Abstract
Objective
To investigate the prevalence of, and associations between, prenatal and perinatal risk factors and developmental vulnerability in twins at age 5.
Design
Retrospective cohort study using bivariate and multivariable logistic regression.
Setting
Western Australia (WA), 2002–2015.
Participants
828 twin pairs born in WA with an Australian Early Development Census (AEDC) record from 2009, 2012 or 2015.
Main outcome measures
The AEDC is a national measure of child development across five domains. Children with scores <10th percentile were classified as developmentally vulnerable on, one or more domains (DV1), or two or more domains (DV2).
Results
In this population, 26.0% twins were classified as DV1 and 13.5% as DV2. In the multivariable model, risk factors for DV1 were maternal age <25 years (adjusted OR (aOR): 7.06, 95% CI: 2.29 to 21.76), child speaking a language other than English at home (aOR: 6.45, 95% CI: 2.17 to 19.17), male child (aOR: 5.08, 95% CI: 2.89 to 8.92), age younger than the reference category for the study sample (≥5 years 1 month to <5 years 10 months) at time of AEDC completion (aOR: 3.34, 95% CI: 1.55 to 7.22) and having a proportion of optimal birth weight (POBW) <15th percentile of the study sample (aOR: 2.06, 95% CI 1.07 to 3.98). Risk factors for DV2 were male child (aOR: 7.87, 95% CI: 3.45 to 17.97), maternal age <25 (aOR: 5.60, 95% CI: 1.30 to 24.10), age younger than the reference category (aOR: 5.36, 95% CI: 1.94 to 14.82), child speaking a language other than English at home (aOR: 4.65, 95% CI: 1.14 to 19.03), mother’s marital status as not married at the time of twins’ birth (aOR: 4.59, 95% CI: 1.13 to 18.55), maternal occupation status in the lowest quintile (aOR: 3.30, 95% CI: 1.11 to 9.81) and a POBW <15th percentile (aOR: 3.11, 95% CI: 1.26 to 7.64).
Conclusion
Both biological and sociodemographic risk factors are associated with developmental vulnerability in twins at 5 years of age.
Keywords: epidemiology, paediatrics, public health
Strengths and limitations of this study.
The study is based on a large population-level sample of 1656 twins.
This is the first twin study to assess developmental vulnerabilities in an otherwise healthy sample of Australian twins, at the time of their first year of full-time school.
Bivariate and multivariable logistic regression analysis with the calculation of adjusted ORs was performed to explore the associations between a large range of prenatal and perinatal risk factors.
Twin pairs for which data were complete were used for the analysis.
The data sets used in this study did not report on twin zygosity nor on complications of pregnancy that are specific to multiple pregnancies (eg, twin reversed arterial perfusion, twin-twin transfusion syndrome).
Introduction
The increased use of assisted reproductive technologies and increasing maternal age at conception have attributed to a significant increase in the number of multifetal pregnancies around the world.1 Multifetal pregnancies are classified as high-risk pregnancies and compared with singleton pregnancies, are associated with higher rates of pregnancy complications and adverse neonatal and perinatal outcomes.2–6 The majority of the literature assessing higher order pregnancies has focused primarily on birth outcomes, including preterm birth,7 low birth weight3 and developmental disabilities such as cerebral palsy.8 Studies that have assessed the longer term developmental outcomes of twins have focused on developmental outcomes around the age of 2.9 Such studies have reported that twins had poorer performance, in comparison to singletons, on a range of domains including communication, gross and fine motor skills, problem solving, personal–social skills and language development.10 11 Furthermore, most studies examining child development outcomes at school starting age have focused on singleton children, from a single family and have compared children across families.12 There is a paucity of research on the developmental vulnerability of multifetal pregnancies such as twins, around the time that they commence formal education.
Child development outcomes can vary significantly based on numerous factors including the child’s personal characteristics, such as personal dispositions and abilities, social constructs and the environments, both intrauterine and extrauterine, in which they develop.13–16 Studies that have assessed cognitive and school performance outcomes at the age of 5 have reported that children who are born preterm,17–24 with a low birth weight,25–28 are small for gestational age,29 30 and male31–34 are more likely to have poorer developmental outcomes. In comparison to singletons, twins are more likely to be classified as preterm35 or low birth weight, and have fetal growth restriction.36 Studies have also reported that twins are more likely to have poorer neurodevelopmental outcomes compared with singletons, even after controlling for gestational age and birth weight.37 A study reported that twins scored lower than singletons in both the Verbal and Performance IQ domains of the Wechsler Preschool and Primary Scale of Intelligence, at the ages of 4 and 5.38 Likewise, twin studies have also reported sex differences, with girls scoring higher than boys at ages 4 and 5.38 The cumulative nature of school-based learning means that developmental gaps at school entry are difficult to close over time.39 Children who begin school with poor school readiness often struggle to catch up with their peers and tend to fall further behind as they progress through the subsequent years of schooling.39 As educational achievement trajectories are largely established by 7 years of age (year 3) children with poor school readiness are more likely to have lower later-life educational achievement.40 Given the higher rates of pregnancy, neonatal and perinatal adversities observed in twins in comparison to singletons, twins are particularly at risk for developmental delays in the early childhood period.
Twin studies, assessing the contribution of genes and the environment, have supported the hypothesis that both factors impact child development.41–44 Yet, a number of studies have reported no significant differences in child development outcomes based on zygosity.38 45 46 Sociodemographic factors such as low socioeconomic status and low levels of parental education have also been identified to adversely impact child development outcomes.47–49 A study conducted in younger twins (assessed at age 6, 12 and 18 months) reported that biological factors including low birth weight were associated with poorer early cognitive and non-cognitive development, independently of environmental factors, such as socioeconomic status.3 Alternatively, a study reported that the environmental factors shared by twins of the same family were more significantly associated with early language skills and school readiness in twins at the age of 5, in comparison to genetic factors.45 Overall, studies assessing both biological and sociodemographic factors, and their impact on the longer term child development of children born from multiple pregnancies, remain sparse and the results of the existing studies are mixed.
The aim of this study was to examine the prevalence of, and the association between, biological and sociodemographic risk factors and developmental vulnerability in twins in their first year of full-time school.
Methods
Data sources and study population
Data sources
This study used anonymised individual-level data from the Midwives Notification System (MNS), which is a statutory record of all births (still-born or live-born) in Western Australia (WA) with either a birth weight >400 g and/or a final gestational length of ≥20 weeks. Variables from MNS were cross validated with corresponding records from WA Birth Registrations. Australian Early Development Census (AEDC) records were obtained for all available years (2009, 2012 and 2015) for all children with WA birth and perinatal records. Across the 2009, 2012 and 2015 AEDC data collections child participation for the State of WA ranged between 98.7% and 99.6%.50 WA Register for Developmental Anomalies (WARDA) records were used to identify children who had a diagnosed developmental disability between birth and age 5. Statistical linkage of all records, by matching identifiers (eg, name, address, date of birth, etc) common to sets of records,51 was provided by the WA Data Linkage Branch from the Department of Health WA.
Patient and public involvement
No patients were involved in the development of the research question or the outcome measures, or in the development of the plans for the design or implementation of the study.
