Abstract
Background and aim of the work:
The incidence of periprostethic femur fractures has increased over the last years; the treatment includes an open reduction and internal fixation or revision implant. The treatment of these fractures can be complex, expensive and associated with risks of systemic and local complications.
Methods:
We evaluated clinical and radiological results in patients treated in our department for periprosthetic femoral fractures from 2011 to 2017. We included 52 cases of periprosthetic fractures regardless of their classification with a mean follow-up of 2 years. The analisys of the result was performed using Harris Hip Score and searching for radiographic signs of loosening, infections or mechanical failure of the implants.
Results:
There was no evidence of septic complications or mechanical failure in cases treated. The average HHS was equal to 92 points with a certificate pain relief and a sufficient independence in daily living activities.
Conclusions:
The treatment of periprosthetic fractures is complex: it depends on type of fracture, on stability of the stem and on the bone quality. A right classification of the fractures, a good experience of the surgeon in prosthetic and trauma surgery is the basis for the best treatment. (www.actabiomedica.it)
Keywords: peri-prosthetic femur fracture, osteosynthesis, angular stability plates
Introduction
In recent decades there has been a progressive number of total hip replacement implants linked to a significant increase in the life expectancy of the population. Suffice it to think that from a life expectancy in 1930 of 53.8 years for men and 56 years for women, in 2016 it rose to 80.6 a year and 85 aa (ISTAT 2017 data).
This growing number of implants, often in very young subjects and with increasing functional demands, has determined a constant increase in the number of peri-prosthetic fractures of the proximal femur.
The peri-prosthetic femoral fracture is the fourth cause of hip prosthetic revision by order of frequency (2.5%), after aseptic loosening (74.9%), dislocation (7.6%) and mobilization septic (7.3%). Femoral fractures in patients with hip replacement in the literature are reported with a frequency varying between 0.3% and 2.5% of all implants, in particular 1.5% in the first implants and 6-7% in revision prosthetic surgery (1, 2).
Traumatic forms are the result of direct or high-energy trauma such as mobilization in narcosis in rigid prostheses (generally for knee prostheses) (3).
Among the systemic causes a decisive role is played by osteoporosis that reduces the resistance of the bone, follow the neurological disorders that increase the risk of falling and rheumatoid arthritis, responsible for a chronic inflammatory process that requires long steroid treatments.
At the local level there are factors that cause weakening of the bone resistance, such as technical errors during implantation, such as fissures and/or iatrogenic cortical defects, misalignment of the prosthetic components, excessive removal of cancellous bone, positioning of the stem in varus, loss of bone substance linked to repeated revision operations, reabsorption from osteolysis due to polyethylene wear and presence of bone windows in the replanting (4-8).
Finally, the prosthetic design must avoid surface stress at the bone-prosthesis interface and excessive bone resection (9).
The treatment of these fractures is a challenge for the orthopedist because it is necessary to obtain an anatomical synthesis and a stable implant, it is essential to re-establish a good anatomical axis and the early mobilization of the patient is fundamental, especially in elderly subjects for whom the entrapment is synonymous with death.
Classification
Among the various classifications proposed for the framing of these fractures we use the one in Vancouver according to Duncan and Masri (1995), which analyzes the site of the fracture and the stability of the stem.
Type A: fractures affecting the trochanteric region GT-AG or PT-AL; they are generally stable fractures.
Type B: fractures around or immediately below the femoral stem with stability or mobilization of the same: B1 stable stem, B2 unstable stem, adequate stock bone, B3 unstable stem and inadequate bone stock.
Type C: distal fractures at the apex of the femoral stem (which remains stable) (Figure 1).
Figure 1.

Classification Vancuver
Treatment options are:
- conservative, burdened by a high percentage of unsatisfactory results (40-50%);
- surgical, indicated in most fractures, but burdened by numerous risks intra, peri and post-operators.
The evaluation of the state of the prosthesis and of the type of fracture, with different radiographic projections and CT, is of fundamental importance in our therapeutic choice.
