Abstract
Background
Past research in population health trends has shown that injuries form a substantial burden of population health loss. Regular updates to injury burden assessments are critical. We report Global Burden of Disease (GBD) 2017 Study estimates on morbidity and mortality for all injuries.
Methods
We reviewed results for injuries from the GBD 2017 study. GBD 2017 measured injury-specific mortality and years of life lost (YLLs) using the Cause of Death Ensemble model. To measure non-fatal injuries, GBD 2017 modelled injury-specific incidence and converted this to prevalence and years lived with disability (YLDs). YLLs and YLDs were summed to calculate disability-adjusted life years (DALYs).
Findings
In 1990, there were 4 260 493 (4 085 700 to 4 396 138) injury deaths, which increased to 4 484 722 (4 332 010 to 4 585 554) deaths in 2017, while age-standardised mortality decreased from 1079 (1073 to 1086) to 738 (730 to 745) per 100 000. In 1990, there were 354 064 302 (95% uncertainty interval: 338 174 876 to 371 610 802) new cases of injury globally, which increased to 520 710 288 (493 430 247 to 547 988 635) new cases in 2017. During this time, age-standardised incidence decreased non-significantly from 6824 (6534 to 7147) to 6763 (6412 to 7118) per 100 000. Between 1990 and 2017, age-standardised DALYs decreased from 4947 (4655 to 5233) per 100 000 to 3267 (3058 to 3505).
Interpretation
Injuries are an important cause of health loss globally, though mortality has declined between 1990 and 2017. Future research in injury burden should focus on prevention in high-burden populations, improving data collection and ensuring access to medical care.
Keywords: burden of disease, global, descriptive epidemiology
Introduction
Injury burden assessments are a critical component of population health measurement. Across the global landscape of population health research, injuries are unique in that they are almost universally avertable yet can cause death or disability at any age. Even common injuries such as concussion resulting from falls, violence or road injuries may cause longer term sequelae, and injuries such as spinal cord injuries or limb amputations can cause long-term disability.1 As a result, injuries are recognised as being a source of lost health and human capital that could be averted with improved safety and prevention programmes as well as ensuring access to care resources.2 Across geographies, certain injuries such as envenomation may be relevant in specific locations where venomous creatures live, while injuries such as those occurring from adverse medical events are an increasing area of research in higher income areas of the world.3–5 Bolstering such programmes, however, requires detailed measurement of when, where and to whom injuries are occurring, necessitating focused research studies to add insight and context to broader geographical trends. Across all domains of injury prevention research, it is important to measure the causes of injury, such as road injuries, and the resulting disability, such as fractures, burns or traumatic brain injury, that can occur as a result. Such detailed measurement lends perspective for understanding burden and anticipating resources needed to care for and hopefully prevent future injury burden. Detailed measurements and assessments of this nature are critical for empowering policy makers and health system planners to appropriately plan and invest for mitigating future health loss from injuries. Reducing injury burden is an important component in global efforts such as the Sustainable Development Goal 3 to ‘ensure healthy lives and promote well-being for all at all ages’.6
While some research has focused on a certain type of injury or outcome from injury or specific area of the world,7–10 it has become important in an era of more sophisticated population health measurement to measure health loss from injuries comprehensively with detailed fatal and non-fatal estimates for different ages, sexes, across time periods and accounting for multiple different types of morbidity that can occur in an injury. Previously published literature on global injury burden through 2015 has provided comprehensive measurements of health loss due to injuries but still require regular updates to help inform research and policy, as new years of estimates are added and as new injuries and injury outcomes are incorporated.11 Comprehensive research of this nature shows how injury burden varies dynamically by age, sex, year, area of the world and type of injury, and hence, it is important to maintain close monitoring of injury burden every year in all parts of the world. In addition, as new datasets and statistical modelling methods become available, producing regular updates to burden estimation also ensures that results are as accurate as possible.
While the burden of injuries is widely studied and monitored through various methods of research, the Global Burden of Diseases, Injuries, and Risk Factors (GBD) Study is the only study framework that routinely provides estimates of morbidity and mortality from an exhaustive list of injuries in all areas of the world across ages and sexes. The most recent update to GBD was published in 2018 and provided morbidity and mortality estimates for 30 mutually exclusive causes of injury for 195 countries from 1990 to 2017.12–17 As part of this regular update, new datasets on cause of death and incidence are incorporated into the study, and additional geographical detail is added to better measure heterogeneity in burden estimates at a subnational level. In addition, updates such as reporting both nature of injury and cause of injury (described in more detail below) are incorporated. In this study, we describe key components in the GBD injury methodology and provide results from key trends in injury burden in terms of incidence, prevalence, years lived with disability (YLDs), cause-specific mortality, years of life lost (YLLs) and disability-adjusted life years (DALYs) by country, age groups, sex, year and injury type.
Methods
The methods and results in this study are the same as are provided in GBD capstone publications, and a detailed description of GBD data and methods used for all processes related to GBD 2017 is provided in associated studies.12–17 Overall, GBD methods are also summarised in online supplementary appendix 1. Below, we summarise the specific methods used for measurement of injuries morbidity and mortality in GBD 2017.
injuryprev-2019-043494supp001.pdf (64.6KB, pdf)
Key components of GBD study design
The GBD study incorporates several key components to allow for internally consistent estimates across all burden measures and metrics. First, population is measured to ensure consistent denominators for all population-level measurement. Second, all-cause mortality is measured using demographic methods. Third, cause-specific mortality for a mutually exclusive, collectively exhaustive hierarchy of diseases and injuries is measured, such that every death has one underlying cause of death and such that estimates for every possible cause of death are included, which requires the use of residual causes like ‘other transport injuries’. This results in the sum of cause-specific mortality equalling total all-cause mortality. Fourth, non-fatal health loss is measured for individuals living with a disease or injury that detracts from their full health status. Fifth, a composite measure of mortality and morbidity is computed. These steps are conducted within an age, sex and location hierarchy constructed such that demographic detail is available but where all estimates are internally consistent with all other estimates. GBD produces estimates for all causes, ages, sexes, years and locations. Risk factors and attributable burden for different are also measured, but those results are not included in this study.
