Abstract
Nutrition plays a decisive role across geographies and societal groups in contributing to human health, strengthening resilience and extending the period of being free from non-communicable diseases (NCD) and increasing the quality of life. The objective of this review article is to shed some light on the multiple, often interconnected facets of the increased healthy longevity of populations, one of the greatest success stories humanity has achieved over the last century. Multiple stakeholders need to align to overcome some of the protective ‘hurdles’ established over decades that focus on treating diseases rather than preventing them whenever possible, and to create coherent policies and incentives with respect to individuals and healthcare systems in order to enable healthier populations.
Keywords: Nutrition, Prevention, Regulatory, Non-Communicable Disease (NCD), Ageing/Aging, Multi-stakeholder, Longevity, Treatment, Patient-centric, Food for Special Medical Purposes (FSMP)
Introduction
We are currently living in a VUCA world: volatile, uncertain, complex, and ambiguous. The ageing populations as one of our greatest success stories in humanity are part of it. To reduce some uncertainty and complexity, we need to find preferably simple solutions and implement them to keep our increased longevity ‘healthy’. Nutrition plays a decisive role in contributing to human health, in extending the period of being free from non-communicable diseases (NCD) and increasing the quality of life, across geographies and divergent societal groups. Hence, even though The Economist article from 2008 on ‘Abolishing Ageing. How to live forever’ concludes that this longstanding dream of mankind may still look unlikely, it seems no longer impossible (1). Yet, to make it happen, multiple stakeholders need to align to overcome some of the protective ‘hurdles’ we have established over decades to treat diseases rather than preventing them whenever possible, and to think out of the box to create coherent policies and incentives with respect to individuals and our healthcare systems.
The World Health Organization (WHO) declared 2020-2030 the ‘Decade of Healthy Ageing’ to bring together governments, civil society, international agencies, professionals, academia, the media and the private sector for concerted, catalytic and collaborative action to improve the lives of older people, their families and the communities in which they live. With already more than one billion people aged 60 years or over, populations around the world are ageing at a faster pace than ever and this demographic transition will have an impact on almost all aspects of society. The world has united around the 2030 Agenda for Sustainable Development: all countries and stakeholders have pledged that no one will be left behind and are determined to ensure that every human being can fulfil their potential in dignity and equality in a healthy environment. A strategic area to advance healthy aging is to improve measurement, monitoring and research, focusing on ‘the process of developing and maintaining the functional ability that enables well-being in older age, with functional ability determined by the intrinsic capacity of the individual, the environments they inhabit and the interaction between them’ (2).
In an ageing world, it is crucial to consider the role of preventative health interventions and to support people to live more active, healthier lives for longer. Preventing disease, along with limiting long term impairment and the compounding impact of multiple diseases not only has positive health and well-being outcomes, but also wider economic significances (3). For the first time in the history of mankind, NCDs have become the largest cause of mortality and Disability Adjusted Life Years (DALYs) globally. To have our healthcare systems cope with this challenge, we shall have to find the right balance between disease treatment and prevention, multi-stakeholder responsibilities and individual ownership. A more human-centric system balances the responsibility and the capacity of individuals towards healthy behavior, while requiring governments, businesses and civil society to cooperate to deliver healthier and more functional environments. A human-centric systems also shifts emphasis towards the early part of the care continuum - awareness and prevention (4).
Adequate nutrition is understood to be fundamental for good health and a good quality of life. Given nutrition’s intrinsic complexity, the impact of various dietary interventions is somewhat less clear, despite multiple studies spanning age, geography and income. Yet, access to quality foods, host immunity and response to inflammation/infections, impaired senses (i.e., sight, taste, smell) or mobility are all factors which can limit intake or increase the body’s need for specific micronutrients and influence physiological integrity throughout life as a primary contributor to a long and productive life (a healthy “lifespan”) (5).
The Paradox and Dilemma of Disease Prevention
Legislation worldwide defines disease prevention under drug (medicinal) law. Hence a food or nutrition preventing a disease becomes per definition a drug, with all its consequences for its development (quality, safety, efficacy) and subsequent lengthy approval process. Drug law - typically focusing on one active ingredient - is not adapted to the complexity of a food, hence this process is hardly ever used nor usable.
Food law, however, exceptionally allows for ‘reduction of disease risk (factor)’ claims, which might be considered somewhat equivalent to disease prevention (e.g. plant sterols lower blood cholesterol; high cholesterol is recognized as a risk factor in the development of coronary heart disease). Yet, only few respective claims have been approved so far world-wide. The typical stumbling blocks are to define an agreed upon biomarker - an approval process that may take even longer than product development - and unequivocal outcomes of long-term studies. Further to the lengthy development and its risks, a limited intellectual property protection (compared to drugs) for those performing the studies makes approved claims quickly become generic.
