Abstract
Objectives
To evaluate the cost, accessibility and patient satisfaction implications of two clinical pathways used in the management of chronic headache.
Intervention
Management of chronic headache following referral from Primary Care that differed in the first appointment, either a Neurology appointment or an MRI brain scan.
Design and setting
A pragmatic, non-randomised, prospective, single-centre study at a Central Hospital in London.
Participants
Adult patients with chronic headache referred from primary to secondary care.
Primary and secondary outcome measures
Participants’ use of healthcare services and costs were estimated using primary and secondary care databases and questionnaires quarterly up to 12 months postrecruitment. Cost analyses were compared using generalised linear models. Secondary outcomes assessed: access to care, patient satisfaction, headache burden and self-perceived quality of life using headache-specific (Migraine Disability Assessment Scale and Headache Impact Test) and a generic questionnaire (5-level EQ-5D).
Results
Mean (SD) cost up to 6 months postrecruitment per participant was £578 (£420) for the Neurology group (n=128) and £245 (£172) for the MRI group (n=95), leading to an estimated mean cost difference of £333 (95% CI £253 to £413, p<0.001). The mean cost difference at 12 months increased to £518 (95% CI £401 to £637, p<0.001). When adjusted for baseline and follow-up imbalances between groups, this remained statistically significant. The utilisation of brain MRI improved access to care compared with the Neurology group (p<0.001). Participants in the Neurology group reported higher levels of satisfaction associated with the pathway and led to greater change in care management.
Conclusion
Direct referral to brain MRI from Primary Care led to cost-savings and quicker access to care but lower satisfaction levels when compared with referral to Neurology services. Further research into the use of brain MRI for a subset of patient population more likely to be reassured by a negative brain scan should be considered.
Trial registration number
Keywords: chronic headache, migraine, direct access, magnetic resonance imaging, cost analysis
Strengths and limitations of this study.
The estimate of healthcare resource use was based on comprehensive and complete data retrieved from hospital databases supplemented by both primary care utilisation data and self-reported participant data.
The evaluation of the intervention’s impact considered different dimensions of analysis (efficiency, quality of care, access to care and patient satisfaction).
This was a single-centre study with participants recruited from one central hospital in London, therefore a multicentre study would be necessary to explore the generalisability of the results.
Introduction
Globally, the percentage of the adult population with an active headache disorder is 47% for episodic headache and 3% for chronic headache (lasting more than 15 days per month).1 Headache is in the top 10 international causes of disability,2 with nearly half of sufferers reporting it affects work, home or social activities.3–5 Most headaches are primary headache disorders, such as migraine or tension-type headaches. Secondary headaches, due to an underlying serious pathology (eg, tumour, brain aneurysm) are far less common.6 In fact, less than 0.1% of the lifetime headache prevalence is associated with a life-threatening condition, which can include primary or secondary brain tumours.2 3
Most headache sufferers self-manage, but over 4% of adults each year consult their general practitioner (GP).7 8 GPs manage 97% of headache presentations, particularly GPs with special interest and training in headache training initiatives,9 with 2% of these referred to neurologists and 1% to other specialists.7 Headache is the most common cause for GP referrals to neurologists accounting for up to 20%–30%,10–13 the vast majority of these are for migraine. Chronic migraine sufferers (>15 days/month) had more emergency department (ED)/hospital visits, and diagnostic tests than those with episodic migraine and consequently, the medical costs were three times higher.14 Hence, despite the benign nature of most headaches, headache management is associated with high healthcare utilisation. Furthermore, a study in multiple countries of the European Union found that headache management was variable in terms of visits with GPs and specialists and medication use.15 Between 2012 and 2014, patients presenting to headache specialists (either neurologists or GPs with a special interest in headache) costed £956 million in the UK.13 16
GP direct access to imaging has been defined as a priority within the National Health Service (NHS), with direct access to brain MRI for the diagnosis of brain cancer identified as a specific initiative.8 GPs have reported referrals for secondary care, both for a neurologist consultation or neuroimaging, when they were unable to reassure the patient.17 18 Furthermore, Morgan et al found that referral for headache is often the outcome of patient pressure and anxiety interacting with GP characteristics, organisational factors and service availability rather than the headache severity itself.17 This contrasts with the recommendations from the National Institute for Health and Care Excellence that does not recommend the use of neuroimaging for reassurance purposes.19 A US study estimated that patients with new onset migraine headache or a flare-up of chronic headache had, respectively, a 39% (95% CI 24% to 54%) and 51% (95% CI 32% to 68%) probability of having neuroimaging routinely ordered even where guidelines specifically recommended against this approach.20 A UK-based randomised controlled trial evaluated the cost implications of using brain MRI for reassurance purposes and found that it led to a decrease in healthcare costs, in particular for patients with higher levels of psychiatric morbidity.21
In summary, despite proportionately low level of referrals to secondary care, high prevalence makes headache the most frequently listed reason for referral to neurologists and thus, uses capacity that is severely constrained. The potential decrease of referral rates to Neurology specialists as a result of direct access to imaging holds the potential release resources. On the other hand, direct access may be associated with a transfer of workload to Radiology, as not all patients directly referred to brain MRI would routinely undergo an MRI scan as part of the management of their chronic headache. This study aims to evaluate the healthcare utilisation and associated costs of GPs using direct access to brain MRI for the management of chronic headache patients compared with referral to a Neurologist.
