Background:
The Institute of Medicine defines health literacy as the degree to which individuals have the capacity to obtain, process, and understand basic health information. Low health literacy is at a crisis level in the United States. Health literacy is a stronger predictor of a person’s health than age, income, employment status, education level, and race. In the plastic surgery literature to date, there is no study that evaluates health communication between plastic surgery patients and providers. This study also aims to establish the readability of the American Society of Plastic Surgeons informed consent forms.
Methods:
A survey instrument was designed to assess health literacy of plastic surgery patient and health communication competencies of providers. The Readability Calculator and Hemingway Editor were used to determine the readability of a sample of the American Society of Plastic Surgeons informed consent forms.
Results:
Twenty-one percent of patients did not complete high school. Fifty-one percent of patients agreed that better communication with their provider would improve their health. Seventy-six percent of providers agreed that they have difficulty communicating with patients with different cultural backgrounds; 29% of providers stated that they offered patients low-literacy educational material. The average readability of the informed consents distributed to plastic surgery patients is above 12th grade.
Conclusions:
This study identifies the gap in communication between plastic surgery patients and providers in a county hospital setting. Failure to take appropriate actions toward eliminating inherent barriers in health communication is costly to both the hospital and the patients. These findings also raise concern about the understanding of informed consent in plastic surgery patients.
INTRODUCTION
The Institute of Medicine defines health literacy as the degree to which individuals have the capacity to obtain, process, and understand basic health information. The 2003 National Assessment of Adult Literacy survey has identified that low health literacy is at a crisis level in the United States.1 Low health literacy is associated with $106–$236 billion annually in increased hospitalizations.2 According to the American Medical Association (AMA), health literacy is a stronger predictor of a person’s health than age, income, employment status, education level, and race. The AMA manual highlights the fact that even well-educated, highly literate patients often struggle with important concepts during the medical consultation. A study conducted by Washington physicians found that low health literacy patients were more likely not to follow preoperative instructions, especially patients over the age of 65 years.3 Training in health literacy increases providers’ usage of health communication techniques.4 This facilitates a movement of empowering patients to understand, actively participate, and take responsibility for their outcomes. Failure to take appropriate actions toward eliminating inherent barriers in health communication is costly to hospitals and patients. In the plastic surgery literature to date, there is no study to our knowledge that assesses health literacy of plastic surgery patients and evaluates health communication between patients and providers. This study also aims to establish the readability of the American Society of Plastic Surgeons (ASPS) informed consent forms during the time of the initial internal quality review.
METHODS
A survey instrument was designed to assess the health literacy of plastic surgery patients and health communication competencies of the providers. Patients were asked specific questions in regards to their encounter with their plastic surgery providers. Plastic surgery attendings, residents, and physician assistants answered questions in regards to their training and confidence in cultural competencies and communication with low health literacy patients. Figures 1 and 2 depict the questions presented to patients and providers, respectively. These survey instruments were validated during the Health Literacy Dallas coalition’s pilot study that received 202 patient and 26 provider responses in a hospital setting. Strong face validity and internal consistency of this pilot study motivated the use of these survey instruments in a broader population of plastic surgery patients. Out of 106 surveys distributed to patients and 21 surveys to providers, there was a 100% response rate. Spanish-speaking patients were given a Spanish version of the survey, and a Spanish interpreter was available when deemed necessary. Participation was voluntary, and all data were collected anonymously. Descriptive statistical analysis was performed using Microsoft Excel (Microsoft Corp., Redmond, Wash.).
Fig. 1.

Patient survey instrument. GED indicates general education diploma.
Fig. 2.

Provider survey instrument.
Four of the ASPS informed consent forms were obtained and formatted into plain text. Descriptive analysis was performed using the Readability Calculator (readabilityformulas.com, My Byline Media). Seven readability scales were used to evaluate the available consent forms including Flesch Reading Ease score, Gunning Fog Index (GFI), Flesch-Kincaid Grade Level, Coleman-Liau Index, Automated Readability Index, and Linsear Write Formula (Table 1).
Table 1.
