Abstract
Since February 21st, 2020 CoVID-19 spread throughout all Italy expanding like a “tsunami” from Codogno (Lodi, Lombardy, Northern Italy) to neighboring cities. In a few days Lodi, Piacenza, Milano, Brescia and Bergamo were forced to deal with this disaster starting the lockdown at different time. No national plan had been prepared. As result, CoVID-19 has paralyzed the Italian healthcare system. At time of writing, in Italy there are 169 323 infected patients and 22 260 deaths. Italy is fighting hard to manage CoVID-19 crisis even if most hospitals were unprepared to deal with massive influx of critically ill CoVID-19 patients. Piacenza in Emilia-Romagna region (Northern Italy) is one of the epicenters of the Italian pandemic, and the local hospital – Guglielmo da Saliceto – has quickly become a “CoVID-19 hospital” with the great effort of all the medical staff. Here we report the experience of our hospital, particularly the strategy adopted in the Orthopedics and Traumatology Department. (www.actabiomedica.it)
Keywords: CoVID-19, Orthopedics, Traumatology, Italian epidemic, emergency medicine, CoVID-19 pandemic, disaster management
Introduction
Since the end of February, 2020 the words “coronavirus” and “CoVID-19” has become routinely used by Italian people because of the rapid spread of the novel coronavirus and the dramatic impact on Italy in terms of infected patients, overcrowding in hospitals and the high number of deaths.
The 2019 novel coronavirus (2019 n-CoV) has been identified in Wuhan, Hubei Province, China, in December 2019, in patients affected by viral pneumonia (1). It rapidly spread across China and all over the world causing a global health crisis. On January 12nd, 2020 the World Health Organization (WHO) named this novel infection as CoVID-19 (coronavirus disease), and on January 30th, 2020 the WHO declared CoVID-19 as the sixth public health emergency of international concern.
The most common symptoms of CoVID-19 infection are dry cough and fever, which can turn into interstitial pneumonia with progression to acute respiratory distress syndrome (ARDS) and end-organ failure (2). ARDS is the main cause of death and must be treated promptly and appropriately (3). Hyper-inflammatory reaction and microvascular pulmonary thrombosis seem to be the cause of multiorgan failure and death in CoVID-19 patients (4).
Since February 21st, 2020 CoVID-19 spread throughout all Italy expanding like a “tsunami” from Codogno (Lodi, Lombardy, Northern Italy) to neighboring cities (Table 1). In a few days Lodi, Piacenza, Milano, Brescia and Bergamo were forced to deal with this disaster starting the lockdown at different time. No national plan had been prepared (5). As result, CoVID-19 has paralyzed the Italian healthcare system. At time of writing, in Italy there are 169 323 infected patients and 22 260 deaths. Italy is fighting hard to manage CoVID-19 crisis even if most hospitals were unprepared to deal with massive influx of critically ill CoVID-19 patients. Piacenza in Emilia-Romagna region (Northern Italy) is one of the epicenters of the Italian pandemic, and the local hospital – “Guglielmo da Saliceto” – has quickly become a “CoVID-19 hospital” with the great effort of all the medical staff.
Table 1.
COVID 19: National casuistry (official data from Italian Civil Protection).
 |
The exponential daily growth of CoVID-19 ill patients and the local outbreak required a rapid and strong stance of the Medical Direction to manage the emergency and to avoid the complete collapse of our local health system (6).
Here we report the experience of our hospital in the epidemic phase and the changes needed to develop “a survival strategy”. Particularly, we will focus the attention on the Orthopedics and Traumatology Department of “Guglielmo da Saliceto” Hospital.