Study population
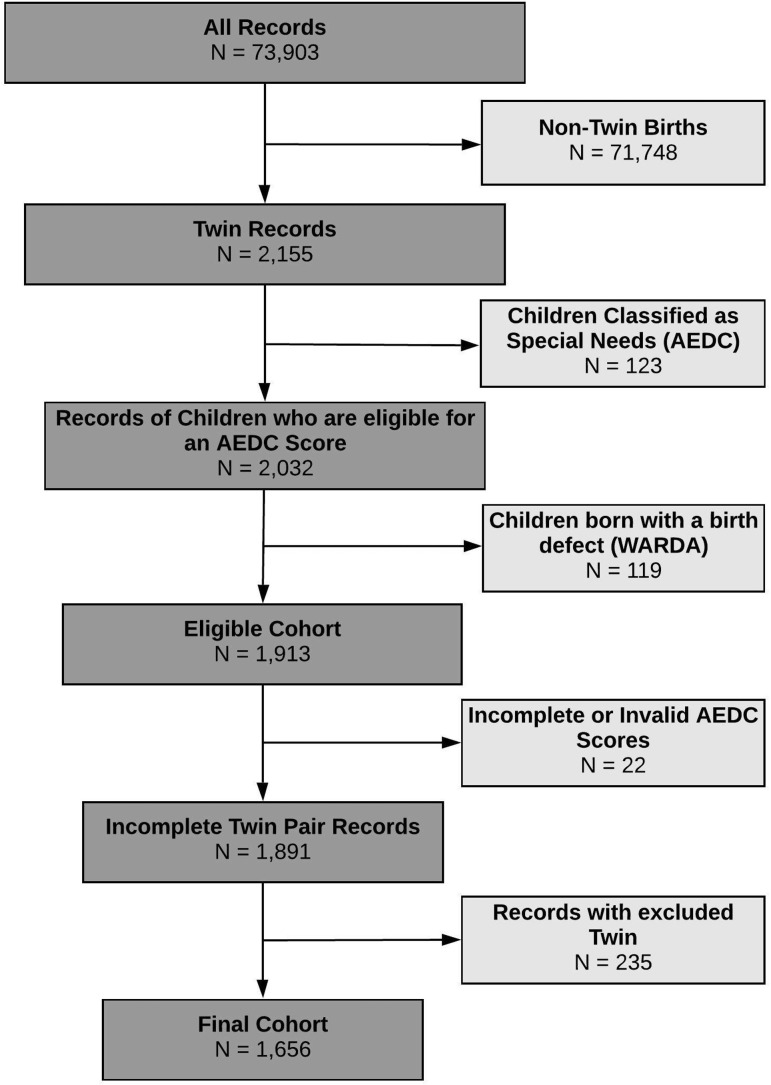
The study population included all children born in WA with an AEDC record in either 2009, 2012 or 2015 (n=73 903). Children were excluded from the study if (1) they were not from a twin birth (n=71 748), (2) they were identified by their teacher as having ‘special-needs’ based on a diagnosed physical and/or intellectual disability (n=123), (3) they were reported as having any birth defect in the WARDA data sets (n=119), (4) they had an AEDC score that was either incomplete or missing (n=22) or (5) their twin sibling was excluded based on the aforementioned exclusion criteria (n=235; figure 1). The final study sample consisted of n=1656 children; n=828 twin pairs. There were 252 opposite sex twin pairs and 576 same sex twin pairs (277 male and 299 female twin pairs).
Figure 1.
Eligible cohort and numbers included for analyses. AEDC, Australian Early Development Census; WARDA, Western Australian register of developmental anomalies.
Outcome measure
The AEDC is a national census of early childhood development spanning five developmental domains; (1) Physical Health and Well-being, (2) Social Competence, (3) Emotional Maturity, (4) Language and Cognitive Skills (school-based) and (5) Communication Skills and General Knowledge. The AEDC is conducted every 3 years, with the first national data collection conducted in 2009. Children with scores <10th percentile in a given domain are classified as ‘developmentally vulnerable’ (DV). For this study children who scored >10th percentile for a given domain were classified as ‘not developmentally vulnerable’ (NDV). AEDC cut-off scores are based on the first national AEDC data collection in 2009 and apply to all AEDC data collections. Domain scores for children with special needs are not included in the AEDC results. In this study, two summarised outcome measures were used; developmentally vulnerable on one or more AEDC domains (DV1) and developmentally vulnerable on two or more AEDC domains (DV2).
Risk variables
Maternal variables
Maternal age and marital status at twins’ birth were obtained from the MNS and Birth Registrations. Maternal occupation at birth was obtained from Birth Registrations data and converted to a four-digit standard code using the Australian and New Zealand Standard Classification of Occupations. These codes were then assigned a value ranging from 0 to 100 using the Australian Socioeconomic Index 2006 (AUSEI06).52 Low AUSEI06 values are representative of low-status occupations and high values represent high-status occupations. This variable was collapsed into two categories: the most disadvantaged quintile (ie, AUSEI06 (0–20)) and greater than the most disadvantaged quintile (ie, AUSEI06 >20). An AUSEI06 value of zero was assigned to records if maternal occupation was reported as ‘unemployed’, ‘stay at home parent’ or ‘pensioner’. For records where maternal occupation was not stated, an AUSEI06 value was not assigned and these cases were reported as missing.
Pregnancy and birth variables
We included several binary pregnancy and birth variables to indicate either the presence or absence; of fertility treatments, smoking during pregnancy, pre-eclampsia, gestational diabetes, threatened abortion, threatened preterm labour, antepartum haemorrhage, placenta praevia, placental abruption, fetal distress, cephalopelvic disproportion, prolapsed cord, precipitate delivery, postpartum haemorrhage (PPH), intubation status, early preterm birth (<34 weeks of gestational age) and time to spontaneous respiration (TSR); with a TSR of ≥2 min forming the ‘at risk’ group, and 5-min Apgar score; with a 5-min Apgar score of <7 forming the ‘at risk’ group.
The proportion of optimal birth weight (POBW) is a measure of fetal growth and is defined as birth weight divided by expected birth weight in the absence of pathologic risk factors. This measure also accounts for non-pathologic determinants of growth, including gestational age, birth order, sex of the child and maternal height,53 and has been validated against ultrasound measurements.54 We derived a binary proxy for fetal growth restriction as POBW <15th percentile, which corresponded to an observed birth weight less than 75.75% of that expected.9
We derived a general category for other pregnancy-related complications (not elsewhere stated; such as urinary tract infection, prelabour rupture of membranes) for all records. As records may have multiple pregnancy-related complications, all records that had a complication that was not elsewhere stated in this study or had multiple complications of which at least one complication was not elsewhere stated in this study, formed the ‘at risk’ group for this variable.
Child variables
Sex and ethnicity of the child were obtained from the MNS and Birth Registrations. Age at the time of AEDC completion and language other than English spoken at home by the child were obtained from the AEDC. Age of children at the time of AEDC completion ranged between ≥3 years 10 months and <6 years 10 months, with a mean of age category of ≥5 years 1 month to 5 years 10 months. To balance frequencies, the age of children at the time of AEDC completion was categorised into three groups: (1) ≥3 years 10 months to <5 years and 1 month, (2) ≥5 years 1 month to <5 years 10 months (reference category) and (3) ≥5 years 10 months to <6 years 10 months.
The total number of siblings was derived as the number of live births to each mother prior to the year that the cohort child had the AEDC conducted. Siblings who died within the neonatal period (ie, mode of separation postbirth from the hospital was death) were excluded in the calculations for the total number of siblings.
Sociodemographic variables
The Index of Relative Socioeconomic Disadvantage (IRSD)19 was calculated using the residential address at the time of birth. ISRD is derived from Australian Census data and reflects area-level disadvantage through variables such as low household income, low educational attainment and high levels of unemployment. This variable was collapsed into two groups: most disadvantaged quintile (ie, ISRD quintile 1) and greater than the most disadvantaged quintile (ie, ISRD quintiles 2–5).
Statistical modelling
For each risk variable, the ‘least risk’ category (eg, not early preterm birth) was used as the reference category (table 1). To estimate the risk of a child being classified as DV1 and DV2, a generalised linear mixed model with a logit link function was used with a random intercept for each twin pair. A total of 30 maternal, pregnancy, birth, child and sociodemographic risk variables were considered for the multivariable models. For DV1, DV2 and each of the five AEDC domains, 24 risk variables were included in the multivariable models; six risk variables were excluded from multivariable analysis due to the prevalence being too small (total n<50 for a given category of a given variable). The variables excluded were: (1) placenta praevia, (2) placental abruption, (3) cephalopelvic disproportion, (4) prolapsed cord, (5) precipitate delivery and (6) a 5-min Apgar score of <7. All variables were added simultaneously to the models. OR and the associated 95% CIs were estimated for both unadjusted and adjusted models. All analyses were undertaken using PROC GLIMMIX in SAS V.9.4 for Windows.55
Table 1.