We treat type A fractures, characterized by the tearing of the small or large trochanter, conservatively: functional rest for 3-4 weeks with the possible use of Newport-type hip brace. Surgery of osteosynthesis with circles or molded plates is reserved for rare cases of secondary fracture dissolution.
In fractures of type B1 (stable stem) we opt for reduction and synthesis with plates, screws and rims that guarantee an excellent primary stability of the synthesis in the presence of stability of the prosthetic implant, resulting in rapid mobilization of the patient and early loading.
In the type B2 fractures (mobilized stem) we remove the mobilized stem and re-implant a non-cemented modular revision prosthetic stem by-passing the fracture; the apex of the femoral stem should overcome the fracture by at least twice the femoral diameter.
Fractures of type B3 (mobilized stem + bone loss) are the most difficult to treat: after removal of the mobilized stem and replanting of a modular revision stem it is often found that insufficient stability of the fracture is not achieved; therefore a bone grafting (allograft - autograft), in chips and/or bone sticks is used, in order to restore an adequate bone stock, a chapter that goes beyond our treatment.
Type C fractures are treated by means of gore reduction and synthesis with plates, screws and rims.
Sometimes they can be considered and treated as conventional diaphyseal fractures.
The same principles set out for B1 fractures apply to their treatment.
The Vancouver classification then analyzes the site of the lesion, traces the guidelines for the framing of peri-prosthetic fractures, thus providing a valid algorithm for their treatment. The surgical treatment approach is the method of choice for the treatment of these fractures, but from various recent works it has been shown that it is not without complications.
According to Erhardt J.B. complications of surgical treatment with traditional osteosynthesis exceed 50% (10-11), in particular: lack of consolidation (pseudoarthrosis) 24%, refracture 24%, vicious consolidation 14%, loss of fixation (mobilization of synthetic resources) 23%, mobilization (loosening) of the prosthesis 21%, recurrent dislocation of the prosthesis 16%.
Surgical treatment
The treatment of these fractures represents a difficult challenge for the orthopedic surgeon with difficulty in obtaining a good fixation due to the presence of a medullary system, stable or mobilized, in a bone with often very compromised quality.
For osteosynthesis there is a need for a stable and reliable fixation system, precisely of the plates: the use of bi-cortical screws around the prosthesis is difficult; the uni-cortical screws and the rims do not always guarantee tightness and stability; the rims can also cause damage to the periosteum.
The presence of cement inside the femoral canal is another reason for technical difficulty.
Our current orientation for the treatment of femoral peri-prosthetic fractures with a stable implant (A, B1, C) is the use of the new Zimmer NCB (Non-Contact Bridging), poly-axial angular stability plates (10, 12, 13).
The system is composed of a proximal femoral plate, a distal and a curve for the femoral diaphysis; the proximal and distal plaques are larger in the area of the prosthesis and contain holes with offset, allowing the placement of bi-cortical screws around the prosthesis (Figure 2).
Figure 2.

Plates
Along the stem there is a diagonal motif with three holes, of which 2 holes with offset and a central hole for mono-cortical screws and cable buttons / cables (Figure 3).
Figure 3.

Cable button
The screws can be fixed freely thanks to the poly-axiality (30° cone) and can be locked to obtain angular stability; thanks to non-contact bridging the risks of damage to the periosteum are reduced.
The screws can be placed through the cement.
There is also a plate to be used in the case of fractures of the trochanteric mass: cable -ready (Figure 4).
Figure 4.

Cable-ready
The plate design is specific for periprosthetic fractures (wide vs. narrow): the “wide” proximal part of the plate allows anchoring of bicortical screws around the prosthesis; the “narrower” part, placed anatomically on the femoral diaphysis, minimizes soft tissue damage.
The poly-axial angular stability technology NCB also guarantees the Periprosthetic Polydial Angular Stability to the system.