Patients and methods
Study design and patient selection
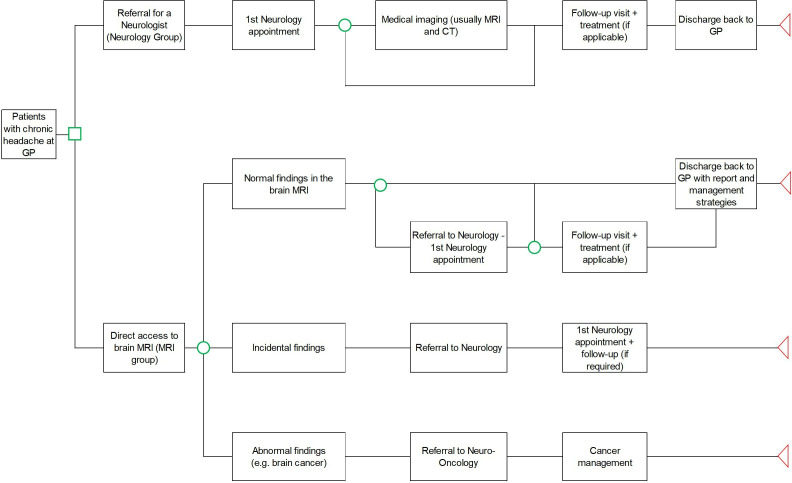
The study was an independent single-centre site, prospective, observational study. The study compared two existing clinical pathways in the management of patients with a chronic headache from either GP referral to the Neurology Department or to direct access to brain MRI. No change to clinical practice was involved. Participants were allocated to two groups, the Neurology group or the MRI group. The allocation was decided a priori, that is, the referrer (in this case the GP) decided which referral route would suit each participant. Subsequent care was consistent with a standard of care for each clinical pathway and depicted in figure 1.
Figure 1.
High-level illustration of two existing clinical pathways associated with the referral from GP due to chronic headache. GP, general practitioner.
Patients eligible for the study included adults aged 16 years or over with chronic migraine defined as occurring ≥15 days per month for more than 3 months (as per International Classification of Headache Disorders 3 (ICHD-3) criteria) and referred from GP practices to a local Hospital in Central London, either for a Neurology outpatient appointment or an MRI examination. Participants were excluded if there were secondary causes for the headache, if they were prisoners, lacked the capacity to give consent or participate in the study, not fluent in English or already taking part in a clinical trial of an investigational medicinal product. Following eligibility assessment, participants completed a written informed consent.
Patient and public involvement statement
This study has involved patient and public involvement during the design and dissemination phase. Prior to the start of the research, a group of patients suffering from chronic headache were consulted to coproduce the study mobile app that was used to monitor symptoms and triggers of chronic headache. The patients who were involved in the study design, as well as all study participants, received a lay summary of the research findings as per their preferences, either via post or email. Research data are available on reasonable request.
Study outcomes
The primary outcome was to estimate the 6-month healthcare costs associated with two existing clinical pathways in the management of chronic headaches. Secondary outcomes comprised: the extension of the cost analysis up to 12 months, the evaluation of access to care, patient satisfaction, headache burden and time off work associated with both clinical pathways.
Service use costs
Total costs were calculated based on the multiplication of any headache-related healthcare events by the unit cost of each event. Resource use data included contacts with any NHS healthcare provider associated with the management of chronic headache. These included, among others, visits to GPs or headache clinical nurse specialist, inpatient care, neurologist or other headache-related outpatient visits (eg, psychiatry), physiotherapist, visits to the ED, advanced imaging such as CT and MRI. Resource use data were retrieved from multiple hospital and primary care databases as well as self-reported data from participants using a participant headache diary (either paper-based or a headache mobile app). For the purposes of the primary outcome, the valuation of unit costs was, whenever possible, based on NHS Reference Costs 2016-17.22 Medication costs were derived from Prescription Cost Analysis23 and estimated from clinical data, specifically secondary care clinic letters and information provided by primary care. Participants were also asked to record time off work due to headache using the weekly participant diary.
Quality of life and headache burden
Headache burden was assessed using validated headache questionnaires and headache diaries. The HIT-6 questionnaire measured the headache burden based on six questions, leading to a score range from 36 to 78. The Migraine Disability Assessment Scale (MIDAS) questionnaire assessed the disability associated with the headache (ranges from 0 to 90). Furthermore, along with the headache diaries completed by participants, the MIDAS questionnaire allowed the estimate of the number of headache days per quarter (maximum of 90 days) and self-reported headache pain scores (ranging from 0, no pain at all, to 10, the worst pain ever).
Access to care
The time elapsed between the GP referral and the first appointment in each group, either the Neurology appointment or the MRI scan, was measured as a proxy for access to care. Furthermore, in the MRI group, the availability of the MRI report to the GP, rather than the actual timing of the diagnostic scan, was considered.
Change in care management
Change in care management in both groups was evaluated. It was considered that a change in care management occurred when patients underwent new treatment options (medication or otherwise, eg, new headache medication, Botox treatment).
Patient satisfaction
Patient satisfaction was evaluated at month 3 postrecruitment using a non-validated questionnaire. This questionnaire evaluated three dimensions of analysis: (a) referral process (time elapsed between referral from primary care to initial secondary care appointment); (b) initial appointment and (c) overall experience 3 months after recruitment.
Statistical analyses
This study was observational but all analyses were based on the principle of ‘intention-to-treat’ so that participants recruited were included in the analysis as per the group they were recruited to, regardless of whether they actually received the intended treatment, any protocol deviations or potential losses to follow-up.24 Given the study’s time horizon of 12 months, no discounting of costs or effects were considered. Descriptive statistics on several socio-demographics baseline characteristics were included. Differences in baseline characteristics between treatment groups were compared using statistical tests: χ2 for categorical data, t-test for Normal data and Mann-Whitney for non-Normal quantitative data. Given the skewness associated with the cost distribution, all cost differences between groups were assessed using generalised linear models (GLM) with an identity-link and gamma distribution. An identity link function instead of a log link was considered in order to avoid potential analytical biases.25 26 An unadjusted GLM cost analysis with the study group (MRI group vs Neurology group) as only univariate analysis was performed as the first step. Given the study’s observational design, the cost difference can be impacted due to the lack of randomisation.27 Baseline variables that differenced between the two groups (p<0.1) were included in the multivariable (adjusted) GLM analyses. For all GLM analyses, group difference estimates and associated confidence intervals were reported, together with p values. Analyses were conducted using Stata V.15.
