Abstract
Background and Objectives:
Polyps are reported on 1–10% of routine transabdominal ultrasound studies of the gallbladder. Prior studies have reported poor sensitivity and specificity for this diagnostic modality at determining malignant potential of polyps. The aim of this study is to determine the incidence of gallbladder polyps documented on ultrasound at a community hospital, evaluate the congruency of ultrasound with final histopathology, and explore factors which may improve ultrasound accuracy at diagnosing true adenomatous polyps.
Methods:
We conducted a 5-year retrospective cohort study of patients undergoing cholecystectomy at Danbury Hospital between 2014 and 2019, identifying those with a pre-operative ultrasound mention of a “polyp” or “mass.” We assessed the congruency of ultrasound findings with pathology reports.
Results:
Of the 2,549 cholecystectomies performed, 1,944 (76%) had pre-operative ultrasounds. Of those, 98 (5.0%) reported a polyp, measuring an average of 8.1 mm (SD 7.1 mm). Three (3.1%) specimens were identified as adenomas on final histopathology; the majority were benign pathologies including cholesterol polyp (18), cholesterolosis (20), adenomyoma (4), adenomyomatosis (7), and chronic or acute cholecystitis (44). Interestingly, only 1 of the 3 adenomas measured > 10 mm on ultrasound, the accepted indication for surgical resection.
Conclusions:
The accuracy of transabdominal ultrasound in diagnosing true polyps is poor, with only 3% of polyps identified as adenomas based on pathology. Surgeons should use caution when making clinical decisions based on polyps identified on ultrasound, and more stringent diagnostic criteria are needed in order to decrease the false positive rate for diagnosis and screening.
Keywords: Gallbladder polyps, Adenocarcinoma, Ultrasound
INTRODUCTION
Gallbladder cancer is a rare but lethal cancer, with an estimated incidence of 2 per 100,000 persons.1 The hypothesized pathophysiology is that of malignant transformation of adenomas. Gallbladder polyps are mucosal folds that protrude into the gallbladder and have historically been classified into two categories based on their malignant potential.2 True polyps have neoplastic changes and include adenomas and adenocarcinomas, while pseudopolyps lack neoplastic risk and include cholesterol, inflammatory, fibromas, hyperplastic, adenomyomatosis, and hamartomatous polyps.3
Transabdominal ultrasound has been shown to be a very poor predictive modality for true gallbladder polyps, with a false positive rate as high as 85%.4 Some studies comparing polyp findings on ultrasound and pathology have demonstrated a consistent overestimation of polyp size on ultrasound by up to 4 mm.5 Such discrepancies between ultrasound findings and final pathology have made the management of polyps challenging for physicians who rely on ultrasound imaging to make clinical recommendations. Despite the ongoing debate regarding the best imaging modality for evaluating gallbladder polyps, ultrasound remains the gold standard; current guidelines recommend a prophylactic cholecystectomy for polyps larger than 10 mm and surveillance for polyps < 10 mm.3 However, some authors have advocated for the removal of smaller polyps due to the poor prognosis of a late stage surgery.6
The purpose of this study is to determine the incidence of gallbladder polyps documented on pre-operative ultrasound for patients who underwent a laparoscopic or open cholecystectomy at Danbury Hospital between January 2014 and January 2019, and evaluate the congruency of pre-operative ultrasound findings with postoperative final pathology. We hypothesize that there will be a high rate of incongruency between pre-operative ultrasound findings and final histopathologic results.
MATERIALS AND METHODS
We conducted a retrospective cohort study with the following inclusion criteria: age 18 years or older with ultrasound documentation of a polyp that preceded an elective or emergent cholecystectomy at Danbury Hospital between January 2014 and January 2019. Patients that had imaging of gallbladder polyps and did not undergo a cholecystectomy or did not have a pathology report were excluded from the study. We queried all available ultrasound reports of patients who underwent a cholecystectomy for a mention either of a “polyp” or “mass”. The primary outcome variables of interest included the final pathology of the polyp; specifically, whether a polyp was present on pathology and whether it was a true or pseudopolyp. Additionally, we established the proportion of patients with polyps on pre-operative ultrasound who also had a magnetic resonance cholangiopancreatography (MRCP) pre-operatively to determine the concordance with the ultrasound and final histopathology. To identify the number of patients who had a cholecystectomy solely for a gallbladder polyp, we used the listed indication for surgery in the operative report.