When the proximal femoral plate was selected and compared with a LCP Broad Curved Femur Shaft Plate, 1 million load cycles were applied in the Materials Laboratory: the NCB PP Proximal Femur Plate broke at a load of 500 N (24.5 Nm bending moment), showing almost double the resistance to the LCP Broad Curved Plate Femur Shaft Plate which broke at a load of 240 N (11.8 Nm bending moment) (6, 10, 12, 14).
Materials and methods
From January 2011 to December 2017, we treated 52 patients with peri-prosthetic femoral fracture, 46 women and 6 men, mean age 82.5 years (69-93). All fractures were caused by accidental fall in patients unable to walk normally except for one case (93-year-old woman), residing at RSA and with poor mobilization capacity.
The 52 patients studied were all carriers of hip replacement: 44 total (24 cemented and 20 non-cemented), 8 cephalic (cemented bipolar), 2 with bilateral prosthesis.
According to the Vancouver classification we recorded 28 type B1 fractures, 6 type B2 fractures (which in consideration of age - 90 years and 93 years - and of the general conditions we treated by synthesis only), 18 type C fractures.
In our series over 60% of periprosthetic fractures is type B, preferential localization area, because if the prosthesis is mobilized the surrounding bone is fragile, while if the prosthesis is stable this constitutes a wedge in a seat with different elasticity (Figure 5).
Figure 5.

Type B: over 60% periprostehetic fractures
The stability of the prosthetic implant was evaluated directly on the operative field, in all the treated cases; in 48 patients the peri-prosthetic fracture involved a first implant and in 4 patients a re-implantation.
The average time between the fracture event and the implant of the prosthesis was 10.6 years.
All patients were given anti-thrombo-embolic therapy with EPBM for a period of 5 weeks and antibiotic prophylaxis with Cefazolin 2 gr. ev. to pre-anesthesia in a single administration (very-short-shot).
All the patients were operated within 48 hours of the trauma, even those suffering from serious multi-pathologies and severe co-morbidities, according to the guidelines issued by the Lombardy Region.
44 patients performed General Anesthesia and 8 Spinal Anesthesia.
The average surgical time was 90 minutes; the average bleeding of 450 ml.
There were no early or late infections, dislocations or peripheral vascular-nervous damage.
Two patients died in the post-operative period due to massive pulmonary embolism.
The average hospitalization time was 14.8 days.
The postoperative protocol provided for the start of bed-assisted mobilization for the recovery of the hip and knee ROM starting from the 2nd day; mobilization in the armchair on the 3rd day and protected overflow load (walker, 2 crutches) in 5th-8th day and maintained for 6-8 weeks (15).
The radiographic controls were performed in the immediate post-operative period, at 1 and 3 months, then every 3 months until consolidation.
All patients were checked using the Harris Hip Score to study pain, autonomy of walking, independence in carrying out daily activities and ROM.
For 6 cases, the last ones execute we only have radiographic control at one month.
The consolidation of peri-prosthetic fractures occurred in all the controlled patients (42 out of 52) at a distance of about 3 months on average (24 months) from the intervention.
The radiographic controls at one year appear to be completely satisfactory.
The ROM appeared complete on all planes in the 8 patients who completed the follow-up at 36 months and in 14 patients of those who completed the follow-up at 24 months.
For all the others, it was possible to check the articularity of the operated hip, but it seemed satisfactory at 12 months.
The HHS of the 2-year controlled patients is on average over 90 (92) “Excellent”, for those controlled at 1 year it is just below 90 (89) “Good”.
8 patients, 1 year after surgery, complained of walking pain.
Regarding the independence in the performance of daily activities, the general conditions and the age of the controlled patients must be taken into account.
Only some, “the youngest” were able to spontaneously fulfill all the daily functions. In fact, we believe that HHS is a complete and valid objective test to have homogeneous data, but that lends itself to even severe criticisms by not taking into account co-morbidities and associated pathologies (Figures 6 and 7).
Figure 6.

Men, 93 y., ASA 4. a) fracture type B2; b) post-operatory X-ray: NCB plate without reimplantation
Figure 7.
