Abstract
Both ischemic heart disease (IHD) and stroke are major causes of death worldwide. We investigated the effects of combined Traditional Chinese medicine (TCM) and western medicine (WM) on stroke risk in IHD patients.
Taiwanese patients with IHD were enrolled in the TCM study during their outpatient visit. Stroke events after TCM or non-TCM treatment were examined. Chi-square tests and Student t-tests were used to examine differences between patients using and not using TCM. The Cox proportional hazards regression model was used to estimate hazard ratios (HRs). Sex, age, and comorbidities were included in a multivariable Cox model to estimate the adjusted HR (aHR). The survival probability and the probability free of stroke were calculated by the Kaplan–Meier method.
There were 733 IHD patients using TCM and 733 using non-TCM treatment, with the same proportion of sex and age within each cohort. Using single Chinese herb such as Dan Shen, San Qi, or Chuan Xiong would have lower stroke events and lower aHR than non-TCM in IHD patients. There was 0.3-fold lower stroke risk in IHD patients with combination TCM and non-TCM treatment (95% CI = 0.11–0.84, P = .02). Moreover, the survival rate was higher (P < .001) and the incidence of hemorrhagic stroke was significantly lower (P = .04) in IHD patients with TCM treatment.
IHD patients using combined TCM and WM had a higher survival rate and lower risk of new onset stroke, especially hemorrhagic stroke than those who did not use TCM treatment.
Keywords: combined medicine, ischemic heart disease, stroke, traditional Chinese medicine
1. Introduction
Traditional Chinese medicine (TCM) has been treating cardiovascular disease in the Chinese communities for more than 3000 years. Ischemic heart disease (IHD), is also called coronary artery disease, is strongly related to stroke; both stroke and IHD are major causes of death worldwide.[1] However, in several East Asian countries, stroke is more prominent than IHD. East Asian countries have higher mortality rates and incidence rates for stroke, especially hemorrhagic stroke, than do Western counties,[2] likely due to a higher prevalence of hypertension and lower serum total cholesterol levels in Asian countries than in Western countries,[2]
Besides IHD, other comorbidities such as diabetes mellitus (DM), hypertension, hyperlipidemia, and chronic obstructive pulmonary disease (COPD) are also related to stroke. Those comorbidities may affect the prognosis of patients with IHD.
1.1. Diabetes mellitus and stroke
Early onset type 2 DM is associated with a markedly elevated risk of cardiovascular disease,[3] thus increasing the risk of stroke. Individuals with DM have a 2- to 4-fold increase in IHD risk and higher mortality rates than those without DM.[4,5] Furthermore, patients with DM but without a previous myocardial infarction (MI) have a risk of MI as high as patients without DM who have previously had a MI.[6] Further, while intracerebral hemorrhage is most often related to hypertension, patients with DM are more prone to deep subcortical intracerebral hemorrhage.[5] A large scale meta-analysis project, the Asia Pacific Cohort Studies Collaboration, shows that the hazard ratios (HRs) of DM for ischemic stroke and IHD are similar for both Asian and Western countries.[7]
1.2. Hypertension and stroke
Apparent treatment-resistant hypertension is associated with an increased risk for coronary heart disease and all-cause mortality.[8] Hypertension, especially uncontrolled arterial hypertension, is the strongest risk factor for stroke and increases the possibility of a more severe stroke; therefore, it is necessary to effectively control this risk factor to prevent stroke and minimize recurrences.[9]
1.3. Hyperlipidemia and stroke
According to the National Cholesterol Education Panel's Adult Treatment Program-3 guidelines, hyperlipidemia can broadly be classified as elevation of LDL cholesterol(>100 mg/dL), total cholesterol(>200 mg/dL), or triglycerides(>150 mg/dL).[10] Serum total cholesterol level, a measure of hyperlipidemia, is positively correlated with IHD morbidity and mortality in Asian countries.[11] The Trial of Org 10172 in Acute Stroke Treatment (TOAST) classification divides patients with ischemic stroke into 5 subgroups:
-
(1)
large-artery atherosclerosis,
-
(2)
cardioembolism,
-
(3)
small-vessel occlusion,
-
(4)
stroke of other determined etiology, and
-
(5)
stroke of undetermined etiology.