Analysis of Readability Scores of 2009 ASPS Informed Consent Forms
| GFI | FKGL | CLI | SMOG | ARI | LWF | |
|---|---|---|---|---|---|---|
| Breast augmentation | 16.3 | 12.6 | 14 | 12 | 13.2 | 13.4 |
| Breast implant removal | 16.6 | 13.1 | 14 | 12.3 | 13.4 | 13.8 |
| Facelift | 16 | 12.6 | 14 | 11.9 | 12.6 | 13 |
| Rhinoplasty | 15.8 | 12.4 | 14 | 11.7 | 12.5 | 12.8 |
| 16.2 | 12.7 | 14 | 12 | 12.9 | 13.3 |
ARI, Automated Readability Index; CLI, Coleman-Liau Index; FKGL, Flesch-Kincaid Grade Level; LWF, Linsear Write Formula; SMOG, Simple Measure of Gobbledygook.
Table 2 demonstrates the overall readability of 4 ASPS informed consent forms using the Hemingway Editor website (hemingwayapp.com, Long LLC). The average readability, number of adverbs, use of passive voice, number of phrases with simpler alternatives, and percent of sentences that were hard and very hard to read were evaluated for each consent form.
Table 2.
Readability of 2009 ASPS Informed Consent Forms Using Hemingway Editor
| Readability | Adverbs | Passive Voice | No. Phrases with Simpler Alternatives | Sentences Are Hard to Read, % | Sentences Very Hard to Read, % | |
|---|---|---|---|---|---|---|
| Breast augmentation | 13 | 45 | 84 | 101 | 17.4 | 37.9 |
| Breast implant removal | 12 | 31 | 63 | 86 | 16 | 38.2 |
| Facelift | 12 | 27 | 51 | 66 | 16.5 | 33.3 |
| Rhinoplasty | 12 | 30 | 51 | 70 | 16.7 | 33.1 |
| 12.3 | 33.3 | 62.3 | 80.8 | 16.7 | 35.6 |
RESULTS
A total of 106 plastic surgery patients and 21 plastic surgery providers completed the surveys at a tertiary county hospital during an internal quality review between June and November 2011.
Twenty percent of patients indicated that their highest level of education completed was less than high school and 30.2% had a high school diploma or general education diploma. Sixty percent of patients agreed that their health care provider understood their cultural and personal beliefs. Fourteen percent of patients agreed that the written instructions were difficult to understand. Fifty-one percent of patients agreed that better communication with their provider would improve their health (Table 3). Most patients responded that they use the Internet as a resource for obtaining information regarding their procedure.
Table 3.
Patient Survey Responses
| No. Responses/106 Patients | Percentage | |
|---|---|---|
| What gender do you identify with the most? | ||
| Man | 49 | 46.2 |
| Woman | 47 | 44.3 |
| Do not wish to answer | 10 | 9.4 |
| What is your age? | ||
| <16 | 0 | 0 |
| 16–25 | 20 | 18.8 |
| 26–35 | 18 | 16.9 |
| 36–45 | 22 | 20.7 |
| 46–55 | 25 | 23.6 |
| 56–65 | 16 | 15.1 |
| 66+ | 3 | 2.8 |
| Do not wish to answer | 2 | 2 |
| What is your highest education level? | ||
| Less than high school | 22 | 20.7 |
| High school diploma/GED | 32 | 30.2 |
| Some college | 26 | 24.5 |
| College degree | 13 | 12.3 |
| Professional degree | 4 | 3.8 |
| Do not wish to answer | 9 | 8.5 |
| My health care provider understands my cultural and personal background | ||
| Strongly disagree | 8 | 7.5 |
| Disagree | 3 | 2.8 |
| Neither agree or disagree | 33 | 31.1 |
| Agree | 40 | 37.7 |
| Strongly agree | 22 | 20.7 |
| Written instructions are difficult to understand | ||
| Strongly disagree | 27 | 25.5 |
| Disagree | 49 | 46.2 |
| Neither agree or disagree | 16 | 15.1 |
| Agree | 11 | 10.4 |
| Strongly agree | 3 | 2.8 |
| Better communication from my provider would improve my health | ||
| Strongly disagree | 16 | 15.1 |
| Disagree | 18 | 17.0 |
| Neither agree or disagree | 21 | 19.8 |
| Agree | 35 | 33.0 |
| Strongly agree | 16 | 15.1 |
| How often do you have difficulty following treatment guidelines due to your provider not communicating clearly with you? | ||
| Never | 38 | 35.8 |
| Rarely | 42 | 39.6 |
| Sometimes | 15 | 14.2 |
| Often | 8 | 7.5 |
| Always | 3 | 2.8 |
| How often do you ask your health care provider questions about what they tell you during a visit? | ||
| Never | 2 | 1.9 |
| Rarely | 14 | 13.2 |
| Sometimes | 33 | 31.3 |
| Often | 33 | 31.3 |
| Always | 24 | 22.6 |
| How often does your health care provider encourage you to ask questions about what they are telling you? | ||
| Strongly disagree | 3 | 2.8 |
| Disagree | 6 | 5.7 |
| Neither agree or disagree | 24 | 22.6 |
| Agree | 34 | 32.1 |
| Strongly agree | 39 | 36.8 |
GED, general education diploma.
