Background:
To detail the early experience with and results of a transfeminine (TF) genital reconstruction at an established plastic surgery practice in Western New York.
Methods:
Between June 2016 and June 2019, 30 patients underwent penile inversion vaginoplasty for TF gender reassignment. All patients fulfilled World Professional Association for Transgender Health and NY State criteria for reassignment surgery. All surgeries were carried out at a large, government-owned tertiary care center.
Results:
There were 30 patients in this retrospective study, with a mean age of 37 years (SD 5.4) and a mean body mass index of 27.3 kg/m2 (SD 3.2 kg/m2). Nineteen patients never smoked, 4 were former smokers, and 7 were current smokers. Primary surgery was an orchiectomy and modified single-stage penile inversion vaginoplasty. Mean operative time was 6.0 hours. Mean initial hospital stay was 8.2 days. Three of the 30 (10%) patients required transfusion. There were 6 (20%) complications. Three complications (10%) required reoperation: 1 patient for wound dehiscence on postoperative day 7, 1 for rectal perforation identified on postoperative day 10, and 1 for urethrovaginal fistula. All complications were addressed without sequalae. Twenty of the 30 (66%) patients have undergone revision surgery. Indications for revision were prolapse correction/deepening, labiaplasty, clitoral hood construction/revision, meatal asymmetry, urinary fistula repair, and posterior vaginal flap revision. Twenty-one of 28 (75%) revisions were outpatient surgeries. There were no complications from these procedures. Overall satisfaction via survey was 92% (24 respondents).
Conclusions:
TF gender reassignment is a novel, challenging set of procedures for the specialty of plastic surgery. With appropriate consideration and technique, penile inversion vaginoplasty is a safe, effective means of achieving this goal.
INTRODUCTION
Over the past several years, gender affirmation surgery (formally described as gender dysphoria or the mismatch between a person’s gender identity and sexual phenotype) has proliferated in the United States. The surgical management of the trans population represents a significant challenge in the field of plastic surgery.1 After entering the spectrum of covered care under the Affordable Care Act in 2010, coverage for healthcare to meet the needs of the transgender population in New York state was formalized and protected in early 2015. The leading organization dedicated to this field is the World Professional Association for Transgender Health (WPATH), which publishes standards of care for transgender medical care.2
The term “gender affirmation surgery” is used to describe a wide variety of cosmetic and noncosmetic procedures related to the management of transgender individuals. Within this subset of procedures is genital reassignment. It has been well described that vaginoplasty, for most trans women, is associated with significantly improved quality of life and sexual satisfaction.3–5 The goals of most methods of gender reassignment vaginoplasty are to create a vaginal vault amenable to penetration, provide somatic and sexual sensation to the perineum and neovagina, maintain urinary function, and create an esthetically appropriate external genitalia.
The most common procedure to achieve these goals for transfeminine (TF) genital reassignment is penile inversion vaginoplasty.6–16 Alternative procedures, including sigmoid vaginoplasty, are described in the literature. However, these are generally recognized as inferior to penile inversion.17,18 In the literature, the overall technical and subjective success rate of penile inversion vaginoplasty is 80%–90%. Complication rate of penile inversion is generally regarded at approximately 20%–30%, while complication rate of alternative procedures is typically 35%–60%.17–22 Penile inversion is preferred due to the neovagina vault being mostly hairless and partially lubricated via urethral mucosa. The most commonly cited shortfall of this reconstruction method is that the neovaginal depth is often insufficient and may require revisions with either enteric mucosa or a full thickness skin graft.10,14 While there remain indications for alternative procedures, primarily based on the amount of donor tissue available, penile inversion is the most widely preformed means of TF genital affirmation in the United States. Consideration must also be given to complications, most significantly, rectovaginal fistula, urinary retention or urethral stenosis, wound dehiscence, or neovaginal prolapse.19–22
TF gender-affirming vaginoplasty was first performed at our institution in 2016. All patients met WPATH standards. This article seeks to characterize our initial experience with this patient population and surgical procedure in a previously unserved area.
METHODS
Patient Selection
Between 2016 and 2019, 30 patients underwent penile inversion vaginoplasty for gender affirmation at Erie County Medical Center in Buffalo, N.Y. Data were collected from a prospectively maintained database for all patients undergoing penile inversion vaginoplasty at this institution. With institutional review board approval, data were extracted from records available within the electronic medical record and from subjective patient feedback. All patients gave informed consent for their deidentified information to be included. All patients met initial WPATH guidelines before being seen in clinic. Patients were required to have lived as their chosen gender for at least 1 year before initial preoperative visit and to have been on hormone therapy uninterrupted for at least a year before surgery.
