404 | -5.779 | 0.000 | ||
| Ln (DAL score) | -47.874 | 12.394 | -0.270 | -3.863 | 0.000 | ||
| Constant | 452.927 | 36.950 | 12.258 | 0.000 | 0.029 | 0.004 (8.581) |
|
| Ln (Borg Scale score) | -57.296 | 9.877 | -0.398 | -5.801 | 0.000 | ||
| Ln (DAL score) | -49.692 | 12.159 | -0.280 | -4.087 | 0.000 | ||
| Ln (sACE) | -26.798 | 9.148 | -0.172 | -2.929 | 0.004 | ||
| Constant | 540.867 | 52.321 | 10.337 | 0.000 | 0.018 | 0.020 (5.503) |
|
| Ln (Borg Scale score) | -53.790 | 9.871 | -0.373 | -5.450 | 0.000 | ||
| Ln (DAL score) | -37.612 | 13.068 | -0.212 | -2.878 | 0.004 | ||
| Ln (sACE) | -25.750 | 9.048 | -0.165 | -2.846 | 0.005 | ||
| Ln (FAS mental score) | -47.073 | 20.067 | -0.159 | -2.346 | 0.020 | ||
| Model 2 – Dependent variable: LCQ - Physical Domain Score Square | |||||||
| The total R2 = 0.394 Durbin-Watson = 1.793 |
Unstandardized Coefficients | Standardized Coefficients | t | p | Change Statistics | ||
| B | SE | Beta | R2 Change | p (F Change) | |||
| Constant | 31.252 | 0.782 | 39.971 | 0.000 | 0.289 | 0.000 (74.972) |
|
| Ln (Borg Scale score) | -7.887 | 0.911 | -0.538 | -8.659 | 0.000 | ||
| Constant | 37.088 | 1.528 | 24.270 | 0.000 | 0.067 | 0.000 (19.146) |
|
| Ln (Borg Scale score) | -5.599 | 1.014 | -0.382 | -5.521 | 0.000 | ||
| Ln (DAL score) | -5.470 | 1.250 | -0.303 | -4.376 | 0.000 | ||
| Constant | 45.370 | 3.762 | 12.061 | 0.000 | 0.020 | 0.017 (5.777) |
|
| Ln (Borg Scale score) | -5.512 | 1.002 | -0.376 | -5.502 | 0.000 | ||
| Ln (DAL score) | -5.630 | 1.236 | -0.312 | -4.555 | 0.000 | ||
| Ln (sACE) | -2.237 | 0.931 | -0.141 | -2.404 | 0.017 | ||
| Constant | 54.106 | 5.331 | 10.149 | 0.000 | 0.018 | 0.023 (5.230) |
|
| Ln (Borg Scale score) | -5.164 | 1.002 | -0.352 | -5.154 | 0.000 | ||
| Ln (DAL score) | -4.429 | 1.330 | -0.245 | -3.330 | 0.001 | ||
| Ln (sACE) | -2.133 | 0.921 | -0.134 | -2.316 | 0.022 | ||
| Ln (FAS mental score) | -4.676 | 2.045 | -0.155 | -2.287 | 0.023 | ||
| Model 3 – Dependent variable: LCQ - Psychological Domain Score Square | |||||||
| The total R2 = 0.329 Durbin-Watson = 1.886 |
Unstandardized Coefficients | Standardized Coefficients | t | p | Change Statistics | ||
| B | SE | Beta | R2 Change | p (F Change) | |||
| Constant | 33.967 | 0.932 | 36.449 | 0.000 | 0.259 | 0.000 (64.371) |
|
| Ln(Borg Scale score) | -8.710 | 1.086 | -0.509 | -8.023 | 0.000 | ||
| Model 3 – Dependent variable: LCQ - Psychological Domain Score Square | |||||||
| Constant | 39.043 | 1.865 | 20.930 | 0.000 | 0.037 | 0.002 (9.723) |
|
| Ln (Borg Scale score) | -6.720 | 1.238 | -0.393 | -5.428 | 0.000 | ||
| Ln (DAL score) | -4.758 | 1.526 | -0.226 | -3.118 | 0.002 | ||