Of the 21 plastic surgery attendings, residents, and physician assistants who completed the survey, 48% agreed that it is often difficult to get patients to understand their medical condition and follow postoperative instructions. Seventy-six percent agreed that they have difficulty communicating with patients with a different cultural background. Twenty-nine percent stated that they currently offer low-literacy educational material for their patients. Seventy-one percent of providers reported that they are not aware of policies at the hospital to support low-literacy patients. Fifty-seven percent of providers felt that they were aware of policies at the hospital to assist culturally diverse patients; 86% stated they felt that better communication with patients would improve their patients’ overall health status and outcomes (Table 4).
Table 4.
Provider Survey Responses
| No. Responses/21 Providers | Percentage | |
|---|---|---|
| Have you had training or education regarding health literacy? | ||
| Yes | 12 | 57.2 |
| Have you had training or education regarding clear health communication techniques? | ||
| Yes | 7 | 33.3 |
| Have you had training or education regarding cultural competency? | ||
| Yes | 12 | 57.2 |
| Do you currently offer low-literacy materials or forms to your patients? | ||
| Yes | 6 | 28.5 |
| Are you aware of policies at your hospital to support low-literacy patients? | ||
| Yes | 6 | 28.6 |
| Are you aware of policies at your hospital to support culturally diverse groups? | ||
| Yes | 12 | 57.2 |
| Do you feel better communication with your patients could improve their overall health status/outcomes? | ||
| Yes | 18 | 86 |
| Patients with a different cultural background than mine can present communication difficulties between us. | ||
| Agree/strongly agree | 16 | 76 |
| It is often difficult to get my patients to understand their medical condition and follow postvisit instructions. | ||
| Agree/strongly agree | 16 | 48 |
| How often do you have difficulty understanding or communicating with your patients? | ||
| Sometimes/often | 16 | 76 |
| Do you feel better communication with your patients could improve patient compliance with postvisit instructions? | ||
| Yes | 18 | 86 |
| Would you be interested in learning how to improve communication with your patients? | ||
| Yes | 16 | 76 |
On average, the readability of the informed consent documents was above a 12th grade, or professional, reading level. The mean Coleman-Liau Index grade level was 14, Gunning Fog Index reading level was 16.2, and Flesch-Kincaid Grade level was 12.7. The Simple Measure of Gobbledygook analysis measured 12th grade level readability. Flesch Reading Ease score, which produces an index score ranging from 0 to 100, with 100 being easiest to read, produced a score of 36.2 (Table 5). The Automated Readability Index reading level was 12.9, and the Linsear Write Formula score was 13.3 (Fig. 3). All indices concluded that each informed consent document was difficult to read. The Hemingway Editor website also identified adverbs and passive voice in the document that contribute to the difficulty of document’s readability (Figs. 4, 5). On average, there were 81 phrases identified with simpler alternatives. Seventeen percent of the sentences were identified as hard to read, and 36% of the sentences were very hard to read (Table 2). The application also highlighted specific words and sentences in the document that may be altered to make the document easier to read at a lower reading level.
Table 5.
Flesch-Kincaid Reading Ease Score
| Flesch-Kincaid Reading Ease | |
|---|---|
| Breast augmentation | 37.4 |
| Breast implant removal | 34.5 |
| Facelift | 35.8 |
| Rhinoplasty | 36.9 |
| 36.2 |
Fig. 3.