Sample size
The sample size estimate was calculated based on the primary endpoint, total 6-month healthcare costs. A total of 150 participants were recruited in the Neurology group and 99 participants in the MRI group to achieve a detection a cost difference of £300 assuming SD of £750 and £500, respectively, with 85% power at the 5% two-sided significance level. A 20% increase in sample size due to unknown cost distribution and attrition rate was considered.
Results
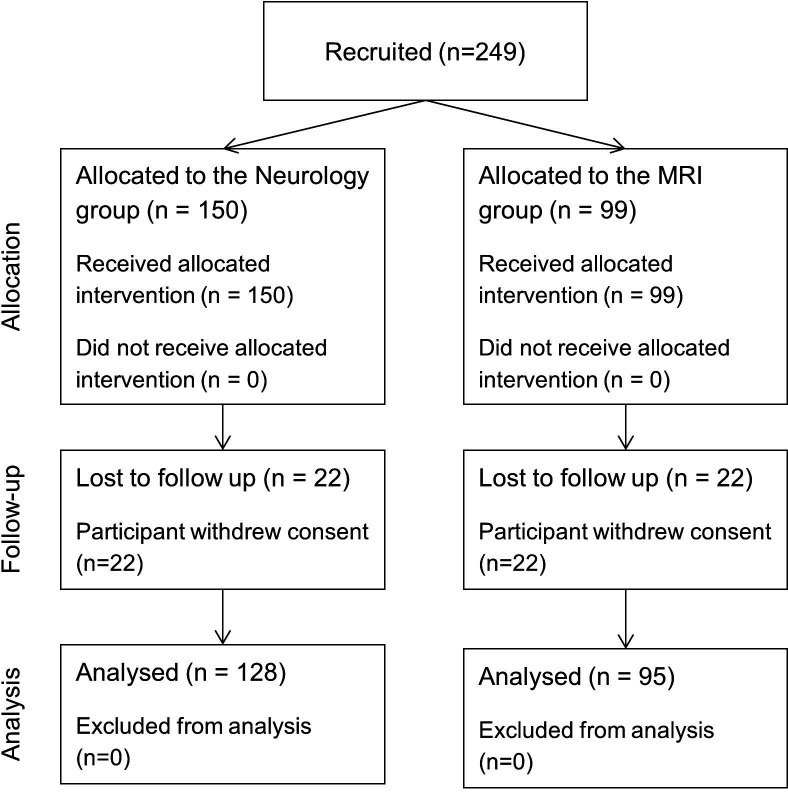
A total of 249 participants were recruited, 150 in the Neurology group and 99 in the MRI group. In total, 100% (n=128) and 97% (n=96) of participants recruited received the treatment allocation in the Neurology and the MRI group, respectively (figure 2). With regards to the follow-up duration, 15% (n=22) and 4.0% (n=4) participants withdrew from the Neurology and MRI group, respectively, and were considered lost to follow-up. Remaining participants (n=223) were included in the analysis, equivalent to 128 (85%) and 95 (96%) participants in the Neurology and MRI group, respectively.
Figure 2.
Participant flow chart for the headache study.
Baseline sociodemographic, clinical variables and resource use in the 12 months prerecruitment are detailed in table 1. A higher proportion of women were recruited to the Neurology group compared with the MRI group (81% vs 68%, p=0.039). Both groups were similar in mean age, ethnic mix, with more than half being White. No significant differences between the groups were found in terms of highest qualification and employment, with high-school and full-time employment being the most common. In terms of clinical variables, no significant difference between groups were found in terms of number of active health problems or number of headache triggers. Participants in the Neurology group reported lower utility and health scores using the generic 5-level EQ-5D (EQ-5D-5L) questionnaire, with a statistically significant difference in health scores (p=0.005). Lower health scores imply lower self-rated quality of life, while for the headache-specific questionnaires (HIT-6 and MIDAS), a higher score implies a higher headache burden. Compared with the MRI group, participants in the Neurology group reported significantly higher headache burden (HIT-6 mean score: 65 vs 63, p=0.006), number of headache days in the past 3 months (MIDAS questionnaire: 52 vs 43, p=0.038). Participants in the Neurology group also had significantly more primary care appointments (3.7 vs 2.4, p<0.001) and all NHS appointments (4.3 vs 2.5, p<0.001).
Table 1.
