Abstract
Objective
This review was done to determine the prevalence of metabolic syndrome (MS) among adult general population in India. We also wanted to find the gender, setting, and region-wide distribution of MS in India.
Methods
We conducted systematic searches in various databases including Medline, ScienceDirect, Cochrane library and Google Scholar from inception until August 2019. We included studies conducted in India reporting the prevalence of MS among adults aged 18 years or more. We used the Newcastle Ottawa scale to assess the quality of included studies. We carried out a meta-analysis with random-effects model and reported pooled prevalence with 95% confidence intervals (CIs). We used the Funnel plot to assess publication biases.
Results
In total, we analysed 113 data from 111 studies with 133,926 participants. Majority of the included studies (76 out of 111) had low risk of bias. We found significant heterogeneity among the included studies (p<0.001). We also found a symmetrical funnel plot indicating an absence of publication bias. The prevalence of MS among adult population in India was 30% (95%CI: 28%-33%). There was a steady increase in the burden across the age groups from 13% (18–29 years group) to 50% (50–59 years). We also found that people living in urban areas (32%; 95%CI: 29%-36%) had higher prevalence when compared to tribal (28%; 95%CI: 21%-36%) or rural adults (22%; 95%CI: 20%-25%). Gender distribution of MS showed that the females had higher prevalence (35%; 95%CI: 31%-38%) when compared to males 26% (95%CI: 22%-29%).
Conclusion
Almost one in three adults in India suffer from MS. Females, people living in urban areas and in northeast region had higher prevalence of MS. Development and implementation of policies and protocols for the screening of MS would enable us in early diagnosis and treatment with special focus towards the vulnerable and high-risk groups.
Introduction
Disease patterns around the globe are undergoing rapid structural changes over the last three decades, with a sudden increase in the burden of Non-Communicable Diseases (NCDs) and a decreasing trend of communicable diseases [1]. The Global Burden of Disease (GBD) study, brings to light this phenomenon of epidemiological transition in India, with a 62.7% of the total mortality in 2016 contributed by the NCDs. Key elements contributing to the development of these NCDs have been identified and are studied together under the heading of Metabolic Syndrome (MS) [2].
Metabolic syndrome is a constellation of interconnected physiological, biochemical, clinical and metabolic factors that directly increases the risk of cardiovascular diseases, type 2 diabetes mellitus (DM) and all-cause mortality. It is constituted by abdominal obesity, insulin resistance, hypertension, and hyperlipidemia [3]. Various diagnostic criteria have been proposed for quantifying MS. But the most widely used ones are from the International Diabetic Federation (IDF) and the National Cholesterol Education Program Adult Treatment Panel III (NCEP ATP III) [4, 5].
Metabolic syndrome increases the risk of developing type 2 DM and cardiovascular diseases over the next 5 to 10 years by five and two-fold respectively [3]. Furthermore the patients with MS have, an average four-fold increased risk of developing stroke & myocardial infarction and a two-fold risk of dying from a similar event compared with those without MS, regardless of previous history of cardiovascular events [6]. Identifying the individuals with (or) at risk of developing MS would help to inform the probabilities of worse outcomes and thus an urgent need for a promotive, preventive or curative action.
A recent study from the United States reported the prevalence of MS to be around 22.9% [7]. Various population-based studies were conducted in India too, to quantify the same and the results ranged from 10 to 30 percentage [8]. A study conducted in the eleven large urban cities of India during 2006–2010 reported the prevalence of MS as high as 35% [9]. Owing to the behavioural habits, urban population, seem to be the most vulnerable group for developing MS [10]. Prevalence of MS, thus, seems to vary greatly from region to region and from ethnicity to ethnicity.
Even though evidences are being generated on MS from different parts of the country, there is no nationwide pooled estimate to comment on the burden of MS in the Indian subcontinent, which could drive policy action [11]. With almost one third of the total population living in the urban areas, and with 40% of the population aged between 30 and 70 years, understanding the overall prevalence of MS in India becomes essential for predicting the future burden of type 2 DM and cardiovascular diseases [12].
While the NCD care in the country is segregated under the broad headings of Diabetes, and Cardiovascular diseases, MS informs us the need to look at the picture as a whole. Results from this study would, thus, help guide national policy making process to give due importance to prevention and treatment of MS in the community and clinical settings. This could thus be an essential key to keep a check on the ever-increasing burden of the NCD epidemic in the country. Hence, this review was conducted to generate a pooled prevalence estimate for MS in India.
Methods
Design and registration
We conducted a systematic review and meta-analysis of cross-sectional studies. We have obtained approval from the JIPMER Scientific Advisory Committee (JSAC). We have also obtained exemption from Institutional Ethics Committee (IEC). We have registered our protocol on the international prospective register of systematic review (PROSPERO). PROSPERO Registration Number is CRD42019147277. We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist for reporting systematic reviews incorporating meta-analyses for reporting our review.
Eligibility criteria
Type of studies
We included studies conducted in India reporting the prevalence of MS for the current review. There was no restriction related to study design, communities (rural/urban) or age groups. We included the studies irrespective of the setting in which the study was conducted (community or facility based or workplace based). Studies reported as full text were included while unpublished data were excluded from the review.
Type of participants
We included studies conducted among adults aged 18 years or more. We excluded the studies conducted among specific diseased population.
Type of outcome measure
Studies reporting the prevalence of MS and diagnosed it as per the NCEP ATP III or IDF guidelines were included to obtain the pooled prevalence estimate for MS in India.
Search strategy
We conducted extensive electronic search in the following databases: Medline, ScienceDirect, Cochrane library and Google Scholar. Combination of medical subject heading (MeSH) and free text terms were used for carrying out literature search. The detailed search strategy used to search the Medline database has been reported in S1 File. Similar strategies were used in Cochrane Library, ScienceDirect and Google scholar for literature search of published studies. Search was conducted in all the databases from inception of the database to August 2019 with English language restriction for publication. We also checked the reference list of primary studies obtained through electronic search and relevant articles were included in the review and analysis.
Selection of studies
Two independent investigators (YK and TR) independently performed the literature search and screened the title, abstract and keywords of all the studies identified for possible inclusion in the review. Full text article was obtained for those studies that are found to be relevant. Further screening of abstract and full text of the retrieved articles was done independently by two investigators (YK and TR) to select the studies which satisfy the eligibility criteria of the current review. Any disagreements during the entire selection process between two authors were resolved either through consensus or consultation with third investigator (SR). Quality of the overall review process was monitored by the third investigator (SR).
Data extraction and management
Primary investigator (YK) extracted the relevant study characteristics for the review from the included studies using the Cochrane Public Health group Data extraction and Assessment Template. Following data were extracted:
General information
Author, Study title, Publication year.
Methods section
Study design, study period, study setting (community/workplace/facility), community (urban/rural/tribal), geographical region, state, sample size, sampling technique, diagnostic criteria, outcome assessment and statistical tests employed.
Outcome section
Mean age, non-response rate and their characteristics, prevalence of MS.
Primary investigator (YK) transferred the obtained data into the software STATA version 14. Data entry was double checked for correct entry by another investigator (SR) through comparison of data presented in review and included study reports.
Risk of bias assessment in included studies
Two independent authors (SR and SM) assessed the quality of all the included studies using the Newcastle-Ottawa (NO) scale adapted for cross sectional studies [13]. Two criteria (selection and outcome) were used to assess the risk of bias. Following domains were used for assessing the risk of bias under selection criteria: representativeness of the sample, justification of sample size, rate of non-respondents and their characteristics and use of validated measurement tool. Under Outcome criteria, outcome assessment and statistical test employed were used to assess the risk of bias. Each of these outcomes was rated as high (1 point) or low (0 points) based on the quality of evidence and availability of information. Studies scoring more than or equal to 3 points were considered to have high risk of bias.
Statistical analysis
Meta-analysis was performed with the selected studies using STATA 14.2 (StataCorp, College Station, TX, USA). For each of the studies, standard error was calculated using the reported prevalence of MS and total sample size. “Metaprop” function was used for performing analysis of the current review [14]. To minimize the effect of extremely small or large prevalence on the overall estimate, Freeman Tukey double arc-sine transformation was done to stabilise the variance [14]. Final pooling of data was done with random effects model and reported as proportion with 95% confidence interval.
Evidence of between-study variance due to heterogeneity was assessed through following methods: Chi square test for heterogeneity and I2 statistics to quantify the inconsistency. I2 less than 25% was mild, 25–75% was moderate and more than 75% was considered as substantial heterogeneity [15]. Sub-group analysis was performed based on age group, gender, geographical region (North/South/West/East/Northeast/Central), study setting (community/workplace/facility), diagnostic criteria, waist circumference measurement, year of publication, quality of studies, representativeness of the sample and urban/rural/tribal communities. Potential covariates for meta-regression were study setting, region, diagnostic criteria, representativeness of the sample, year of publication, mean age and quality of evidence. We performed multivariable meta-regression analysis by including the study level factors with p value less than 0.2 in the univariate model. We performed sensitivity analysis to assess the robustness of the results by excluding the studies conducted exclusively on elderly (≥60 years), studies having high risk of bias or not conducted on a representative sample, and studies conducted before 2007.
Study specific prevalence estimates and pooled estimates were graphically represented through forest plot for both combined and subgroup analysis. Publication bias was assessed and graphically represented by funnel plot; asymmetry of the plot was tested using Egger’s test and p value less than 0.10 was considered as statistically significant publication bias [16].
Results
Study selection
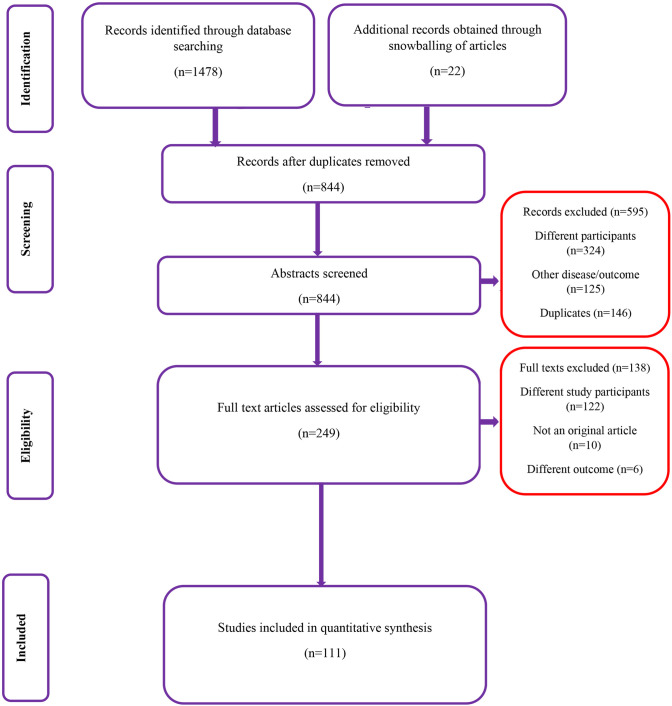
We conducted a systematic search to find studies that report the prevalence of MS from the dates of database inception until August 2019. During the first stage of screening (title, abstract and keywords), we retrieved 310 studies from the following databases: Medline, ScienceDirect, Cochrane library and Google Scholar. After removal of duplicates, we reviewed 249 articles’ full texts against our eligibility criteria for the possible inclusion in the review. We reviewed the bibliographies of the retrieved articles and found four more relevant studies. Finally, we analysed 111 studies with 133,926 participants satisfying the inclusion criteria (Fig 1) [17–127].
Fig 1. Flow chart showing the search strategy and selection of studies.