All of the above does not speak against the principle attributed to Hippocrates to ‘let your food be thy medicine’. It rather speaks for establishing the right incentives to have food, or nutrition, become the true, valuable partner within a more holistic disease prevention approach. Campaigns for vaccine, anti-caries, anti-smoking and increasing levels of physical activity, for instance, have successfully demonstrated that disease prevention works. Evidence indicates that up to 80% of premature heart disease, stroke and diabetes can be prevented (6). Changing dietary habits plays a crucial role in this: a large proportion of type 2 diabetes could be prevented - or even reverted. In legal terms this could equate to disease mitigation or treatment, however few healthcare systems fully reimburse individuals for changing dietary patterns.
The economic case for investing in population health and specifically in the primary prevention of chronic non-communicable diseases (NCDs) has been made across the years. Taking effective measures to prevent and control NCDs costs just an additional US$ 1.27 per person per year in Low and Low to Middle Income Countries (LMICs). The health gains from this investment will, in turn, generate US$350 billion through averted health costs and increased productivity by 2030, and save 8.2 million lives during the same period. For every US$1 invested in each policy area, various positive returns have been documented, including US$12.82 from promoting healthy diets (7, 8). Despite some large scale efforts, health promotion activities and disease prevention efforts targeting particularly the nutritional status and food consumption of older populations remain far from ideal.
Fineberg (9) reviewed in-depth, why disease prevention - though celebrated in principle - is such a difficult sell and often difficult to put into practice. Among the obstacles are that the success of prevention is invisible, lacks drama, often requires persistent behavior change, and may be long delayed; statistical lives have little emotional effect, and benefits often do not accrue to the payer; avoidable harm is accepted as normal, preventive advice may be inconsistent, and bias against errors of commission may deter action; prevention is expected to produce a net financial return, whereas treatment is expected only to be worth its cost; and commercial interests as well as personal, religious, or cultural beliefs may conflict with disease prevention.
Six strategies can help overcome these obstacles (9): 1. pay for preventive services. 2. make prevention financially rewarding for individuals and families. 3. involve employers to promote health in the workplace and provide incentives to employees to maintain healthy practices. 4. reengineer products and systems to make prevention simpler, lower in cost, and less dependent on individual action. 5. use policy to reinforce choices that favor prevention. 6. use multiple media channels to educate, elicit health promoting behavior, and strengthen healthy habits. Fineberg concludes that prevention of disease will succeed over time insofar as it can be embedded in a culture of health, where living a healthy life is the easiest and most affordable option for all (9).
NCD Prevention – Elevating the Role of Nutrition in an Ageing World
During the last century, we have made impressive progress in terms of longevity through improving healthcare, hygiene conditions, as well as food variety. Physicians likely know the already quoted ‘let your food be thy medicine’ by their forefather Hippocrates. Yet, in the last century, we seem to have forgotten or replaced this, realizing little to no apparent impact on a treatment focused curriculum for healthcare professionals during their studies, nor any emphasis on nutrition in the clinical setting. As a consequence, laudable yet long-haul efforts for instance by ESPEN (European Society for Clinical Nutrition and Metabolism) (10) and individual countries (e.g., Spain, Italy) are underway to make up for this (11).
In recent decades, however, after nutrient deficiency diseases have been largely eradicated, at least in the so-called middle-high income countries, an over-abundant food consumption combined with a more sedentary lifestyle has led to dramatic increases in NCDs, such as obesity, cardiovascular disease (CVD), diabetes and cancers. In parallel, nutrition science and policies have evolved to become more holistic, with better understanding of the role of nutrition in the broader context of dietary patterns, and ultimately the complex interactions between nutritional, dietary, social, behavioral and environmental factors - and how nutrition impacts health maintenance and promotion (12). Unfortunately, our well-established, system(at)ic healthcare reaction still incentivizes disease-care rather than prevention (e.g. health-care cost reimbursement; regulatory frameworks; patent protection).
More than 100 countries worldwide have developed dietary guidelines to provide simple, science-based recommendations, at times visualized as food pyramids or plates as a useful tool for building a healthy, balanced diet (13). Even though most policies over the last three decades are reasonably consistent with current, more science based recommendations (e.g., Mediterranean, Dietary Approaches to Stop Hypertension (DASH), Polymeal, Healthy Eating Index) (14), making best use of them may not always be straightforward, as they are often developed based on prevention of disease or nutrient deficiency, and less attention is paid to how well they promote health outcomes (15).
Studies of effects of nutrients or single foods on ageing often show inconsistent results. This is mostly due to taking the nutrient in isolation and not as part of the overall diet and patterns of food consumption. High intake of fruits, vegetables, fish, (whole) grains and legumes/pulses coupled with no smoking, moderate alcohol consumption and physically active routines have been associated with higher functionality and reduced risk of NCDs. Dietary patterns rich in red meat and ultra-processed foods, smoking, harmful consumption of alcohol and sedentary lifestyles have been associated with an increased risk of mortality and worse cardiometabolic outcomes (15). While understanding the role of specific components of foods for NCD risk is necessary, it may not be sufficient to generalize as it first requires to fully understand the importance of overall diets in reducing risk (14, 16), followed with investing into rethinking and developing sustainable health policies (17).