Small vessel disease was significantly associated with hyperlipidemia and current smoking.[12,13]
1.4. COPD and stroke
COPD is not only a respiratory disease but is increasingly recognized as a systemic disease with significant clinical extra-pulmonary effects.[14] COPD may be complicated by cardiovascular diseases including right ventricular dysfunction, pulmonary hypertension, IHD, dysrhythmias,[15,16] and stroke.[17] There is a strong epidemiological link between IHD and COPD, especially in severe COPD cases[18–20]; in fact, airflow limitations caused by COPD affects almost one-third of IHD patients.[19] The usual treatment for IHD is antithrombotic therapy using various combinations of antiplatelet and anticoagulant drugs.[21] The risk of hemorrhagic stroke is particularly high in patients receiving dual antiplatelet therapy during first year after stroke or a transient ischemic attack.[22]
Since 1995, Traditional Chinese medicine (TCM) has been covered by the National Health Insurance program in Taiwan. Both TCM and WM are covering in NIH.[23] Common single herbs such as Dan Shen (Salvia miltiorrhiza Bunge, rhizome) or herbal formulas such as Zhi-gan-cao-tang (ZGCT), San Qi, Xue-fu-zhu-yu-tang (XFZYT), Bu-yang-huan-wu-tang (BYHWT) and Zhi-gan-cao-tang (ZGCT) are used to treat heart disease and cerebrovascular diseases.[24–26] This investigation aimed to provide an analysis of combined TCM and western medicine (WM) therapy effectiveness regarding stroke prevention in IHD patients.
2. Methods and materials
2.1. Data source
The National Health Insurance Research Database (NHIRD) is a secondary database that integrates National Health Insurance data. The NHIRD contains almost all the medical care data of Taiwan residents since 1996 including conventional outpatient visits, inpatient visits, and TCM outpatient visits. Information regarding encrypted identification, visit date, International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM), prescriptions, and operations are recorded when the patient receives medical treatment. Information in the Longitudinal Health Insurance Database 2000 (LHID 2000) containing one million individuals from the NHIRD was used in this study. This study was approved and waived the need for patient consent by Research Ethics committee China Medical University and Hospital, Taichung, Taiwan (CMUH104-REC2-115(CR-3)).
2.2. Study population
We selected data records for IHD patients (ICD-9CM: 411-414) between the years 2000 and 2010. Individuals younger than 20 years were excluded. The expired date was set as the patients was dead, withdrawn by NHIRD or out of December 31, 2011. IHD patients have all been examined by electrocardiogram and diagnosed by a cardiologist. We classified the IHD patients into 2 groups by receipt of TCM after diagnosis of IHD (TCM user) or no receipt of TCM (non-TCM user). The index date signifying the date of the first TCM outpatient visit was collected for each patient. Frequency matching was used and the ratio was 1:1 for the sex, age, index year, and first IHD diagnosis year.
2.3. Outcome and confounding factors
The incidence of stroke was obtained for IHD patients after receiving TCM treatment; ischemic stroke and hemorrhagic stroke were identified according to ICD-9-CM codes 433-438 and 430-432, respectively. Patients diagnosed with stroke before the index date were excluded. Patients with additional documentation for hyperlipidemia (ICD-9-CM: 272), DM (ICD-9-CM: 250), hypertension (ICD-9-CM: 401-405) and COPD (ICD-9-CM: 490-493, 494, 496), chronic kidney disease (ICD-9-CM: 585), and cirrhosis (ICD-9-CM: 571) were considered to be comorbidities. In order to reduce any concerns surrounding disease misclassification, the criteria for a patient to be included in the main outcome and comorbidity analyses were at least 2 outpatient visits or 1 inpatient visit. WM including warfarin, dipyridamole, and aspirin were also confounding factors included in the statistical evaluation.
2.4. Statistical analysis
Associations of demographic characteristics and confounding factors were examined using Chi-square tests and Student t-tests. The Chi-square test was used to test the differences in categorical variables and Student t-tests was used to test the differences in continuous variables.
The frequency of TCM prescriptions for IHD patients was calculated along with other information. The event for stroke was calculated in both cohorts. The multivariable Cox proportional hazards regression model was used to assess the stroke risk associated with TCM treatment, and the hazard ratios (HRs) with 95% confidence intervals (CIs) were estimated.
The multivariable model was developed by adjusted for age, sex, hyperlipidemia, DM, hypertension, COPD, chronic kidney disease, and cirrhosis, and warfarin, dipyridamole, and aspirin use. We further analyzed the data to assess the effect of the single Chinese herbal product (CHP) and formula CHPs on the risk of stroke. In addition, we performed Cox proportional hazards regression analysis to measure hazard ratio of stroke among IHD patients by different TCM and non-TCM treatments. The Kaplan-Meier method was used to calculate the survival probability and cumulative incidence of stroke. All analyses were performed using SAS 9.3 software (SAS Institute Inc., Cary, NC). The significance level was set at P < .05 in 2-sided tests.
3. Results
The characteristics of the study population are displayed in Table 1. There were 733 patients using TCM and 733 patients who did not, with the same proportion of sex and age in each group. IHD patients over the age of 65 had a greater risk of stroke (P = .04; Table 2). There was a significant difference DM, hypertension, COPD, chronic kidney disease, and cirrhosis comorbidities between the groups. (P < .001; Table 1) However, only hypertension may affect the risk of stroke (P = .004; Table 2). Other comorbidities including hyperlipidemia, DM, COPD, chronic kidney disease, and cirrhosis did not affect the risk of stroke.
Table 1.
Characteristics of patients with IHD according to TCM use.
