Abstract
Background
The epidemiological transition of non-communicable diseases replacing infectious diseases as the main contributors to disease burden has been well documented in global health literature. Less focus, however, has been given to the relationship between sociodemographic changes and injury. The aim of this study was to examine the association between disability-adjusted life years (DALYs) from injury for 195 countries and territories at different levels along the development spectrum between 1990 and 2017 based on the Global Burden of Disease (GBD) 2017 estimates.
Methods
Injury mortality was estimated using the GBD mortality database, corrections for garbage coding and CODEm—the cause of death ensemble modelling tool. Morbidity estimation was based on surveys and inpatient and outpatient data sets for 30 cause-of-injury with 47 nature-of-injury categories each. The Socio-demographic Index (SDI) is a composite indicator that includes lagged income per capita, average educational attainment over age 15 years and total fertility rate.
Results
For many causes of injury, age-standardised DALY rates declined with increasing SDI, although road injury, interpersonal violence and self-harm did not follow this pattern. Particularly for self-harm opposing patterns were observed in regions with similar SDI levels. For road injuries, this effect was less pronounced.
Conclusions
The overall global pattern is that of declining injury burden with increasing SDI. However, not all injuries follow this pattern, which suggests multiple underlying mechanisms influencing injury DALYs. There is a need for a detailed understanding of these patterns to help to inform national and global efforts to address injury-related health outcomes across the development spectrum.
Keywords: epidemiology, descriptive epidemiology, burden of disease
Introduction
Injury is an important cause of morbidity and mortality in nations at any point of the development spectrum. Previous research has shown that in 2015, injuries accounted for 11% of the global burden of disease, expressed in disability-adjusted life years (DALYs), with an estimated 973 million people sustaining injuries warranting some type of healthcare and 4.7 million deaths.1 Globally, since 1990, focused injury burden research has documented a declining trend in the burden of injury of all the major causes of injury.2
The epidemiological transition of non-communicable diseases (NCDs) replacing infectious diseases as the main contributors to disease burden has been well-documented.1 3 4 However, less focus has been given to the relationship between sociodemographic changes and injury outcomes. Up till now, few studies have been performed that studied the relationship between sociodemographic changes and overall injury rates. There have been reports on the associations of gross domestic product and unemployment with suicides, homicides, road injury and unintentional injuries.5–12 However, these studies focused on one specific cause of injury and on one type of injury outcome, mostly mortality. The findings of these studies indicated that the relationship between economic development and injury burden is not straightforward and mediated by many factors. A better understanding of this relationship may be achieved by investigating all causes of injury as well as looking at both fatal and non-fatal injury outcome.
Insight into the epidemiological transitions with regard to injuries can be achieved by a systematic analysis of the relationship between development and trends in mortality, incidence and burden of disease using a standardised approach. A systematic analysis may also reveal where health gains outpace or fall behind changes in development and allow for the identification of determinants and mediating factors of injury burden. This information allows identification determinants of injury burden. This information serves as a crucial input for guiding health system investments and priority-setting at the global, regional, national and subnational levels.
The Global Burden of Disease (GBD) 2015 study introduced a measure of development, the Socio-demographic Index (SDI). SDI combines information on income per capita, education and fertility. Comparisons between DALYs and SDI showed that age-standardised DALY rates for many communicable diseases declined profoundly over time, whereas improvements in SDI correlated strongly with the increasing importance of NCDs.4
This paper aims to provide an overview of injury mortality, incidence and DALYs from the GBD 2017 study, with detailed information on a range of causes of injuries; to examine the association between years of life lost (YLLs), YLDs and DALYs from injury and development, as measured by SDI, cause of injury, GBD region and over time; and to assess in which regions injury DALYs outpace or fall behind changes in development.
Methods
GBD 2017 study
The GBD 2017 study methods and results have been described in extensive detail elsewhere, including description of the analytical estimation framework used to measure deaths, YLLs, YLDs and DALYs.4 13 14 A summary overview of the GBD study is provided in online supplementary appendix 1. The methodological components specific to injuries estimation and SDI calculation are summarised below.
injuryprev-2019-043296supp001.pdf (64.6KB, pdf)
Injury incidence and death are defined as ICD-9 codes E800–E999 and ICD-10 chapters V–Y, except for deaths and cases of drug overdoses and unintentional alcohol poisoning, which are classified under drug and alcohol use disorders. These external cause-of-injury codes or ‘E codes’ are designated as mutually exclusive and collectively exhaustive within the injuries estimation process. In terms of the nature-of-injury codes (eg, the lower extremity amputation that can occur with a road injury), injuries were categorised into 47 mutually exclusive and collectively exhaustive nature-of-injury categories using chapters S and T in International Classification of Disease (ICD) ICD-10 and codes 800–999 in ICD-9 to quantify the various disabling outcomes of each cause of injury. Some injuries are trivial and unlikely to account for an important number of DALYs; hence, we only included injuries in our morbidity analysis that warranted some form of healthcare.