Patient Follow-up
All patients were seen in the plastic surgery clinic preoperatively. At this time, surgical options and needs were discussed with the patient. If not already obtained, clinical assessments from Psychiatry and Psychology department were obtained. A second preoperative visit was carried out in all patients, following authorization for surgical scheduling and planning. Postoperatively, all patients were seen in clinic within 1 week of hospital discharge and then subsequently on a staggered follow-up regimen weekly, eventually continuing to a 3-month regular follow-up. One patient moved out of the area; the rest continued to be seen in clinic.
Surgical Approach
The surgical procedure for genital reassignment is a single-stage bilateral orchiectomy with subsequent penile inversion vaginoplasty. All surgeries were performed by 1 of 2 attending surgeons in the Department of Head and Neck/Plastic Surgery at Erie County Medical Center in Buffalo. Both surgeons (Dr. Burke and Dr. Loree) are board-certified plastic surgeons with a combined 45 years’ experience in clinical practice.
Intraoperatively, all patients underwent induction of general anesthesia and endotracheal intubation, with administration of standard intraoperative prophylactic antibiotics. Patients were positioned in the dorsal lithotomy position and had their perineum prepared and draped in the usual fashion. A Foley catheter was placed within the sterile field.
Initial incision was an “inverted-V” with apex midline, approximately halfway along the scrotum, leaving a triangle of vascularized skin with the base just anterior to the anus. This scrotal flap will eventually supplement the penile skin and urethral mucosa to line the neovagina. The scrotal flap will form the posterior vaginal wall and portions of the lateral walls (Fig. 1). At this time, dissection along the plane separating the rectum and urethra/prostate/bladder is carried out until the desired anchoring distance for the neovagina is exposed, for a depth of approximately 15 cm. This dissection is carried out above Denonvilliers’ fasica. The remaining scrotal skin is divided along the midline and dissected off the testicles, and bilateral orchiectomy with ligation of the vas deferens at the external inguinal ring is carried out.
Fig. 1.
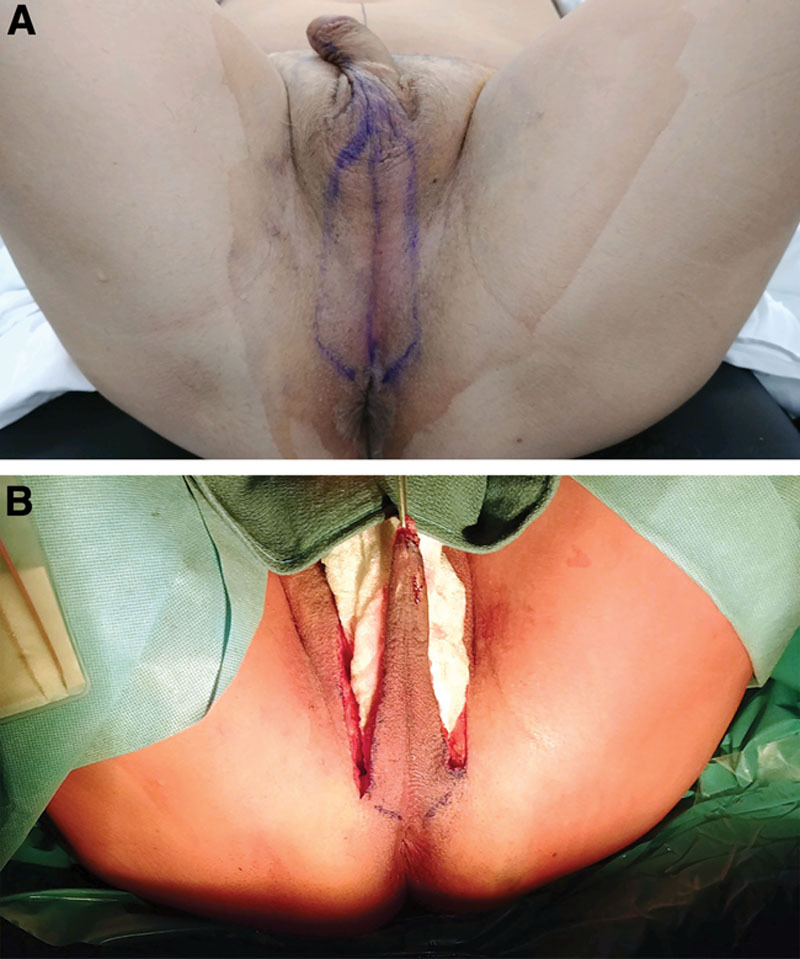
Operative photographs. A, Preoperative markings demonstrating dissection borders for posterior wall vascularized scrotal flap. B, Intraoperative dissection of vascularized scrotal flap before inset into neovaginal vault.