Case definition and cause hierarchy
The GBD case definition for an injury death is a death where the injury was the underlying cause of death. For example, if an individual falls on ice and sustains an epidural haematoma and dies after a seizure, the fall is the underlying cause. If an individual sustains a myocardial infarction and then falls and sustains the same epidural haematoma, then the myocardial infarction is the underlying cause of death. For non-fatal injuries, we define a case as an injury that warranted medical care. For example, if an individual slips and falls but does not sustain any bodily injury, it is not considered an injury. Online supplementary appendix table 1 provides the International Classification of Disease (ICD) codes used to identify causes of injury.
injuryprev-2019-043494supp002.pdf (82.7KB, pdf)
Cause-specific mortality estimation
Cause-specific mortality from injuries is measured using the Cause of Death Ensemble model (CODEm). CODEm is described in more detail elsewhere; a summary of its use for injuries is as follows.18 First, all available data that can be used for cause of death estimation are identified. For injuries, this includes vital registration, verbal autopsy, police records, mortuary data and census data. These data are processed for use in the GBD cause and demographic hierarchy via a series of data processing steps including a process whereby ill-defined causes of death are reassigned to true underlying causes of death, which is described in more detail elsewhere but essentially is the process by which ill-defined causes of death are reclassified to causes of death in the GBD cause hierarchy.19 20 Next, a cause-specific mortality model is developed for each one of the 30 different causes of injury. For example, falls are modelled differently than road injuries, though both use the same CODEm modelling architecture. For each cause of injury, covariates that may be associated with the cause are identified and added as candidate covariates. CODEm runs different combinations of models using different covariates and outcome variables, specifically cause fraction models and cause-specific mortality rate models. Ensembles of models are also conducted to test performance of overall models formed from submodels. Once all models have been run, the top-performing models are selected based on out-of-sample predictive validity, wherein the model makes predictions on data that were not included in developing the model. The top-performing models are then weighted according to performance, and the final estimates form the penultimate estimate for cause-specific mortality from that injury. Those estimates are then adjusted to fit within the all-cause mortality estimate, so that cause-specific deaths sum up to the overall mortality estimate for each population and demographic. YLLs are computed as the cause-specific mortality rate at a given age multiplied by the residual life expectancy at that age, which is based on the observed maximum global life expectancy.
Non-fatal injury estimation
Non-fatal injury estimation is also described in more detail in GBD literature. Key components in this process are as follows. First, data on incidence of non-fatal injury causes (eg, road injuries) is obtained from the GBD collaborator network and other injury research groups and researchers around the world. Data are cleaned and organised according to GBD study guidelines. Next, incidence of each cause of injury is modelled in DisMod-MR 2.1, which is a Bayesian meta-analysis tool used extensively in GBD research. Incidence estimates of injuries requiring medical care for each cause of injury then stream through an analytical pipeline. During this process, injury incidence is split into inpatient and outpatient to account for the different severity that is expected to occur. The coefficient that determines this split is derived from locations where both inpatient and outpatient data are available. After this, we measure the proportion of each cause of injury that leads to one of 47 different natures of injury using clinical data where both cause and nature are coded as well a Dirichlet statistical modelling process. Based on these steps, the incidence of each cause is also split into incidence of each cause-nature, which is the proportion of a given cause’s incidence leading to some specific nature of injury being the most severe injury sustained as estimated by the Dirichlet regression. These estimates are then converted to short-term and long-term injuries based on probability of each injury becoming long term, as determined by long-term follow-up injury surveys.21–27 For short-term injuries, incidence is converted to prevalence based on multiplying incidence by an expected duration of injury as determined by physicians and injury experts involved in the GBD study. For long-term injuries, incidence is converted to prevalence using differential equations that take into account the increased mortality for certain types of injury, for example, traumatic brain injury.1 Disability weights as derived elsewhere in the GBD study are then used to measure disability based on nature of injury.28 These measures are then summed across natures of injury for each cause to calculate YLDs. Each of these steps is conducted for every cause, age, sex, year and location in the GBD study design. Associated literature provides more detail on each of these steps.12–17
DALY measurement
DALYs are calculated by summing YLLs and YLDs for each cause, age, sex, year and location.
Uncertainty measurement
Uncertainty is measured at each step of the analytical process based on the sample size, SE or original uncertainty interval (UI) from each input to the study. Uncertainty is propagated through each step of the analysis by maintaining distributions of 1000 draws on which each analytical step is conducted. Final 95% UIs are determined based on the 25th and 975th values of the ordered values across draws.
Code and results
Steps of the analytical process were conducted in Python version 2.7, Stata V.13.1 or R version 3.3. All steps of the analytical process are available online at ghdx.healthdata.org. This study reports a subset of measures and metrics for every cause of injury. All results and results with additional detail by age, sex, year and location can be downloaded at ghdx.healthdata.org.