Notably, nutrition also has a role in disease management. The current regulatory approach with respect to food and nutrition tends to categorize individuals as consumers or patients, yet these states often occur simultaneously (18). Disease-related malnutrition, i.e. when the body does not get or cannot absorb enough nutrients, has become a leading global health problem. It frequently goes unrecognized and untreated. Efficiently leveraging nutrition, including personalization, is key to better prevent and manage major chronic diseases, based on implementing guidelines highlighting the importance of proper nutrition and the role it can play in preventing specific health disorders (19).
There is the growing field of research on the importance of nutrition in specific populations, such as the elderly, the hospitalized, and pre- and post-operative patients (19). However, even less than one half of patients identified as being malnourished receive nutritional intervention. The consequences include increased morbidity and mortality, as well as significant economic costs to health care systems and society.
As countries age, it will be important to support people to live healthier lives for longer. By doing so, we can not only improve well-being and enable people to remain active, but also reduce dependency, bringing down the impact on healthcare systems. Health systems have a key role to play in proactively supporting people to age well, through the provision of effective and well targeted interventions right throughout the life course. It is never too late to take preventative action, with adults in mid and later life to be included in health promotion programs right throughout life courses, if we are to live well for longer (3). Such interventions may include:
Screening programs for early detection of disease or those at risk of developing a specific disease
Supporting people to manage long-term multiple chronic conditions
Supporting adoption of healthier lifestyles (e.g., stop smoking; increased physical activity; nutrition) (3, 20, 21)
Despite governments across the globe acknowledging the case for prevention, investments are typically significantly lower than spending or incentives for healthcare treatment - even more so during economic downturns when prevention has tended to be more vulnerable to funding cuts. While preventative interventions do not have to come with large price tags to be effective, governments need to ensure that their stated commitments to promote health and well-being are backed with actions. Approximately one tenth of the total number of years lived with disability can be attributed to cardiovascular disease, and largely in older adults (3). The true impact of our current failure to invest in prevention could well be decades of additional health and economic burden in the years to come, hence the scale of the potential benefits from effective prevention should not be underestimated.
How is Nutrition Regulated?
The current global food and nutrition regulatory framework is built in a somewhat stratified way from health to disease (Figure 1). It transitions from general food to food supplements (US: dietary supplements) and food for specific groups (US: food for special dietary uses). While food for special medical purposes (FSMP; US: medical food) is governed by food law and standards, parenteral (i.e. intravenous) nutrition is regulated under drug (medicinal) law, largely for safety reasons as it requires sophisticated good manufacturing practices (GMP) and proper medical usage.
Figure 1.
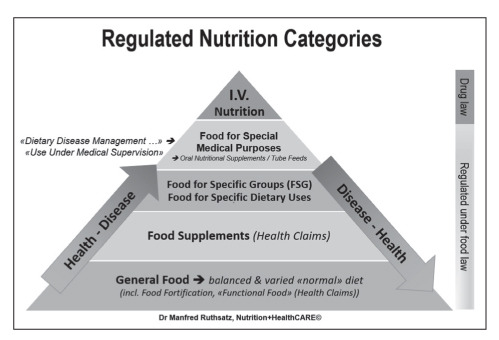
Regulatory Nutrition Science Pyramid (Schematic): Healthy Consumer vs Patient Continuum
FSMP is the only food category permitted to state the dietary management of disease as its intended use. However, only medicines are permitted to prevent, treat or cure a disease. Nutritional therapy hence is a term that still prompts pharmaceutical legislation in the mind of many regulators. For patients, the most concerned stakeholder, this instead signifies a nutritional solution to their disease or medical condition, that is safe and also nourishes them, the latter being an often overlooked benefit which medicines would not provide (22).
The current regulatory approach, with respect to food and nutrition, tends to categorize individuals as consumers or patients, yet these states often occur simultaneously (18, 23), as emphasized by novel diagnostic ‘omics’ technologies and new evidence from the gut microbiome, leading to personalized, targeted or precision approaches (23-25).
What are the regulatory and/or intellectual property issues that need to be addressed to overcome the existing hurdles and lack of incentives to instigate prevention, personalized nutrition and nutrition therapy as a partner to well established treatment options that consumers, patients (citizens!) and society would benefit? It may at first sight be surprising, but here nutrition seemingly is in a similar situation as developing medicines for Alzheimer’s disease in its early stages, where prevention and therapy definition or terminology appear to overlap (26). What are the legal hurdles or procedures (concerning market access processes, intellectual property patents or market exclusivity) that impede development for prevention or technology transfer from basic science to real world applications? What are some of the changes needed in current law or regulations that would facilitate or provide incentives to develop prevention approaches? (26).