Results
For its proximity to Codogno, the hospital of Piacenza has been quickly and suddenly overcrowded by a massive flux of critically ill CoVID-19 patients firstly coming from Lombardy, but in a few days from Piacenza and nearby provinces. “Guglielmo da Saliceto” is the main hospital with a hub-and-spoke organization, a Radiology Department and an Intensive Care Unit (ICU) for all the inhabitants of Piacenza and the surrounding four valleys - Val Nure, Val d’Arda, Val Tidone, Val Trebbia (for a total of 287172 inhabitants at 2019). As result, the sudden and massive wave of CoVID-19 patients in such a short time of period has paralyzed our health system and hospital organization. It was soon clear that we needed to develop a long-term plan to avoid the complete collapse of our hospital. On Sunday 23rd February 2020 all the heads of the hospital departments have been gathered to define together a plan against CoVID-19 outbreak. While writing, we have 2516 CoVID-19 cases, 1414 out of them needed hospital admission for acute respiratory failure and 210 were admitted to ICU.
The overcrowding of our ED, the limited human resources and the poor technical skills to deal with the CoVID-19 epidemic have required a great effort to maintain the normal standard of care for each patient. For this reason, we quickly modified several times the hospital organization increasing the number of emergency clinicians thanks to the help of the EDs of “Castel San Giovanni” and “Fiorenzuola d’Arda” Hospitals, moving away the Orthopedics and Traumatology Department in another local building in Piacenza – “Casa di Cura Piacenza”-, and designing a disaster plan.
All the planned activities were stopped, the ICU tripled its beds from 15 to 45, and the hospital has been converted into a “CoVID-19 hospital” with 80% of beds for ill CoVID-19 patients. Immediately the Emergency Department (ED) created a strategy to discriminate CoVID-19 and no CoVID-19 patients at admission in order to limit CoVID-19 spread (7).
The Emergency Room was divided in six CoVID-19 areas according to different grades of respiratory failure (50 beds), and Observation Unit was turned into a Sub-intensive Care Unit for patients with ARDS who needed CPAP/NIV (13 beds). A “temporary CoVID-19 ward” of 40 beds with an extra medical team of 2 clinicians and 2 non-expert nurses to manage the high number of recovered patients was created for patients who were waiting for admission to two CoVID-19 hospitals located in Castel San Giovanni (128 beds) and Fiorenzuola d’Arda (61 beds), and the Military Hospital, set up in Piacenza for CoVID-19 disaster (40 beds). A “free CoVID-19 first aid station” (Advanced Medical Facility) has been arranged outside the hospital, in front of the entry of the ED, to ensure a “free CoVID-19 way”. Two bed managers handled all the patients’ hospitalization and transfer 7/7 days and 12/24 hours (8 a.m. – 8 p.m). All the areas, including the Advanced Medical Facility, had an ultrasound workstation to perform point-of-care lung US (8) and a dedicated medical staff made by an emergency clinician and 1 or 2 expert nurses.
In the respect of human being and in absence of the family affection we hospitalized all the terminal patients in a dedicated CoVID-19 palliative care ward, made by 12 beds powered by a team of palliative care specialists and surgeons.
We want to point the attention on the Orthopedics and Traumatology Department, because of the strong impact of CoVID-19 due the fact that the PPE (Personal Protective Equipment) was available later than 21st February (Figure 1 and 2) (9). The medical staff of the Orthopedics and Traumatology Unit is made by 14 orthopedists, 5 general practitioners and 2 geriatrics. The available beds are usually 47, twelve of them are for prosthetic surgery (hip, knee and shoulder). Two operating rooms (one for the traumatology team) are active 12 hours a day (8 a.m. - 8 p.m.). The orthopedic emergency service is available 24/24 hours 7/7 days. Three out-patient clinics manage one hundred patients a day both for orthopedic and traumatological problems. At the beginning of the epidemic phase, seven orthopaedic surgeons had become ill causing a significant reduction of the medical staff. Six developed CoVID-19 infection with a good response to treatment. Three of them were on shift in the Emergency Room at the beginning of our local outbreak and none was confident with the right use of PPE. All the diagnoses have been confirmed by Real Time-Polymerase Chain Reaction for 2019-nCoV from the nasopharyngeal swab.
Figure 1.

General protection.
Figure 2.

Personal Protective Equipment (PPE).
All the colleagues have been treated at home with hydroxychloroquine and antiviral therapy (10) with good response and complete remission in three weeks. Only in one case, low molecular weight heparin (LMWH) at anticoagulant dose has been used.