After this initial phase of the operation, attention is directed to the penis, which undergoes subsequent disassembly and dissection. The penile skin is divided circumferentially just below the glans and using sharp and blunt dissection is separated from the corpora and urethra. The ventral neurovascular bundle is exposed and preserved attached to the penile glans. Resection of the corpus cavernosum and spongiosum is performed with ligation at the level of the pubic bone. The penile glans is preserved, with its base de-epithelialized in preparation for creation of the clitoris. Suprapubic connective tissue dissection is then carried out with inferior advancement and fixation of these tissues to the pubic fascia. The penile skin is used to create the lateral vaginal walls, clitoral hood, and labia minora, while the penile urethra is divided and used to create the anterior vaginal wall.
Following preparation of the donor penile tissue, clitoral hood creation with clitoral inset is carried out, with the penile glans brought through a small incision through the midline of the inverted penile skin at the level of the pubic bone at the equivalent cis-female anatomic position. Next the penile urethra is brought out through a small incision in the midline just posterior to the neo-clitoris. The penile urethra is divided longitudinally and inset into a longitudinal division of the inverted penile skin. The V flap is then inset into a longitudinal division of the inverted penile skin to construct the posterior vaginal wall. The completed neovaginal vault lining is then secured into the previously dissected space between the rectum and the urethra/prostate/bladder. Two additional, symmetric incisions are made from the base of the inverted-V flap incisions directed toward the midline just anterior to the anal opening, into which the excess scrotal skin (preserved after orchiectomy) is inset to create the labia majora. Two Jackson-Pratt drains are placed intraoperatively, one suprapubic and one in the neovaginal vault. A xeroform gauze pack is inserted into the neovagina until there is no laxity in the wall of the neovagina and dressed with an antibiotic ointment. The labia majora are then sutured closed over the packing (to be removed postoperatively at packing removal) (Fig. 2). Above this dressing, another dressing is applied. Dressings and Foley catheter are removed on postoperative days 4–7.
Fig. 2.

Final result of penile inversion vaginoplasty.
Postoperatively, all patients receive antibiotics coverage. Pain management is achieved using intraoperative liposomal bupivacaine injection and postoperative analgesia as needed. Drains are left to suction postoperatively and removed when they achieve minimal drainage. Patients are discharged from the hospital when in stable condition without drains in place. The packing is removed in the office 7–21 days postoperatively.
Patient Data Collection
Patient-specific factors recorded for all patients included age, time living as a female, duration on hormone therapy, body mass index, tobacco use, HIV status, operative time, postoperative hospital stay, hemoglobin/hematocrit preoperatively and postoperatively, transfusion, complication rate, revision rate, and subjective patient satisfaction.
Subjective satisfaction feedback was obtained using a standard questionnaire (Appendix 1) before each 3-month follow-up. These data were not formally collected until 6-month follow-up after primary surgery to allow for maturation of the surgical result. Patients were called before clinic visit, and questions were focused on a patient’s overall satisfaction with surgery, satisfaction with the esthetic appearance of the neovagina, ability to successfully orgasm regularly, and whether they were undertaking penetrative intercourse. Secondary questions were focused on patient’s psychosocial and urinary functioning postoperatively.
Definition of Complications
Patient-specific complications were recorded prospectively. Recorded complications include wound dehiscence, rectal perforation, hospital-acquired infections, urinary tract breakdown, and seroma. Further stratification of complications into those requiring early reoperation or not was also maintained. Complications were assessed at the time of first presentation. Reason(s) for revision surgery (most frequently to address neovaginal depth or external esthetic appearance) were also recorded in the database.
Statistical Analysis
Demographic characteristics were summarized using frequencies of categorical data and mean of continuous data with range. Due to series size and relatively few numbers of complications, statistical analysis regarding operative risk factors was not carried out.