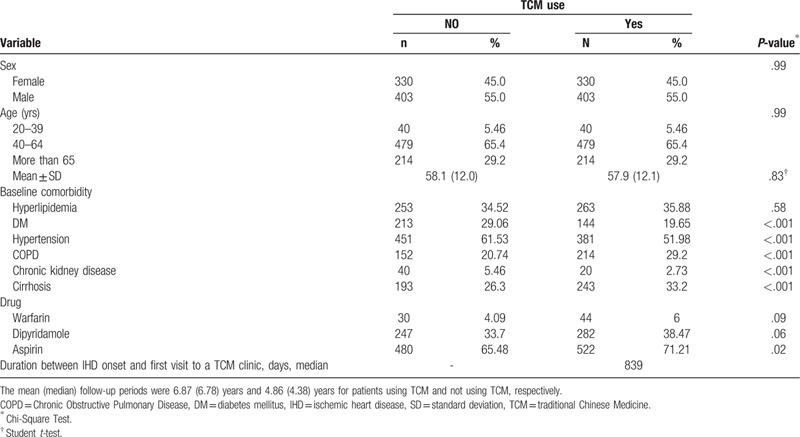
Table 2.
Stroke risk factors among IHD patients.
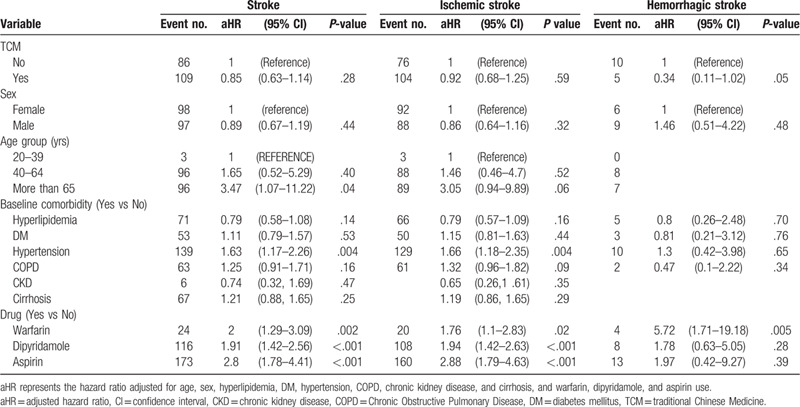
Our data suggests that combined TCM and WM use may be likely to reduce the risk of stroke, ischemic stroke, and hemorrhagic stroke. (aHR = 0.85, 0.92, and 0.34 respectively; Table 2) However, only the aHR difference in hemorrhagic stroke between TCM and non-TCM group was nearly significant (P = .05; Table 2). We also found the survival probability was higher for patients using TCM than patients not using TCM (P < .001; Fig. 1A). The incidence of hemorrhagic stroke was significantly lower in patients using TCM than patients not using TCM (P = .04; Fig. 1D).
Figure 1.
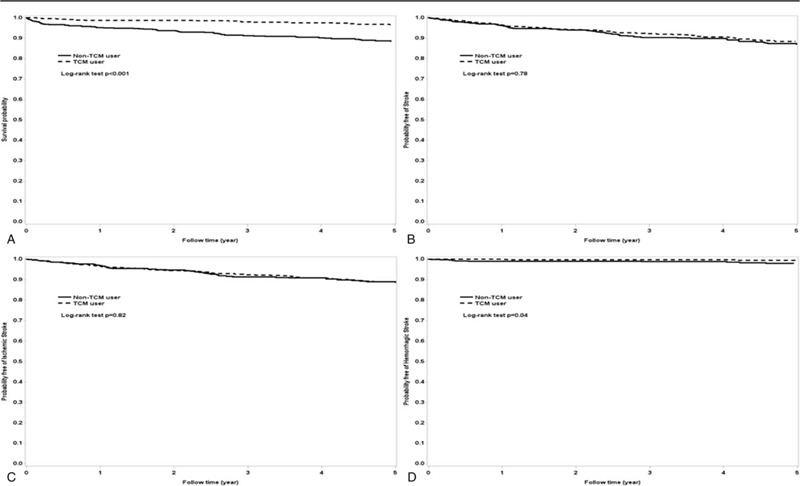
Kaplan-Meier analysis of estimating (A) survival probability; (B) probability free of stroke; (C) probability free of ischemic stroke; (D) probability free of hemorrhagic stroke between ischemic heart disease patients using TCM and those not using TCM. TCM = traditional Chinese Medicine.