Baseline characteristics of the population analysed
| Variables | Neurology group (n=128) | MRI group (n=95) | P value |
| Age, years, mean (SD) | 38.4 (14.1) | 40.0 (14.6) | 0.514 |
| Gender, Female, n (%) | 103 (81) | 65 (68) | 0.039 |
| Ethnicity | 0.079 | ||
| Asian | 13 (10) | 6 (6.3) | |
| Black | 40 (31) | 17 (18) | |
| White | 68 (53) | 60 (63) | |
| Mixed | 5 (3.9) | 8 (8.4) | |
| Other | 2 (1.6) | 4 (4.2) | |
| Qualification, n (%) | 0.565 | ||
| Advanced work or PhD | 3 (2.3) | 4 (4.2) | |
| Master’s degree | 15 (12) | 12 (13) | |
| Bachelor’s degree | 31 (24) | 29 (31) | |
| High school | 57 (45) | 33 (35) | |
| Did not finish high school | 8 (6.3) | 10 (11) | |
| Prefer not to answer | 14 (11) | 7 (7.4) | |
| Employment, n (%) | 0.839 | ||
| Employee in full-time job (30 hours or more a week) | 50 (39) | 36 (38) | |
| Employee in part-time job (under 30 hours a week) | 18 (14) | 18 (19) | |
| Self-employed, full or part time | 12 (9.4) | 8 (8.4) | |
| Full-time education at school, college or university | 16 (13) | 9 (9.5) | |
| Doing something else | 2 (1.6) | 2 (2.1) | |
| Permanently sick/disabled | 8 (6.3) | 6 (6.3) | |
| Looking after the home | 4 (3.1) | 6 (6.3) | |
| Unemployed and available for work | 12 (9.4) | 6 (6.3) | |
| Wholly retired from work | 4 (3.1) | 4 (4.2) | |
| Prefer not to answer | 2 (1.6) | 0 (0) | |
| Presence of mental health condition, n (%) | 22 (17) | 11 (12) | 0.243 |
| Number of active health problems: mean (SD) | 2.0 (1.5) | 1.8 (1.4) | 0.277 |
| Number of headache triggers: mean (SD) | 2.1 (1.8) | 1.8 (1.4) | 0.378 |
| Self-reported questionnaires | |||
| EQ-5D-5L, mean utility (SD) | 0.809 (0.182) | 0.830 (0.195) | 0.097 |
| EQ-5D-5L, mean score (SD) | 64 (19) | 71 (20) | 0.005 |
| HIT-6, mean score (SD) | 65 (5.3) | 63 (7.3) | 0.006 |
| MIDAS, mean score (SD) | 58 (54) | 45 (45) | 0.075 |
| MIDAS, mean headache days (SD) | 52 (32) | 43 (31) | 0.038 |
| MIDAS, mean pain score (SD) | 6.9 (1.8) | 6.9 (1.9) | 0.778 |
| Resource use in the 12 months prior to recruitment | |||
| GP appointments, mean (SD) | 3.7 (2.9) | 2.4 (1.5) | <0.001 |
| All NHS events, mean (SD) | 4.3 (3.7) | 2.5 (1.5) | <0.001 |
EQ-5D-5L, 5-level EQ-5D; GP, general practitioner; HIT-6, Headache Impact Test; MIDAS, Migraine Disability Assessment Scale; NHS, National Health Service.
Service use
Table 2 summarises the NHS resource use of primary care and hospital-based services over a period of 12 months following recruitment. With regards to primary care utilisation, participants in the Neurology group had a significantly higher number of GP face-to-face appointments (mean number per participant: 1.82 vs 1.19, p=0.006). Regarding secondary care, participants in the Neurology group had a higher mean number of outpatient appointments (2.52 vs 0.26, p<0.001) and other treatments such as Botox and nerve root injection (mean 0.30 vs 0.05, p<0.001). In contrast, they had a lower mean number of brain MRIs (0.59 vs 1.05, p<0.001). There were no statistically significant differences in the utilisation levels of any of the other healthcare events.
Table 2.
Breakdown of number of NHS appointments per type of activity organised per group and respective number of participants responsible for these appointments (12 months postrecruitment)
| Type of NHS appointment | Neurology group (n=128) | MRI group (n=95) | P value | ||||
| Total of episodes | Mean (SD) | N (%) | Total of episodes | Mean (SD) | N (%) | ||
| Primary care services | |||||||
| GP face-to-face appointment | 233 | 1.82 (2.11) | 91 (71) | 113 | 1.19 (1.64) | 57 (60) | 0.006 |
| GP phone appointment | 37 | 0.29 (0.75) | 24 (19) | 25 | 0.26 (0.49) | 23 (24) | 0.420 |
| Hospital-based services | |||||||
| Hospital outpatient appointment | 322 | 2.52 (1.19) | 128 (100) | 25 | 0.26 (0.55) | 20 (21) | <0.001 |
| Inpatient episode | 4 | 0.03 (0.35) | 1 (0.8) | 1 | 0.01 (0.10) | 1 (1.1) | 0.837 |
| Emergency department episode | 8 | 0.06 (0.24) | 8 (6.3) | 5 | 0.05 (0.22) | 5 (5.3) | 0.756 |
| Head CT | 1 | 0.01 (0.09) | 1 (0.8) | 1 | 0.01 (0.10) | 1 (1.1) | 0.832 |
| Brain MRI | 75 | 0.59 (0.49) | 75 (59) | 100 | 1.05 (0.30) | 95 (100) | <0.001 |
| Others (eg, botox and nerve injection treatments) | 39 | 0.30 (0.79) | 25 (20) | 5 | 0.05 (0.30) | 3 (3.2) | <0.001 |
GP, general practitioner; NHS, National Health Service.
The NHS resource use pre and postrecruitment for both groups was also compared. Table 3 summarises the difference between headache-related events 12 months postrecruitment compared with the 12 months prerecruitment. A reduction of 197 and 87 GP visits (mean 1.54/0.92 per participant or a percentage reduction of 85%/77%) was noted in the Neurology and MRI group, respectively. Similarly, there was a reduction in ED utilisation with a decrease of 23 and 6 episodes (mean 0.18 and 0.07 per participant or a percentage reduction of 288% and 120%) in the Neurology and MRI group, respectively.
Table 3.
