Abstract
Background
The Birmingham Hip Resurfacing (BHR) prosthesis is the most commonly used metal-on-metal hip resurfacing arthroplasty device. The current manufacturer-recommended target demographic for the BHR is male patients, younger than 65 years requiring a femoral head size of ≥ 50 mm. Female patients, older patients, and individuals with smaller femoral-head diameter (≤ 50 mm) are known to have higher revision rates. Prior studies suggest that the survivorship of the BHR when used in the target demographic is comparable with that of primary conventional THA, but comparing survivorship of the most durable hip resurfacing arthroplasty device to the survivorship of all conventional THA prostheses is not ideal because the THA group comprises a large number of different types of prostheses that have considerable variation in prosthesis survival. A more informative comparison would be with the THA implants with the best survivorship, as this might help address the question of whether survivorship in the BHR target population can be improved by using a well-performing conventional THA.
Questions/purposes
We compared the difference in cumulative percent revision, reasons for revision and types of revision for procedures reported to the Australian Orthopaedic Association National Joint Replacement Registry (AOANJRR) using the BHR prosthesis (femoral-head size > 50 mm) and three conventional THA prostheses identified as having the lowest 10-year cumulative percent revision in the currently recommended BHR target population to ask: (1) Does the BHR have a lower cumulative revision rate than the group of three conventional THA prostheses? (2) Is there a difference in the revision diagnosis between the BHR and the three best conventional THA prostheses? (3) What is the difference in the components used for a revision of a BHR compared with the three best conventional THA prostheses?
Methods
Data reported to the AOANJRR between September 1, 1999 and December 31, 2018 was used for this analysis. This study period includes almost the entire use of the BHR in Australia. The AOANJRR is a large national joint registry with almost 100% completeness, high accuracy, rigorous validation, and little to no loss to follow-up. The study population included males younger than 65 years that had received one hip replacement procedure for osteoarthritis. All patients with bilateral procedures, no matter the time interval between hips, were excluded. Only BHR prostheses with a femoral-head size ≥ 50 mm and conventional THA prostheses with femoral head sizes ≥ 32 mm and either ceramic-on-ceramic or metal, ceramic, ceramicized metal-on-crosslinked polyethylene (XLPE) bearings were included. These femoral head sizes and bearings were selected because they reflect modern conventional THA practice. There is no difference in the revision rate of these bearings in the AOANJRR. There were 4790 BHR procedures and 2696 conventional THA procedures in the study group. The mean (± SD) age for BHR procedures was 52 ± 7.8 years and 56 ± 7.1 years for conventional THA procedures. All comparative analyses were adjusted for age. Other demographics data including American Society Anesthesiologists (ASA) score and BMI were only included in AOANJRR data collection since 2012 and 2015, respectively, and have not been included in this analysis because of the low use of BHR in Australia since that time. The maximum follow-up was 18.7 years for both groups and mean follow-up of 11.9 years for the BHR and 9.3 years for the conventional THA group. Revision rates were determined using Kaplan-Meier estimates of survivorship to describe the time to the first revision, with censoring at the time of death or closure of the database at the time of analysis. A revision was defined as removal, replacement or addition of any component of a joint replacement. Revisions can be further classified as major revisions (removal of a component articulating with bone—usually the stem and/or the shell) or minor revisions (removal of other components—usually the head and/or the liner). The unadjusted cumulative percent revision after the primary arthroplasty (with 95% confidence intervals) was calculated and compared using Cox proportional hazard models adjusted for age.
Results
The BHR prosthesis had a statistically higher rate of all-cause revision at 17 years than the selected conventional THA prostheses (HR 2.77 [95% CI 1.78 to 4.32]; p < 0.001). The revision diagnoses differed between the groups, with the BHR demonstrating a higher revision rate for loosening after 2 years than the conventional THA protheses (HR 4.64 [95% CI 1.66 to 12.97]; p = 0.003), as well as a higher fracture rate during the entire period (HR 2.57 [95% CI 1.24 to 5.33]; p = 0.01). There was a lower revision rate for infection for the BHR compared with the THA group in the first 5 years, with no difference between the two groups after this time. All revisions of the BHR were major revisions (such as, removal or exchange of the femoral and/or acetabular components) and this occurred in 4.5% of the primary BHR procedures. Major revision was the most common type of revision for primary THA accounting for 1.7% of all primary THA procedures. Minor revisions (head, inset or both) were undertaken in a further 0.6% of primary THA procedures.
Conclusions
Given the increasing revision risk of the BHR compared with better-performing conventional THA prostheses in the target population, we recommend that patients be counseled about this risk. We suggest that a THA with proven low revision rates might be the better choice, particularly for patients who are concerned about implant durability. Well-controlled prospective studies that show appreciable clinically important differences in patient-reported outcomes and functional results favoring the BHR over conventional THA prostheses using modern bearings are needed to justify the use of the BHR in view of this revision risk.
Level of Evidence
Level III, therapeutic study.