Example of readability score results.
Fig. 4.
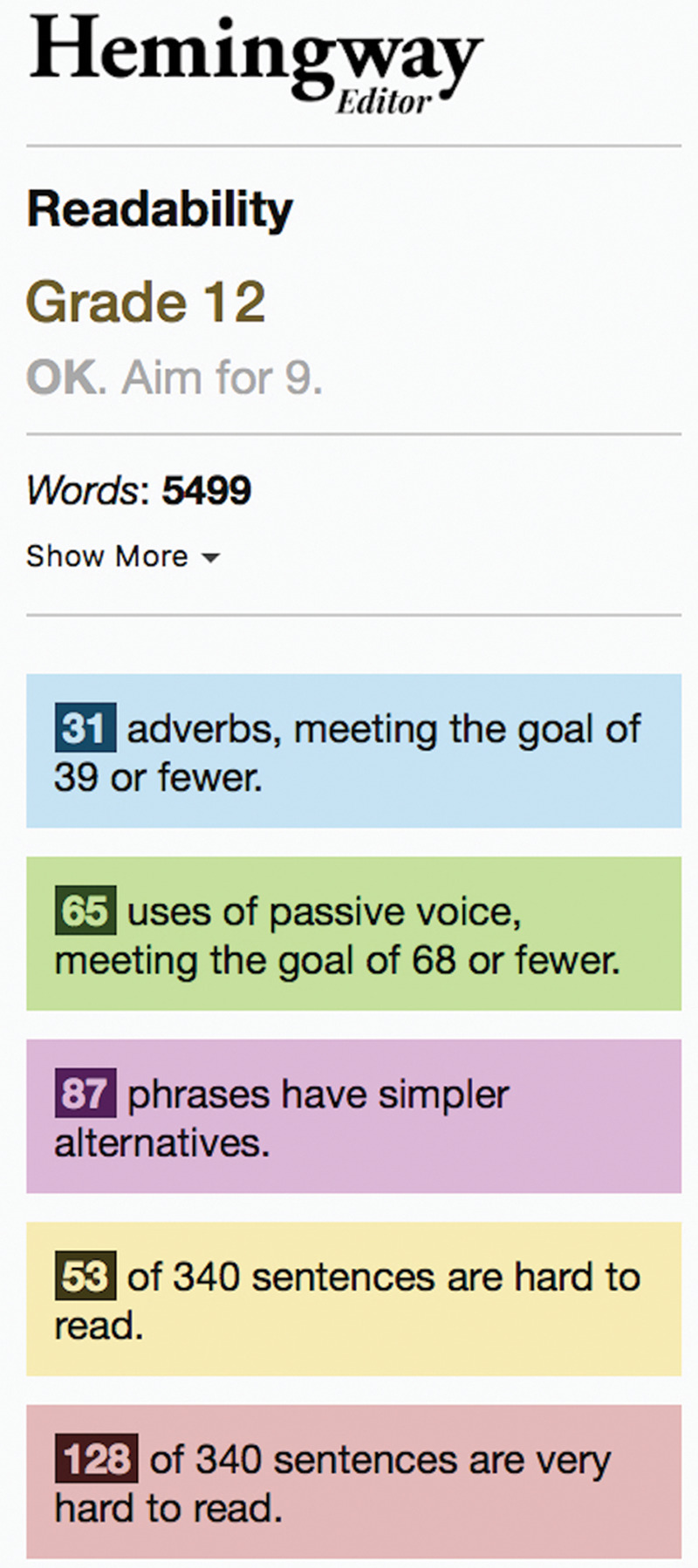
Example of Hemingway Editor readability of a document.
Fig. 5.

Example of highlighted text to improve readability of a document.
