Abstract
Background
India is the second most populated country in the world with 41% of the population (492 million) under 18 years of age. While numerous studies have shown an increasing prevalence of myopia worldwide, there continues to be uncertainty about the magnitude of myopia in Indian school going population.
Design
Systematic review and meta-analysis.
Methods
We systematically identified published literature of last four decades from 1980 to March 2020 and assessed them for methodological quality. Data were gathered into 5-year age groups from 5–15, in urban or rural populations, and standardized to definition of myopia as refractive error ≥ -0.50 dioptre. Random effects meta-analysis was done.
Results
We included data from 59 quality assessed studies, covering nearly 1,66,000 urban and 1,20,000 rural children. The overall crude prevalence of myopia over last four decades is 7.5% (95% CI, 6.5–8.5%) in 5-15-year age group. The prevalence of myopia is 8.5% (95% CI, 7.1–9.9%) in urban and 6.1% (95% CI, 4.5–7.7%) in rural children, with highest prevalence in urban 11-15-year age group [15.0% in last decade]. A significant increment in prevalence is noted in the last decade in rural children from 4.6% to 6.8%, reflecting changing rural environment.
Conclusion
Myopia is an emerging public health problem in both urban and rural school going adolescents in India requiring urgent efforts.
Introduction
Rising prevalence of myopia is a major challenge worldwide, giving rise to an epidemic in certain regions. It is the most common refractive error and an important cause of ocular morbidity especially affecting school going children and young adults. Uncorrected myopia has huge social, economic, psychological and developmental implications [1]. Various studies in the literature have predicted dramatic rise of myopia in the coming years causing a great concern among stakeholders and is projected to affect 50% of world population by 2050 [2]. There is a large regional variation in the myopia prevalence with the dominance of East Asian countries that report a far greater prevalence as compared to other countries [2, 3].
India is the second most populated country in the world, with around 41% of its population (492 million) being less than 18 year age group [4]. This young population is an important asset for development of the country and their challenges must be addressed in time. While rising myopia is a cause of concern in most of the countries, it is not given due importance in India due to lack of adequate nationwide prevalence data and prospective studies comparing the trend of myopia over decades [5]. Due to this, the representation of India is poor in studies predicting global trends of myopia [6]. Previous studies by the authors have reported a prevalence of myopia of only 13.1% among school going children in north India with an annual incidence of 3.4% [7, 8]. However, due to the large regional differences in culture, habits, socioeconomic status, educational levels and urbanisation, there continues to be an uncertainty about the exact magnitude of myopia burden in Indian school going children and its trend over time. The study was undertaken to fill up this lacuna which can help in understanding the prevalence of myopia, regional variations and prediction of trend, using all the published literature of the last four decades from India.
Methods
The study followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines for the purpose of this review.
Search strategy
We performed a systematic search and review of the prevalence of myopia in India using published data of the last four decades. We searched PubMed, Medline, Embase, OVID, Web of Science, CINAHL and Cochrane library databases from 1st January 1980 to 31st March, 2020. Many research articles from India are not available in PubMed search. Thus, we also searched other indexing systems- Index Copernicus and Google Scholar to make our search more inclusive. The search was restricted to all the online available articles mentioning prevalence of myopia in any region of India and published till March 2020. We searched these databases using the following MeSH (Medical Subject Heading) terms and keywords: myopia AND prevalence AND India and refractive error AND prevalence AND India. Broad search strategy also used terms related to epidemiology like epidemiology, incidence, rates, proportion and prevalence, terms related to disease (including medical subject headings search using exp refractive error*, exp myopia* and keyword search using the terms refractive error, myopia and shortsight*) and terms related to population (including medical subject headings search using exp India* and keyword search using the word India). We also identified and included relevant studies by manually searching the reference lists of eligible studies. Further details about search strategy are available in S1 File.
Definitions, inclusion and exclusion criteria and quality assessment
We conducted an initial broad search focusing on all studies that estimated the prevalence and/or incidence of refractive errors and/ or myopia among all age groups from any region in India. Later, the search was restricted to age group of 5–15 years for this systematic review. Prevalence was defined as the number of individuals in a population that have myopia at a given point of time divided by those at risk. Myopia was defined as spherical equivalent of -0.5 Dioptre or worse [2, 7–9]. This standard definition was applied to most of the studies to shortlist them for data abstraction. We covered both urban and rural settings, making our search more representative as majority of Indian population resides in rural villages. Cross-sectional studies including population-based as well as school-based studies were included. Qualitative studies, review articles, articles published in languages other than English and articles which did not have relevant information available online were excluded. A data extraction form was later developed to include all the studies which met our inclusion criteria. Various study characteristics like study design, study population, study location/ region, demographic details (age, gender), screening tools, case definitions used and epidemiological data were compiled from the above studies. We extracted separate urban and rural myopia prevalence rates and gender-based rates, wherever possible. The data was combined and later stratified in each 5-year age groups- 5–10; 11–15 years wherever possible. A detailed uniform methodological quality assessment of each of the included study was done by three independent observers using the critical appraisal checklist developed for prevalence studies by Hoy et al. (2012) [10]. Those studies which obtained aggregate score more than six were labelled as ‘high risk’ studies. Those studies which obtained aggregate score less than four and between four-six were labelled as ‘low risk’ and ‘moderate risk’ studies, respectively. Final score was decided based on consensus among the three observers.
Statistical methods
Meta-analysis was carried out using Stata 12.0 (StataCorp LP, Texas, USA). The random effects model using DerSimonian and Laird method was used to calculate pooled effect sizes and its 95% confidence interval (CI) limit [11]. Forest plots were generated displaying prevalence of myopia with corresponding 95% CI. The variation in the magnitude of the effect was examined and heterogeneity was quantified using I2 statistic. The funnel plot was used to detect potential reporting bias and small/large study effects and Egger method was used to assess asymmetry.
Studies which were categorised as ‘high risk’ based on assessment of methodological quality described above, were excluded from the final analysis. All studies (low, moderate and high risk) were included in a sensitivity analysis. Urban and rural data was analysed separately. The studies which represented both urban and rural population were later subdivided into separate datasets based on study settings (urban or rural) for detailed analysis. Rural-urban and time-stratified estimates of prevalence of myopia across included studies were obtained. For time stratified estimates, year of publication of study was taken for subgroup analysis unless study period was mentioned in the study. Decadal variation was assessed by subgroup analysis of 2009–2019 studies with those of previous decades. Results of rural were compared with urban studies, and studies conducted during 2009–2019 were compared with older studies, by computing z-scores. A sub-group separate analysis for children aged 11–15 years was also done for urban and rural studies. No such analysis can be carried out in 5-10-year age group due to limited number of available studies.
Results
Using the above described search strategy, 469 potentially relevant titles/ abstracts were identified, 165 relevant articles were assessed for eligibility, and 77 studies were found to be eligible [12–87]. The detailed quality assessment of eligible studies is reported in S1 Table. 18 studies were found to be “high risk”. Thus, 59 studies were included in the main analysis, while data from all 77 eligible studies were included in sensitivity analysis. The summary of review strategy is presented in S1 Fig.
Out of 59 studies included in main analysis, 37 showed representation of only urban data, 12 showed only rural data and 10 studies showed both urban and rural data. Region wise representation of studies is as follows: North India (12), North East India (4), Central India (6), East India (7), West India (8) and South India (22). All studies were cross sectional in nature. Most of the studies were school-based, with only 4 being population-based. Most of the studies were conducted in the last decade (2009–2019) with only few studies being available before 2009. Gender-based data was available only in few studies, precluding a gender stratified analysis. Overall, the review included around 1,66,000 urban school going children and 1,20,000 rural children over the last 4 decades. The studies were stratified into urban and rural settings and separate analysis was done for the same. Those studies which represented both urban and rural study settings were subdivided into separate datasets as urban or rural subset depending on study setting and data availability. Nine additional datasets were created to represent nine studies where data was available separately for urban and rural setting. The total number of datasets included in analysis were 68 (59 original studies + 9 additional datasets). The details of studies which were included for final statistical analysis are presented in Table 1, along with their study coverage area (urban/ rural/ both). One study did not give rural-urban data separately and was excluded from rural-urban sub-group analysis [22].