Introduction
Metal-on-metal hip resurfacing arthroplasty was introduced in the 1990s to provide a durable bearing surface without the complications of polyethylene wear [24]. The proposed advantages of hip resurfacing arthroplasty include the restoration of a more anatomic hip that theoretically should permit a greater range of movement and better proprioception and allow quicker recovery from surgery [1, 27]. Other potential benefits include a reduction in revision for dislocation because of larger head sizes and preservation of femoral bone stock, which would potentially lead to more straightforward revision surgery [8, 11]. One of these hip resurfacing arthroplasty devices is the Birmingham Hip Resurfacing (BHR) System (Smith & Nephew Orthopaedics, Memphis, TN, USA). This device is considered one of the better-performing hip resurfacing prostheses [9, 11, 23, 24, 30]. There was a rapid uptake in the use of hip resurfacing arthroplasty after its introduction into the market. The National Joint Registry (NJR) for England and Wales, Northern Island, and the Isle of Man reported that in 2010, 14% of conventional THAs in patients younger than 55 years were resurfacing procedures [32]. In Australia, the use of resurfacing procedures accounted for 6% of all primary THAs in 2001 and peaked at 9% in 2005 [2].
In 2006, the Australian Orthopaedic Association National Joint Replacement Registry (AOANJRR) was the first to report a higher revision rate in patients undergoing hip resurfacing arthroplasty compared with patients undergoing conventional THA performed for osteoarthritis (OA) [2]. The revision risk was most evident in patients aged ≥ 55 years. There were also higher revision rates for specific patient populations receiving hip resurfacing arthroplasty. Female patients with a hip resurfacing arthroplasty had a 1.9-fold increase in revision risk at 3 years compared to male patients. Revision rates were also increased when femoral head sizes < 50 mm were used, and this was irrespective of sex [3, 28]. Smaller head sizes had a higher cumulative incidence of loosening or lysis, metal-related pathology, and fracture than > 50 mm head sizes [4]. The Nordic Arthroplasty Registries, the NJR, and surgeon case series also reported similar findings with respect to sex, age, and head size differences in revision after hip resurfacing arthroplasty [9, 13, 17, 19].
The BHR was the most commonly used hip resurfacing arthroplasty prosthesis throughout the period in which these findings were reported. In 2014, the AOANJRR reported that the use of the BHR had increased to 67% of all resurfacing procedures in Australia [4]. However in June 2015, the BHR manufacturer (Smith & Nephew) issued an urgent field safety notice, with the Australian Government’s device regulatory authority issuing a recall action notification indicating that the use of the BHR was contraindicated in females and recalling femoral and acetabular head components with femoral head sizes < 50 mm [31, 33].
Since then, the manufacturer has recommended that the BHR prosthesis be limited to males younger than 65 years and to femoral head sizes of ≥ 50 mm [31]. When limited to this specific patient population, the BHR prosthesis and several other hip resurfacing arthroplasty devices have had acceptable results [6, 18, 23, 24]. In 2018, the AOANJRR reported that the BHR prosthesis had one of the lowest cumulative percent revisions (CPR) compared with other hip resurfacing arthroplasty devices (6.6% at 10 years) [5]. Furthermore, it has also been reported that the BHR prosthesis has a revision rate that is equal to or lower than that of conventional THA prostheses in the current target population [7, 10, 11, 20, 23, 24, 30].
The evident problem of studies that compared the BHR prosthesis to all conventional THA prostheses is that a single better-performing prosthesis from one class is compared with the average performance of many different devices of another class where there is considerable variation in the revision rate of those many different conventional THA prostheses [5]. A potentially more relevant comparison is how the BHR revision rate compares with conventional THA prostheses with low revision rates in the target population. This analysis has the potential to provide further insight into the question of whether the revision rate in the resurfacing target population can be improved by using the BHR or alternatively one of a number of well-performing conventional THA prostheses.
Using AOANJRR data, the survivorship of the BHR in young males was compared with those of the three best-performing conventional THA prostheses when used in the same population. This was done to determine: (1) Does the BHR have a lower cumulative revision rate than the group of three conventional THA prostheses? (2) Is there a difference in the revision diagnosis between the BHR and the three best conventional THA prostheses? (3) What is the difference in the components used for a revision of a BHR compared with the three best conventional THA prostheses?
Patients and Methods
The AOANJRR longitudinally maintains data on all primary and revision joint replacement procedures. These are cross-validated with independently collected state and territory health department data using a sequential, multilevel matching process. Data are also matched biannually with data in the Department of Health and Ageing National Death Index to obtain information on date of death.
The study included procedures reported to the AOANJRR between September 1, 1999 and December 31, 2018. The study population comprised males younger than 65 years with a primary diagnosis of OA who had a single hip replacement procedure with either a BHR prosthesis or one of three identified conventional THA prostheses.
The exclusion criteria for both groups included all females, patients aged 65 years or older, diagnoses other than OA, and all bilateral hip replacement procedures. As the use of BHR femoral head < 50 mm sizes are no longer recommended, all BHR procedures using these femoral head sizes were also excluded.
