Abstract
Background:
Posttraumatic stress disorder (PTSD) results in high costs to society, particularly among military personnel. Much is known about PTSD treatments, such as exposure therapies, and their outcomes, but less is known about how treatment might impact social support and PTSD symptoms over the course of treatment.
Methods:
In the current study, soldiers with PTSD (N = 162) were randomized to complete prolonged exposure therapy (either with or without virtual reality) or a waitlist control condition. We examined the impact of treatment on perceived social support as a secondary treatment outcome, as well as associations between social support and PTSD symptoms over time.
Results:
Exposure therapy increased perceived social support at the end of treatment compared to waitlist control, β = 0.43, 95% CI [0.13, 0.73]. Multigroup structural equation modeling using a cross-lagged panel design provided evidence that perceived social support was an antecedent of PTSD symptom improvement for participants engaging in treatment, but not for participants in the waitlist control. Treatment effects on change in PTSD symptoms was mediated by change in perceived social support (B = 1.10, 95% CI [0.20, 3.05]).
Limitations:
The results should be considered in light of limitations, including the characteristics of the sample of active duty soldiers, the measurement of social support and missingess over the course of the study.
Conclusions:
These results suggest that increased perceived social support is a secondary outcome of exposure therapy and may be one pathway through which treatment reduces PTSD symptoms.
Keywords: PTSD, prolonged exposure, social support, avoidance, virtual-reality exposure
Veterans and active duty soldiers are at higher risk for developing posttraumatic stress disorder (PTSD) when compared to U.S. adults broadly (Kilpatrick et al., 2013; Peterson, Luethcke, Borah, & Young-McCaughan, 2011). Prevalence rates are estimated between 2-17% for Vietnam veterans and 4-17% for Iraq veterans (Richardson, Frueh, & Acierno, 2011). PTSD is a particularly costly disorder, resulting in high levels of impairment, negative impacts on mental and physical wellbeing, and high economic costs to society (Kessler, 2000).
Fortunately, there are efficacious treatments that reduce PTSD symptoms, such as prolonged exposure (PE; Foa, Hembree, & Rothbaum, 2007). PE is widely regarded as a frontline treatment for PTSD among U.S. adults broadly, as well as for military populations more specifically (Foa et al., 2018; Forbes et al., 2010; Reger et al., 2016). PE is rooted in emotional processing theory (Foa & Kozak,1986), which posits that the traumatic event is represented in memory as a specific fear structure. Unless processed, the fear structure is easily activated, prompting distress that results in cognitive and behavioral avoidance as a method to reduce this distress. Avoidance prevents processing of the trauma memory and thus, maintains the symptoms of PTSD. Clinically, PE works by countering avoidance to trauma-related stimuli through planned exposures (imaginal and in-vivo), which are thought to facilitate therapeutic emotional processing and a resulting reduction in symptoms.
The experience of PTSD and the treatment of PTSD symptoms both impact—and are impacted by—the social context in which they occur. The perceived availability of others to provide emotional or practical help when needed (Sherbourne & Stewart, 1991) is theorized to play an essential role in the development, maintenance, and treatment of PTSD (Brewin, Andrews, and Valentine, 2000; Koenen et al., 2003; Ozer et al., 2003; Pietrzak et al., 2009; Price et al., 2013; Tsai, Harpaz-Rotem, Pietrzak, & Southwick, 2012). This can include models of social erosion—in which PTSD symptomology reduces the available social support for people with PTSD over time—and social causation, in which having less social support can in turn predict greater PTSD symptoms over time (Shallcross, Arbisi, Polusny, Kramer, & Erbes, 2016).
King and colleagues (2006) found empirical support for the social erosion model; PTSD symptoms predict lower later social support, but not vice versa. The timing of trauma, however, may impact the directionality of these associations. Norris and Kaniasty (2008) found that social support predicted PTSD symptoms in the first 6 months following trauma, whereas PTSD symptoms appear to predict perceived social support following this period. In contrast, Shallcross and colleagues (2016) found the opposite pattern; higher levels of PTSD symptoms predicted lower later perceived social support and perceptions of lower social support predicted greater PTSD symptoms, but only in a later period following the traumatic experience. As highlighted by the authors, this may be due to the different social contexts in which these two studies were conducted—recovery from a natural disaster and following military deployment, respectively.
There is also empirical evidence linking greater perceived social support and positive outcomes for those with PTSD. For example, Koenen and colleagues (2003) followed Vietnam veterans for 14 years post combat and found that greater community involvement predicted lower risk of subsequent PTSD symptoms. Soldiers with higher levels of social support post-deployment also were protected from developing of PTSD (Polusny, Erbes, Murdoch, & Arbisi, 2011) and depressive symptoms after deployment (Pietrzak, Johnson, Goldstein, Malley, & Southwick, 2009).
The interplay between perceived social support and PTSD is also relevant to treatment of PTSD (Markowitz, Milrod, Bleiberg, & Marshall, 2009). Veterans were twice as likely to complete PE and cognitive processing therapy if they reported having loved ones who supported their PTSD treatment by encouraging them to engage in the difficult parts of treatment, and there was evidence that the opposite was true of those whose loved ones accommodated their PTSD (Meis et al., 2019), though these effects for accommodation we not significant in multivariate analyses. Evidence-based treatments, such as cognitive behavioral conjoint therapy (CBCT) for PTSD, can explicitly leverage the benefits of close relationships to treat PTSD (Monson & Fredman, 2012; Monson, Fredman, & Adair, 2008). Similarly, pre-treatment social support from a significant other improves treatment outcomes in CBCT for PTSD (Shnaider, Sijercic, Wanklyn, Suvak, & Monson, 2017). Thrasher and colleagues (2010) found that social support moderated PTSD treatment outcomes. Price and colleagues (2013, 2018) also found that social support at baseline predicted PTSD symptoms at baseline, and that social support predicted treatment response to PE. Furthermore, social support increased across the course of treatment, but this increase was not moderated by PTSD symptom change, suggesting that social support level predicted changes in PTSD treatment, but not vice versa (Price et al., 2018). However, neither of these two studies of PE included a control condition that would allow for direct comparisons between of the impact of PE on the association between social support and PTSD symptoms over time. As a result, it remains unclear how social support may operate as a mediator of change within exposure therapy for PTSD.