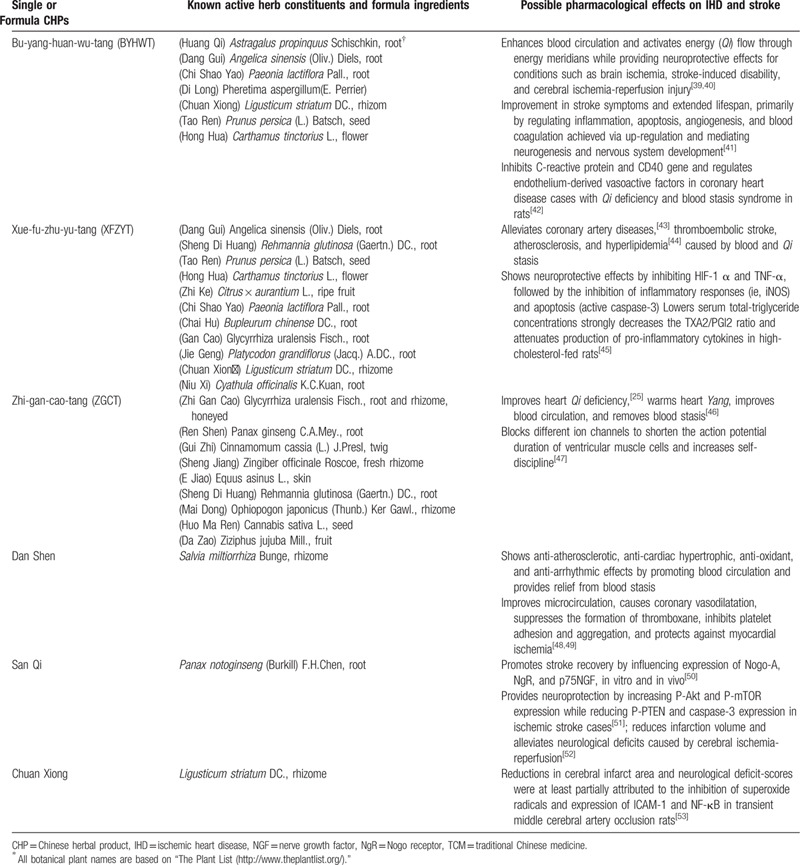
TCM consists of either single Chinese herbal products (CHPs) or formula CHPs. We compared the hazard ratios of stroke among IHD patients associated with the commonest single CHPs such as Dan Shen, San Qi, Chuan Xiong or formula CHPs such as Xue-fu-zhu-yu-tang, Bu-yang-huan-wu-tang, Zhi-gan-cao-tang, respectively. Neither common single CHPs nor formula CHPs demonstrated a significantly effective reduction in the risk of stroke among IHD patients (Table 3). IHD patients with combination TCM and WM treatment would have a 0.3-fold lower risk of stroke risk (95% CI = 0.11–0.84, P = .02; Table 4). The possible mechanisms of frequently used CHPs (single and formula) for IHD and stroke are presented in Table 5.
Table 3.
Hazard Ratios and 95% confidence intervals of stroke associated with TCM use among IHD patients.
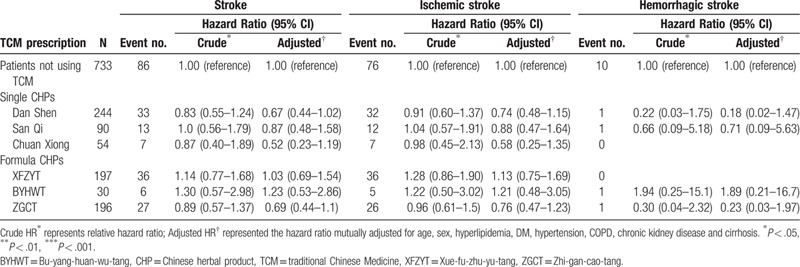
Table 4.
The risk of stroke in IHD patients with different prescription combination.
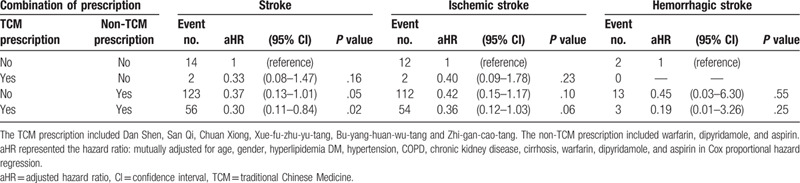
Table 5.
Possible mechanisms of frequently used CHPs for IHD.
4. Discussion
This population-based study using the health insurance database can be almost regarded as the real-world evidence in Taiwan. Through this nationwide cohort analysis, we showed that combined TCM and WM may decrease the risk of stroke and increase the survival rate in IHD patients.