Historically, the regulatory approval paradigms of today were developed to safeguard the public while treating or diagnosing a medically well recognized or accepted disease. Present guidelines presume the existence of well spelled out criteria for diagnosis and clear-cut therapeutic targets or outcome measures that would allow regulatory agencies to determine the efficacy of potential treatments. The assumptions and rationales of current regulatory guidelines are not directly applicable to interventions to prevent NCDs in asymptomatic people or those in a phase where they do not yet have a disease (26).
Rapidly evolving areas such as the human gut microbiome as well as personalized nutrition - i.e. in addition to population-based nutrition approaches - show promise with regards to their transformational potential in personalized and preventive healthcare concerning NCD related issues of an ageing society. New evidence is also created quickly due to novel technologies (e.g. “omics”; apps; wearables). Establishing the right framework conditions is foundational for progress in these areas, yet it is still largely not considered in the current regulations or policies. A reliable and trustworthy science base is a major criterion for healthcare systems to support novel interventions or to take up in novel dietary guidelines. Regulatory systems should accept the concept of a continuum between health and disease, food and drug, consumer and patient, as part of a more holistic approach. Creating awareness and understanding for regulators, policy makers, citizens and healthcare providers is essential (28), while at the same time not encouraging the hype currently associated to these fields (Table 1) (25). These consumer - directly consumer and patient-centric regulatory topics have been discerned and addressed for instance in the annual RAPS publication series ‘Nutrition in Health and Disease Management’ (27).
Table 1.
Policy needs: The gut microbiome as a target for personalized nutrition (adapted from (25))
REGULATORY NEEDS
|
CREATING VALUE
|
The ‘Forgotten Food’
Food for Special Medical Purposes (FSMP) - or medical food (US), artificial nutrition, enteral nutrition, including Oral Nutritional Supplements (ONS) - is globally regulated as ‘food’(29). It has been a significant evolution since the 1950s with FSMP first falling under the drug law, then being considered a food for special dietary uses (FSDU), and ultimately in the European Union (EU) being regulated amongst the Foods for Specific Groups (22). Here, the EU Commission, together with the European Food Safety Authority (EFSA), has made a significant step forward to include also the practical aspects, i.e. patient-centered usage, into its recent revision of respective regulations and guidelines (30).
Still, somewhat ‘forgotten’, leveraging the targeted benefits of nutrition in general is certainly underrated in the healthcare professionals’ education worldwide, despite significant awareness building efforts for instance by the ESPEN medical association. There is a definite need to improve patient access to a more holistic treatment approach that includes medical nutrition coupled with medicinal treatments or services (10, 11, 31).
On the one hand, one reason for FSMP being an underrated resource, is a relatively low level of reimbursement (albeit with few exceptions, e.g. for some inborn errors of metabolism (IEM) related diseases), typically based on kilo-calories provided, founded on a perceived ‘food image’, i.e. an undisputed necessity to eat. Yet, despite FSMPs’ proven clinical and physiological benefits, this intrinsically limits, to the detriment of patients and health-care systems, the access to safe, low-cost, cost-efficient factor in a holistic treatment approach.
On the other hand, a perceived ‘medical image’ of FSMP due to its intended use for the dietary management of a disease or medical condition, i.e. for a ‘vulnerable’ population, can lead to avoidable situations: though having to fulfil technical requirements like other foods, it is sometimes unjustifiably considered closer to medicines than general food. This can significantly delay patient access to FSMP in some countries, even if it is already beneficially used in many other countries. Unlike any other food, which is largely mutually replaceable in case of a short-term unavailability, this may create serious (safety) issues for patients, be it for technical, regulatory, or reimbursement reasons. FSMPs save lives (Table 2), a clear plaidoyer for a patient-centric approach.
Table 2.
Medical Nutrition: Improving Nutritional Status / Clinical Advantage (adapted from (21))
| Medical Nutrition | Medical Condition | Clinical Benefit |
| Nutrition as Disease-related Malnutrition Management | Short Bowel Syndrome; Stroke | Life-saving Intervention |
| COPD | Increased Ventilatory Capacity | |
| Surgical Patients | Less Complications | |
| Older Patients | Increased Quality of Life, Decreased Morbidity/ Mortality | |
| Nutrition as Disease Management (‘Treatment’) | Crohn’s Disease | Induction of Remission |
| Cow’s Milk Allergy | Reduced Symptoms, Catch-up Growth | |
| IEMs: PKU, MSUD, FAOD, GSD… | Normal Growth & Development | |
| Intractable Epilepsy | Less Seizures; Normal Growth & Development |
Currently, more than one in three patients in care homes or older persons living independently, are malnourished or at risk of malnourishment. Malnutrition has a particularly high adverse effect in this population, impairing function, mobility and independence. It is an independent predictor of mortality even after adjusting for age and comorbidity (19). With an increasingly ageing population across Europe, interventions to prevent, identify and manage malnutrition are vital. People of all ages are affected, yet malnutrition is significantly more common in older people. Disease-related malnutrition, specifically undernutrition, continues to go undetected and untreated. Malnutrition affects the lives of millions of people and poses a significant burden on the healthcare economy with estimated costs of beyond €170 billion in Europe alone. Whilst most commonly identified in institutions, particularly amongst patients in hospitals and care homes, the majority of people who are malnourished or who are at risk of malnutrition live in the community.