RESULTS
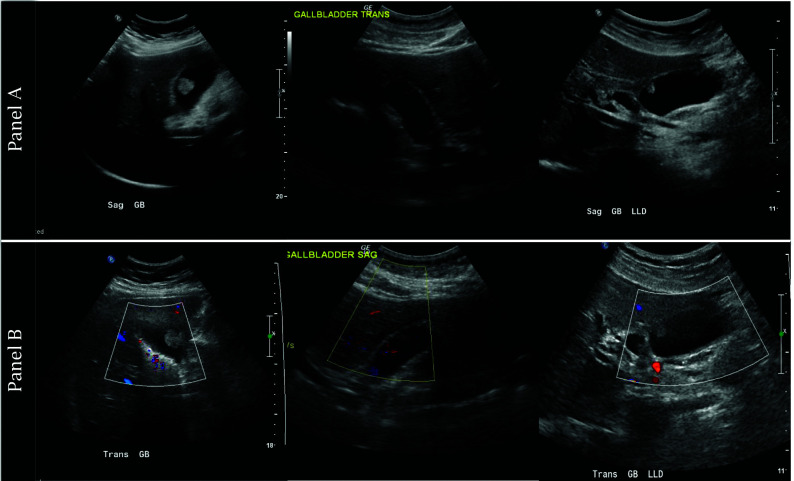
In the 5-year period of our study, 2,549 patients underwent a cholecystectomy at Danbury Hospital. Of these, 1,944 (76%) patients met inclusion criteria. Ninety-eight patients (5.1%) had ultrasound reports, which described the presence of a mass or polyp. Seventy-eight (80%) of reports stated a measured size of the polyp, with an average measurement of 8.1 mm (SD 7.1 mm), Figure 1. The final pathology of 45 specimens (46%) was not associated with any mass or polyp, but was either acute or chronic cholecystitis, cholelithiasis, or a benign gallbladder. A complete breakdown is reported in Table 1. Only 3 (3.1%) of the specimens were positive for an adenoma; none were malignant. The 3 ultrasounds of the adenomas are displayed in Figure 2 (panel A). None had significant vascular flow to the polyp, as noted by color Doppler mode in Figure 2 (panel B).
Figure 1.
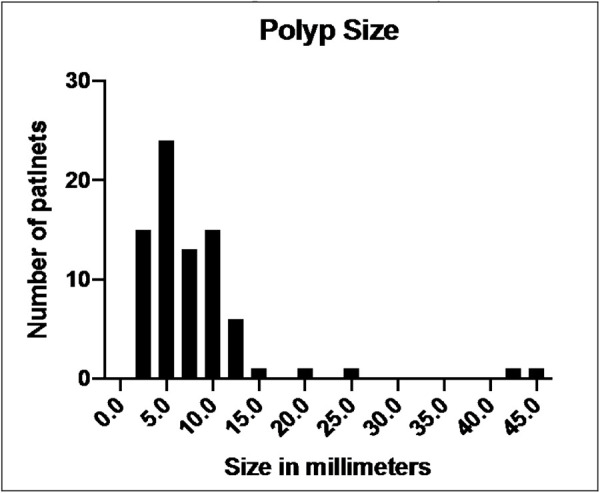
Histogram distribution of size of polyps visualized on ultrasound (n = 78, polyps with no documented size on report are excluded).
Table 1.