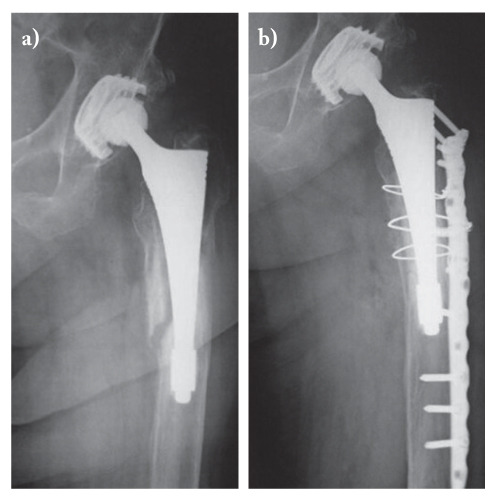
Woman, 90 y., ASA 3. a) fracture type B2; b) post-operatory X-ray: NCB plate without reimplantation
Discussion
One aim of this work was to evaluate if the consolidation time of the peri-prosthetic femoral fractures treated with NCB plates is superimposable to that required by a first in patients of the same age.
According to our experience, the functional recovery is a function of age and general conditions and the recovery after a first femoral fracture is superimposable to that after a peri-prosthetic fracture treated with NCB plates. Consolidation times in the presence or absence of a prosthetic implant are saturated overlapping.
The presence or absence of cement inside the femoral canal in patients with peri-prosthetic femoral fracture did not have significant significance both during the execution of the operation, both in the post-operative period and during consolidation.
It was very important to be able to use an instrument that guaranteed the possibility of perforating the peri-prosthetic cement and anchoring the screws both in the plaque and in the two femoral cortices (medial to lateral) even in the presence of interposed cement.
The ease of execution of the osteosynthesis and the consequent reduced time of execution of the intervention is of particular importance in large elderly patients affected by pluripathologies; the duration of the intervention and the consequent reduced bleeding certainly lead to early mobilization and functional recovery.
NCB plates, compared to the means of synthesis used in the past, are technologically innovative tools, much more resistant, conceptually better, and easier to apply in the operating field. Their flexibility helps to solve practically all the technical problems that are typical of their osteosynthesis (5, 10, 12).
Conclusions
In our opinion it was important to verify the correspondence between the radiographic classification and the clinical classification, even if the Vancouver classification does not consider the patient’s clinic, although leaving the final therapeutic decision to the intraoperative picture.
We consider the synthesis valid, without the need to re-implant the prosthetic femoral stem, in all B1 and C fractures, taking into account the patient’s age, co-morbidities and ASA risk. Exploiting the ductility of the NCB plates we performed an osteosynthesis also in some type B2 fractures (3 cases) in order to reduce the surgical time and the perioperative bleeding, obtaining good stability of the fracture and of the prosthetic implant; these were large elderly patients, with very high operative risk, short life expectancy and sometimes limited functional needs, with only the aim of an early mobilization aimed at disallowing, in the absence of pain.
For B3 fractures, the revision of the prosthetic stem with bone graft is indispensable.
The learning curve in the use of NCB plates, in an experienced surgeon, is very fast, the instruments are simple and complete. In the planning of osteosynthesis interventions of peri-prosthetic hip fractures, we always keep a prosthetic revision device available in the operating room.
After treating patients with ASA Score of 3 or 4, then with a very serious compromise of the general conditions and observed consolidations even at 3 months, we can firmly affirm the validity of the method.
The therapeutic choice therefore always depends on the preoperative radiographic picture, on the intra-operative finding, on the type of patient and, last but not least, on the experience of the surgeon.