Social support is especially relevant in the context of exposure therapies, such as PE. In-vivo exposure exercises could be either supported—or avoidance of distressing and previously avoided situations could be accommodated—by others (Monson et al., 2008; Monson & Fredman, 2012). A partner or friend might be sought out to help facilitate engagement in a feared activity or might simply be present during an in-vivo exercises, such as eating with the patient in a crowded restaurant (Hernandez-Tejada, Acierno, & Sanchez-Carracedo, 2017; Price et al., 2018). In this way, increased social support may also be a secondary outcome of exposure therapy, as suggested by the results of Price and colleagues (2018). To our knowledge, however, longitudinal studies have not examined PTSD symptoms and perceived social support over time within the context of exposure therapies in comparison to a control condition.
The Present Study
To examine the impact of exposure therapy on perceived social support, as well as the time ordering of social support and PTSD symptom improvement during treatment, the current study used a sample of active duty soldiers with PTSD (N = 162) who either completed PE (traditional or VR-assisted) or a waitlist control. We hypothesized that participants who completed the exposure treatments would report significantly greater social support compared to participants in the waitlist control condition. In addition, we hypothesized that greater perceived social support would predict PTSD symptom improvement over time for participants in both treatment conditions, whereas this pattern would not occur for participants in the waitlist control condition. Finally, we hypothesized that changes in perceived social support would mediate the association between treatment and PTSD symptom change.
Method
Participants
Participants were active duty soldiers (N = 162) who participated in a randomized controlled trial evaluating the efficacy of PE with and without virtual reality (Reger et al., 2016). All soldiers were diagnosed with deployment related PTSD according to the Clinician-Administered PTSD Scale (CAPS-IV; Blake et al., 1995), which is based on criteria in the Diagnostic and Statistical Manual of Mental Disorders-Fourth Edition-Text Revision (DSM-IV-TR; American Psychiatric Association, 2000). Participants were predominantly male (n = 156; 96%), with some college education (n = 107; 66%), and White (n = 97; 60%). At the time of the clinical trial, 64% (n =104) of participants were married, 10% (n = 17) were divorced, and 12% (n =19) were separated. Psychiatric medication use at baseline included antidepressants (44%, n = 71), benzodiazepines (24%, n = 39), and other (46%, n = 75). There were no significant differences in demographics by treatment condition. Table 1 includes sample demographics; see Reger and colleagues (2016) for the full demographics and CONSORT diagram from the original trial.
Table 1.
Demographics for Study Variables by Condition
| VR n = 54 |
PE n = 54 |
Control n = 54 |
|
|---|---|---|---|
| Age | 29.5 ± 6.5 | 30.9 ± 7.1 | 30.4 ± 6.5 |
| Sex | 96.3% | 94.4% | 98.1% |
| Married | 63.0% | 72.2% | 57.4% |
| Some college | 53.7% | 59.3% | 48.1% |
| Ethnicity | |||
| Caucasian | 72.2% | 55.6% | 51.9% |
| African American | 3.7% | 9.3% | 14.8% |
| Asian | 7.4% | 5.6% | 5.6% |
| Hispanic | 13.0% | 22.2% | 16.7% |
| Other | 3.8% | 7.5% | 11.2% |
| Baseline perceived social support | 1.76 ± 0.70 | 1.96 ± 0.80 | 1.84 ± 0.75 |
| Mid-treatment perceived social support | 2.04 ± 0.72 | 2.18 ± 0.93 | 1.83 ± 0.78 |
| Post-treatment perceived social support | 2.14 ± 0.95 | 2.46 ± 0.97 | 1.86 ± 0.91 |
| Baseline PTSD symptoms | 80.4 ± 16.2 | 78.3 ± 16.3 | 78.9 ± 16.9 |
| Mid-treatment PTSD symptoms | 71.2 ± 23.3 | 65.0 ± 29.2 | 74.7 ± 21.8 |
| Post-treatment PTSD symptoms | 57.1 ± 32.32 | 44.3 ± 33.7 | 68.1 ± 24.3 |
Note: Data are means ± standard deviations from all available data unless otherwise noted. Married represents the percent married. Some college represents the percent of the sample with some college education. Sex is percentage men. The groups did not significantly vary on any of these variables. Ns were reduced to levels presented in Figure 1 for mid- and post-treatment statistics reported for perceived social support and PTSD symptoms.
Participants were recruited from a large military installation using referrals from health care providers or self-referrals to the study from study recruitment flyers. The study was approved by the local institutional review board and all participants were treated in accordance with established ethical guidelines (American Psychological Association, 2002). Inclusion criteria required that the index trauma be nonsexual and the trauma occurred at least 3-months before the baseline assessment in an environment similar to those available in the Virtual Iraq/Virtual Afghanistan software. Participants also had to agree not to initiate other psychotherapy for PTSD or new psychotropic medications during the treatment phase of the study. Exclusion criteria included a change in the type or strength of psychotropic medications in the last 30 days and hospitalization in the past 6 months for suicidal risk or self-harm, as well as additional criteria fully outlined in prior work (Reger et al., 2016).
Procedure
Participants were randomly assigned to either PE, VR-assisted PE, or a minimal attention waitlist control. Treatment included ten 90 to 120-minute sessions. The VR-assisted PE varied from traditional PE only in that the VR exposures to the trauma memory were used in session in place of traditional imaginal exposures. All homework and in vivo exposure instructions were identical between conditions and followed the published PE treatment manual (Foa et al., 2007). Treatment fidelity, coded by an expert consultant external to the study team, was high in both conditions, as reported in the parent trial (Reger et al., 2016). PTSD symptoms were assessed at the pre-treatment baseline, mid-treatment (after five therapy sessions), and post-treatment (after 10 therapy sessions). Given the lack of significant differences in treatment outcomes for the two exposure therapy groups at post-treatment (Reger et al., 2016), the PE and VR-assisted PE groups were combined (n =108) and compared to the waitlist (n = 54) for the purposes of this study. Notably, we tested all models in the current paper comparing traditional and virtual reality PE directly, and there were no significant differences in the substantive results between these conditions.