Final Histopathology of Resected Gallbladder Polyps1
| Histopathology | All Gallbladder Polyps (n = 98) |
|
|---|---|---|
| n | % | |
| Pseudopolyps | ||
| Benign gallbladder | 1 | 1 |
| Acute cholecystitis | 13 | 13.3 |
| Chronic cholecystitis | 86 | 87.8 |
| Gangrenous or necrotizing cholecystitis | 3 | 3.1 |
| Cholesterol polyp | 19 | 19.4 |
| Cholesterolosis | 19 | 19.4 |
| Adenomyomatosis | 1 | 1 |
| Adenomyoma | 11 | 11.2 |
| Adenomyomatous Hyperplasia | 5 | 5.1 |
| True Polyps | ||
| Adenoma | 3 | 3.1 |
| Malignancy | 0 | 0 |
Table displays count data and percentage of total polyps included. Gallbladders with more than 1 pathology were counted separately.
Figure 2.
Ultrasound images of the 3 gallbladder polyps that were adenomas on final histopathology. Panel A displays gallbladder in B mode and panel B shows color Doppler to evaluate vascularity of polyps. None of the polyps had significant vascularity.
We determined that 17 out of 98 cholecystectomies (17.3%) were performed solely for a polyp, mass, or concern for cancer. Only one of the 17, or 5.9%, of the patients who had surgery performed solely for a gallbladder polyp on ultrasound ended up being a true polyp.
Of the 98 patients with a polyp on pre-operative ultrasound, 27 (27.6%) had a pre-operative MRCP. Twelve (44.4%) of the MRCP studies describe a polyp or a gallbladder mass; however, none of these patients resulted in a true polyp. The 3 adenomas we identified within our cohort did not have a pre-operative MRCP study.
DISCUSSION
Concordant with rates reported in the literature, the prevalence of reported gallbladder polyps on routine transabdominal ultrasounds in our study was 5.1%.7–9 Despite the frequency of this finding, the positive predictive value of ultrasound in diagnosing a true gallbladder polyp continues to remain low. In this study, only 3.1% of polyps were true polyps with malignant potential. This is similar to rates reported in other studies, which range between 1–5% when evaluating a polyp of any size.9,10 Subgroup analyses of patients with polyps > 10 mm on ultrasound report better predictive values, ranging between 5 – 6.5%. However, this study demonstrates a rate that still remains low for this group, at around 5%.
The goal of utilizing ultrasound for gallbladder polyps is to identify and remove adenomas to prevent progression to malignant carcinomas or to resect carcinomas at an early stage, thus improving prognosis. Gallbladder carcinoma is a rare but aggressive cancer with a 5-year survival between 3–13%.11,12 However, early T1 tumors can have a 10-year survival rate as high as 87%, demonstrating the importance of early resection.
In our study, none of the patients who underwent a cholecystectomy with a preoperative polyp on ultrasound had gallbladder cancer on final histopathology. Most studies report the incidence rate of gallbladder cancer after any cholecystectomy as < 1%; however, the incidence of cancer in cholecystectomy performed in patients with a gallbladder polyp can be as high as 6%.13,14 As the surgical community becomes more experienced and comfortable with laparoscopic cholecystectomy and with the implementation of the “critical view of safety,” the occurrence of common bile duct injuries has become exceedingly rare. Recent large retrospective reviews of elective cholecystectomies performed over the last two decades have reported biliary injuries to occur between 0.08 – 0.22% of cases.15,16 Given the reported incidence of polyps with malignant potential of around 6%, surgeons should consider resecting polyps in good surgical candidates with high risk factors for a malignancy.
Predictive risk factors for gallbladder cancer in patients with a gallbladder polyp are age > 50 years, sessile polyp morphology, primary sclerosing cholangitis, polyp size, and presence of large gallstones.17,18 Among these, polyp size > 10 mm has been one of the strongest predictors driving the consensus to perform a cholecystectomy.3,19 Interestingly, in our study only 1 out of 20 (5%) patients with a polyp ≥ 10 mm was a true polyp.
