Supplemental Digital Content is available in the text.
Summary:
With the shift in public opinion and legalization of cannabis for therapeutic and recreational use, cannabis consumption has become more common. This trend will likely continue as decriminalization and legalization of marijuana and associated cannabinoids expand. Despite this increase in use, our familiarity with this drug and its associated effects remains incomplete. The aim of this review is to describe the physiologic effects of marijuana and its related compounds, review current literature related to therapeutic applications and consequences, discuss potential side effects of marijuana in surgical patients, and provide recommendations for the practicing plastic surgeon. Special attention is given to areas that directly impact plastic surgery patients, including postoperative pain, nausea and vomiting and wound healing. Although the literature demonstrates substantial support for marijuana in areas such as chronic pain and nausea and vomiting associated with chemotherapy, the data supporting its use for common perioperative problems are lacking. Its use for treating perioperative problems, such as pain and nausea, is poorly supported and requires further research.
INTRODUCTION
Over the last decade, the use of marijuana and opinions regarding its safety and potential therapeutic applications have risen to the forefront of American cultural consciousness. A large shift in public opinion (Fig. 1),1 coupled with the legalization of marijuana in several states for medical and recreational use (Fig. 2),2 has made cannabis consumption more common than in previous eras,3 and the rise of its use has seen a proportional increase in claims about its therapeutic applications (“medicinal” marijuana) (see figure, Supplemental Digital Content 1, which displays marijuana trends in the United States, http://links.lww.com/PRSGO/B3773).
Fig. 1.
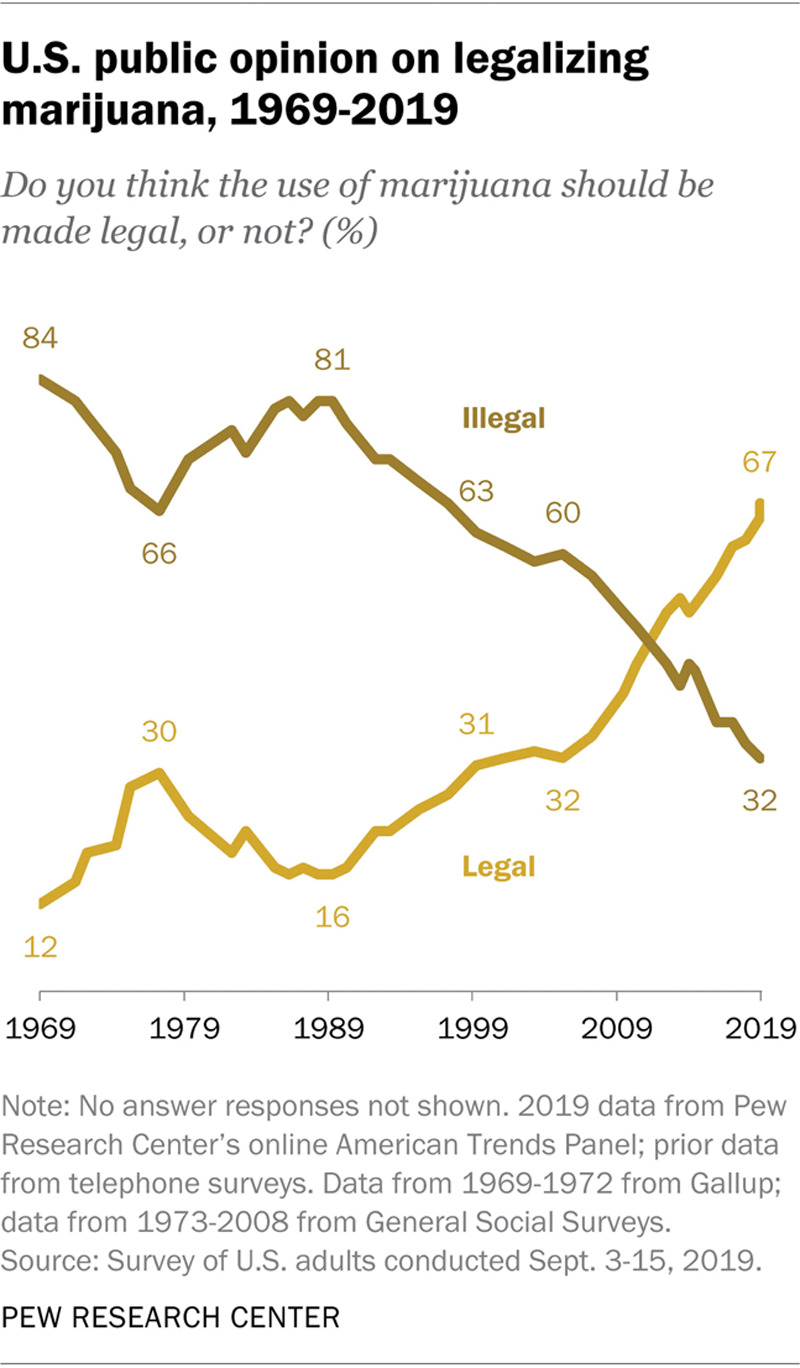
US public opinion on marijuana legalization, 1969–2019.1 Reprinted with permission from Pew Research Center, Washington, D.C.
Fig. 2.