Injury mortality and YLLs
The overall approach to estimate causes of death is provided in related publications.13 15 16 A summary is as follows. We first mapped data sources using different versions of ICD or alternative classification systems to the GBD cause list. These data sources included vital registration, verbal autopsy, mortality surveillance, censuses, surveys, hospitals, police records and mortuary data. We then made adjustments for ill-defined causes of death such that they mapped to an underlying cause of death. Next, we conducted ensemble models using GBD cause of death ensemble modelling (CODEm) software to estimate cause-specific mortality by age, sex, country, year and cause. CODEm is described in more detail elsewhere but in summary explores a large variety of possible models to estimate trends in causes of death using an algorithm to select varying combinations of covariates that are run through several modelling classes. The method then creates an ensemble of best-performing models that are determined by evaluating out-of-sample predictive validity. Deaths are then rescaled for each cause so that the sum equals the number of deaths from all causes to ensure internal consistency. YLLs were calculated by multiplying deaths by the residual life expectancy at the age of death based on the GBD 2017 standard model life table.12
Injury incidence, prevalence and years lived with disability
Our method for estimating the incidence, prevalence and years lived with disability in non-fatal injury outcomes is provided in other GBD publications.2 14 A summary is as follows. We used DisMod-MR V.2.1 (a meta-regression tool for epidemiological modelling) to model injury incidence using data from emergency department and hospital records and survey data to produce cause-of-injury incidence by location, year, age and sex. Across every injury cause model, we used national income per capita as a covariate on excess mortality, which forces a negative relationship between income and mortality to take into account higher case fatality in lower-resource settings. After modelling incidence of each cause of injury, we used a severity hierarchy to identify the nature-of-injury category that would lead to the most long-term burden when an individual experiences multiple injuries. This hierarchy is based on pooled data sets of follow-up studies in which we translated each individual’s health status measure at 1 year after injury into a disability weight. This process is described in more detail in the GBD literature.12 14 17–22 Then, we generated matrices of the proportions of each cause of injury that are expected to lead to each nature of injury as determined in dual-coded (eg, both cause-of-injury and nature-of-injury coded) hospital and emergency department data sets and data from the Chinese National Injury Surveillance System.23 These data sets were used because the data were available in microdata format and they included dual-coded data in the format required for this specific part of the analysis. The resulting cause–nature matrices varied by injury warranting hospital admission versus injury warranting other healthcare, high-income/low-income countries, male/female and age group. In the next stage, we estimated short-term disability by cause and nature‐of‐injury category based on average duration for treated cases for each nature-of-injury category and for inpatient and outpatient injuries from the Dutch Injury Surveillance System.17 18 For 19 of the 47 nature-of-injury categories (eg, foreign body in ear, poisoning and fracture in ear), we supplemented these estimates with expert-driven estimates of short-term duration for nature-of-injury categories when the data set had insufficient information. For untreated injuries, the average factor by which the duration of short-term injury outcomes is increased for a given nature-of-injury category when the injury goes untreated was estimated.
For longer-term injuries, we calculated the proportion of injuries that would result in disability lasting more than a year for each nature-of-injury category by admission status and age. This calculation was based on an assumption that disability from injury affects all cases in the short term with a proportion having persistent disability 1 year after the injury greater than the pre-injury health status. These probabilities of developing permanent health loss were based on a pooled data set of seven large follow-up studies from China, the Netherlands and the USA that used patient-reported outcome measures to assess health status.17–22 24 25 We used the GBD healthcare access and quality (HAQ) index to estimate the ratio of treated to untreated injuries for each country–year grouping.26 The HAQ index is scaled from 0 to 100 and is based on 32 causes of death, covering a range of health service areas, which should not occur if effective care is present. Finally, we used DisMod-MR V.2.1 to compute the long-term prevalence (ie, 1 year or more) for each cause–nature combination from incidence, which also incorporated increased mortality risk of certain nature of injuries, such as traumatic brain injury based on meta-analyses of studies providing standardised mortality ratios of these conditions. YLDs were calculated as prevalence of a health state multiplied by a disability weight. These estimates were then corrected for comorbidity with other non-fatal diseases using methods described elsewhere in the GBD study.13
Socio-demographic Index
SDI is a composite indicator that includes income per capita, average educational attainment over age 15 years and total fertility rate under age 25 years. The SDI has a value that ranges from 0 to 1. 0 represents the lowest income per capita, lowest educational attainmentand highest fertility under age 25 years observed across all GBD geographies from 1980 to 2017. 1 represents the highest income per capita, highest educational attainment and lowest fertility under 25 years observed across all GBD geographies from 1980 to 2017. The average relationship between YLLs, YLDs and YLDs divided by DALYs was calculated with SDI using Gaussian process regression modelling. We used these estimates of expected DALY rates that were predicted based on the full range of SDI to determine whether observed health patterns deviated from trends associated with changes along the development spectrum.
GATHER compliance
This study complies with the GATHER (Guidelines for Accurate and Transparent Health Estimates Reporting) recommendations (online supplementary appendix 2).
injuryprev-2019-043296supp002.pdf (65.2KB, pdf)
Results
Mortality, incidence and burden of injury, 2017
In 2017, worldwide 55.9 million (95% Uncertainty Interval (UI) 55.4 to 56.5 million) people died. Of these deaths, 4.5 million (95% UI 4.3 to 4.6 million), 8.0% (95% UI 7.7% to 8.2%), were due to injuries. Major causes of injury deaths were road injury (27.7%), self-harm (17.7%), falls (15.5%) and interpersonal violence (9.0%).
There were 521 million (95% UI 493 to 548 million) cases of non-fatal injuries in 2017, representing an increase of 167 million from the 354 million (95% UI 338 to 372 million) cases of non-fatal injuries in 1990. The global age-standardised injury death rate was 57.9 per 100 000 (95% UI 55.9 to 59.2), with highest death rates for road injury (15.8 deaths per 100 000 (95% UI 15.2 to 16.3)), self-harm (10.0 deaths per 100 000 (95% UI 9.4 to 10.3)) and falls (9.2 deaths per 100 000 (95% UI 8.5 to 9.8)) (see online supplementary appendix table 1). Injury death rates were over twice as high in men compared with women (80.9 per 100 000 (95% UI 77.7 to 83.0) and 35.5 per 100 000 (95% UI 33.9 to 36.5), respectively). The global age-standardised injury incidence rate was 6762.6 per 100 000 (95% UI 6412.0 to 7118.1)), with highest incidence rates for falls (2237.6 new cases per 100 000 (95% UI 1989.7 to 2532.3)) and mechanical forces (943.6 new cases per 100 000 (95% UI 808.7 to 1100.6)) (see online supplementary appendix table 1). Injury incidence rates were almost twice as high in men compared with women (7827.1 per 100 000 (95% UI 7435.3 to 8242.9) and 5654.5 per 100 000 (95% UI 5351.3 to 5962.1), respectively).