Difference in the number, mean and percentage reduction of NHS appointments per type of activity organised per group 12 months postrecruitment compared with the 12 months prerecruitment (note: a negative/positive percentage denotes a decrease/increase in activity following recruitment)
| Type of NHS appointment | Neurology group (n=128) | MRI group (n=95) | ||||
| Total of episodes | Mean | % | Total of episodes | Mean | % | |
| Primary care services | ||||||
| GP face-to-face appointment | −197 | −1.54 | −85 | −87 | −0.92 | −77 |
| GP phone appointment | −11 | −0.09 | −30 | 5 | 0.05 | 20 |
| Hospital-based services | ||||||
| Hospital outpatient appointment | 301 | 2.36 | 93 | 23 | 0.24 | 92 |
| Inpatient episode | 3 | 0.02 | 75 | 1 | 0.01 | 100 |
| Emergency department episode | −23 | −0.18 | −288 | −6 | −0.07 | −120 |
| Head CT | −9 | −0.07 | −12 | 1 | 0.01 | 1.0 |
| Brain MRI | 55 | 0.43 | 141 | 100 | 1.05 | NA |
GP, general practitioner; NHS, National Health Service.
Cost analyses
The mean (SD) cost management per participant at 6 months postrecruitment was lower in the MRI group compared with the Neurology group (£245 (£172) vs £578 (£420)), leading to a mean cost difference between groups of −£333 per participant (95% CI: −£413 to −£253, p<0.001). The MRI group had a higher proportion of participants with lower costs (£0–£250 range) than the Neurology group (73% vs 4.7%). The initial cost analysis was extended to 12 months postrecruitment and the mean cost difference between groups increased, with the MRI group generating cost savings of £518 per participant (95% CI: −£637 to −£401, p<0.001).
Given the non-randomised study design, an additional GLM analysis was performed to adjust for baseline characteristics. The unadjusted 6-month cost difference between groups (−£333; 95% CI: −£413 to −£253) hardly changed after adjustment (−£308; 95% CI: −£408 to −£209). In all analyses, at both 6 and 12 months postrecruitment, direct access to MRI for the management of chronic headache was associated with statistically significant mean cost savings for the NHS.
Abnormal findings in the MRI group
Out of the 95 participants recruited in the MRI group, three MRIs were not performed during the initial appointment due to claustrophobia events. From a total number of 92 MRIs, 85 (92%) were normal and 7 (7.6%) presented abnormal findings (table 4), with one diagnosis being particularly significant (two small intracranial aneurysms). This participant was referred to neurovascular team for assessment, at which point no intervention was performed during the follow-up period (participant included in an active surveillance group). Two other participants had a change in their clinical management for less significant findings, leading to either a follow-up appointment or scan. No brain malignancies were diagnosed.
Table 4.
Description of incidental findings, its clinical relevance and subsequent pathway
| Abnormal findings | Significant (yes/no)? | Changes in diagnostic or treatment pathway |
| Mature striatocapsular lacune | No | |
| Sinusitis with complete opacification | No | Ear, nose, and throat (ENT) specialist review only |
| Pituitary abnormality (T1) | No | |
| Low lying cerebellar tonsils | No | |
| Previous petrous surgery noted | No | |
| Two aneurysms AcomA (anterior communicating artery) and right ICA | Yes | Referred to neurovascular—no coiling (no intervention) |
| No definitive lesion | No | Follow-up MRI only |
ICA, internal carotid artery.
Access to care
The mean time (SD) elapsed from GP referral to the initial Neurology and MRI scan was, respectively, 110 (35) days and 39 days (17), a statistically significant difference (p<0.001). Second, if the MRI report, than the actual scan, is considered as a proxy for access to care, the mean time elapsed was 70 days (35) (p<0.001).
Change in management
Participants in the Neurology group were more likely to have a change in therapeutic management compared with participants in the MRI group (97% vs 64%, p<0.001). Similarly, among participants that had not started on preventative medication prerecruitment, a higher proportion of participants in the Neurology group were started on preventative medication as part of their clinical management (93% vs 53%, p<0.001).
Quality of life and headache burden
At baseline, mean utility was lower in the Neurology group but not significant (mean utility of 0.809 vs 0.830, p=0.097), while their self-perceived mean health score was significantly lower (EQ-5D-5L: visual analogue scale score of 64.0 vs 70.8, p=0.005) (table 5). There was no statistically significant differences between the groups at 6 months for the utility and self-reported healthcare scores.
Table 5.
Descriptive statistics for one generic questionnaire (EQ-5D-5L) and two headache-specific questionnaires (HIT-6 and MIDAS) at baseline and 6 months postrecruitment
| N | Mean | SD | P value | ||||
| Baseline | EQ-5D-5L | Utility | Neurology | 127 | 0.809 | 0.182 | 0.097 |
| Radiology | 95 | 0.830 | 0.195 | ||||
| Score | Neurology | 126 | 64.0 | 18.8 | 0.005 | ||
| Radiology | 95 | 70.8 | 20.2 | ||||
| HIT-6 | Score | Neurology | 128 | 65.0 | 5.3 | 0.006 | |
| Radiology | 92 | 62.6 | 7.3 | ||||
| MIDAS | Score | Neurology | 124 | 57.8 | 54.0 | 0.075 | |
| Radiology | 90 | 44.8 | 44.9 | ||||
| Headache days | Neurology | 124 | 51.6 | 31.5 | 0.038 | ||
| Radiology | 90 | 42.8 | 30.7 | ||||
| Pain score | Neurology | 124 | 6.9 | 1.8 | 0.778 | ||
| Radiology | 90 | 6.9 | 1.9 | ||||
| Month 6 | EQ-5D-5L | Utility | Neurology | 55 | 0.770 | 0.263 | 0.243 |
| Radiology | 26 | 0.681 | 0.346 | ||||
| Score | Neurology | 53 | 68.2 | 20.6 | 0.463 | ||
| Radiology | 23 | 62.5 | 24.7 | ||||
| HIT-6 | Score | Neurology | 35 | 60.0 | 8.7 | 0.968 | |
| Radiology | 12 | 53.1 | 22.8 | ||||
| MIDAS | Score | Neurology | 32 | 52.6 | 58.1 | 0.827 | |
| Radiology | 12 | 40.7 | 36.0 | ||||
| Headache days | Neurology | 46 | 41.2 | 28.6 | 0.152 | ||
| Radiology | 15 | 26.5 | 28.1 | ||||
| Pain score | Neurology | 44 | 4.5 | 2.3 | 0.663 | ||
| Radiology | 15 | 4.2 | 2.0 |
EQ-5D-5L, 5-level EQ-5D; HIT-6, Headache Impact Test; MIDAS, Migraine Disability Assessment Scale.