| Constant | 51.463 | 4.555 | 11.299 | 0.000 | 0.033 | 0.003 (8.861) |
|
| Ln (Borg Scale score) | -6.590 | 1.213 | -0.385 | -5.432 | 0.000 | ||
| Ln (DAL score) | -4.998 | 1.496 | -0.237 | -3.340 | 0.001 | ||
| Ln (sACE) | -3.354 | 1.127 | -0.181 | -2.977 | 0.003 | ||
| Model 4 – Dependent variable: LCQ - Social Domain Score Square | |||||||
| The total R2 = 0.348 Durbin-Watson = 1.854 |
Unstandardized Coefficients | Standardized Coefficients | t | p | Change Statistics | ||
| B | SE | Beta | R2 Change | p (F Change) | |||
| Constant | 36.256 | 0.998 | -0.494 | 36.324 | 0.000 | 0.244 | 0.000 (59.399) |
| Ln (Borg Scale score) | -8.961 | 1.163 | -7.707 | 0.000 | |||
| Constant | 42.951 | 1.970 | -0.349 | 21.799 | 0.000 | 0.058 | 0.000 (15.159) |
| Ln (Borg Scale score) | -6.337 | 1.308 | -0.281 | -4.846 | 0.000 | ||
| Ln (DAL score) | -6.276 | 1.612 | -3.894 | 0.000 | |||
| Constant | 56.388 | 5.533 | -0.321 | 10.191 | 0.000 | 0.025 | 0.010 (6.724) |
| Ln (Borg Scale score) | -5.819 | 1.303 | -0.202 | -4.466 | 0.000 | ||
| Ln (DAL score) | -4.517 | 1.726 | -0.185 | -2.617 | 0.010 | ||
| Ln (FAS mental score) | -6.890 | 2.657 | -2.593 | 0.010 | |||
| Constant | 66.305 | 6.846 | -0.316 | 9.685 | 0.000 | 0.021 | 0.017 (5.771) |
| Ln (Borg Scale score) | -5.732 | 1.287 | -0.215 | -4.454 | 0.000 | ||
| Ln (DAL score) | -4.799 | 1.708 | -0.177 | -2.810 | 0.005 | ||
| Ln (FAS mental score) | -6.579 | 2.626 | -0.145 | -2.505 | 0.013 | ||
| Ln (sACE) | -2.842 | 1.183 | -2.402 | 0.017 | |||
Ln = Natural logarithm; sACE = Serum Angiotensin Converting Enzyme; Borg = Borg dyspnea category-ratio-10 scale; FAS = Fatigue Assessment Scale; DAL = List of Daily Activities; LCQ = Leicester Cough Questionnaire; SE = Standard Error
Fig. 1.
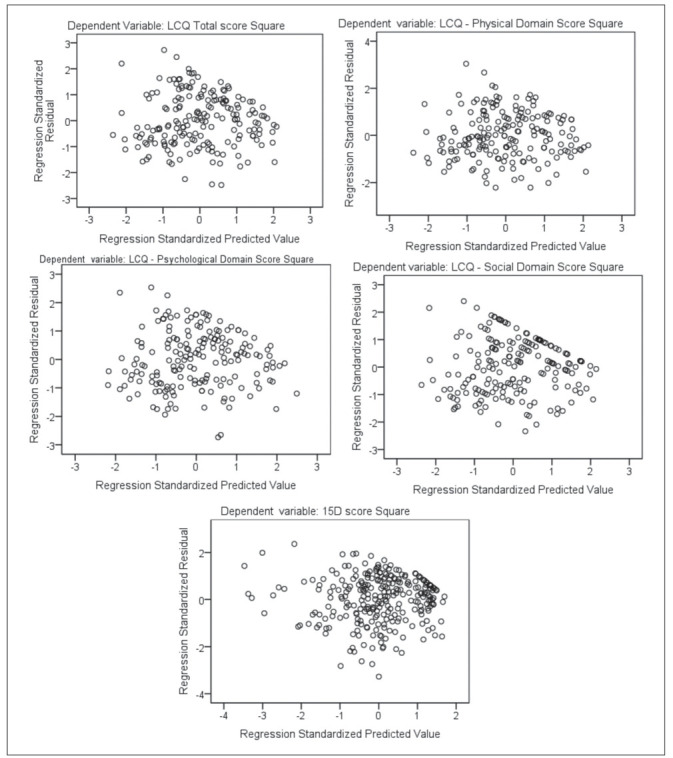
Scatterplots of standardised residuals vs. standardised predicted values for LCQ – Total and Domains Scores and 15D Score
LCQ = Leicester Cough Questionnaire; 15D = Fifteen-dimensional measure of health-related quality of life
Parameters of multivariate multiple linear regression for predictors of generic QoL are given in Table 4. 15D score square significantly correlated with four independent predictors. It negatively correlated with the MRC and natural logarithm of FAS Total scores. On the other side, it positively correlated with natural logarithm of LCQ Physical Domain Score. This linear model also showed good adequacy characteristics (Durbin-Watson statistic = 1.844), the variance of the residuals was constant (Figure 1) and the values of the residuals were normally distributed (Kolmogorov-Smirnov statistic = 0.064; p = 0.058).