injuryprev-2019-043296supp003.pdf (64.7KB, pdf)
Injuries contributed 10.1% (9.7%–10.5%) to the global burden of disease in 2017 (3267.0 DALYs per 100 000 (95% UI 3058.2 to 3505.1)). YLLs were responsible for the majority of the injury DALYs (77%; 2548 YLLs per 100 000 (95% UI 2462 to 2610)). The main contributors to injury DALYs were road injuries (871.1 DALYs per 100 000 (95% UI 827.9 to 917.3); 26.7%), falls (459.5 DALYs per 100 000 (95% UI 387.1 to 547.5); 14.1%), self-harm (429.0 per 100 000 (95% UI 401.6 to 443.5); 13.1%), interpersonal violence (334.3 DALYs per 100 000 (95% UI 304.7 to 360.5); 10.2%) and drowning (230.0 DALYs per 100 000 (95% UI 219.1 to 241.2); 7.0%) (see online supplementary appendix table 2). The injury burden was highest in Syria (16 341.1 DALYs per 100 000 (95% UI 15 892.7 to 16 858.4), Central African Republic (11 012.7 DALYs per 100 000 (95% UI 8807.9 to 12 913.8)) and Lesotho (7951.3 DALYs per 100 000 (95% UI 6424.8 to 9407.4)) and lowest in Maldives (1282.4 DALYs per 100 000 (95% UI 1138.1 to 1572.9)), Bermuda (1432.2 DALYs per 100 000 (95% UI 1267.5 to 1606.7)) and Italy (1458.1 DALYs per 100 000 (95% UI 1237.2 to 1739.4)) (see online supplementary appendix table 3. SDI level for each country in 2017 is also provided).
injuryprev-2019-043296supp004.pdf (64.5KB, pdf)
injuryprev-2019-043296supp005.pdf (108.4KB, pdf)
Change over time
Between 1990 and 2017, the age-standardised injury DALY rates have declined from 4946 (95% UI 4655 to 5233) to 3267 DALYs (95% UI 3058 to 3505) per 100 000, with largest absolute declines in drowning (from 635 (95% UI 571 to 689) to 230 (95% UI 219 to 241) DALYs per 100 000), road injuries (from 1259 (95% UI 1182 to 1330) to 871 (95% UI 828 to 917) DALYs per 100 000), self-harm (from 687 (95% UI 621 to 723) to 429 (95% UI 402 to 443) DALYs per 100 000), and fire, heat and hot substances (from 197 (95% UI 157 to 228) to 111 (95% UI 93 to 129) DALYs per 100 000). Between 1990 and 2017, the age-standardised rates of YLDs and YLLs from injuries declined by 7.8% and 38.8%, respectively, while incidence of injuries only declined by 0.9%.
Burden of injury by SDI level
The contribution of cause-of-injury category DALY rates to the total injury DALY rates differed by year, age category, sex and SDI level. The largest disparity in DALY rate by SDI level was found in 0–6 days olds, ranging from a high of 52 374 DALYs per 100 000 in the lowest SDI quintile to a low of 6109 DALYs per 100 000 in the highest SDI quintile. In men aged 15–49 years, conflict and terrorism stands out because of the high difference between highest and lowest DALY rates by level of SDI (countries with low SDI 496 DALYs (95% UI 414 to 589) per 100 000; countries with high SDI 2 DALYs (95% UI 1 to 2) per 100 000).
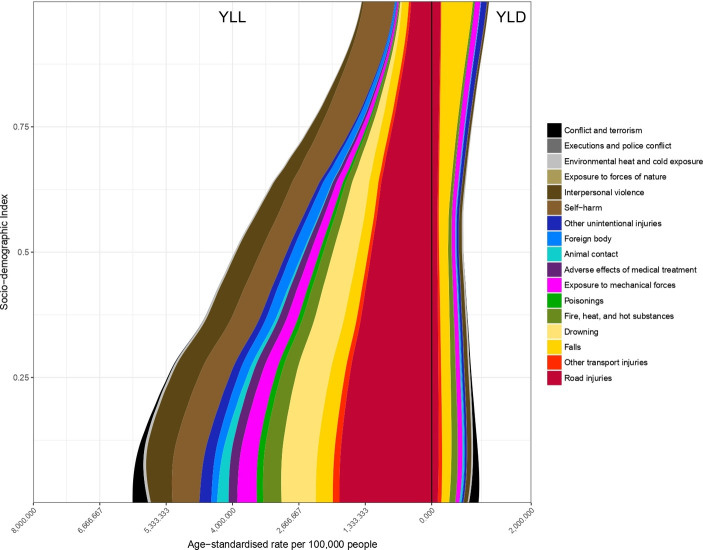
YLL and YLD rates by SDI level
For many causes of injury, age-standardised YLL and YLD rates declined strikingly with increasing SDI, with proportionally largest decreases in YLL rates for conflict and terrorism (low SDI level 163.4 YLLs per 100 000; high SDI level 0.06 YLLs per 100 000), animal contact (low SDI level 140.0 YLLs per 100 000; high SDI level 2 YLLs per 100 000) and other unintentional injuries (low SDI level 7993 YLLs per 100 000; high SDI level 8.4 YLLs per 100 000). Figure 1 shows the level of age-standardised YLLs and YLDs per 100 000 against SDI (all regions, all years 1990–2017) by cause-of-injury. Largest decreases in YLD rates were seen for cause-of-injury categories conflict and terrorism, exposure to forces of nature and adverse effects of medical treatment. Exceptions were road injuries, self-harm and interpersonal violence. The age-standardised YLL rate of road injuries was highest at the low-middle range SDI levels and lowest at higher SDI levels, whereas YLDs from road injuries increased at higher SDI. The age-standardised road injuries YLL rate increased from low SDI to low-middle SDI, but declined at higher levels of SDI. For falls, at higher levels of SDI, the composition of the disease burden shifted towards YLDs as the primary driver of DALYs. YLLs made up 63%, 61% and 20% of DALYs from falls in low, middle and high SDI quintiles, respectively. For road injuries, the proportion of YLLs dropped from 91% in countries with low SDI to 70% in countries with high SDI.
Figure 1.