A growing body of evidence demonstrates the benefits of medical nutrition (19). Covering the full spectrum of medical nutrition, from oral nutrition supplements (ONS) to enteral tube feeding and parenteral nutrition, MNI’s publication «Better care though better nutrition: value and effects of medical nutrition» draws on a wide range of independent evidence to address the worldwide prevalence, causes and consequences of malnutrition, as well as the health and economic benefits of nutritional care, good practice examples and guidance. Endorsed by other key stakeholders (ESPEN, EUGMS, ESPGHAN, EFAD, ENHA), this report provides a unique evidence-base of the burden of malnutrition and the value and effects of medical nutrition, encompassing healthcare settings (hospital, community), age groups (children, adult, elderly) and patient groups (19).
Steps to tackle the malnutrition epidemic include implementing routine nutrition risk screening across the EU, increasing education campaigns to raise public awareness, and implementing proper science-based nutrition care for patients, as exemplified by the Optimal Nutrition Care for All (ONCA) campaign across 18 countries (32, 33).
Oral nutritional supplements (ONS) as FSMP, not to be mistaken for ‘food supplements’, have proven functional and clinical benefits in older malnourished patients in the community, improving physical activity, quality of life, and independence measures. ONS usage is consistently linked to lower mortality and complication rates when compared to standard care. Malnourished patients given ONS show improved rehabilitation, have fewer readmissions to hospital, as well as a reduction of length of stay by some two days (19). The clinical benefits of using ONS can help to significantly reduce healthcare costs, with substantial savings in both hospital and community settings (34, 35).
R&D and Multiple Stakeholder Initiatives Going Forward
Given its complexity and the interdependency of its elements, enabling healthier and longer living through food and nutrition interventions is not just a health agenda; it is an imperative for all of society. For sustained impact, multi-stakeholder collaboration – including public, private and civil society stakeholders – is the only systematic way to comprehensively promote healthy living. Since multiple factors influence these behaviours, single-sector or stakeholder actions cannot effectively influence all aspects of Healthy Living. Each of these influences interacts through a variety of actors, some of which may seem to have little or nothing to do with health per se. To create the necessary scale of Healthy Living change, all actions will need to comprehensively address each specific influence – and only multiple stakeholders working together have the ability to execute actions of greater value and impact.
Working together will maximize impact. Stakeholders often work in silos, unaware of the ambition and activities of other relevant stakeholders. Collaboration – aligning goals, resources and metrics, and working in a coordinated manner – can multiply the impact of individual stakeholders. Moreover, exploring mutually beneficial linkages across stakeholders and programmes can contribute to building organizational capacity, particul also in low- and middle-income countries. Resources are limited for all stakeholders, therefore a multi-stakeholder approach means a pooling of resources, allowing the collaboration to maximize its financial and technical expertise, which is particularly important in fiscally constrained environments.
By working together, stakeholders can draw on collective core competencies to create a more comprehensive set of capabilities. The digital revolution offers innovative tools for promoting healthy lives; applying these tools will require participation from partners across different sectors.(36)
Making changes to an established system is complex - with individual stakeholders like researchers, regulators, industries, payers already well positioned, rules and incentives well in place. Even when potential benefits may sound compelling to most, here, putting combined efforts from different stakeholders behind a simple, straightforward goal and a clear path to implementation appears to be most promising. As an African proverb states: ‘If you want to go fast, go alone, if you want to go far, go together’.
Over the last years and decades, numerous initiatives have been focusing on NCDs, longevity and an ageing world, including relevant scientific, regulatory or policy related congresses. The predominant focus is on finding treatment or therapeutic solutions. Nutrition rarely plays a significant role, and if at all, then rather as a ‘low-tech’, junior partner to a medicinal treatment approach. All stakeholders will have to admit that nutrition is more than just “one also has to eat” phenomenon or avoiding those reputedly unhealthy diets high in saturated or trans fats, sugars, or salt.
