Abstract
Background and aim:
Coronavirus disease 2019 (COVID-19) is caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Its outbreak in many states of the world, forced the World Health Organization (WHO) to declare a pandemic. Currently, COVID-19 has infected 1 991 562 patients causing 130 885 deaths globally as of 16 April 2020. The aim of this review is to underline the epidemiological, clinical and management characteristics in children affected by COVID-19.
Methods:
We searched Pubmed, from January to April 2020, for the following search terms: “COVID-19”, “children”, “SARS-COV2”, “complications”, “epidemiology”, “clinical features”, focusing our attention mostly on epidemiology and symptoms of COVID-19 in children.
Results:
Usually, infants and children present milder symptoms of the disease with a better outcome than adults. Consequently, children may be considered an infection reservoir that may play a role as spreader of the infection in community. (www.actabiomedica.it)
Keywords: COVID-19, SARS Cov-2, children, symptoms
Background
In the last few months, some cases of pneumonia of unknown aetiology were identified worldwide. The first cases were detected in Wuhan, China.
Collecting the samples of these patients, scientists have discovered a new coronavirus (COVID-19) that is now known as the cause of the disease named severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) (1). By 16 April 2020, 1 991 562 cases have been confirmed and 130 885 deaths have been reported globally (2). Transmission takes place through respiratory droplets or contact with symptomatic cases. Transmission from asymptomatic cases, especially children, seems to have also an important role (3). Moreover, SARS-CoV-2 RNA has been detected in stool of some patients, so faecal-oral transmission could be possible (4).
The most common symptoms in adults are fever, dry cough, sore-throat, myalgia, fatigue and in severe cases (usually older patients with comorbidities) acute respiratory distress syndrome (ARDS) with lung failure or severe coagulation dysregulation as a result of an uncontrolled inflammation (5). According to the experience of Wuhan, children usually present milder symptoms.
Pathogenesis
The initial viral replication occurs in mucosal epithelium of upper respiratory tract and later in lower respiratory tract and gastrointestinal mucosa. COVID-19, like others coronavirus, uses a specific receptor to infect human cells. This receptor is angiotensin-converting enzyme 2 (ACE2) and it’s a functional receptor that is widely expressed in many organs, especially in lungs, but also in heart, kidney, vascular endothelium and intestine (6).
Severe complications of COVID-19 infections are ARDS with consequently lung failure, immune disfunction and coagulation disorders. The rapid viral replication may cause massive epithelial and endothelial cell death, stimulating the production of pro-inflammatory cytokines and chemokines. This ‘cytokine storm’ with an uncontrolled inflammation is considered a leading cause of fatality (7).
Clinical manifestations
Current data show that children with SARS-COV2 usually belong to cluster family cases. Infected children may appear asymptomatic or present mild symptoms like cough, fever, nasal congestion. In addition, gastrointestinal symptoms such as diarrhea, nausea, vomiting, abdominal discomfort are more frequent in children than in adults.
Despite mild respiratory symptoms with interstitial pneumonia, radiographycally assessed, only few cases have needed intensive care because of respiratory complications (8).
A recent study analysed 44,672 laboratory-confirmed cases across China and reported that only 416 (0.9%) were less than 10 years of age and 549 (1.2%) between 10 and 20 years of age. According to this study, children usually have a good prognosis and they recover within 1-2 weeks after the onset of the disease (9).
Data provided by The Centers for Disease and Control in USA are stackable. Only 5.7% of children have been hospitalized because of the appearance of dyspnoea. According to this report, children aged < 1 year and children with comorbidities have presented the highest percentage of complications. The most common underlying conditions have been cardiovascular disease, chronic lung disease especially asthma and immunosuppression. However, compared with the adult cases, the severity of children’s COVID-19 cases has been milder (10).
At variance, in Spain around 60% of children affected by COVID-19 have been hospitalized for mild symptoms and 9.7% of these patients have requested intensive care because of the comparison of respiratory complications. Only one patient had recurrent wheezing as previous condition. No patients died. The Spanish series agrees with those previously published except for the number of admissions. This probably depends on the fact that the percentage of children tested have been higher than in other countries and it could be associated with different hospitalization criteria (11).
Children usually are asymptomatic or with few accompanying symptoms. Fever and mild cough are common symptoms at onset of the disease. Other symptoms at presentation include sore throat, nasal congestion and rhinorrhea, diarrhea. For mild case, fever is brief and resolved rapidly. Usually children do not need admission in hospital. Only a small percentage of all the patients have been in need of intensive care and usually they have been children with comorbidities or children aged < 1 year (12).