Age-standardised YLL and YLD rates for 17 cause-of-injury categories by level of Socio-demographic Index. YLL, years of life lost.
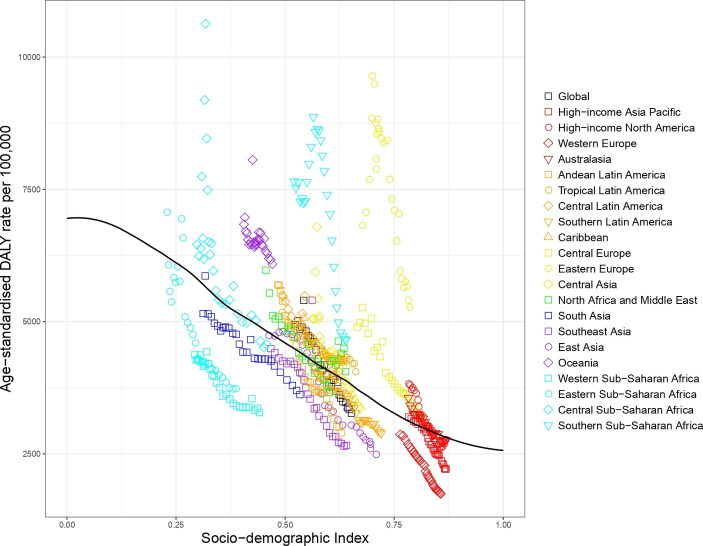
Expected based on SDI versus observed burden of injury by SDI level, 1990–2017
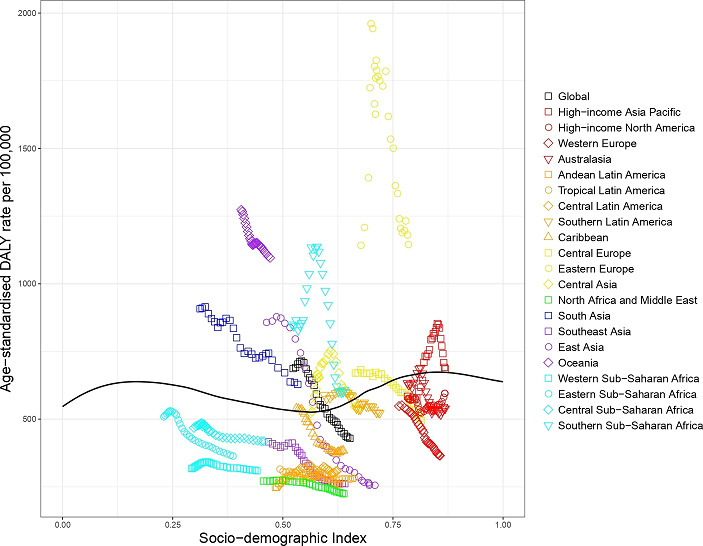
Figure 2 shows the level of all injury age-standardised DALYs per 100 000 against SDI by GBD region from 1990 to 2017 in comparison with expected values (black line) based on SDI alone. The icons appearing above the black line for DALYs represent worse than expected injury DALYs and the icons appearing below represent better than expected injury DALYs. As SDI generally increases over time, successive markers represent years between 1990 and 2017. Regions where injury DALY rates were notably greater than expected based on SDI included Central and Southern Sub-Saharan Africa, Oceania, Eastern Europe, Central Europe and high-income North America. Regions where injury DALY rates were notably lower than expected based on SDI included Eastern and Western Sub-Saharan Africa, South Asia, Southeast Asia and Western Europe.
Figure 2.
Co-evolution of all injury age-standardised DALY rates with SDI for the world and 21 GBD regions for 1990–2017 with comparison with the values expected on the basis of SDI alone. DALY, disability-adjusted life year; GBD, Global Burden of Disease; SDI, Socio-demographic Index.
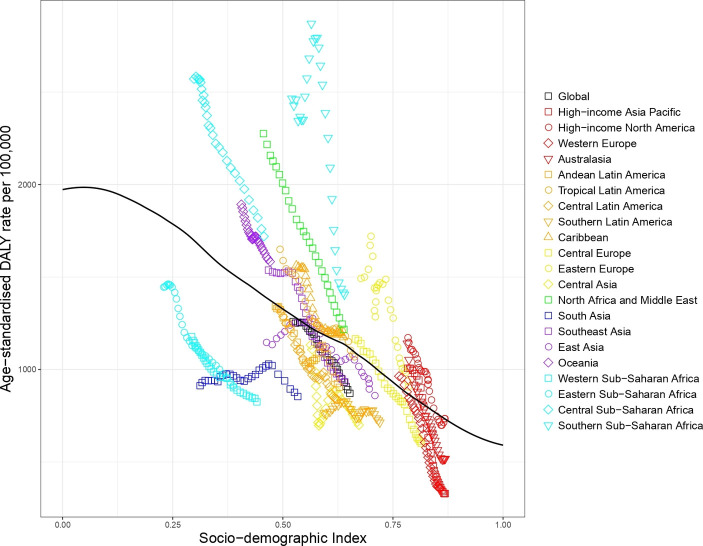
Road injury
The expected road injury DALY rate by SDI shows that most regions decreased in terms of road injury DALYs as SDI increased over time (see figure 3). South Asia, East Asia, Southern Sub-Saharan Africa and Eastern Europe are exceptions to this pattern, showing an initial increase and then a decline. In GBD 2017, the regions with worse than expected road injury DALYs based on SDI included North Africa and Middle East, Southern and Central Sub-Saharan Africa, Eastern Europe and Oceania, while regions with markedly better than expected rates included Eastern Sub-Saharan Africa, South Asia and Southern Latin America.
Figure 3.
Co-evolution of road injury age-standardised DALY rates with SDI for the world and 21 GBD regions for 1990–2017 with comparison with the values expected on the basis of SDI alone. DALY, disability-adjusted life year; GBD, Global Burden of Disease; SDI, Socio-demographic Index.