Risk factors for children who are developmentally vulnerable on one or more AEDC domains (DV1)
| Characteristic | DV1 | NDV1 | Bivariate | Multivariable | ||
| (N=431) | (N=1225) | (N=1352) | ||||
| N (%) | N (%) | OR (95% CI) | P value | aOR (95% CI) | P value | |
| Maternal | ||||||
| Age at time of child’s birth (years) | ||||||
| <25 | 105 (24.36) | 117 (9.55) | 9.66 (3.68 to 25.32) | <0.001 | 7.06 (2.29 to 21.76) | <0.001 |
| 25–29 | 90 (20.88) | 294 (24.00) | 1 (referent) | 1 (referent) | ||
| 30–34 | 130 (30.16) | 476 (38.86) | 0.81 (0.38 to 1.72) | 0.576 | 0.89 (0.38 to 2.07) | 0.780 |
| ≥35 | 106 (24.59) | 338 (27.59) | 1.06 (0.48 to 2.36) | 0.886 | 1.19 (0.47 to 2.99) | 0.715 |
| Overall P value | <0.001 | Overall P value | 0.003 | |||
| Marital status | ||||||
| Married (inc. de facto) | 357 (82.83) | 1123 (91.67) | 1 (referent) | 1 (referent) | ||
| All Other | 72 (16.71) | 98 (8.00) | 5.99 (2.43 to 14.75) | <0.001 | 2.26 (0.76 to 6.71) | 0.140 |
| Unavailable | 2 (0.46) | 4 (0.33) | ||||
| Occupational status scale at time of child’s birth | ||||||
| 0–20 | 122 (28.31) | 187 (15.27) | 5.58 (2.71 to 11.46) | <0.001 | 1.83 (0.79 to 4.26) | 0.159 |
| >20–100 | 279 (64.73) | 1006 (82.12) | 1 (referent) | 1 (referent) | ||
| Unavailable | 30 (6.96) | 32 (2.61) | ||||
| Pregnancy and birth | ||||||
| Fertility treatments | ||||||
| No | 377 (87.47) | 1011 (82.53) | 1 (referent) | 1 (referent) | ||
| Yes | 54 (12.53) | 214 (17.47) | 0.43 (0.19 to 0.97) | 0.042 | 0.84 (0.32 to 2.23) | 0.729 |
| Smoking status during pregnancy | ||||||
| No | 339 (78.65) | 1079 (88.08) | 1 (referent) | 1 (referent) | ||
| Yes | 92 (21.35) | 146 (11.92) | 4.31 (1.95 to 9.53) | <0.001 | 0.87 (0.34 to 2.27) | 0.779 |
| Pre-eclampsia | ||||||
| No | 375 (87.01) | 1085 (88.57) | 1 (referent) | 1 (referent) | ||
| Yes | 56 (12.99) | 140 (11.43) | 1.40 (0.59 to 3.34) | 0.444 | 1.82 (0.68 to 4.88) | 0.237 |
| Gestational diabetes | ||||||
| No | 402 (93.27) | 1152 (94.04) | 1 (referent) | 1 (referent) | ||
| Yes | 29 (6.73) | 73 (5.96) | 1.30 (0.40 to 4.22) | 0.657 | 1.15 (0.33 to 4.09) | 0.826 |
| Threatened abortion | ||||||
| No | 416 (96.52) | 1156 (94.37) | 1 (referent) | 1 (referent) | ||
| Yes | 15 (3.48) | 69 (5.63) | 0.36 (0.09 to 1.45) | 0.151 | 0.23 (0.04 to 1.35) | 0.103 |
| Other pregnancy-related complications | ||||||
| No | 125 (29.00) | 451 (36.82) | 1 (referent) | 1 (referent) | ||
| Yes | 306 (71.00) | 774 (63.18) | 2.08 (1.12 to 3.85) | 0.020 | 1.79 (0.85 to 3.79) | 0.129 |
| Threatened preterm labour | ||||||
| No | 376 (87.24) | 1088 (88.82) | 1 (referent) | 1 (referent) | ||
| Yes | 55 (12.76) | 137 (11.18) | 1.34 (0.55 to 3.24) | 0.519 | 0.68 (0.25 to 1.83) | 0.446 |
| APH | ||||||
| No | 411 (95.36) | 1187 (96.90) | 1 (referent) | 1 (referent) | ||
| Yes | 20 (4.64) | 38 (3.10) | 2.38 (0.53 to 10.73) | 0.260 | 0.67 (0.12 to 3.85) | 0.650 |
| Placenta praevia* | ||||||
| No | 429 (99.54) | 1217 (99.35) | ||||
| Yes | 2 (0.46) | 8 (0.65) | ||||
| Placental abruption* | ||||||
| No | 427 (99.07) | 1223 (99.84) | ||||
| Yes | 4 (0.93) | 2 (0.16) | ||||
| Fetal distress | ||||||
| No | 382 (88.63) | 1136 (92.73) | 1 (referent) | 1 (referent) | ||
| Yes | 49 (11.37) | 89 (7.27) | 2.92 (1.13 to 7.58) | 0.028 | 1.76 (0.60 to 5.13) | 0.301 |
| Cephalopelvic disproportion* | ||||||
| No | 431 (100.00) | 1221 (99.67) | ||||
| Yes | 0 (0.00) | 4 (0.33) | ||||
| Prolapsed cord* | ||||||
| No | 428 (99.30) | 1215 (99.18) | ||||
| Yes | 3 (0.70) | 10 (0.82) | ||||
| Precipitate delivery* | ||||||
| No | 424 (98.38) | 1206 (98.45) | ||||
| Yes | 7 (1.62) | 19 (1.55) | ||||
| PPH ≥500 mL | ||||||
| No | 281 (65.20) | 918 (74.94) | 1 (referent) | 1 (referent) | ||
| Yes | 150 (34.80) | 307 (25.06) | 2.59 (1.39 to 4.82) | 0.003 | 1.52 (0.73 to 3.16) | 0.260 |
| TSR ≥2 min | ||||||
| No | 364 (84.45) | 1060 (86.53) | 1 (referent) | 1 (referent) | ||
| Yes | 67 (15.55) | 165 (13.47) | 1.06 (0.56 to 1.99) | 0.863 | 0.52 (0.22 to 1.21) | 0.128 |
| Apgar 5 min<7* | ||||||
| No | 425 (98.61) | 1198 (97.80) | ||||
| Yes | 6 (1.39) | 27 (2.20) | ||||
| Intubation | ||||||
| No | 353 (81.90) | 1036 (84.57) | 1 (referent) | 1 (referent) | ||
| Yes | 78 (18.10) | 189 (15.43) | 1.36 (0.75 to 2.45) | 0.313 | 1.54 (0.71 to 3.37) | 0.277 |
| Early preterm birth | ||||||
| No | 352 (81.67) | 1058 (86.37) | 1 (referent) | 1 (referent) | ||
| Yes | 79 (18.33) | 167 (13.63) | 2.08 (0.94 to 4.56) | 0.069 | 1.29 (0.53 to 3.15) | 0.579 |
| POBW <15th percentile | ||||||
| No | 305 (70.77) | 926 (75.59) | 1 (referent) | 1 (referent) | ||
| Yes | 81 (18.79) | 136 (11.10) | 2.09 (1.14 to 3.84) | 0.017 | 2.06 (1.07 to 3.98) | 0.031 |
| Unavailable | 45 (10.44) | 163 (13.31) | ||||
| Parity | ||||||
| 0 | 150 (34.80) | 512 (41.80) | 1 (referent) | 1 (referent) | ||
| 1 | 154 (35.73) | 429 (35.02) | 1.62 (0.83 to 3.16) | 0.158 | 1.96 (0.77 to 5.00) | 0.159 |
| ≥2 | 127 (29.47) | 284 (23.18) | 2.50 (1.20 to 5.22) | 0.015 | 2.03 (0.55 to 7.48) | 0.288 |
| Overall P value | 0.048 | Overall P value | 0.351 | |||
| Child | ||||||
| Sex | ||||||
| Female | 176 (40.84) | 674 (55.02) | 1 (referent) | 1 (referent) | ||
| Male | 255 (59.16) | 551 (44.98) | 4.44 (2.68 to 7.36) | <0.001 | 5.08 (2.89 to 8.92) | <0.001 |
| Ethnicity | ||||||
| Other | 385 (89.33) | 1187 (96.90) | 1 (referent) | 1 (referent) | ||
| Indigenous Australian | 46 (10.67) | 38 (3.10) | 16.98 (4.85 to 59.46) | <0.001 | 2.46 (0.46 to 13.03) | 0.291 |
| Child speaks language other than English at home | ||||||
| No | 367 (85.15) | 1149 (93.80) | 1 (referent) | 1 (referent) | ||
| Yes | 64 (14.85) | 76 (6.20) | 6.28 (2.48 to 15.90) | <0.001 | 6.45 (2.17 to 19.17) | <0.001 |
| Age category at time of AEDC completion † | ||||||
| 1 | 109 (25.29) | 212 (17.31) | 2.93 (1.45 to 5.90) | 0.003 | 3.34 (1.55 to 7.22) | 0.002 |
| 2 | 288 (66.82) | 911 (74.37) | 1 (referent) | 1 (referent) | ||
| 3 | 34 (7.89) | 102 (8.33) | 1.18 (0.43 to 3.27) | 0.746 | 0.77 (0.23 to 2.54) | 0.666 |
| Overall P value | 0.011 | Overall P value | 0.006 | |||
| Total number of siblings | ||||||
| 1 | 119 (27.61) | 389 (31.76) | 1 (referent) | 1 (referent) | ||
| 2 | 160 (37.12) | 494 (40.33) | 1.15 (0.58 to 2.30) | 0.685 | 0.70 (0.27 to 1.83) | 0.461 |
| 3 | 74 (17.17) | 240 (19.59) | 1.04 (0.45 to 2.41) | 0.926 | 0.44 (0.13 to 1.55) | 0.120 |
| >3 | 78 (18.10) | 102 (8.33) | 7.28 (2.73 to 19.45) | <0.001 | 2.71 (0.60 to 12.22) | 0.194 |
| Overall P value | <0.001 | Overall P value | 0.025 | |||
| Sociodemographic | ||||||
| Index of relative socioeconomic disadvantage | ||||||
| Lowest quintile | 327 (75.87) | 1046 (85.39) | 3.55 (1.62 to 7.78) | 0.002 | 1.63 (0.66 to 4.02) | 0.287 |
| >Lowest quintile | 87 (20.19) | 150 (12.24) | 1 (referent) | 1 (referent) | ||
| Unavailable | 17 (3.94) | 29 (2.37) | ||||
*Excluded from multivariable analysis due to small N.