At baseline, participants in the Neurology group presented a higher headache burden compared with the MRI group (mean score of 65.0 vs 62.6, p=0.006) (table 5). This trend seemed to be maintained over the follow-up period but was difficult to interpret due to high attrition rates: mean HIT-6 score at 6 months (60.0 vs 53.1, p=0.968). At baseline, participants in the Neurology group had higher headache severity compared with the MRI group, but this was not significant (mean MIDAS score of 57.8 vs 44.8, p=0.075) (table 5). In both groups, the headache severity decreased over the follow-up period. At baseline, participants in the Neurology group reported a significantly higher mean number of headache days compared with the MRI group (51.6 vs 42.8, p=0.038). This trend was observed at month 6 but was not significant (41.2 vs 26.5, p=0.152). A third variable assessed self-reported headache pain scores. At baseline, participants at baseline showed almost identical mean headache pain scores (6.9 vs 6.9, p=0.827). During the follow-up period, no statistical differences were found at month 6 (4.5 vs 4.2, p=0.663).
Time off work
Participants in the Neurology group (n=83) had a higher mean number of days off work due to headache compared with participants in the MRI group (n=35) but these were not statistically significant at 6 (13.9 vs 9.7, p=0.563) or 12 months (27.9 vs 19.1, p=0.808) postrecruitment.
Patient satisfaction
Patient satisfaction was evaluated at month 3 postrecruitment using a non-validated questionnaire (online supplemental file 1). Participants in both groups reported no difference in terms of receiving an appointment in a suitable timeframe (p=0.193). Participants in the MRI group reported higher satisfaction levels (p=0.005) compared with the Neurology group associated with the information received prior to the actual appointment. No statistically significant difference (p=0.366) between the groups was found regarding the satisfaction levels of both appointments (either MRI scan or Neurologist appointment) but a higher proportion of participants in the Neurology group reported a better experience compared with their expectation (p=0.002). At month 3 postrecruitment in all variables, except frequency of appointments (p=0.166), participants in the Neurology group reported higher levels of satisfaction with: amount of time spent with clinical staff (p=0.001); consistency of care (p=0.028); how informed you felt about your condition (p=0.010)/your treatment (p=0.004) and the overall experience (p<0.001).
bmjopen-2019-036097supp001.pdf (29.3KB, pdf)
Discussion
Previous UK studies assessed the use of direct access to advanced imaging in the management of chronic headache patients.10 21 Howard et al21 performed a randomised controlled trial, which showed that the use of imaging in patients led to a reduction of referral rates to Neurology services in secondary care from 23% to 1.3% (1/76) in the treatment group (ie, patients being scanned).21 Thomas et al10 estimated that direct access to brain imaging, in this case CT, reduced referral rates to Neurology in 86% of the cases during the follow-up period (average of 1.3 years per patient).10
The study’s underlying hypothesis was that the early use of an advanced and accurate diagnostic tool (in this case MRI) would reassure both patients and GPs that no serious underlying cause (particularly brain tumour) is present. This would, in turn, reduce the headache burden and NHS resource use associated with the patient’s subsequent management. Given the high prevalence of headache and the increased referral of patients with chronic headaches and other neurological conditions from primary care to hospital-based care,7 it is relevant to assess the implications of using different management strategies. To our knowledge, no previous prospective study in the UK has assessed the economic implications of these two coexisting management strategies based on GP referral decision.
The primary outcome was total costs at 6 months postrecruitment. The study showed that the use of advanced imaging produced cost-savings to the NHS compared with referral to Neurology, with mean cost-savings per participant of £333 and £518 at month 6 and 12 postrecruitment, respectively (p<0.001). These cost differences were multifactorial but primarily driven by: (1) the lower unit cost of a brain MRI scan (£146) compared with the initial Neurology appointment (£240); (2) the lower number of outpatient appointments in the MRI group (25 vs 322); (3) the fact that 75/128 (59%) of participants in the Neurology group ended up having a brain MRI scan in the 12-month period of follow-up and (4) the increased likelihood of patients in the Neurology arm receiving management with Botox injections or nerve block procedures (39 vs 5 events). Direct access to brain MRI seemed to reassure most participants as only 17 (18%) participants in the MRI group ended up being referred to a neurologist. Furthermore, over 66% of participants in the MRI group had no further hospital-based care, compared with 5% in the Neurology group. Similarly, at primary care level, participants in the MRI group presented lower utilisation rates per participant when compared with the Neurology group (mean GP appointments of 1.82 vs 1.19, p=0.006). In order to mitigate the potential confounding by indication introduced by GPs referring patients to both clinical pathways, adjusted GLMs were conducted. All cost differences between groups remained statistically significant (p<0.001) when adjusted for differences in baseline characteristics or follow-up attrition rates.