According to this analysis and previous studies,[25,27,28] single and formula CHPs including Dan Shen, San Qi, Chuan Xiong, XFZYT, BYHWT, and ZGCT can be used to treat IHD and stroke. Dan Shen, a common CHP used to improve blood stasis in IHD patients, has antioxidant effects, inhibits smooth-muscle-cell proliferation, and protects against vascular atherosclerotic lesions by suppressing reactive oxygen species via the PKC/p44/42 MAPK-dependent pathway.[29,30] Salvianolic acid is an active polyphenol component in Dan Shen (Salvia miltiorrhiza) that protects against ischemia/reperfusion injury; neuroprotection is dependent on mitochondrial connexin-43 via the PI3K/Akt pathway.[31] San Qi could promote stroke recovery by influencing expression of Nogo-A, NgR, and p75NGF, in vitro and in vivo[37] and provide neuroprotection by increasing P-Akt and P-mTOR expression while reducing P-PTEN and caspase-3 expression in ischemic stroke cases.[38] The other Chuan Xiong would reduce cerebral infarct area and neurological deficit-scores partially attributed to the inhibition of superoxide radicals and expression of ICAM-1 and NF-κB in transient middle cerebral artery occlusion rats.[40] BYHWT has been used to treat and prevent ischemic cardio-cerebral vascular diseases and stroke-induced disabilities for thousands of years. Additionally, ZGCT has been frequently used for generations to treat heart disease, especially arrhythmia, in patients with a knotted irregular pulse and severe palpitations.[32] ZGCT enhances Qi, nourishes Yin, tonifies Yang, nourishes the blood and reduces palpitations.
The survival rate during follow-up was higher in patients using TCM, and the incidence of hemorrhagic stroke was lower. Our results support the findings of a meta-analysis of 22 randomized-controlled trials on ischemic stroke and four on hemorrhagic stroke reporting the benefits of TCM and highlighting improvements in neurological function and overall therapeutic efficacy in poststroke patients.[33]
We did not find differences among patients using single or formula CHPs; this may due to variations in TCM prescriptions since adjustments are made during each visit according to the patient's chief complaints which affects the different TCM syndrome. Nevertheless, a randomized, double-blind, parallel-controlled clinical trial revealed similarities between prescriptions and TCM syndrome; ischemic stroke analyses showed complete (series of formulas) and incomplete (only one formula) prescriptions and TCM syndromes have similar effects on the central clinical manifestations of ischemic stroke, such as neurological deficits and difficulty performing activities in daily living. However, there were significant differences in individual dysfunctions, such as subjective symptoms.[34]
Our results revealed there is a higher risk of stroke in IHD patients over 65 years old. A global study reported that the mean age of people with incident hemorrhagic stroke was 69.1 ± 0.15 years in high-income countries and 63.8 ± 0.13 years in low- and middle-income countries.[35] In other studies of Chinese epidemiology, stroke incidence increased with age. The highest rates were in people aged over 75 years, where the incidence rate was 30 times that of individuals aged 35 to 44 years.[36] These results are consistent with our finding. In addition, there were some significant differences between 2 groups in baseline comorbidities. It might mean the patients with COPD preferred to use TCM, while the patients with DM and hypertension were not disposed to receive TCM. Besides, patients received aspirin in TCM group might have more will to accept TCM treatment. Aspirin was one of the first-choice drugs not only for IHD but also for ischemic stroke. It was interesting that in our study, patients using TCM might have the lower incidence of hemorrhage stroke. Comparing the most common used single and formula CHPs, most of prescriptions are promoting blood circulation and relieving blood stasis. This result might give us other hint that combining of TCM and anticoagulation/antiplatelet agents might not increase the risk of hemorrhage. The mechanism was unclear and it might need more studies to prove it.
There were some several limitations in this study. First, the patients not using TCM may have received other complementary therapies during the study. Second, The TCM data from the NHIRD database was confined to CHPs, and herbal decoctions were not recorded. Third, lifestyle-related information such as data on alcohol use, cigarette smoking, weight, or socioeconomic status was not available. Forth, novel oral anticoagulants for stroke prevention such as dabigatran, rivaroxaban, and apixaban were not included in our analysis. Finally, the study cases were selected according to ICD-9 codes, potentially causing a misclassification bias despite the ability of the auditing mechanism used by the National Health Insurance Administration to minimize diagnostic uncertainty and misclassification.[37] Recently, linking across the NHIRD and other health-related databases for data management and analyses are trying to execute.[38] This might decrease the coding and data inaccuracy rate in the future.
5. Summary/Conclusions
IHD patients using combined TCM and WM had a higher survival rate and a lower risk of new onset stroke, especially hemorrhagic stroke than those who did not use TCM treatment. Therefore, combination of TCM and WM may prevent stroke in IHD patients.
Author contributions
Conceptualization: Wen-Long Hu, Yu-Chiang Hung.
Data curation: Chung Y. Hsu, Yuan-Chih Su.
Formal analysis: Yuan-Chih Su.
Investigation: Yu-Chen Cheng, Wen-Long Hu, Yu-Chiang Hung.
Methodology: Wen-Long Hu, Chung Y. Hsu, Yuan-Chih Su, Yu-Chiang Hung.
Project administration: Wen-Long Hu, Chung Y. Hsu, Yu-Chiang Hung.
Supervision: Chung Y. Hsu, Yu-Chiang Hung.
Validation: Cheng-Nan Lu, Wen-Long Hu, Yu-Chiang Hung.