Unfortunately, on March 22nd one of our young colleagues has been hospitalized for ARDS (Figure 3) and he is still intubated in a critical condition in the Intensive Care Unit of another hospital. In addition, the two geriatrics resulted positive for 2019-nCoV by Real Time-Polymerase Chain Reaction from the nasopharyngeal swab, and they have been quarantined too.
Figure 3.
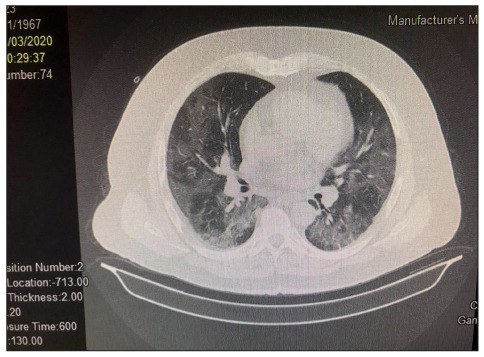
CT scan findings of our colleague with severe interstitial pneumonia, intubated in critical condition in the Intensive Care Unit.
In our Department 37.5% of nursing staff had have a positive nasopharyngeal swab. Most of them had complained of flu-like symptoms and none had needed to be hospitalized. Only one female nurse affected by several comorbidities died for CoVID-19 pneumonia.
The increasing number of CoVID-19 patients admitted to our ED and ICU, and the dramatic reduction of our medical staff forced our Department to adopt a “defensive strategy”, which can be summarized in two steps. First of all, on Monday 24th February all the activities were stopped; and second, on 13rd March all the Department was transferred to another local building “Casa di Cura di Piacenza” to create another new “CoVID-19 ward” in the hospital powered by cardiologists, surgeons, otorhinolaryngologists and urologists.
As consequence, we have reduced our agenda: we stopped all the planned surgical activities (7 operating rooms) in order to increase the number of intensivists available for the CoVID-19 emergency, and we reduced of 50% the activity of the out-patient clinic.
Unfortunately, the director of our Department developed fever and dyspnea on March 17th. High resolution chest CT scan and nasopharyngeal swab confirmed the diagnosis of CoVID-19 pneumonia (Figure 4). Chest CT scan is considered the gold standard technique for the diagnosis and assessment of lung involvement in CoVID-19 pneumonia (11,12). The typical radiological findings are ground glass opacity, crazy-paving pattern and consolidation with the greatest severity approximately 10 days after the onset of symptoms (13). CT scan can depict the extent of lung involvement in CoVID-19 pneumonia. Data from a recent retrospective study in patients admitted to our ED for COVID-19 respiratory failure show that visual and software-based quantification of the well aerated lung on chest CT are predictors of ICU admission or death in CoVID-19 patients. In particular, the reduction of 70% well aerated lung parenchyma is a negative prognostic factor independent of clinical and demographic parameters, including inflammatory markers such as C-reactive protein (14).
Figure 4.
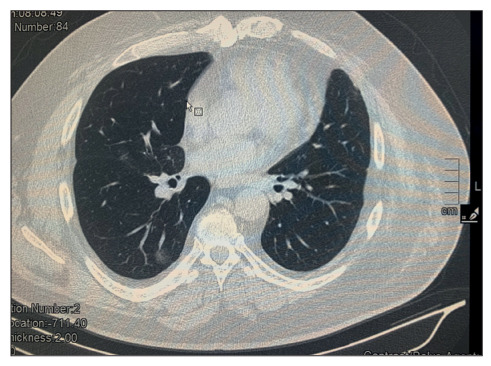
CT scan findings of paucisymptomatic patient.
We decided to leave only one orthopedist, available from 8 a.m. to 7 p.m. in the “Guglielmo da Saliceto” Hospital with these main aims: - consulting for hospitalized CoVID-19 patients and for all the patients admitted to the ED – CoVID-19 or not CoVID-19; - recovering and discharging of patients with traumatological diseases. In case of traumatological emergency, the “Emergency operating room” was always available.
We planned our activities in the “Casa di Cura Piacenza” as follows:
- in-patient clinic: 25 beds powered by expert nurses and medical staff, 7/7 days, 24/24 hours.