This study explored the diagnostic utility of ultrasound of diagnosing gallbladder polyps, however, some authors have proposed using MRCP to diagnose or confirm gallbladder polyps.21 We demonstrated that the concordance rate MRCP with ultrasound is poor with only 44.4% of MRCP studies describing the polyp seen on ultrasound. The predictive value of an MRCP in our study is also poor, with none of the patients resulting in a true polyp. However, the three true polyps we identified did not have a preoperative MRCP performed.
Several hypotheses have been postulated to explain the poor sensitivity of ultrasound in distinguishing true polyps. Kratzer et al. proposed that the initial diagnosis of a polyp might be incorrect.7 In that study, 34 patients with gallbladder polyps were followed with serial/surveillance ultrasound at 30 and 84 months; the authors noted that on follow-up imaging 7 patients did not have a detectable polyp, supporting the argument that the initial diagnosis was a false positive. French et al. argued that perhaps polyps break off at the stalk, either through trauma from gallstones or during a cholecystectomy, and are therefore absent from final histopathology.9 Other authors have postulated that small polyps seen on ultrasounds are simply mucosal folds or gallstones without posterior shadowing that were adherent or within the gallbladder wall, creating an appearance of a polyp.5
In the field of gastroenterology, colonic polyps are frequently removed during routine colonoscopies. Similar to a common bile duct injury during a cholecystectomy, a risk of perforation and bleeding accompanies each colonic polypectomy. These complications are estimated to occur in 5.8 per 10,000 colonoscopies.20 Most resected colonic polyps are benign with no malignant potential; nevertheless, gastroenterologists continue to resect polyps due to the benefit of early diagnosis and resection of colon cancer. A similar approach may be considered with gallbladder polyps. Since malignancy cannot be excluded with an ultrasound study, surgeons may choose to accept the low risk of bile duct injury or bile leak in order to remove an early gallbladder adenoma or carcinoma. Surgeons should discuss with patients the benefits of removing a very rare, albeit aggressive gallbladder cancer with the possibility of performing an unnecessary cholecystectomy and subjecting a patient to the risks of a complication such as a bile duct injury.
CONCLUSION
The accuracy of transabdominal ultrasound in diagnosing true polyps is poor, with only 3% of polyps identified as adenomas based on pathology. Surgeons should use caution when making clinical decisions based on polyps identified on ultrasound, and more stringent diagnostic criteria are needed in order to decrease the false positive rate for diagnosis and screening.
Contributor Information
Alexander Ostapenko, Department of General Surgery, Danbury Hospital, Danbury CT..
Shawn Liechty, Department of General Surgery, Danbury Hospital, Danbury CT..
Minha Kim, Department of General Surgery, Danbury Hospital, Danbury CT..
Daniel Kleiner, Department of General Surgery, Danbury Hospital, Danbury CT..
References:
- 1.Henley SJ, Weir HK, Jim MA, Watson M, Richardson LC. Gallbladder cancer incidence and mortality, United States 1999–2011. Cancer Epidemiol Biomarkers Prev. 2015;24(9):1319–1326. [DOI] [PubMed] [Google Scholar]
- 2.Terzioglu SG, Kilic MO, Sapmaz A, Karaca AS. Predictive factors of neoplastic gallbladder polyps: outcomes of 278 patients. Turk J Gastroenterol. 2017;28(3):202–206. [DOI] [PubMed] [Google Scholar]