Interpersonal violence
In 2017, in all regions except for Southern Sub-Saharan Africa, Central Latin America, Tropical Latin America, Eastern Europe, Caribbean, Oceania and high-income North America, the observed interpersonal violence DALY rates were better than expected based on SDI (see figure 4). Between 1990 and 2017, in most regions with higher than expected DALYs, the gap between observed and expected interpersonal violence DALY rates decreased, except for Caribbean and Tropical Latin America, where the gap increased.
Figure 4.
Co-evolution of interpersonal violence age-standardised DALY rates with SDI for the world and 21 GBD regions for 1990–2017 with comparison with the values expected on the basis of SDI alone. DALY, disability-adjusted life year; GBD, Global Burden of Disease; SDI, Socio-demographic Index.
Self-harm
The patterns of observed and expected self-harm DALYs based on SDI by GBD regions between 1990 and 2017 differed markedly from those of other injuries (see figure 5). In 1990, observed self-harm DALY rates in East Asia and Eastern Europe were worse than expected based on SDI but rapidly declined over time, with observed DALY rates lower than expected in 2017. Southern Sub-Saharan Africa had worse than expected DALY rates but the other regions of Sub-Saharan Africa had better than expected DALY rates. North Africa and Middle East, Western Europe, Southeast Asia, and Andean, Central and Tropical Latin America all had better than expected DALY rates.
Figure 5.
Co-evolution of self-harm age-standardised DALY rates with SDI for the world and 21 GBD regions for 1990–2017 with comparison with the values expected on the basis of SDI alone. DALY, disability-adjusted life year; GBD, Global Burden of Disease; SDI, Socio-demographic Index.
Drowning
Drowning DALY rates between 1990 and 2017 decreased in almost every GBD region regardless of their SDI value (figure 6), except for Oceania, Eastern Europe and Southern Sub-Saharan Africa. Eastern and Western Sub-Saharan Africa, North Africa and Middle East, Andean, Tropical, Central and Southern Latin America, Western Europe and Australasia had better than expected DALY rates, while Oceania, East Asia and Eastern Europe had worse than expected DALY rates based on SDI.
Figure 6.

Co-evolution of drowning age-standardised DALY rates with SDI for the world and 21 GBD regions for 1990–2017 with comparison with the values expected on the basis of SDI alone. DALY, disability-adjusted life year; GBD, Global Burden of Disease; SDI, Socio-demographic Index.
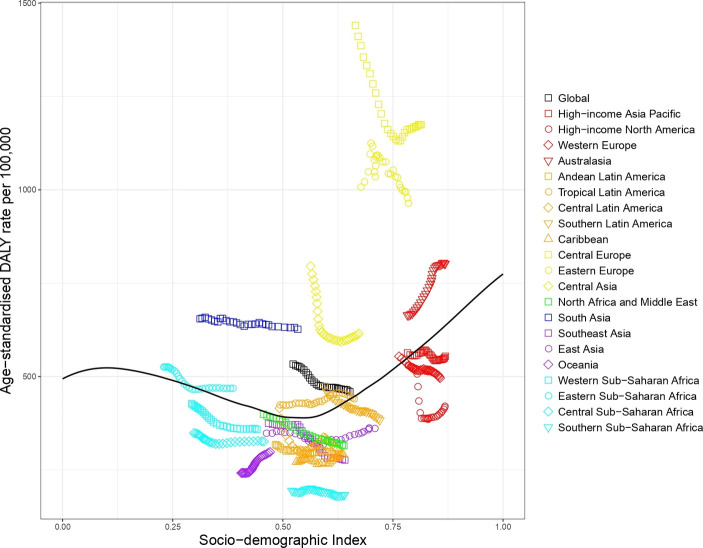
Falls
The patterns in falls globally followed more dynamic trends across regions as SDI increased from 1990 to 2017 (see figure 7). The regions that performed worse than expected in terms of SDI were Central Europe, Eastern Europe, South Asia, Central Asia and Australasia. Among these, Central Asia and Central Europe decreased and then increased, while Eastern Europe increased and then decreased. South Asia decreased steadily, while Australasia increased steadily until recent years. Among regions that performed better than expected, Oceania had increasing rates as SDI increased, while high-income North America dropped precipitously and then started increasing as SDI increased.
Figure 7.
Co-evolution of falls age-standardised DALY rates with SDI for the world and 21 GBD regions for 1990–2017 with comparison with the values expected on the basis of SDI alone. DALY, disability-adjusted life year; GBD, Global Burden of Disease; SDI, Socio-demographic Index.
Discussion
For many causes of injury, age-standardised DALY rates declined strikingly with increasing SDI, although road injury, interpersonal violence and self-harm did not strictly follow this pattern. Particularly for self-harm opposing patterns were observed in regions with similar SDI levels, for example, the trends in high-income Asia Pacific were opposite the trends in Western Europe, despite their proximity in terms of SDI. For road injuries, this effect was less pronounced; for nearly all regions, road injury DALY rates declined after 2005.
In Southern Sub-Saharan Africa, injury DALYs were worse than expected based on SDI in the overall injuries category as well as many of the specific injuries. In this region, road injury and interpersonal violence were important causes explaining the gap between observed and expected levels of overall injury DALYs. Many underlying and intertwining determinants of the high levels of interpersonal violence have been cited, including income inequality and poverty, high unemployment, rapid social change, corruption and poor rule of law, gender inequality, family breakdown, access to firearms, and alcohol and drug abuse.27 Despite these difficulties, however, and the worse-than-expected performance relative to SDI, our findings show that the DALY rates in Southern Sub-Saharan Africa have decreased from 2000 to 2017. This trend tallies with a reported declining number of injury deaths among young adults in South Africa.28
Of regions with a middle-high SDI, Eastern Europe stands out, because for most causes of injury, DALYs were much worse than expected based on SDI, particularly in the period 1990–2005. A compelling explanation for this finding may be the dissolution of the former Soviet Union and the resulting social and economic consequences on health and mortality.29 However, others have argued that causes of the health crisis are more complex and may result from a combination of historical and contemporary forces, including lifestyle habits, such as alcohol use, economic impoverishment, widening social inequality and the breakdown of political institutions.30 31 It should be noted that our study did aim to assess determinants of the burden of injury and caution is needed in attempting to draw conclusions with regard to possible reasons for regional trends and differences.