Characteristics of the included studies
Table 1 lists the characteristics of the studies analysed. Most of the studies (46) were conducted in Southern states like Andhra Pradesh, Karnataka, Kerala and Tamil Nadu. The mean age of study participants ranged from 19.6 to 69.4 years. Coming to the study setting, 83 were from community-based studies followed by 21 from facility-based studies and 9 from workplace-based studies. The sample sizes in the studies varied from 60 to 9,886. Majority of the studies (49 out of 111) have reported separate estimates for urban region, while 34 studies reported for rural and 4 studies for tribal region. Rest of the studies did not provide separate estimates for urban, rural or tribal regions because of the study setting (facility or workplace-based studies). Majority (82 out of 111) studies have reported estimates for female burden of MS while 76 studies have reported estimates for male adult population.
Table 1. Characteristics of the studies included (N = 111).
| S.N. | Author and year | State | Geographical Region | Setting | Urban/Rural/Tribal | Age group (years) | Gender | Sample size | Diagnostic criteria | Prevalence (95%CI) |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. | Bal 2011 | Chandigarh | North | Facility | NA | 25–50 | Males & Females | 440 | NCEP ATP -III | 37% (32%-42%) |
| 2. | Bandella 2017 | Andhra Pradesh | South | Community | Urban, rural and tribal | 20–60 | Males & Females | 1032 | NCEP ATP -III | 32% (29%-35%) |
| 3. | Bansal 2009 | New Delhi | North | Facility | NA | ≥18 | Males & Females | 1905 | NCEP ATP -III | 48% (45%-50%) |
| 4. | Bansal 2017 | Uttar Pradesh | Central | Facility | NA | 30–70 | Males & Females | 350 | NCEP ATP -III | 17% (13%-21%) |
| 5. | Bansal A 2015 | New Delhi | North | Community | Urban | 35–65 | Males & Females | 406 | NCEP ATP -III | 75% (71%-79%) |
| 6. | Barik A 2017 | West Bengal | East | Community | Rural | ≥18 | Males & Females | 9886 | NCEP ATP -III | 16% (15%-17%) |
| 7. | Basha 2018 | Andhra Pradesh | South | Community | Urban | ≥18 | Males & Females | 802 | NCEP ATP -III | 32% (29%-35%) |
| 8. | Bhagat 2017 | Chandigarh | North | Community | Urban | 18–25 | Males & Females | 611 | IDF | 18% (15%-22%) |
| 9. | Bhat R 2010 | Jammu & Kashmir | North | Facility | NA | ≥18 | Males & Females | 500 | NCEP ATP -III | 9% (6%-11%) |
| 10. | Bhattacharya 2016 | Telangana | South | Facility | NA | ≥60 | Males & Females | 114 | NCEP ATP -III | 42% (33%-52%) |
| 11. | Bhutia 2017 | Sikkim | Northeast | Facility | NA | ≥20 | Males & Females | 361 | IDF | 34% (29%-39%) |
| 12. | Chakraborty 2015 | West Bengal | East | Community | Urban | ≥18 | Males & Females | 690 | NCEP ATP -III | 33% (29%-36%) |
| 13. | Chhabra 2014 | Not mentioned | North | Community | Urban & Rural | 25–60 | Females | 200 | NCEP ATP -III | 33% (27%-40%) |
| 14. | Chinawale 2018 | Gujarat | West | Community | Not mentioned | 20–80 | Males & Females | 473 | IDF | 41% (37%-46%) |
| 15. | Chow 2007 | Andhra Pradesh | South | Community | Rural | ≥30 | Males & Females | 4535 | NCEP ATP -III | 25% (23%-26%) |
| 16. | Das 2011 | West Bengal | East | Community | Urban & Rural | ≥30 | Males & Females | 350 | NCEP ATP -III | 48% (43%-54%) |
| 17. | Das 2017 | West Bengal | East | Community | Not mentioned | 18–24 | Males & Females | 397 | IDF | 5% (3%-7%) |
| 18. | Das M 2011 | West Bengal | East | Community | Urban & Rural | ≥30 | Males & Females | 448 | NCEP ATP -III | 29% (25%-34%) |
| 19. | Deedwania 2014 | 11 cities in India | India | Community | Urban | ≥20 | Males & Females | 6198 | NCEP ATP -III | 36% (35%-37%) |
| 20. | Deepa M 2006 | Tamil Nadu | South | Community | Urban | ≥20 | Males & Females | 2350 | NCEP ATP -III | 18% (17%-20%) |
| 21. | Deshmukh 2012 | Maharashtra | Central | Community | Rural | ≥18 | Males & Females | 300 | NCEP ATP -III | 17% (13%-22%) |
| 22. | Dhabriya 2015 | Rajasthan | North | Community | Urban | ≥18 | Males & Females | 1130 | IDF | 23% (20–25%) |
| 23. | Goyal 2013 | Uttarkhand | North | Facility | NA | ≥18 | Males & Females | 380 | IDF | 21% (17%-26%) |
| 24. | Gupta 2012 | Rajasthan | North | Community | Urban | ≥20 | Males & Females | 6106 | NCEP ATP -III | 26% (25%-27%) |
| 25. | Gupta A 2004 | Rajasthan | North | Community | Urban | ≥20 | Males & Females | 1091 | NCEP ATP III | 32% (29%-34%) |
| 26. | Gupta R 2007 | Rajasthan | North | Community | Urban | ≥20 | Males & Females | 644 | NCEP ATP III | 47% (43%-51%) |
| 27. | Gupta R 2012 | Rajasthan | North | Community | Urban | 20–60 | Males & Females | 739 | NCEP ATP III | 23% (20%-26%) |
| 28. | Harikrishnan 2018 | Kerala | South | Community | Urban & Rural | ≥20 | Males & Females | 5063 | NCEP ATP III | 24% (23%-25%) |
| 29. | Ismail 2016 | Kerala | South | Community | Tribal | ≥18 | Males & Females | 120 | NCEP ATP III | 28% (20%-37%) |
| 30. | Jain 2015 | Maharashtra | Central | Facility | NA | 18–25 | Males & Females | 668 | NCEP ATP III | 11% (9%-14%) |
| 31. | Jeyasheela 2018 | Tamil Nadu | South | Facility | NA | ≥45 | Females | 154 | IDF | 64% (56%-72%) |
| 32. | Jones 2016 | Andhra Pradesh | South | Community | Rural | ≥18 | Males & Females | 6217 | NCEP ATP III | 14% (13%-15%) |
| 33. | Kamble 2010 | Maharashtra | Central | Community | Rural | ≥18 | Males & Females | 300 | NCEP ATP III | 9% (6%-13%) |
| 34. | Kandpal 2016 | Uttarkhand | North | Community | Tribal | 20–60 | Males & Females | 288 | NCEP ATP III | 39% (34%-45%) |
| 35. | Kanjilal 2008 | Karnataka, Maharashtra | South & Central | Facility | NA | ≥20 | Males & Females | 2315 | NCEP ATP III | 58% (56%-60%) |
| 36. | Kapil 2018 | Uttarkhand | North | Community | Rural | ≥60 | Males & Females | 979 | IDF | 29% (26%-32%) |
| 37. | Kaur J 2014 | Punjab | North | Community | Urban & Rural | ≥20 | Males & Females | 351 | NCEP ATP III | 17% (14%-22%) |
| 38. | Kaur P 2010 | Tamil Nadu | South | Workplace | NA | ≥20 | Males | 1077 | IDF | 41% (38%-44%) |
| 39. | Kaushal 2016 | Uttar Pradesh | Central | Community | Urban | ≥20 | Males & Females | 127 | NCEP ATP III | 37% (29%-46%) |
| 40. | Kempegowda 2011 | Karnataka | South | Community | Rural | ≥20 | Males & Females | 495 | NCEP ATP III | 20% (16%-23%) |
| 41. | Khan 2018 | Uttar Pradesh | Central | Facility | NA | ≥20 | Males & Females | 420 | NCEP ATP III | 41% (36%-46%) |
| 42. | Kotokey 2013 | Assam | Northeast | Community | Urban | ≥20 | Males & Females | 502 | IDF | 33% (29%-37%) |
| 43. | Kunti 2019 | West Bengal | East | Facility | NA | ≥18 | Males & Females | 330 | NCEP ATP III | 64% (58%-69%) |
| 44. | Lakshmipriya 2012 | Tamil Nadu | South | Community | Urban | ≥20 | Males & Females | 1875 | IDF | 28% (26%-30%) |
| 45. | Lateef 2007 | Andhra Pradesh | South | Community | Urban | ≥20 | Males & Females | 1519 | NCEP ATP III | 24% (22%-27%) |
| 46. | Lavanya 2012 | Andhra Pradesh | South | Community | Urban | ≥20 | Males & Females | 350 | NCEP ATP III | 23% (19%-28%) |
| 47. | Madan G 2016 | Maharashtra | West | Community | Urban & Rural | 18–65 | Males | 313 | IDF | 40% (34%-46%) |
| 48. | Madhav 2013 | Andhra Pradesh | South | Workplace | NA | ≥20 | Males | 180 | IDF | 22% (16%-28%) |
| 49. | Mahadik 2007 | Maharashtra | West | Community | Urban & Rural | ≥20 | Males & Females | 1071 | NCEP ATP III | 24% (22%-27%) |
| 50. | Mahajan 2012 | New Delhi | North | Community | Urban & Rural | ≥20 | Males & Females | 7174 | NCEP ATP III | 57% (56%-58%) |
| 51. | Mahanta 2013 | Assam | Northeast | Community | Urban & Rural | ≥35 | Males & Females | 297 | NCEP ATP III | 27% (22%-32%) |
| 52. | Mahanta 2017 | Assam | Northeast | Community | Urban & Rural | 20–60 | Males & Females | 3372 | NCEP ATP III | 48% (46%-49%) |
| 53. | Majumdar 2011 | Karnataka | South | Community | Not available | 18–75 | Males & Females | 441 | NCEP ATP III | 28% (24%-32%) |
| 54. | Majumdar 2017 | Andhra Pradesh | South | Community | Urban | ≥60 | Males & Females | 112 | IDF | 54% (45%-64%) |
| 55. | Mangat 2010 | Chandigarh | North | Community | Urban & Rural | ≥18 | Males & Females | 605 | NCEP ATP III | 39% (35%-43%) |
| 56. | Manjunath 2014 | Andhra Pradesh | South | Community | Urban | 18–25 | Males & Females | 473 | NCEP ATP III | 4% (2%-6%) |