- Out-patient clinic: from 8 a.m. to 7 p.m., one patient every 20 minutes to avoid overcrowding. Before being admitted to the visit, all the patient needed to fill out an easy and quick questionnaire based on clinical and epidemiological criteria, and to check body temperature.
- Orthopedic emergency service: 7/7 days, 24/24 hours. All the patients were firstly evaluated in a “triage area” and in case of flu-like symptoms (clinical data) or epidemiological criteria, they were transferred to the ED in the “Guglielmo da Saliceto” Hospital.
- Surgical activity: one operating room from 8 a.m. to 4 p.m., from Monday to Friday, always available for traumatological emergencies (24/24 hours, 7/7 days).
The changes adopted by our Department have been paramount to create “space” in our hospital for dedicated CoVID-19 wards, and to help emergency clinicians and intensivists to manage such a disaster.
Surely, the national lockdown has contributed to limit traumatological problems. From 25th February to 31st March 2020, we have observed a significant reduction in traumatological diseases: from 281 (139 orthopedic problems and 142 traumatological diseases) to 96 (all traumatological patients, 52 out of them admitted to our hospital before 13rd March, and 39 to “Casa di Cura Piacenza”). Since 14th March 2020 we have had only 5 emergencies in CoVID-19 patients, all treated in the local hospital. Overall, we have treated 96 fractures in March 2020, down to 23.2% compared to March 2019 (125). In particular as regard fractures in older people (15,16,17,18,19), we have observed 41 fractures of the femur (down to 16.33%, 49 in March 2019) (Figure 5), 2 humeral head breaks (down to 75%, 8 in March 2019) (Figure 6), and 3 wrist fractures (down to 50%, 6 in March 2020) (Figure 7).
Figure 5.

X-Ray femur fracture.
Figure 6.

X-Ray homer fracture.
Figure 7.

X-Ray wrist fracture.
In the out-patient clinic we have drastically reduced the number of visits: from 100 until 21st February, to 30 since 13rd March, and we decided to extend the time between two successive visits to avoid the spread of CoVID-19 due to potential asymptomatic carriers.
From 7th to 21st April 2020, 2730/3720 (73.4%) hospital employees have been tested with immunochromatography for n-CoV19. Among them, 2152 (78.8%) were negative for IgG, and 2145 (78.5%) for IgM. Rapid test (chromatography) resulted positive in 578 cases; 453 (78.3%) out of them were confirmed positive for IgG (serum) too. One hundred and twenty-eight cases resulted positive both for IgM and IgG at the rapid Kit: 125 (97.6%) out of them have been confirmed IgG positive, and 107 (83.5%) IgM positive (positive threshold value >= 10 AU/mL).
In our Department only the seven CoVID-19 orthopedics have been found immunized.
On 9th April 2020, the General Director of our hospital called a “skype” meeting to discuss together with all the heads of the Departments, the general situation and plan a new strategy in the so-called phase 2 of the CoVID-19 epidemic.
We think that the significative reduction of the number of CoVID-19 patients admitted to the ED and particularly, those with acute respiratory failure, observed in the last two weeks, can be the result of several factors, such as: the Italian lockdown and the activation of a local healthcare system thanks to the great intuition by Dr. Luigi Cavanna.
Based on the observation that the ED has been overcrowded with CoVID-19 infected people already in serious condition and all these patient had a story of days or weeks spent at this home with flu-like symptoms and exertional dyspnea at first, then dyspnea at rest with urgent hospitalization for acute respiratory failure, dr Cavanna designed a plan to dramatically reduce admission to ED. Since the treatment of patients admitted to the Piacenza hospital was based on hydroxychloroquine tablets 400 mg daily plus darunavir and cobicistat 800/150 daily for seven days, dr Cavanna and his medical staff choose to treat early at home CoVID-19 patients at the onset of symptoms to avoid a rapid progressive worsening of the infection (20).