Table 1. Characteristics of various studies that reported data on prevalence of myopia in Indian school-age children and are included in the final meta-analysis.
| S No. | First Author (Year of Publication) [Citation] | Study Place | Region (India) | Coverage | Age Group (years) | Coverage | Cycloplegic Refraction | Total Sample Size (Subdivision when both urban and rural data separately available) | No. of myopic cases (Subdivision when both urban and rural data separately available) | Prevalence of myopia (%) | Overall Quality Assessment Score** |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Ahmed (2008) [12] | Srinagar | North | School | 6–22 | Urban | Yes | 4360 | 207 | 4.74 | Low Risk |
| 2 | Bansal (2012) [13] | Kolar | South | School | 6–16 | Urban | Yes | 2680 | 307 | 11.5 | Moderate risk |
| 3 | Aroor (2014) [14] | Surathkal | South | School | 4–16 | Urban | Yes | 755 | 102 | 13.5 | Moderate risk |
| 4 | Ande (2015) [15] | Guntur | South | School | 10–15 | Rural | Yes | 3174 | 148 | 4.66 | Low Risk |
| 5 | Mondal (2014) [16] | Kolkata | East | School | 8–17 | Urban | Yes | 1649 | 128 | 7.76 | Low Risk |
| 6 | Gupta (2012) [17] | Shimla | North | School | 5–15 | Urban | Yes | 2000 | 48 | 2.4 | Low Risk |
| 7 | Datta (1983) [18] | Kolkata | East | School | 5–13 | Urban | Yes | 24007 | 216 | 0.89 | Moderate risk |
| 8 | Batra (2007) [19] | Ludhiana | North | School | 5–15 | Urban, Rural | Yes | 19610 (Urban- 11185, Rural- 8425) | 1366 (Urban-1115, rural-251) | 6.97 | Low Risk |
| 9 | Chandra (1982) [20] | Prayagraj | Central | School | 8–16 | Urban | Yes | 8600 | 1430 | 16.43 | Moderate risk |
| 10 | Chatterjee (2014) [21] | Kolkata | East | School | 5–14 | Urban | Yes | 16597 | 960 | 5.78 | Low Risk |
| 11 | Dandona (2002a) [22] | Hyderabad, West Godavari, Adilabad, Mahbubnagar | South | Population | 0–15 | Urban, Rural | Yes | 1810 (5–15 yr age) | 66 | 3.6 | Low Risk |
| 12 | Dandona (2002b) [23] | Mahbubnagar | South | Population | 7–15 | Rural | Yes | 4074 | 163 | 4.1 | Low Risk |
| 13 | Das (2007) [24] | Kolkata | East | School | 5–10 | Urban | NA* | 2317 | 325 | 14.02 | Moderate risk |
| 14 | Agrawal (2018) [25] | Raipur | Central | School | 5–15 | Urban, Rural | NA | 1557 (urban- 836, rural- 721) | 50 (urban- 36, rural- 14) | 3.21 | Low Risk |
| 15 | Dhanya (2016) [26] | Bangalore | South | School | 5–15 | Urban | Yes | 958 | 45 | 4.7 | Moderate risk |
| 16 | Ganapathi (2017) [27] | Salem | South | School | 10–17 | Urban | NA | 828 | 98 | 11.8 | Moderate risk |
| 17 | Ghosh (2012) [28] | Kolkata | East | School | 6–14 | Urban | Yes | 2732 | 307 | 11.23 | Low Risk |
| 18 | Singh (2013) [29] | Bhopal | Central | School | 5–15 | Urban, Rural | Yes | 18500 (Urban-7955, Rural-10545) | 1313 (Urban-299, rural-1014) | 7.09 | Moderate risk |
| 19 | Krishnamurthy (2014) [30] | Mysore | South | School | 5–15 | Urban, Rural | Yes | 1123 (Urban-724, Rural-399) | 58 (Urban-39, rural-19) | 5.16 | Low Risk |
| 20 | Jha (2008) [31] | Leh | North | School | 3–15 | Urban | Yes | 843 | 35 | 4.1 | Low Risk |
| 21 | Sarma (2016) [32] | Guwahati | North East | School | 6–16 | Urban | Yes | 400 | 77 | 19.25 | Low Risk |
| 22 | Kalikivayi (1997) [33] | Hyderabad | South | School | 3–18 | Urban | Yes | 3987 | 341 | 8.6 | Low Risk |
| 23 | Kannan (2016) [34] | Chennai | South | School | 6–12 | Urban, Rural | Yes | 1203 (Urban-603, Rural-600) | 88 (Urban-52, rural-36) | 7.3 | Low Risk |
| 24 | Murthy (2014) [35] | Chittoor | South | School | 5–16 | Rural | Yes | 1412 | 34 | 2.4 | Moderate risk |
| 25 | Basu (2011) [36] | Surat | West | School | 7–15 | Urban | Yes | 3002 | 418 | 13.9 | Low Risk |
| 26 | Megala (2015) [37] | Krishnanagar | South | School | 10–14 | Urban | Yes | 422 | 83 | 19.7 | Low Risk |
| 27 | Meundi (2014) [38] | Kodagu | South | School | 5–17 | Rural | Yes | 1938 | 332 | 17.13 | Low Risk |
| 28 | Saha (2017) [39] | Kolkata | East | School | 5–15 | Urban | Yes | 1840 | 151 | 8.2 | Low Risk |
| 29 | Murthy (2002) [40] | Delhi | North | Population | 5–15 | Urban | Yes | 5696 | 422 | 7.4 | Low Risk |
| 30 | Krishnan (2015) [41] | Puducherry | South | School | 9–14 | Urban | Yes | 1460 | 100 | 6.8 | Moderate risk |
| 31 | Singh (2019) [42] | Gurugram | North | School | 5–15 | Urban | Yes | 1234 | 261 | 21.1 | Low Risk |