DISCUSSION
Approximately 90 million American adults have low health literacy; 14% of American adults have below basic health literacy and 22% have only basic health literacy. According to the Office of Disease Prevention and Health Promotion, only 12% of American adults can be considered “health literacy proficient,” meaning the individual could interpret a healthcare pamphlet, deduce prescription instructions from a label, or use a table to calculate healthcare costs.5 In fact, the AMA, National Institutes of Health, and US National Library of Medicine recommend that medical information be written at a sixth-grade reading level.6 Furthermore, studies evaluating characteristics of plastic surgery patients population have demonstrated that these patients may have lower levels of education than the general population.7,8
According to the study assessing the plastic surgeons’ perception of patient health literacy conducted by Lee et al, when asked about the methods used to enhance patient understanding during counseling, participating surgeons reported using simple, nonmedical terms (94%), explaining difficult topics slowly (76.9%), or drawing pictures or diagrams (84.6%).9 Only 8.1% of surgeons reported using the teach-back methods during patient counseling. Few surgeons used validated verbal or written assessments to determine their patient’s health literacy. Although as many as one-third of English-speaking patients in some settings have been found to have limited health literacy, health-related materials are frequently written at levels that far exceed many patients’ reading abilities.
The internal quality review conducted at a county hospital in 2011 demonstrated the gap in communication between the plastic surgery patients and providers. Approximately 15% of patients found the written postoperative instructions to be difficult to understand. Approximately half of plastic surgery patients felt that better communication with their provider would improve their health. Hospital reimbursement is now linked to patient satisfaction; patient satisfaction increases with improved communication.
Moreover, approximately half of the plastic surgery providers expressed difficulty in having their patients understand their medical conditions and follow their instructions. Plastic surgery providers need to feel empowered in delivering information to their patients in an effective manner. They also need to feel confident that they are distributing information the plastic surgery patients will understand. Although the determinants of noncompliance to preoperative instructions are complicated, studies demonstrate that low health literacy may be a contributing cause in surgical patients.3 This leads to poor communication between providers and patients, resulting in nonadherence to preoperative instructions and ultimately avoidable surgery cancellations and postponements, wasted operating room time, and additional hospital expenses.2 This finding also raises concern about the understanding of the informed consent process in a plastic surgery patient with low health literacy.
Readability of Plastic Surgery Documents
In 2015, 84% of adults in America used the internet regularly, of which approximately 49% initially turned to the internet to answer healthcare-related questions.9–11 Written online educational resources for plastic surgery procedures are available to the public. A survey of patients who had undergone breast augmentation reported that 59% of patients began their search for information about the procedure online, and 41% specifically started with a Google search. Of those patients, 49% indicated the most powerful influence on their choice of surgeon for breast augmentation was the plastic surgeon’s website.12 Momeni et al found that the readability of facial plastic surgery procedural information is written at a 10th grade reading level.13,14 Readability, complexity, and suitability of online resources available for mastectomy and subsequent reconstruction are also above the recommended literacy level.15 This material currently exceeds the recommended reading level of sixth grade. Online education materials may serve as a possible obstacle to patient education, decision making, and satisfaction.8
Readability of ASPS Informed Consent Documents
Studies show that 75% of malpractice lawsuits indicate a physician’s communication style and attitude were significant contributing factors. These patients reported that their doctor failed to provide an adequate explanation of diagnosis or treatment or felt their concerns were dismissed.5 Boyll et al16 studied methods for better understanding variables of the informed consent process that may contribute to reducing malpractice claims in plastic surgery. Questionnaires were obtained from plastic surgeons; respondents who provided procedure-specific brochures to their patients were significantly less likely to be sued for medical malpractice (P = 0.004) than those who did not.17 The study concluded variables that may reduce malpractice claims, and thereby improve both the quality and affordability of healthcare, include (1) the use of procedure-specific patient education brochures and (2) physician participation in malpractice insurance carrier–required courses.
The 2009 ASPS informed consent forms were the most updated version of consent forms in use during the time of this internal quality review. According to the readability indices, the overall grade level for informed consents was at a professional level and was found to be difficult to read. The informed consent documents were written at a reading level approximately 20% of the plastic surgery patients would not understand simply because they did not complete high-school education. The Hemingway Editor website may be used to identify certain words and phrases that may improve the readability of each informed consent document. The GFI differs from the other readability indices because variables including percentage of words with >3 syllables and average number of words per sentence are considered. The GFI may serve as the most sensitive index in this context. In addition, the ASPS informed consent forms list the possible complications to a procedure without providing the incidence of the complication. The role of the physician is to deliver and incorporate this important information while educating the patient.