Visualization: Cheng-Nan Lu, Wen-Long Hu, Yu-Chiang Hung.
Writing – original draft: Yu-Chen Cheng, Yuan-Chih Su, Yu-Chiang Hung.
Writing – review & editing: Cheng-Nan Lu, Wen-Long Hu, Yu-Chiang Hung.
Footnotes
Abbreviations: BYHWT = Bu-yang-huan-wu-tang, COPD = chronic obstructive pulmonary disease, DM = diabetes mellitus, IHD = ischemic heart disease, MI = myocardial infarction, NHIRD = National Health Insurance Research Database, TCM = traditional Chinese medicine, XFZYT = Xue-fu-zhu-yu-tang, ZGCT = Zhi-gan-cao-tang.
How to cite this article: Cheng YC, Lu CN, Hu WL, Hsu CY, Su YC, Hung YC. Decreased stroke risk with combined traditional Chinese and western medicine in patients with ischemic heart disease: a real-world evidence. Medicine. 2020;99:42(e22654).
Availability of data and materials: The National Health Research Institutes Database (NHIRD) which are managed by National Health Research Institutes in Taiwan. The information in the Longitudinal Health Insurance Database 2000 (LHID 2000) containing one million individuals from the NHIRD was used in this study.
This study is supported in part by Taiwan Ministry of Health and Welfare Clinical Trial Center (MOHW108-TDU-B-212-133004), China Medical University Hospital, Academia Sinica Stroke Biosignature Project (BM10701010021), MOST Clinical Trial Consortium for Stroke (MOST 107-2321-B-039 -004-), Tseng-Lien Lin Foundation, Taichung, Taiwan, and Katsuzo and Kiyo Aoshima Memorial Funds, Japan. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. The biostatistics revision was by the Biostatistics Center, Kaohsiung Chang Gung Memorial Hospital and Cheng-Li Lin, the chief biostatistician of Management Office for Health Data (DryLab), Clinical Trial Center (CTC), China Medical University Hospital.
The authors have no conflicts of interests to disclose.
All data generated or analyzed during this study are included in this published article [and its supplementary information files].
References
- [1].Hata J, Kiyohara Y. Epidemiology of stroke and coronary artery disease in Asia. Circ J 2013;77:1923–32. [DOI] [PubMed] [Google Scholar]
- [2].Ueshima H, Sekikawa A, Miura K, et al. Cardiovascular disease and risk factors in Asia: a selected review. Circulation 2008;118:2702–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Huo X, Gao L, Guo L, et al. Risk of non-fatal cardiovascular diseases in early-onset versus late-onset type 2 diabetes in China: a cross-sectional study. Lancet Diabetes Endocrinol 2016;4:115–24. [DOI] [PubMed] [Google Scholar]
- [4].Fujihara K, Sone H. Cardiovascular disease in Japanese patients with type 2 diabetes mellitus. Ann Vasc Dis 2018;11:2–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Hill MD. Stroke and diabetes mellitus. Handbook of Clinical Neurology. Vol. 126 2014;167–174. [DOI] [PubMed] [Google Scholar]
- [6].Haffner SM, Lehto S, Ronnemaa T, et al. Mortality from coronary heart disease in subjects with type 2 diabetes and in nondiabetic subjects with and without prior myocardial infarction. N Engl J Med 1998;339:229–34. [DOI] [PubMed] [Google Scholar]
- [7].Woodward M, Zhang X, Barzi F, et al. The effects of diabetes on the risks of major cardiovascular diseases and death in the Asia-Pacific region. Diabetes Care 2003;26:360–6. [DOI] [PubMed] [Google Scholar]
- [8].Irvin MR, Booth JN, 3rd, et al. Apparent treatment-resistant hypertension and risk for stroke, coronary heart disease, and all-cause mortality. J Am Soc Hypertens 2014;8:405–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Hisham NF, Bayraktutan U. Epidemiology, pathophysiology, and treatment of hypertension in ischaemic stroke patients. J Stroke Cerebrovasc Dis 2013;22:e4–14. [DOI] [PubMed] [Google Scholar]
- [10].Nelson RH. Hyperlipidemia as a risk factor for cardiovascular disease. Prim Care 2013;40:195–211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Zhang X, Patel A, Horibe H, et al. Cholesterol, coronary heart disease, and stroke in the Asia Pacific region. Int J Epidemiol 2003;32:563–72. [DOI] [PubMed] [Google Scholar]
- [12].Adams HP, Jr, Bendixen BH, Kappelle LJ, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke 1993;24:35–41. [DOI] [PubMed] [Google Scholar]
- [13].Ihle-Hansen H, Thommessen B, Wyller TB, et al. Risk factors for and incidence of subtypes of ischemic stroke. Funct Neurol 2012;27:35–40. [PMC free article] [PubMed] [Google Scholar]