Measures
CAPS-IV.
The Clinician-Administered PTSD Scale (CAPS-IV; Blake et al., 1995) is a structured interview for assessing the symptoms and diagnosis of PTSD. Clinicians using the scale assess 17 items related to symptoms of PTSD on a scale from 0 to 4 for both frequency and intensity of symptoms over the past week, with higher scores corresponding to greater PTSD symptoms. Diagnosis was based on “F1/I2/TSEV65” algorithm developed by Weathers and colleagues (1999). The CAPS-IV has been shown to have strong inter-rater reliability, test-retest reliability, and internal consistency (Blake et al., 1995; Hovens et al., 1994). Convergent validity with the Structured Clinical Interview for DSM-IV (SCID) was shown to be .83 for PTSD (Foa & Tolin, 2000). The intraclass correlation for CAPS severity at post assessment for this sample was 0.99, and all time point internal consistencies were acceptable (αs > .70).
BASIS-24.
The revised Behavior and Symptom Identification Scale (BASIS-24) is a brief, self-report measure of patient-rated psychopathology and functioning (Eisen, Normand, Belanger, Gevorkian, & Irvin, 2004). Answers are given for the past week and in a five-item Likert scale ranging from “All of the time” to “None of the time.” The BASIS-24 has six domains; five items make up the domain of interpersonal relationships. These items include: getting along with those in and outside of the family, getting along in social situations, perceived closeness to someone, and feeling they could rely on another in a time of need. Scores on this scale were recoded so that higher scores corresponded to greater perceived social support. The BASIS-24 has been previously well validated (Cameron et al., 2007), and internal consistency reliability for the perceived social support subscale in the current sample was α = .69, .77, and .85, for the baseline, mid-treatment, and post-treatment assessments, respectively.
Data Analysis
In the current study, participants’ self-reported perceived social support—as measured by the BASIS-SS—and PTSD symptoms—as measured by clinician assessment on the CAPS-IV—were assessed at three occasions: baseline, mid treatment, and post treatment. We first examined the effect of PE on social support compared to waitlist control at the mid and post assessment using multiple regression. Treatment condition was coded control = 0 and exposure therapy = 1 in all models. All regression model results predicting mid- and post-treatment outcomes represented residualized change by accounting for baseline levels of perceived social support. We then examined the time ordering of social support and PTSD symptoms over the time points using a cross-lagged panel model (Cole & Maxwell, 2003) within a multigroup structural equation modeling (SEM) framework, with exposure therapy and control making up the two conditions. The modeling strategy proceeded from free estimation of model parameters to more restricted estimation of the cross-lagged model within each treatment group (Anderson & Gerbing, 1988). Specifically, we examined the iterative equality of within-variable autocorrelations, cross-lagged associations, and within-occasion residual covariances separately for each treatment group. To specify these models, BASIS social support and CAPS scores at each occasion (except baseline) were regressed on both their previous assessment scores (autocorrelations; e.g., baseline CAPS predicting mid-treatment CAPS) and the previous assessment of the relevant predictor (cross-lagged associations; e.g. baseline BASIS social support predicting mid-treatment CAPS). We then included within-occasion correlations between BASIS social support and CAPS scores at each time point. Next, we tested the equality of the within-variable autocorrelations, the cross-lagged associations, and the within-occasion residual covariances. Iterative restrictions to the model estimation were compared against the less restrictive model. Finally, we collapsed the multigroup SEM into a single model and included treatment condition as a predictor of PTSD symptoms and social support to examine indirect effects of condition on the relevant outcomes.
To account for missing data in our models, we used full information maximum likelihood (FIML). This method incorporates all available information from all participants with available data, and FIML produces unbiased estimates that outperform other missing data treatments, such as listwise deletion and similar response pattern imputation, under conditions when data are missing at random (Graham, 2009). Prior studies have established that there is no evidence this study data are not missing at random, making FIML a useful missing data treatment (Reger et al., 2016). When specifying our models, we assessed whether constraining associations of interest resulted in a significant change in nested model fit using chi squared difference testing and retained all constraints when they did not negatively impact model fit, consistent with a two-step modeling approach (Anderson & Gerbing, 1988). Finally, we used ML estimation when running all regression models in MPLUS version 7.31, and bias corrected bootstrapping (N = 10,000) and examined the confidence intervals to determine whether there were non-zero indirect effects in all mediation models (Muthén & Muthén, 1998-2012; Preacher & Hayes, 2008).
Results
Treatment Effects on Perceived Social Support Over Time
We first tested whether there was a main effect of exposure therapy on BASIS-SS at mid and post-treatment. Exposure therapy predicted increased BASIS-SS scores from baseline to mid-treatment assessment, β = 0.29, 95% CI [0.12, 0.46], p = .029, and post-treatment assessments, β = 0.43, 95% CI [0.13, 0.73], p = .004. These results suggest that exposure therapy increases BASIS-SS over time compared to waitlist control, and the effects are illustrated in Figure 1.
Figure 1.