†Age categories classified as (1) ≥3 years 10 months to <5 years and 1 month, (2) ≥5 years and 1 month to <5 years and 10 months (reference category), (3) ≥5 years and 10 months to <6 years 10 months.
AEDC, Australian Early Development Census; aOR, adjusted OR; APH, antepartum haemorrhage; DV1, developmentally vulnerable on one or more AEDC domains; NDV1, not developmentally vulnerable on one or more AEDC domains; POBW, proportion of optimal birth weight; PPH, postpartum haemorrhage; TSR, time to spontaneous respiration.
Results
Prevalence of developmental vulnerability in twins
A total of 431 (26.0%) twins were classified as DV1 (table 1). A total of 151 (18.2%) twin pairs had one twin identified as DV1 and 140 (16.9%) twin pairs had both twins were identified as DV1. Of the 24 maternal, pregnancy and birth, child and sociodemographic risk variables considered in the multivariable models, five variables had a statistically significant association with an increased risk of a twin being classified as DV1. In order of decreasing magnitude of associated risk, the ORs were maternal age of <25 years at time of twins’ birth (adjusted OR (aOR): 7.06, 95% CI: 2.29 to 21.76), child speaks a language other than English at home (aOR: 6.45, 95% CI: 2.17 to 19.17), male twins (aOR: 5.08, 95% CI: 2.89 to 8.92), child’s age younger than the reference category for the study sample (≥5 years 1 month to 5 years 7 months) at the time of AEDC completion (aOR: 3.34, 95% CI: 1.55 to 7.22) and POBW <15th percentile (aOR: 2.06, 95% CI: 1.07 to 3.98). There was a statistically significant association between an increased risk of a twin being classified as DV1 and maternal age at the time of twins’ birth (p=0.003), age category at time of ADEC completion (p=0.006) and the total number of sibling (p=0.0248).
A total of 223 (13.5%) twins were classified as DV2 (table 2). In 95 (11.5%) twin pairs, one twin was identified as DV2 and in 64 twin pairs (7.7%), both twins were identified as DV2. Of the 24 maternal, pregnancy and birth, child and sociodemographic risk variables considered in the adjusted models, seven variables had a statistically significant association with an increased risk of a twin being classified as DV2. Risk factors for DV2 were, in order of decreasing magnitude, male twins (aOR: 7.87, 95% CI: 3.45 to 17.97), maternal age of <25 years at time of twins’ birth (aOR: 5.60, 95% CI: 1.30 to 24.10), child’s age younger than the reference category at time of AEDC completion (aOR: 5.36, 95% CI: 1.94 to 14.82), child speaking a language other than English at home (aOR: 4.65, 95% CI: 1.14 to 19.03), mother’s marital status as not married at the time of twins’ birth (aOR: 4.59, 95% CI: 1.13 to 18.55), maternal occupation status in the lowest quintile (aOR: 3.30, 95% CI: 1.11 to 9.81) and POBW <15th percentile (aOR: 3.11, 95% CI: 1.26 to 7.64). There was a statistically significant association between an increased risk of a twin being classified as DV2 and the age category at the time of ADEC completion (p=0.001).
Table 2.
Risk factors for children who are developmentally vulnerable on two or more AEDC domains (DV2)
| Characteristic | DV2 | NDV2 | Bivariate | Multivariable | ||
| (N=223) | (N=1433) | (N=1352) | ||||
| N (%) | N (%) | OR (95% CI) | P value | aOR (95% CI) | P value | |
| Maternal | ||||||
| Age at time of child’s birth (years) | ||||||
| <25 | 63 (28.25) | 159 (11.10) | 7.81 (2.60 to 23.45) | <0.001 | 5.60 (1.30 to 24.10) | 0.021 |
| 25–29 | 48 (21.52) | 336 (23.45) | 1 (referent) | 1 (referent) | ||
| 30–34 | 64 (28.70) | 542 (37.82) | 0.65 (0.26 to 1.63) | 0.356 | 0.92 (0.29 to 2.91) | 0.885 |
| ≥35 | 48 (21.52) | 396 (27.63) | 0.67 (0.25 to 1.81) | 0.434 | 0.77 (0.22 to 2.76) | 0.689 |
| Overall P value | <0.001 | Overall P value | 0.072 | |||
| Marital status | ||||||
| Married (inc. de facto) | 172 (77.13) | 1308 (91.28) | 1 (referent) | 1 (referent) | ||
| All other | 49 (21.97) | 121 (8.44) | 9.91 (3.54 to 27.77) | <0.001 | 4.59 (1.13 to 18.55) | 0.033 |
| Unavailable | 2 (0.90) | 4 (0.28) | ||||
| Occupational status scale at time of child’s birth | ||||||
| 0–20 | 78 (34.98) | 231 (16.12) | 8.82 (3.72 to 20.89) | <0.001 | 3.30 (1.11 to 9.81) | 0.032 |
| >20–100 | 130 (58.30) | 1155 (80.60) | 1 (referent) | 1 (referent) | ||
| Unavailable | 15 (6.73) | 47 (3.28) | ||||
| Pregnancy and birth | ||||||
| Fertility treatments | ||||||
| No | 200 (89.69) | 1188 (82.90) | 1 (referent) | 1 (referent) | ||
| Yes | 23 (10.31) | 245 (17.10) | 0.35 (0.13 to 0.97) | 0.042 | 0.67 (0.17 to 2.69) | 0.567 |
| Smoking status during pregnancy | ||||||
| No | 166 (74.44) | 1252 (87.37) | 1 (referent) | 1 (referent) | ||
| Yes | 57 (25.56) | 181 (12.63) | 5.83 (2.32 to 14.65) | <0.001 | 1.27 (0.38 to 4.30) | 0.700 |
| Pre-eclampsia | ||||||
| No | 195 (87.44) | 1265 (88.28) | 1 (referent) | 1 (referent) | ||
| Yes | 28 (12.56) | 168 (11.72) | 1.25 (0.41 to 3.86) | 0.693 | 2.45 (0.65 to 9.17) | 0.184 |
| Gestational diabetes | ||||||
| No | 208 (93.27) | 1346 (93.93) | 1 (referent) | 1 (referent) | ||
| Yes | 15 (6.73) | 87 (6.07) | 1.44 (0.32 to 6.42) | 0.635 | 2.29 (0.46 to 11.44) | 0.312 |
| Threatened abortion | ||||||
| No | 214 (95.96) | 1358 (94.77) | 1 (referent) | 1 (referent) | ||
| Yes | 9 (4.04) | 75 (5.23) | 0.54 (0.10 to 2.94) | 0.478 | 0.24 (0.02 to 3.08) | 0.274 |
| Other pregnancy related complications | ||||||
| No | 57 (25.56) | 519 (36.22) | 1 (referent) | 1 (referent) | ||
| Yes | 166 (74.44) | 914 (63.78) | 2.64 (1.22 to 5.69) | 0.014 | 1.64 (0.58 to 4.61) | 0.351 |
| Threatened preterm labour | ||||||
| No | 191 (85.65) | 1273 (88.83) | 1 (referent) | 1 (referent) | ||
| Yes | 32 (14.35) | 160 (11.17) | 2.04 (0.66 to 6.29) | 0.216 | 0.72 (0.20 to 2.61) | 0.613 |
| APH | ||||||
| No | 209 (93.72) | 1389 (96.93) | 1 (referent) | 1 (referent) | ||
| Yes | 14 (6.28) | 44 (3.07) | 5.96 (0.95 to 37.40) | 0.057 | 1.45 (0.36 to 5.87) | 0.599 |
| Placenta praevia* | ||||||
| No | 223 (100.00) | 1423 (99.30) | ||||
| Yes | 0 (0.00) | 10 (0.70) | ||||
| Placental abruption* | ||||||
| No | 221 (99.10) | 1429 (99.72) | ||||
| Yes | 2 (0.90) | 4 (0.28) | ||||
| Fetal distress | ||||||
| No | 195 (87.44) | 1323 (92.32) | 1 (referent) | 1 (referent) | ||
| Yes | 28 (12.56) | 110 (7.68) | 3.03 (0.90 to 10.23) | 0.074 | 1.56 (0.59 to 4.15) | 0.368 |
| Cephalopelvic disproportion* | ||||||
| No | 223 (100.00) | 1429 (99.72) | ||||
| Yes | 0 (0.00) | 4 (0.28) | ||||
| Prolapsed cord* | ||||||
| No | 220 (98.65) | 1423 (99.30) | ||||
| Yes | 3 (1.35) | 10 (0.70) | ||||
| Precipitate delivery* | ||||||
| No | 219 (98.21) | 1411 (98.46) | ||||