- [14].Vestbo J, Hurd SS, Agusti AG, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med 2013;187:347–65. [DOI] [PubMed] [Google Scholar]
- [15].Roversi S, Fabbri LM, Sin DD, et al. Chronic obstructive pulmonary disease and cardiac diseases. an urgent need for integrated care. Am J Respir Crit Care Med 2016;194:1319–36. [DOI] [PubMed] [Google Scholar]
- [16].Raparelli V, Pastori D, Pignataro SF, et al. Major adverse cardiovascular events in non-valvular atrial fibrillation with chronic obstructive pulmonary disease: the ARAPACIS study. Intern Emerg Med 2018;13:1349. [DOI] [PubMed] [Google Scholar]
- [17].Morgan AD, Sharma C, Rothnie KJ, et al. Chronic obstructive pulmonary disease and the risk of stroke. Ann Am Thorac Soc 2017;14:754–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Reed RM, Eberlein M, Girgis RE, et al. Coronary artery disease is under-diagnosed and under-treated in advanced lung disease. Am J Med 2012;125:1228.e1213–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Franssen FM, Soriano JB, Roche N, et al. Lung function abnormalities in smokers with ischemic heart disease. Am J Respir Crit Care Med 2016;194:568–76. [DOI] [PubMed] [Google Scholar]
- [20].Ambrosino P, Lupoli R, Iervolino S, et al. Clinical assessment of endothelial function in patients with chronic obstructive pulmonary disease: a systematic review with meta-analysis. Intern Emerg Med 2017;12:877–85. [DOI] [PubMed] [Google Scholar]
- [21].Hirsh J, Guyatt G, Albers GW, et al. Antithrombotic and thrombolytic therapy: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest 2008;133: 6 Suppl: 110s–2s. [DOI] [PubMed] [Google Scholar]
- [22].Ducrocq G, Amarenco P, Labreuche J, et al. A history of stroke/transient ischemic attack indicates high risks of cardiovascular event and hemorrhagic stroke in patients with coronary artery disease. Circulation 2013;127:730–8. [DOI] [PubMed] [Google Scholar]
- [23].Chang LC, Huang N, Chou YJ, et al. Utilization patterns of Chinese medicine and Western medicine under the National Health Insurance Program in Taiwan, a population-based study from 1997 to 2003. BMC Health Serv Res 2008;8:170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Su CY, Ming QL, Rahman K, et al. Salvia miltiorrhiza: Traditional medicinal uses, chemistry, and pharmacology. Chin J Nat Med 2015;13:163–82. [DOI] [PubMed] [Google Scholar]
- [25].Hung YC, Tseng YJ, Hu WL, et al. Demographic and prescribing patterns of Chinese herbal products for individualized therapy for ischemic heart disease in Taiwan: population-based study. PloS One 2015;10:e0137058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Tsai MY, Hu WL, Lin CC, et al. Prescription pattern of Chinese herbal products for heart failure in Taiwan: a population-based study. Int J Cardiol 2017;228:90–6. [DOI] [PubMed] [Google Scholar]
- [27].Hung IL, Hung YC, Wang LY, et al. Chinese herbal products for ischemic stroke. Am J Chin Med 2015;43:1365–79. [DOI] [PubMed] [Google Scholar]
- [28].Hung YC, Cheng YC, Muo CH, et al. Adjuvant Chinese herbal products for preventing ischemic stroke in patients with atrial fibrillation. PloS One 2016;11:e0159333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Zhou L, Zuo Z, Chow MS. Danshen: an overview of its chemistry, pharmacology, pharmacokinetics, and clinical use. J Clin Pharmacol 2005;45:1345–59. [DOI] [PubMed] [Google Scholar]
- [30].Hung YC, Wang PW, Pan TL. Functional proteomics reveal the effect of Salvia miltiorrhiza aqueous extract against vascular atherosclerotic lesions. Biochim Biophys Acta 2010;1804:1310–21. [DOI] [PubMed] [Google Scholar]
- [31].Hou S, Zhao MM, Shen PP, et al. Neuroprotective effect of salvianolic acids against cerebral ischemia/reperfusion injury. Int J Mol Sci 2016;17:1190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Chen WG, Ba ZM. ZHANG Yi's experience in treating severe arrhythmia. J Tradit Chin Med. 2010;30:47–50. [DOI] [PubMed] [Google Scholar]
- [33].Xu JH, Huang YM, Ling W, et al. Wen Dan Decoction for hemorrhagic stroke and ischemic stroke. Complement Ther Med 2015;23:298–308. [DOI] [PubMed] [Google Scholar]