Guidelines for Accurate and Transparent Health Estimates Reporting (GATHER) statement
This study is adherent with guidelines from the GATHER (described in more detail in online supplementary appendix 2).29
injuryprev-2019-043494supp003.pdf (87.6KB, pdf)
Results
Online supplementary appendix table 2 shows age-standardised incidence, prevalence, YLDs, deaths, YLLs and DALYs in 2017 by country as well as percentage change and UI from 1990 for each metric. Online supplementary appendix table 3 shows all-age numbers (ie, not divided by population) of incidence, prevalence, YLDs, deaths, YLLs and DALYs in 2017 by country as well as percentage change from 1990 and UI for each metric. In some instances, the UI for the per cent change crosses zero, meaning that statistically there was no significant difference. Online supplementary appendix figures 1–6, show the incidence and mortality from transport injuries, unintentional injuries, and interpersonal violence and self-harm by country for 2017 as well as the percentage change for both incidence and mortality between 1990 and 2017. All other results including age-specific and sex-specific results can be viewed and downloaded via freely and publicly available tools at ghdx.healthdata.org.
injuryprev-2019-043494supp004.pdf (147.8KB, pdf)
injuryprev-2019-043494supp005.pdf (167.9KB, pdf)
injuryprev-2019-043494supp006.pdf (17MB, pdf)
injuryprev-2019-043494supp007.pdf (17MB, pdf)
injuryprev-2019-043494supp008.pdf (17MB, pdf)
injuryprev-2019-043494supp009.pdf (17MB, pdf)
injuryprev-2019-043494supp010.pdf (17MB, pdf)
injuryprev-2019-043494supp011.pdf (17MB, pdf)
Global trends in overall injury burden
In terms of fatal outcomes, deaths due to all injuries increased from 4 260 493 (4 085 700 to 4 396 138) in 1990 to 4 484 722 (4 332 010 to 4 585 554) in 2017, while YLLs decreased from 232 104 206 (219 920 058 to 241 973 733) to 195 231 148 (188 807 653 to 199 825 464) and age-standardised mortality rates decreased from 1079 (1073 to 1086) to 738 (730 to 745) per 100 000. In terms of non-fatal outcomes, all-injury incidence (new cases) increased from 354 064 302 (338 174 876 to 371 610 802) in 1990 to 520 710 288 (493 430 247 to 547 988 635) in 2017, and YLDs increased from 37 452 031 (27 805 854 to 49 010 103) to 57 174 469 (42 073 855 to 75 427 036), while age-standardised incidence rates decreased non-significantly from 6824 (6534 to 7147) to 6763 (6412 to 7118) per 100 000. In terms of DALYs, age-standardised DALY rates decreased from 4947 (4655 to 5233) per 100 000 in 1990 to 3267 (3058 to 3505) in 2017.
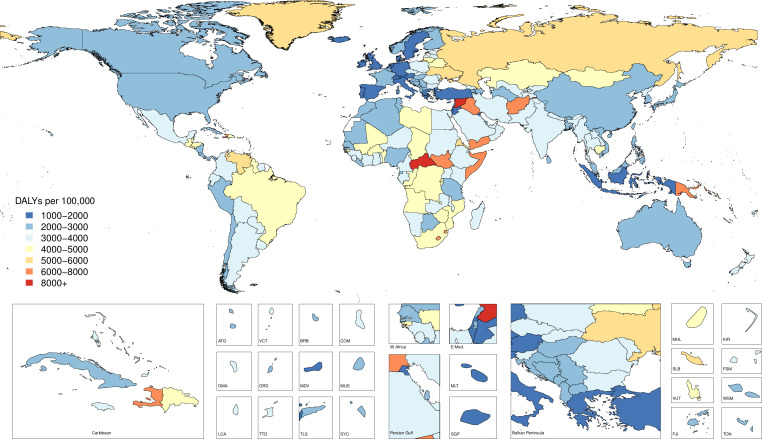
Figure 1 shows age-standardised DALY rates by country for 2017. While certain countries—specifically, Syria, Central African Republic and Iraq—have much higher DALY rates than most other countries, there still exists considerable heterogeneity across countries that are not among these countries with the highest burden. South Sudan, Somalia and Yemen have much higher injury burden than much of the rest of the world, for example, with age-standardised DALY rates of 7391.51 per 100 000 (6536.44 to 8440.14), 7364.66 per 100 000 (6143.11 to 8960.58) and 7297.88 per 100 000 (6525.7 to 8438.15), respectively. Papua New Guinea also demonstrates high all-injury burden with 6803.33 DALYs per 100 000 (5652.2 to 8040.89) in 2017.
Figure 1.
Age-standardised DALY rates by country, 2017. DALYs, disability-adjusted life years.
Figure 2 presents deaths as a stacked graph for overall injury groups and population from 1990 to 2017 with labelled fatal discontinuities, defined as changes in deaths due to sudden, unexpected spikes in mortality that depart from the underlying mortality trend.13 Although population has steadily increased in the 28 years of the study, deaths per year due to injuries have remained relatively consistent over time. Natural disasters, such as earthquakes, have caused pronounced spikes in unintentional injuries deaths, while conflict and genocide have caused spikes in deaths in the interpersonal violence injury category.
Figure 2.
Global deaths for level 2 injuries and population from 1990 to 2017 with labelled fatal discontinuities.
All-injury YLDs and YLLs by country in 2017
Figure 3 shows the percentage of total all-age, combined-sex YLDs by country in 2017. This figure shows several geographical patterns that help depict the non-fatal burden of injuries globally in terms of their relative contribution to overall disability. First, the percentage of total disability caused by injuries varies widely by country. Mauritius experiences only 3.04% (2.79% to 3.29%) of non-fatal burden from injuries, while Slovenia experiences 19.11% (17.11% to 21.27%) of non-fatal burden from injuries. In other words, if all disability in these two populations is combined in 2017, there is over sixfold variation in how much of this disability was caused by injuries. These patterns also reflect burden from non-injury conditions, since locations with higher burden from communicable disease may have correspondingly lower proportion due to injuries. As an extension of these geographical trends, this map makes it evident that there are striking regional patterns in non-fatal injury burden. Eastern and Central Europe and Central Asia as well as Australasia have a notably higher percentage of total non-fatal burden from injuries than countries in other regions, while these percentages are relatively lower in most areas of Africa, the Americas and areas of South, East and Southeast Asia. To some extent, this map also reflects the underlying burden from non-injury causes, too, since areas of the world with high non-fatal disability from conditions such as anaemia, communicable diseases and other types of health loss could have correspondingly higher percentages of disability from these conditions instead of injuries. This map also shows examples of positive deviations from global trends; Indonesia, for example, has a relatively low percentage of non-fatal health loss due to injuries compared with many other countries.