| 57. | Mini 2018 | Kerala | South | Workplace | NA | 18–64 | Males & Females | 2287 | NCEP ATP III | 19% (18%-21%) |
| 58. | Misra 2011 | Haryana | North | Community | Rural | ≥20 | Males & Females | 307 | NCEP ATP III | 12% (9%-16%) |
| 59. | Mittal 2018 | Uttar Pradesh | Central | Community | Urban & Rural | ≥20 | Males & Females | 125 | IDF | 35% (27%-44%) |
| 60. | Mohan 2007 | Tamil Nadu | South | Community | Urban & Rural | ≥20 | Males & Females | 1736 | NCEP ATP III | 17% (15%-19%) |
| 61. | Mohan 2009 | Tamil Nadu | South | Community | Urban & Rural | ≥20 | Males & Females | 541 | NCEP ATP III | 37% (33%-41%) |
| 62. | Nag 2015 | West Bengal | East | Community | Rural | ≥20 | Males & Females | 1007 | IDF | 26% (23%-29%) |
| 63. | Naik 2016 | Andhra Pradesh | South | Community | Urban | ≥60 | Males & Females | 295 | IDF | 35% (29%-40%) |
| 64. | Nithya 2015 | Tamil Nadu | South | Community | Rural | ≥60 | Males & Females | 514 | NCEP ATP III | 20% (17%-24%) |
| 65. | Pai 2019 | Karnataka | South | Community | Urban & Rural | ≥20 | Males & Females | 420 | NCEP ATP III | 4% (2%-6%) |
| 66. | Pandey 2010 | Maharashtra | West | Community | Urban | 35–65 | Females | 498 | IDF | 57% (52%-61%) |
| 67. | Parale 2008 | Karnataka | South | Workplace | NA | ≥30 | Males & Females | 700 | NCEP ATP III | 27% (24%-30%) |
| 68. | Patel 2016 | Gujarat | West | Facility | NA | 25–65 | Males & Females | 478 | NCEP ATP III | 26% (22%-30%) |
| 69. | Pathak 2018 | Haryana | North | Community | Rural | ≥20 | Males & Females | 1200 | IDF | 9% (8%-11%) |
| 70. | Pemminati 2010 | Karnataka | South | Community | Urban | ≥20 | Males & Females | 451 | IDF | 30% (26%-34%) |
| 71. | Prabhakaran 2005 | New Delhi | North | Workplace | NA | 20–59 | Males | 2120 | NCEP ATP III | 35% (33%-37%) |
| 72. | Prabhakaran 2007 | New Delhi | North | Community | Urban & Rural | 35–64 | Males & Females | 4044 | NCEP ATP III | 33% (32%-35%) |
| 73. | Pradeepa 2016 | Tamil Nadu | South | Community | Urban | ≥60 | Males & Females | 222 | IDF | 37% (31%-44%) |
| 74. | Prakash 2013 | Uttar Pradesh | North | Facility | NA | ≥18 | Males & Females | 1340 | NCEP ATP III | 32% (30%-35%) |
| 75. | Prasad 2012 | Orissa | East | Community | Urban | 20–80 | Males & Females | 1178 | IDF | 43% (40%-46%) |
| 76. | Rajput 2014 | Haryana | North | Community | Urban & Rural | ≥20 | Males & Females | 3042 | IDF | 29% (27%-31%) |
| 77. | Ramachandran 2003 | Tamil Nadu | South | Community | Not mentioned | 20–75 | Males & Females | 475 | NCEP ATP III | 41% (37%-46%) |
| 78. | Ramachandran 2008 | Tamil Nadu | South | Workplace | NA | ≥20 | Males & Females | 2499 | NCEP ATP III | 29% (27%-31%) |
| Ramachandran 2008 | Tamil Nadu | South | Community | Urban | ≥20 | Males & Females | 3278 | NCEP ATP III | 41% (37%-46%) | |
| 79. | Randhwa 2015 | Punjab | North | Community | Rural | 25–55 | Females | 300 | NCEP ATP III | 26% (21%-31%) |
| 80. | Ravikiran 2010 | Chandigarh | North | Community | Urban & Rural | ≥20 | Males & Females | 2225 | NCEP ATP III | 45% (43%-47%) |
| 81. | Roopa 2010 | Tamil Nadu | South | Community | Urban | ≥20 | Males & Females | 358 | NCEP ATP III | 35% (30%-40%) |
| 82. | Sachdev 2009 | New Delhi | North | Community | Urban | 26–32 | Males & Females | 1492 | IDF | 25% (23%-27%) |
| 83. | Sarkar P 2016 | Karnataka | South | Community | Rural | ≥30 | Males & Females | 448 | NCEP ATP III | 26% (22%-30%) |
| 84. | Sarkar S 2006 | West Bengal | East | Community | Tribal | ≥20 | Males & Females | 588 | NCEP ATP III | 25% (22%-29%) |
| 85. | Sarma 2015 | Andhra Pradesh | South | Community | Rural | 30–50 | Females | 60 | NCEP ATP III | 20% (11%-32%) |
| 86. | Sawant 2011 | Maharashtra | West | Community | Urban | ≥20 | Males & Females | 548 | NCEP ATP III | 20% (16%-23%) |
| 87. | Selvaraj 2012 | Tamil Nadu | South | Community | Rural | 30–50 | Females | 150 | NCEP ATP III | 31% (23%-39%) |
| 88. | Selvaraj 2019 | Tamil Nadu | South | Community | Rural | 20–40 | Males | 360 | NCEP ATP III | 17% (13%-21%) |
| 89. | Shalini 2013 | Karnataka | South | Community | Urban & Rural | ≥18 | Females | 1023 | NCEP ATP III | 57% (54%-60%) |
| 90. | Sharma MK 2018 | Uttar Pradesh | Central | Community | Urban & Rural | 20–55 | Males & Females | 290 | NCEP ATP III | 20% (16%-25%) |
| 91. | Sharma R 2019 | Jammu & Kashmir | North | Community | Not mentioned | ≥18 | Males & Females | 210 | NCEP ATP III | 35% (29%-42%) |
| 92. | Sharma S 2016 | Chandigarh | North | Facility | NA | 45–55 | Females | 350 | NCEP ATP III | 63% (57%-68%) |
| 93. | Sharma S 2016 | Karnataka | South | Workplace | NA | 20–50 | Males & Females | 210 | NCEP ATP III | 12% (8%-17%) |
| 94. | Singh 2016 | Haryana | North | Community | Rural | ≥20 | Males & Females | 1700 | IDF | 27% (25%-29%) |
| 95. | Singh 2017 | Uttar Pradesh | North | Community | Urban | ≥25 | Males & Females | 2002 | NCEP ATP III | 19% (18%-21%) |
| 96. | Sinha N 2016 | Telangana | South | Community | Urban | ≥60 | Males & Females | 114 | IDF | 42% (33%-52%) |
| 97. | Sinha S 2012 | New Delhi | North | Community | Urban | ≥20 | Females | 226 | NCEP ATP III | 30% (24%-36%) |
| 98. | Srimani 2017 | West Bengal | East | Community | Rural | 45–70 | Females | 222 | IDF | 46% (39%-53%) |
| 99. | Srimani 2018 | West Bengal | East | Community | Rural | 45–70 | Females | 509 | IDF | 38% (34%-42%) |
| 100. | Srinivasan 2016 | Kerala | South | Facility | NA | ≥20 | Males & Females | 432 | NCEP ATP III | 61% (56%-66%) |
| 101. | Subramani 2018 | Madhya Pradesh | Central | Facility | NA | 20–79 | Males & Females | 1190 | NCEP ATP III | 50% (47%-53%) |
| 102. | Tandon 2010 | Jammu & Kashmir | North | Community | Rural | ≥45 | Females | 500 | NCEP ATP III | 13% (10%-16%) |
| 103. | Tharkar 2010 | Tamil Nadu | South | Community | Urban | ≥20 | Males & Females | 2021 | NCEP ATP III | 32% (30%-34%) |
| 104. | Tharkar S 2008 | Tamil Nadu | South | Workplace | NA | ≥30 | Males & Females | 318 | IDF | 57% (52%-63%) |
| Tharkar S 2008 | Tamil Nadu | South | Community | Urban | ≥30 | Males & Females | 410 | IDF | 28% (23%-32%) | |
| 105. | Thayyil 2012 | Kerala | South | Workplace | NA | ≥30 | Males | 823 | NCEP ATP III | 17% (14%-19%) |
| 106. | Thiruvagounder 2010 | Tamil Nadu | South | Facility | NA | ≥20 | Males & Females | 1568 | NCEP ATP III | 29% (27%-31%) |
| 107. | Thyagi 2013 | Uttar Pradesh | Central | Facility | NA | 25–65 | Males & Females | 405 | NCEP ATP III | 43% (38%-48%) |
| 108. | Vatakanchery 2019 | Kerala | South | Facility | NA | 20–60 | Males & Females | 520 | IDF | 76% (72%-80%) |
| 109. | Venugopal 2019 | Pondicherry | South | Community | Rural | ≥30 | Males & Females | 489 | IDF | 40% (35%-44%) |
| 110. | Wani 2014 | Jammu & Kashmir | North | Facility | NA | 20–60 | Males & Females | 500 | NCEP ATP III | 9% (6%-11%) |
| 111. | Zafar 2017 | Uttar Pradesh | West | Community | Rural | 18–55 | Males & Females | 2982 | NCEP ATP III | 12% (11%-13%) |
NCEP ATP III–National Cholesterol Education Program Adult Treatment Panel III.
IDF–International Diabetes Federation.
NA–Not applicable.
Methodological quality of the included studies
We performed assessments of risk of bias for all the included studies using NO scale. First, selection bias domains were assessed and it was found that 64 out of 111 studies (58% of studies) had high risk of bias related to representativeness of the sample for our review, 80 (72%) studies did not report proper justification for sample size, 69 (62%) studies did not report non-response rate or their characteristics. All the studies reported use of validated measurement tool. Under the outcome domain, only one study did not independently assess the outcome; nine studies did not report the statistical methods used in the study. Almost one-third i.e. 35 (31.5%) of the included studies had high risk of bias as per NO scale.
Burden of metabolic syndrome in India
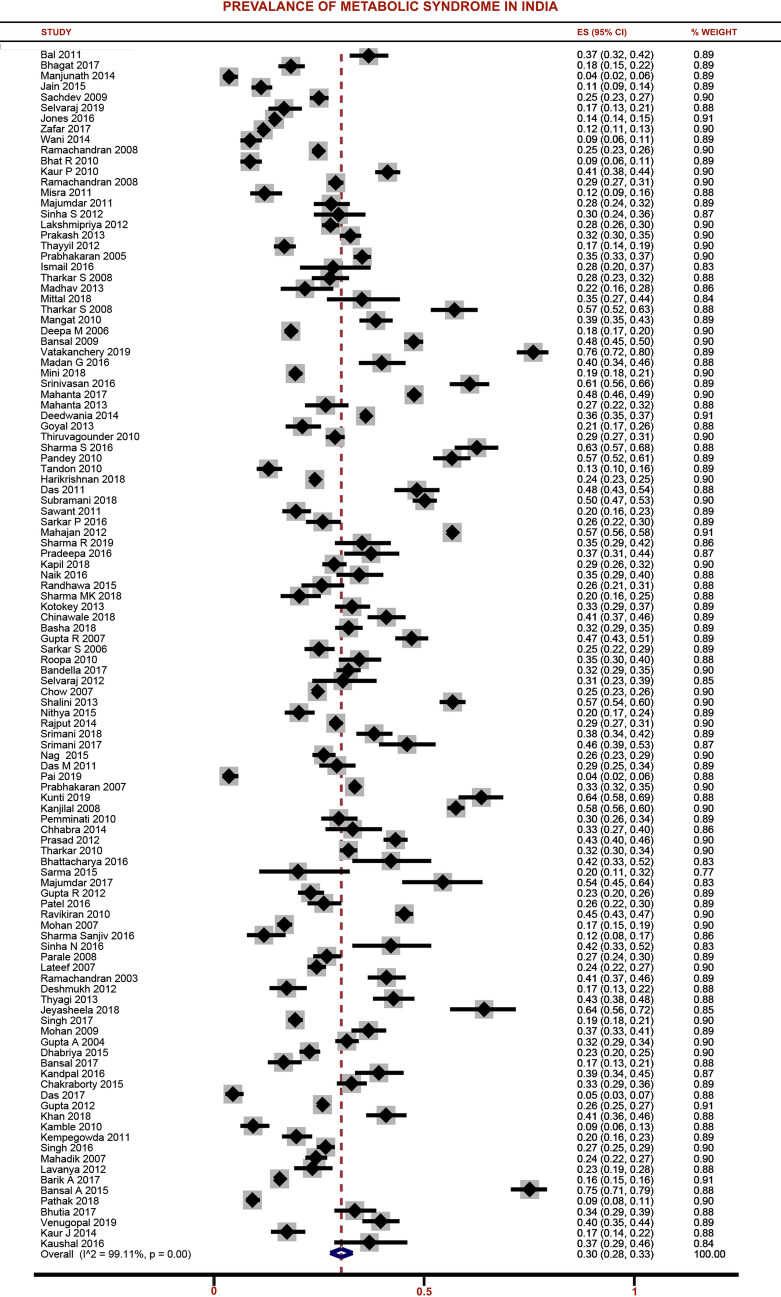
Pooled estimate was calculated after adjusting for population size weights and graphically depicted in Fig 2. The overall pooled prevalence of MS among adult population in India was 30% (95%CI: 28%-33%).