Table 4.
Parameters of multivariate multiple linear regression for predictors of 15D Score
| Dependent variable: 15D Score Square | |||||||
|
The total R2 = 0.633 Durbin-Watson = 1.808 |
Unstandardized Coefficients | Standardized Coefficients | t | p | Change Statistics | ||
| B | SE | Beta | R2 Change | p (F Change) | |||
| Constant | 0.907 | 0.013 | 70.682 | 0.000 | 0.512 | 0.000 (280.233) |
|
| MRC score | -0.191 | 0.011 | -0.716 | -16.740 | 0.000 | ||
| Constant | 1.663 | 0.102 | 16.331 | 0.000 | 0.085 | 0.000 (55.820) |
|
| MRC score | -0.146 | 0.012 | -0.546 | -12.127 | 0.000 | ||
| Ln (FAS total score) | -0.251 | 0.034 | -0.337 | -7.471 | 0.000 | ||
| Constant | 1.225 | 0.130 | 9.412 | 0.000 | 0.036 | 0.000 (25.866) |
|
| MRC score | -0.117 | 0.013 | -0.439 | -9.156 | 0.000 | ||
| Ln (FAS total score) | -0.211 | 0.033 | -0.282 | -6.363 | 0.000 | ||
| Ln (LCQ - Physical Domain Score) | 0.171 | 0.034 | 0.237 | 5.086 | 0.000 | ||
Ln = Natural logarithm; FAS = Fatigue Assessment Scale; LCQ = Leicester Cough Questionnaire; 15D = Fifteen-dimensional measure of health-related quality of life; MRC = Modified Medical Research Council Dyspnea Scale; SE = Standard Error
We did not notice significant relationship between pulmonary function parameters (FEV1, FVC, FEV1/FVC, DLCO) and QoL scores.
Discussion
Evaluation of PROs is very important in chronic diseases like sarcoidosis where objective outcomes cannot fully direct physicians in therapeutic decision making and follow up of their patients. It was previously recognized that potential endpoints in sarcoidosis research should include: QoL measures, symptoms of cough, dyspnea, and wheeze, the frequency of disease exacerbations (requiring corticosteroid bursts or additional anti-sarcoidosis therapy), and corticosteroid-sparing effects of interventions [33,34]. In addition, Moor and coauthors recently evaluated the needs and perceptions of patients with sarcoidosis and their partners and demonstrated that 40% of sarcoidosis patients identified fatigue as their most disabling symptom, followed by painful joint/muscles (20%) and dyspnea (15%). Cough and ocular symptoms followed by frequency of 10% [35].
In this study we assessed significant predictors of both cough-specific and generic Qol in patients with pulmonary sarcoidosis.
We noticed that dyspnea was the strongest predictor of cough-specific and generic QoL in our study population. Increased natural logarithm of Borg dyspnea scores had the biggest negative influence on all almost every cough-specific QoL domains scores square and the highest correlation was noticed with the total LCQ score square (B = -57.296, p < 0.001). On the other side, dyspnea measured by MRC score was the strongest predictor of generic QoL score square (B = -0.117, p < 0.001). Hinz and coauthors showed that dyspnea is an important symptom in the prediction of anxiety and depression in sarcoidosis patients [36].
It has been previously demonstrated that impaired exercise tolerance, fatigue and muscle weakness appeared to have a negative influence on the QoL of patients with sarcoidosis [37,38]. In our study we obtained similar results regarding the influence of fatigue, as common symptom of sarcoidosis, on both cough-specific and generic QoL. Mental aspect of patients’ fatigue significantly correlated with all LCQ domains except with psychological QoL domain, while total FAS score was significant predictor of generic QoL. It is very important to stress here that the LCQ is not synonymous with cough but rather it is a cough QoL PRO. So, the fatigue itself may not worsen cough but worsen the effect of cough on the patient’s QoL.