| 32 | Padhye (2009) [43] | Pune | West | School | 5–15 | Urban, Rural | Yes | 12422 (Urban-5021, Rural-7401) | 268 (Urban-160, rural-108) | 2.15 | Low Risk |
| 33 | Shukla (2018) [44] | Delhi | North | School | 9–12 | Urban | Yes | 6056 | 152 | 2.5 | Low Risk |
| 34 | Kumar (2014) [45] | Pune | West | School | 6–16 | Urban | NA | 1157 | 68 | 5.9 | Low Risk |
| 35 | Pavithra (2013) [46] | Bangalore | South | School | 7–15 | Urban, Rural | Yes | 1378 (Urban-687, Rural-691) | 61 (Urban-38, rural-23) | 4.4 | Low Risk |
| 36 | Singh (2015) [47] | Bhopal | Central | School | 6–10 | Urban, Rural | Yes | 560 (Urban-280, Rural-280) | 30 (Urban-16, rural-14) | 5.35 | Moderate risk |
| 37 | Cholera (2018) [48] | Pune | West | School | 5–15 | Urban | Yes | 500 | 113 | 22.6 | Moderate risk |
| 38 | Rahman (2015) [49] | Dibrugarh | North East | School | 10–15 | Urban | Yes | 600 | 43 | 7.17 | Low Risk |
| 39 | Kotabal (2017) [50] | Shivamogga | South | School | 13–16 | Urban | Yes | 300 | 69 | 23 | Moderate risk |
| 40 | Bigyabati (2016) [51] | Thoubal | North East | School | 5–15 | Rural | Yes | 1770 | 108 | 6.1 | Low Risk |
| 41 | Ravinder (2016) [52} | Warangal | South | School | 7–12 | Urban | Yes | 5000 | 90 | 1.8 | Moderate risk |
| 42 | Hashia (2017) [53] | Jammu | North | School | 5–16 | Rural | Yes | 642 | 28 | 4.36 | Low Risk |
| 43 | Saxena (2015) [8] | Delhi | North | School | 5–15 | Urban | Yes | 9884 | 1297 | 13.12 | Low Risk |
| 44 | Naik (2013) [54] | Ahmednagar | West | School | 6–15 | Rural | Yes | 1095 | 45 | 4.1 | Moderate risk |
| 45 | Samant (2015) [55] | Loni | West | School | 10–12 | Rural | Yes | 1220 | 209 | 17.13 | Moderate risk |
| 46 | Sandeep (2015) [56] | Hubli | South | School | 7–15 | Urban | Yes | 2400 | 109 | 4.54 | Moderate risk |
| 47 | Kumar K. (2016) [57] | Imphal | North East | School | 11–13 | Urban | Yes | 302 | 88 | 29.14 | Moderate risk |
| 48 | Sharma (2009) [58] | Rohtak | North | School | 6–15 | Rural | Yes | 1265 | 153 | 12.7 | Low Risk |
| 49 | Shakeel (2016) [59] | Dehradun | North | School | 5–16 | Urban | Yes | 3146 | 156 | 5 | Low Risk |
| 50 | Kumar (2016) [60] | Hyderabad | South | School | 12–16 | Urban | Yes | 600 | 120 | 20 | Low Risk |
| 51 | Sethi (2000) [61] | Ahmedabad | West | School | 12–17 | Urban | Yes | 1647 | 265 | 16 | Moderate risk |
| 52 | Tirkey (2018) [62] | Nalhar | Central | School | 5–10 | Urban | Yes | 1300 | 128 | 9.84 | Moderate risk |
| 53 | Uzma (2009) [63] | Hyderabad | South | School | 7–15 | Urban, Rural | Yes | 3314 (Urban-1789, Rural-1525) | 248 (Urban-229, rural-19) | 7.48 | Low Risk |
| 54 | Sharma (2018) [64] | Kangra | North | School | 5–12 | Urban | Yes | 1007 | 33 | 3.27 | Low Risk |
| 55 | Karavadi (2018) [65] | Bangalore | South | School | 7–16 | Rural | Yes | 1140 | 48 | 4.21 | Low Risk |
| 56 | Trivedi (2012) [66] | Sabarkantha | West | Population | 7–15 | Rural | Yes | 452 | 18 | 4.1 | Low Risk |
| 57 | Warad (2014) [67] | Devangere | South | School | 10–12 | Urban | Yes | 7496 | 396 | 5.28 | Low Risk |
| 58 | Warkad (2018) [68] | Bhubaneshwar | East | School | 6–17 | Urban | Yes | 10038 | 56 | 0.63 | Low Risk |
| 59 | Shukla (2016) [69] | Jabalpur | Central | School | 5–15 | Rural | Yes | 200 | 4 | 2 | Moderate risk |
*NA- not available
** Based on Standard quality assessment tool given by Hoy et al. [10].
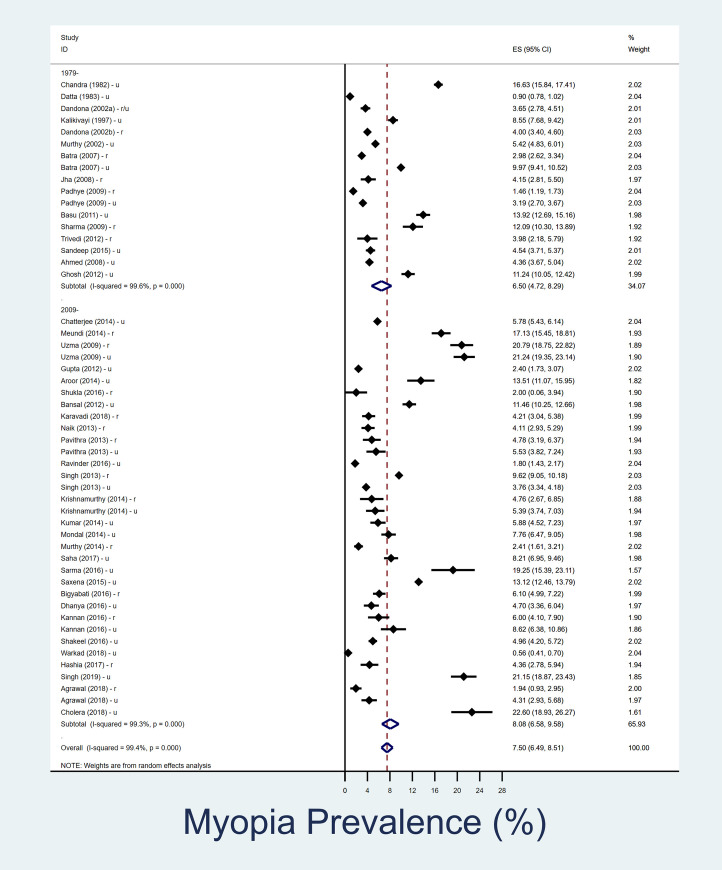
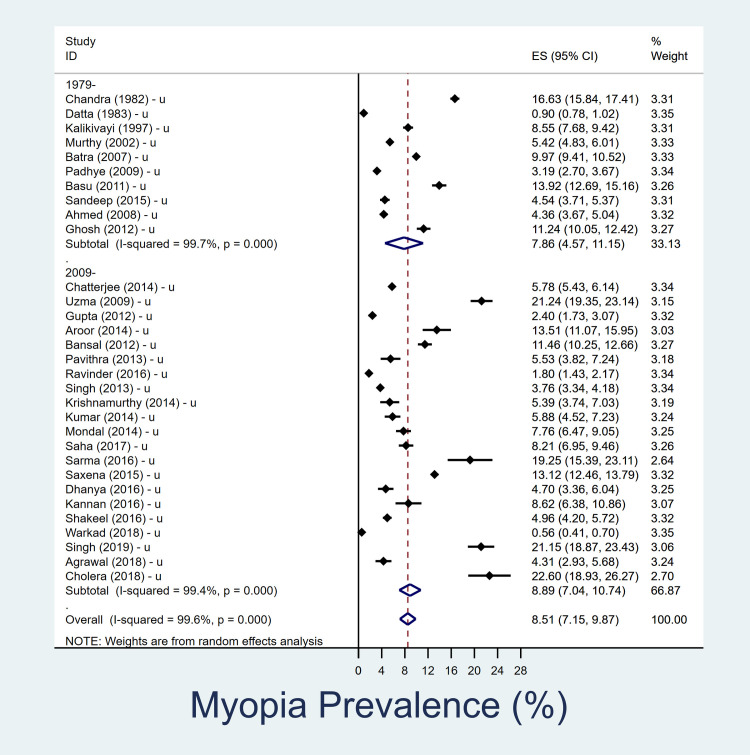
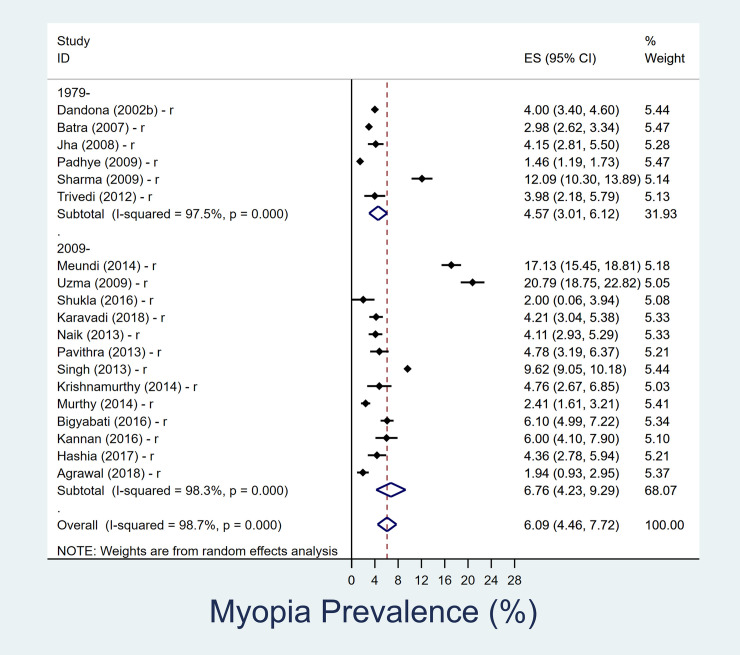
Prevalence of myopia in 5–15 year age group
The summary of the results is shown in Table 2. In the 5-15-year age group, overall pooled prevalence of myopia over last four decades is 7.5% (95% CI, 6.5–8.5%) (Fig 1). The overall pooled prevalence of myopia in urban children is 8.5% (95% CI, 7.1–9.9%) and in rural settings is 6.1% (95% CI, 4.5–7.7%) in past four decades (Figs 2 and 3). In rural Indian children, the prevalence of myopia increased from 4.6% (95% CI, 3.0–6.1) in 1980–2008 to 6.8% (95% CI, 4.2–9.3) in 2009–2019. The increment among urban Indian children was lower, changing from 7.9% (95% CI, 4.6–11.2) in 1980–2008 to 8.9% (95% CI, 7.1–10.7) in 2009–2019. The heterogeneity of the studies included in pooled analysis, as well as urban-rural subgroups analysis were high (S2 and S3 Figs).