Fig 2. Forest plot showing the prevalence of metabolic syndrome among adult population in India.
State wise analysis of MS showed that the maximum prevalence of MS was reported in Madhya Pradesh (50%) followed by New Delhi (43%), Odisha (43%) and Telangana (42%). Least pooled prevalence of MS was found in Jammu & Kashmir (15%) followed by Haryana (18%) and Punjab (21%). There was a significant heterogeneity found among the studies included in our review (I2 = 99.1%; p<0.001). Additional subgroup analysis was performed to explore the source of heterogeneity and obtain separate estimates based on age group, gender, study setting, geographical area and regions, year of publication, representativeness of sample, waist circumference measurement, quality of studies and diagnostic criteria (Table 2).
Table 2. Summary of findings and subgroup analysis of studies reporting prevalence of metabolic syndrome in India.
| Characteristic | Number of studies pooled | Pooled ES# (95% CI) | I2 | P for heterogeneity/trend |
|---|---|---|---|---|
| Pooled prevalence of Metabolic syndrome in India = 30% (95%CI: 28%-33%) | ||||
| AGE GROUP | ||||
| 18–29 years | 12 | 13% (8%-18%) | 93.3% | <0.001 |
| 30–39 years | 11 | 32% (24%-41%) | 96.7% | |
| 40–49 years | 11 | 41% (33%-48%) | 95.9% | |
| 50–59 years | 10 | 50% (43%-57%) | 94.3% | |
| ≥60 years | 17 | 41% (34%-49%) | 97.3% | |
| GENDER | ||||
| Male | 76 | 26% (22%-29%) | 98.6% | 0.04 |
| Female | 82 | 35% (31%-38%) | 98.8% | |
| URBAN VS RURAL VS TRIBAL | ||||
| Urban | 49 | 32% (29%-36%) | 98.9% | <0.001 |
| Rural | 34 | 22% (20%-25%) | 97.7% | |
| Tribal | 4 | 28% (21%-36%) | 88.4% | |
| STUDY SETTING | ||||
| Community | 83 | 29% (26%-32%) | 99.1% | 0.08 |
| Facility | 21 | 38% (30%-47%) | 99.1% | |
| Workplace | 9 | 28% (22%-35%) | 98.2% | |
| GEOGRAPHICAL REGION | ||||
| North | 31 | 30% (25%-35%) | 99.2% | 0.83 |
| South | 46 | 30% (26%-33%) | 98.5% | |
| East | 11 | 33% (23%-43%) | 99.1% | |
| West | 7 | 30% (19%-44%) | 99% | |
| Central | 10 | 27% (17%-39%) | 98.4% | |
| Northeast | 4 | 35% (25%-46%) | 96.7% | |
| DIAGNOSTIC CRITERIA | ||||
| NTEP-ATP III | 81 | 29% (26%-32%) | 99.2% | 0.05 |
| IDF | 32 | 34% (30%-39%) | 98.3% | |
| WAIST CIRCUMFERENCE MEASUREMENT | ||||
| Tip of iliac crest | 34 | 29% (25%-33%) | 98.6% | 0.67 |
| Midline of iliac crest & costal margin | 22 | 32% (26%-39%) | 99% | |
| YEAR OF PUBLICATION | ||||
| 2003–2006 | 5 | 30% (22%-39%) | 98.2% | 0.62 |
| 2007–2010 | 26 | 32% (27%-36%) | 98.9% | |
| 2011–2014 | 30 | 27% (23%-33%) | 99.1% | |
| 2015–2019 | 52 | 31% (27%-36%) | 99.1% | |
| SAMPLING (REPRESENTATIVENESS) | ||||
| Random | 47 | 29% (25%-33%) | 99.3 | 0.37 |
| Non-random | 64 | 31% (27%-35%) | 98.8% | |
| QUALITY OF STUDIES | ||||
| Low | 35 | 32% (28%-36%) | 98.4% | 0.40 |
| High | 76 | 29% (26%-33%) | 99.2% | |
Age wise distribution of metabolic syndrome in India
The pooled prevalence of MS differed significantly across the age groups (p<0.001). There was a steady increase in the burden across the age groups from 13% (18–29 years group) to 50% (50–59 years). There was significant heterogeneity among the studies reporting prevalence across all the age groups with I2>90% and p<0.001.
Gender distribution of metabolic syndrome in India
In total, 82 studies have reported prevalence of MS among female adult population while 76 studies have reported for males. The pooled prevalence of MS among adult females in India was 35% (95%CI: 31%-38%); while for males, the pooled prevalence was 26% (95%CI: 22%-29%). There was significant heterogeneity among the studies reporting prevalence in females and males (I2 = 98%, p<0.001).
Urban vs rural vs tribal
Overall, 49 studies have reported separate estimates for urban region, 34 for rural and 4 for tribal region. The pooled prevalence of MS among adult urban population in India was 32% (95%CI: 29%-36%); while in rural population, the pooled prevalence was 22% (95%CI: 20%-25%) and in tribal population, it was 28% (95%CI: 21%-36%). Significant heterogeneity was found among the studies reporting prevalence across urban, rural and tribal regions (p<0.001).
Study setting (community vs facility vs workplace)
Subgroup analysis based on study setting showed that the facility-based studies showed higher prevalence (38%; 95%CI: 30%-47%) followed by community based (29%; 95%CI: 26%-32%) and workplace-based studies (28% 95%CI: 22%-35%). However, this difference was not statistically significant (p = 0.08). There was significant heterogeneity among the studies reporting prevalence of MS irrespective of the study setting (p<0.001).
Geographical regions
North India. In total, 31 studies reporting the burden of MS were from Northern region. The pooled prevalence of MS in North India was 30% (95%CI: 25%-35%). There was a significant heterogeneity found among the studies conducted in North India (I2 = 99.2%; p<0.001). Among the 31 studies, 15 reported separate estimates for urban and 10 for rural regions. Prevalence of MS in urban North India was 35% (95%CI: 27%-44%; I2 = 99.3%; p<0.001) while for rural North India, the pooled prevalence was 21% (95%CI: 15%-27%; I2 = 97.4%, p<0.001). We also checked for gender wise distribution of MS in North India. The prevalence of MS among adult females in North India was 33% (95%CI: 26%-40%; I2 = 98.9%, p<0.001); while for adult male population, it was 26% (95%CI: 20%-34%; I2 = 99%, p<0.001) (S1 Fig).
Central India. Ten studies have reported prevalence of MS in Central India. The pooled estimate for prevalence of MS in Central India was 27% (95%CI: 17%-39%; I2 = 98.4%, p<0.001). Only one study was conducted in urban community of Central India. It reported a prevalence of 25% with 95%CI: 18%-33%. Three studies were conducted in the rural community of Central India, with which we found a pooled prevalence of 14% with 95%CI: 9%-20%. Gender wise distribution showed that the prevalence of MS was higher among adult females in Central India (30%; 95%CI: 17%-46%; I2 = 97.3%, p<0.001) when compared to males (21%; 95%CI: 12%-33%; I2 = 97.2%, p<0.001) (S2 Fig).
Western India. In total, 7 studies from Western India were included in our review. The pooled prevalence of MS in Western India was 30% (95%CI: 19%-44%; I2 = 99%, p<0.001). There was a significant urban-rural difference in the prevalence of MS in Western India. The prevalence of MS in urban Western India was 37% (95%CI: 21%-55%, I2 = 98.1%, p<0.001); while in rural Western India, it was 13% (95%CI: 12%-15%). Gender wise distribution of MS showed that the prevalence was higher among females (32%; 95%CI: 15%-51%; I2 = 98.3%, p<0.001) when compared to males (25%; 95%CI: 14%-35%; I2 = 95%, p<0.001) (S3 Fig).
Eastern India. Eleven studies have reported the prevalence of MS in Eastern India. The pooled prevalence of MS in Eastern India was 33% (95%CI: 23%-43%; I2 = 99.1%, p<0.001). The prevalence was higher among urban Eastern India (38%; 95%CI: 31%-45%; I2 = 90.3%, p<0.001) when compared to rural Eastern India (29%; 95%CI: 18%-40%; I2 = 98.5%, p<0.001). Gender distribution of MS showed that the burden was higher among the females (39%; 95%CI: 27%-53%; I2 = 98.8%, p<0.001) when compared to males (23%; 95%CI: 12%-36%, I2 = 98.5%, p<0.001) (S4 Fig).
Southern India. In total, 46 studies reporting the burden of MS were from Southern region. The pooled prevalence of MS in South India was 30% (95%CI: 26%-33%). There was a significant heterogeneity found among the studies conducted in South India (I2 = 98.6%; p<0.001). Prevalence of MS in urban South India was 30% (95%CI: 25%-34%; I2 = 98.1%; p<0.001) while for rural South India, the pooled prevalence was 25% (95%CI: 20%-30%; I2 = 97.9%, p<0.001). Gender wise prevalence of MS in South India was also checked. The prevalence of MS among adult females in South India was 34% (95%CI: 28%-40%; I2 = 98.1%, p<0.001); while for adult male population, it was 26% (95%CI: 21%-31%; I2 = 97.9%, p<0.001) (S5 Fig).
Northeast India. Only 4 studies were conducted in Northeast India to determine the prevalence of MS. The pooled prevalence of MS in Northeast India was 35% (95%CI: 25%-46%). There was a significant heterogeneity found among the studies conducted in South India (I2 = 96.9%; p<0.001) (S6 Fig). There was no sufficient number of studies to see the urban-rural and gender-based differences in the burden of MS.
Additional subgroup analysis and sensitivity analysis
Subgroup analysis based on diagnostic criteria revealed a statistically significant difference in the pooled estimate between NCEP ATP-III and IDF criteria (29% vs 34%; p = 0.05). However, we did not see any statistically significant difference in the burden of MS based on year of publication, difference in measurement of waist circumference, quality of studies or representativeness of sample.
We performed sensitivity analysis by excluding the studies conducted exclusively on elderly (≥60 years), studies having high risk of bias or not conducted on a representative sample, and studies conducted before 2007. This is to provide robust and latest estimate on the burden of MS among adult population in India. In total, 47 out of the 111 studies satisfied these criteria and included in the sensitivity analysis. The pooled prevalence of MS obtained in sensitivity analysis was still almost similar to the overall findings (29%; 95%CI: 25%-33%) indicating that the estimate is robust to the changes in age group, year, and quality of studies.
Meta-regression
First, we conducted univariate meta-regression with individual study level factors such as study setting, geographical region, diagnostic criteria, year of publication, mean age, representativeness of the sample and quality of studies (Table 3). We found significant association with mean age and study setting. However, we performed multivariable meta-regression with factors having p value less than 0.2 such as study setting, mean age, and diagnostic criteria used. The adjusted model was able to explain 24.5% of the between-study variability and the model was statistically significant (p = 0.004).