The three conventional THA devices were chosen by selecting the three prostheses with more than 1000 implantations in the target group that had the lowest 5 year CPR. The AOANJRR has previously published on this type of analysis because it reduces the potential for confounding based on the wide variation in performance of conventional THA prostheses [32]. All three conventional THA prostheses were cementless devices, and included the Secur-Fit™ Plus/Trident® (Shell) (Stryker Orthopaedics, Mahwah, NJ, USA), Synergy™/R3 (Smith & Nephew Orthopaedics, Memphis, TN, USA), and Synergy™/Reflection™ (Shell) (Smith & Nephew Orthopaedics). To ensure that conventional THA prosthesis use was consistent with contemporary practice, only conventional THA procedures using modern bearings (ceramic-on-ceramic bearings or ceramic, metal or ceramicized metal-on-XLPE) and head sizes of ≥ 32 mm were included. There is almost no difference in the performance of these bearings when compared using Australian registry data [5]. The most common femoral head size was 36 mm (51% [1368 of 2696]) followed by 32 mm (47% [1278 of 2696]) and ≥ 40 mm (2% [50 of 2696]). Head sizes of ≤ 28 mm were excluded for two reasons. In Australia, they are now rarely used and account for only 6% of all procedures using the selected conventional THA prostheses. The second reason is because when used these smaller femoral head sizes are most commonly associated with acetabular shells of smaller diameter (< 52 mm). Patients requiring smaller-sized acetabular prostheses no longer have the option of a resurfacing procedure due to the discontinuation of femoral heads < 50 mm (see Fig. 1; Supplemental Digital Content, http://links.lww.com/CORR/A407).
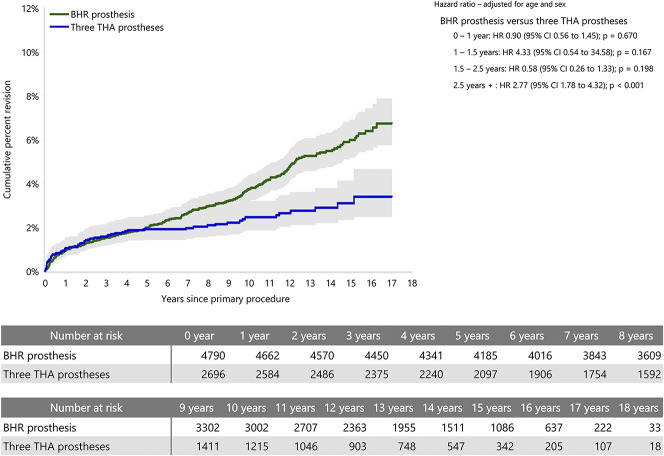
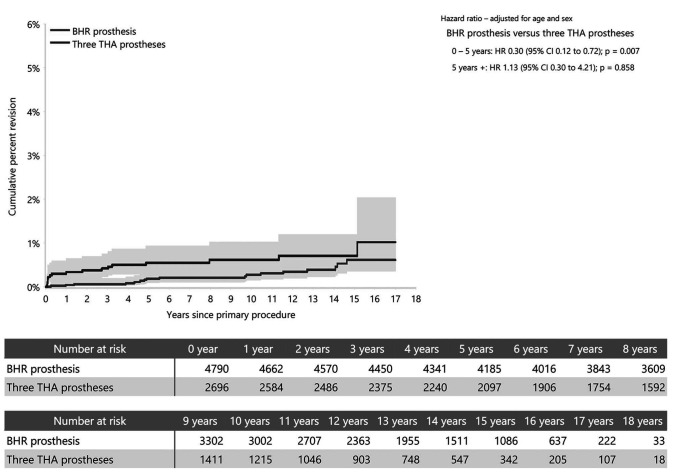
Fig. 1.
This graph shows the CPR of the BHR prosthesis and three primary conventional THA prostheses with the lowest 10-year CPR for men younger than 65 years (primary diagnosis of osteoarthritis).
The AOANJRR records reasons for revision and the type of revision. It further categorizes revision surgery as major or minor. A minor revision is the replacement of a modular femoral head, liner, or addition of any other component that is not a major component. A major revision is the replacement of a component that interfaces with bone, such as a femoral prosthesis (femoral stem for conventional THA, femoral head for BHR and/or acetabular shell or cup).
The study included 4790 BHR procedures and 2696 conventional THA procedures, all performed for OA. The mean (± SD) age for BHR procedures was 52 ± 7.8 years and 56 ± 7.1 years for conventional THA procedures (p < 0.001). The maximum follow-up for both groups was 18.7 years and the mean follow-up was 11 ± 4.5 years for the BHR group and 9 ± 4.8 years for the conventional THA group (p < 0.001).
Revision rates were determined using Kaplan-Meier estimates of survivorship to describe the time to the first revision, with censoring at the time of death or closure of the database at the time of analysis. Competing risk analysis was not used as the number of deaths in this younger age group was low. The CPR after the primary arthroplasty was calculated with 95% confidence intervals using unadjusted point-wise Greenwood estimates. Hazard ratios adjusting for age were calculated using Cox proportional hazards models and were used to statistically compare revision rates between the groups. The assumption of the proportional hazard was checked analytically for each model; if the interaction between the predictor and the log of time was significant, then we used a time-varying model. Timepoints were iteratively chosen until the assumption of proportionality was met, and the HRs were calculated for each selected time period. All tests were two-tailed at the 5% significance level. The statistical analysis was performed using SAS version 9.4 (SAS Institute Inc, Cary, NC, USA). The reasons for revision and type of revision were also determined for the BHR and three THA prostheses.
Results
Revision Rate
The risk of all-cause revision at 17 years was greater for the BHR group (6.7% [95% CI 5.8 to 7.9]) compared with the THA group (3.4% [95% CI 2.5 to 4.6]). There was no difference in the revision rate between the groups in the first 2.5 years. After that time, the BHR prosthesis had a higher revision rate than the three conventional THA prostheses (HR 2.77 [95% CI 1.78 to 4.32]; p < 0.001) (Fig. 1).