| Yes | 4 (1.79) | 22 (1.54) | ||||
| PPH ≥500 mL | ||||||
| No | 141 (63.23) | 1058 (73.83) | 1 (referent) | 1 (referent) | ||
| Yes | 82 (36.77) | 375 (26.17) | 3.43 (1.49 to 7.94) | 0.004 | 1.38 (0.16 to 11.79) | 0.766 |
| TSR ≥2 min | ||||||
| No | 183 (82.06) | 1241 (86.60) | 1 (referent) | 1 (referent) | ||
| Yes | 40 (17.94) | 192 (13.40) | 1.78 (0.81 to 3.89) | 0.149 | 0.91 (0.30 to 2.72) | 0.863 |
| Apgar 5 min<7* | ||||||
| No | 219 (98.21) | 1404 (97.98) | ||||
| Yes | 4 (1.79) | 29 (2.02) | ||||
| Intubation | ||||||
| No | 178 (79.82) | 1211 (84.51) | 1 (referent) | 1 (referent) | ||
| Yes | 45 (20.18) | 222 (15.49) | 1.91 (0.90 to 4.05) | 0.093 | 1.53 (0.54 to 4.35) | 0.429 |
| Early preterm birth | ||||||
| No | 172 (77.13) | 1238 (86.39) | 1 (referent) | 1 (referent) | ||
| Yes | 51 (22.87) | 195 (13.61) | 4.18 (1.50 to 11.67) | 0.006 | 2.06 (0.64 to 6.58) | 0.224 |
| POBW <15th percentile | ||||||
| No | 162 (72.65) | 1069 (74.60) | 1 (referent) | 1 (referent) | ||
| Yes | 42 (18.83) | 175 (12.21) | 2.72 (1.25 to 5.93) | 0.012 | 3.11 (1.26 to 7.64) | 0.014 |
| Unavailable | 19 (8.52) | 189 (13.19) | ||||
| Parity | ||||||
| 0 | 79 (35.43) | 583 (40.68) | 1 (referent) | 1 (referent) | ||
| 1 | 73 (32.74) | 510 (35.59) | 1.18 (0.51 to 2.76) | 0.700 | 1.12 (0.31 to 4.04) | 0.861 |
| ≥2 | 71 (31.84) | 340 (23.73) | 2.66 (1.04 to 6.83) | 0.042 | 3.61 (0.61 to 21.22) | 0.155 |
| Overall P value | 0.109 | Overall P value | 0.283 | |||
| Child | ||||||
| Sex | ||||||
| Female | 83 (37.22) | 767 (53.52) | 1 (referent) | 1 (referent) | ||
| Male | 140 (62.78) | 666 (46.48) | 5.42 (2.79 to 10.55) | <0.001 | 7.87 (3.45 to 17.97) | <0.001 |
| Ethnicity | ||||||
| Other | 197 (88.34) | 1375 (95.95) | 1 (referent) | 1 (referent) | ||
| Indigenous Australian | 26 (11.66) | 58 (4.05) | 11.00 (2.78 to 43.60) | <0.001 | 2.32 (0.32 to 16.84) | 0.404 |
| Child speaks language other than English at home | ||||||
| No | 192 (86.10) | 1324 (92.39) | 1 (referent) | 1 (referent) | ||
| Yes | 31 (13.90) | 109 (7.61) | 3.19 (0.96 to 10.63) | 0.059 | 4.65 (1.14 to 19.03) | 0.033 |
| Age category at time of AEDC completion | ||||||
| 1 | 66 (29.60) | 255 (17.79) | 4.11 (1.80 to 9.39) | <0.001 | 5.36 (1.94 to 14.82) | 0.001 |
| 2 | 142 (63.68) | 1057 (73.76) | 1 (referent) | 1 (referent) | ||
| 3 | 15 (6.73) | 121 (8.44) | 0.95 (0.26 to 3.46) | 0.942 | 0.28 (0.05 to 1.70) | 0.167 |
| Overall P value | 0.003 | Overall P value | 0.001 | |||
| Total number of siblings | ||||||
| 1 | 58 (26.01) | 450 (31.40) | 1 (referent) | 1 (referent) | ||
| 2 | 84 (37.67) | 570 (39.78) | 1.35 (0.57 to 3.19) | 0.489 | 1.26 (0.34 to 4.71) | 0.733 |
| 3 | 38 (17.04) | 276 (19.26) | 1.14 (0.40 to 3.24) | 0.810 | 0.47 (0.08 to 2.70) | 0.395 |
| >3 | 43 (19.28) | 137 (9.56) | 7.14 (2.24 to 22.72) | <0.001 | 2.52 (0.34 to 18.73) | 0.366 |
| Overall P value | 0.006 | Overall P value | 0.175 | |||
| Sociodemographic | ||||||
| Index of relative socioeconomic disadvantage | ||||||
| Lowest quintile | 175 (78.48) | 1198 (83.60) | 2.14 (0.76 to 6.02) | 0.151 | 0.68 (0.21 to 2.25) | 0.529 |
| >Lowest quintile | 39 (17.49) | 198 (13.82) | 1 (referent) | 1 (referent) | ||
| Unavailable | 9 (4.04) | 37 (2.58) | ||||
All bold face values are statistically signficant.
*Excluded from multivariable analysis due to small N.
†Age categories classified as: (1) ≥3 years 10 months to <5 years and 1 month, (2) ≥5 years and 1 month to <5 years and 10 months (reference category), (3) ≥5 years and 10 months to <6 years 10 months.
AEDC, Australian Early Development Census; aOR, adjusted OR; APH, antepartum haemorrhage; DV2, developmentally vulnerable on two or more AEDC domains; NDV2, not developmentally vulnerable on two or more AEDC domains; POBW, proportion of optimal birth weight; PPH, postpartum haemorrhage; TSR, time to spontaneous respiration.
Associations with domain-specific developmental vulnerability
A total of 188 (11.4%) children were classified as DV for the domains of: Physical Health and Well-being, 151 (9.1%) for Social Competence, 147 (8.9%) for Emotional Maturity, 195 (11.8%) for Language and Cognitive Skills (school-based) and 200 (12.1%) for Communication Skills and General Knowledge (see online supplemental tables 1–5, respectively). These results were broadly consistent with the findings for the aggregate measures of developmental vulnerability (DV1 and DV2). All variables that were statistically significant in the aggregated measures of developmental vulnerability were statistically significant for the domains.
bmjopen-2020-038846supp001.pdf (190.5KB, pdf)
Discussion
This study examined the associations between biological and sociodemographic risk factors and developmental vulnerability in twins in their first year of full-time school. To the best of our knowledge, our study is the first of this scale (population-level sample of twins; n>1600) to report on the prevalence of developmental vulnerabilities, in an otherwise healthy sample of twins, at the time of their first year of full-time school. As studies have reported that twins are more likely to have poorer performance, in comparison to singletons, at the age of 2,10 11 it was pertinent to assess if the prevalence rates of developmental vulnerabilities are higher in twins at age 5. We reported that in the WA population, 26.0% of twins were classified as DV1 and 13.5% as DV2 across the 2009, 2012 and 2015 AEDC cycles. In the general WA population, which includes twins and higher order multiples, 23.0% of children were classified as DV1 and 11.3% of children were classified as DV2, across these AEDC cycles.50 A large cohort study of 99 530 singleton children from New South Wales reported that 20.8% were classified as DV1 across the 2009 and 2012 AEDC cycles.56 Thus, we found that twins are at an elevated risk of developmental vulnerability relative to a general population of children in the state of WA and in a singleton population in New South Wales. This is consistent with findings from a study of 142 twin pairs from the Louisville Twin Study that reported twins scored lower than singletons in both the Verbal and Performance IQ domains of the Wechsler Preschool and Primary Scale of Intelligence at both 4 and 5 years of age.38 As our results were obtained from a sample of twins without any diagnosed developmental disabilities, the higher prevalence rates of twins being classified as DV1 and DV2 observed in our study, when compared with the general Australian population, suggests that healthy twins are more likely to be classified as DV on AEDC domains at school starting age when compared with their singleton counterparts.