Informed Consent Process in Plastic Surgery: Room for Improvement
This study highlights the need for simplification of vocabulary and grammar to improve the overall readability of plastic surgery consent documents. Several online language simplification tools exist, and the plastic surgery society may consider applying similar techniques to consent document language. The high technical complexity of plastic surgery procedures does merit comprehensiveness in consent documents of risks, benefits, and alternatives. Patients may have difficulty understanding what the surgery entails when reviewing complicated handouts and may therefore have an inaccurate assessment of perceived risks. Language should be simplified when feasible, while also supplementing with visual aids. Michalski et al18 found that the use of multimedia may help patients better assimilate and retain information during the informed consent process. Incorporating images depicting sites of incisions, organs, and soft tissues to be operated on and examples of dressings and drains to be anticipated may help achieve better understanding of procedure expectations in the plastic surgery population. Moreover, visual representations of statistics in the form of pie charts or bar graphs may better exemplify potential risks of complications. The use of videos in the informed consent process may also help improve patient understanding. Lin et al19 demonstrated in a randomized controlled trial that a video-assisted informed consent process improved patient comprehension, as well as perceived helpfulness and satisfaction of the informed consent process in the context of trauma surgery. The esthetic nature of plastic surgery naturally lends itself to visual education, and patients may benefit from incorporation of multimedia in patient–provider consent interactions.
A successful informed consent process hinders on capturing patients’ attention. A crucial aspect to strong patient–provider communication is assessment of patient personality, comfort level, and understanding. The informed consent process should be an interaction individualized to the patient to optimize engagement and comprehension. Tools to engage patients may include visual aids, tactile demonstrations of supplies to be utilized (eg, tissue expanders, breast implants, drains), humor, and assessment techniques. Alternatives to the well-known “teach-back” method may include providing patients with materials ahead of time, short quizzes, and more thorough consent documentation. For instance, providing patients with surgical procedure information, visual aids, and the consent document while waiting to meet with the provider may help remove perceived pressure to understand information quickly and may provide time for development of questions. Administering a short quiz assessing understanding of procedure risks/benefits/alternatives and preoperative instructions may then help the provider identify gaps in knowledge to focus on during the patient–provider interaction. Moreover, in addition to signatures at the end of the consent document indicating completion of the informed consent process, the requirement of initials to be placed by both the patient and provider at sections throughout the consent document may better ensure that all aspects of the consent are discussed. This more thorough documentation may also provide proof of adequate informed consent processes from a medicolegal perspective.
Limitations
This study has several limitations in addition to those inherent to a single institution, internal quality review. The internal quality review was conducted at a county hospital, which limits the generalizability of the study. The overall small sample size of 106 patients and 21 providers may account for potential selection bias because all survey responses were from patients at one county hospital who may not represent the broader plastic surgery patient population. Moreover, this study presents descriptive statistics of aggregate patient and provider survey responses. Further statistical analysis investigating how patient and provider characteristics may influence perceptions of communication may help better identify gaps in patient–provider communication. A future analysis may include investigating how sex, age, level of education, cultural background, geographic location, surgical procedure, follow-up with clinical outcomes, and providers’ years in practice influence patient perception of provider communication during the informed consent process. The study is also limited by the use of readability scales to assess written text. These scales are a calculation of text complexity and do not necessarily measure true comprehension or a patient’s ability to apply the given information. Also, there is no consensus regarding which scale is optimal for calculating readability. Each readability scale calculates reading grade level differently.
CONCLUSIONS
This study identifies the gap in communication between plastic surgery patients and providers in a county hospital setting. Failure to take appropriate actions toward eliminating inherent barriers in health communication is costly to both the hospital and the patients. Although online resources on plastic surgery procedures are available in abundance, high readability scores and complexity of resources may limit their utility. These findings also raise concern about the informed consent documents in plastic surgery patients.
ACKNOWLEDGMENTS
The authors would like to thank Ekaterina Tiourin for her review of the literature and contributions to the editing of the submission. This study was considered exempt from IRB approval.
Footnotes
Published online 13 May 2020.
Presented at Plastic Surgery The Meeting 2019, September 21, 2019, San Diego, Calif.