Figure 3.
Percentage of YLDs in all ages due to injuries in 2017. YLDs, years lived with disability.
Figure 4 similarly shows the percentage of total all-age, combined-sex YLLs by country in 2017. This figure interestingly shows how mortality patterns demonstrate different geographical trends than the non-fatal burden, as depicted in figure 2, though it should be noted that YLLs will also be disproportionately higher in younger populations, all else being equal. In particular, the locations with the highest percentage of YLLs due to injuries are in certain countries in North Africa and the Middle East, including Syria, where 59.51% (56.59% to 62.35%) of YLLs were due to injuries in 2017, and Iraq, where 41.34% of YLLs were due to injuries in 2017. Areas of Latin America including Venezuela, Honduras and Belize also have a relatively high percentage of total YLLs due to injuries. Conversely, certain areas of the world also demonstrate a relatively low percentage of total YLLs due to injuries, specifically, certain countries in Africa such as Nigeria and Madagascar have relatively lower percentages, though this also reflects relatively higher mortality from other non-injury causes in these countries.
Figure 4.
Percentage of YLLs in all ages due to injuries in 2017. YLLs, years of life lost.
Cause-specific DALY rates by sex
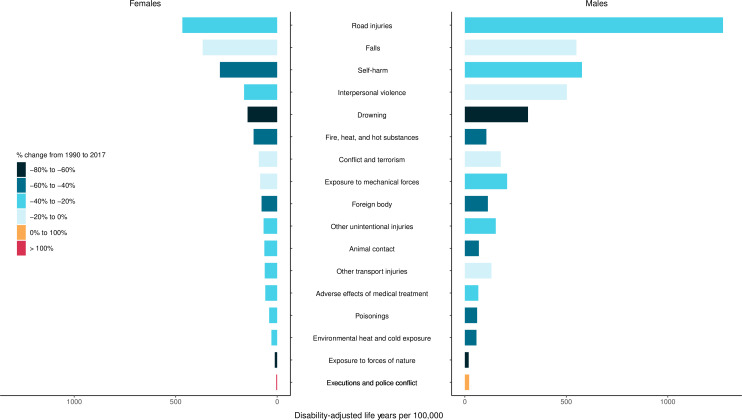
Figure 5 shows cause-specific DALY rates by sex for 17 injuries in 2017 as well as percentage change from 1990 to 2017 by cause and sex. The black and dark blue bars show causes with greater relative improvement over the time period of this study, while lighter blue, orange and red show injuries that have had lesser improvements, no improvements or increasing burden over time.
Figure 5.
Age-standardised DALY rates by sex for injuries in level 3 of the GBD cause hierarchy in 2017 and percentage change from 1990 to 2017. DALY, disability-adjusted life year; GBD, Global Burden of Disease.
In 2017, men experienced higher age-standardised DALY rates than women for all injuries except fire, heat and hot substances. The most marked differences, where DALY rates for men are more than double those of women, can be seen in self-harm, interpersonal violence, road injuries, other transport injuries, exposure to mechanical forces, environmental heat and cold exposure, and executions and police violence. Road injuries (1272 (1209 to 1331) per 100 000), self-harm (577 (525 to 604)) and falls (550 (462 to 653)) were the causes with the highest DALY rates for men in 2017. Women had the highest DALY rates due to the same injuries, but at a lesser magnitude, with rates of 467 (432 to 502) per 100 000 for road injuries, 367 (304 to 442) for falls and 282 (268 to 293) for self-harm.
The causes with the largest decreases in DALY rates for men from 1990 to 2017 were exposure to forces of nature (72.4% (63.8% to 79.1%)), drowning (62.7% (58.8% to 65.4%)) and fire, heat and hot substances (43.6% (26.4% to 49.9%)). For women, exposure to forces of nature (72.8% (63.8% to 79.6%)), drowning (65.8% (58.6% to 69.2%)) and self-harm (50.8% (48.2% to 55.9%)) had the largest decreases in DALY rates. The only increases in DALY rates were seen in executions and police conflict for both women (298.0% (257.1% to 389.0%)) and men (46.4% (31.2% to 173.0%)).
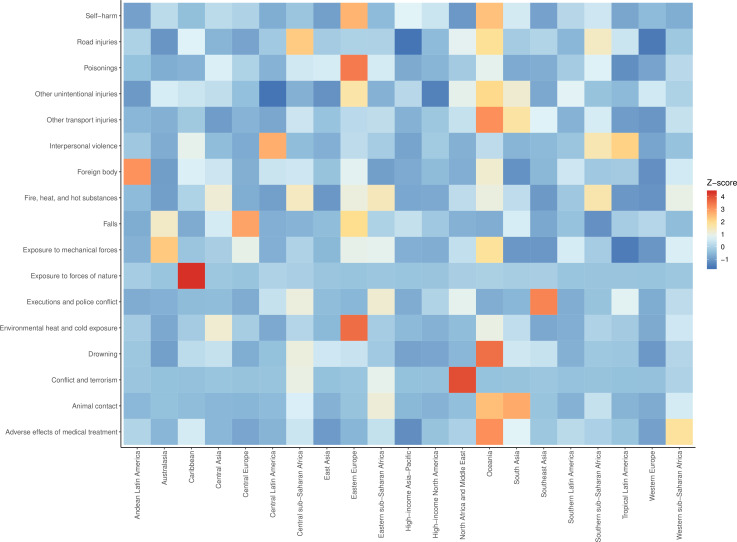
Comparative regional DALY rates in 2017
Figure 6 shows a heatmap of the number of standard deviations (SD) above or below the mean of a row (ie, a Z-score) of age-standardised DALY rates for select injuries by GBD region in 2017. For example, the figure shows that the rate of age-standardised DALYs in Eastern Europe is approximately three SD higher than the across mean age-standardised DALY rates of environmental heat and cold exposure across all regions. Poisonings is also a cause with an age-standardised DALY rate that is approximately three SD higher than in other regions. Positive deviance is seen in high-income Asia Pacific for road injuries, where age-standardised DALYs are one SD lower than the mean across regions. Conversely, Central sub-Saharan Africa has age-standardised DALY rates that are two SD higher than the mean across regions. This figure also demonstrates how certain causes have relatively less variation across regions, for example, most regions do not deviate from the mean age-standardised DALY rates across regions for exposure to forces of nature, with the exception of the Caribbean, which had an age-standardised DALY rate that was approximately four SD above the mean across regions in 2017. Oceania and Eastern Europe stand out as having higher DALY rates for select injuries than other regions, while East Asia, high-income Asia Pacific, high-income North America, Western Europe and Southern Latin America experienced less than average burden of injuries in 2017.