Discussion and Conclusion
The clinical spectrum of CoVID-19 infection can vary from asymptomatic forms to flu-like symptoms and interstitial pneumonia with different lung damage and the development of ARDS. Some patients can complain of anosmia and dysgeusia (21). ARDS is the main cause of death (22).
Piacenza is a small city with many inhabitants of advanced age, surrounded by four valleys al Nure, Val d’Arda, Val Tidone, Val Trebbia - for a total of 287172 inhabitants at 2019. Piacenza has quickly become one of the epicenters of the Italian epidemic for its proximity to Codogno, where the first case of CoVID-19 has been identified. The “Guglielmo da Saliceto” Hospital has struggled to deliver regular services, but in a few days, it changed its perspectives to avoid the complete collapse of its health system. A plan against CoVID-19 epidemic has been designed thank to the collaboration of all the Departments. The great flexibility and cooperation of all the medical and nursing staff of our hospital is the real key of the success of our strategy.
Based on this evidence and the overcrowding of our ED and ICU, we decided to stop all the planned orthopedic surgery and to move to another building in Piacenza, “Casa di Cura Piacenza”. This choice has allowed to create a new dedicated CoVID-19 ward in our hospital. Surely, the national quarantine since March 10th has contributed to reduce the incidence of traumatological diseases. Surprisingly, we observed a reduction of typical bone fractures in old people, who generally occurred at home. We believe that a gradual resumption of all the activities is necessary but with a tailored strategy for every Department. A long-term plan is necessary to keep the system operational and to be ready for a possible second wave of the “tsunami”. For this reason, the Orthopedics and Traumatological Department will be split into two units until the complete resolution of the Italian pandemic: the traumatological surgery and the emergency room in the “Guglielmo da Saliceto” Hospital, the out-patient clinic and the orthopedic surgery in “Casa di Cura Piacenza” (25 beds). In addition, we will create specific routes designed to be prepared for a future pandemic and based on this dramatic experience. At time of writing, we are living the so-called phase 2 of CoVID-19 pandemic and we have just rearranged our organization, confirming the common idea that CoVID-19 is a real challenge for all the EDs (Table 2).
Table 2.
COVID 19: emergency department access.
 |
We strongly believe that we have to learn a clear lesson from what happened in the world and in Italy particularly, just one month ago. We need to be prepared for a possible “second wave” of this “tsunami”, but certainly, we need to have a long-term plan for the next pandemic based on the evidence that we live in a globalized world with globalized diseases.
Acknowledgements
All the authors wish to thank all the staff of the “Guglielmo da Saliceto” Hospital for their strength, energy and resiliency to face and manage such a difficult public health crisis. The authors are in debt with Davide Colombi, Luca Baldino, Guido Pedrazzini, Flavio Santilli, Maria Gamberini, Vincenzo Nardacchione, Mirella Gubbelini, Andrea Vercelli, Matteo Silva, Valeria Burgio, Ivo Monica, Giuseppe Leddi, Mattia Pugliese, Simona Montani, Giorgia Balogh, Alessandra Magro, Valentina Salotti, Laura Ghidoni, Elena Belli, Cosimo Franco, Emanuele Michieletti, Giampietro Scaglione, Franco Pugliese, Daniele Vallisa, Massimo Nolli, Marco Stabile, Giovanni Quinto Villani, Daniela Aschieri, Roberta Schiavo, Mauro Codeluppi, Davide Imberti, Gian Piero Gregori, Caterina Fiazza, Simonetta Radici, Francesca Carini, Donata Guidetti, Fabio Mozzarelli, Massimiliano Mazzilli, Gaetano Maria Cattaneo & Filippo Banchini for their high levels of involvement, commitment, responsibility, accountability, adaptability, flexibility, care, and dedication to work.