Physical activity offers great health benefits for a wide range of conditions. Hendriks at al recently evaluated the self-reported experiences with physical activity among 233 patients with sarcoidosis [39]. Most patients emphasized that exercise and physical activity was beneficial to them. In our study limitation of daily activities, as assessed by DAL, significantly influenced all domains of cough-specific QoL but it did not predict the generic QoL.
Among the spectrum of subjective QoL predictors, sACE was the only objective disease outcome that significantly influenced all domains of cough-specific QoL. Serum ACE has been the most frequently used laboratory test in sarcoidosis. It is produced by epithelioid cells derived from recently-activated macrophages in granulomas and it is a well-known marker for sarcoidosis activity. The enzyme is also supposed to give indication of total body granuloma burden (not ones found in the lungs only) [40] and disease severity [41], although the clinical value of this marker is still under debate as results of different studies are conflicting [42]. Yasar and coauthors showed that serum ACE was a predictor of extrathoracic involvement of sarcoidosis [43]. We have recently demonstrated that severity of cough in sarcoidosis correlated with the disease activity as measured by the concentration of sACE [44]. In our study natural logarithm of sACE was independent predictor of all cough-specific QoL domains in a negative direction, i.e. its lower values indicated reduced cough perception and a better QoL. The degree of these correlations is generally low and the most prominent impact sACE had on the total LCQ scores (B = -25.750, p = 0.005, Table 3). According to the available information, we are the first who demonstrated the impact of disease activity, as measured by sACE, on the cough-specific and generic QoL in sarcoidosis patients, together with other subjective outcomes like dyspnea, fatigue and limitation of daily activities.
Regarding the generic QoL, measured by 15D, we obtained its different predictors. Dyspnea measured by MRC scale, overall fatigue (as assessed by total FAS score) and physical domain of LCQ were significant predictors of patients’ generic QoL. We showed that dyspnea determines generic QoL (R2 change = 0.512) significantly more than physical domain of LCQ (R2 change = 0.036) and fatigue (R2 change = 0.085) – Table 4. This might indicate that psychological and social domains of LCQ measure QoL aspects which are not covered by the 15D instrument emphasizing the importance not only to use the generic QoL questionnaire, but also the LCQ in sarcoidosis patients. Although the disease activity measured by the sACE was not a significant predictor of generic QoL in our study group, it still can indirectly affect it in sarcoidosis patients by influencing physical domain of cough-specific QoL that was significant predictor of generic QoL. Therefore, we suggest that antitussives should be considered in the treatment of chronic cough in sarcoidosis since it can influence improvement of overall QoL without safety risks of masking the symptomatology caused by increasing of disease activity, since we demonstrated a weak correlation between the cough-specific QoL and disease activity.
We confirmed that the LCQ provides a significant contribution in measurement and understanding of complex relationships between the disease activity, dyspnea, limitation of daily activities, fatigue, cough-specific and overall QoL of sarcoidosis patients. In other published studies [45-48] correlations between LCQ scores and different PROs (mainly generic QoL instruments) were mostly moderate as it was also the case with the original LCQ validation [10]. In the process of validation of the German version of the LCQ (among 200 sarcoidosis patients), Schupp and coauthors demonstrated only a moderate correlation of LCQ scores with generic and respiratory-specific QoL questionnaires (SF-36, Borg, VAS Dyspnea) [12]. The Physical Component Summary Score of the SF-36 showed a quite high correlation with the LCQ, while the Mental Component Summary Score did not.
Altlhough our patients were fatigued, had significant dyspnea, perceived limitations in their physical activities, and had a poor QoL, they had normal pulmonary function. This is in line with results of previous studies demonstrating that pulmonary function testing cannot function as a surrogate for these other parameters and cannot be used to assess the overall health of sarcoidosis patients [49-50]. All pulmonary function parameters in our study have not been significantly correlated with both LCQ and 15D scores. Judson et al found that cough was not statistically significantly different in terms of spirometric measures (FEV1%, FVC% and FEV1/FVC) [11].