On the basis of these studies and clinical experience, COVID-19 vertical transmission hasn’t been detected but further studies are needed. The infection of 2019-nCoV during pregnancy seems less serious compared to infection of SARS-COV and MERS-COV with no cases of maternal death, or perinatal death (13-15). Usually, neonates have evolved favourably. There are no contraindications to breastfeeding if mothers observe proper hygiene rules (16).
Diagnosis
In adults, it is usually possible to find a decreased lymphocyte count and increased liver enzymes and muscle enzymes. Many patients present elevated C-reactive protein levels and erythrocyte sedimentation rates, and normal procalcitonin levels. With the worsening of the disease, it is possible to find also a high D-dimer level with a dysregulation of the coagulation. Unfortunately, there are limited data on children in literature. According to a study published by Brandon MH et al., only few infants experienced lymphopenia. Usually in children the leukocyte count is normal and CPR and procalcitonin sometimes are elevated. The lack of significant lymphopenia may depend on the relative immaturity of the children’s immune system (17,18) (Table 1).
Table 1.
Laboratory findings in children. Unlike adults, children usually don’t present lymphopenia and the leukocyte count is normal. In a small percentage of children, it is possible to find increased CRP and LDH17,18.
| Laboratory tests | |
| Leukocytes count | Usually normal. Lymphopenia is uncommon in children. |
| CRP | Normal or increased |
| LDH | Normal or increased |
| Liver and cardiac function | Usually normal |
| Coagulation function | Usually normal |
Currently, the better method to detect RNA the virus through RT-PCR is to collect samples from throat swabs (better using nasopharyngeal swab in children), sputum, or lower respiratory tract secretions. Another important technique for COVID-19 diagnosis is using imaging technology (CT scan or chest X-ray). In fact, chest images show a characteristic distribution with interstitial changes which are initially in the lung periphery and further deteriorate to small nodular ground glass opacities (19,20) (Figure 1).
Figure 1.
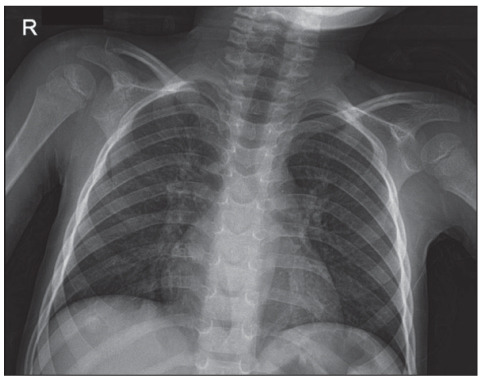
Chest X-ray of a 4-year old patient with Covid-19, admitted for high fever and dry cough. Reticular interstitial densities and bilateral lung involvement are shown.
In infants and children, it may be also useful to make lung ultrasound to avoid radiation and to obtain images directly at patient bedside. Lung ultrasound clearly document signs suggestive for interstitial-alveolar damage showing bilateral, diffuse pleural line abnormalities, subpleural consolidations, white lung areas and irregular vertical artefacts (21) (Figure 2).
Figure 2.
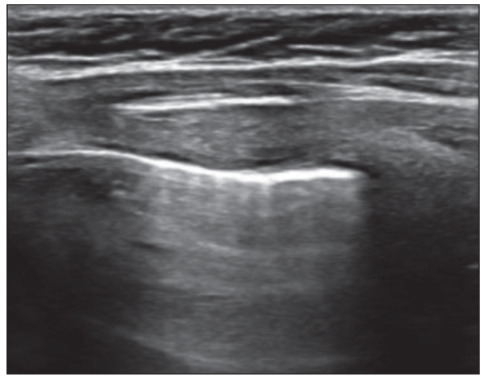
Lung Ultrasound of a 6-year child with Covid-19 and admitted for fever and cough. Vertical artifacts, named B lines, are shown, with increased thickness of pleural line.
Severity of infection
On the basis of the Chinese experience, the severity of COVID-19 disease in children is defined by clinical features, laboratory testing and chest radiograph into 5 groups (22) (Table 2).
Table 2.