RESULTS
Demographics
Between June 2016 and August 2019, 30 patients underwent penile inversion vaginoplasty. All patients underwent surgery as described in the methods. Patient demographics are described in Table 1. Mean time on hormone therapy was 6.1 years. There were 7 (23%) active smokers at the time of initial preoperative visit. All quit smoking at least 1 month before surgery. All patients met New York state and WPATH criteria for eligibility for the surgery.
Table 1.
Patient Demographics
| Characteristic | Mean (median) | Range |
|---|---|---|
| Age | 37 (33) | 21–64 |
| Hormone therapy, y | 6.1 (5.3) | 2–27 |
| BMI, kg/m2 | 27.3 (26.4) | 16.1–47.0 |
| Tobacco use, n | ||
| Never | 19 | |
| Former | 4 | One, 1 y since cessation; three, 10+ y |
| Current | 7 | All quit 1–4 months before surgery |
| HIV status | ||
| Positive | 4 | 13.33% |
| Negative | 26 | 86.67% |
BMI, body mass index.
Primary Intraoperative and Short-term Postoperative Results
Primary single-stage penile inversion vaginoplasty was technically successful in all 30 cases (100%). Mean operative time was 6 hours (3.8–7.8 hours), and mean postoperative hospital stay was 8.2 days (5–20 days). Intraoperative blood loss was recorded using hemoglobin/hematocrit pre- and postoperatively. Mean hemoglobin/hematocrit recorded preoperatively was 13.9/41.1 (11.6/35.1–16.3/47.5) and postoperatively was 10.0/29.9 (7.6/22.8–12.4/37.4). This equated to a mean blood loss of 28% of blood volume. Intraoperative transfusion of 2 units packed red blood cells was carried out in 1 patient (3.33%). Two (6.67%) patients required postoperative transfusion of packed red blood cells for symptomatic anemia.
There were 5 (16.67%) perioperative complications associated with primary surgery. There were 2 (6.67%) rectal perforations, one identified during primary surgery and repaired intraoperatively and one that required early reoperation for primary closure on postoperative day 10. There was 1 wound dehiscence, 1 seroma, and 1 hospital-acquired C. Difficile infection was observed during initial postoperative hospital stay. All patients were successfully managed without sequalae. Further details can be found in Table 2. There were no instances of urinary retention or dysfunction and no other infections reported in the immediate postoperative period.
Table 2.
Short-term Complications
| Complication | Management | Treatment Outcome/Sequalae |
|---|---|---|
| Labial wound dehiscence | Primary repair POD No. 7 | Successful repair, no sequalae |
| Rectal perforation | Primary closure POD No. 10 | Successful repair, no sequalae |
| Rectal perforation (dx during primary surgery) | Intraoperative primary repair | Successful repair, no sequalae |
| Pelvic floor seroma | IR-guided drain placement | Successful treatment, no sequalae |
| Clostridium difficile colitis | Outpatient antibiotic therapy | Successful treatment, no sequalae |
POD, postoperative day.
Long-term Complications and Revision Surgery
All patients were followed until the current date. Mean follow-up duration was 15.2 months (SD 9.9 months). Complete follow-up information was available on all patients upon database review. There was one late complication: formation of urethrovaginal fistula 3.2 months after primary surgery, which was repaired during elective revision without sequalae.
In total, of the 23 patients >6 months in follow-up after primary surgery, 20 (87%) patients have undergone revision surgery. There have been 28 total revision surgeries, with 13/20 (65%) patients undergoing 1 additional surgery, 6/20 (30%) patients undergoing 2 surgeries, and 1 patient who has had 3 surgeries. Indications and timing for revision surgery can be found in Table 3. The most common indication for revision surgery was deepening followed by labiaplasty/labial reduction. The majority of labiaplasties were performed to improve esthetic outcomes. There have been no complications related to revision surgery.
Table 3.