A major limitation of this study is that the data were collected in a tertiary health-care setting, i.e. a specialised referral clinic for sarcoidosis patients. This means that our patients had predominantly severe forms of the disease and the scores for all patient reported outcomes were probably more severe than for the average sarcoidosis patient. Therefore, our results may not be generalizable to patients in primary care settings. In addition, 40% of our study patients were receiving oral corticosteroid therapy, and this may have had a postive or negative impact upon their health status and other measured variables like sACE. Namely, corticosteroid medications may reduce sACE levels [51] and indirectly influence cough-specific QoL. Moreover, corticosteroids should improve cough and therefore improve QoL on that basis. However, corticosteroids may worsen QoL on the basis of their numerous side effects. Besides that, we did not measure the frequency of coughing in our study group and sarcoidosis patients were included regardless of the presence of cough. Overrall, the predictors evaluated suit general QOL better and therefore only a limited assessment of cough was possible. Finally, important limitation of our study is that we did not record the use of ACE inhibitors in our study population, which may have reduced sACE levels [52] or cause a dry, debilitating cough [53]. On the other hand, several nominal or ordinal variables that could potentially affect cough [gender, smoking, radiology variables (extent, fibrosis, consolidation, PET active), multiorgan disease, immunosuppressive drugs, reflux, rhinitis], could not be used in our linear regression models. Nominal or ordinal variables (even if they prove significant) impair the linearity of the regression model and make it inadequate, as well as lead to the failure to fulfill other assumptions for accepting it (normality of residual distribution and constant residual variance).
We conclude that increase of disease activity as measured by sACE, together with increased dyspnea and mental fatigue component as well as limited daily activities, significantly influences deterioration of the cough-specific QoL in sarcoidosis patients. In addition, disease activity indirectly impacts overall QoL by decreasing physical domain of cough-specific QoL that is correlated to generic QoL. In order to improve overall QoL, we suggest that chronic cough in sarcoidosis should be treated with antitussives without safety risks of masking the symptomatology caused by increased disease activity. It is important to measure both cough-specific and generic QoL in sarcoidosis patients since they measure different health aspects and their predictors can be different.
Conflict of interest statement:
None of the authors disclosed any potential conflicts of interest
References
- 1.Hunninghake GW, Costabel U, Ando M, et al. ATS/ERS/WASOG statement on sarcoidosis. American Thoracic Society/European Respiratory Society/World Association of Sarcoidosis and other Granulomatous Disorders. Sarcoidosis Vasc Diffuse Lung Dis. 1999;16:149–73. [PubMed] [Google Scholar]
- 2.Michielsen HJ, Peros-Golubicic T, Drent M, et al. Relationship between symptoms and quality of life in a sarcoidosis population. Respiration. 2007;74:401–5. doi: 10.1159/000092670. [DOI] [PubMed] [Google Scholar]
- 3.Vučinić V, Stojković M, Milenković B, et al. Fatigue in Sarcoidosis: Detection and Treatment. Srp Arh Celok Lek. 2012;139:104–9. [PubMed] [Google Scholar]
- 4.Thunold RF, Løkke A, Cohen AL, et al. Patient reported outcome measures (PROMs) in sarcoidosis. Sarcoidosis Vasc Diffuse Lung Dis. 2017;34(1):2–17. doi: 10.36141/svdld.v34i1.5760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Food and Drug Administration (FDA) Rockville, MD: Dec 2009. Draft Guidance for Industry. Patient-reported outcome measures: use in medical product development to support labeling claims. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gvozdenovic BS, Mihailović-Vučinić V, Vuković M, et al. Effect of obesity on patient reported outcomes in sarcoidosis. Int J Tuberc Lung Dis. 2013;17(4):559–64. doi: 10.5588/ijtld.12.0665. [DOI] [PubMed] [Google Scholar]