Another notable finding from our study was that for falls, at the higher levels of SDI, the composition of the disease burden shifted towards YLDs, rather than YLLs, as a more prominent driver of DALYs compared with areas with lower SDI. The proportion of DALYs due to YLDs also increases with higher levels of SDI among other injuries. It is possible that this shift in distribution reflects decreased mortality among injuries when people in higher SDI locations have access to better healthcare services. The shift in road injuries, for example, could be brought about by injury-prevention measures reducing the severity of the injury sustained (eg, seat belts and helmets) or by improved access to better quality care after an injury (eg, trauma systems). It is also possible that in age-standardised analyses, the shift towards YLDs may be due to the ageing of the population of countries with high SDI with commensurate age-related increases in injury incidence. For example, the incidence of falls increases substantially with age and most of the burden from falls in high-SDI countries occurs in the very old.32
Limitations
Our analysis has several limitations. First, as SDI and time are correlated, we may be over interpreting SDI as a driver of change as it could well be driven largely by other factors changing over time, not necessarily linked to SDI, such as climate change.
Second, limited data are available to quantify burden of injuries in the world. Major limitations of the cause-of-death data are low or absent coverage of vital registration or verbal autopsy data in many parts of the world, incompleteness of death certification systems and differences in the proportion of injury deaths classified in ill-defined codes.33–36 Few data were available for non-fatal injuries, and if data were available, injury was frequently recorded as a mix of cause and nature-of-injury codes and often a preponderance of nature-of-injury codes, while our analyses require attributing health outcomes to cause of injury. As a result, many non-fatal injury hospitals and emergency departments data sets could not be used. Furthermore, short-term duration of several nature-of-injury categories was based on expert-driven estimates because patient data was not available. Besides, gathering data on deaths and morbidity due to forces of nature (ie, disasters) and collective violence is complicated by the fact that their aftereffects may severely disrupt the infrastructure of vital and health registration systems.37 The statistical methods that we have used to assess mortality, incidence and prevalence can borrow strength over time and geography to ensure an estimate for all causes and all countries. Nevertheless, estimates for populations and time periods with few or absent data are inherently less precise.
Non-fatal injuries are reported by both cause of injury and nature of injury. Since our model requires a one-to-one relationship between cause-of-injury and nature-of-injury category, we developed a nature-of-injuries severity hierarchy that selects the injury that was likely to be responsible for the largest burden in a person with more than one injury. This means that we ignore the other injuries sustained by such individuals and this may have led to some underestimation of the burden of non-fatal injury. We decided to use such a hierarchy after it proved difficult to use statistical methods on sparse data to parse estimates across co-occurring injuries.
A second methodological limitation is the assessment of the probability of permanent health loss, one of the main drivers of non-fatal burden of disease. The probability of long-term injury was based on patient-reported outcome data from follow-up studies in just three countries. Also, long-term patient-reported outcome data may be influenced by response shift bias. Response shift is a change of outcome due to a change of the measurement perspective of the respondent (‘internal measurement scale’), where the usual change is towards adaptation. In our study, response shift may have resulted in an underestimation of the severity of long-term consequences of injury and consequently, to an underestimation of the non-fatal burden of injury.
Third, even though a strong correlation between SDI and injury DALYs, YLLs and YLDs was found, this cannot be interpreted as being causal in nature, because income per capita and education, two of the three components of SDI, were also used as covariates in all of the injury models except exposure to forces of nature and collective violence and legal intervention. In its original formulation, Murray et al suggested that SDI utility may be improved in the future through consideration of additional societal elements, such as inequality in each component.1
Conclusions
The overall pattern is that of declining injury burden with increasing development. Not all injuries follow this pattern, suggesting that there are multiple underlying mechanisms influencing injury outcomes. The detailed understanding of these patterns helps to inform countries how best to respond to changes in injury outcomes that occur with development and, in case of countries where health gains outpace development, may help to identify which prevention and/or healthcare measures have been taken in these countries.
What is already known on the subject.
Morbidity and mortality from injuries are known to be affected by socioeconomic development.
What this study adds.
This study provides more recent estimates of global morbidity and mortality from injuries with a greater level of detail than has previously been reported and with an updated method for measuring sociodemographic development.
This study found that many injuries decreased in terms of morbidity and mortality as sociodemographic development increased over time, but also identified important exceptions to this trend.
The study adds to the body of discussion on how economic development and sociodemographic changes should be considered in preventing future injury burden.
Acknowledgments
Mihajlo Jakovljevic Serbia acknowledges support through the Grant OI 175 014 of the Ministry of Education Science and Technological Development of the Republic of Serbia. Shahrzad Bazargan-Hejai acknowledges support through the NIH National Center for Advancing Translational Science (NCATS) UCLA CTSI Grant Number UL1TR001881". Ashish Awasthi acknowledges support from the Department of Science and Technology, Government of India, New Delhi through INSPIRE Faculty program. Rafael Tabarés-Seisdedos acknowledges support in part by grant number PROMETEOII/2015/021 from Generalitat Valenciana and the national grant PI17/00719 from ISCIII-FEDER. Abdallah M Samy acknowledges support from a fellowship from the Egyptian Fulbright Mission Program. Eduarda Fernandes acknowledges support ID/MULTI/04378/2019 and UID/QUI/50006/2019 with FCT/MCTES support through Portuguese national funds. Félix Carvalho acknowledges support ID/MULTI/04378/2019 and UID/QUI/50006/2019 with FCT/MCTES support through Portuguese national funds. Ilais Moreno Velásquezis acknowledges support from the Sistema Nacional de Investigacion, SENACYT (Panama). Louisa Degenhardt acknowledges support by an NHMRC research fellowship (#1135991) and by NIH grant NIDA R01DA1104470; The National Drug and Alcohol Research Centre is supported by funding from the Australian Government Department of Health under the Drug and Alcohol Program. Milena Santric Milicevic acknowledges the support from the Ministry of Education, Science and Technological Development, Republic of Serbia (Contract No. 175087). Kebede Deribe KD is supported by a grant from the Wellcome Trust [grant number 201900] as part of his International Intermediate Fellowship. Syed Aljunid acknowledges support from the International Centre for Casemix and Clinical Coding, Faculty of Medicine, National University of Malaysia and Department of Health Policy and Management, Faculty of Public Health, Kuwait University for the approval and support to participate in this research project. Jan-Walter De Neve was supported by the Alexander von Humboldt Foundation. Michael R Phillips acknowledges support from the Chinese National Natural Science Foundation of China (NSFC, No. 81371502). Sheikh Mohammed Shariful Islam acknowledges support from the National Heart Foundation of Australia and from a senior research fellowship from Deakin University. Duduzile Edith Ndwandwe acknowledges support from Cochrane South Africa, South African Medical Research Council.Tissa Wijeratne acknowledges the Department of Medicine, Faculty of Medicine, University of Rajarata, Saliyapura, Anuradhapura, Sri Lanka for their support.