Revision Diagnoses
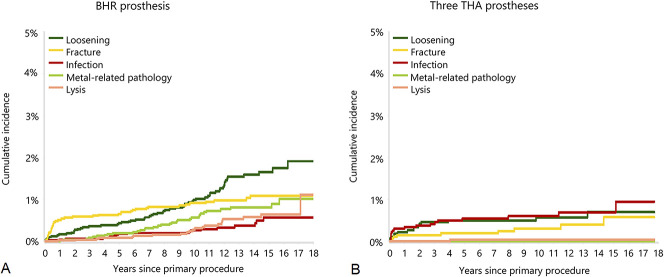
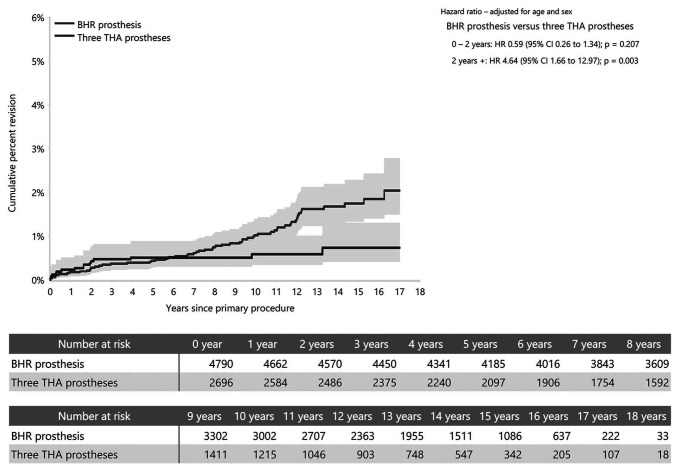
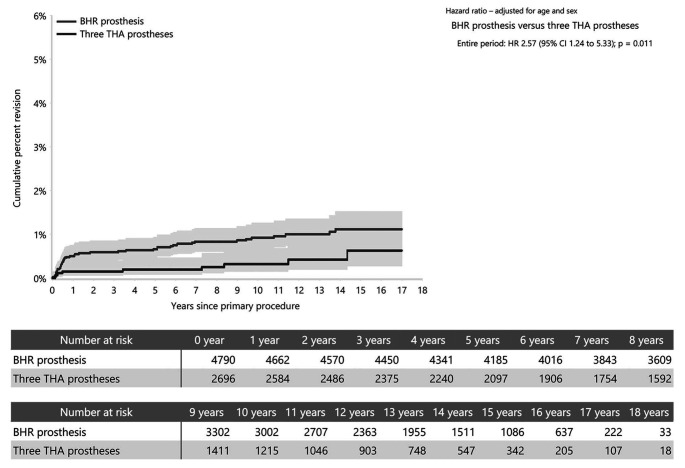
The BHR group had a higher rate of revision for loosening, fracture, metal-related pathology and lysis (Table 1). The THA group had a higher rate of revision for dislocation and infection (Fig. 2). The BHR group had a higher rate of revision for loosening after 2 years (HR 4.64 [95% CI 1.66 to 12.97]; p = 0.003) (Fig. 3) and a higher rate of revision for fracture during the entire period compared to the THA group (HR 2.57 [95% CI 1.24 to 5.33]; p = 0.01) (Fig. 4). There was a lower rate of revision for infection for the BHR compared with the THA group in the first 5 years (HR 0.30 [95% CI 0.12 to 0.72]; p = 0.007), with no difference between the two groups after that time (Fig. 5). Metal-related pathology was the revision diagnosis in 0.7% of all primary procedures (32 of 4790) in the BHR group, and there were no revisions for metal-related pathology in the conventional THA group.
Table 1.
Revision diagnosis in men younger than 65 years (primary diagnosis of OA) with BHR total hip resurfacing and primary conventional THA using the three prosthesis combinations with the lowest 10-year CPR (excluding bilateral procedures)
| Revision diagnosis | BHR total hip resurfacing | Three THA prostheses | ||
| Type of revision as a percentage of primary procedures (n = 4790) | Type of revision as a percentage of revision procedures (n = 215) | Type of revision as a percentage of primary procedures (n = 2696) | Type of revision as a percentage of revision procedures (n = 63) | |
| Loosening | 1.3 (60) | 28 (60) | 0.6 (15) | 24 (15) |
| Fracture | 0.9 (45) | 21 (45) | 0.3 (9) | 14 (9) |
| Metal-related pathology | 0.7 (32) | 15 (32) | ||
| Lysis | 0.4 (21) | 10 (21) | 0.0 (1) | 2 (1) |
| Infection | 0.4 (17) | 8 (17) | 0.6 (17) | 27 (17) |
| Pain | 0.2 (12) | 6 (12) | 0.1 (2) | 3 (2) |
| Osteonecrosis | 0.2 (10) | 5 (10) | ||
| Prosthesis dislocation | 0.2 (6) | 10 (6) | ||
| Malposition | 0.1 (5) | 2 (5) | 0.1 (3) | 5 (3) |
| Other | 0.3 (13) | 6 (13) | 0.4 (10) | 16 (10) |
| Number of revisions | 4.5 (215) | 100 (215) | 2.3 (63) | 100 (63) |
Fig. 2.
A-B These graphs show (A) The cumulative incidence revision diagnosis of the BHR prosthesis for men age younger than 65 years (primary diagnosis of osteoarthritis; bilaterals excluded). (B) The cumulative incidence revision diagnosis of the three THA prostheses for men age younger than 65 years (primary diagnosis of osteoarthritis; patients with bilateral procedures were excluded).