- 7.Baughman RP, Barriuso R, Beyer K, et al. Sarcoidosis: patient treatment priorities. ERJ Open Res. 2018;4:00141–2018. doi: 10.1183/23120541.00141-2018. [https://doi.org/10.1183/23120541.00141-2018. ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.European Lung Foundation/European Respiratory Society. Online survey: Sarcoidosis treatment and outcomes: what is most important to you? 2018 www.surveymonkey.com/r/Preview/?sm=Xx2rw_2BFgeFmjWLPJHyKFSL_2FGkgBGq0Etg8oJa8_2Fgx_2BhrNQw8VqA5UIgMkFwqvqD_2F . [Google Scholar]
- 9.Tully T, Birring SS. Cough in sarcoidosis. Lung. 2016;194:21–4. doi: 10.1007/s00408-015-9799-2. [DOI] [PubMed] [Google Scholar]
- 10.Birring SS, Prudon B, Carr AJ, Singh SJ, Morgan MDL, Pavord ID. Development of a symptom specific health status measure for patients with chronic cough: Leicester Cough Questionnaire (LCQ) Thorax. 2003;58:339–43. doi: 10.1136/thorax.58.4.339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Judson MA, Chopra A, Conuel E, et al. The Assessment of Cough in a Sarcoidosis Clinic Using a Validated instrument and a Visual Analog Scale. Lung. 2017;195(5):587–94. doi: 10.1007/s00408-017-0040-3. [DOI] [PubMed] [Google Scholar]
- 12.Schupp JC, Fichtner UA, Frye BC, et al. Psychometric properties of the German version of the Leicester Cough Questionnaire in sarcoidosis. PLoS One. 2018;13(10):e0205308. doi: 10.1371/journal.pone.0205308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pirozzi CS, Mendoza DL, Xu Y, Zhang Y, Scholand MB, Baughman RP. Short-Term Particulate Air Pollution Exposure is Associated with Increased Severity of Respiratory and Quality of Life Symptoms in Patients with Fibrotic Sarcoidosis. Int J Environ Res Public Health. 2018;15(6):E1077. doi: 10.3390/ijerph15061077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Medical Research Council. London: MRC; 1986. Questionnaire on Respiratory Symptoms: instructions to interviewers. MRC Committee on Environmental and Occupational Health. [Google Scholar]
- 15.Borg GA. Psychophysical bases of perceived exertion. Med Sci Sports Exerc. 1982;14(5):377–81. [PubMed] [Google Scholar]
- 16.Michielsen HJ, De Vries J, Van Heck GL. Psychometric qualities of a brief self-rated fatigue measure: the Fatigue Assessment Scale (FAS) J Psychosom Res. 2003;54:345–52. doi: 10.1016/s0022-3999(02)00392-6. [DOI] [PubMed] [Google Scholar]
- 17.Stewart AL, Ware JE, Brook RH. Advances in the measurement of functional status: constructioon of aggregate indexes. Med Care. 1981;19:473–88. doi: 10.1097/00005650-198105000-00001. [DOI] [PubMed] [Google Scholar]
- 18.Sintonen H, Pekurinen M. A fefteen-dimensional measure of health-related quality of life (15D) and its applications. Quality of life assessment: key issues in 1990s. In: Walker SR, Rosser R, editors. Dordrecht: Kluwer Academic Publishers; 1993. pp. 185–95. [Google Scholar]
- 19.Gvozdenovic BS, Mihailovic-Vucinic V, Ilic–Dudvarski A, Zugic V, Judson MA. Differences in symptom severity and health status impairment between patients with pulmonary and pulmonary plus extrapulmonary sarcoidosis. Respir Med. 2008;102(11):1636–42. doi: 10.1016/j.rmed.2008.05.001. [DOI] [PubMed] [Google Scholar]
- 20.Gvozdenovic BS, Mihailovic-Vucinic V, Videnovic J, Zugic V, Ilic–Dudvarski A, Filipovic S. Quality of life and health status in sarcoidosis patients. Chapter 6. Health-related quality of life. In: Hoffmann EC, editor. New York: Nova Science Publishers, Inc.; 2009. pp. 119–32. [Google Scholar]
- 21.Michielsen HJ, De Vries J, Van Heck GL, Van de Vijver FJR, Sijtsma K. Examination of the dimensionality of fatigue: the construction of the Fatigue Assessment Scale (FAS) Eur J Psychol Assess. 2004;20(1):39–48. [Google Scholar]