Table 3. Univariate and multivariate meta-regression performed to explore the heterogeneity between the studies (N = 113).
| Characteristics | Unadjusted Co-efficient | Unadjusted p-Value | Adjusted Co-efficient | Adjusted p-value |
|---|---|---|---|---|
| Mean age | 0.0069 | 0.002 | 0.0068 | 0.002 |
| Study setting | ||||
| Community | Ref | - | Ref | - |
| Facility | 0.10 | 0.006 | 0.10 | 0.04 |
| Workplace | -0.004 | 0.93 | 0.04 | 0.49 |
| Diagnostic criteria | ||||
| IDF | Ref | - | Ref | - |
| NCEP-ATP | -0.05 | 0.10 | -0.07 | 0.11 |
| Year of publication | {Not included in the multivariate model} | |||
| 2003–2006 | Ref | - | ||
| 2007–2010 | 0.02 | 0.75 | ||
| 2011–2014 | -0.01 | 0.82 | ||
| 2015–2019 | 0.02 | 0.75 | ||
| Geographical region | ||||
| North | Ref | - | ||
| South | 0.05 | 0.41 | ||
| East | 0.02 | 0.61 | ||
| West | 0.07 | 0.40 | ||
| Central | 0.02 | 0.63 | ||
| Northeast | 0.03 | 0.69 | ||
| Representativeness of the sample | ||||
| Representative | Ref | - | ||
| Non-representative | 0.03 | 0.34 | ||
| Quality of studies | ||||
| Low risk | Ref | - | ||
| High risk | -0.02 | 0.46 | ||
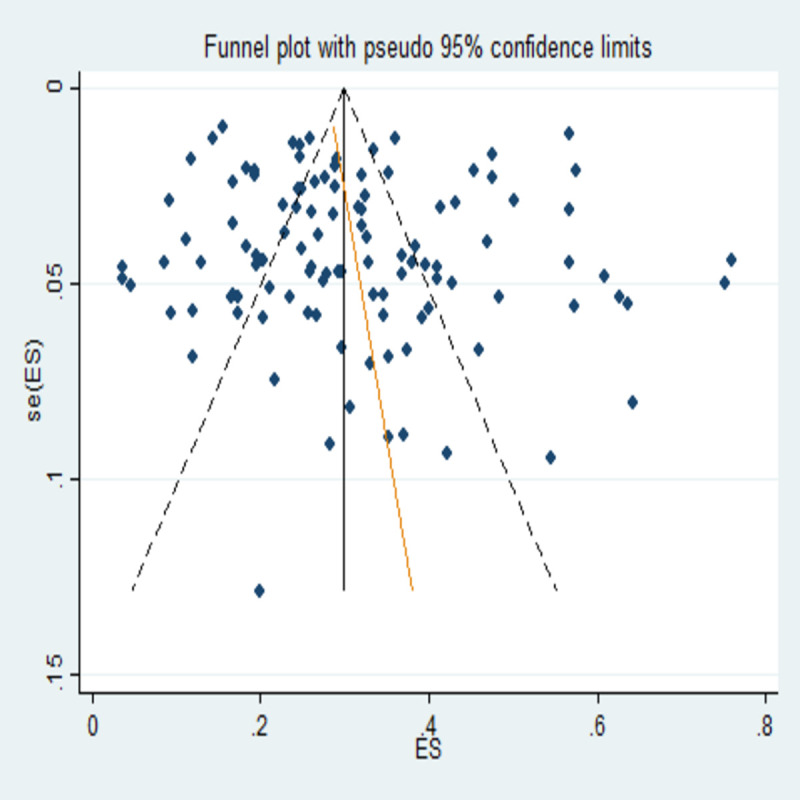
Publication bias
Egger’s test was performed for the assessment of publication bias. There were no small study effects with non-significant coefficient value (Co-efficient: 0.78; 95%CI: -0.95 to 2.52; p = 0.372) which shows lack of evidence of publication bias. Graphical representation of the test of publication bias was depicted through funnel plot in Fig 3. Funnel plot also showed symmetric plot indicating the absence of publication bias.
Fig 3. Funnel plot checking the publication bias in the current review.
Discussion
We have conducted this review to obtain a comprehensive estimate of burden of MS among adult population in India. We have also captured the gender distribution, urban-rural-tribal differences and geographical region wise estimates to find any significant difference in the estimates of MS. In total, we analysed data from 111 studies with 133,926 participants. Majority of the studies were conducted in Southern states followed by Northern states. Majority (83) were from community-based studies. Out of these, 49 have reported separate estimates for urban region, 34 for rural and 4 for tribal region. Majority of the included studies (76 out of 111) had low risk of bias.
The prevalence of MS among adult population in India was 30% (95%CI: 28%-33%). Similar reviews published from other low middle income countries in Middle East, South East Asia and Latin American region also reported that almost one third of general population have MS [128–130]. This recent upsurge in the prevalence of MS among low middle income countries including India might be directly linked with rapid economic development and urbanization in the country. This rapid industrialization can influence drastic changes in lifestyle patterns and nutrition [131–133].
We also found that people living in urban areas (32%; 95%CI: 29%-36%) were found to have higher prevalence of MS when compared to people living in tribal (28%; 95%CI: 21%-36%) or rural areas (22%; 95%CI: 20%-25%). These findings were in line with the studies conducted in neighbouring low middle-income countries [129]. Unhealthy lifestyles, better socio-economic status, decreased physical activity, stress, excessive salt and red meat consumption might be the contributory factors influencing the higher prevalence of MS in urban areas [134].
Age wise distribution showed that there is a steady rise in the burden of MS with increase in age groups and it differed significantly (p<0.001). Gender distribution of MS showed that the females had higher prevalence (35%; 95%CI: 31%-38%) when compared to males 26% (95%CI: 22%-29%). Similar reviews in Eastern Mediterranean [135], South East Asian [136], and Western pacific [137] regions abide by our findings. Major reason for this finding could be the gender specific risk factors such as menopause, polycystic ovarian syndrome and use of hormonal contraceptives among women [138]. Other probable reasons could be the excess risk women carries in terms of elevated body weight, increased waist girth, and low high density lipoprotein cholesterol when compared to men [139–142].
Highest prevalence of MS was reported in Madhya Pradesh (50%) followed by New Delhi (43%), Orissa (43%) and Telangana (42%). Stratified analysis across the geographical regions showed that people living in Northeast India (35%) have highest prevalence of MS followed by Eastern India (33%), regions with unique lifestyle and culture [142]. This highlights the need of understanding the influence of sociocultural, ethno-geographical factors in determining the risk of MS. This high prevalence among the north eastern states could also be due to lesser number of studies (n = 4) from the region. Hence, the current review may not be representative of the entire north eastern population. Further studies should be carried out in this region to have conclusive evidence on the burden of MS.
The major strength of the study is that we have tried to provide the first comprehensive review on burden of MS among adult general population in India. We also provided estimates based on gender, study setting, community and geographical regions. Test for publication bias have found that there was no significant bias in the current review. However, our review has certain limitations. Summarizing and concluding the burden of MS as 30% among adults in India with demographic and socio-economic differences is difficult because of the inherent heterogeneity. We have tried to overcome this limitation by conducting subgroup analysis based on study setting, geographical regions and provided individual prevalence estimates. The chi square test for heterogeneity also revealed significant variability across the national and region wise included studies. Hence, we tried to explain the between-study variability using meta-regression and found the potential sources of heterogeneity.
In spite of these limitations, current review provides important baseline information on the burden of MS among adult population in India. Our review has showed a higher prevalence among women, people living in urban areas and in specific geographical pockets. The findings of our review highlight that MS is a major public health problem in India. It is necessary for the government to allocate adequate resources and establish appropriate cost-effective interventions to tackle the burden of MS. Development and implementation of policies and protocols for the screening (focusing on population level screening strategies) would enable us in early diagnosis and treatment. Special focus should be given towards the vulnerable and high-risk groups. A wholesome comprehensive health care approach encompassing various levels of health care is necessary to achieve better management of MS.
This crucial step would not only enable us to reduce the mortality imposed by its individual components but also to curtail the out-of-pocket expenditure incurred by these conditions. Further comprehensive meta-analysis on population-based studies is necessary to find the factors responsible for MS which will help the policy makers, especially in the low and low middle-income regions to devise region specific interventions.
Supporting information
(DOC)
Forest plot showing the setting wise and gender wise distribution of metabolic syndrome in North India a) North India–Male b) North India–Female c) North India–Urban d) North India–Rural.
(TIFF)
Forest plot showing the setting wise and gender wise distribution of metabolic syndrome in Central India a) Central India–Male b) Central India–Female c) Central India–Rural.
(TIFF)
Forest plot showing the setting wise and gender wise distribution of metabolic syndrome in Western India a) Western India–Male b) Western India–Female c) Western India–Urban d) Western India–Rural.
(TIFF)
Forest plot showing the setting wise and gender wise distribution of metabolic syndrome in Eastern India a) Eastern India–Male b) Eastern India–Female c) Eastern India–Urban d) Eastern India–Rural.
(TIFF)
Forest plot showing the setting wise and gender wise distribution of metabolic syndrome in South India a) South India–Male b) South India–Female c) South India–Urban d) South India–Rural.
(TIFF)
Forest plot showing the setting wise and gender wise distribution of metabolic syndrome in Northeast India a) Northeast India–Male b) Northeast India–Female.
(TIFF)
(PDF)
(DTA)
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
The authors received no specific funding for this work.