At baseline, participants in the Neurology group presented lower self-reported quality of life and higher headache burden. HIT-6 scores did improve over time but we were unable to assess whether there was a statistically significant difference in both groups due to the high attrition rates, particularly in the MRI group. As mentioned, out of the 95 participants recruited to the MRI group, 17 (18%) were subsequently referred to a Neurologist. Interestingly, at baseline, these 17 patients reported higher headache burden compared with all 95 patients recruited to the MRI group (MIDAS score: 51.2 vs 44.8; MIDAS headache days: 55.8 vs 42.8). This finding seems to suggest that these data might be useful to risk stratify patients and support GPs in their referral criteria. However, further research into this area is required.
Participants in the Neurology group presented a higher probability of being started on a preventative medication and had a change in therapeutic management following referral from primary care. A small proportion (7.6%) of participants in the MRI group had abnormal findings in the initial brain MRI. Only one participant had clinically significant lesions (two small aneurysms) which were also incidental and no brain tumour was diagnosed.
Time off work was also evaluated as a proxy of headache burden. Participants in the Neurology group presented a trend (p>0.05) of a higher number of days off work due to headache compared with participants in the MRI group. This difference was not, however, statistically significant.
Lastly, patient satisfaction in both groups was compared based on three dimensions of analysis: during the referral period, the initial appointment and overall satisfaction. Twenty-five per cent of participants in the Neurology group (vs 18% in the MRI group) reported dissatisfaction with the waiting time. This finding is not unexpected as the mean waiting time associated with the Neurology appointment was almost three times the one associated with the MRI scan (110 vs 39 days). Contrary to the referral period, participants in the Neurology group reported trends of higher satisfaction levels associated with the first appointment (neurology outpatient visit vs MRI scan) and a better experience compared with their expectations (60% vs 29% in the Neurology and MRI group, respectively). Participants in the Neurology group reported improved satisfaction levels at 3 months across different variables (time spent with clinician, consistency of care, information about the condition and its treatment). Almost three quarters of Neurology participants reported being satisfied or very satisfied with their headache management compared with only 21% in the MRI group (p<0.001). Both participants and GP referrers in the MRI group reported dissatisfaction associated with the waiting time elapsed between the MRI scan and the availability of results (mean time of 31 days). This might have contributed to increased anxiety in some participants.
Strengths of this study
The estimate of NHS resource use data was primarily based on comprehensive and complete data retrieved from hospital-based databases that captured both the acute and elective elements of the pathway associated with the management of patients with chronic headache. These data were supplemented by both primary care utilisation data, collected from each participant’s GP and self-reported participant data. The aim was to guarantee that any chronic headache-related NHS event was costed regardless of the healthcare provider and its location. The prospective collection of healthcare utilisation and the evaluation of the impact of the interventions across different dimensions of analysis (efficiency, quality of care, access to care and patient satisfaction) were other key factors that contributed to the overall strength of the study.
Limitations of this study
There were some limitations to this study. First, this was a single-centre study with participants recruited from one central hospital in London. A multicentre study would be necessary to explore the generalisability of the results. Second, as with any observational study, no randomisation between groups was performed and there were significant differences in baseline of headache burden and health-scores and utilisation of resources. In order to mitigate potential confounding factors, adjusted multivariate analyses showed that the primary outcome was hardly affected and remained statistically significant. Nevertheless, residual confounding factors remain a limitation of the study. Third, specific inclusion and exclusion criteria were considered and as such, the study sample might not be representative of all patients with chronic headache. Fourth, for the purpose of secondary outcomes, most data were self-reported and hence prone to recall bias. Lastly, there were high follow-up attrition rates, particularly for participants in the MRI group, which affected some of the study’s secondary outcomes.
Conclusions
This study found that the referral from primary care to direct access to brain MRI compared with referral for a neurologist for patients with chronic headache was associated with lower NHS overall costs at 6 and 12 months postrecruitment. Despite waiting longer from referral to appointment, participants in the Neurology group reported higher satisfaction levels associated with the care received compared with the MRI group and were more likely to benefit from changes to their therapeutic management.
Implications for further research and clinical practice
Baseline measures of headache burden, such as the HIT-6 or MIDAS, could potentially be used to determine which pathway may be suitable for patients but further research into the risk stratification of chronic headache patients is required. Future study designs should consider the confounding by indication introduced by recruiting participants referred to the two pathways based on GP decision. With regards to clinical practice, and based on the study findings, we plan to provide GPs with headache management advice along with the MRI report.
Supplementary Material
Acknowledgments
The authors would like to thank all patients and staff members at Guy’s and St Thomas’ NHS Trust, particularly neurology and radiology consultants, for making this study possible.
Footnotes
Contributors: TR, AM, YA, JT, RR, JLP, PM and SA contributed to conception and design of data. TR, YA, CM and JO contributed to acquisition of data. TR, JLP, PM and JS involved in analysis and interpretation of data. TR, AM, JLP, PM, VG, JS and SA involved in drafting the manuscript. TR, AM, YA, CM, JT, RR, JLP, PM, VG, JS and SA contributed to final approval of the completed manuscript.
Funding: This work was supported by the Guy’s and St Thomas’ Charity.
Competing interests: None declared.
Patient consent for publication: Not required.
Ethics approval: The Health Research Authority and Research Ethics Committee (West of Scotland—REC 4) approved the study research on 12 April 2016 (REC reference 16/WS/0028).
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data are available upon reasonable request. Extra data can be accessed via the Dryad data repository at http://datadryad.org/ with the doi: 10.5061/dryad.d7wm37pzn.