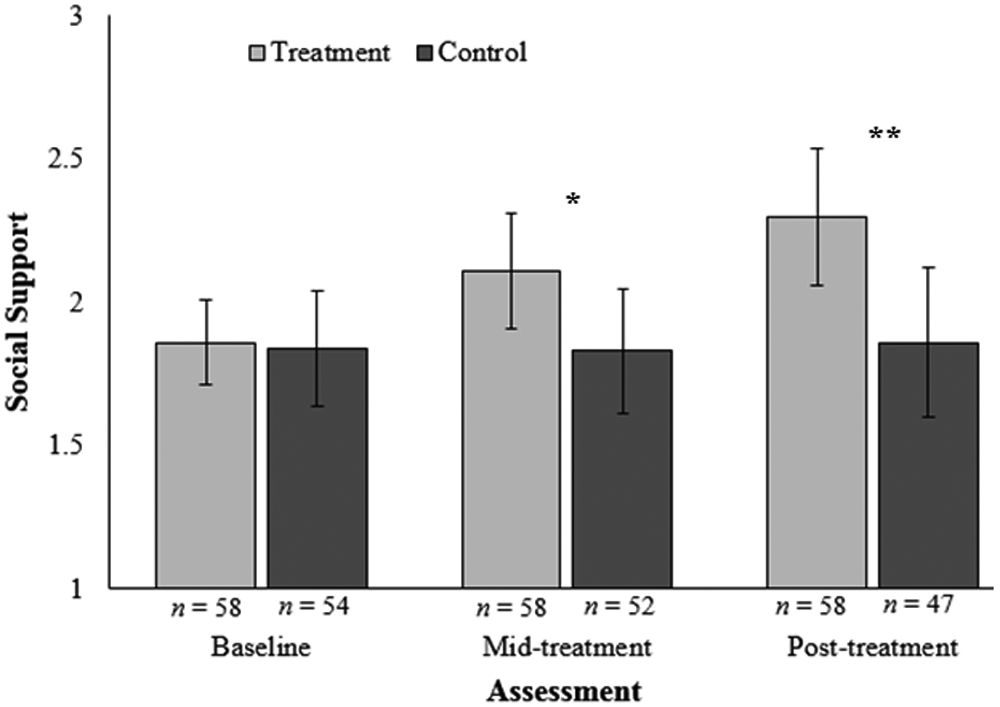
Treatment effect on social support at each occasion for control and treatment (traditional and VR-assisted PE) participants. The full BASIS subscale ranges from 0 to 4.
* = p < .05, ** = p < .01
Associations Between Perceived Social Support and PTSD Symptoms Over Time
We next examined the association of BASIS-SS and CAPS scores over the course of treatment using a cross-lagged panel design within a multi-group SEM framework, in which we specified a baseline model that was allowed to vary between treatment conditions. Our final model fit the data well overall, χ2 (20, N = 162) = 21.19, p = .386, CFI = 1.00, RMSEA = .027 [.000, .101]. Figure 2 outlines the process of model specification employed in this study (see Table 2 for model fit statistics). Employing the fully restricted model did not reduce model fit, ΔX2 (12, N = 162) = 17.67, p = .126 compared to the fully unrestricted model, and the contributions in X2 did not significantly vary between the treatment and control conditions, X2 difference = 1.67, p = .195.
Figure 2.
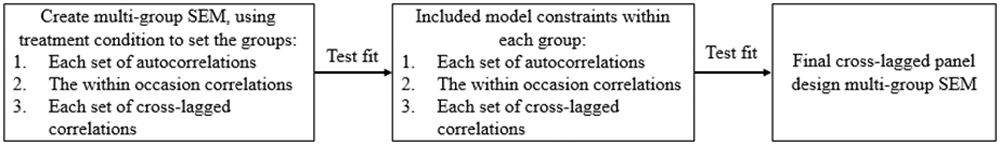
Flow chart illustrating the process of model specification for the multi-group cross-lagged panel SEM.
Table 2.
Model Fit Change During Model Specification
| Change in model specification | Δ in df | Δ Chi-sq | p | CFI | RMSEA |
|---|---|---|---|---|---|
| Fully unconstrained cross-lagged panel model | 1.00 | .000 | |||
| Constraining BASIS-SS autocorrelations to equality | 2 | 2.60 | 0.273 | 1.00 | .000 |
| Constraining CAPS autocorrelations to equality | 2 | 1.15 | 0.283 | 1.00 | .000 |
| Constraining within occasion correlations to equality | 4 | 4.15 | 0.386 | 1.00 | .000 |
| Constraining BASIS-SS → CAPS crosslags to equality | 2 | 5.03 | 0.080 | 1.00 | .000 |
| Constraining CAPS → BASIS-SS crosslags to equality | 2 | 4.74 | 0.093 | 1.00 | .000 |
Note: Change in model fit was compared to the previous model moving down the table. CAPS = Clinician Administered PTSD Scale; BASIS SS = Behavior And Symptom Identification Scale Social Support subscale; CFI = Confirmatory Fit Index; RMSEA = Root Mean Squared Error of Approximation.
We then examined the associations of interest within the models by group. Both BASIS-SS and CAPS scores had significant autocorrelations for both treatment and control participants. Similarly, there were significant within-occasion correlations for both groups at each occasion. We then examined the cross-lagged associations, which were of primary interest. For the control group, there were no significant cross-lagged associations between BASIS-SS and CAPS scores. For the treatment group, however, there was a significant effect of BASIS-SS predicting later CAPS scores, but not CAPS scores predicting later BASIS-SS. The final model results are presented for PE condition and Control condition in Figure 3. Constraining the cross-lagged associations between BASIS-SS and CAPS scores for the control condition to the value of the treatment condition did not reduce model fit ΔX2 (1, N = 162) = 1.98, p = .159. These results suggest that BASIS-SS scores are significantly associated with later CAPS scores within the treatment condition and not significantly associated in the Control condition, but these effects did not significantly differ in size when this difference was directly tested.
Figure 3.
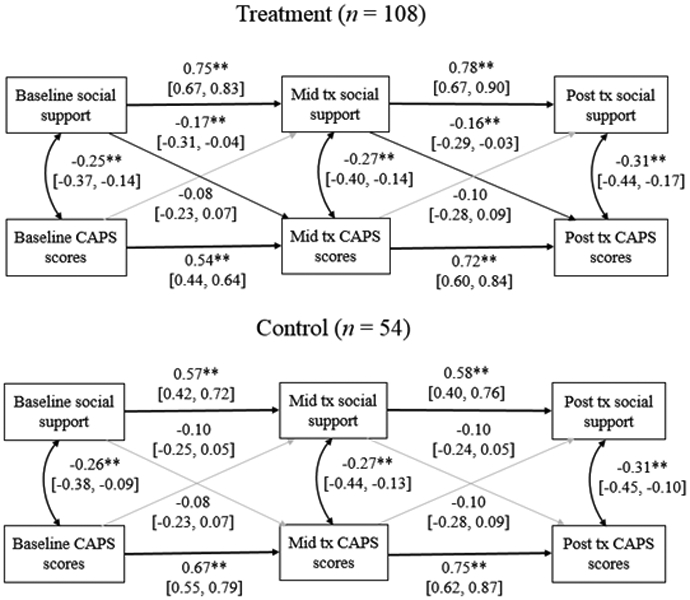
Multigroup SEM cross-lagged panel model figures for participants involved in exposure treatment and waitlist control. All values are standardized effect sizes with associated 95% confidence intervals. Grey pathways are nonsignificant.