- 22.Michielsen HJ, De Vries J, Drent M, Peros-Golubicic T. Psychometric qualities of the Fatigue Assessment Scale in Croatian sarcoidosis patients. Sarcoidosis Vasc Diffuse Lung Dis. 2005;22(2):133–8. [PubMed] [Google Scholar]
- 23.Drent M, Lower EE, De Vries J. Sarcoidosis-associated fatigue. Eur Respir J. 2012;40(1):255–263. doi: 10.1183/09031936.00002512. [DOI] [PubMed] [Google Scholar]
- 24.Lapčević M, Vuković M, Gvozdenović BS, Mioljević V, Marjanović S. Socioeconomic and therapy factor influence on self-reported fatigue, anxiety and depression in rheumatoid arthritis patients. Rev Bras Reumatol. 2017;57(6):545–556. doi: 10.1016/j.rbre.2017.02.004. [DOI] [PubMed] [Google Scholar]
- 25.Vucinic V, Patel AS, Birring SS, et al. Vol. 90. Paris, France: 2013. King’s Sarcoidosis Questionnaire (KSQ): New instrument for assessing health status in sarcoidosis: the relationship between KSQ and other health status questionnaires. [Abstract SAR 37] Abstracts from the 6th International WASOG Conference on Diffuse Parenchymal Lung Diseases, June 6-7 2013. [Google Scholar]
- 26.Schrier AC, Dekker FW, Kaptein AA, Dijkman JH. Quality of life in elderly patients with chronic nonspecific lung disease seen in family practice. Chest. 1990;98(4):894–9. doi: 10.1378/chest.98.4.894. [DOI] [PubMed] [Google Scholar]
- 27.Gvozdenović BS, Mitić S, Žugić VG, Gvozdenović AT, Lazović NM, Plavšić S. Relationship between the degree of dyspnea and health-related quality of life in patients with chronic obstructive pulmonary disease. Srp Arh Celok Lek. 2007;135(9-10):547–53. doi: 10.2298/sarh0710547g. [DOI] [PubMed] [Google Scholar]
- 28.Stjepanovic M, Gvozdenovic B, Maskovic J, Vukovic M, Vucinic V. Fatigue and limitation of daily activities as predictors of health status in COPD patients. Abstracts from the 26th European Respiratory Society (ERS) Annual Congress, London, UK, September 3–7, 2016. ERJ. 2016;48(Suppl 60):PA1334. [Google Scholar]
- 29.Gvozdenović BS, Mihailović-Vučinić VV, Vuković MH, Stjepanović MI, Mihailović SV, Marić NB. Psychometric characteristics of the Serbian version of the Leicester cough questionnaire in sarcoidosis patients. Hospital Pharmacology. 2019;6(1):728–37. https://www.hophonline.org/wp-content/uploads/2019/05/1111.pdf . [Google Scholar]
- 30.Gvozdenovic BS, Mihailovic-Vucinic V, Vukovic M, et al. Predictors of health status and symptoms impairment in sarcoidosis patients. Chapter 5. Sarcoidosis: Diagnosis, Epidemiology and Treatment Options. In: Connor MR, Stevens RS, editors. New York: Nova Science Publishers, Inc.; 2012. pp. 95–110. [Google Scholar]
- 31.Miller MR, Hankinson J, Brusasco V, et al. Standardisation of spirometry. Eur Respir J. 2005;26:319–38. doi: 10.1183/09031936.05.00034805. [DOI] [PubMed] [Google Scholar]
- 32.Tabachnick BG, Fidell LS. fifth edition. Boston: Pearson education, Inc.; 2007. Using multivariate statistics. [Google Scholar]
- 33.Baughman RP, Drent M, Culver DA, et al. Endpoints for clinical trials of sarcoidosis. Sarcoidosis Vasc Diffuse Lung Dis. 2012;29(2):90–8. [PubMed] [Google Scholar]
- 34.Judson MA. Endpoints in sarcoidosis: More like IPF or asthma? Respir Med. 2018;138S:S3–S4. doi: 10.1016/j.rmed.2017.11.010. [DOI] [PubMed] [Google Scholar]
- 35.Moor CC, van Manen MJG, van Hagen PM, et al. Needs, perceptions and education in sarcoidosis: a live interactive survey of patients and partners. Lung. 2018;196:569–75. doi: 10.1007/s00408-018-0144-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hinz A, Brähler E, Möde R, Wirtz H, Bosse-Henck A. Anxiety and depression in sarcoidosis: the influence of age, gender, affected organs, concomitant diseases and dyspnea. Sarcoidosis Vasc Diffuse Lung Dis. 2012;29(2):139–46. [PubMed] [Google Scholar]
- 37.Drent M, Wirnsberger RM, Breteler MH, Kock LM, De Vries J, Wouters EF. Quality of life and depressive symptoms in patients suffering from sarcoidosis. Sarcoidosis Vasc Diffuse Lung Dis. 1998;15(1):59–66. [PubMed] [Google Scholar]