Revision Surgery Details
| Characteristic | N | Percent |
|---|---|---|
| Total number of patients with revisions | 20 | 20/30, 66.67% |
| 1 | 13 | 13/30, 46.33% |
| 2 | 6 | 6/30, 20% |
| 3 | 1 | 1/30, 3.33% |
| Too early to evaluate | 7 | 7/30, 23.33% |
| Total number of revision surgeries | 28 | NA |
| Hospital stay for revision | ||
| Same day surgery | 21 | 21/28, 75% |
| 1 d | 2 | 2/28, 7.1% |
| 2 d | 2 | 2/28, 7.1% |
| 3 d | 3 | 3/28, 10.7% |
| Indication for revision | ||
| Vaginal deepening | 13 | 13/28, 46.4% |
| Labiaplasty/reduction | 12 | 12/28, 42.9% |
| Meatal asymmetry repair | 1 | 1/28, 3.6% |
| Urinary fistula repair | 1 | 1/28, 3.6% |
| Posterior vaginal wall revision | 1 | 1/28, 3.6% |
Subjective Feedback
Of the 25 patients eligible to provide subjective feedback, 24 (96%) have provided response. When asked their overall satisfaction with surgery, 22/24 (92%) said that they were satisfied with their results. Additionally, 22/24 (92%) reported having successfully achieved orgasm with their neovagina, and 22/24 (92%) reported satisfaction with the esthetic result. Twenty-two of 24 patients reported the potential/having successfully had penetrative intercourse, with breakdown as follows: 5/24 (21%) with male partner without issue, 5/24 (21%) with male partner with minor difficulty (issues: depth, dryness, or discomfort), 7/24 (29.2%) using largest dilator without male partner, 5/24 (21%) not attempting due to disinterest, and 2/24 (8.3%) unable due to depth or issue. Details on patients who did not respond positively to all questions surveyed can be found in Table 4. Overall subjective success across satisfaction, ability to achieve orgasm, and penetrative intercourse was 80% (20/25).
Table 4.
Subjective Failures via Survey
| Overall Satisfaction | Ability to Orgasm | Ability to Have Penetrative Intercourse | Total Success | |
|---|---|---|---|---|
| Patient 1 | Dissatisfied | Yes | Unable | 1/3 |
| Patient 2 | Dissastisfied | Yes | Unable | 1/3 |
| Patient 3 | Satisfied | No | Yes | 2/3 |
| Patient 4 | Satisfied | No | No attempt | 1/3 |
| Patient 5 | No answer | No answer | No answer | NA |
| Failures | 3/5 | 3/5 | 3/5 |
DISCUSSION
This series represents the initial experience of our practice in TF genital reassignment surgery for gender affirmation using penile inversion vaginoplasty. Although performed by surgeons with an extensive experience in reconstructive plastic surgery, this cohort represented the first set of procedures for genital reassignment preformed in Buffalo, N.Y. Both surgeons represented within this cohort used the operative technique as described in the Methods, and their results were consistent across all measured statistics.
A few general limitations of this study are that the patient satisfaction survey used has not been formally validated and does not use a numeric scale (eg, Likert scale). Additionally, due to the setting of this study, this is a relatively small series of patients without an internal control to compare complication and patient outcomes data between surgical techniques. However, given the irreversibility of gender-affirming surgeries, a comparison series would be difficult to accrue without undo harm onto one of the arms of a study. A possible workaround to this issue would be to combine the experiences of several institutions in this procedure to better understand the general differences between techniques.
Across all patients in this study, there were 6 complications recorded, leading to an overall complication rate of 20%. The most concerning complications of penile inversion vaginoplasty were rectal perforation and rectovaginal fistula. The rate of rectal perforation in this study is 6.67%, which is higher than that presented elsewhere (between 2% and 5%).7–11,19–22 However, there were only 2 instances of rectal perforation, which were within the first 10 patients operated on. There have been no further perforations since, and with accrual of further data, the rate of rectovaginal perforation will likely decline to be consistent with the literature. With appropriate attention, rectal perforation/fistula can be identified and repaired without major sequalae, as in our cohort. Other complications, including wound dehiscence, infection, and seroma, were successfully managed in the perioperative period, whose occurrences are somewhat infrequent.
Most interestingly, however, was the relative lack of significant urinary complications. There was only 1 case (3.33%) of urethrovaginal fistula and no cases of urinary retention or urethral stricture. Potential causes for this are as follows: all patients received prophylactic antibiotics in the perioperative period, Foley catheters were removed within 5 days postoperatively, and manipulation of the internal urethral anatomy was avoided intraoperatively.
Early in the series, the neovaginal packing was removed after approximately 7 days as traditionally described in the literature.7–11 As experience has increased, the packing has been left in longer. This has led to a better maintenance of neovaginal depth and a lower incidence of prolapse. There has been no corollary increase in the perioperative infection rate. This is likely secondary to the routine use of peri- and postoperative antibiotics in the initial phases of wound healing. Additionally, the packing used is made of bismuth impregnated gauze, which further reduces the likelihood of bacterial colonization.