* =p < .05, ** = p < .01
Perceived Social Support Mediating the Treatment Effect on PTSD Symptoms
Finally, having established that increases in BASIS-SS scores are associated with reductions in CAPS scores over time, we specified an additional cross-lagged panel SEM that included treatment condition as a predictor of both BASIS-SS and CAPS scores to test whether changes in social support mediated treatment effects on CAPS scores. We specified our model using the same conceptual model as previously employed, and then included treatment condition as a predictor of mid- and post-treatment CAPS scores and social support. This model fit the data well, χ2 (12, N = 162) = 9.08, p = .696, CFI = 1.00, RMSEA < .001 [.000, .062]. Treatment condition significantly predicted BASIS-SS (greater in treatment) and CAPS scores (lower in treatment) from baseline to mid-treatment, but only significantly predicted CAPS at post-treatment. The confidence interval for the indirect effect of treatment on social support at the post assessment via CAPS scores crossed zero, B = 0.03, 95% CI [<−0.01, 0.09], p = .208, whereas there was a significant non-zero indirect effect of treatment on post-assessment CAPS scores via mid-assessment BASIS-SS, B = 1.10, 95% CI [0.15, 3.01], p = .105. Notably the symmetrical p value for the indirect effect was greater than .05. When investigating indirect effects, however, bias corrected bootstrap confidence intervals are the preferred way to interpret results due to the nonsymmetrical nature of indirect effects (Preacher & Hayes, 2008).
Discussion
In the current study, we examined the longitudinal effect of exposure therapy on perceived social support in sample of active duty soldiers (N = 162) with PTSD who were randomly assigned to PE (traditional or VR-assisted) or a waitlist control. In addition, we also assessed the associations between perceived social support and PTSD symptoms over time using a cross-lagged panel design. The results evidenced that treatment increased perceived social support compared to participants in the waitlist control condition. These results are consistent with prior studies of social support during the treatment of PTSD, which found that perceived social support increases during treatment (Price et al., 2013, Price et al., 2018). Importantly, the current study expands on these previous studies by including a subsample of participants randomly assigned to a waitlist control group. As a result, we can be more confident that the changes in social support in Price and colleagues (2018) and differences in perceived social support by condition evidenced in the current sample are due to exposure therapy, rather than other potential confounding effects (e.g. maturation, regression to the mean, etc.).
Our models also evidenced a lagged association between perceived social support and later PTSD symptom change in the treatment condition, such that changes in perceived social support appear to precede changes in PTSD symptoms. Changes in social support did not significantly predict PTSD symptoms for control participants, but it should be noted that the size of the lagged associations did not significantly differ between conditions. There was, however, a significant indirect effect of treatment on post assessment PTSD symptoms through changes in perceived social support. In this way, exposure therapy appears to predict increased perceived social support, which appears to change temporally prior to changes in PTSD symptoms. The results for the exposure group align with the results from Price and colleagues (2018) and suggest that perceived social support may be one potential mediator through which exposure therapy predicts PTSD symptoms over time. The results within the waitlist group were in contrast with previous longitudinal studies of social support and PTSD symptoms over time that found evidence for either social erosion or social causation (King et al., 2006; Norris & Kaniasty 2008; Polusny et al., 2012; Shallcross et al., 2016). The current study did not find significant lagged effects in either direction, though notably the current study included a smaller sample than many previous investigations. If the sample—and resulting power to detect effects—were larger in the current study it may have resulted in significant findings in the control group, as the point estimates in our models were similar in size to previous studies (though slightly smaller), −0.10 < βs < −0.08 compared to −0.19 < βs < −0.08 (Shallcross et al., 2016).
Several proposed mechanisms have been shown to explain how exposure therapies, such as PE, reduce PTSD symptoms. Cooper, Clifton, and Feeney (2018) outlined six mechanisms that have been empirically investigated for explaining change in PE, finding strong evidence for the effect of changing beliefs and between session habituation, moderate evidence for inhibitory learning and emotional engagement, and minimal support for narrative organization and within-session habituation. Less attention has been given to the potential role that perceived social support or changes in social engagement might play in the reduction of PTSD symptoms during exposure therapy. Previous studies have found that perceived social support can moderate outcomes during PTSD treatment, with higher social support predicting better treatment efficacy (Thrasher et al., 2010). The current study builds on this research by proposing that perceived social support may play a role in how exposure therapy impacts PTSD outcomes. Although it seems unlikely that perceived social support explains changes in PTSD symptoms in exposure therapy independent of the mechanisms described by Cooper et al. (2018), it is important that future studies investigate the role social support plays in the pathway from exposure therapy to treatment outcome effects. Future studies would particularly benefit from ongoing longitudinal assessment of social support and PTSD symptoms using more proximal measurement, such as ecological momentary assessment, that would better tease apart the association between these outcomes as they change across time, both in those with PTSD and during PTSD treatment. Until such studies are undertaken, we cannot confidently determine whether social support acts as a mediator of treatment in exposure therapies or is an epiphenomenon of symptom change.
One important question arising from these results is how exposure therapy might translate to changes in perceived social support over time. Two potential pathways that might explain this effect are (1) completing exposures may increase people’s time spent in social situations, and (2) the process of completing in-vivo exposures may cause patients to explicitly recruit people from their social networks to complete in-vivo exposures. The PE groups included in-vivo exposures as a necessary component completed outside the therapy room. These exposures are selected by patients in the therapy process and are often socially mediated. For example, someone with PTSD who has avoided crowded restaurants might plan to enter that environment as part of an in-vivo exposure. Similarly, they might choose to watch a movie in a crowded theater. In-vivo exposures such as these are often completed in the company of others, helping to increase the time patients spend in social activities. This increase in time spent with others may then translate to decreased PTSD symptoms (e.g., numbing, withdrawal). It is important to note, however, that without having additional treatment conditions using different therapies, we cannot be sure that the changes in perceived social support were due to exposure specifically, or to engaging in treatment for PTSD more generally.