Table 2. Meta-analysis of prevalence of myopia in Indian school-age children, overall and stratified by time-periods and rural-urban population during 1980–2019.
| 5–15 years age group | 11–15 years age sub-group | |||
|---|---|---|---|---|
| Number of study datasets | Prevalence of Myopia (%) [95% CI] | Number of study datasets | Prevalence of Myopia (%) [95% CI] | |
| Rural and Urban | ||||
| Overall | 51 | 7.5 (6.5–8.5) | 26 | 10.7 (9–12.4) |
| 1980–2008 period | 17 | 6.4 (4.7–8.1) | 11 | 6.6 (4.8–8.3) |
| 2009–2019 period | 34 | 8.1 (6.6–9.6) | 15 | 14.2 (11.2–17.2) |
| Rural | ||||
| Overall | 19 | 6.1 (4.5–7.7) | 7 | 10 (6.4–13.5) |
| 1980–2008 period | 6 | 4.6 (3.0–6.1) | 3 | 6.9 (2.1–11.8) |
| 2009–2019 period | 13 | 6.8 (4.2–9.3) | 4 | 12.3 (5.4–19.2) |
| Urban | ||||
| Overall | 31 | 8.5 (7.1–9.9) | 18 | 11.5 (9.3–13.6) |
| 1980–2008 period | 10 | 7.9 (4.6–11.2) | 7 | 6.8 (4.1–9.4) |
| 2009–2019 period | 21 | 8.9 (7.1–10.7) | 11 | 15.0 (11.2–18.7) |
Fig 1. Forest plot showing overall prevalence of myopia in school going children (5–15 year) and its decadal variation.
The datasets which represented urban and rural data are separately denoted as ‘u’ and ‘r’ respectively. Those studies in which urban/rural segregated data was not available are denoted as ‘r/u’.
Fig 2. Forest plot showing prevalence of myopia in school going children (5–15 year) in urban setting and its decadal variation.
The datasets which represented urban and rural data are separately denoted as ‘u’ and ‘r’ respectively. Those studies in which urban/rural segregated data was not available are denoted as ‘r/u’.
Fig 3. Forest plot showing prevalence of myopia in school going children (5–15 year) in rural setting and its decadal variation.
The datasets which represented urban and rural data are separately denoted as ‘u’ and ‘r’ respectively. Those studies in which urban/rural segregated data was not available are denoted as ‘r/u’.
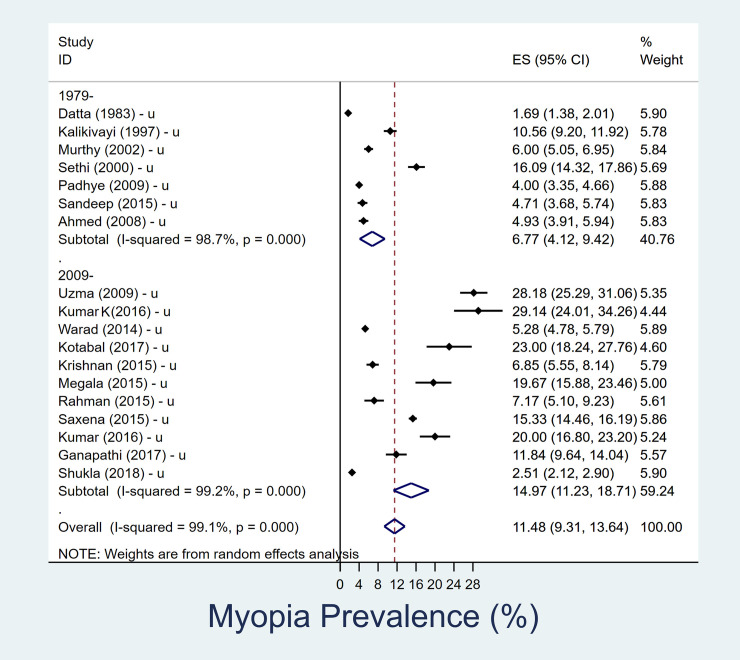
Prevalence of myopia in 11–15 year age group
In the older 11-15-year age sub-group, the pooled prevalence of myopia over last four decades was 10.7% (95% CI, 9–12.4). Prevalence of myopia increased, in rural children aged 11–15 years, from 6.9% (95% CI, 2.1–11.8) in 1980–2008 to 12.3% (95% CI, 5.4–19.2) between 2009–2019 (Table 2). Similarly, near doubling of prevalence from 6.8% (95% CI, 4.1–9.4) in 1980–2008 to 15.0% (95% CI, 11.2–18.7) in 2009–2019 was observed among urban children aged 11–15 years (Fig 4). The heterogeneity of the pooled estimates was high.
Fig 4. Forest plot showing change in prevalence of myopia over time in urban adolescent age group (11–15 years).
The datasets which represented urban and rural data are separately denoted as ‘u’ and ‘r’ respectively. Those studies in which urban/rural segregated data was not available are denoted as ‘r/u’.
Sensitivity analysis
Eighteen studies classified as “high risk” were included in the sensitivity analysis (S2 Table). Similar trends were obtained as main analysis, with 7.4% (95% CI, 7–7.8%) overall pooled prevalence of myopia over last four decades in 5–15 year age group. The overall pooled prevalence of myopia in urban school going children (5–15 years age) was 9.2% (95% CI, 8.2–10.2%) and in rural settings was 7% (95% CI, 5.5–8.5%) in past four decades. Additional details of sensitivity analysis are available in S3 Table.
Discussion
Myopia is emerging as a major public health problem worldwide [2, 5]. School going children are one of the most important risk group who constitute a large part of the Indian population [4, 5]. The current systematic review estimates the pooled prevalence of myopia, with a focus on studying rural-urban differences and time trends, and included fifty-nine quality assessed studies ensuring adequate rural-urban representation over different time intervals in the main analysis. Results show that the crude prevalence of myopia over last four decades is 7.5% in 5-15-year age group, being 8.5% and 6.1% in urban and rural school going children respectively. The prevalence has increased in rural India from 4.6% in 1980–2008 to 6.8% in 2009–2019, compared to a change from 7.9% to 8.9% in urban India during the same period.