Of technical concern within this cohort, however, was the need for revision surgery to improve neovaginal depth. Of the 28 elective revision surgeries in this cohort, 13/28 (46%) were carried out to improve depth. The overall rate of revision in eligible patients was 87%, largely secondary to this issue. Possible causes for this effect are that patients underwent penile inversion vaginoplasty regardless of penile length, used as a surgical selection criterion in the literature.7,9–12,14,17 Based on the literature and our experience, intraoperative packing of the neovagina and regular and aggressive postoperative dilation regimens are found to be strongly correlated with optimal neovaginal depth and vaginal diameter. Patients are encouraged to dilate multiple times daily for several months.
Additionally, skin grafting is not carried out in primary surgery. As described in the methods section, a vascularized flap from the midportion of the scrotum is used to augment the penile skin and urethral mucosa for neovaginal lining. We believe that this technique is superior to skin grafting. The flap is well vascularized and is less vulnerable to necrosis and possibly contracture. In this series, there were no instances of neovaginal necrosis, as opposed to rates of up to 5% in the literature.9
Consistent with the available literature, comorbid conditions and obesity does not appear to correlate with complication rate.11,14–16,19,20 Although formal statistical analysis was not able to be carried out in a cohort this size, body mass index, smoking status, HIV status, and comorbid disease did not show a clear risk for complication.
Additionally, it appears that within this initial cohort, subjective satisfaction and success was achieved at a rate consistent with that published in the literature.3–20 Ninety-two percent of patient queried reported achieving overall satisfaction, sexual satisfaction, penetrative intercourse, and esthetic satisfaction. Eighty percent (20/25) of queried patients had positive responses across all categories. This is consistent with data available in the literature and provides further evidence that with appropriate training and surgical background, TF gender affirmation surgery is a viable addition to a plastic surgeon’s practice. A caveat to this statement, however, is that this study was carried out in a tertiary care hospital with a full complement of specialty services.
CONCLUSIONS
TF gender reassignment surgery is a challenging set of procedures for the specialty of plastic surgery. With appropriate consideration and technique, penile inversion vaginoplasty is a safe and effective means of achieving an important affirmation goal for transgender women. Upon review of our initial experience with TF surgery in an established reconstructive plastic surgery practice at a tertiary care hospital in Buffalo, NY, penile inversion vaginoplasty has been successfully and safely incorporated into the range of offered procedures. Although clinical support and appropriate facilities are required to undertake gender affirmation surgery, TF gender-confirming surgery can be a viable inclusion into the scope of reconstructive plastic surgery at a larger scale.
APPENDIX
Item 1: Subjective Feedback Questionnaire
All patients were contacted to respond to the questionnaire via phone call; after obtaining informed consent for response to be recorded, patients were asked the following questions with their responses recorded into the database
Questions were open ended; patient response was preserved for internal quality improvement
Are you satisfied with your overall result, if not, why?
Are you satisfied with the external appearance of your vagina, if not, why?
Are you able to attain orgasm? With a partner or on your own?
Have you had intercourse using your neovagina? If so, penetrative or not? If not, why?
Are there any issues with your neovagina we should be aware of?
Footnotes
Published online 21 May 2020.
Presented at Plastic Surgery The Meeting (ASPS) 2019, September 20-23, 2019, San Diego, CA.
Disclosure: The authors have no financial interest to declare in relation to the content of this article.
REFERENCES
- 1.American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders (DSM-5). 20135th ed Arlington, VA: American Psychiatric Association; [Google Scholar]
- 2.WPATH. World Professional Association for Transgender Health (WPATH) Standards of Care Version 7. https://www.wpath.org/publications/soc. Accessed September 1, 2019.