Nutrition may indeed be the most promising way forward to help solve NCDs in this VUCA world. Key to all success will be that, beyond awareness building, appropriate implementation measures will take place. With this in mind, here come a few outstanding science and public health based examples with a focus on the value of nutrition (a list that by definition asks to remain far from complete):
EU Commission initiated, supported or funded activities such as:
European Innovation Partnership (EIP) on Active and Healthy Ageing (AHA) - which includes the Action Group A3 on Lifespan Health Promotion and Prevention of Age-Related Frailty and Disease (37-39)
Optimal Nutrition Care for All (ONCA/ENHA) campaign across 18 countries, on assessing malnutrition and implementing the most appropriate nutrition care (32-36)
Joint Programming Initiative (JPI) - A Healthy Diet for a Healthy Life (40)
The World Health Organization (WHO) has been setting up an Action Plan for the Prevention and Control of Noncommunicable Disease in the WHO European Region (2016-2025) (41). Most recently the All Party Parliamentary Group for Longevity (APPG, UK) started to develop the Health of the Nation. A Strategy for Healthier Longer Lives to be achieved by 2030 (42). In the US, the National Academies of Sciences, Engineering, Medicine (NASEM) are very active with initiatives leveraging nutrition and NCDs (16), while China developed its National Nutrition Plan (Year 2017-2030) which includes actions to improve nutrition for the elderly (43). Foundation driven initiatives, such as the Fondation Mérieux’s Better Foods for Better Health platform (44), round out the above approaches.
Well-orchestrated multi-stakeholder initiatives can be considered a gold standard to provide a promising way for an open dialogue to promote a science and technology based, yet flexible, regulatory and policy guidance framework in the food-medicine continuum, which includes nutrition for prevention and potentially therapeutic public health measures.
Conclusion – a call for action
Increasing longevity is one of our greatest success stories in humanity. Though never too late, NCD prevention for an active and healthy ageing starts much earlier than once one becomes an older adult or ‘senior’. To keep our lives healthy, also in an ageing world, action is required. We do already have enough knowledge to act now, even though additional research is required on how NCDs are influenced by multiple factors, such as genes, human behaviour, lifestyle, diets. We shall have to accept a certain uncertainty in our decision making and this may require taking some - very limited - risks, as doing nothing is not an option.
Our world will remain a “VUCA World”, i.e. volatile, uncertain, complex and ambiguous, with changes occurring more rapidly than ever before. In simplifying complexity to create solutions, working together responsibly in multi-stakeholder initiatives is one proactive way forward. Here, understanding and making the regulatory and policy environments work in context, is fundamental to developing and implementing workable solutions.
Elevating the role of nutrition is a core element to tackle issues of global concern to an ageing society in our daily lives and as a well-integrated part of standard medical treatment in fighting disease-related malnutrition. Driven by trained healthcare professionals, medical nutrition has been shown to lead to significant clinical and cost-efficient outcomes, and with the usage of oral nutritional supplements (ONS), to reduce the length of stay for patients, impacting the economic model for hospitals and health care institutions.
Disease prevention whenever possible is ultimately more cost-efficient than treatment of a preventable NCD. Ensuring consumer- and patient-centric access, nutrition in all its regulated forms is a crucial partner to medical treatment, increasing access. Patients need to be made aware of and included in their holistic treatment agenda to develop and implement the best possible (product) solution.
An innovation-friendly environment and incentives (including regulatory framework; intellectual property protection; reimbursement), along with a timely decision-making, will significantly impact the development, launch and usage of suitable products. For low risk yet essential nutrition solutions, this avoids potential harm to consumers or patients in the areas of obesity, NCD prevention and nutrition therapy. An ageing world will benefit through longevity in better health.
Disclaimer:
This article reflects the personal opinion and experience of the authors. It should not be construed as an official position by any organization with which the authors are affiliated.
Conflict of interest:
Each author declares that he or she has no commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangement etc.) that might pose a conflict of interest in connection with the submitted article
References
- 1.Abolishing Ageing. How to live forever. The Economist. Science and technology. 2008 January 5:64–66. [Google Scholar]
- 2.WHO - Decade of Healthy Ageing (2020-2030) https://www.who.int/ageing/decade-of-healthy-ageing .
- 3.International Longevity Centre - UK (ILC) Never too late: Prevention in an ageing world. 2019. https://ilcuk.org.uk/
- 4.World Economy Forum (WEF) White Paper: Human-Centric Health: Behaviour Change and the Prevention of Non-Communicable Diseases. 2017. http://www3.weforum.org/docs/IP/2016/HE/HCH_Report2017.pdf .
- 5.Marsman D, Belsky DW, Gregori D, et al. Healthy ageing: the natural consequences of good nutrition - a conference report. European Journal of Nutrition. Supplement. 2018 doi: 10.1007/s00394-018-1723-0. https://doi.org/10.1007/s00394-018-1723-0 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Organization (WHO) Noncommunicable diseases (NCD) https://www.who.int/gho/ncd/en/
- 7.World Health Organization (WHO) Geneva, Switzerland: 2018. Saving lives, spending less: a strategic response to noncommunicable diseases. (WHO/NMH/NVI/18.8) [Google Scholar]
- 8.World Economy Forum (WEF) Maximizing Healthy Life Years. 2015. http://www3.weforum.org/docs/WEF_Maximizing_Healthy_Life_Years.pdf .