Fig. 3.
This graph shows the CPR for loosening of the BHR prosthesis and three primary conventional THA prostheses with the lowest 10-year CPR for men younger than 65 years (primary diagnosis of osteoarthritis; excluding patients with bilateral procedures).
Fig. 4.
This graph shows the CPR for fracture of the BHR prosthesis and three primary conventional THA prostheses with the lowest 10-year CPR for men younger than 65 years (primary diagnosis of osteoarthritis; excluding patients with bilateral procedures).
Fig. 5.
This graph shows the CPR for infection of the BHR prosthesis and three primary conventional THA prostheses with the lowest 10-year CPR for men younger than 65 years (primary diagnosis of osteoarthritis; excluding patients with bilateral procedures).
Major Versus Minor Revisions
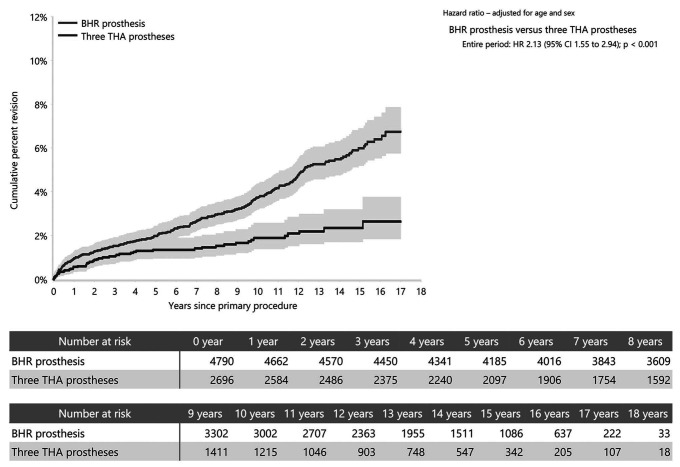
The design of the BHR prosthesis does not enable minor revisions to be performed. Therefore, all revisions in the BHR group were major revisions and these occurred in 4.5% of the primary BHR procedures. Major revision was the most common type of revision for primary conventional THA accounting for 1.7% of all primary THA procedures. The remaining revisions in the THA group were minor and occurred in 0.6% of primary procedures (Table 2). The CPR at 17 years for major revisions was 6.7% (95% CI 5.8 to 7.9) for BHR and 2.6% (95% CI 1.8 to 3.8) for the THA group (HR 2.13 [95% CI 1.55 to 2.94]; p < 0.001) (Fig. 6).
Table 2.
Type of revision of BHR total hip resurfacing and primary conventional THA using the three prosthesis combinations with the lowest 10-year CPR in men younger than 65 years (primary diagnosis of OA, excluding bilateral procedures)
| Type of revision | BHR prosthesis | Three THA prostheses | ||
| Type of revision as a percentage of primary procedures (n = 4790) | Type of revision as a percentage of revision procedures (n = 215) | Type of revision as a percentage of primary procedures (n = 2696) | Type of revision as a percentage of revision procedures (n = 63) | |
| THA (Femoral/acetabular) | 2.9 (138) | 64 (138) | 0.4 (10) | 16 (10) |
| Femoral component | 1.2 (56) | 26 (56) | 0.5 (14) | 22 (14) |
| Acetabular component | 0.2 (10) | 5 (10) | 0.7 (19) | 30 (19) |
| Head/insert | 0.4 (11) | 17 (11) | ||
| Cement spacer | 0.2 (8) | 4 (8) | 0.1 (3) | 5 (3) |
| Head only | 0.1 (3) | 5 (3) | ||
| Removal of prosthesis | 0.1 (3) | 1.4 (3) | 0.0 (1) | 2 (1) |
| Minor components | 0.1 (2) | 3 (2) | ||
| Number of revisions | 4.5 (215) | 100 (215) | 2.3 (63) | 100 (63) |
Fig. 6.
This graph shows the CPR of major revision of the BHR prosthesis and three primary conventional THA prostheses with the lowest 10-year CPR for men younger than 65 years (primary diagnosis of osteoarthritis; excluding patients with bilateral procedures).
Discussion
One justification for the use of the BHR has been that it has a similar or lower revision rate to conventional THA [7, 10, 11, 20, 23, 24, 30]. The comparison of BHR to the entire class of conventional THA does not account for the considerable variation in the revision rate of the many different conventional THA prostheses included in the comparator group. The comparison is of one of the better performing resurfacing devices to the outcome of all conventional total hip prostheses irrespective of performance. This study provides a more relevant and appropriate analysis by comparing the BHR prosthesis with conventional THA prostheses that are known to have lower revision rates. When this comparison is undertaken in the BHR target population then the BHR (> 50 mm femoral head size) has a higher CPR rate compared with the three best conventional THA prostheses.
Limitations
There are several limitations to this study. The main criticism is the potential for selection bias because there may be differences between the patients who have been selected for hip resurfacing arthroplasty compared with those who were selected for THA. The analytical approach taken in this study has reduced the variation in both prosthesis and patient factors compared with other studies. However, it is still likely that patient-specific differences between the two groups remain. Within the resurfacing group there is likely to be a higher proportion of patients who have better general health and are more active. With the large reduction in the use of resurfacing in recent years, the potential difference in the proportion of fitter, more active patients is likely to have decreased. Despite this, it remains a possible explanation for the higher revision rate of the BHR in that a higher proportion of more active patients could potentially increase the incidence of wear-related complications. A major justification for the use of metal-on-metal bearings was, however, the theoretical advantage of increased wear resistance. The lower incidence of revision in the conventional THA group potentially indicates that this may not be the case.