Figure 6.
Heatmap showing the Z-score of age-standardised mean DALY rates for select injuries by GBD region in 2017. GBD, Global Burden of Disease.
Discussion
Measuring, understanding and acting on the global burden of injuries should be considered a foundational component of population health research. While this study has reviewed injury burden trends from GBD 2017, it is also evident that these trends are sufficiently different by injury type and geography that it becomes difficult to succinctly generalise the findings in this study. Nevertheless, this study reveals themes and principles germane to the state of global injury burden in 2017 that are relevant to injury burden and prevention research.
First, it should be recognised that despite global population growth with increases in injury cases and deaths, age-standardised death rates from injuries declined from 1990 to 2017. More research into successful improvements for specific injuries in specific countries should be more investigated to help guide efforts towards future improvements. In general terms, the reduction in injury mortality likely represent the combined effects of improvements in healthcare systems, investments in injury prevention programmes and, in certain circumstances, safety improvement such as vehicle safety testing, helmet, seatbelt and drinking and driving laws. While burden trends across all diseases and injuries vary by geography and time, these improvements in injury burden are generally consistent with reporting of communicable and non-communicable disease trends reported in GBD 2017.
Despite improvements in terms of rates, however, it is important to consider the impact of absolute injury burden in younger and adult ages on the social capital and workforce in a country. Second, in reviewing temporal trends in figure 2, it becomes evident that war and conflict and environmental disasters can cause profound increases in deaths over a short period of time. This unfortunate and tragic reality should be made more broadly visible as issues such as war, conflict and climate change continue to threaten the populations of the 21st century. Third, sex differentials in the burden of different injury types are large, with men experiencing significantly higher burden from the four leading causes of injury DALYs in 2017. Preventive research and focused interventions into why this is occurring in road injuries, falls, self-harm, interpersonal violence and drowning is critical. It is also critical to address injuries such as fire, heat and hot substance and sexual violence where females experience greater burden and to better understand the factors that drive sex differences. As a fourth theme, we observed that there are cases of both positive and negative deviance from cross-region trends for each injury, as shown in figure 6, which appear to occur even outside of expected differences by income group. For example, understanding why high-income Asia Pacific and Western Europe are performing better than high-income North America in road injury burden could help improve road injury burden even in this higher income setting.
Beyond these four themes, there are evidently a great deal of nuances and specific outcomes to measure and understand in future injury research. While every cause of health loss in a population is important to measure and understand, injuries are unique in that understanding burden requires investigation of an array of circumstances such as infrastructure, the built environment, rates of interpersonal violence in a population and individual behaviours such as alcohol intoxication or drug use. The findings in this paper also demonstrate how it is critical to measure and understand the spectrum of health loss due to injuries ranging from relatively silent injuries to injuries that profoundly affect functional status. An incident as elemental as a trip and fall can lead to profoundly disabling health consequences such as spinal cord injury, which can have lifelong disability. The disability caused by shorter term injuries, such as an arm fracture, in addition to causing suffering and disability, can cause loss of human capital.30 While this study focused more on the causes of injury as defined in the GBD cause hierarchy, future GBD studies should focus also on depicting the distribution of nature of injury results to better understand how these types of disability affect an individual’s functional status. Such analyses become increasingly meaningful as research emerges on, for example, the increased risk of dementia that traumatic brain injury patients may experience.31 The findings in this paper also demonstrate how measuring injury burden necessitates review of the population factors that affect injury risk. For example, an event as disastrous as an earthquake may have radically different impacts on a population depending on infrastructure and access to care resources. Understanding how populations can protect themselves against future, unanticipated catastrophe could lead to averted death and disability in the future. As was shown in figure 2, catastrophic events both in terms of natural disasters and war and conflict can significantly add to the death and disability experienced by a population in a short period of time.
The geographical trends shown in this paper are also critical to review and understand by the broader global health community. As shown in figure 6, considerable heterogeneity exists across regions for certain causes. While vehicles were driven in nearly every populated area of earth in 2017, this study shows that different regions of the world have markedly different rates of death and disability resulting from road injuries, underscoring the importance of measuring and understanding the effects of specific factors on injury burden.32 It is not necessarily surprising to observe that countries or regions with relatively lower healthcare access and quality, less road safety infrastructure and lower utilisation of vehicles with modern safety standards would have higher rates of road injuries DALYs. The question that extends from this observation, however, is the extent to which burden from this type of injury cause could be avoided were every country to have the safety and prevention factors available in higher income settings. The injury and safety research communities should consider future investigation of counterfactual analyses to better measure and understand the impact that road safety legislation, modernisation of roads and vehicles and improving first response medical care could have on road injury burden, as an example, though parallel examples can be developed for other injury causes as well. This research could help cost-effectiveness analyses and guide investment in safer infrastructure.