References
- 1.Boutayeb A. The double burden of communicable and non-communicable diseases in developing countries. Trans R Soc Trop Med Hyg. 2006;100(3):191–9. 10.1016/j.trstmh.2005.07.021 [DOI] [PubMed] [Google Scholar]
- 2.GBD Compare | IHME Viz Hub [Internet]. [cited 2019 Aug 28]. Available from: http://vizhub.healthdata.org/gbd-compare
- 3.A comprehensive review on metabolic syndrome.—PubMed—NCBI [Internet]. [cited 2019 Oct 22]. Available from: https://www.ncbi.nlm.nih.gov/pubmed/24711954
- 4.The National Cholesterol Education Program Adult Treatment Panel III Guidelines [Internet]. [cited 2019 Oct 22]. Available from: https://www.jmcp.org/doi/pdf/10.18553/jmcp.2003.9.s1.2
- 5.Consensus statements [Internet]. [cited 2019 Oct 22]. Available from: https://www.idf.org/e-library/consensus-statements/60-idfconsensus-worldwide-definitionof-the-metabolic-syndrome.html
- 6.Type 2 diabetes and cardiovascular disease: Have all risk factors the same strength? [Internet]. [cited 2019 Oct 22]. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4127581/
- 7.Bloom D.E., Cafiero-Fonseca E.T., Candeias V, Adashi E., Bloom L., Gurfein L., et al. Economics of Non-Communicable Diseases in India: The Costs and Returns on Investment of Interventions to Promote Healthy Living and Prevent, Treat, and Manage NCDs. World Economic Forum, Harvard School of Public Health, 2014. [Google Scholar]
- 8.Davina JJ, Priyadarssini M, Rajappa M, Parameswaran S, Sahoo J, Mohan Raj PS, et al. Assessment of bone turnover markers to predict mineral and bone disorder in men with pre-dialysis non-diabetic chronic kidney disease. Clin Chim Acta. 2017; 469:195–200. 10.1016/j.cca.2017.04.010 [DOI] [PubMed] [Google Scholar]
- 9.Kulkarni V, Kanchan T, Palanivel C, Papanna MK, Kumar N, Unnikrishnan B. Awareness and practice of road safety measures among undergraduate medical students in a South Indian state. J Forensic Leg Med. 2013; 20(4):226–9. 10.1016/j.jflm.2012.09.022 [DOI] [PubMed] [Google Scholar]
- 10.Mendis S, World Health Organization. Global status report on noncommunicable diseases 2014. 2014. [DOI] [PubMed] [Google Scholar]
- 11.Upadhyay RP, Misra P, Chellaiyan VG, Das TK, Adhikary M, Chinnakali P, et al. Burden of diabetes mellitus and prediabetes in tribal population of India: A systematic review. Diabetes Res Clin Pract. 2013; 102(1):1–7. 10.1016/j.diabres.2013.06.011 [DOI] [PubMed] [Google Scholar]
- 12.World Health Organization. Global action plan for the prevention and control of noncommunicable diseases: 2013–2020. [Internet]. 2013. [cited 2019 Oct 22]. Available from: http://apps.who.int/iris/bitstream/10665/94384/1/9789241506236_eng.pdf 10.1016/j.pcad.2013.09.001 [DOI] [PubMed] [Google Scholar]
- 13.Peterson J, Welch V, Losos M, Tugwell P. The Newcastle-Ottawa scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Ottawa: Ottawa Hospital Research Institute; 2011. [Google Scholar]
- 14.Nyaga VN, Arbyn M, Aerts M. Metaprop: a Stata command to perform meta-analysis of binomial data. Arch Public Health. 2014; 72(1):39 10.1186/2049-3258-72-39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Higgins JP, Green S, editors. Cochrane handbook for systematic reviews of interventions. John Wiley & Sons; 2011. [Google Scholar]
- 16.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997; 315:629–634 10.1136/bmj.315.7109.629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Misra P, Upadhyay RP, Krishnan A, Vikram NK, Sinha S. A Community-Based Study of Metabolic Syndrome and Its Components Among Women of Rural Community in Ballabgarh, Haryana. Metab Syndr Relat Disord. 2011. December;9(6):461–7 10.1089/met.2011.0033 [DOI] [PubMed] [Google Scholar]
- 18.Bhat R, Wani Z. A Cross-Sectional Analysis of Metabolic Syndrome Factors in North Indian Adult Population of Kashmir. Sub Saharan Africa J Med. 2014;1(2):95. [Google Scholar]
- 19.Mohan V, Sandeep S, Deepa M, Gokulakrishnan K, Datta M, Deepa R. A diabetes risk score helps identify metabolic syndrome and cardiovascular risk in Indians? the Chennai Urban Rural Epidemiology Study (CURES-38). Diabetes Obes Metab. 2007. May;9(3):337–43. 10.1111/j.1463-1326.2006.00612.x [DOI] [PubMed] [Google Scholar]
- 20.Kandpal V, Sachdeva MP, Saraswathy KN. An assessment study of CVD related risk factors in a tribal population of India. BMC Public Health. 2016; 16:434 10.1186/s12889-016-3106-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kaur J. Assessment and Screening of the Risk Factors in Metabolic Syndrome. Med Sci. 2014; 2(3):140–52. [Google Scholar]
- 22.Pathak R, Agarwalla R, Pathania D. Assessment of metabolic syndrome and health related quality of life in community dwellers: A cross sectional study from North India. Indian J Med Spec. 2018; 9(1):15–9. [Google Scholar]
- 23.Bal SS, Khurana D, Sharma A, Lal V, Bhansali A, Prabhakar S. Association of metabolic syndrome with carotid atherosclerosis in the young North Indian population. Diabetes Metab Syndr: Clin Res Rev. 2011; 5(3):153–7. [DOI] [PubMed] [Google Scholar]
- 24.Bansal S, Paliwal A, Verma V, Chauhan J. A study on prevalence of metabolic syndrome in general population in Western Uttar Pradesh, India. Int J Res Med Sci. 2017; 5(6):2641. [Google Scholar]
- 25.Bhattacharyya A, Sinha N. Attributes of metabolic syndrome in geriatric institutional residents in Secunderabad, India. Int J Res Med Sci. 2016; 398–402. [Google Scholar]
- 26.Bandela PV, Dongre NN, Ambekar JG, Prasad KD, Devaranavadagi BB. Study of Metabolic Syndrome and Its Components Among Kurnool District Population of Andhra Pradesh with Different Ethnic Backgrounds. J Cardiovasc Dis Res. 2017; 8(3):83–88. [Google Scholar]
- 27.Bansal M, Shrivastava S, Mehrotra R, Agarwal V, Kasliwal RR. Low Framingham risk score despite high prevalence of metabolic syndrome in asymptomatic North-Indian population. JAPI. 2009; 57:17–22 [PubMed] [Google Scholar]
- 28.Basha DA, Reddy KS, Naik JL. Association between physical activity and metabolic syndrome in an urban adult population of Chittoor District, Andhra Pradesh. Indian J Health Wellbeing. 2018; 9(2). [Google Scholar]
- 29.Bhagat A, Malhotra AS, Kaur G, Kapoor N. Metabolic Syndrome: Not Even the Urban Indian Youth is Spared. Indian J Physiol Pharmacol. 2017; 61(4):368–77. [Google Scholar]
- 30.Dhabriya R, Agrawal M, Gupta R, Mohan I, Sharma KK. Cardiometabolic risk factors in the Agarwal business community in India: Jaipur Heart Watch-6. Indian Heart J. 2015; 67(4):347–50. 10.1016/j.ihj.2015.03.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chakraborty SN, Roy SK, Rahaman MA. Epidemiological predictors of metabolic syndrome in urban West Bengal, India. J Family Med Prim Care. 2015; 4(4):535 10.4103/2249-4863.174279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chhabra N, Sodhi K, Kukreja S, Chhabra S, S V, Chhabra S, et al. Central obesity and prevalence of metabolic syndrome in post-menopausal women. Central Obes. 2014; 5(1):WMC004532 [Google Scholar]
- 33.Kaushal S, Gupta V, Prakash G, Misra S. Correlates of metabolic syndrome and prevalence among urban population of Agra, Uttar Pradesh, India. Int J Community Med Public Health. 2016;3570–5. [Google Scholar]
- 34.Das M, Pal S, Ghosh A. Prevalence of the metabolic syndrome in people of Asian Indian origin: outcomes by definitions: cardiovascular topics. Cardiovasc J Africa. 2011; 22(6):303–5. [DOI] [PubMed] [Google Scholar]
- 35.Mahanta TG, Joshi R, Mahanta B, Gogoi P. Determinants of metabolic syndrome (MetS) amongst persons living in Dibrugarh District of Assam. Clin Epidemiol Glob Health. 2017; 5(2):52–61. [Google Scholar]
- 36.Prabhakaran D, Chaturvedi V, Shah P, Manhapra A, Jeemon P, Shah B, et al. Differences in the prevalence of metabolic syndrome in urban and rural India: a problem of urbanization. Chronic Illness. 2007; 3(1):8–19. 10.1177/1742395307079197 [DOI] [PubMed] [Google Scholar]
- 37.Vijayanchali SS. Elderly: nutrition and health New Delhi: APH Pub. Corp.; 2013. [Google Scholar]
- 38.Mahajan A, Jaiswal A, Tabassum R, Podder A, Ghosh S, Madhu SV, et al. Elevated levels of C-reactive protein as a risk factor for Metabolic Syndrome in Indians. Atherosclerosis. 2012; 220(1):275–81. 10.1016/j.atherosclerosis.2011.10.031 [DOI] [PubMed] [Google Scholar]
- 39.Gupta R, Kaul V, Bhagat N, Agrawal M, Gupta VP, Misra A, et al. Trends in prevalence of coronary risk factors in an urban Indian population: Jaipur Heart Watch-4. Indian Heart J. 2007;59(4):346–53. [PubMed] [Google Scholar]
- 40.Gupta R, Deedwania PC, Achari V, Bhansali A, Gupta BK, Gupta A, et al. Normotension, prehypertension, and hypertension in urban middle-class subjects in India: prevalence, awareness, treatment, and control. Am J Hypertens. 2012; 26(1):83–94. [DOI] [PubMed] [Google Scholar]
- 41.Harikrishnan S, Sarma S, Sanjay G, Jeemon P, Krishnan MN, Venugopal K, et al. Prevalence of metabolic syndrome and its risk factors in Kerala, South India: Analysis of a community based cross-sectional study. PLoS ONE. 2018; 13(3): e0192372 10.1371/journal.pone.0192372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Deedwania PC, Gupta R, Sharma KK, Achari V, Gupta B, Maheshwari A, et al. High prevalence of metabolic syndrome among urban subjects in India: A multisite study. Diabetes Metab Syndr Clin Res Rev. 2014; 8(3):156–61. [DOI] [PubMed] [Google Scholar]
- 43.Mahadik SR, Deo SS, Mehtalia SD. Increased Prevalence of Metabolic Syndrome in Non-Obese Asian Indian—An Urban-Rural Comparison. Metab Syndr Relat Disord. 2007; 5(2):142–52. 10.1089/met.2006.0029 [DOI] [PubMed] [Google Scholar]
- 44.Nag T, Ghosh A. Indian diabetes risk score and clustering of metabolic syndrome phenotype in a rural community of Asian Indian origin. Diabetes Res Clin Pract. 2016; 112:44–9. 10.1016/j.diabres.2015.11.005 [DOI] [PubMed] [Google Scholar]
- 45.Kamble P, Deshmukh PR, Garg N. Metabolic syndrome in adult population of rural Wardha, central India. Indian J Med Res. 2010; 132(6):701. [PMC free article] [PubMed] [Google Scholar]
- 46.Kanjilal S, Shanker J, Rao VS, Khadrinarasimhaih NB, Mukherjee M, Iyengar SS, et al. Prevalence and component analysis of metabolic syndrome: an Indian atherosclerosis research study perspective. Vasc Health Risk Manag. 2008; 4(1):189 10.2147/vhrm.2008.04.01.189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kaur P, Radhakrishnan E, Rao SR, Sankarasubbaiyan S, Rao TV, Gupte MD. The metabolic syndrome and associated risk factors in an urban industrial male population in South India. J Assoc Physicians India. 2010; 58(6):363–71. [PubMed] [Google Scholar]
- 48.Latheef SA, Subramanyam G. Prevalence of coronary artery disease and coronary risk factors in an urban population of Tirupati. Indian Heart J. 2007; 59(2):157–64. [PubMed] [Google Scholar]
- 49.Madhav KP, Mallavarapu S, Baer PR. Prevalence of Metabolic Syndrome among workers of Dolomite Mine at Madharam, Khammam District Andhra Pradesh. Medica Innovatica. 2013; 2(2):40–44 [Google Scholar]
- 50.Sneha M, Arlappa N, Suryanarayana P, Balakrishna N, Santosh VS. Prevalence of Metabolic Syndrome among Urban Older Adults of Hyderabad Metropolitan City in South India. J Nutr Obes. 2017; 1(1):101 [Google Scholar]