Disclosure: The authors have no financial interest to declare in relation to the content of this article.
REFERENCES
- 1.National Assessment of Adult Literacy (NAAL). What is NAAL? Available at: https://nces.ed.gov/naal/. Accessed August 7, 2019. [DOI] [PMC free article] [PubMed]
- 2.Lambert V, Keogh D.Health literacy and its importance for effective communication. Part 1. Nurs Child Young People. 2014;26:31–37; quiz 38. [DOI] [PubMed] [Google Scholar]
- 3.Chew LD, Bradley KA, Flum DR, et al. The impact of low health literacy on surgical practice. Am J Surg. 2004;188:250–253. [DOI] [PubMed] [Google Scholar]
- 4.Schlichting JA, Quinn MT, Heuer LJ, et al. Provider perceptions of limited health literacy in community health centers. Patient Educ Couns. 2007;69:114–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vargas CR, Chuang DJ, Lee BT.Assessment of patient health literacy: a national survey of plastic surgeons. Plast Reconstr Surg. 2014;134:1405–1414. [DOI] [PubMed] [Google Scholar]
- 6.National Library of Medicine. How to write easy-to-read health materials. Available at: http://www.nlm.nih.gov/medcineplus/etr.html. Accessed August 28, 2019.
- 7.Didie ER, Sarwer DB.Factors that influence the decision to undergo cosmetic breast augmentation surgery. J Womens Health (Larchmt). 2003;12:241–253. [DOI] [PubMed] [Google Scholar]
- 8.Vargas CR, Chuang DJ, Lee BT.The readability of online resources for mastopexy surgery. Ann Plast Surg. 2016;77:110–114. [DOI] [PubMed] [Google Scholar]
- 9.U.S. Department of Health and Human Services America’s Health Literacy: why we need accessible health information. U.S. Department of Health and Human Services. 2008. Available at: http://health.gov/communication/literacy/issuebrief. Accessed August 7, 2019.
- 10.Cook JA, Sasor SE, Tholpady SS, et al. Hand surgery resources exceed American health literacy. Hand (N Y). 2018;13:547–551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Perrin A, Duggan M.Americans’ Internet Access: 2000–2015. 2015Washington, DC: Pew Research Center; [Google Scholar]
- 12.Hesse BW, Nelson DE, Kreps GL, et al. Trust and sources of health information: the impact of the internet and its implications for health care providers: findings from the first Health Information National Trends Survey. Arch Intern Med. 2005;165:2618–2624. [DOI] [PubMed] [Google Scholar]
- 13.Chu MW, Cook JA, Tholpady SS, et al. Facial plastic surgery patient resources exceed national institute recommendations. J Craniofac Surg. 2017;28:759–763. [DOI] [PubMed] [Google Scholar]
- 14.Santos PJF, Daar DA, Paydar KZ, et al. Readability of online materials for rhinoplasty. World J Plast Surg. 2018;7:89–96. [PMC free article] [PubMed] [Google Scholar]
- 15.Walden JL, Panagopoulous G, Shrader SW.Contemporary decision making and perception in patients undergoing cosmetic breast augmentation. Aesthet Surg J. 2010;125:108. [DOI] [PubMed] [Google Scholar]
- 16.Boyll P, Kang P, Mahabir R, et al. Variables that impact medical malpractice claims involving plastic surgeons in the United States. Aesthet Surg J. 2018;38:785–792. [DOI] [PubMed] [Google Scholar]
- 17.Tran BN, Singh M, Lee B.Abstract P3: readability, complexity, and suitability of online resources for mastectomy and lumpectomy. Plast Reconstr Surg Glob Open. 2017;54 Suppl104. [DOI] [PubMed] [Google Scholar]
- 18.Michalski A, Stopa M, Miskowiak B.Use of multimedia technology in the doctor-patient relationship for obtaining patient informed consent. Med Sci Monit. 2016;22:3994–3999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lin Y, Chen C, Cheng Y, et al. Educational video-assisted versus conventional informed consent for trauma-related debridement surgery: a parallel group randomized controlled trial. BMC Medical Ethics. 2018;19:23. [DOI] [PMC free article] [PubMed] [Google Scholar]