Our results show that there is an increasing trend of myopia in India over the last four decades. Other meta-analyses from different parts of the world have also shown similar trends [2, 6, 88–91]. The prevalence of myopia is much less in Indian school going children as compared to other Asian countries where it could be as high as 70–80% [2, 88, 89]. While the prevalence may not be as high as that of East Asian countries, the actual numbers of myopes will be large considering our huge population and that 29% of the population consists of children less than 15 years of age (National Health Profile 2015, published by Government of India) [88–92]. This epidemiological variation also holds great importance as it pertains to world’s second most populated country which has more than 40% of young population who are at risk of developing myopia. Holden et al has estimated the prevalence of myopia in South Asia region (which includes India) to be around 20% in 2010, 38% in 2030 and 53% in 2050 [2]. We have found a lower prevalence of myopia in school going children in India over the last four decades as compared to other Asian countries where myopia is far more prevalent. Rudnicka et al has also found that increment in myopia prevalence in South Asian countries is less as compared to East Asian countries [90]. Thus, various meta-analyses which predicts global myopia trends fail to bring out this regional variation due to under representation of Indian studies [2, 6, 90].
This study has shown for the first time that there appears to be a significant rise in the prevalence of myopia in rural school going children. The percentage increment in myopia prevalence among rural school going children was 4 times more as compared to their urban counterparts, in the last decade (48% vs 12%). This is a novel epidemiological finding challenging the previous notion that myopia was less prevalent in rural areas in India as compared to urban areas [5, 91]. Systematic review by Sheeladevi et al. showed very low prevalence of myopia in rural settings as compared to urban settings in Indian children (3.5% vs 10.8%) [91]. While this might be a result of a demographic transition, their study assessed only eight school based and four population based studies.
There could be multiple reasons for the increase observed in rural school children. For the past few years, many Indian villages have become developed with access to basic amenities just like their urban counterparts. India is also witnessing a digital revolution starting from the past decade with increasing number of televisions, mobiles, laptops and computers. Internet usage has increased dramatically owing to reduced data tariff, low cost smartphones and improved telecom connectivity in Indian villages. This might have resulted in decreased outdoor activities, increased near work, and computer-related visual stress and fatigue [5, 90]. Changing schooling pattern to high pressure education system can also be another contributory factor [93, 94]. While direct causal relationship may be difficult to prove, but the rapidly changing environment (nurture) especially the ongoing urbanisation of rural environment in India could be implicated as a potential factor for this rising myopic prevalence.
This study confirms the findings of existing literature that urban adolescents (11–15 year age group) constitute an important ‘at risk’ subset of the general population requiring immediate attention and intervention where the prevalence of myopia increased to more than double in the last decade. Rural adolescents are also achieving the similar growth rate. Similar trend was obtained in other countries as well because myopia tends to develop after the natural curve of emmetropisation is over [3, 88, 89, 95].
India is geographically and demographically a large country with distinct regional identity and characteristics. Lack of studies reflecting the myopia prevalence from different regions of India and long-time gap between these studies were some important limitations of the study. The studies using inappropriate methodology, not published in English or where the relevant details in study text was unavailable, were excluded. We could not evaluate the prevalence and increment of high myopia which is important to prevent myopia related complications. Although numerous studies have shown an effect of gender on the myopia prevalence, gender-based variations could not be assessed due to limited data availability. Despite great heterogeneity in the results of the studies, we tried to address the differences and bring out some meaningful trends by using stratification, subgroup analysis and random effects model.
Similar trends were noted even after including eighteen high risk studies in the sensitivity analysis. Most of the studies which had poor methodological quality were conducted in the last decade. By excluding high risk studies, we adopted a conservative approach. The sensitivity analysis reaffirms the possibility of definite change in epidemiology of myopia in India over time. This large database is also one of the strengths of the present study which has helped to predict better trends and highlight subtle variations in epidemiology of myopia. Assessment of the time trends can be accurately done by observing the same population though repeated surveys at definite time intervals but these are rarely collected. Thus, the trend analysis from compiling available data might help in planning policies and setting priorities.
Myopia control programs require consistent efforts to increase awareness about risk factors, encourage lifestyle modification and changes in the school curriculum and education policy of the country. Therefore, this review should help stimulate the initiation of various preventive and corrective measures for myopia control, resource planning and infrastructure augmentation especially targeting the school going children [90, 95, 96].
Conclusion
To conclude, this is the first Indian study to show and compare the prevalence of myopia in urban and rural settings over the last four decades. It has shown for the first time the rapidly rising trend of myopia in rural school going children compared to their urban counterparts. This should result in adoption of urgent preventive and curative measures among various stakeholders to tackle this menace on time. Future prospective studies should be planned among various diverse regions of India to elucidate the trend of myopia and study various local epidemiological risk factors involved.
Supporting information
(TIF)
(TIF)
(TIF)
Standard quality assessment tool given by Hoy et al. Aggregate score <4- low risk, 4–6 moderate risk, >6 high risk. High risk studies are excluded (0- low risk, 1- high risk) [10].
(DOCX)
*NA- not available, ** Based on Standard quality assessment tool given by Hoy et al. [10].
(DOCX)
(DOCX)
(DOCX)
(DOC)
(ZIP)
Data Availability
All relevant data are within the manuscript and its Supporting Information files.
Funding Statement
The authors received no specific funding for this work.
References
- 1.Congdon N, Burnett A, Frick K. The impact of uncorrected myopia on individuals and society. Community Eye Health. 2019;32(105):7–8. [PMC free article] [PubMed] [Google Scholar]
- 2.Holden BA, Fricke TR, Wilson DA, Jong M, Naidoo KS, Sankaridurg P, et al. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology. 2016. May;123(5):1036–42. 10.1016/j.ophtha.2016.01.006 [DOI] [PubMed] [Google Scholar]
- 3.Saw S-M, Pan CW, Dirani M, Cheng C-Y, Wong TY. Is myopia more common in Asians? A systematic review and meta-analysis. Invest Ophthalmol Vis Sci. 2014. April 30;55(13):3632–3632. [Google Scholar]
- 4.Census of India: age structure and marital status. [cited 2020 Mar 10]. Available from: http://censusindia.gov.in/Census_And_You/age_structure_and_marital_status.aspx