- 38.De Vries J, Drent M. Quality of life and health status in interstitial lung diseases. Curr Opin Pulm Med. 2006;12(5):354–8. doi: 10.1097/01.mcp.0000239553.93443.d8. [DOI] [PubMed] [Google Scholar]
- 39.Hendriks CMR, Deenstra DD, Elfferich MDP, et al. Experience with Activity Monitors of Patients with COPD, Sarcoidosis and Pulmonary Fibrosis in the Netherlands. Psychol Behav Sci Int J. 2019;12(4):555843. DOI: 10.19080/PBSIJ.2019.12.555843. [Google Scholar]
- 40.Muthuswamy PP, Lopez-Majano V, Panginwala M, Trainor WD. Serum angiotensin-converting enzyme as an indicator of total body granuloma load and prognosis in sarcoidosis. Sarcoidosis. 1987;4:142–8. [PubMed] [Google Scholar]
- 41.Studdy P, Bird R, James DG. Serum angiotensin-converting enzyme (SACE) in sarcoidosis and other granulomatous disorders. Lancet. 1978;2(8104-5):1441–54. doi: 10.1016/s0140-6736(78)91972-4. [DOI] [PubMed] [Google Scholar]
- 42.Keir G, Wells AU. Assessing Pulmonary Disease and Response to Therapy: Which Test? Semin Respir Crit Care Med. 2010;31(4):409–18. doi: 10.1055/s-0030-1262209. [DOI] [PubMed] [Google Scholar]
- 43.Yasar Z, Özgül MA, Cetinkaya E, et al. Angiotensin-converting Enzyme as a Predictor of Extrathoracic Involvement of Sarcoidosis. Sarcoidosis Vasc Diffuse Lung Dis. 2016;32(4):318–24. [PubMed] [Google Scholar]
- 44.Vucinic V, Milenkovic B, Gvozdenovic B. Leicester Cough Questionnaire (LCQ) for Measuring Cough in Sarcoidosis. [Abstract O2-1] Abstracts from the Joint Conference of International Conference on Sarcoidosis and Interstitial Lung Diseases 2019 (WASOG) and The 39th Annual Meeting of Japan Society of Sarcoidosis and other Granulomatous Disorders, October 9-11 2019, Yokohama, Japan, 2019:34 [Google Scholar]
- 45.Dąbrowska M, Krakowiak K, Radlińska O, et al. Validation of the Polish Version of the Chronic Cough Quality of Life Questionnaire (Leicester Cough Questionnaire) Adv Clin Exp Med. 2016;25(4):649–53. doi: 10.17219/acem/59512. [DOI] [PubMed] [Google Scholar]
- 46.Kwon JW, Moon JY, Kim SHSHSH, et al. Reliability and Validity of a Korean Version of the Leicester Cough Questionnaire. Allergy Asthma Immunol Res. 2015;7(3):230–3. doi: 10.4168/aair.2015.7.3.230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gao YH, Guan WJ, Xu G, et al. Validation of the Mandarin Chinese version of the Leicester Cough Questionnaire in bronchiectasis. Int J Tuberc Lung Dis. 2014;18(12):1431–7. doi: 10.5588/ijtld.14.0195. [DOI] [PubMed] [Google Scholar]
- 48.Pornsuriyasak P, Kawamatawong T, Rattanasiri S, et al. Validity and Reliability of Thai Version of the Leicester Cough Questionnaire in Chronic Cough. Asian Pacific J Allergy Immunol. 2016;34(3):212–6. doi: 10.12932/AP0685.34.3.2016. [DOI] [PubMed] [Google Scholar]
- 49.Baydur A, Alsalek M, Louie SG, et al. Respiratory muscle strength, lung function, and dyspnea in patients with sarcoidosis. Chest. 2001;120:102–8. doi: 10.1378/chest.120.1.102. [DOI] [PubMed] [Google Scholar]
- 50.Cox CE, Donohue JF, Brown CD, et al. The Sarcoidosis Health Questionnaire: A new measure of health-related quality of life. Am J Respir Crit Care Med. 2003;168:323–9. doi: 10.1164/rccm.200211-1343OC. [DOI] [PubMed] [Google Scholar]
- 51.Baughman RP, Ploysongsang Y, Roberts RD, et al. Effects of sarcoid and steroids on ACE. Am Rev Respir Dis. 1983;128(4):631–3. doi: 10.1164/arrd.1983.128.4.631. [DOI] [PubMed] [Google Scholar]
- 52.Krasowski MD, Savage J, Ehlers A, et al. Ordering of the Serum Angiotensin-Converting Enzyme Test in Patients Receiving Angiotensin-Converting Enzyme Inhibitor Therapy: An Avoidable but Common Error. Chest. 2015;148(6):1447–53. doi: 10.1378/chest.15-1061. [DOI] [PubMed] [Google Scholar]
- 53.Sato A, Fukuda S. A prospective study of frequency and characteristics of cough during ACE inhibitor treatment. Clin Exp Hypertens. 2015;37(7):563–8. doi: 10.3109/10641963.2015.1026040. [DOI] [PubMed] [Google Scholar]