- 51.Mangat C, Goel NK, Walia DK, Agarwal N, Sharma MK, Kaur J, et al. Metabolic syndrome: a challenging health issue in highly urbanized Union Territory of north India. Diabetol Metab Syndr. 2010; 2(1):19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Vaidya R, Pandey S, Srinivas M, Agashe S, Joshi J, Galvankar P, et al. Menopause and metabolic syndrome: A study of 498 urban women from western India. J Mid-life Health. 2010; 1(2):63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Chinawale C, Parmar D, Kavathia P, Rangnani T, Thakkar J, Kartha G. Metabolic syndrome among adults of surendranagar District of Saurashtra, Gujarat: A cross-sectional Study. Indian J Community Med. 2018; 43(1):24 10.4103/ijcm.IJCM_339_16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Barik A, Das K, Chowdhury A, Rai RK. Metabolic syndrome among rural Indian adults. Clin Nutr ESPEN. 2018; 23:129–35. 10.1016/j.clnesp.2017.11.002 [DOI] [PubMed] [Google Scholar]
- 55.M. S. Metabolic Syndrome among Urban and Rural Women Population–A Cross Sectional Study. J Clin Diag Res. 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Manjunath D, Uthappa CK, Kattula SR, Allam RR, Chava N, Oruganti G. Metabolic Syndrome Among Urban Indian Young Adults: Prevalence and Associated Risk Factors. Metab Syndr Relat Disord. 2014; 12(7):381–9. 10.1089/met.2014.0003 [DOI] [PubMed] [Google Scholar]
- 57.Ismail I, Azeez K, Antomy A, Kunnummal S. Metabolic syndrome and its associated factors among the adult population residing in Kannavam tribal area of Kannur District, Kerala. Tropical J Med Res. 2016; 19(1):36. [Google Scholar]
- 58.Bhutia RD, Singh TA, Sherpa ML, Khandelwal B. “Metabolic Syndrome and Its Risk Determinants in Sikkim”: A Glimpse from a Hospital Study. Indian J Clin Biochem. 2017; 32(4):480–6. 10.1007/s12291-017-0635-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kunti SK, Ghosh S, Samanta A, Chakraborty I. Metabolic syndrome and its socio demographic and behavioral correlates: a cross sectional study among adult patients attending medicine outpatient department in a tertiary care hospital, West Bengal. Int J Community Med Public Health. 2019; 6(4):1585. [Google Scholar]
- 60.Sharma S, Chandrashekar A, Singh V. Metabolic Syndrome in Military Aircrew Using a Candidate Definition. Aerosp Med Hum Perform. 2016; 87(9):790–4. 10.3357/AMHP.4663.2016 [DOI] [PubMed] [Google Scholar]
- 61.Parale GP, Patil VC, Patil SP, Sabale SV, Pethe CV, Manjunath GS, et al. Metabolic Syndrome in Railway Employees and its Relation to Lifestyle Factors. Metab Syndr Relat Disord. 2008; 6(1):58–63. 10.1089/met.2007.0025 [DOI] [PubMed] [Google Scholar]
- 62.Srinivasan S, Lingegowda J, Rajan C, Muddegowda P, R. R. Metabolic syndrome in rural Kerala: a hospital based study. Int J Adv Med. 2016; 898–904. [Google Scholar]
- 63.Deshmukh P, Kamble P, Goswami K, Garg N. Metabolic syndrome in the rural population of Wardha, Central India: An exploratory factor analysis. Indian J Community Med. 2013; 38(1):33 10.4103/0970-0218.106625 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Ramachandran A, Snehalatha C, Satyavani K, Sivasankari S, Vijay V. Metabolic syndrome in urban Asian Indian adults—a population study using modified ATP III criteria. Diabetes Res Clin Prac. 2003; 60(3):199–204. [DOI] [PubMed] [Google Scholar]
- 65.Thomas V. Metabolic Syndrome (Ms) among Adults in Urban Slums–A Cross Sectional Study in Hyderabad, Andhra Pradesh, India. J Community Med Health Educ. 2012; 02(11). [Google Scholar]
- 66.Pai NN, Meenakshi G. Metabolic syndrome risk assessment among adults in Udupi District, Karnataka. Clin Epidemiol Glob Health. 2020; 8:142–8 [Google Scholar]
- 67.Gupta R, Deedwania PC, Achari V, Bhansali A, Gupta BK, Gupta A, et al. Normotension, Prehypertension, and Hypertension in Urban Middle-Class Subjects in India: Prevalence, Awareness, Treatment, and Control. Am J Hypertens. 2013; 26(1):83–94. 10.1093/ajh/hps013 [DOI] [PubMed] [Google Scholar]
- 68.Mini GK, Sarma PS, Thankappan KR. Overweight, the major determinant of metabolic syndrome among industrial workers in Kerala, India: Results of a cross-sectional study. Diabetes Metab Syndr: Clin Res Rev. 2019; 13(5):3025–30. [DOI] [PubMed] [Google Scholar]
- 69.Patel NR, Patel HL, Gunjalia AP. Prevalence of metabolic syndrome in higher socioeconomic class of Ahmedabad, Gujarat, India. Int J Med Sci Public Health. 2016; 5(1):35–40. [Google Scholar]
- 70.Pemminati S, Adhikari PM, Pathak R, Pai MR. Prevalence of metabolic syndrome (METS) using IDF 2005 guidelines in a semi urban south Indian (Boloor Diabetes Study) population of Mangalore. J Assoc Physicians India. 2010; 58:674–7. [PubMed] [Google Scholar]
- 71.Prabhakaran D, Shah P, Chaturvedi V, Ramakrishnan L, Manhapra A, Reddy KS. Cardiovascular risk factor prevalence among men in a large industry of northern India. Natl Med J India. 2005; 18(2):59 [PubMed] [Google Scholar]
- 72.Pradeepa R, Surendar J, Indulekha K, Chella S, Anjana RM, Mohan V. Prevalence of metabolic syndrome and its association with coronary artery disease among an urban elderly south Indian population (CURES-145). J Assoc Physicians India. 2016; 64(5):20–5. [PubMed] [Google Scholar]
- 73.Prakash A, Prakash J. Metabolic Syndrome and its components: a hospital-based study from north India. Indian J Med Spec. 2013; 4:1. [Google Scholar]
- 74.Sachdev HPS, Osmond C, Fall CHD, Lakshmy R, Ramji S, Dey Biswas SK, et al. Predicting adult metabolic syndrome from childhood body mass index: follow-up of the New Delhi birth cohort. Arch Dis Child. 2009; 94(10):768–74. 10.1136/adc.2008.140905 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Bansal A, Joshi PC. Predictor of Metabolic Syndrome: A community study from Urban Delhi, India. Int J Human Sci. 2015; 12(1):1451. [Google Scholar]
- 76.Srimani S, Saha I, Chaudhuri D. Prevalence and association of metabolic syndrome and vitamin D deficiency among postmenopausal women in a rural block of West Bengal, India. Slominski AT, editor. PLOS ONE. 2017; 12(11):e0188331 10.1371/journal.pone.0188331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Jain J, Rao T. Prevalence and Correlates of Metabolic Syndrome in Young Population: A Cross Sectional Study. J Diabetes Metab. 2016; 6:3 [Google Scholar]
- 78.Das TP, Sen M, Saha I, Chaudhuri D. Prevalence and Gender Differentials of Metabolic Syndrome Among College Students of Kolkata, West Bengal, India. Int J Cur Res Rev| Vol. 2017; 9(14):14. [Google Scholar]
- 79.Prasad DS, Kabir Z, Dash AK, Das BC. Prevalence and risk factors for metabolic syndrome in Asian Indians: A community study from urban Eastern India. J Cardiovasc Dis Res. 2012; 3(3):204–11. 10.4103/0975-3583.98895 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Naik J, Reddy K, Reddy B, Basha D. Prevalence and risk factors for metabolic syndrome in urban elderly: a community study from Tirupati, Chittoor district, Andhra Pradesh, India. Int J Community Med Public Health. 2016; 2106–11. [Google Scholar]
- 81.Ravikiran M, Bhansali A, RaviKumar P, Bhansali S, Dutta P, Thakur JS, et al. Prevalence and risk factors of metabolic syndrome among Asian Indians: A community survey. Diabetes Res Clin Pract. 2010; 89(2):181–8. 10.1016/j.diabres.2010.03.010 [DOI] [PubMed] [Google Scholar]
- 82.Srimani S, Das P, Chaudhuri D. Prevalence of Anaemia and Metabolic Syndrome and their Relationship among Postmenopausal Women in Rural West Bengal, India. J Clin Diag Res. 2018; 12(3):LC22–5 [Google Scholar]
- 83.Das M, Pal S, Ghosh A. Prevalence of Cardiovascular Disease Risk Factors by Habitat: A Study on Adult Asian Indians in West Bengal, India. Anthropologischer Anzeiger. 2011; 68(3):253–64. [DOI] [PubMed] [Google Scholar]
- 84.Tandon V, Mahajan A, Sharma S, Sharma A. Prevalence of cardiovascular risk factors in postmenopausal women: A rural study. J Mid-life Health. 2010; 1(1):26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Vatakencherry RM, Saraswathy L. Prevalence of Metabolic syndrome among adults in a teaching hospital in Kochi, Central Kerala: A cross-sectional study. J Family Med Prim Care. 2019; 8(6):2079 10.4103/jfmpc.jfmpc_241_19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.K. J, Ebenezer ED, Londhe V, Paul TV, Yadav B, Kekre AN. Prevalence of metabolic syndrome among postmenopausal women in South India. Int J Reprod Contracept Obstet Gynecol. 2018; 7(6):2364. [Google Scholar]
- 87.Selvaraj I, Gopalakrishnan S, Logaraj M. Prevalence of metabolic syndrome among rural women in a primary health centre area in Tamil Nadu. Indian J Public Health. 2012; 56(4):314 10.4103/0019-557X.106423 [DOI] [PubMed] [Google Scholar]
- 88.Kapil U, Khandelwal R, Ramakrishnan L, Khenduja P, Gupta A, Sareen N, et al. Prevalence of metabolic syndrome and associated risk factors among geriatric population living in a high altitude region of rural Uttarakhand, India. J Family Med Prim Care. 2018;7(4):709 10.4103/jfmpc.jfmpc_261_17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Khan Y, Lalchandani A, Gupta A, Khadanga S, Kumar S. Prevalence of metabolic syndrome crossing 40% in Northern India: Time to act fast before it runs out of proportions. J Family Med Prim Care. 2018; 7(1):118 10.4103/jfmpc.jfmpc_10_17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Gupta R, Deedwania PC, Gupta A, Rastogi S, Panwar RB, Kothari K. Prevalence of metabolic syndrome in an Indian urban population. Int J Cardiol. 2004; 97(2):257–61. 10.1016/j.ijcard.2003.11.003 [DOI] [PubMed] [Google Scholar]
- 91.Zafar KS, Pious T, Singh PS, Gautam RK, Yadav SK, Singh P, et al. Prevalence of metabolic syndrome in a rural population- a cross sectional study from Western Uttar Pradesh, India. Int J Res Med Sci. 2017; 5(5):2223. [Google Scholar]
- 92.Subramani SK, Mahajan S, Chauhan P, Yadav D, Mishra M, Pakkirisamy U, et al. Prevalence of metabolic syndrome in Gwalior region of Central India: A comparative study using NCEP ATP III, IDF and Harmonized criteria. Diabetes Metab Syndr Clin Res Rev. 2019; 13(1):816–21. [DOI] [PubMed] [Google Scholar]
- 93.Bhat R, Zargar A, Laway B. Prevalence of metabolic syndrome in Kashmir valley of Indian subcontinent. Indian J Med Sci. 2010;64(6):259 10.4103/0019-5359.99599 [DOI] [PubMed] [Google Scholar]
- 94.Madan J, Narsaria A. Prevalence of metabolic syndrome in Mumbai City, India. J Obes Metab Res. 2016; 3(1):16. [Google Scholar]
- 95.Sharma S, Aggarwal N, Joshi B, Suri V, Badada S. Prevalence of metabolic syndrome in pre- and post-menopausal women: A prospective study from apex institute of North India. J Mid-life Health. 2016; 7(4):169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Sawant A, Mankeshwar R, Shah S, Raghavan R, Dhongde G, Raje H, et al. Prevalence of Metabolic Syndrome in Urban India. Cholesterol. 2011; 2011:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Kotokey RK, Kalita D, Agarwala R, Purkayastha S. Prevalence of Metabolic Syndrome in urban population of Dibrugarh town of upper Assam. J Indian College Cardiol. 2013; 3(2):52–6. [Google Scholar]
- 98.Deepa M, Farooq S, Datta M, Deepa R, Mohan V. Prevalence of metabolic syndrome using WHO, ATPIII and IDF definitions in Asian Indians: the Chennai Urban Rural Epidemiology Study (CURES-34). Diabetes/Metab Res Rev. 2007; 23(2):127–34. [DOI] [PubMed] [Google Scholar]