- [34].Gao Y, Zhong H, Ma B, et al. Randomized, double-blind, parallel-controlled clinical trial on correspondence of prescriptions and traditional Chinese medicine syndrome of ischemic stroke. J Tradit Chin Med 2012;32:335–42. [DOI] [PubMed] [Google Scholar]
- [35].Krishnamurthi RV, Moran AE, Forouzanfar MH, et al. The global burden of hemorrhagic stroke: a summary of findings from the GBD 2010 study. Global Heart 2014;9:101–6. [DOI] [PubMed] [Google Scholar]
- [36].Liu M, Wu B, Wang W-Z, et al. Stroke in China: epidemiology, prevention, and management strategies. Lancet Neurol 2007;6:456–64. [DOI] [PubMed] [Google Scholar]
- [37].Cheng CL, Kao YH, Lin SJ, et al. Validation of the national health insurance research database with ischemic stroke cases in Taiwan. Pharmacoepidemiol Drug Saf 2011;20:236–42. [DOI] [PubMed] [Google Scholar]
- [38].Hsieh CY, Su CC, Shao SC, et al. Taiwan's National Health Insurance Research Database: past and future. Clin Epidemiol 2019;11:349–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Danesh J, Wheeler JG, Hirschfield GM, et al. C-reactive protein and other circulating markers of inflammation in the prediction of coronary heart disease. N Engl J Med 2004;350:1387–97. [DOI] [PubMed] [Google Scholar]
- [40].Li XM, Bai XC, Qin LN, et al. Neuroprotective effects of Buyang Huanwu decoction on neuronal injury in hippocampus after transient forebrain ischemia in rats. Neurosci Lett 2003;346:29–32. [DOI] [PubMed] [Google Scholar]
- [41].Wang HW, Liou KT, Wang YH, et al. Deciphering the neuroprotective mechanisms of Bu-yang Huan-wu decoction by an integrative neurofunctional and genomic approach in ischemic stroke mice. J Ethnopharmacol 2011;138:22–33. [DOI] [PubMed] [Google Scholar]
- [42].Zhang H, Wang WR, Lin R, et al. Buyang Huanwu decoction ameliorates coronary heart disease with Qi deficiency and blood stasis syndrome by reducing CRP and CD40 in rats. J Ethnopharmacol 2010;130:98–102. [DOI] [PubMed] [Google Scholar]
- [43].Chu FY, Wang J, Yao KW, et al. Effect of Xuefu Zhuyu Capsule on the symptoms and signs and health-related quality of life in the unstable angina patients with blood-stasis syndrome after percutaneous coronary intervention: a Randomized controlled trial. Chin J Integr Med 2010;16:399–405. [DOI] [PubMed] [Google Scholar]
- [44].Lee JJ, Hsu WH, Yen TL, et al. Traditional Chinese medicine, Xue-Fu-Zhu-Yu decoction, potentiates tissue plasminogen activator against thromboembolic stroke in rats. J Ethnopharmacol 2011;134:824–30. [DOI] [PubMed] [Google Scholar]
- [45].Liu L, Cheng Y, Zhang H. Phytochemical analysis of anti-atherogenic constituents of Xue-Fu-Zhu-Yu-Tang using HPLC-DAD-ESI-MS. Chem Pharm Bull 2004;52:1295–301. [DOI] [PubMed] [Google Scholar]
- [46].TF T. Meridian related myocardial infarction- a case report. Taiwan J Clin Chin Med 2008;14:308–15. [Google Scholar]
- [47].Liu W, Xiong X, Feng B, et al. Classic herbal formula Zhigancao Decoction for the treatment of premature ventricular contractions (PVCs): a systematic review of randomized controlled trials. Complement Ther Med 2015;23:100–15. [DOI] [PubMed] [Google Scholar]
- [48].Cheng TO. Danshen: a versatile Chinese herbal drug for the treatment of coronary heart disease. Int J Cardiol 2006;113:437–8. [DOI] [PubMed] [Google Scholar]
- [49].Cheng TO. Danshen: a popular Chinese cardiac herbal drug. J Am Coll Cardiol 2006;47:1498.author reply 1499–1500. [DOI] [PubMed] [Google Scholar]
- [50].Liu L, Zhu L, Zou Y, et al. Panax notoginseng saponins promotes stroke recovery by influencing expression of Nogo-A, NgR and p75NGF, in vitro and in vivo. Biol Pharm Bull 2014;37:560–8. [DOI] [PubMed] [Google Scholar]
- [51].Yan YT, Li SD, Li C, et al. Panax notoginsenoside saponins Rb1 regulates the expressions of Akt/mTOR/PTEN signals in the hippocampus after focal cerebral ischemia in rats. Behav Brain Res 2018;345:83–92. [DOI] [PubMed] [Google Scholar]
- [52].Zeng XS, Zhou XS, Luo FC, et al. Comparative analysis of the neuroprotective effects of ginsenosides Rg1 and Rb1 extracted from Panax notoginseng against cerebral ischemia. Can J Physiol Pharmacol 2014;92:102–8. [DOI] [PubMed] [Google Scholar]
- [53].Cheng CY, Ho TY, Lee EJ, et al. Ferulic acid reduces cerebral infarct through its antioxidative and anti-inflammatory effects following transient focal cerebral ischemia in rats. Am J Chin Med 2008;36:1105–19. [DOI] [PubMed] [Google Scholar]