The biological factors associated with developmental vulnerability in twins were male sex, fetal growth restriction and younger chronological age at the time of AEDC completion. These results are in line with singleton studies31 57 which have reported that male children are more likely to be classified as DV in their first year of full-time school, in comparison to female children. A study conducted in South Australia of 13 827 children, of which 3.4% were twins, also reported that male twins were more likely to be classified as DV2 when compared with female twins, however, this finding was not statistically significant.58 The Louisville Twin Study also reported sex differences, with females scoring higher on Full Scale, Verbal and Performance IQ than males at ages 4 and 5, however, scores tended to converge at 6 years of age.38
We also reported that twins younger than the reference category for this sample were more likely to be classified as DV in their first year of full-time school. A study of 840 Canadian 5-year-old twins, aiming to assess the genetic and environmental factors influencing school readiness, reported that in the preliminary models age was positively correlated with the spatial recognition, numbers and letters components of the Lollipop test.59 Furthermore, a recent discussion paper identified the need for further research to assess the effects of delaying school entry for twins60 thus, highlighting that further research is required to better understand if delaying school entry is beneficial for both short-term and long-term academic outcomes in twins.
The sociodemographic risk factors associated with developmental vulnerability in twins included maternal age, maternal occupational status and a not married maternal marital status, at the time of twins’ birth, and the child speaking a language other than English at home. These results are supported by the South Australian study, which examined a range of variables also included in our study.58 This study reported that maternal age, marital status and maternal occupation were associated with an increased risk of children being classified as DV2 on the AEDC.58 The South Australian study also reported that parity and smoking during pregnancy were associated with an increased risk of children being classified as DV2.58 In our study, we observed an increased but statistically insignificant association between these risk variables and twins being classified as either DV1 or DV2.
An interesting finding from our study was that speaking a language other than English at home was associated with an increased risk for twins being classified as DV1 and DV2. Previous studies have reported that approximately a fifth of Australian children are bilingual,61 and the prevalence of twins speaking a language other than English at home in our study were in line with these results. Results from an Australia-wide study of 261 147 children (including singletons and multiples) from the 2009 AEDC cycle reported that bilingual children proficient in English have an equal or slightly lower odds of being classed as DV1 when compared with their English-speaking background peers.61 However, unlike our study, this study61 did not report differences in developmental vulnerability based on plurality. Additionally, a Canadian study examining the school readiness profiles of 95 537 children in British Columbia62 reported that bilingualism was associated with positive social, emotional and cognitive development, as measured by the Early Development Index.34 Differences in results may be attributed to the fact bilingualism may be a risk factor for twins, however, it may not be a significant risk factor in a general population sample. The language groups most commonly spoken in WA after English (Mandarin, Italian and Vietnamese)63 are different to those most prevalent in British Colombia (Punjabi, Chinese and German).64 Thus, the difference in findings between the Canadian study and our results may be attributable to this fact.
Our findings have some accord with a cohort study examining the associations between biological and sociodemographic risk factors on late language emergence in 473 twins pairs at the age of 2.9 Taylor et al reported that the risk factors for late language emergence in twins, without developmental disabilities, include fetal growth restriction.9 Interestingly, our study also identified fetal growth restriction as a risk factor for developmental vulnerability at age 5, suggesting that the biological implications of a suboptimal intrauterine environment may persist beyond infancy and into early childhood in twins not diagnosed developmental disabilities. In contrast to our study, the Taylor et al twin sample excluded twins with exposure to languages other than English. This study reported that sociodemographic risk factors (low maternal education, socioeconomic area disadvantage) were not associated with late language emergence at age 2. Our results suggest that sociodemographic factors including maternal, age, marital status and occupational status, at time of twins’ birth and the child speaking a language other than English at home are associated with an increased risk of developmental vulnerability at age 5.9 The differences in findings between this study and our study suggest that sociodemographic characteristics may play a more significant role as risk variables at age 5 compared with at the age of 2. This hypothesis is supported by a subsequent study of twins aged 4 and 6, which reported that higher maternal education and older maternal age showed positive effects on language and non-verbal phenotypes.6 Furthermore, a study of a twin sample from the Quebec Newborn Twin Study reported that environmental factors, such as socioeconomic status, rather than genetic factors were attributable to the predictive association observed between early language skills and school readiness, as measured by the Lollipop Test, in twins 63 months of age.45 In our study, the zygosity of twins could not be established as WA administrative data do not contain information on zygosity. Furthermore, we did not aim to assess the impact of within twin-pair discordance in regard to developmental vulnerabilities at age 5. Thus, further research is required to better elucidate the impact and interplay of biological and sociodemographic risk variables at different stages of development in twins.
Studies assessing twin-singleton differences often control for or select for factors such as prematurity, low birth weight or parental socioeconomic status.57 65 66 Our study, however, draws attention to the adverse effects of other risk factors, including POBW and maternal marital status, on child development outcomes at age 5. An Australian cohort study of 1922 children from the Northern Territory using linked administrative data, reported an increased, but non-statistically significant, risk of twins being classified as DV1 on the AEDC, after controlling for a range of biological and sociodemographic variables used in our study including sex, 5-min Apgar score <7, area remoteness, ethnicity, child speaks a language other than English at home and maternal age at the time of the child’s birth.57 Although this study gave consideration to plurality as a risk factor for developmental vulnerability, it did not aim to assess the association between a comprehensive set of biological and sociodemographic risk factors. A Canadian study of 5-year-old twins reported that shared environmental factors substantially accounted for cognitive school readiness (as measured by the Lollipop Test) as compared with genetic effects.59 Likewise, other studies have also reported that a range of family factors, which would be assumed to be shared by both twins, such as family income, maternal occupation and employment status are associated with cognitive school readiness.67 68 Further studies in this area are required, as the extent and nature of the risk factors associated with developmental vulnerability at age 5 in twins remain not well established.
Preventative intervention studies have reported that programmes designed to improve school readiness and high-quality early childhood education and care, are effective for at-risk populations and can have significant long-term results.69 70 The higher prevalence rates of DV1 and DV2 in twins observed in this study are indicative of the fact that twins form an at-risk group in terms of developmental vulnerability at the time at which children commence full-time school. Therefore, it is pertinent for those working in the early childhood education sector and for parents to be aware of the developmental vulnerabilities present in twins at the age at which children begin full-time school. In Australia, there has been a call to provide increased quantity and quality of support service and resources for twins and their families due to increased vulnerability,60and the results of our study highlight this need.
Conclusions
Both biological and sociodemographic risk factors are associated with developmental vulnerability at the age of 5 in twins. The findings of our study suggest that twins are more likely to be classified as DV at school starting age when compared with their singleton counterparts. In particular, the results draw attention to the hypothesis that prenatal, and more significantly perinatal, risk factors and the sociodemographic environments in which twins are raised can impact developmental vulnerability in early childhood.
Supplementary Material
Acknowledgments
We gratefully acknowledge the Western Australia (WA) Data Linkage Branch and the data custodians who provided data for this study and the people of WA for the use of their administrative data. This study does not necessarily reflect their views. This study uses data from the Australian Early Development Census (AEDC). The AEDC is funded by the Australian Government Department of Education and Training. The findings and views reported are those of the authors and should not be attributed to the Department or the Australian Government.
Footnotes
Contributors: GKD: led study conceptualisation and design, conducted the literature review, performed data manipulation, analysis and interpretation of findings, drafted the initial manuscript and reviewed and revised the manuscript critically for important intellectual content. DC, GP and CLT: contributed to the study inception, the development of the design, interpretation of the results, manuscript revisions, the interpretation of the results and revised the manuscript critically for important intellectual content. GKD, DC, GP and CLT approved the final manuscript as submitted and agreed to be accountable for all aspects of the work.
Funding: This study was supported by National Health and Medical Research Grants (GNT1173991 and GNT1099655 to GP), the Research Council of Norway through its Centres of Excellence funding scheme (#262700 to GP) and the Australian Research Council Centre of Excellence for Children and Families over the Life Course (CE140100027 to CLT and DC). GKD was supported by the ARC Centre of Excellence for Children and Families over the Life Course Scholarship, the ARC Centre of Excellence for Children and Families over the Life Course Top-Up Scholarship and the Stan and Jean Perron Top-Up Scholarship.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting or dissemination plans of this research.