- 5.Saxena R, Vashist P, Menon V. Is myopia a public health problem in India? Indian J Community Med. 2013. April 1;38(2):83 10.4103/0970-0218.112436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hashemi H, Fotouhi A, Yekta A, Pakzad R, Ostadimoghaddam H, Khabazkhoob M. Global and regional estimates of prevalence of refractive errors: Systematic review and meta-analysis. J Curr Ophthalmol. 2017. September 27;30(1):3–22. 10.1016/j.joco.2017.08.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Saxena R, Vashist P, Tandon R, Pandey RM, Bhardawaj A, Gupta V, et al. Incidence and progression of myopia and associated factors in urban school children in Delhi: The North India Myopia Study (NIM Study). PloS One. 2017;12(12):e0189774 10.1371/journal.pone.0189774 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Saxena R, Vashist P, Tandon R, Pandey RM, Bhardawaj A, Menon V, et al. Prevalence of myopia and its risk factors in urban school children in Delhi: the North India Myopia Study (NIM Study). PloS One. 2015;10(2):e0117349 10.1371/journal.pone.0117349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Luo H.D, Gazzard G., Liang Y., Shankar A., Tan D.T., Saw S.M. Defining myopia using refractive error and uncorrected logMAR visual acuity >0.3 from 1334 Singapore school children ages 7–9 years. Br. J. Ophthalmol. 2006;90:362–366. 10.1136/bjo.2005.079657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hoy D, Brooks P, Woolf A, Blyth F, March L, Bain C, et al. Assessing risk of bias in prevalence studies: modification of an existing tool and evidence of interrater agreement. J Clin Epidemiol. 2012. September;65(9):934–9. 10.1016/j.jclinepi.2011.11.014 [DOI] [PubMed] [Google Scholar]
- 11.DerSimonian R, Laird N. Meta-analysis in clinical trials. Controlled clinical trials. 1986. September 1;7(3):177–88. 10.1016/0197-2456(86)90046-2 [DOI] [PubMed] [Google Scholar]
- 12.Ahmed I, Mian S, Mudasir S, Andrabi KI. Prevalence of myopia in students of Srinagar city of Kashmir, India. Int J Health Sci. 2008. January;2(1):77–81. [PMC free article] [PubMed] [Google Scholar]
- 13.Bansal A, Krishnappa K, Datti NP, Guruprasal BS, Guha J. Ocular morbidity in school going children of Kolar district, South India. J Clin Biomed Sci. 2012;2(4):175–84. [Google Scholar]
- 14.Aroor AR, Sathyajith KA, Mahale R, Ravikiran SR, Shetty S, Rao AR. Anthropometry and prevalence of common health problems among school going children in Surathkal, Karnataka. J Clin Diagn Res. 2014. December; 8(12): PC01–PC05. 10.7860/JCDR/2014/8769.5233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ande VR, Peeta RK, Chella MR, Gujjarlapudi C. Prevalence of refractive errors among school children in a rural setting. International Medical Journal. 2015. March;2(3):4 Available from: https://www.medpulse.in/Article/Volume2Issue3/MedPulse_2_3_3.pdf [Google Scholar]
- 16.Mondal DA, Chatterjee DA, Pattanayak DU, Sadhukhan DSK, Mukhopadhyay DU. A study on ocular morbidity and its associates among madrasah students of Kolkata. Indian Journal of Basic and Applied Medical Research. 2014. June; 3(3):6 Available from: http://ijbamr.com/pdf/358-362.pdf.pdf [Google Scholar]
- 17.Gupta A, Lal R, Mazta SR, Sharma D. Prevalence of refractive errors, color vision defects and other ocular disorders in school-going children: primary screening by school teachers. JIMSA. 2012;25(4):223–224. Available from: http://medind.nic.in/jav/t12/i4/javt12i4p223.pdf [Google Scholar]
- 18.Datta A, Choudhury N, Kundu K. An epidemiological study of ocular condition among primary school children of Calcutta Corporation. Indian J Ophthalmol. 1983. September;31(5):505–10. [PubMed] [Google Scholar]
- 19.Nitin Batra, Kaushal D Gill AS. Refractive errors in school children: a review from Punjab. NPCB India Quarterly Newsletter. 2007;1(4):2–4. Available from: http://npcb.nic.in/writereaddata/mainlinkfile/File137.pdf [Google Scholar]
- 20.Chandra DB, Swarup D, Srivastava RK. Prevalence and pattern along with socio-economic factors of myopia in school going children-8 to 16 years. Indian J Ophthalmol. 1982;30:517–8. 7183546 [Google Scholar]
- 21.Chatterjee S, Biswas D, Kumar K. Prevalence of refractive errors in school children in the urban population of Kolkata, India: A prospective study. Int J Res Health Sci. 2014. October 31;2(4):1185–7. Available from: http://www.ijrhs.com/issues.php?val=Volume2&iss=Issue4. [Google Scholar]
- 22.Dandona R, Dandona L, Srinivas M, Giridhar P, McCarty CA, Rao GN. Population‐based assessment of refractive error in India: the Andhra Pradesh eye disease study. Clinical & experimental ophthalmology. 2002. February;30(2):84–93. [DOI] [PubMed] [Google Scholar]
- 23.Dandona R, Dandona L, Srinivas M, Sahare P, Narsaiah S, Muñoz SR, et al. Refractive error in children in a rural population in India. Invest Ophthalmol Vis Sci. 2002. March;43(3):615–22. [PubMed] [Google Scholar]
- 24.Das A, Dutta H, Bhaduri G, De SA, Sarkar K, Bannerjee M. A study on refractive errors among school children in Kolkata. J Indian Med Assoc. 2007. April;105(4):169–72. [PubMed] [Google Scholar]
- 25.Agrawal D, Sahu A, Agrawal D. Prevalence of ocular morbidities among school children in Raipur district, India. Indian J Ophthalmol. 2020. February;68(2):340 10.4103/ijo.IJO_1454_19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dhanya D, Pandu S, Sujatha V, Pallavi BA, Srinivas B. A population based study of refractive errors in children among age group of 7–15 years. J. Evid. Based Med. Healthc. 2016; 3(20), 815–817. 10.18410/jebmh/2016/185 [DOI] [Google Scholar]
- 27.Chellavel Ganapathy K. A study on prevalence of myopia and its associated factors in school children of Salem, Tamil Nadu. International Journal of Community Medicine and Public Health. 2017. August;4(8):2741. [Google Scholar]
- 28.Ghosh S, Mukhopadhyay U, Maji D, Bhaduri G. Visual impairment in urban school children of low-income families in Kolkata, India. Indian J Public Health. 2012. June;56(2):163–7. 10.4103/0019-557X.99919 [DOI] [PubMed] [Google Scholar]
- 29.Singh H, Saini VK, Yadav A, Soni B. Refractive errors in school going children–data from a school screening survey programme. Natl J Community Med 2013; 4(1): 137–40. Available from: http://njcmindia.org/uploads/4-1_137-140.pdf [Google Scholar]
- 30.Krishnamurthy H, Tanushree V¸ D'Silva AJ, Mobin G, Kantharaju KP. Prevalence of refractive errors among school children of 5–15 years age group in Mysore district. Int J Sci Stud 2014;2(8):150–154. Available from: http://www.ijss-sn.com/volume-2-issue-8—november-2014.html [Google Scholar]
- 31.Jha KN. Baseline ophthalmic data of schoolchildren aged 15 years or younger at Leh, Jammu and Kashmir, India. J Clin Diagn Res. 2008;64:1186–90. [Google Scholar]
- 32.Sarma KD, Krishnatreya M. A study on refractive errors among the school children of Guwahati city. International Journal of Contemporary Medical Research 2016;3(8):2258–2260. Available from: https://www.ijcmr.com/uploads/7/7/4/6/77464738/ijcmr_796_jul_28.pdf [Google Scholar]
- 33.Kalikivayi V, Naduvilath TJ, Bansal AK, Dandona L. Visual impairment in school children in southern India. Indian J Ophthalmol. 1997. June;45(2):129–34. [PubMed] [Google Scholar]
- 34.Kannan U, Rajendiran A, Yeraballi D, Shanmugavel K, John NA, Rene S. Refractive error and associated risk factors in 6–12 years schoolchildren. Natl J Physiol Pharm Pharmacol 2016;6(6):554–558. Available from: https://www.bibliomed.org/mnsfulltext/28/28-1461601228.pdf?1583861034 [Google Scholar]
- 35.Sridhar MS. A study on prevalence of refractive errors among 5–16 years rural children in Chandragiri, Chittoor district, Andhra Pradesh. Journal of Evolution of Medical and Dental Sciences. 2014. September 25;3(47):11411–9. [Google Scholar]