Severity of Covid-19 infection in children. This classification has been formulated on the basis of Chinese data and experience to standardize prevention and management of 2019-nCoV infections in children22.
| Severity of infection | Clinical and radiological features |
| Asymptomatic | No clinical symptoms and signs, normal chest imaging, with positive 2019-nCoV nucleic acid test. |
| Mild | Symptoms of acute upper respiratory tract infection, including fever, fatigue, myalgia, cough, sore throat, runny nose and sneezing. Some cases may have nausea, vomiting, abdominal pain and diarrhoea. |
| Moderate | Pneumonia with fever and cough (mostly dry cough, followed by productive cough) without hypoxemia. Some cases may have no clinical signs and symptoms, but chest computed tomography shows typical lung lesions. |
| Severe | The disease progresses with dyspnoea and central cyanosis. Oxygen saturation is <92%. |
| Critical | Children and particularly adolescents and young adults can progress to respiratory failure and shock or other organs failure (encephalopathy, acute kidney injury, heart failure, coagulation dysfunction) . |
Management and treatment
Actually, there aren’t any drug trials specific for the children and adolescents.
According to the Chinese management protocol, the recommended treatment is usually supportive. In severe cases, when there is a respiratory involvement characterized by dyspnoea, central cyanosis and an oxygen saturation of less than 92%, they suggest to start oxygen therapy and antibiotics for bacterial superinfections (23).
The antiviral treatment and gamma globulin treatment are currently disputed (24).
Conclusion
COVID-19 infections remain undiagnosed in children because they often present mild symptoms. Fortunately, according to literature only a small proportion of children become critically ill. Children represented 2% of diagnosed cases in China (25), 1.2% of cases in Italy (26), and 1.7% of COVID-19 positive cases in the US (27).
The prognosis seems to be good with a recovery in 12-14 days for the majority of the reported cases worldwide. Only a death has been reported in a study of Lu X and Zhang, because of a secondary intussusception in a 10 month old child (28). Another report has showed that of the 2135 paediatric patients included in the study, only 1 child died (14-year-old boy from Hubei province) and most cases were mild (12).
Children are often exposed to viral infections so it is possible that they have higher levels of antibody against virus than adults. Another possible explanation is that children may be protected against SARS-CoV-2 because ACE-2 is less expressed at a younger age. Moreover, children’s immune system is still developing and may respond to pathogens differently from adult immune system.
Despite all, asymptomatic cases may have a lower transmission rate but remain a great source of infection.
The determination of the potential cluster transmission is very important for an epidemiological survey and to develop adequate measures for a better pandemic control.
Paediatricians are responsible for testing patients on the presence of signs and symptoms compatible with COVID-19, in order to protect vulnerable people, such as elderly and people with comorbidities.
Conflict of interest:
Each author declares that he or she has no commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangement etc.) that might pose a conflict of interest in connection with the submitted article
References
- 1.Zhu N, Zhang D, Wang W, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382(8):727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. Geneva, Switzerland: 2020. Coronavirus Disease 2019 (COVID-19): Situation Report; World Health Organization. [Google Scholar]
- 3.Niet A, Waanders BL, Walraven I. The role of children in the transmission of mild SARS-CoV-2 infection. Acta Paediatr. 2020 doi: 10.1111/apa.15310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Matthai J, Shanmugam N, Sobhan P. Coronavirus Disease (COVID-19) and the Gastrointestinal System in Children. Indian Pediatr. 2020:pii. doi: 10.1007/s13312-020-1851-5. S097475591600162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fu L, Wang B, Yuan T, et al. Clinical characteristics of coronavirus disease 2019 (COVID-19) in China: a systematic review and meta-analysis. J Infect. 2020 doi: 10.1016/j.jinf.2020.03.041. S0163-4453(20)30170-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhou P, Yang X.L, Wang X, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020:1–4. doi: 10.1038/s41586-020-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jin Y, Yang H, Ji W, et al. Virology, Epidemiology, Pathogenesis, and Control of COVID-19. Viruses. 2020;12(4) doi: 10.3390/v12040372. pii: E372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liu W, Zhang Q, Chen J, et al. Detection of Covid-19 in Children in Early January 2020 in Wuhan, China. N Engl J Med. 2020;382(14):1370–1371. doi: 10.1056/NEJMc2003717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Qing C, Yi-Ching C, Chyi-Liang C. Cheng-Hsun Chiu. SARS-CoV-2 infection in children: Transmission dynamics and clinical characteristics. J Formos Med Assoc. 2020;119(3):670–673. doi: 10.1016/j.jfma.2020.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. CDC. Coronavirus disease 2019 (COVID-19): cases in United States, February 12–April 2, 2020 CDC 2020. https://www.cdc.gov/coronavirus/2019-ncov/downloads/pui-form.pdf . [Google Scholar]