- 99.Mahanta TG, Joshi R, Mahanta BN, Xavier D. Prevalence of modifiable cardiovascular risk factors among tea garden and general population in Dibrugarh, Assam, India. J Epidemiol Glob Health. 2013; 3(3):147–56. 10.1016/j.jegh.2013.04.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Mohan V, Farooq S, Deepa M, Ravikumar R, Pitchumoni CS. Prevalence of non-alcoholic fatty liver disease in urban south Indians in relation to different grades of glucose intolerance and metabolic syndrome. Diabetes Res Clin Pract. 2009; 84(1):84–91. 10.1016/j.diabres.2008.11.039 [DOI] [PubMed] [Google Scholar]
- 101.Kempegowda P, Marcus SR, Solanki P, Reddy RS, D. R. N, Dharmalingam M. Prevalence of the metabolic syndrome in rural India—a disparity in definitions. Int J Diabetes Dev Ctries. 2011; 31(4):188–93. [Google Scholar]
- 102.Rajput R, Rajput M, Bairwa M, Singh J, Saini O, Shankar V. Waist height ratio: A universal screening tool for prediction of metabolic syndrome in urban and rural population of Haryana. Indian J Endocrinol Metab. 2014; 18(3):394 10.4103/2230-8210.131201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Ramachandran A, Snehalatha C, Yamuna A, Murugesan N. High prevalence of cardiometabolic risk factors among young physicians in India. JAPI. 2008; 56:17–20. [PubMed] [Google Scholar]
- 104.Randhawa Ramanpreet and Sidhu Sharda. Prevalence of Metabolic Syndrome in rural premenopausal and postmenopausal females of Amritsar (Punjab) using three international definitions: ATP-III, IDF and mATP-III. J Exerc Sci Physio. 2015; 11(1):29–41 [Google Scholar]
- 105.Roopa M, Deepa M, Indulekha K, Mohan V. Prevalence of Sleep Abnormalities and Their Association with Metabolic Syndrome among Asian Indians: Chennai Urban Rural Epidemiology Study (CURES− 67). J Diabetes Sci Technol. 2010; 4(6):1524–31. 10.1177/193229681000400630 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Sarkar P, Mahadeva SK, Raghunath H, Upadhya S, Hamsa M. Metabolic syndrome and its components among population of Holalu village, Karnataka. Int J Med Sci Public Health. 2016; 5(5):860–6. [Google Scholar]
- 107.Sarkar S, Das M, Mukhopadhyay B, Chakrabarti CS, Majumder PP. High prevalence of metabolic syndrome & its correlates in two tribal populations of India & the impact of urbanization. Indian J Med Res. 2006; 123(5):679 [PubMed] [Google Scholar]
- 108.Sarma R., Srikanth S. Prevalence of Metabolic Syndrome in Women of Different Age Groups in Rural Population of Andhra Pradesh. Int J Med Health Res. 2015; 1(1):1–6 [Google Scholar]
- 109.Selvaraj P, Muthunarayanan L. Prevalence of Metabolic Syndrome and Associated Risk Factors among Men in a Rural Health Centre Area in Tamil Nadu. J Lifestyle Med. 2019; 9(1):44 10.15280/jlm.2019.9.1.44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Sharma MK, Pandey S, Nagtilak S. Metabolic syndrome and risk of cardiovascular disease in rural and urban patients in north India. World J Pharm Res. 2018; 7(7):1309–1320 [Google Scholar]
- 111.Sharma R, Sharma R and Kumar A: Metabolic syndrome: Prevalence (IDF & NCEP-ATP III) in Udhampur, Jammu city. Int J Pharm Sci Res 2019; 10(3):1420–25. [Google Scholar]
- 112.Chow CK, Naidu S, Raju K, Raju R, Joshi R, Sullivan D, et al. Significant lipid, adiposity and metabolic abnormalities amongst 4535 Indians from a developing region of rural Andhra Pradesh. Atherosclerosis. 2008; 196(2):943–52. 10.1016/j.atherosclerosis.2007.02.027 [DOI] [PubMed] [Google Scholar]
- 113.Singh RB, Fedacko J, Saboo B, Niaz MA, Maheshwari A, Verma N, et al. Association of higher omega-6/omega-3 fatty acids in the diet with higher prevalence of metabolic syndrome in North India. MOJ Public Health. 2017; 6(6):00193. [Google Scholar]
- 114.Singh J, Rajput M, Rajput R, Bairwa M. Prevalence and predictors of metabolic syndrome in a North Indian rural population: A community based study. J Glob Diabetes Clin Metab. 2016; 5:2. [Google Scholar]
- 115.Sinha N, Bhattacharya A, Deshmukh PR, Panja TK, Yasmin S, Arlappa N. Metabolic syndrome among elderly care-home residents in southern India: a cross sectional study. WHO South East Asia J Public Health 2016; 5(1): 62–69 10.4103/2224-3151.206556 [DOI] [PubMed] [Google Scholar]
- 116.Sinha S, Misra P, Kant S, Krishnan A, Nongkynrih B, Vikram NK. Prevalence of metabolic syndrome and its selected determinants among urban adult women in South Delhi, India. Postgrad Med J. 2013; 89(1048):68–72. 10.1136/postgradmedj-2012-130851 [DOI] [PubMed] [Google Scholar]
- 117.Goyal R, Kumar A, Singhai M. Study of Metabolic Syndrome and Its Risk Components in Patients Attending Tertiary Care Center of Uttarakhand. Indian J Clin Biochem. 2014; 29(3):362–6. 10.1007/s12291-013-0366-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Tharkar S, Viswanathan V. Effect of obesity on cardiovascular risk factors in urban population in South India. Heart Asia. 2010; 2(1):145–9. 10.1136/ha.2009.000950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Tharkar S, Kumpatla S, Muthukumaran P, Viswanathan V. High prevalence of metabolic syndrome and cardiovascular risk among police personnel compared to general population in India. JAPI. 2008; 56:845 [PubMed] [Google Scholar]
- 120.Thayyil J, Jayakrishnan TT, Raja M, Cherumanalil JM. Metabolic syndrome and other cardiovascular risk factors among police officers. North Am J Med Sci. 2012; 4(12):630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Jones AD, Hayter AKM, Baker CP, Prabhakaran P, Gupta V, Kulkarni B, et al. The co-occurrence of anemia and cardiometabolic disease risk demonstrates sex-specific sociodemographic patterning in an urbanizing rural region of southern India. European J Clin Nutr. 2016; 70(3):364–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Mittal M, Gupta H D. The study of prevalence of metabolic syndrome in the first degree relatives of type 2 diabetes mellitus patients. Int J Res Med Sci. 2018; 6(9):3042. [Google Scholar]
- 123.Thiruvagounder M, Khan S, Sheriff DS. The prevalence of metabolic syndrome in a local population in India. Biochemia Medica. 2010; 20(2):249–52. [Google Scholar]
- 124.Tyagi H, Modgil V, Nath M. Metabolic Syndrome: The Prevalence of Mounting Public Health Problem in Ghaziabad, India. J Pure Applied Sci Technol. 2013; 3(2). [Google Scholar]
- 125.Lakshmipriya N, Gayathri R, Praseena K, Vijayalakshmi P, Geetha G, Sudha V, et al. Type of vegetable oils used in cooking and risk of metabolic syndrome among Asian Indians. Int J Food Sci Nutrition. 2013; 64(2):131–9. [DOI] [PubMed] [Google Scholar]
- 126.Venugopal V, Dongre AR, Saravanan S. Prevalence and determinants of metabolic syndrome among the rural adult population of Puducherry. Indian J Community Med. 2019; 44(1):21 10.4103/ijcm.IJCM_132_18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Majumdar V, Nagaraja D, Christopher R. Vitamin D status and metabolic syndrome in Asian Indians. Int J Obesity. 2011. August;35(8):1131–4. [DOI] [PubMed] [Google Scholar]
- 128.Chowdhury MZI, Anik AM, Farhana Z, Bristi PD, Abu Al Mamun BM, Uddin MJ, et al. Prevalence of metabolic syndrome in Bangladesh: a systematic review and meta-analysis of the studies. BMC Public Health. 2018; 18(1) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Li R, Li W, Lun Z, Zhang H, Sun Z, Kanu JS, et al. Prevalence of metabolic syndrome in mainland china: a meta-analysis of published studies. BMC Public Health. 2016; 16(1) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Márquez-Sandoval F, Macedo-Ojeda G, Viramontes-Hörner D, Fernández Ballart J, Salas Salvadó J, Vizmanos B. The prevalence of metabolic syndrome in Latin America: a systematic review. Public Health Nutr. 2011; 14(10):1702–13 10.1017/S1368980010003320 [DOI] [PubMed] [Google Scholar]
- 131.Popkin BM. Global nutrition dynamics: the world is shifting rapidly toward a diet linked with noncommunicable diseases. Am J Clin Nutr. 2006; 84(2):289–98 10.1093/ajcn/84.1.289 [DOI] [PubMed] [Google Scholar]
- 132.Nutrition Health Topics Introduction. World Health Organization [Internet]. [cited 2020 Aug 8]. Available from: https://www.who.int/nutrition/topics/1_introduction/en/
- 133.Kearney J. Food consumption trends and drivers. Philos Trans R Soc Lond B Biol Sci. 2010; 365(1554):2793–807. 10.1098/rstb.2010.0149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Sepp T, McGraw KJ, Kaasik A, Giraudeau M. A review of urban impacts on avian life-history evolution: Does city living lead to slower pace of life? Glob Change Biol. 2018; 24(4):1452–69 [DOI] [PubMed] [Google Scholar]
- 135.Ostovar R, Kiani F, Sayehmiri F, Yasemi M, Mohsenzadeh Y, Mohsenzadeh Y. Prevalence of metabolic syndrome in Iran: A meta-analysis. Electr Physician. 2017; 9(10):5402–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Kim Y, Je Y. Meat Consumption and Risk of Metabolic Syndrome: Results from the Korean Population and a Meta-Analysis of Observational Studies. Nutrients. 2018; 10(4):390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Xu S, Gao B, Xing Y, Ming J, Bao J, Zhang Q, et al. Gender Differences in the Prevalence and Development of Metabolic Syndrome in Chinese Population with Abdominal Obesity. Stover CM, editor. PLoS ONE. 2013; 8(10):e78270 10.1371/journal.pone.0078270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Beigh SH, Jain S. Prevalence of metabolic syndrome and gender differences. Bioinformation. 2012; 8(13):613 10.6026/97320630008613 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Bentley-Lewis R, Koruda K, Seely EW. The metabolic syndrome in women. Nature Clin Pract Endocrinol Metab. 2007; 3(10):696–704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Dallongeville J, Cottel D, Arveiler D, Tauber JP, Bingham A. et al. The association of metabolic disorders with the metabolic syndrome is different in men and women. Ann Nutr Metab. 2004; 48(1):43–50 10.1159/000075304 [DOI] [PubMed] [Google Scholar]
- 141.Jahan F, Qureshi R, Borhany T, Hamza HB. Metabolic syndrome: frequency and gender differences at an out—patient clinic. J Coll Physicians Surg Pak. 2007; 17(1):32–5. doi: 01.2007/JCPSP.3235 [PubMed] [Google Scholar]
- 142.Prasad DS, Kabir Z, Dash AK, Das BC. Prevalence and risk factors for metabolic syndrome in Asian Indians: A community study from urban Eastern India. J Cardiovasc Dis Res. 2012; 3(3):204–11 10.4103/0975-3583.98895 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOC)
Forest plot showing the setting wise and gender wise distribution of metabolic syndrome in North India a) North India–Male b) North India–Female c) North India–Urban d) North India–Rural.
(TIFF)
Forest plot showing the setting wise and gender wise distribution of metabolic syndrome in Central India a) Central India–Male b) Central India–Female c) Central India–Rural.
(TIFF)
Forest plot showing the setting wise and gender wise distribution of metabolic syndrome in Western India a) Western India–Male b) Western India–Female c) Western India–Urban d) Western India–Rural.
(TIFF)
Forest plot showing the setting wise and gender wise distribution of metabolic syndrome in Eastern India a) Eastern India–Male b) Eastern India–Female c) Eastern India–Urban d) Eastern India–Rural.
(TIFF)
Forest plot showing the setting wise and gender wise distribution of metabolic syndrome in South India a) South India–Male b) South India–Female c) South India–Urban d) South India–Rural.
(TIFF)
Forest plot showing the setting wise and gender wise distribution of metabolic syndrome in Northeast India a) Northeast India–Male b) Northeast India–Female.
(TIFF)
(PDF)
(DTA)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.