- 36.Basu M, Das P, Pal R, Kar S, Desai VK, Kavishwar A. Spectrum of visual impairment among urban female school students of Surat. Indian J Ophthalmol. 2011;59(6):475–9. 10.4103/0301-4738.86317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Megala M. A study on prevalence of refractive error and its associated factors among school children in Krishnagiri district, Tamilnadu, 2016 April. Available from: http://repository-tnmgrmu.ac.in/2137/1/2015001megalam.pdf
- 38.Meundi AD, Athavale AV, Suruliraman SM, Anjan S, Gururaj MS, Dhabadi BB, et al. Prevalence of ocular morbidities among school children in a rural area of South India. South American Journal of Medicine. 2014;2(2). Available from: https://www.texilajournal.com/thumbs/article/Medicine_Vol%202_Issue%202_ [Google Scholar]
- 39.Saha M, Ranjan A, Islam MN, Mukherji S. Prevalence of refractive errors among the school going children at a tertiary center of West Bengal. Int J Sci Stud 2017;5(4):179–182. Available from: https://www.ijss-sn.com/uploads/2/0/1/5/20153321/ijss_july_oa38_-_2017.pdf [Google Scholar]
- 40.Murthy GV, Gupta SK, Ellwein LB, Munoz SR, Pokharel GP, Sanga L, et al. Refractive error in children in an urban population in New Delhi. Investigative ophthalmology & visual science. 2002. March 1;43(3):623–31. [PubMed] [Google Scholar]
- 41.Krishnan DV, Baba DD, Poovitha M, Pranav M. Study of prevalence of refractive errors in school children of Villupuram & Puducherry. Sch J App Med Sci. 2015; 3(7B):2568–2573. Available from: https://www.semanticscholar.org/paper/Study-of-Prevalence-of-Refractive-Errors-in-School-Krishnan-Baba/e268cf2521fa78f5e824301e5c13cedb605ce4f9 [Google Scholar]
- 42.Singh NK, James RM, Yadav A, Kumar R, Asthana S, Labani S. Prevalence of myopia and associated risk factors in schoolchildren in North India. Optometry and Vision Science. 2019. March 1;96(3):200–5. 10.1097/OPX.0000000000001344 [DOI] [PubMed] [Google Scholar]
- 43.Padhye AS, Khandekar R, Dharmadhikari S, Dole K, Gogate P, Deshpande M. Prevalence of uncorrected refractive error and other eye problems among urban and rural school children. Middle East Afr J Ophthalmol. 2009. Apr;16(2):69 10.4103/0974-9233.53864 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Shukla P, Vashist P, Singh SS, Gupta V, Gupta N, Wadhwani M, et al. Assessing the inclusion of primary school children in vision screening for refractive error program of India. Indian J Ophthalmol. 2018. July;66(7):935 10.4103/ijo.IJO_1036_17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kumar P, Pore P, Dixit AK, Singh N. Prevalence and demographic distribution of refractory error in school children of Pune, India. Int J Res Health Sci. 2014 Jan31;2(1):5867. Available from http://www.ijrhs.com/issues.php?val=Volume2&iss=Issue1
- 46.Pavithra MB, Maheshwaran R, Rani Sujatha MA. A study on the prevalence of refractive errors among school children of 7–15 years age group in the field practice areas of a medical college in Bangalore. Int J Med Sci Public Health 2013; 2:641–645. [Google Scholar]
- 47.Singh P, Agarwal R, Kashiv Y, Gupta S B, Kumar R. Comparison between primary school children of urban and rural areas for prevalence of uncorrected refractive errors and amblyopia. Int J Med Res Rev 2015;3(8):871–876. 10.17511/ijmrr.2015.i8.164 [DOI] [Google Scholar]
- 48.Priyadarshini PC. Qualitative analysis of refractive errors in school children. Indian Journal of Clinical and Experimental Ophthalmology. 2018;4(2):284–286. 10.18231/2395-1451.2018.0063 [DOI] [Google Scholar]
- 49.Rahman M., Devi B, Kulli JJ, Gogoi G. A study on the refractive status of school going children aged between 10 to 15 years in Dibrugarh town, Assam, India. IOSR-JDMS. 2015. February;14(2):27–33. Available from: https://www.semanticscholar.org/paper/A-Study-On-The-Refractive-Status-Of-School-Going-10-Rahman-Devi/504c7d6ffdf860d3d6567354713f0427d0393610 [Google Scholar]
- 50.Kotabal R, Belur MN, Nandini C, Nagendra K. A study on prevalence of myopia among high school children in an urban area of Shivamogga: a cross sectional study. Int J Community Med Public Health. 2017;4:2373–6. Available from: http://www.ijcmph.com [Google Scholar]
- 51.Bigyabati R, Victor R, Rajkumari B. A study of prevalence of ocular morbidities in school going children in a rural district of Manipur. J Evolution Med Dent Sci. 2016;5(53):3540–3543. 10.14260/jemds/2016/816 [DOI] [Google Scholar]
- 52.Ravinder K, Reddy BG, Soujanya T. A study of prevalence of ocular disorders in primary school children in Warangal. Asian Pac. J. Health Sci., 2016; 3 (2):33–42. Available from: https://www.apjhs.com/pdf/8-A-study-of-prevalence-of-ocular-disorders-in-primary-school-children-in-Warangal.pdf [Google Scholar]
- 53.Hashia R, Slathia A. Pattern of refractive errors in primary school children in rural areas of Jammu city of Jammu and Kashmir, India. Int J Sci Stud. 2017;5(6):115–119. [Google Scholar]
- 54.Naik R. Prevalence of ocular morbidity among school going children (6-15years), Sch. J. App Med Sci. 2013; 1(6):848–851. Available from: www.saspublisher.com [Google Scholar]
- 55.Samant PL, Bangal SV, Purushottam AG, Bhandari AJ. Refractive errors as a cause of childhood blindness in school going children of a rural set-up. International J Healthcare Biomed Research. 2015. April; 3(3):45–51. Available from: http://ijhbr.com/pdf/April%202015%2045-51.pdf [Google Scholar]
- 56.Sandeep K, Venkatram K, Mahesh JB. Prevalence of myopia among urban school children. Journal of Evolution of Medical and Dental Sciences. 2015. April; 4(34):5859–66. 10.14260/jemds/2015/857 [DOI] [Google Scholar]
- 57.Kumar KS, Akoijam BS. Prevalence of refractive error among school-going children of Imphal, Manipur. Int J Med Sci Public Health 2016;5:1364–1368. Available from: https://www.bibliomed.org/mnsfulltext/67/67-1444625937.pdf?1583890719 [Google Scholar]
- 58.Seema S, Vashisht B, Meenakshi K, Manish G. Magnitude of refractive errors among school children in a rural block of Haryana. The Internet Journal of Epidemiology. 2009;6(2). 10.5580/1e5f [DOI] [Google Scholar]
- 59.Shakeel T, Mittal SK. Pattern of refractive errors in primary school children in Dehradun city of Uttrakhand State. The Official Scientific Journal of Delhi Ophthalmological Society. 2016. September 10;27(2):106–10. [Google Scholar]
- 60.Kumar AS, Rao BB, Reddy NA. A study on the prevalence of myopia among high school students in urban field practice area of Osmania Medical College, Hyderabad, Telangana. International Journal of Contemporary Medical Research. 2016. June;3(6):1859–61. [Google Scholar]
- 61.Sethi S, Kartha GP. Prevalence of refractive errors in school children (12–17 years) of Ahmedabad City. Indian J Community Medicine. 2000. October;25(4):181. [Google Scholar]
- 62.Tirkey ER, Adlakha N. Epidemiological study of eye diseases in primary school children in private schools in Vindhya Region. The Official Scientific Journal of Delhi Ophthalmological Society. 2018. August 5;29(1):64–7. [Google Scholar]
- 63.Uzma N, Kumar BS, Salar BK, Zafar MA, Reddy VD. A comparative clinical survey of the prevalence of refractive errors and eye diseases in urban and rural school children. Canadian J Ophthalmol. 2009. June;44(3):328–33. [DOI] [PubMed] [Google Scholar]
- 64.Sharma V. Refractive error screening among school going children of age group 5-11years in district Kangra, Himachal Pradesh. International Journal of Scientific Research. 2020. January 22;8(12). [Google Scholar]
- 65.Vidusha KS, Damayanthi MN. Prevalence of refractive errors among school children in the rural field practice area of a tertiary care hospital. Bengaluru Int J Community Med Public Health. 2018. April;5(4):1471–6. [Google Scholar]