In addition, the exposures described above include an implicit social activity that activates existing support networks. For people with PTSD who have avoided such social activities, reaching out to close others to complete these in-vivo exposures might help activate social networks that had laid dormant because of avoidance, or may spur the initialization of new social connections. This process would be similar to the characteristics of conjoint exposures used in CBCT for PTSD (Monson et al., 2008; Monson & Fredman, 2012), in which romantic partners are explicitly involved as a part of in-vivo exposures, albeit in an informal way. Additionally, the trauma processing component following imaginal exposures (traditional and VR-assisted) could also have played a role in altering the way that those with PTSD think about their social connections by promoting new learning regarding the social support available to them or their willingness or ability to interact with or seek out social support. The process of seeking and engaging in treatment may also promote more supportive response from others in the social environments of those with PTSD, prompting increased perceived support on the part of the traumatized individual. The current study did not, however, assess the nature of the in-vivo exposures that participants completed, the degree of social content in trauma processing, nor the impact of seeking treatment on specific members of participants’ social networks, so empirical tests of these questions are not possible with the current data. Future studies of social support in PTSD treatment would benefit from assessing whether socially mediated in-vivo exposures or socially focused trauma processing explain increased perceived social support within treatment, as well as whether the treatment process interacts with other aspects of the social network of people with PTSD, such as improving their relationship satisfaction (Edwards-Stewart et al., 2018), that might impact the treatment process. Specific assessment of avoidance behaviors may also be of benefit, as potential pathways for how social support might support PTSD treatment.
The results from the current study also carry direct clinical implications. Social support has been identified as a key treatment target in the Veterans Affairs/Department of Defense PTSD clinical practice guidelines (Management of Post-Traumatic Stress Working Group, 2017). Results from the current study suggest that PE (traditional and VR-assisted) is one treatment that can be used to target perceived social support among military personnel with combat-related PTSD. This may be particularly effective for those who are avoidant of social situations, as in-vivo exposures would directly target this avoidance. The finding that changes in social support precede changes in PTSD symptoms suggests that clinicians should attend to ways to increase perceived social support early in treatment, particularly as social support predicts lower levels of treatment dropout (Meis et al., 2019). The initial assessment of symptoms in exposure treatment includes specific questions characterizing the participant’s current social support at the beginning of treatment, and this could be useful in targeting exposures. The purposeful identification of in-vivo exposures that will explicitly facilitate increased social engagement could be a useful strategy. For example, PE encourages the inclusion of exposures specifically designed to increase re-engagement in social relationships, even if these exposures do not trigger anxiety or distress (Foa et al., 2007). Importantly, given prior research demonstrating the potential deleterious effects of some types of social support, such as accommodation (Campbell & Renshaw, 2018; Campbell, Renshaw, Kashdan, Curby, & Carter, 2017), clinicians should be attentive to the over reliance on social supports during exposures or potential interpersonal relationships that may inadvertently undermine exposures. In some contexts, social supports can function as safety aids and prevent the necessary violation of negative expectancies required for an effective exposure (Blakey & Abramowitz, 2018; Korte, Norr, & Schmidt, 2018). Thus, within the context of exposure therapy clinicians should leverage the treatment’s ability to increase perceived social support while helping patients ensure their reliance on socials supports does not interfere with the necessarily corrective learning.
Limitations
The results of the current study should be understood in the context of its limitations. First, the sample was composed of active-duty soldiers with deployment-related traumas, who were largely male (96%). This is a specific population that might not generalize to all military or civilian populations. Future studies using broader samples that replicate these results would provide additional evidence about the extent to which these results may apply to other groups. Second, the study included participants that did not complete all assessments. Although we used gold-standard missing data techniques (Graham, 2009) and included all data points available, it is possible that attrition over the course of the study might have impacted the current results. Third, the measure of social support used in the current study (Eisen et al., 2004) did not include multiple types of social support or structural aspects of social support. Given research that has shown social support is a multifaceted construct (Jacobson, 1986), future studies assessing social support in the context of PTSD treatment would benefit from the use of comprehensive measures of social support, such as behavioral or observational measures. Fourth, the current study assessed perceived social support solely over the course of treatment. It is unclear if the current improvements in social support evidenced in the exposure therapy group would be maintained over time. It should be noted that social support was assessed in the treatment groups at a 12 and 26-week follow up, which did not show any significant reduction in social support from the levels reported at the end of treatment, but high levels of attrition and a lack of comparison group (as the waitlist group was not maintained or assessed at these occasions) make drawing strong conclusions about the maintenance of these results problematic. Fifth, the current study used a subscale measure of the BASIS measure. Although it has been validated, it is possible that other self-report measures of social support, or behavioral measures of social support, might result in different findings. Finally, the current study included only the minimum necessary timepoints to conduct a cross-lagged panel design. Future studies would benefit from additional timepoints.
Conclusion
The current study assessed a sample of 162 active-duty soldiers with PTSD who completed exposure therapy (traditional or VR-assisted PE) to examine the association of perceived social support and PTSD symptoms over time. The results indicated that exposure therapy increased perceived social support during treatment compared to waitlist control. In addition, cross-lagged panel models found that increases in perceived social support predicted decreases in PTSD symptoms over time in the treatment group, but these associations were not present in the waitlist control group. There was a significant indirect effect of treatment on PTSD symptom change via change in perceived social support. These results suggest that exposure therapy increases perceived social support, which may be one pathway by which treatment may reduce PTSD symptoms.
Table 3.