These observations converge on a common theme: much of the injury burden may be largely preventable and understanding the success or failure of different prevention efforts should be a prioritised area of health research. Moreover, it is critical for there to be continued engagement across different areas of the world for the purposes of discussing effective and ineffective injury prevention strategies. Dialogue focused on findings across injury prevention efforts via forums such as global safety conferences as well as studies published in research journals should continue to help policy makers and public health planners make strategic investments for preventing future injury burden.33 In addition, more research into the cause of injury and resulting bodily injury and environmental and contextual features where injuries occur such type of road in a road injury or fires in factories versus in residences may provide further insight into preventing future injury burden.
Known limitations of injury burden estimation in the GBD framework have been reported previously in peer-reviewed literature.1 11 13 16 Generally, identified limitations include data sparsity and correspondingly greater uncertainty in certain geographies, limited geographical coverage of data informing long-term disability estimates and cause–nature relationships, and potential reporting biases for injuries such as self-harm and interpersonal violence. These limitations have been discussed in the aforementioned literature, and this overview study was additionally limited in scope due to the extensive size of the GBD cause hierarchy and location hierarchy. Indeed, over 1400 different cause–nature combinations are available for reporting in the GBD cause hierarchy, and future research would benefit from examining results in the detailed cause hierarchy and across the detailed location, age and sex hierarchy. The GBD Study platform and collaborator network provide a constructive collaborative platform on which future assessments can be conducted and published.
Conclusion
Injury burden is complex but foundational in formulating global health loss. We have identified four broad trends in global injury burden that converge on the principle that injuries should be considered largely preventable but that detailed burden estimates through recent years are a critical global resource to inform meaningful policy. It will be important accurate measurement to continue into the future to guide injury prevention policy.
What is already known on the subject.
Injury burden globally varies across many dimensions but remains as an important component of global health loss. Regular updates in injury burden measurement are critical.
Injuries can be largely preventable, but prevention efforts must be guided by up-to-date estimates of injury burden that can be used on an age-specific, sex-specific, year-specific, location-specific and injury-specific basis.
What this study adds.
This study incorporates updated data and methods that were used in Global Burden of Disease 2017 with updated burden estimates for the year 2017, as well as newly available results in terms of nature of injury.
Global age-standardised mortality and disability-adjusted life years decreased between 1990 and 2017. Decreases in age-standardised incidence were not statistically significant.
Trends over time vary depending on the specific injury, sex and location.
Injury burden in a population can be radically affected by war, civil conflict and natural disasters.
Acknowledgments
Syed Aljunid acknowledges the Department of Health Policy and Management, Faculty of Public Health, Kuwait University and International Centre for Casemix and Clinical Coding, Faculty of Medicine, National University of Malaysia and for the approval and support to participate in this research project. Alaa Badawi acknowledges support from the Public Health Agency of Canada. Till Bärnighausen acknowledges support from the Alexander von Humboldt Foundation through the Alexander von Humboldt Professor award, funded by the German Federal Ministry of Education and Research. Felix Carvalho acknowledges UID/MULTI/04378/2019 support with funding from FCT/MCTES through national funds. Vera M Costa acknowledges her grant (SFRH/BHD/110001/2015), received by Portuguese national funds through Fundação para a Ciência e Tecnologia (FCT), IP, under the Norma Transitória DL57/2016/CP1334/CT0006. Kebede Deribe acknowledges support from a grant from the Wellcome Trust [grant number 201900] as part of his International Intermediate Fellowship. Tim Driscoll acknowledges the work on occupational risk factors was partially supported by funds from the World Health Organization. Eduarda Fernandes acknowledges UID/QUI/50006/2019 support with funding from FCT/MCTES through national funds. Yuming Guo acknowledges support from Career Development Fellowships of the Australian National Health and Medical Research Council (numbers APP1107107 and APP1163693). Sheikh Mohammed Shariful Islam acknowledges funding by a Fellowship from National Heart Foundation of Australia and Institute for Physical Activity and Nutrition, Deakin University. Mihajlo Jakovljevic acknowledges support by the Ministry of Education Science and Technological Development of the Republic of Serbia through the Grant number OI175014; publication of results was not contingent upon Ministry's censorship or approval. Sudha Jayaraman acknowledges support from: NIH R21: 1R21TW010439-01A1 (PI); Rotary Foundation Global Grant #GG1749568 (PI); NIH P20: 1P20CA210284-01A1 (Co-PI); DOD grant W81XWH-16-2-0040 (Co-I) during the submitted work. Yun Jin Kim acknowledges support from a grant from the Research Management Centre, Xiamen University Malaysia [grant number: XMUMRF/2018-C2/ITCM/0001]. Kewal Krishan acknowledges support by UGC Centre of Advanced Study (CAS II) awarded to the Department of Anthropology, Panjab University, Chandigarh, India. Manasi Kumar acknowledges FIC/NIH funding from grant K43 1K43MH114320-01. Amanda Mason-Jones acknowledges institutional support from the University of York. Walter Mendoza is currently Program Analyst Population and Development at the Peru Country Office of the United Nations Population Fund-UNFPA, which not necessarily endorses this study. Mariam Molokhia acknowledges support from the National Institute for Health Research Biomedical Research Center at Guy’s and St Thomas’ National Health Service Foundation Trust and King’s College London. Ilais Moreno Velásquez acknowledges support by the Sistema Nacional de Investigación (SNI, Senacyt, Panama). Mukhammad David Naimzada acknowledges support from Government of the Russian Federation (Agreement No – 075-02-2019-967). Stanislav S. Otstavnov acknowledges the support from the Government of the Russian Federation (Agreement No – 075-02-2019-967). Ashish Pathak acknowledges support from the Indian Council of Medical Research (ICMR), New Delhi, India (Grant number 2013-1253). Michael R Phillips acknowledges support in part by a grant from the National Science Foundation of China (No. 81761128031). Marina Pinheiro acknowledges FCT for funding support through program DL 57/2016-Norma transitória. Abdallah M. Samy acknowledges support from a fellowship from the Egyptian Fulbright Mission Program. Milena Santric Milicevic acknowledges the support from the Ministry of Education, Science and Technological Development, the Republic of Serbia (Contract No. 175087). Seyedmojtaba Seyedmousavi acknowledges support from the Intramural Research Program of the National Institutes of Health, Clinical Center, Department of Laboratory Medicine, Bethesda, MD, USA. Rafael Tabarés-Seisdedos acknowledges support in part by the national grant PI17/00719 from ISCIII-FEDER. Sojib Bin Zaman acknowledges support from an "Australian Government Research Training Program (RTP) Scholarship." Louisa Degenhardt acknowledges support from an Australian National Health and Medical Research Council (NHMRC) Senior Principal Research Fellowship (#1135991) and by a National Institute of Health (NIH) National Institute on Drug Abuse (NIDA) grant (R01DA1104470).