Patient consent for publication: Not required.
Ethics approval: Ethics approval for this study was granted by the Western Australian Department of Health Human Research Ethics Committee (2016/51) and the University of Western Australia Human Research Ethics Committee (RA/4/20/4776).
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: No data are available. The linked administrative data are owned by the government departments who approved the linkage and use of the data for this study. Use of the study data is restricted to named researchers. The current Human Research Ethics Committee approvals were obtained for public sharing and presentation of data on group level only, meaning the data used in this study cannot be shared by the authors. Collaborative research may be conducted according to the ethical requirements and relevant privacy legislations. Potential collaborators should contact author GP with their expression of interest. The steps involved in seeking permission for linkage and use of the data used in this study are the same for all researchers.
References
- 1.Umstad MP, Gronow MJ. Multiple pregnancy: a modern epidemic? Med J Aust 2003;178:613–5. 10.5694/j.1326-5377.2003.tb05384.x [DOI] [PubMed] [Google Scholar]
- 2.Marlow N, Roberts BL, Cooke RW. Motor skills in extremely low birthweight children at the age of 6 years. Arch Dis Child 1989;64:839–47. 10.1136/adc.64.6.839 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Riese M. Risk and early development: findings from the louisville twin study : Blickstein I, Keith LG, Multiple pregnancy: epidemiology, gestation, and perinatal outcome. 2nd edn CRC Press, 2005. [Google Scholar]
- 4.Births, Australia 2015, 2015Australian Bureau of Statistics Canberra; Available: http://www.abs.gov.au/AUSSTATS/abs@.nsf/Previousproducts/3301.0Main%20Features32015?opendocument&tabname=Summary&prodno=3301.0&issue=2015&num=&view= [Google Scholar]
- 5.Australian Institute of Health and Welfare Perinatal deaths in Australia 2013–2014. Canberra, 2018. [Google Scholar]
- 6.Rice ML, Zubrick SR, Taylor CL, et al. Longitudinal study of language and speech of twins at 4 and 6 years: twinning effects decrease, zygosity effects disappear, and heritability increases. J Speech Lang Hear Res 2018;61:79–93. 10.1044/2017_JSLHR-L-16-0366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fuchs F, Senat M-V. Multiple gestations and preterm birth. Semin Fetal Neonatal Med 2016;21:113–20. 10.1016/j.siny.2015.12.010 [DOI] [PubMed] [Google Scholar]
- 8.Yokoyama Y, Shimizu T, Hayakawa K. Prevalence of cerebral palsy in twins, triplets and quadruplets. Int J Epidemiol 1995;24:943–8. 10.1093/ije/24.5.943 [DOI] [PubMed] [Google Scholar]
- 9.Taylor CL, Rice ML, Christensen D, et al. Prenatal and perinatal risks for late language emergence in a population-level sample of twins at age 2. BMC Pediatr 2018;18:41. 10.1186/s12887-018-1035-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Taylor CL, Zubrick SR, Christensen D. Multiple risk exposures for reading achievement in childhood and adolescence. J Epidemiol Community Health 2019;73:427–34. 10.1136/jech-2018-211323 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nan C, Piek J, Warner C, et al. Trajectories and predictors of developmental skills in healthy twins up to 24 months of age. Infant Behav Dev 2013;36:670–8. 10.1016/j.infbeh.2013.07.003 [DOI] [PubMed] [Google Scholar]
- 12.DiLalla LF. Social development of twins. Twin Res Hum Genet 2006;9:95–102. 10.1375/twin.9.1.95 [DOI] [PubMed] [Google Scholar]
- 13.Bronfenbrenner U. Making human beings human: Bioecological perspectives on human development. Thousand Oaks, California: Sage Publications, Inc, 2005. [Google Scholar]
- 14.Fox SE, Levitt P, Nelson CA. How the timing and quality of early experiences influence the development of brain architecture. Child Dev 2010;81:28–40. 10.1111/j.1467-8624.2009.01380.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Barker DJP. The developmental origins of adult disease. J Am Coll Nutr 2004;23:588S–95. 10.1080/07315724.2004.10719428 [DOI] [PubMed] [Google Scholar]
- 16.Bradley RH, Corwyn RF. Socioeconomic status and child development. Annu Rev Psychol 2002;53:371–99. 10.1146/annurev.psych.53.100901.135233 [DOI] [PubMed] [Google Scholar]
- 17.Howard K, Roberts G, Lim J, et al. Biological and environmental factors as predictors of language skills in very preterm children at 5 years of age. J Dev Behav Pediatr 2011;32:239–49. 10.1097/DBP.0b013e31820b7882 [DOI] [PubMed] [Google Scholar]
- 18.Msall ME, Buck GM, Rogers BT, et al. Kindergarten readiness after extreme prematurity. Am J Dis Child 1992;146:1371–5. 10.1001/archpedi.1992.02160230129033 [DOI] [PubMed] [Google Scholar]
- 19.Roberts G, Lim J, Doyle LW, et al. High rates of school readiness difficulties at 5 years of age in very preterm infants compared with term controls. J Dev Behav Pediatr 2011;32:117–24. 10.1097/DBP.0b013e318206d5c9 [DOI] [PubMed] [Google Scholar]
- 20.Shah PE, Kaciroti N, Richards B, et al. Gestational age and kindergarten school readiness in a national sample of preterm infants. J Pediatr 2016;178:61–7. 10.1016/j.jpeds.2016.06.062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chen J-H, Claessens A, Msall ME. Prematurity and school readiness in a nationally representative sample of Australian children: does typically occurring preschool moderate the relationship? Early Hum Dev 2014;90:73–9. 10.1016/j.earlhumdev.2013.09.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Poulsen G, Wolke D, Kurinczuk JJ, et al. Gestational age and cognitive ability in early childhood: a population-based cohort study. Paediatr Perinat Epidemiol 2013;27:371–9. 10.1111/ppe.12058 [DOI] [PubMed] [Google Scholar]
- 23.Quigley MA, Poulsen G, Boyle E, et al. Early term and late preterm birth are associated with poorer school performance at age 5 years: a cohort study. Arch Dis Child Fetal Neonatal Ed 2012;97:F167–73. 10.1136/archdischild-2011-300888 [DOI] [PubMed] [Google Scholar]
- 24.Patrianakos-Hoobler AI, Msall ME, Huo D, et al. Predicting school readiness from neurodevelopmental assessments at age 2 years after respiratory distress syndrome in infants born preterm. Dev Med Child Neurol 2010;52:379–85. 10.1111/j.1469-8749.2009.03343.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McCormick MC, Brooks-Gunn J, Workman-Daniels K, et al. The health and developmental status of very low-birth-weight children at school age. JAMA 1992;267:2204–8. 10.1001/jama.1992.03480160062035 [DOI] [PubMed] [Google Scholar]
- 26.Reichman NE. Low birth weight and school readiness. Future Child 2005;15:91–116. 10.1353/foc.2005.0008 [DOI] [PubMed] [Google Scholar]
- 27.Roth J, Figlio DN, Chen Y, et al. Maternal and infant factors associated with excess kindergarten costs. Pediatrics 2004;114:720–8. 10.1542/peds.2003-1028-L [DOI] [PubMed] [Google Scholar]
- 28.Avchen RN, Scott KG, Mason CA. Birth weight and school-age disabilities: a population-based study. Am J Epidemiol 2001;154:895–901. 10.1093/aje/154.10.895 [DOI] [PubMed] [Google Scholar]
- 29.Noeker M. Neurocognitive development in children experiencing intrauterine growth retardation and born small for gestational age: pathological, constitutional and therapeutic pathways. Horm Res Paediatr 2005;64:83–8. 10.1159/000089322 [DOI] [PubMed] [Google Scholar]
- 30.de Bie HMA, Oostrom KJ, Delemarre-van de Waal HA. Brain development, intelligence and cognitive outcome in children born small for gestational age. Horm Res Paediatr 2010;73:6–14. 10.1159/000271911 [DOI] [PubMed] [Google Scholar]
- 31.Janus M, Duku E. The school entry gap: socioeconomic, family, and health factors associated with children's school readiness to learn. Early Educ Dev 2007;18:375–403. 10.1080/10409280701610796a [DOI] [Google Scholar]
- 32.Mendez LMR, Mihalas ST, Hardesty R. Gender differences in academic development and performance, 2006. [Google Scholar]