Footnotes
Funding: Funding for GBD 2017 was provided by the Bill and Melinda Gates Foundation.
Competing interests: Dr. Carl Abelardo T Antonio reports personal fees from Johnson & Johnson (Philippines), Inc., outside the submitted work. Dr. Jasvinder Singh reports personal fees from Crealta/Horizon, Medisys, Fidia, UBM LLC, Medscape, WebMD, Clinical Care options, Clearview healthcare partners, Putnam associates, Spherix, the National Institutes of Health and the American College of Rheumatology, stock options in Amarin pharmaceuticals and Viking pharmaceuticals, participating in the steering committee of OMERACT, an international organization that develops measures for clinical trials and receives arm’s length funding from 12 pharmaceutical companies, including Amgen, Janssen, Novartis, Roche, UCB Group, Ardea/Astra Zeneca, Bristol Myers Squibb, Celgene, EliLilly, Horizon Pharma, Pfizer, and Centrexion. Dr. Josep Maria Haro reports personal fees from Roche and Lundbeck, and that the institute for which they work provides services to Eli Lilly and Co., outside the submitted work. Dr. Mete Saylan is an employee of Bayer AG, outside the submitted work. Dr Sheikh Mohammed Shariful Islam is funded by National Heart Foundation of Australia and supported by a senior research fellowship from Deakin University, outside the submitted work. Dr. Spencer James reports grants from Sanofi Pasteur, outside the submitted work.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data are available in a public, open access repository (ghdx.healthdata.org). Select data are available on reasonable request. Select input data may be obtained from a third party and are not publicly available.
References
- 1. Murray CJL, Barber RM, Foreman KJ, et al. . Global, regional, and national disability-adjusted life years (DALYs) for 306 diseases and injuries and healthy life expectancy (HALE) for 188 countries, 1990–2013: quantifying the epidemiological transition. The Lancet 2015;386:2145–91. 10.1016/S0140-6736(15)61340-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Haagsma JA, Graetz N, Bolliger I, et al. . The global burden of injury: incidence, mortality, disability-adjusted life years and time trends from the global burden of disease study 2013. Inj Prev 2016;22:3–18. 10.1136/injuryprev-2015-041616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Omran AR. The epidemiologic transition. A theory of the epidemiology of population change. Milbank Mem Fund Q 1971;49:509–38. 10.2307/3349375 [DOI] [PubMed] [Google Scholar]
- 4. Kassebaum NJ, Arora M, Barber RM, et al. . Global, regional, and national disability-adjusted life-years (DALYs) for 315 diseases and injuries and healthy life expectancy (HALE), 1990–2015: a systematic analysis for the global burden of disease study 2015. The Lancet 2016;388:1603–58. 10.1016/S0140-6736(16)31460-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ahmed N, Andersson R. Unintentional injury mortality and socio-economic development among 15-44-year-olds: in a health transition perspective. Public Health 2000;114:416–22. 10.1038/sj.ph.1900646 [DOI] [PubMed] [Google Scholar]
- 6. Moniruzzaman S, Andersson R. Relationship between economic development and risk of injuries in older adults and the elderly. A global analysis of unintentional injury mortality in an epidemiologic transition perspective. Eur J Public Health 2005;15:454–8. 10.1093/eurpub/cki014 [DOI] [PubMed] [Google Scholar]
- 7. Moniruzzaman S, Andersson R. Economic development as a determinant of injury mortality - a longitudinal approach. Soc Sci Med 2008;66:1699–708. 10.1016/j.socscimed.2007.12.020 [DOI] [PubMed] [Google Scholar]
- 8. Muazzam S, Nasrullah M. Macro determinants of cause-specific injury mortality in the OECD countries: an exploration of the importance of GDP and unemployment. J Community Health 2011;36:574–82. 10.1007/s10900-010-9343-5 [DOI] [PubMed] [Google Scholar]
- 9. Fountoulakis KN. Suicide and the economic situation in Europe: are we experiencing the development of a ‘reverse stigma’? Br J Psychiatry 2016;209:273–4. 10.1192/bjp.bp.115.171785 [DOI] [PubMed] [Google Scholar]
- 10. Vallin J. Socio-Economic determinants of mortality in industrialized countries. Popul Bull UN 1980;13:26–41. [PubMed] [Google Scholar]
- 11. Bishai D, Quresh A, James P, et al. . National road casualties and economic development. Health Econ 2006;15:65–81. 10.1002/hec.1020 [DOI] [PubMed] [Google Scholar]
- 12. Khan UR, Sengoelge M, Zia N, et al. . Country level economic disparities in child injury mortality. Arch Dis Child 2015;100(Suppl 1):S29–S33. 10.1136/archdischild-2013-305847 [DOI] [PubMed] [Google Scholar]