- 3.De Cuypere G, T’Sjoen G, Beerten R, et al. Sexual and physical health after sex reassignment surgery. Arch Sex Behav. 2005;34:679–690. [DOI] [PubMed] [Google Scholar]
- 4.Ainsworth TA, Spiegel JH.Quality of life of individuals with and without facial feminization surgery or gender reassignment surgery. Qual Life Res. 2010;19:1019–1024. [DOI] [PubMed] [Google Scholar]
- 5.Rolle L, Ceruti C, Timpano A, et al. Trombetta C, Liguori G, Bertolotto M.Quality of life after sexual reassignment surgery. In: Management of Gender Dysphoria: A Multidisciplinary Approach. 2015:New York, N.Y.: Springer; 193–199. [Google Scholar]
- 6.Perovic SV, Stanojevic DS, Djordjevic ML.Vaginoplasty in male transsexuals using penile skin and a urethral flap. BJU Int. 2000;86:843–850. [DOI] [PubMed] [Google Scholar]
- 7.Krege S, Bex A, Lümmen G, et al. Male-to-female transsexualism: a technique, results and long-term follow-up in 66 patients. BJU Int. 2001;88:396–402. [DOI] [PubMed] [Google Scholar]
- 8.Goddard JC, Vickery RM, Qureshi A, et al. Feminizing genitoplasty in adult transsexuals: early and long-term surgical results. BJU Int. 2007;100:607–613. [DOI] [PubMed] [Google Scholar]
- 9.Horbach SE, Bouman MB, Smit JM, et al. Outcome of vaginoplasty in male-to-female transgenders: a systematic review of surgical techniques. J Sex Med. 2015;12:1499–1512. [DOI] [PubMed] [Google Scholar]
- 10.Buncamper ME, van der Sluis WB, van der Pas RS, et al. Surgical outcome after penile inversion vaginoplasty: a retrospective study of 475 transgender women. Plast Reconstr Surg. 2016;138:999–1007. [DOI] [PubMed] [Google Scholar]
- 11.Neto RR, Hintz F, Krege S, et al. Gender reassignment surgery—a 13 year review of surgical outcomes. Int Braz J Urol. 2017;38:97–107. [DOI] [PubMed] [Google Scholar]
- 12.Opsomer D, Gast KM, Ramaut L, et al. Creation of clitoral hood and labia minora in penile inversion vaginoplasty in circumcised and uncircumcised transwomen. Plast Reconstr Surg. 2018;142:729e–733e. [DOI] [PubMed] [Google Scholar]
- 13.Salim A, Poh M.Gender-affirming penile inversion vaginoplasty. Clin Plast Surg. 2018;45:343–350. [DOI] [PubMed] [Google Scholar]
- 14.Levy JA, Edwards DC, Cutruzzula-Dreher P, et al. Male-to-female gender reassignment surgery: an institutional analysis of outcomes, short-term complications, and risk factors for 240 patients undergoing penile-inversion vaginoplasty. Urology. 2019;00:e1–e6. [DOI] [PubMed] [Google Scholar]
- 15.Massie JP, Morrison SD, Van Maasdam J, et al. Predictors of patient satisfaction and postoperative complications in penile inversion vaginoplasty. Plast Reconstr Surg. 2018;141:911e–921e. [DOI] [PubMed] [Google Scholar]
- 16.Ives GC, Fein LA, Finch L, et al. Evaluation of BMI as a risk factor for complications following gender-affirming penile inversion vaginoplasty. Plast Reconstr Surg Glob Open. 2019;7:e2097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bouman MB, van der Sluis WB, Buncamper ME, et al. Primary total laparoscopic sigmoid vaginoplasty in transgender women with penoscrotal hypoplasia: a prospective cohort study of surgical outcomes and follow-up of 42 patients. Plast Reconstr Surg. 2016;138:614e–623e. [DOI] [PubMed] [Google Scholar]
- 18.Salgado CJ, Nugent A, Kuhn J, et al. Primary sigmoid vaginoplasty in transwomen: technique and outcomes. BioMed Res Int. 2018;4907208:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cristofari S, Bertrand B, Leuzzi S, et al. Postoperative complications of male to female sex reassignment surgery: a 10-year French retrospective study. Ann Chir Plast Esthet. 2019;64:24–32. [DOI] [PubMed] [Google Scholar]
- 20.Gaither TW, Awad MA, Osterberg EC, et al. Postoperative complications following primary penile inversion vaginoplasty among 330 male-to-female transgender patients. J Urol. 2018;199:760–765. [DOI] [PubMed] [Google Scholar]
- 21.Shoureshi P, Dugi D., III.Penile inversion vaginoplasty technique. Urol Clin North Am. 2019;46:511–525. [DOI] [PubMed] [Google Scholar]
- 22.Dy GW, Sun J, Granieri MA, et al. Reconstructive management pearls for the transgender patient. Curr Urol Rep. 2018;19:36. [DOI] [PubMed] [Google Scholar]