- 33.Angenent H, Man Ade, De Man A. Intelligence, gender, social maturity, and school readiness in Dutch FIRSTGRADERS. Soc Behav Pers 1989;17:205–9. 10.2224/sbp.1989.17.2.205 [DOI] [Google Scholar]
- 34.Janus M, Offord DR. Development and psychometric properties of the early development instrument (EDI): a measure of children's school readiness. Can J Behav Sci 2007;39:1–22. 10.1037/cjbs2007001 [DOI] [Google Scholar]
- 35.Martin JA, Hamilton BE, Ventura SJ, et al. Births: final data for 2009. Natl Vital Stat Rep 2011;60:1–70. [PubMed] [Google Scholar]
- 36.Puccio G, Giuffré M, Piccione M, et al. Intrauterine growth pattern and birthweight discordance in twin pregnancies: a retrospective study. Ital J Pediatr 2014;40:43. 10.1186/1824-7288-40-43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lorenz JM. Neurodevelopmental outcomes of twins. Semin Perinatol 2012;36:201–12. 10.1053/j.semperi.2012.02.005 [DOI] [PubMed] [Google Scholar]
- 38.Wilson RS. Twins: patterns of cognitive development as measured on the Wechsler preschool and primary scale of intelligence. Dev Psychol 1975;11:126–34. 10.1037/h0076458 [DOI] [Google Scholar]
- 39.Schools HJ. Skills, and synapses. Econ Inq 2008;46:289–324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Entwisle DR, Alexander KL. Entry into school: the beginning school transition and educational stratification in the United States. Annu Rev Sociol 1993;19:401–23. 10.1146/annurev.so.19.080193.002153 [DOI] [Google Scholar]
- 41.Friend A, DeFries JC, Olson RK, et al. Heritability of high reading ability and its interaction with parental education. Behav Genet 2009;39:427–36. 10.1007/s10519-009-9263-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Harden KP, Turkheimer E, Loehlin JC. Genotype by environment interaction in adolescents’ cognitive aptitude. Behav Genet 2007;37:273–83. 10.1007/s10519-006-9113-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Turkheimer E, Haley A, Waldron M, et al. Socioeconomic status modifies heritability of IQ in young children. Psychol Sci 2003;14:623–8. 10.1046/j.0956-7976.2003.psci_1475.x [DOI] [PubMed] [Google Scholar]
- 44.Rowe DC, Jacobson KC, Van den Oord EJ. Genetic and environmental influences on vocabulary IQ: parental education level as moderator. Child Dev 1999;70:1151–62. 10.1111/1467-8624.00084 [DOI] [PubMed] [Google Scholar]
- 45.Forget-Dubois N, Dionne G, Lemelin J-P, et al. Early child language mediates the relation between home environment and school readiness. Child Dev 2009;80:736–49. 10.1111/j.1467-8624.2009.01294.x [DOI] [PubMed] [Google Scholar]
- 46.Sadeghi N, Gilmore JH, Gerig G. Twin-singleton developmental study of brain white matter anatomy. Hum Brain Mapp 2017;38:1009–24. 10.1002/hbm.23435 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gonski D, Boston K, Greiner K, et al. Review of funding for schooling - final report. Canberra: ACT, 2011. [Google Scholar]
- 48.Australian Institute of Family Studies The longitudinal study of Australian children annual statistical report 2013. Melbourne, 2014. [Google Scholar]
- 49.Begum L, Islam A, Smyth R. Girl power: stipend programs and the education of younger siblings. J Dev Stud 2017;53:1882–98. 10.1080/00220388.2016.1277020 [DOI] [Google Scholar]
- 50.Australian early development census national report 2015. Canberra, Australia, 2016. Available: https://www.aedc.gov.au/Websilk/Handlers/ResourceDocument.ashx?id=45cf2664-db9a-6d2b-9fad-ff0000a141dd
- 51.Holman C D’Arcy J, Bass AJ, Rosman DL, et al. A decade of data linkage in Western Australia: strategic design, applications and benefits of the WA data linkage system. Aust Health Rev 2008;32:766–77. 10.1071/AH080766 [DOI] [PubMed] [Google Scholar]
- 52.McMillan J, Beavis A, Jones F. The AUSEI06:A new socioeconomic index for Australia. J Sociol 2009;45:123–49. [Google Scholar]
- 53.Blair EM, Liu Y, de Klerk NH, et al. Optimal fetal growth for the Caucasian singleton and assessment of appropriateness of fetal growth: an analysis of a total population perinatal database. BMC Pediatr 2005;5:13. 10.1186/1471-2431-5-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Pereira G, Blair E, Lawrence D. Validation of a model for optimal birth weight: a prospective study using serial ultrasounds. BMC Pediatr 2012;12:73. 10.1186/1471-2431-12-73 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.SAS Institute SAS Cary. SAS Institute, 2013. [Google Scholar]
- 56.Falster K, Hanly M, Banks E, et al. Maternal age and offspring developmental vulnerability at age five: a population-based cohort study of Australian children. PLoS Med 2018;15:e1002558. 10.1371/journal.pmed.1002558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Guthridge S, Li L, Silburn S, et al. Early influences on developmental outcomes among children, at age 5, in Australia’s Northern Territory. Early Child Res Q 2016;35:124–34. 10.1016/j.ecresq.2015.12.008 [DOI] [Google Scholar]
- 58.Chittleborough CR, Searle AK, Smithers LG, et al. How well can poor child development be predicted from early life characteristics?: a whole-of-population data linkage study. Early Childhood Res Quarterly 2016;35:19–30. [Google Scholar]
- 59.Lemelin J-P, Boivin M, Forget-Dubois N, et al. The genetic-environmental etiology of cognitive school readiness and later academic achievement in early childhood. Child Dev 2007;78:1855–69. 10.1111/j.1467-8624.2007.01103.x [DOI] [PubMed] [Google Scholar]
- 60.Twins Research Australia (TRA) Multiple perspectives: what support do multiple birth families need to live happy and healthy lives. Melbourne, 2019. [Google Scholar]
- 61.Goldfeld S, O’Connor M, Mithen J, et al. Early development of emerging and English-proficient bilingual children at school entry in an Australian population cohort. Int J Behav Dev 2014;38:42–51. 10.1177/0165025413505945 [DOI] [Google Scholar]
- 62.Guhn M, Gadermann AM, Almas A, et al. Associations of teacher-rated social, emotional, and cognitive development in kindergarten to self-reported wellbeing, peer relations, and academic test scores in middle childhood. Early Child Res Q 2016;35:76–84. 10.1016/j.ecresq.2015.12.027 [DOI] [Google Scholar]
- 63.Australian Bureau of Statistics 2016 census QuickStats Western Australia. Canberra, 2017. Available: https://quickstats.censusdata.abs.gov.au/census_services/getproduct/census/2016/quickstat/5?opendocument
- 64.Statistics Canada Visual census. Ottawa, 2012. Available: http://www12.statcan.gc.ca/census-recensement/2011/dp-pd/vc-rv/index.cfm?Lang=ENG&TOPIC_ID=4&GEOCODE=59 [Accessed 20 Jun 2020].
- 65.Tsou M-T, Tsou M-W, Wu M-P, et al. Academic achievement of twins and singletons in early adulthood: Taiwanese cohort study. BMJ 2008;337:a438. 10.1136/bmj.a438 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Record RG, McKeown T, Edwards JH. An investigation of the difference in measured intelligence between twins and single births. Ann Hum Genet 1970;34:11–20. 10.1111/j.1469-1809.1970.tb00215.x [DOI] [PubMed] [Google Scholar]
- 67.Brooks-Gunn J, Han W-J, Waldfogel J. Maternal employment and child cognitive outcomes in the first three years of life: the NICHD study of early child care. National Institute of child health and human development. Child Dev 2002;73:1052–72. 10.1111/1467-8624.00457 [DOI] [PubMed] [Google Scholar]
- 68.Dearing E, McCartney K, Taylor BA. Change in family income-to-needs matters more for children with less. Child Dev 2001;72:1779–93. 10.1111/1467-8624.00378 [DOI] [PubMed] [Google Scholar]
- 69.Abbott-Shim M, Lambert R, McCarty F. A comparison of school readiness outcomes for children randomly assigned to a head start program and the program’s wait list. J Educat Student Placed at Risk 2003;8:191–214. 10.1207/S15327671ESPR0802_2 [DOI] [Google Scholar]
- 70.Ramey CT, Ramey SL. Early learning and school readiness: can early intervention make a difference? Merrill Palmer Q 2004;50:471–91. 10.1353/mpq.2004.0034 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2020-038846supp001.pdf (190.5KB, pdf)