References
- 1.Lu H, et al. Oubreak of pneumonia of unkwown etiology in Wuhan China: the mistery and the miracle. J Med Virol. 2020 doi: 10.1002/jmv.25678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gorbalenya AE, et al. Severe acute respiratory syndrome-related coronavirus: the species and its viruses – a statement of the Coronavirus Study Group. BioRxiv. 2020, Feb 11 [Google Scholar]
- 3.Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gattinoni L, et al. COVID-19 pneumonia: ARDS or not? Critical care. 2020;24:154. doi: 10.1186/s13054-020-02880-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ciceri F, et al. Critical care and Resuscitation. 2020 Epub ahead of print. [Google Scholar]
- 6.Grasselli G, Pesenti A, Cecconi M. Critical Care Utilization for the COVID-19 Outbreak in Lombardy, Italy: Early Experience and Forecast During an Emergency Response. JAMA. Published online March 13, 2020 doi: 10.1001/jama.2020.4031. doi:10.1001/jama.2020.4031. [DOI] [PubMed] [Google Scholar]
- 7.Murthy S, Gomersall CD, Fowler RA. Care for Critically Ill Patients With COVID-19. JAMA. Published online March 11, 2020 doi: 10.1001/jama.2020.3633. doi:10.1001/jama.2020.3633. [DOI] [PubMed] [Google Scholar]
- 8.Poggiali , et al. Triage-decision making at the time of COVID-19 infection: the Piacenza strategy. Internal and Emergency Medicine. doi: 10.1007/s11739-020-02350-y. accepted 16 April. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Poggiali E, Dacrema A, Bastoni D, et al. Can Lung US Help Critical Care Clinicians in the Early Diagnosis of Novel Coronavirus (COVID-19) Pneumonia? Radiology. 2020 doi: 10.1148/radiol.2020200847. (Epub ahead of print) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhai P, Ding Y, Wu X, Long J, Zhong Y, Li Y. The epidemiology, diagnosis and treatment of COVID-19. Int J Antimicrob Agents. 2020 Mar 28:105955. doi: 10.1016/j.ijantimicag.2020.105955. doi: 10.1016/j.ijantimicag.2020.105955. (Epub ahead of print) PubMed PMID: 32234468; PubMed Central PMCID: PMC7138178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Arnold SL, Buckner F. Hydroxychloroquine for treatment of SARS-CoV-2 infection? Improving our confidence in a model-based approach to dose selection. Clin Transl Sci. 2020 Apr 8 doi: 10.1111/cts.12797. doi: 10.1111/cts.12797. (Epub ahead of print) PubMed PMID: 32268005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Thachil J. The versatile heparin in COVID-19. J Thromb Haemost. 2020 Apr 2 doi: 10.1111/jth.14821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Carr J. The anti-inflammatory action of heparin: heparin as an antagonist to histamine, bradykinin, and prostaglandin E1. Thromb Res. 1979;16:507–516. doi: 10.1016/0049-3848(79)90097-5. [DOI] [PubMed] [Google Scholar]
- 14.Ning Tang 1, Dengju Li 2, Xiong Wang 1, Ziyong Sun1. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost. 2020;00:1–4. doi: 10.1111/jth.14768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chuan Qin, Luoqi Zhou, Ziwei Hu, et al. Dysregulatiopn of immune response in patients with COVID-19 in Wuhan, China. Clinical Infectious Disease. 2020, March 13 pii: ciaa248. doi: 10.1093/cid/ciaa248. (Epub ahead of print) [Google Scholar]