Conversely, it is more likely that patients with poor-quality bone, more severe disease, and greater deformity are less likely to have been selected for a procedure using the BHR. This is because of the associated technical difficulties. The AOANJRR is not able to identify these differences and therefore has not taken them into account. They are likely to be associated with an increased revision risk in the conventional THA group.
Although the analysis used in this study has reduced bias by limiting the analysis to the target population and reducing the number of comparator conventional THA prostheses, it has not been able to prevent all potential confounding. The AOANJRR considers several analytical approaches other than stratification and age adjustment to address this, including propensity score matching and instrument variable analysis. It was decided not to proceed with either of these approaches. To have effectively undertaken propensity score analysis would have required the inclusion of additional conventional THA prostheses, increasing the likelihood of prosthesis-specific confounding and at the same time substantially reducing the sample size. In addition, because the AOANJRR does not collect all relevant data elements, it is still not possible to match on some known potentially important variables. Similarly, it was not possible to undertake an instrument variable analysis because this is most effective with a large volume of procedures and patient selection bias still needs to be addressed. The tight stratification used limited the number of procedures included in the study. In addition, resurfacing was undertaken preferentially by high-volume hip surgeons This generally results in lower revision rates which are not reflected in the BHR revision rates reported in this study.
A further limitation of this study is that the comparative outcome is limited to revision. The AOANJRR has only recently commenced collection of functional and patient-reported outcome measures. As this data was not collected during the period of this study, it was not possible to compare the results of this study to those that have reported improved patient-reported outcome measures with the BHR [15, 26]. The issue of whether a BHR provides a better functional result and/or a better result from the patient perspective has not been addressed by this study.
When comparing the two groups, it is also important to contrast the reasons for revision. The BHR has a higher rate of revision for aseptic loosening, fracture, metal-related pathology and lysis. In this study, metal-related pathology is a mode of failure that is unique to the BHR when compared with the three selected conventional THA prostheses. Fracture is a problem known to be associated with resurfacing. Revisions for aseptic loosening and lysis reported for the BHR are due to an adverse tissue response to metal-related particles and/or metal ions. It appears that the reasons for an increased revision rate is very much related to the design and bearing surface of the BHR.
Revision Rate
We found the overall revision rate to be considerably higher for the BHR group than for the THA group after 2.5 years. There are a number of cohort studies that report BHR survivorship ranging from 89% at 13 years to 98% at 10 years (Table 3) [1, 6, 10, 11, 14, 16, 17, 21, 22, 25, 29, 34], but there are no published studies that directly compare the revision rates of the BHR with a THA in younger males with OA. Ideally, a prospective study would randomize a series of patients to have either a BHR or a THA to answer our key question: Which implant offers the best survivorship in this group? In the absence of such studies, this joint registry analysis provides the best-available data.
Table 3.
Mid- to longer-term studies of BHR in younger patients
| Study | Number of BHR | Mean age (years) | Mean follow-up (years) | Survivorship |
| Current study | 4790 | Males 52 | 19 | 93.3% 17 years |
| Frew et al. [14] | 155 | Males 47 | 8.2 | 88.8% 13 years |
| Azam et al. [6] | 244 | Males 58 Females 55 |
12 | Males 95.4% Females 89.8% |
| Halawi et al. [16] | 442 | 48 | 6 | Not documented |
| Oak et al. [25] | 541 | 53 | 6.2 | 98.8% 5 years |
| Rahman et al. [29] | 329 | 56 | 6.6 | 96.5% 9 years |
| Madhu et al. [21] | 117 | 54 | 7 | 91.5% 7 years |
| Coulter et al. [10] | 230 | 52 | 10.4 | Males 97.5% Females 89.1% 10 years |
| Holland et al. [17] | 100 | 51 | 9.5 | Males 94.6% Females 84.6% 10 years |
BHR = Birmingham Hip Resurfacing.
Revision Diagnoses
There are substantial differences between the design and implantation of the BHR prosthesis and THA prostheses. It is therefore no surprise that there are differences in the modes of failure of these two types of prostheses. When considering the reasons for revision, it is apparent that loosening, metal-related pathology, lysis, and osteonecrosis are greater problems when the BHR is used than when a conventional THA prosthesis is used (Table 2). Loosening is the most common reason for revision for hip replacement in the AOANJRR. It was apparent in higher numbers in the BHR group and the rate appears to be increasing with time. The later increase in revisions due to loosening, metal-related pathology, and lysis are major concerns because these are likely to reflect the metal-on-metal bearing. Also, of concern is that the incidence of these metal particle and metal ion-related problems are increasing with longer follow-up.
Metal-related pathology revisions can be evident in THA prostheses without metal-on-metal bearings. This is due to fretting corrosion (trunnionosis) but it is only rarely reported [12]. Revision for metal-related pathology occurred in 0.7% of the BHR group but was not a reason for revision in the THA group. Metal-related pathology may be the reason loosening and lysis occur more often in the BHR group. Head size is independently associated with revision risk for dislocation. The BHR allows a much larger head size than a THA and therefore revisions for instability in patients with a BHR are uncommon. No BHR patients in our dataset had a revision for dislocation. Revision for dislocation is observed at a higher rate in THA; however, this only occurred in 0.2% of these procedures in our series.