Footnotes
Funding: Bill and Melinda Gates Foundation OPP1152504.
Map disclaimer: The depiction of boundaries on the map(s) in this article do not imply the expression of any opinion whatsoever on the part of BMJ (or any member of its group) concerning the legal status of any country, territory, jurisdiction or area or of its authorities. The map(s) are provided without any warranty of any kind, either express or implied.
Competing interests: Dr. James reports grants from Sanofi Pasteur, outside the submitted work. Dr. Driscoll reports grants from World Health Organization, during the conduct of the study. Dr. Ivers reports grants from National Health and Medical Research Council of Australia, during the conduct of the study. Dr. Jozwiak reports personal fees from TEVA, personal fees from ALAB, personal fees from BOEHRINGER INGELHEIM, personal fees from SYNEXUS, non-financial support from SERVIER, non-financial support from MICROLIFE, non-financial support from MEDICOVER, outside the submitted work. Dr. Rakovac reports grants from World Health Organization, during the conduct of the study. Dr Shariful Islam is funded by National Heart Foundation of Australia and Institute for Physical Activity and Nutrition, Deakin University. Dr. Sheikh reports grants from Health Data Research UK, outside the submitted work. Dr. Singh reports personal fees from Crealta/Horizon, Medisys, Fidia, UBM LLC, Trio health, Medscape, WebMD, Clinical Care options, Clearview healthcare partners, Putnam associates, Spherix, Practice Point communications, the National Institutes of Health and the American College of Rheumatology, and Speaker’s bureau of Simply Speaking, owns stock options in Amarin pharmaceuticals and Viking pharmaceuticals, serves on the steering committee of OMERACT, an international organization that develops measures for clinical trials and receives arm’s length funding from 12 pharmaceutical companies, serves on the FDA Arthritis Advisory Committee, is a member of the Veterans Affairs Rheumatology Field Advisory Committee, and is the editor and the Director of the UAB Cochrane Musculoskeletal Group Satellite Center on Network Meta-analysis, outside the submitted work. Dr. Stein reports personal fees from Lundbeck, personal fees from Sun, outside the submitted work. Dr. Degenhardt reports grants from Indivior, Seqirus, Reckitt Benckiser, outside the submitted work.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Availability of input data depends on original source. Select data are available in a public, open access repository. Select data are available on reasonable request. Select data may be obtained from a third party and are not publicly available. All results relevant to the study are included in the article or uploaded as supplementary information or are available online.
References
- 1. GBD 2016 Traumatic Brain Injury and Spinal Cord Injury Collaborators Global, regional, and national burden of traumatic brain injury and spinal cord injury, 1990-2016: a systematic analysis for the global burden of disease study 2016. Lancet Neurol 2016;18:56–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Kotagal M, Agarwal-Harding KJ, Mock C, et al. Health and economic benefits of improved injury prevention and trauma care worldwide. PLoS One 2014;9:e91862 10.1371/journal.pone.0091862 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Sunshine JE, Meo N, Kassebaum NJ, et al. Association of adverse effects of medical treatment with mortality in the United States: a secondary analysis of the global burden of diseases, injuries, and risk factors study. JAMA Netw Open 2019;2:e187041 10.1001/jamanetworkopen.2018.7041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Dandona R, Kumar GA, Kharyal A, et al. Mortality due to snakebite and other venomous animals in the Indian state of Bihar: findings from a representative mortality study. PLoS One 2018;13:e0198900 10.1371/journal.pone.0198900 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Jha AK, Larizgoitia I, Audera-Lopez C, et al. The global burden of unsafe medical care: Analytic modelling of observational studies. BMJ Qual Saf 2013;22:809–15. 10.1136/bmjqs-2012-001748 [DOI] [PubMed] [Google Scholar]
- 6. Goal 3. sustainable development knowledge platform. Available: https://sustainabledevelopment.un.org/sdg3 [Accessed 29 Sep 2019].