Correlation Matrix of Variable of Interest for the Treatment and Control Conditions
| Variables | 1 | 2 | 3 | 4 | 5 | 6 |
|---|---|---|---|---|---|---|
| Baseline social support (1) | — | 0.58** | 0.48** | −0.26* | −0.40** | −0.29* |
| Mid-treatment social support (2) | 0.71** | — | 0.61** | −0.11 | −0.31* | −0.20 |
| Post-treatment social support (3) | 0.66** | 0.84** | — | −0.21 | −0.36** | −0.45** |
| Baseline CAPS (4) | −0.22* | −0.30** | −0.26* | — | 0.71** | 0.62** |
| Mid-treatment CAPS (5) | −0.30** | −0.52** | −0.43** | 0.51** | — | 0.77** |
| Post-treatment CAPS (6) | −0.33** | −0.51** | −0.50** | 0.43** | 0.81** | — |
Note: All values used full-information maximum likelihood for missing data. Values above the diagonal equal correlations for the control group, below the diagonal equal values for the exposure therapy group.
Acknowledgments
This work was supported by Grant W81XWH-08-2–0015 from the U.S. Army Medical Research and Materiel Command Military Operational Medicine Research Program. This work was supported in part by the National Institute on Aging (NIA) Training Grant (T32-AG000029), provided to the first author. No authors report competing interests.
References
- Anderson JC, & Gerbing DW (1988). Structural equation modeling in practice: A review and recommended two-step approach. Psychological Bulletin, 103(3), 411–423. [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, & Keane TM (1995). The development of a clinician-administered PTSD scale. Journal of Traumatic Stress, 8, 75–90. 10.1002/jts.2490080106 [DOI] [PubMed] [Google Scholar]
- Brewin CR, Andrews B, & Valentine JD (2000). Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. Journal of Consulting and Clinical Psychology, 68, 748–766. 10.1037//0022-006X.68.5.748 [DOI] [PubMed] [Google Scholar]
- Cameron IM, Cunningham L, Crawford JR, Eagles JM, Eisen SV, Lawton K, … Hamilton RJ (2007). Psychometric properties of the BASIS-24 (Behaviour and Symptom Identification Scale-Revised) mental health outcome measure. International Journal of Psychiatry in Clinical Practice, 11, 36–43. [DOI] [PubMed] [Google Scholar]
- Campbell SB, & Renshaw KD (2018). Posttraumatic stress disorder and relationship functioning: A comprehensive review and organizational framework. Clinical Psychology Review, 65, 152–62. 10.1016/j.cpr.2018.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cole DA, Maxwell SE, 2003. Testing mediational models with longitudinal data: questions and tips in the use of structural equation modeling. Journal of Abnormal Psychology 112(4), 558–577. Accessed via https://www.ncbi.nlm.nih.gov/pubmed/14674869 [DOI] [PubMed] [Google Scholar]
- Cooper AA, Clifton EG, & Feeny NC (2017). An empirical review of potential mediators and mechanisms of prolonged exposure therapy. Clinical Psychology Review, 56, 106–121. 10.1016/j.cpr.2017.07.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Craske MG, Kircanski K, Zelikowsky M, Mystkowski J, Chowdhury N, & Baker A (2008). Optimizing inhibitory learning during exposure therapy. Behaviour Research and Therapy, 46(1), 5–27. Accessed via https://www.ncbi.nlm.nih.gov/pubmed/18005936 [DOI] [PubMed] [Google Scholar]
- Edwards-Stewart A, Rennebohm SB, DeSimone J, Willey B, Smolenski DJ, & Hoyt T (2018). Relationship Satisfaction and Mental Health Treatment Among Active-Duty Military. Couple and Family Psychology: Research and Practice, 7(3-4), 201–211. [Google Scholar]
- Eisen SV, Normand SLT, Belanger AJ, Gevorkian S, & Irvin EA (2004). BASIS-32 and the Revised Behavior and Symptom Identification Scale (BASIS) In: Maruish M (ed.). The use of psychological testing for treatment planning and outcome assessment, 3rd ed. NJ: Lawrence Erlbaum Associates, p. 79–115. [Google Scholar]
- Eisen SV, Normand SLT, Belanger AJ, Spiro A, & Esch D (2004). The revised behavior and symptom identification scale (BASIS-R): reliability and validity. Medical Care, 42, 1230–1241. https://www.jstor.org/stable/4640879 [DOI] [PubMed] [Google Scholar]
- Foa EB, Hembree EA, & Rothbaum BO (2007). Prolonged exposure therapy for PTSD: Emotional processing of traumatic experiences: Therapist guide. USA: Oxford University Press. [Google Scholar]
- Foa EB, & Tolin DF (2000). Comparison of the PTSD symptom scale-interview version and the clinician-administered PTSD scale. Journal of Traumatic Stress, 13, 181–191. 10.1023/A:1007781909213 [DOI] [PubMed] [Google Scholar]
- Graham JW (2009). Missing data analysis: Making it work in the real world. Annual review of psychology, 60, 549–576. http://dx.doi.org/annurev.psych.58.110405.085530 [DOI] [PubMed] [Google Scholar]
- Hernandez-Tejada MA, Acierno R, & Sanchez-Carracedo D (2017). Addressing Dropout From Prolonged Exposure: Feasibility of Involving Peers During Exposure Trials. Military Psychology, 29(2), 157–163. 10.1037/mil0000137 [DOI] [Google Scholar]
- Hovens JE, van Der Ploeg HM, Klaarenbeek MTA, Bramsen I, Schreuder JN, & Rivero VV (1994). The assessment of posttraumatic stress disorder: With the clinician administered PTSD scale: Dutch results. Journal of Clinical Psychology, 50, 325–340. 10.1002/1097-4679 [DOI] [PubMed] [Google Scholar]
- Jacobson DE (1986). Types and timing of social support. Journal of Health and Social Behavior, 250–264. 10.2307/2136745 [DOI] [PubMed] [Google Scholar]
- Koenen KC, Stellman JM, Stellman SD, & Sommer JF Jr. (2003). Risk factors for course of posttraumatic stress disorder among Vietnam veterans: A 14-year follow-up of American Legionnaries. Journal of Consulting and Clinical Psychology, 71, 980–986. 10.1037/0022-006X.71.6.980 [DOI] [PubMed] [Google Scholar]