- 16.Simpson S, Kay FU, Abbara S, Bhalla S, Chung JH, Chung M, Henry TS, Kanne JP, Kligerman S, Ko JP, Litt H. Radiological Society of North America Expert Consensus Statement on Reporting Chest CT Findings Related to COVID-19. Endorsed by the Society of Thoracic Radiology, the American College of Radiology, and RSNA. Radiology. 2020 doi: 10.1097/RTI.0000000000000524. (in press). doi: 10.1148/ryct.2020200152. Accessed April 4, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sverzellati N, Milanese G, Milone F, Balbi M, Ledda RE, Silva M. Integrated Radiologic Algorithm for COVID-19 Pandemic. J Thorac Imaging. 2020 Apr 7 doi: 10.1097/RTI.0000000000000516. doi: 10.1097/RTI.0000000000000516. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Feng P, Tianhe Y, Peng S, Shan G, Bo L, Lingli L, Dandan Z, Jiazheng W, Richard LH, Lian Y, Chuansheng Z. The course of lung changes on chest CT during recovery from 2019 novel coronavirus (COVID-19) Pneumonia. Radiology. 2020 doi: 10.1148/radiol.2020200370. [Google Scholar]
- 19.Colombi D, Bodini FC, Petrini M, Maffi G, Morelli N, Milanese G, Silva M, Sverzellati N, Michieletti E. Well-aerated Lung on Admitting Chest CT to Predict Adverse Outcome in COVID-19 Pneumonia. Radiology. 2020 Apr 17:201433. doi: 10.1148/radiol.2020201433. doi: 10.1148/radiol.2020201433. Epub ahead of print. PMID: 32301647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Caforio M, Maniscalco P, Colombo M, Calori GM. Long endomedullary nail in proximal third humeral shaft fractures. Injury. 2016 Oct;47(Suppl 4):S64–S70. doi: 10.1016/j.injury.2016.07.037. doi: 10.1016/j.injury.2016.07.037. Epub 2016 Aug 6. PubMed PMID: 27507546. [DOI] [PubMed] [Google Scholar]
- 21.Ruffilli A, Traina F, Pilla F, et al. Marchetti Vincenzi elastic retrograde nail in the treatment of humeral shaft fractures: review of the current literature. Musckoloskelet Surg. 2015 Dec;99(3):201–9. doi: 10.1007/s12306-015-0387-7. [DOI] [PubMed] [Google Scholar]
- 22.Rivera F, Leonardi F, Maniscalco P, Caforio M, Capelli R, Molinari G, Esopi P. Uncemented fully hydroxyapatite-coated hip stem for intracapsular femoral neck fractures in osteoporotic elderly patients: a multicenter study. Arthroplast Today. 2015 Aug 28;1(3):81–84. doi: 10.1016/j.artd.2015.02.002. doi: 10.1016/j.artd.2015.02.002. eCollection 2015 Sep. PubMed PMID: 28326377; PubMed Central PMCID: PMC4956684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rebuzzi E, Pannone A, Schiavetti S, et al. IMHS clinical experience in the treatment of peritrochanteric fractures. The results of a multicentric Italian study of 981 cases. Injury. 2002 Jun;33(5):407–12. doi: 10.1016/s0020-1383(02)00070-0. [DOI] [PubMed] [Google Scholar]
- 24.Maniscalco P, Benazzo F, Ruggieri P, Di Maggio B. CIO: 360° in trauma care. Injury. 2019 Aug;50(Suppl 4):S1. doi: 10.1016/j.injury.2019.08.008. [DOI] [PubMed] [Google Scholar]
- 25.Li Z, Yi Y, Luo X, Xiong N, Liu Y, Li S, Sun R, Wang Y, Hu B, Chen W, Zhang Y, Wang J, Huang B, Lin Y, Yang J, Cai W, Wang X, Cheng J, Chen Z, Sun K, Pan W, Zhan Z, Chen L, Ye F. Development and Clinical Application of A Rapid IgM-IgG Combined Antibody Test for SARS-CoV-2 Infection Diagnosis. J Med Virol. 2020 Feb 27 doi: 10.1002/jmv.25727. doi: 10.1002/jmv.25727. (Epub ahead of print) PubMed PMID: 32104917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Berardi F. The Italian Doctor Flattening the Curve by Treating COVID-19 Patients in Their Homes. Time. April 9, 2020 [Google Scholar]
- 27.No Authors Signed The Country Won’t Work Without Them. 12 Stories of People Putting Their Lives on the Line to Help Others During Coronavirus. Time. April 9, 2020 [Google Scholar]
- 28.Noel Lorenzo Villalba, Yasmine Maouche, Maria Belen Alonso Ortiz, Zaida Cordoba Sosa, Jean Baptiste Chahbazian, Aneska Syrovatkova, Pierre Pertoldi, Emmanuel Andres, Abrar-Ahmad Zulfiqar. Anosmia and Dysgeusia in the Absence of Other Respiratory Diseases: Should COVID-19 Infection Be Considered? EJCRIM. 2020 doi: 10.12890/2020_001641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]