- 3.Wiles R, Thoeni RF, Barbu ST, et al. Management and follow-up of gallbladder polyps. Eur Radiol. 2017;27(9):3856–3866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Martin E, Gill R, Debru E. Diagnostic accuracy of transabdominal ultrasonography for gallbladder polyps: systematic review. Canadian Journal of Surgery. 2018;61(3):200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zielinski MD, Atwell TD, Davis PW, Kendrick ML, Que FG. Comparison of surgically resected polypoid lesions of the gallbladder to their pre-operative ultrasound characteristics. J Gastrointest Surg. 2009;13(1):19–25. [DOI] [PubMed] [Google Scholar]
- 6.Zielinski MD, Davis PW, Que FG, Kendrick ML, Atwell TD. 250 Comparison of Surgically Resected Polypoid Lesions of the Gallbladder to Their Pre-Operative Ultrasound Characteristics. Gastroenterology. 2008;134(4):A-845. [DOI] [PubMed] [Google Scholar]
- 7.Kratzer W, Haenle MM, Voegtle A, et al. Ultrasonographically detected gallbladder polyps: a reason for concern? A seven-year follow-up study. BMC Gastroenterology. 2008;8(1):41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Okamoto M, Okamoto H, Kitahara F, et al. Ultrasonographic evidence of association of polyps and stones with gallbladder cancer. The American Journal of Gastroenterology. 1999;94(2):446–450. [DOI] [PubMed] [Google Scholar]
- 9.French DG, Allen PD, Ellsmere JC. The diagnostic accuracy of transabdominal ultrasonography needs to be considered when managing gallbladder polyps. Surgical Endoscopy. 2013;27(11):4021–4025. [DOI] [PubMed] [Google Scholar]
- 10.Damore LJ, Cook CH, Fernandez KL, Cunningham J, Ellison EC, Melvin WS. Ultrasonography incorrectly diagnoses gallbladder polyps. Surg Laparosc Endosc Percutan Tech. 2001;11(2):88–91. [PubMed] [Google Scholar]
- 11.Cubertafond P, Gainant A, Cucchiaro G. Surgical treatment of 724 carcinomas of the gallbladder. Results of the French Surgical Association Survey. Ann Surg. 1994;219(3):275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wilkinson DS. Carcinoma of the gall‐bladder: an experience and review of the literature. Aust N Z J Surg. 1995;65(10):724–727. [DOI] [PubMed] [Google Scholar]
- 13.Dorobisz T, Dorobisz K, Chabowski M, et al. Incidental gallbladder cancer after cholecystectomy: 1990 to 2014. OncoTargets and Therapy. 2016;9:4913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ryong H, Jang G-C, Ryu D-M, Ji C-S. Laparoscopic cholecystectomy for gallbladder polyp is significant in the prevention of gallbladder cancer? Digestive Medicine Research. 2019;2. [Google Scholar]
- 15.Halbert C, Pagkratis S, Yang J, et al. Beyond the learning curve: incidence of bile duct injuries following laparoscopic cholecystectomy normalize to open in the modern era. Surg Endosc. 2016;30(6):2239–2243. [DOI] [PubMed] [Google Scholar]
- 16.Fong ZV, Pitt HA, Strasberg SM, et al. Diminished survival in patients with bile leak and ductal injury: management strategy and outcomes. J Am Coll Surg. 2018;226(4):568–576. e561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bhatt NR, Gillis A, Smoothey CO, Awan FN, Ridgway PF. Evidence based management of polyps of the gall bladder: a systematic review of the risk factors of malignancy. Surgeon. 2016;14(5):278–286. [DOI] [PubMed] [Google Scholar]
- 18.Buckles DC, Lindor KD, LaRusso NF, Petrovic LM, Gores GJ. In primary sclerosing cholangitis, gallbladder polyps are frequently malignant. Am J Gastroenterol. 2002;97(5):1138–1142. [DOI] [PubMed] [Google Scholar]
- 19.Babu BI, Dennison AR, Garcea G. Management and diagnosis of gallbladder polyps: a systematic review. Langenbecks Arch Surg. 2015;400(4):455–462. [DOI] [PubMed] [Google Scholar]
- 20.Kothari ST, Huang RJ, Shaukat A, et al. ASGE review of adverse events in colonoscopy. Gastrointest Endosc. 2019;90(6):863–876. e833. [DOI] [PubMed] [Google Scholar]
- 21.Elmasry M, Lindop D, Dunne DF, Malik H, Poston GJ, Fenwick SW. The risk of malignancy in ultrasound detected gallbladder polyps: a systematic review. Int J Surg. 2016;33:28–35. [DOI] [PubMed] [Google Scholar]