The revision rate for infection appears to be lower for the BHR group. However, the AOANJRR only captures revision procedures that involve component removal or replacement. It is likely that there are BHR infections treated with débridement and implant retention that have not been captured in this dataset. The same procedure for a THA mostly involves exchange of head and liner, which are captured as a minor revision by the registry. Therefore, the AOANJRR cannot provide comparative data on the overall infection rates of the BHR and THA, only the rate of component removal or exchange for this diagnosis.
Major Versus Minor Revisions
Revisions are recorded as major or minor in the registry, but dividing revisions into these two groups is contentious. Some surgeons argue that any revision procedure is a major operation regardless of what the revision entails. We have taken a more nuanced approach to the analysis. In cases of instability, changing a head or liner is mostly a lower-acuity procedure with a shorter operation time and a quicker recovery than procedures that involve removal of the stem or cup. Some of the minor THA revisions will be part of a débridement and implant retention for infection. This is recorded in the registry as a minor component exchange for infection but by its nature, it is a larger operation with commensurate morbidity. The BHR has no removable or replaceable parts so every BHR revision procedure recorded in the AOANJRR is a major revision. In fact, 64% of the BHR revisions involved replacement of the entire prosthesis compared with only 16% of conventional THA revisions. Balanced against this is the fact that the BHR is relatively protected against conditions such as instability that would account for a number of the minor revisions in THA.
Conclusions
We found that males younger than 65 years with OA who underwent BHR had a higher rate of revision after 2.5 years compared with a selected group of three conventional THA with modern bearing surfaces and this difference increased with time. Patients with a BHR should continue to be monitored. The purported functional advantages of the BHR in this relatively young cohort of patients must be balanced against a higher revision rate.
Acknowledgments
We thank the AOANJRR staff, orthopaedic surgeons, hospitals, and patients whose data made this work possible.
Footnotes
Each author certifies that neither he or she, nor any member of his or her immediate family, has funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
This work was performed at the Australian Orthopaedic Association National Joint Replacement Registry, based at the South Australian Health and Medical Research Institute, Adelaide, Australia.
References
- 1.Amstutz HC, Le Duff MJ. Hip resurfacing: a 40-year perspective. HSS J. 2012;8:275-282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.AOANJRR. 2006. Annual Report: Hip & Knee Arthroplasty Adelaide, AOA, 2006. Available at https://aoanjrr.sahmri.com/annual-reports-2006. Accessed June 10, 2019.
- 3.AOANJRR. 2010. Annual Report: Hip & Knee Arthroplasty Adelaide, AOA, 2010. Available at https://aoanjrr.sahmri.com/annual-reports-2010. Accessed June 10, 2019.
- 4.AOANJRR. 2014. Annual Report: Hip & Knee Arthroplasty Adelaide, AOA, 2014. Available at https://aoanjrr.sahmri.com/annual-reports-2014. Accessed June 10, 2019.
- 5.AOANJRR. 2019. Annual Report: Hip, Knee & Shoulder Arthroplasty Adelaide, AOA, 2019. Available at https://aoanjrr.sahmri.com/annual-reports-2019. Accessed November 10, 2019.
- 6.Azam MQ, McMahon S, Hawdon G, Sankineani SR. Survivorship and clinical outcome of Birmingham hip resurfacing: a minimum ten years’ follow-up. Int Orthop. 2016;40:1-7. [DOI] [PubMed] [Google Scholar]
- 7.Braaksma C, Wolterbeek N, Veen RM. Survival, Complications and Outcomes of the Birmingham Hip Resurfacing Compared to Cementless Total Hip Arthroplasty. Int Orthop. 2018;5:896-900. [Google Scholar]
- 8.Clarke MT, Lee PT, Villar RN. Dislocation after total hip replacement in relation to metal-on-metal bearing surfaces. J Bone Joint Surg Br. 2003;85:650-654. [PubMed] [Google Scholar]
- 9.Corten K, MacDonald SJ. Hip resurfacing data from national joint registries: what do they tell us? What do they not tell us? Clin Orthop Relat Res. 2010;468:351-357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Coulter G, Young D, Dalziel R, Shimmin A. Birmingham hip resurfacing at a mean of ten years: results from an independent centre. J Bone Joint Surg Br. 2012;94:315-321. [DOI] [PubMed] [Google Scholar]
- 11.Daniel J, Pradhan C, Ziaee H, Pynsent PB, McMinn DJ. Results of Birmingham hip resurfacing at 12 to 15 years: a single-surgeon series. J Bone Joint Surg Am. 2014;96-B:1298-1306. [DOI] [PubMed] [Google Scholar]
- 12.de Steiger RN, Hatton A, Peng Y, Graves S. What Is the Risk of THA Revision for ARMD in Patients with Non-metal-on-metal Bearings? A Study from the Australian National Joint Replacement Registry. Clin Orthop Relat Res. 2020;478:1244-1253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Della Valle CJ, Nunley RM, Raterman SJ, Barrack RL. Initial American experience with hip resurfacing following FDA approval. Clin Orthop Relat Res. 2009;467:72-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Frew N, Johnson G. Survival of the Birmingham hip resurfacing in young men up to 13 years post-operatively. Acta Orthop Belg. 2017;83:1-2017. [PubMed] [Google Scholar]