- 9.Fineberg HV. The Paradox of Disease Prevention: Celebrated in Principle, Resisted in Practice. JAMA. 2013 Jul 3;310(1):85–90. doi: 10.1001/jama.2013.7518. [DOI] [PubMed] [Google Scholar]
- 10.European Society for Clinical Nutrition and Metabolism (ESPEN) Guidelines. www.espen.org . [Google Scholar]
- 11.Cuerda C, Muscaritoli M, Donini LM, et al. Nutrition education in medical schools (NEMS) An ESPEN position paper – Clinical Nutrition. 2019;38:969–974. doi: 10.1016/j.clnu.2019.02.001. [DOI] [PubMed] [Google Scholar]
- 12.Shao A, Drewnowski A, Willcox DC, et al. Optimal nutrition and the ever-changing dietary landscape: a conference report. Eur J Nutr. doi: 10.1007/s00394-017-1460-9. Supplement 2017 published online 05 May. DOI 10.1007/s00394-017-1460-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.European Food Information Council (EUFIC) Make sense of dietary guidelines. 2020 Brussels. www.eufic.org . [Google Scholar]
- 14.Schneeman BO. Impact of Changing Scientific Recommendations on Nutrition Policies. Regulatory Focus. Regulatory Affairs Professionals Society (RAPS) July 2018 [Google Scholar]
- 15.Kiefte-de Jong JC, Mathers JC, Franco OH. Nutrition and healthy ageing: The key ingredients. Proc Nutr Soc. 2014;73(02):1–11. doi: 10.1017/S0029665113003881. February. https://www.researchgate.net/publication/260119669_Nutrition_and_healthy_ageing_The_key_ingredients . [DOI] [PubMed] [Google Scholar]
- 16.Food and Nutrition Boardy; Health and Medicine Division; National Academies of Sciences, Engineering, and Medicine (NASEM) Washington (DC): 2016 Jul 13. Meeting the Dietary Needs of Older Adults. Exploring the Impact of the Physical, Social, and Cultural Environment: Workshop Summary. ISBN-13: 978-0-309-44227-5ISBN-10: 0-309-44227-3. http://www.nationalacademies.org/hmd/Activities/Aging/Dietary-Needs-Older-Adults.aspx . [PubMed] [Google Scholar]
- 17.Magni P, Bier DM, Pecorelli S, et al. Perspective: Improving Nutritional Guidelines for Sustainable Health Policies: Current Status and Perspectives. Adv Nutr. 2017;8:532–545. doi: 10.3945/an.116.014738. doi: 10.3945/an.116.014738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schneeman BO. Does nutrition have a role in disease management? Regulatory Focus. Regulatory Affairs Professionals Society (RAPS) 2017 October [Google Scholar]
- 19.Medical Nutrition International Industry (MNI) Better care through better nutrition: Value and effects of Medical Nutrition. A summary of the evidence base. 2018 https://european-nutrition.org/wp-content/uploads/2018/03/Better-care-through-better-nutrition.pdf . [Google Scholar]
- 20.Richardson DP. Nutrition, Healthy Ageing and Public Policy. International Alliance of Dietary/Food Supplement Associations (IADSA): (2007) https://www.iadsa.org/nutrition-health-ageing-and-public-policy . [Google Scholar]
- 21.Kalache A, de Hoogh I, Howlett SE, et al. Nutrition interventions for healthy ageing across the lifespan: a conference report. Eur J Nutr. Supplement. 2019 doi: 10.1007/s00394-019-02027-z. https://doi.org/10.1007/s00394-019-02027-z . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bushell C, Ruthsatz M. Revising the EU FSMP Regulatory Framework: Laying the Foundation for Future Nutritional Patient Care. Regulatory Focus. Regulatory Affairs Professionals Society (RAPS) 2018 July [Google Scholar]
- 23.Ruthsatz M. Role of Nutritional Therapy in Healthcare Innovation: The Need for Reshaping Regulatory Paradigms. In: Réalités Industrielles - a series of Annales des Mines. 2017:80–85. [Google Scholar]
- 24.Kaput J, Draper C, Descombes P, Rezzi S, Kussmann M. Targeted (Personalized) Nutrition. Regulatory Focus, August 2016, Regulatory Affairs Professionals Society (RAPS) http://www.raps.org/regulatoryDetail.aspx?id=25724 . [Google Scholar]
- 25.D’Hondt K, Kaput J, Ruthsatz M. Personalized nutrition for better health - targeting the human microbiome. Regulatory Focus. June 2019, RAPS, US. https://www.raps.org/news-and-articles/news-articles/2019/6/personalized-nutrition-for-better-health-targetin . [Google Scholar]
- 26.Organisation for Economic Co-operation and Development (OECD) Emerging Trends in Biomedicine and Health Technology Innovation: Addressing the Global Challenge of Alzheimer’s, OECD Science, Technology and Industry Policy Papers, 2013; No. 6, OECD Publishing [Google Scholar]