- 7. Wong E, Leong MKF, Anantharaman V, et al. Road traffic accident mortality in Singapore. J Emerg Med 2002;22:139–46. 10.1016/S0736-4679(01)00455-3 [DOI] [PubMed] [Google Scholar]
- 8. Hsiao M, Malhotra A, Thakur JS, et al. Road traffic injury mortality and its mechanisms in India: nationally representative mortality survey of 1.1 million homes. BMJ Open 2013;3:e002621 10.1136/bmjopen-2013-002621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Montazeri A. Road-traffic-related mortality in Iran: a descriptive study. Public Health 2004;118:110–3. 10.1016/S0033-3506(03)00173-2 [DOI] [PubMed] [Google Scholar]
- 10. Ohlin M, Algurén B, Lie A. Analysis of bicycle crashes in Sweden involving injuries with high risk of health loss. Traffic Inj Prev 2019;20:613–8. 10.1080/15389588.2019.1614567 [DOI] [PubMed] [Google Scholar]
- 11. Haagsma JA, Graetz N, Bolliger I, et al. The global burden of injury: incidence, mortality, disability-adjusted life years and time trends from the global burden of disease study 2013. Injury Prevention 2015:injuryprev-2015-041616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Dicker D, Nguyen G, Abate D, et al. Global, regional, and national age-sex-specific mortality and life expectancy, 1950–2017: a systematic analysis for the global burden of disease study 2017. The Lancet 2018;392:1684–735. 10.1016/S0140-6736(18)31891-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Roth GA, Abate D, Abate KH, et al. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: a systematic analysis for the global burden of disease study 2017. The Lancet 2018;392:1736–88. 10.1016/S0140-6736(18)32203-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Stanaway JD, Afshin A, Gakidou E, et al. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990–2017: a systematic analysis for the global burden of disease study 2017. The Lancet 2018;392:1923–94. 10.1016/S0140-6736(18)32225-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kyu HH, Abate D, Abate KH, et al. Global, regional, and national disability-adjusted life-years (DALYs) for 359 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2017: a systematic analysis for the global burden of disease study 2017. The Lancet 2018;392:1859–922. 10.1016/S0140-6736(18)32335-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. James SL, Abate D, Abate KH, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the global burden of disease study 2017. The Lancet 2018;392:1789–858. 10.1016/S0140-6736(18)32279-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Murray CJL, Callender CSKH, Kulikoff XR, et al. Population and fertility by age and sex for 195 countries and territories, 1950–2017: a systematic analysis for the global burden of disease study 2017. The Lancet 2018;392:1995–2051. 10.1016/S0140-6736(18)32278-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Foreman KJ, Lozano R, Lopez AD, et al. Modeling causes of death: an integrated approach using CODEm. Popul Health Metr 2012;10:1 10.1186/1478-7954-10-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Naghavi M, Makela S, Foreman K, et al. Algorithms for enhancing public health utility of national causes-of-death data. Popul Health Metr 2010;8:9 10.1186/1478-7954-8-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Foreman KJ, Naghavi M, Ezzati M. Improving the usefulness of US mortality data: new methods for reclassification of underlying cause of death. Popul Health Metr 2016;14 10.1186/s12963-016-0082-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. China Zhuhai Study 2006-2007 - China CDC | GHDx. Available: http://ghdx.healthdata.org/record/china-zhuhai-study-2006-2007-china-cdc [Accessed 15 May 2018].
- 22. Functional outcome at 2.5, 5, 9, and 24 months after injury in the Netherlands | GHDx. Available: http://ghdx.healthdata.org/record/functional-outcome-25-5-9-and-24-months-after-injury-netherlands [Accessed 15 May 2018].
- 23. Health-Related quality of life after burns: a prospective multicentre cohort study with 18 months follow-up | GHDx. Available: http://ghdx.healthdata.org/record/health-related-quality-life-after-burns-prospective-multicentre-cohort-study-18-months-follow [Accessed 15 May 2018]. [DOI] [PubMed]
- 24. Netherlands injury surveillance system 2007 | GHDx. Available: http://ghdx.healthdata.org/record/netherlands-injury-surveillance-system-2007 [Accessed 15 May 2018].
- 25. Netherlands injury surveillance system 2010 | GHDx. Available: http://ghdx.healthdata.org/record/netherlands-injury-surveillance-system-2010 [Accessed 14 May 2018].
- 26. Mackenzie EJ, Rivara FP, Jurkovich GJ, et al. The national study on costs and outcomes of trauma. J Trauma 2007;63:S54–67. 10.1097/TA.0b013e31815acb09 [DOI] [PubMed] [Google Scholar]
- 27. Traumatic Brain Injury(TBI) Follow-Up Registry and Surveillance of TBI in the Emergency Department (ED); Notice of Availability of Funds. Federal Register, 2002. Available: https://www.federalregister.gov/documents/2002/05/08/02-11359/traumatic-brain-injurytbi-follow-up-registry-and-surveillance-of-tbi-in-the-emergency-department-ed [Accessed 14 May 2018].
- 28. Salomon JA, Haagsma JA, Davis A, et al. Disability weights for the global burden of disease 2013 study. Lancet Glob Health 2015;3:e712–23. 10.1016/S2214-109X(15)00069-8 [DOI] [PubMed] [Google Scholar]
- 29. Stevens GA, Alkema L, Black RE, et al. Guidelines for accurate and transparent health estimates reporting: the gather statement. The Lancet 2016;388:e19–23. 10.1016/S0140-6736(16)30388-9 [DOI] [PubMed] [Google Scholar]
- 30. Lim SS, Updike RL, Kaldjian AS, et al. Measuring human capital: a systematic analysis of 195 countries and territories, 1990–2016. The Lancet 2018;392:1217–34. 10.1016/S0140-6736(18)31941-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Fann JR, Ribe AR, Pedersen HS, et al. Long-Term risk of dementia among people with traumatic brain injury in Denmark: a population-based observational cohort study. The Lancet Psychiatry 2018;5:424–31. 10.1016/S2215-0366(18)30065-8 [DOI] [PubMed] [Google Scholar]
- 32. Who | global status report on road safety, 2018. Available: https://www.who.int/violence_injury_prevention/road_safety_status/2018/en/ [Accessed 22 Jul 2019].
- 33. Safety 2020 Safety 2020. Available: https://www.worldsafety2020.com [Accessed 22 Jul 2019].
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
injuryprev-2019-043494supp001.pdf (64.6KB, pdf)
injuryprev-2019-043494supp002.pdf (82.7KB, pdf)
injuryprev-2019-043494supp003.pdf (87.6KB, pdf)
injuryprev-2019-043494supp004.pdf (147.8KB, pdf)
injuryprev-2019-043494supp005.pdf (167.9KB, pdf)
injuryprev-2019-043494supp006.pdf (17MB, pdf)
injuryprev-2019-043494supp007.pdf (17MB, pdf)
injuryprev-2019-043494supp008.pdf (17MB, pdf)
injuryprev-2019-043494supp009.pdf (17MB, pdf)
injuryprev-2019-043494supp010.pdf (17MB, pdf)
injuryprev-2019-043494supp011.pdf (17MB, pdf)