- 15.Haddad FS, Konan S, Tahmassebi J. A prospective comparative study of cementless total hip arthroplasty and hip resurfacing in patients under the age of 55 years: a ten-year follow-up. J Bone Joint Surg Am. 2015;97-B:617-622. [DOI] [PubMed] [Google Scholar]
- 16.Halawi MJ, Oak SR, Brigati D, Siggers A, Messner W, Brooks PJ. Birmingham hip resurfacing versus cementless total hip arthroplasty in patients 55 years or younger: A minimum five-year follow-up. J Clin Orthop Trauma. 2017;9:285-288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Holland J, Langton D, Hashmi M. Ten-year clinical, radiological and metal ion analysis of the Birmingham Hip Resurfacing: from a single, non-designer surgeon. J Bone Joint Surg Br. 2012;94:471-476. [DOI] [PubMed] [Google Scholar]
- 18.Issa K, Palich A, Tatevossian T, Kapadia BH, Naziri Q, Mont MA. The outcomes of hip resurfacing compared to standard primary total hip arthroplasty in Men. BMC Musculoskelet Disord. 2013;14:161-167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Johanson P-E, Fenstad AM, Furnes O, Garellick G, Havelin LI, Overgaard S, Pedersen AB, Kärrholm J. Inferior outcome after hip resurfacing arthroplasty than after conventional arthroplasty: evidence from the Nordic Arthroplasty Register Association (NARA) database, 1995 to 2007. Acta Orthop. 2010;81:535-541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jonas SC, Whitehouse MR, Bick S, Bannister GC, Baker RP. An 18-year comparison of hybrid total hip replacement and Birmingham hip resurfacing in active young patients. HIP Int. 2019;29:630-637. [DOI] [PubMed] [Google Scholar]
- 21.Madhu TS, Akula MR, Raman RN, Sharma HK, Johnson VG. The Birmingham hip resurfacing prosthesis: an independent single surgeon's experience at 7-year follow-up. J Arthroplasty. 2011;26:1-8. [DOI] [PubMed] [Google Scholar]
- 22.Matharu G, McBryde C, Pynsent W, Pynsent P, Treacy R. The outcome of the Birmingham Hip Resurfacing in patients aged< 50 years up to 14 years post-operatively. J Bone Joint Surg Am. 2013;95:1172-1177. [DOI] [PubMed] [Google Scholar]
- 23.McMinn D, Daniel J, Ziaee H, Pradhan C. Indications and results of hip resurfacing. Int Orthop. 2011;35:231-237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McMinn D, Treacy R, Lin K, Pynsent P. Metal on metal surface replacement of the hip. Experience of the McMinn prothesis. Clin Orthop Relat Res. 1996:S89-98. [DOI] [PubMed] [Google Scholar]
- 25.Oak SR, Strnad GJ, O'Rourke C, Higuera CA, Spindler KP, Brooks PJ. Mid-Term Results and Predictors of Patient-Reported Outcomes of Birmingham Hip Resurfacing. J Arthroplasty. 2017;32:110-118. [DOI] [PubMed] [Google Scholar]
- 26.Ortiz-Declet VR, Iacobelli DA, Yuen LC, Perets I, Chen AW, Domb BG. Birmingham hip resurfacing vs total hip arthroplasty: a matched-pair comparison of clinical outcomes. J Arthroplasty. 2017;32:3647-3651. [DOI] [PubMed] [Google Scholar]
- 27.Pitto RP. CORR Insights (R): Hip resurfacing does not improve proprioception compared with THA. Clin Orthop Relat Res. 2014;472:562-563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Prosser GH, Yates PJ, Wood DJ, Graves SE, de Steiger RN, Miller LN. Outcome of primary resurfacing hip replacement: Evaluation of risk factors for early revision: 12,093 replacements from the Australian Joint Registry. Acta Orthop. 2010;81:66-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rahman L, Muirhead-Allwood SK, Alkinj M. What is the midterm survivorship and function after hip resurfacing? Clin Orthop Relat Res. 2010;468:3221-3227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Seppanen M, Makela K, Virolainen P, Remes V, Pulkkinen P, Eskelinen A. Hip resurfacing arthroplasty: short-term survivorship of 4,401 hips from the Finnish Arthroplasty Register. Acta Orthop. 2012;83:207-213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Smith & Nephew. Statement regarding BHR System. Smith & Nephew, 2015. Available at https://www.smith-nephew.com/news-and-media/media-releases/news/statement-regarding-bhr-system/. Accessed June 20, 2020. [Google Scholar]
- 32.Smith AJ, Dieppe P, Howard PW, Blom AW. Failure rates of metal-on-metal hip resurfacings: analysis of data from the National Joint Registry for England and Wales. Lancet. 2012;380:1759-1766. [DOI] [PubMed] [Google Scholar]
- 33.Therapeutic Goods Administration (TGA) Alert: Birmingham Hip Resurfacing system.Hazard alert - additional warnings for use in certain patient groups. TGA, Department of Health, Australian Government, 2015. Available at https://www.tga.gov.au/alert/birmingham-hip-resurfacing-system. Accessed June 20, 2020. [Google Scholar]
- 34.Treacy RB, McBryde CW, Shears E, Pynsent PB. Birmingham hip resurfacing: a minimum follow-up of ten years. J Bone Joint Surg Br. 2011;93:27-33. [DOI] [PubMed] [Google Scholar]