- 27.Hall G. Editorial to ‘Nutrition in Health and Disease Management’. Regulatory Focus (RF). July 2019, Regulatory Affairs Professionals Society (RAPS) https://www.raps.org/news-and-articles/news-articles/2019/7/nutrition-in-health-and-disease-management . [Google Scholar]
- 28.Organisation for Economic Co-operation and Development (OECD) The Microbiome, Diet and Health. Towards a Science and Innovation Agenda. OECD Science, Technology and Innovation Policy Papers. September 2017; No. 42. https://www.oecd-ilibrary.org/docserver/d496f56d-en.pdf?expires=1583531353&id=id&accname=guest&checksum=DD5B4ECF5CC2F384F318A13D3C4E2EDF . [Google Scholar]
- 29.Ruthsatz M, Morck T. Medical Food/Food for Special Medical Purposes: Global Regulatory Challenges and Opportunities. Regulatory Focus, August 2016, Regulatory Affairs Professionals Society (RAPS) [Google Scholar]
- 30.EU Commission Notice on the Classification of Food for Special Medical Purposes (2017/C 401/01), Official Journal of the European Union. https://eur-lex.europa.eu/legal-content/EN/TXT/PDF/?uri=CELEX:52017XC1125(01)&from=EN . [Google Scholar]
- 31.EPF, EGAN and ENHA. Patient Perspectives on Nutrition. 2013 http://www.european-nutrition.org/images/uploads/pub-pdfs/Patient_perspectives_on_nutrition_pdf . [Google Scholar]
- 32.Optimal Nutrition Care for All (ONCA) Campaign. https://european-nutrition.org . [Google Scholar]
- 33.De Man F, Smit C, Ruthsatz M. Innovating patient driven nutritional care in Europe: The Optimal Nutrition Care for All (ONCA) multi-stakeholder initiative. Regulatory Focus. October 2017, Regulatory Affairs Professionals Society (RAPS) https://www.raps.org/regulatory-focus%E2%84%A2/news-articles/2017/10/innovating-patient-driven-nutritional-care-across-europe-the-optimal-nutritional-care-for-all-(onca . [Google Scholar]
- 34.Elia M, Normand C, Laviano A, Norman K. A Systematic Review of the Cost and Cost Effectiveness of Using Standard Oral Nutritional Supplements in Community and Care Home Settings. Clin Nutr. 2016;35:125–137. doi: 10.1016/j.clnu.2015.07.012. [DOI] [PubMed] [Google Scholar]
- 35.Elia M, Normand C, Norman K, Laviano A. A Systematic Review of the Cost and Cost Effectiveness of Using Standard Oral Nutritional Supplements in the Hospital Setting. Clin Nutr. 2016;35:370–380. doi: 10.1016/j.clnu.2015.05.010. [DOI] [PubMed] [Google Scholar]
- 36.World Economic Forum, The Pan American Health Organization, In collaboration with Bain & Company. Multistakeholder Collaboration for Healthy Living. Toolkit for Joint Action (March 2013) http://www3.weforum.org/docs/WEF_HE_HealthyLiving_Toolkit_2013.pdf . [Google Scholar]
- 37.European Innovation Partnership (EIP) on Active and Healthy Ageing (AHA) https://ec.europa.eu/research/innovation-union/pdf/active-healthy-ageing/rs_catalogue.pdf . [Google Scholar]
- 38.Ning Mak T, Caldeira S. The Role of Nutrition in Active and Healthy Ageing. For prevention and treatment of age-related diseases: evidence so far. EU Commission. JRC Science and Policy Reports. 2014 https://publications.jrc.ec.europa.eu/repository/bitstream/JRC90454/lbna26666enn.pdf . [Google Scholar]
- 39.EIP AHA Action Group A3. Lifespan Health Promotion & Prevention of Age Related Frailty and Disease. https://ec.europa.eu/eip/ageing/actiongroup/index/a3_en . [Google Scholar]
- 40.Joint Programming Initiative (JPI). A Healthy Diet for a Healthy Life (HDHL) https://www.healthydietforhealthylife.eu/index.php/ec-partnerships/era-hdhl . [Google Scholar]
- 41.World Health Action Plan for the Prevention and Control of Noncommunicable Diseases in the WHO European Region (2016-2025) http://www.euro.who.int/__data/assets/pdf_file/0008/346328/NCD-ActionPlan-GB.pdf?ua=1 . [Google Scholar]
- 42.All Party Parliamentary Group (UK) for Longevity. The Health of the Nation. A Strategy for Healthier Longer Lives. 2020 https://appg-longevity.org/events-publications . [Google Scholar]
- 43.The Notice by the General Office of the State Council on Printing and Distributing National Nutrition Plan (Year 2017-2030) China. 2017 https://extranet.who.int/nutrition/gina/sites/default/files/CHN%202017%20National%20Nutrition%20Plan.pdf . [Google Scholar]
- 44.Fondation Mérieux. 5th Better Foods for Better Health interviews (2015) https://www.fondation-merieux.org/en/media-gallery/ Websites accessed on May 8, 2020. [Google Scholar]