Conflict of interest:
Each author declares that he or she has no commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangement etc.) that might pose a conflict of interest in connection with the submitted article
References
- 1.Duwelius PJ, Schmidt AH, Kyle RF, Talbott V, Ellis TJ, Butler JBV. A prospective, modernized treatment protocol for periprosthetic femur fractures. Orthop. Clin. N. Am. 2004;35:485–492. doi: 10.1016/j.ocl.2004.05.001. [DOI] [PubMed] [Google Scholar]
- 2.Tsaridis E, Haddad FS, Gie GA. The management of periprosthetic femoral fractures around hip replacement. Injury. 2003;34:95–105. doi: 10.1016/s0020-1383(02)00257-7. [DOI] [PubMed] [Google Scholar]
- 3.Calvosa G, Bonicoli E, Tenucci M, Morescalchi G, Po F. Le fratture periprotesiche di femore dopo una protesi totale d’anca. GIOT. 2004;30:100–4. [Google Scholar]
- 4.Pike J, Davidson D, Garbuz D, Duncan CP, O’Brien PJ, Masri BA. Principles of treatment for periprosthetic femoral shaft fractures around well-fixed total hip arthroplasty. J Am Acad Orthop Surg. 2009;17:677–688. doi: 10.5435/00124635-200911000-00002. [DOI] [PubMed] [Google Scholar]
- 5.Peyrani A, Mellano D, Negretto R. Le fratture periprotesiche in pazienti portatori di protesi totale di anca. GIOT. 2013;39:62–66. [Google Scholar]
- 6.Biggi F, Di Fabio S, D’Antimo C, Trevisani S. Periprosthetic fractures of the femur: the stability of the implant dictates the type of treatment. J. Orthop. Traumatol. 2010;11:1–5. doi: 10.1007/s10195-010-0085-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lindhal H, Malchau H, Odèn A, Garellick G. Risk factors for failure after treatment of a periprosthetic fracture of the femur. J. Bone Joint Surg Br. 2006;88:26–30. doi: 10.1302/0301-620X.88B1.17029. [DOI] [PubMed] [Google Scholar]
- 8.Holley K, Zelken J, Padgett D, Yun A, Buly R. Periprosthetic fractures of the femur after hip arthroplasty: an analysis of 99 patients. HSS J. 2007;3:190–7. doi: 10.1007/s11420-007-9045-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Capone A, Ennas F, Podda D. Periprosthetic femoral fractures: risk factors and current options to treatment. Aging Clin. Exp. Res. 2011;23(Suppl. 2):33–5. [PubMed] [Google Scholar]
- 10.Erhardt JB, Grob K, Roderer G, Hoffmann A, Forster TN, Kuster MS. Treatment of periprosthetic femur fractures with the non-contact bridging plate: a new angular stable implant”. Arch Orthop Trauma Surgery. 2008;128:409–16. doi: 10.1007/s00402-007-0396-6. [DOI] [PubMed] [Google Scholar]
- 11.Park SK, Kim YG, Kim SY. Treatment of periprosthetic femoral fractures in hip arthoplasty. Clin Orthop Surg. 2011;3:101–6. doi: 10.4055/cios.2011.3.2.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kampshoff J, Stoffel KK, Yates PJ, Erhardt JB, Kuster MS. The treatment of periprosthetic fractures with locking plates: effect of drill and screw type on cement mantles: a biomechanical analysis. Arch Orthop Trauma Surgery. 2010;130:627–32. doi: 10.1007/s00402-009-0952-3. [DOI] [PubMed] [Google Scholar]
- 13.Berlusconi M, Accetta R, Pascale V, Pagani A, Mineo G. Locking compression plates (LCP) for the treatment of periprosthetic fractures of the hip. J. Orthop. Trauma. 2004;18(suppl. 9):20–21. [Google Scholar]
- 14.Marsland D, Mears SC. A Review of periprosthetic fractures associated with total hip arthoplasty. Geriatr. Orthop. Surg. Rehabil. 2012;3:107–120. doi: 10.1177/2151458512462870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Briant-Evans TW, Veeramootoo D, Tsiridis E, Hubble JW. Cement in cement stem revision for Vancouver Type B periprosthetic femoral fractures after total hip arthrplasty. Acta Orthop. 2009;80:584–52. doi: 10.3109/17453670903316827. [DOI] [PMC free article] [PubMed] [Google Scholar]