- 11.Tagarro A, Epalza C, Santos M, et al. Screening and Severity of Coronavirus Disease 2019 (COVID-19) in Children in Madrid, Spain. JAMA Pediatr. doi: 10.1001/jamapediatrics.2020.1346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yuanyuan D, Xi M, Yabin H, et al. Epidemiology of COVID-19 Among Children in China. Pediatrics. 2020:e20200702. doi: 10.1542/peds.2020-0702. [DOI] [PubMed] [Google Scholar]
- 13.Chen H, Guo J, Wang C, et al. Clinical characteristics and intrauterine vertical transmission Journal Pre-proof 6 potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records. Lancet. 2020;395(10226):809–815. doi: 10.1016/S0140-6736(20)30360-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chen Y, Peng H, Wang L, et al. Infants Born to Mothers with a New Coronavirus (COVID-19). Front. Pediatr. 2020 doi: 10.3389/fped.2020.00104. Doi: https://doi.org/10.3389/fped.2020.00104 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Saccone G, Carbone FI, Zullo F. The novel coronavirus (2019-nCoV) in pregnancy: What we need to know. Eur J Obstet Gynecol Reprod Biol. 2020 doi: 10.1016/j.ejogrb.2020.04.006. pii: S0301-2115(20)30174-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Morand A, Fabre A, Minodier P, et al. COVID-19 virus and children: What do we know. Arch Pediatr. 2020;27(3):117–118. doi: 10.1016/j.arcped.2020.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Brandon MH, Lippi G, Plebani M. Laboratory abnormalities in children with novel coronavirus disease 2019. Clin Chem Lab Med. 2020 doi: 10.1515/cclm-2020-0272. Doi: 10.1515/cclm-2020-0272. [DOI] [PubMed] [Google Scholar]
- 18.Du W, Yu J, Wang H. Clinical characteristics of COVID-19 in children compared with adults in Shandong Province, China. Infection. 2020 doi: 10.1007/s15010-020-01427-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Li W, Cui H, Li K, Fang Y, Li S. Chest computed tomography in children with COVID-19 respiratory infection. Pediatr Radiol. 2020 doi: 10.1007/s00247-020-04656-7. Doi: 10.1007/s00247-020-04656-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Liu H, Liu F, Li J, et al. Clinical and CT imaging features of the Covid-19 pneumonia: focus on pregnant woman and children. J Infect. 2020 doi: 10.1016/j.jinf.2020.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Vetrugno L, Bove T, Orso D, et al. Our Italian Experience Using Lung Ultrasound for Identification, Grading and Serial Follow-up of Severity of Lung Involvement for Management of Patients with COVID-19. Echocardiography. 2020 doi: 10.1111/echo.14664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fang F, Zhao D, Chen Y, et al. Recommendations for the diagnosis, prevention and control of the 2019 novel coronavirus infection in children (first interim edition) Zhonghua Er Ke Za Zhi. 2020;145(6):e20200834. doi: 10.3760/cma.j.issn.0578-1310.2020.0004. [DOI] [PubMed] [Google Scholar]
- 23.Kunling Shen, Yonghong Yang, Tianyou Wang, Dongchi Zhao, Yi Jiang, et al. Diagnosis, treatment, and prevention of 2019 novel coronavirus infection in children: experts’ consensus statement. World Journal of Pediatrics. 2020 doi: 10.1007/s12519-020-00343-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhang L, Liu Y. Potential interventions for novel coronavirus in China: A systematic review. J Med Virol. 2020;92(5):479–90. doi: 10.1002/jmv.25707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhang Y. The Epidemiological Characteristics of an Outbreak of 2019 Novel Coronavirus Diseases (COVID-19) China, 2020. Chinese Journal of Epidemiology. 2020;41(2):145–151. [Google Scholar]
- 26.Livingston E, Bucher K. Coronavirus Disease 2019 (COVID-19) in Italy. Jama. 2020 doi: 10.1001/jama.2020.4344. [DOI] [PubMed] [Google Scholar]
- 27. CDC. Coronavirus disease 2019 (COVID-19): cases in United States, April 14, 2020 CDC 2020 https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html#demographic-characteristics . [Google Scholar]
- 28.Lu X, Zhang L, Du H, et al. SARS-CoV-2 Infection in Children. N Engl J Med. 2020 doi: 10.1056/NEJMc2005073. [DOI] [PMC free article] [PubMed] [Google Scholar]