- 13. Wang H, Naghavi M, Allen C, et al. . Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the global burden of disease study 2015. The Lancet 2016;388:1459–544. 10.1016/S0140-6736(16)31012-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. GBD 2015 Disease and Injury Incidence and Prevalence Collaborators Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015: a systematic analysis for the global burden of disease study 2015. Lancet 2016;388:1545–602. 10.1016/S0140-6736(16)31678-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Lozano R, Naghavi M, Foreman K, et al. . Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the global burden of disease study 2010. The Lancet 2012;380:2095–128. 10.1016/S0140-6736(12)61728-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. GBD 2013 Mortality and Causes of Death Collaborators Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the global burden of disease study 2013. Lancet 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. A Haagsma J, Van Beeck EF, Toet H. Posttraumatic stress disorder following injury: trajectories and impact on health-related quality of life. J Depress Anxiety 2013;S4 10.4172/2167-1044.S4-002 [DOI] [Google Scholar]
- 18. Polinder S, van Beeck EF, Essink-Bot ML, et al. . Functional outcome at 2.5, 5, 9, and 24 months after injury in the Netherlands. J Trauma 2007;62:133–41. 10.1097/TA.0b013e31802b71c9 [DOI] [PubMed] [Google Scholar]
- 19. Ringburg AN, Polinder S, van Ierland MCP, et al. . Prevalence and prognostic factors of disability after major trauma. J Trauma 2011;70:916–22. 10.1097/TA.0b013e3181f6bce8 [DOI] [PubMed] [Google Scholar]
- 20. Ringburg AN, Polinder S, Meulman TJ, et al. . Cost-effectiveness and quality-of-life analysis of physician-staffed helicopter emergency medical services. Br J Surg 2009;96:1365–70. 10.1002/bjs.6720 [DOI] [PubMed] [Google Scholar]
- 21. United States National Study on the Costs and Outcomes of Trauma Care 2001-2003. Johns Hopkins Bloomberg School of Public Health, University of Washington, Westat, Inc.
- 22. van Loey NE, van Beeck EF, Faber BW, et al. . Health-related quality of life after burns: a prospective multicenter cohort study with 18 months follow-up. J Trauma Acute Care Surg 2011. [DOI] [PubMed] [Google Scholar]
- 23. Duan L, Deng X, Wang Y, et al. . The National injury surveillance system in China: a six-year review. Injury 2015;46:572–9. 10.1016/j.injury.2014.12.013 [DOI] [PubMed] [Google Scholar]
- 24. Agency for Healthcare Research and Quality (AHRQ) Medical Expenditure Panel Survey 1996-2012. [PubMed]
- 25. Mackenzie EJ, Rivara FP, Jurkovich GJ, et al. . The national study on costs and outcomes of trauma. J Trauma 2007;63(6 Suppl):S54–S67. 10.1097/TA.0b013e31815acb09 [DOI] [PubMed] [Google Scholar]
- 26. Fullman N, Yearwood J, Abay SM, et al. . Measuring performance on the healthcare access and quality index for 195 countries and territories and selected subnational locations: a systematic analysis from the global burden of disease study 2016. The Lancet 2018;391:2236–71. 10.1016/S0140-6736(18)30994-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Norman R, Matzopoulos R, Groenewald P, et al. . The high burden of injuries in South Africa. Bull World Health Organ 2007;85:695–702. 10.2471/BLT.06.037184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Bah S. Unnoticed decline in the number of unnatural deaths in South Africa. S Afr Med J 2004;94:442–3. [PubMed] [Google Scholar]
- 29. Grigoriev P, Shkolnikov V, Andreev E, et al. . Mortality in Belarus, Lithuania, and Russia: divergence in recent trends and possible explanations. Eur J Population 2010;26:245–74. 10.1007/s10680-010-9210-1 [DOI] [Google Scholar]
- 30. Chen LC, Wittgenstein F, McKeon E. The upsurge of mortality in Russia: causes and policy implications. Popul Dev Rev 1996;22:517–30. 10.2307/2137719 [DOI] [Google Scholar]
- 31. Men T, Brennan P, Boffetta P, et al. . Russian mortality trends for 1991-2001: analysis by cause and region. BMJ 2003;327 10.1136/bmj.327.7421.964 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Hartholt KA, Stevens JA, Polinder S, et al. . Increase in fall-related hospitalizations in the United States, 2001-2008. J Trauma 2011;71:255–8. 10.1097/TA.0b013e31821c36e7 [DOI] [PubMed] [Google Scholar]
- 33. Mahapatra P, Shibuya K, Lopez AD, et al. . Civil registration systems and vital statistics: successes and missed opportunities. The Lancet 2007;370:1653–63. 10.1016/S0140-6736(07)61308-7 [DOI] [PubMed] [Google Scholar]
- 34. Joubert J, Rao C, Bradshaw D, et al. . Characteristics, availability and uses of vital registration and other mortality data sources in post-democracy South Africa. Glob Health Action 2012;5:19263–19. 10.3402/gha.v5i0.19263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Obermeyer Z, Rajaratnam JK, Park CH, et al. . Measuring adult mortality using sibling survival: a new analytical method and new results for 44 countries, 1974-2006. PLoS Med 2010;7:e1000260 10.1371/journal.pmed.1000260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Setel PW, Macfarlane SB, Szreter S, et al. . A scandal of invisibility: making everyone count by counting everyone. The Lancet 2007;370:1569–77. 10.1016/S0140-6736(07)61307-5 [DOI] [PubMed] [Google Scholar]
- 37. Obermeyer Z, Murray CJL, Gakidou E. Fifty years of violent war deaths from Vietnam to Bosnia: analysis of data from the world health survey programme. BMJ 2008;336:1482–6. 10.1136/bmj.a137 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
injuryprev-2019-043296supp001.pdf (64.6KB, pdf)
injuryprev-2019-043296supp002.pdf (65.2KB, pdf)
injuryprev-2019-043296supp003.pdf (64.7KB, pdf)
injuryprev-2019-043296supp004.pdf (64.5KB, pdf)
injuryprev-2019-043296supp005.pdf (108.4KB, pdf)