- 66.Trivedi V, Zalawadiya S, Bhatt JV, Pawar T, Kupmavat B. Prevalance of refractive errors in children (age group 7–15 years) of rural and urban area of gujarat: A population based study. Indian Journal of Applied Basic Medical Sciences. 2006;8(1). [Google Scholar]
- 67.Warad C, Suranagi PV, Poornima N. Prevalence of refractive errors among school children in and around Davangere. J Pub Health Med Res. 2014;2(2):28–31. [Google Scholar]
- 68.Warkad VU, Panda L, Behera P, Das T, Mohanta BC, Khanna R. The Tribal Odisha Eye Disease Study (TOES) 1: prevalence and causes of visual impairment among tribal children in an urban school in Eastern India. Journal of American Association for Pediatric Ophthalmology and Strabismus. 2018. April;22(2):145–e1. 10.1016/j.jaapos.2017.10.020 [DOI] [PubMed] [Google Scholar]
- 69.Shukla Y, Gupta P, Tiwari R, Kasar PK. Uncorrected refractive error in schoolchildren at Jabalpur district of Madhya Pradesh. International Journal of Medical Science and Public Health. 2016. April;5(4):764–9. [Google Scholar]
- 70.Afroz AK, Nasti AR, Dar MA, Lone SA. Prevalence of refractive errors in school children. JK-Practitioner 2005;12(3): 156–159 [Google Scholar]
- 71.Ansari MA, Ahmad A, Khan Z. Prevalence of refractive errors and colour blindness among school children in district Aligarh. HSE. 2015;1(3):62–69. [Google Scholar]
- 72.Prabhu AV, Ve RS, Talukdar J, Chandrasekaran V. Prevalence of visual impairment in school-going children among the rural and urban setups in the Udupi district of Karnataka, India: A cross-sectional study. Oman J Ophthalmol. 2019;12(3):145–149. 10.4103/ojo.OJO_190_2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Bhat PA, Ishtiyaq J, Nisa AU, Balwan WK, Wani PM. Prevalence and Spectrum of Refractive Errors in Children Attending Out-Patient Department of Ophthalmology, Sher-I-Kashmir Institute of Medical Sciences, Srinagar. Journal of Medical Science and Clinical Research. 2015;3(8):7058–63. [Google Scholar]
- 74.Binu J, Jose R, Simon C. Prevalence of myopia and its associated risk factors among school children in Kollam- Kerala. Int J Health Sci Res. 2016; 6(6):30–38. [Google Scholar]
- 75.Gupta Y, Sukul RR, Gupta M, Phougat A, Jain R, Varshney A. School eye survey in rural population in UP, India. Nepalese Journal of Ophthalmology. 2011;3(1):78–9. 10.3126/nepjoph.v3i1.4282 [DOI] [PubMed] [Google Scholar]
- 76.Hittalamani SB, Jivangi VS. Prevalence of myopia among school going children. Int J Res Med Sci 2015;3:2786–90. [Google Scholar]
- 77.John DD, Paul P, Kujur ES, David S, Jasper S, Muliyil J. Prevalence of Refractive Errors and Number Needed to Screen among Rural High School Children in Southern India: A Cross-sectional Study. J Clin Diagn Res. 2017;11(8):NC16–NC19. 10.7860/JCDR/2017/25388.10476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Kavitha K, Rahesh SG, Sharmila N, Kumar CS. Analysis of Refractive Error Pattern in School Children in South Tamil Nadu. Int J Sci Stud 2016;4(5):26–28. [Google Scholar]
- 79.Kemmanu V, Hegde K, Giliyar SK, Shetty BK, Kumaramanickavel G, McCarty CA. Prevalence of Childhood Blindness and Ocular Morbidity in a Rural Pediatric Population in Southern India: The Pavagada Pediatric Eye Disease Study-1. Ophthalmic Epidemiol. 2016;23(3):185–192. 10.3109/09286586.2015.1090003 [DOI] [PubMed] [Google Scholar]
- 80.Kher P. Prevalence of myopia and its risk factors in rural schoolchildren. International Journal of Recent Surgical and Medical Sciences. 2017. June;3(01):029–33. [Google Scholar]
- 81.Maheshgauri RD, Paaranjpe RR, Gahlot A, Gohil A, Pote S, Bhavsar D. Prevalence of vitamin-A deficiency & refractive errors in primary school-going children. National Journal of Medical Research. 2016;6(1):23–27. [Google Scholar]
- 82.Pradhan N, Sachdeva A, Goel T, Bhola B, Jha D. Prevalence of refractive errors among school children of 6-12-years of age group and reason for not using spectacles even after correction. Int J Res Med Sci 2018;6:798–801. [Google Scholar]
- 83.Rajendran K, Haneef M, Chandrabhanu K, Muhammed M, Pillai RT. A prevalence study on myopia among school going children in a rural area of South India. Indian Journal of Clinical Practice. 2014;25(4):374–80. [Google Scholar]
- 84.Rao KRS, Krishna N, Vasantha G. Refractive errors in school children in Nizamabad district area. IAIM, 2016; 3(10): 21–26. [Google Scholar]
- 85.Sathyan S, Unnikrishnan M, Kunjachan A, Praseetha KP, Santy N, Wilson D, et al. Demographic profile of newly detected refractive errors among school going children in Thrissur district of Kerala. Kerala J Ophthalmol 2018;30:32–7. [Google Scholar]
- 86.Akarkar SO, Naik PG, Cacodcar JA. Prevalence and distribution of ocular morbidities among primary school children in Goa. J Clin Ophthalmol Res 2019;7:61–4. [Google Scholar]
- 87.Sudhan A, Pandey A, Pandey S, Srivastava P, Pandey KP, Jain BK. Effectiveness of using teachers to screen eyes of school-going children in Satna district of Madhya Pradesh, India. Indian J Ophthalmol. 2009;57(6):455–458. 10.4103/0301-4738.57157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Dong L, Kang YK, Li Y, Wei WB, Jonas JB. Prevalence and time trends of myopia in children and adolescents in China: A Systemic Review and Meta-Analysis. Retina Phila Pa. 2020. March;40(3):399–411. [DOI] [PubMed] [Google Scholar]
- 89.Chen M, Wu A, Zhang L, Wang W, Chen X, Yu X, et al. The increasing prevalence of myopia and high myopia among high school students in Fenghua city, eastern China: a 15-year population-based survey. BMC Ophthalmol. 2018. July 3;18(1):159 10.1186/s12886-018-0829-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Rudnicka AR, Kapetanakis VV, Wathern AK, Logan NS, Gilmartin B, Whincup PH, et al. Global variations and time trends in the prevalence of childhood myopia, a systematic review and quantitative meta-analysis: implications for aetiology and early prevention. Br J Ophthalmol. 2016. July;100(7):882–90. 10.1136/bjophthalmol-2015-307724 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Sheeladevi S, Seelam B, Nukella PB, Modi A, Ali R, Keay L. Prevalence of refractive errors in children in India: a systematic review. Clinical and Experimental Optometry. 2018. July;101(4):495–503. 10.1111/cxo.12689 [DOI] [PubMed] [Google Scholar]
- 92.National Health Profile 2015 [Internet] [cited Aug 8 2020]. Available from: https://www.cbhidghs.nic.in/WriteReadData/l892s/NHP-2015.pdf
- 93.Mountjoy E, Davies NM, Plotnikov D, Smith GD, Rodriguez S, Williams CE, et al. Education and myopia: assessing the direction of causality by mendelian randomisation. BMJ 2018. June 6;361:k2022 10.1136/bmj.k2022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Morgan IG, Rose KA. Myopia and international educational performance. Ophthalmic Physiol Opt J Br Coll Ophthalmic Opt Optom. 2013. May;33(3):329–38. [DOI] [PubMed] [Google Scholar]
- 95.Grzybowski A, Kanclerz P, Tsubota K, Lanca C, Saw S-M. A review on the epidemiology of myopia in school children worldwide. BMC Ophthalmol. 2020. January 14;20(1):27 10.1186/s12886-019-1220-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Gupta V, Saxena R, Vashist P, Bhardwaj A, Pandey RM, Tandon R, et al. Spectacle coverage among urban schoolchildren with refractive error provided subsidized spectacles in North India. Optom Vis Sci Off Publ Am Acad Optom. 2019;96(4):301–8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(TIF)
(TIF)
(TIF)
Standard quality assessment tool given by Hoy et al. Aggregate score <4- low risk, 4–6 moderate risk, >6 high risk. High risk studies are excluded (0- low risk, 1- high risk) [10].
(DOCX)
*NA- not available, ** Based on Standard quality assessment tool given by Hoy et al. [10].
(DOCX)
(DOCX)
(DOCX)
(DOC)
(ZIP)
Data Availability Statement
All relevant data are within the manuscript and its Supporting Information files.