- Korte KJ, Norr AM, & Schmidt NB (2018) Targeting safety behaviors in the treatment of anxiety disorders: A case study on the use of False Safety Behavior Elimination Treatment (F-SET). American Journal of Psychotherapy, 71, 9–20. 10.1176/appi.psychotherapy.20180001 [DOI] [PubMed] [Google Scholar]
- Management of Post-Traumatic Stress Working Group. (2017). VA/DoD clinical practice guideline for management of post-traumatic stress, v. 3.0. Washington (DC): Veterans Health Administration, Department of Defense, 1–251. [Google Scholar]
- Markowitz JC, Milrod B, Bleiberg K, & Marshall RD (2009). Interpersonal factors in understanding and treating posttraumatic stress disorder. Journal of Psychiatric Practice, 15(2), 133–140. 10.1097/01.pra.0000348366.34419.28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meis LA, Noorbaloochi S, Hagel Campbell EM, Erbes CR, Polusny MA, Velasquez TL, … & Tuerk PW (2019). Sticking it out in trauma-focused treatment for PTSD: It takes a village. Journal of Consulting and Clinical Psychology, 87(3), 246–256. 10.1037/ccp0000386 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monson CM, & Fredman SJ (2012). Cognitive-behavioral conjoint therapy for PTSD: Harnessing the healing power of relationships. New York: Guilford Press. [Google Scholar]
- Monson CM, Fredman SJ, & Adair KC (2008). Cognitive–behavioral conjoint therapy for posttraumatic stress disorder: Application to Operation Enduring and Iraqi Freedom veterans. Journal of Clinical Psychology, 64(8), 958–971. 10.1002/jclp.20511 [DOI] [PubMed] [Google Scholar]
- Muthén LK, and Muthén BO. Mplus User’s Guide. Seventh Edition. Los Angeles, CA: Muthén & Muthén; (1998-2012). [Google Scholar]
- Kaniasty K, & Norris FH (2008). Longitudinal linkages between perceived social support and posttraumatic stress symptoms: Sequential roles of social causation and social selection. Journal of Traumatic Stress, 21(3), 274–281. 10.1002/jts.20334 [DOI] [PubMed] [Google Scholar]
- King DW, Taft C, King LA, Hammond C, & Stone ER (2006). Directionality of the association between social support and Posttraumatic Stress Disorder: a longitudinal investigation 1. Journal of Applied Social Psychology, 36(12), 2980–2992. 10.1111/j.0021-9029.2006.00138.x [DOI] [Google Scholar]
- Ozer EJ, Best SR, Lipsey TL, & Weiss DS (2003). Predictors of posttraumatic stress disorder and symptoms in adults: A meta-analysis. Psychological Bulletin, 129, 52–73. 10.1037/0033-2909.129.1.52 [DOI] [PubMed] [Google Scholar]
- Polusny MA, Erbes CR, Murdoch M, Arbisi PA, Thuras P, & Rath MB (2011). Prospective risk factors for new-onset post-traumatic stress disorder in National Guard soldiers deployed to Iraq. Psychological Medicine, 41(4), 687–698. 10.1017/S003329171000204 [DOI] [PubMed] [Google Scholar]
- Preacher KJ, & Hayes AF (2008). Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods, 40(3), 879–891. 10.3758/BRM.40.3.879 [DOI] [PubMed] [Google Scholar]
- Price M, Gros DF, Strachan M, Ruggiero KJ, & Acierno R (2013). The role of social support in exposure therapy for Operation Iraqi Freedom/Operation Enduring Freedom veterans: A preliminary investigation. Psychological Trauma: Theory, Research, Practice, and Policy, 5(1), 93–100. 10.1037/a0026244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Price M, Lancaster CL, Gros DF, Legrand AC, van Stolk-Cooke K, & Acierno R (2018). An Examination of Social Support and PTSD Treatment Response During Prolonged Exposure. Psychiatry: Interpersonal and Biological Processes, 1–13. 10.1080/00332747.2017.1402569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reger GM, Koenen-Woods P, Zetocha K, Smolenski DJ, Holloway KM Rothbaum BO, … Gahm GA (2016). Randomized controlled trial of prolonged exposure using imaginal exposure vs. virtual reality exposure in active duty soldiers with deployment-related posttraumatic stress disorder (PTSD). Journal of Consulting and Clinical Psychology, 84, 946–956. 10.1037/ccp0000134 [DOI] [PubMed] [Google Scholar]
- Shallcross SL, Arbisi PA, Polusny MA, Kramer MD, & Erbes CR (2016). Social causation versus social erosion: Comparisons of causal models for relations between support and PTSD symptoms. Journal of Traumatic Stress, 29(2), 167–175. 10.1002/jts.22086 [DOI] [PubMed] [Google Scholar]
- Sherbourne CD, & Stewart AL (1991). The MOS social support survey. Social Science & Medicine, 32(6), 705–714. 10.1016/0277-9536(91)90150-B [DOI] [PubMed] [Google Scholar]
- Shnaider P, Sijercic I, Wanklyn SG, Suvak MK, & Monson CM (2017). The Role of Social Support in Cognitive-Behavioral Conjoint Therapy for Posttraumatic Stress Disorder. Behavior Therapy, 48(3), 285–294. 10.1016/j.beth.2016.05.003 [DOI] [PubMed] [Google Scholar]
- Thrasher S, Power M, Morant N, Marks I, & Dalgleish T (2010). Social support moderates outcomes in a randomized controlled trial of exposure therapy and (or) cognitive restructuring for chronic posttraumatic stress disorder. Canadian Journal of Psychiatry, 55, 187–190. 10.1177/070674371005500311 [DOI] [PubMed] [Google Scholar]
- Tsai J, Harpaz-Rotem I, Pietrzak RH, & Southwick SM (2012). The role of coping, resilience, and social support in mediating the relationship between PTSD and social functioning in veterans returning from Iraq and Afghanistan. Psychiatry, 75, 135–149. 10.1521/psyc.2012.75.2.135 [DOI] [PubMed] [Google Scholar]
- Weathers FW, Ruscio AM, & Keane TM (1999). Psychometric properties of nine scoring rules for the Clinician-Administered Posttraumatic Stress Disorder Scale. Psychological Assessment, 11, 124–133. 10.1037/1040-3590.11.2.124 [DOI] [Google Scholar]