References
- 1.Jensen R, Stovner LJ. Epidemiology and comorbidity of headache. Lancet Neurol 2008;7:354–61. 10.1016/S1474-4422(08)70062-0 [DOI] [PubMed] [Google Scholar]
- 2.Stovner L, Hagen K, Jensen R, et al. . The global burden of headache: a documentation of headache prevalence and disability worldwide. Cephalalgia 2007;27:193–210. 10.1111/j.1468-2982.2007.01288.x [DOI] [PubMed] [Google Scholar]
- 3.Boardman HF, Thomas E, Croft PR, et al. . Epidemiology of headache in an English district. Cephalalgia 2003;23:129–37. 10.1046/j.1468-2982.2003.00468.x [DOI] [PubMed] [Google Scholar]
- 4.Vos T, Flaxman AD, Naghavi M, et al. . Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the global burden of disease study 2010. The Lancet 2012;380:2163–96. 10.1016/S0140-6736(12)61729-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Leonardi M, Raggi A. Burden of migraine: international perspectives. Neurological Sciences 2013;34:117–8. 10.1007/s10072-013-1387-8 [DOI] [PubMed] [Google Scholar]
- 6.Rasmussen BK, Jensen R, Schroll M, et al. . Epidemiology of headache in a general population--a prevalence study. J Clin Epidemiol 1991;44:1147–57. 10.1016/0895-4356(91)90147-2 [DOI] [PubMed] [Google Scholar]
- 7.Latinovic R, Gulliford M, Ridsdale L. Headache and migraine in primary care: consultation, prescription, and referral rates in a large population. J Neurol Neurosurg Psychiatry 2006;77:385–7. 10.1136/jnnp.2005.073221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Department of Health Direct access to diagnostic tests for cancer: best practice referral pathways for general practitioners, 2012. [Google Scholar]
- 9.Braschinsky M, Haldre S, Kals M, et al. . Structured education can improve primary-care management of headache: the first empirical evidence, from a controlled interventional study. J Headache Pain 2016;17:24. 10.1186/s10194-016-0613-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Thomas R, Cook A, Main G, et al. . Primary care access to computed tomography for chronic headache. Br J Gen Pract 2010;60:426–30. 10.3399/bjgp10X502146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Patterson VH, Esmonde TF. Comparison of the handling of neurological outpatient referrals by general physicians and a neurologist. J Neurol Neurosurg Psychiatry 1993;56:830. 10.1136/jnnp.56.7.830 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ridsdale L, Doherty J, McCrone P, et al. . A new GP with special interest headache service: observational study. Br J Gen Pract 2008;58:478–83. 10.3399/bjgp08X319440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Osumili B, McCrone P, Cousins S, et al. . The economic cost of patients with migraine headache referred to specialist clinics. Headache 2018;58:287–94. 10.1111/head.13210 [DOI] [PubMed] [Google Scholar]
- 14.Bloudek LM, Stokes M, Buse DC, et al. . Cost of healthcare for patients with migraine in five European countries: results from the International burden of migraine study (IBMS). J Headache Pain 2012;13:361–78. 10.1007/s10194-012-0460-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Katsarava Z, Mania M, Lampl C, et al. . Poor medical care for people with migraine in Europe - evidence from the Eurolight study. J Headache Pain 2018;19:10. 10.1186/s10194-018-0839-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McCrone P, Seed PT, Dowson AJ, et al. . Service use and costs for people with headache: a UK primary care study. J Headache Pain 2011;12:617–23. 10.1007/s10194-011-0362-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Morgan M, Jenkins L, Ridsdale L. Patient pressure for referral for headache: a qualitative study of GPs’ referral behaviour. Br J Gen Pract J R Coll Gen Pract 2007;57:29–35. [PMC free article] [PubMed] [Google Scholar]
- 18.Underwood R, Kilner R, Ridsdale L. Primary care management of headaches and how direct-access MRI fits: a qualitative study of UK general practitioners' views. BMJ Open 2017;7:e018169. 10.1136/bmjopen-2017-018169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.NICE Management of headaches, 2018. Available: https://pathways.nice.org.uk/pathways/headaches [Accessed 28 Jan 2019].
- 20.Callaghan BC, Kerber KA, Pace RJ, et al. . Headache neuroimaging: routine testing when guidelines recommend against them. Cephalalgia 2015;35:1144–52. 10.1177/0333102415572918 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Howard L, Wessely S, Leese M, et al. . Are investigations anxiolytic or anxiogenic? a randomised controlled trial of neuroimaging to provide reassurance in chronic daily headache. J Neurol Neurosurg Psychiatry 2005;76:1558–64. 10.1136/jnnp.2004.057851 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.NHS Improvement Reference costs | NHS improvement, 2017. Available: https://improvement.nhs.uk/resources/reference-costs/#rc1718 [Accessed 31 Jul 2019].
- 23.NHS Business Services Authority Prescription cost analysis (PCA) data, 2018. Available: https://www.nhsbsa.nhs.uk/prescription-data/dispensing-data/prescription-cost-analysis-pca-data [Accessed 31 Jul 2019].
- 24.Gupta SK. Intention-To-Treat concept: a review. Perspect Clin Res 2011;2:109–12. 10.4103/2229-3485.83221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Polgreen LA, Brooks JM. Estimating incremental costs with skew: a cautionary note. Appl Health Econ Health Policy 2012;10:319–29. 10.2165/11632430-000000000-00000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Barber JA, Thompson SG. Analysis of cost data in randomized trials: an application of the non-parametric bootstrap. Stat Med 2000;19:3219–36. [DOI] [PubMed] [Google Scholar]
- 27.Moran JL, Solomon PJ, Peisach AR, et al. . New models for old questions: generalized linear models for cost prediction. J Eval Clin Pract 2007;13:381–9. 10.1111/j.1365-2753.2006.00711.x [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2019-036097supp001.pdf (29.3KB, pdf)