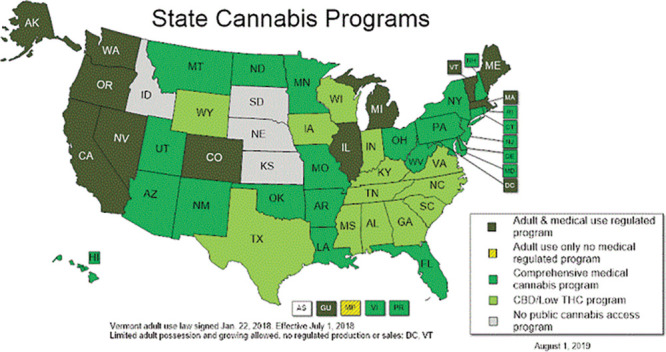
State cannabis laws.2 Vermont adult use law signed January 22, 2018. Effective July 1, 2018. Limited adult possession and growing allowed. No regulated production or sales: DC, VT. Reprinted with permission from © National Conference of State Legislatures.
According to the latest World Health Organization data, 2.5% of the world’s population consume the cannabis plant in its various forms.4 In the United States, 33 states and the District of Columbia have approved medical marijuana laws (MMLs) and 10 states and the District of Columbia have legalized marijuana for recreational use (Fig. 2),2 and a recent public survey demonstrated increased support for legalization of marijuana, especially among millennials (Fig. 1).1,5 Subsequently, there has been an increase in marijuana use over the last decade. In 2018, 15.9% (nearly 44 million people) of the US population over the age of 12 years reported using marijuana with the highest concentration of marijuana use seen in adults between the ages of 18 and 25 (34.8%).3
These developments, many of which have occurred in the last several years, have made it imperative for the practicing surgeon to understand the effects of marijuana on their patients and the impact it may have on surgical outcomes. Given the paucity of articles discussing marijuana use in plastic surgery, and its increasing use, a review of marijuana, its therapeutic applications, and the consequences associated with recreational use may be valuable to the practicing plastic surgeon. The aim of this study is to review the current literature in regard to the therapeutic use of marijuana, discuss the side effects of marijuana use as it relates to surgical patients, and provide recommendations for the practicing plastic surgeon.
BACKGROUND
The use of cannabis and its related compounds (Table 1) for recreational, religious, and medicinal use has been recorded as early as 5000 years ago.7 The 2 active compounds in the Cannabis plants are tetrahydrocannabinol (THC) and cannabidiol (CBD). THC is responsible for the psychoactive and cognitive effects (“getting high”) of marijuana, whereas CBD may offer therapeutic effects for a range of maladies, including epilepsy, glaucoma, symptomatic treatment of cancer, muscle spasm, nausea, and pain.5,6,11–15
Table 1.
Related Terminology
| Term | Description |
|---|---|
| CBD | One of the main chemical compounds present in the plant Cannabis sativa6 |
| Cannabinoid | Chemical compounds found in the plant C. Sativa, including THC and CBD7,8 |
| Cannabis | Term used to describe the products made from the plant C. sativa9 |
| Cannador | Medicinal cannabis containing THC and CBD in 2:1 ratio10 |
| Dronabinol | FDA-approved, synthetic THC-based medication, in pill form7 |
| Endocannabinoid | Endogenous cannabinoids in the body8 |
| Endocannabinoid system | Endogenous cannabinoids together with cannabinoid receptors8 |
| Marijuana | Mixture of dried leaves and flowers of the C. sativa plant7 |
| Nabilone | FDA-approved, synthetic THC-based medication, in pill form7 |
| THC | Chemical compounds present in the plant C. sativa that has psychoactive properties6,7 |
FDA, Food and Drug Administration.
At a cellular level, cannabinoids work as a partial agonist for 2 types of receptors: cannabinoid receptor type 1 (CB1) and cannabinoid receptor type 2 (CB2). Both CB1 and CB2 are G-coupled receptors, and their activation leads to inhibition of adenylyl cyclase and decrease in cyclic adenosine monophosphate (cAMP)14 (see figure, Supplemental Digital Content 2, which displays cannabinoid receptor signaling, http://links.lww.com/PRSGO/B378). CB1 receptors are found throughout the body but are most highly concentrated in brain, nervous system, liver, adipose tissue, and vascular endothelium. Physiologically, activation of these receptors causes vasodilation of arterioles, attenuation of acetylcholine in gastrointestinal (GI) tract, and hepatocyte lipid synthesis regulation.16 CB2 is mostly found in the immune system and some neurons.6,11,13,14 When compared with the effects of CB1, activation of CB2 receptors causes modulation of immunogenic cytokine proliferation and regulation of neuronal cell proliferation.16
Cannabinoids are primarily metabolized by the liver through the CYP450 system. Roughly 65% of the metabolized cannabinoid is secreted through the GI tract and about 20% filtered through the kidney. It takes approximately 5 days to eliminate 80%–90% of the consumed cannabinoid, with slight variation depending on the route of administration.6,13
Since 2009, synthetic cannabinoids have become increasingly more popular, especially with the ease of online purchasing. These products are often referred to as “Spice,” “K2,” or “Eclipse” and have a high affinity to CB1 receptors, making them desirable for recreational use due to the CB1-mediated psychotropic side effects. However, the increased affinity to CB1 receptors leads to a higher potential for toxicity and over the last few years, there has been a significant increase in deaths related to synthetic marijuana.5,17–19 These deaths have been linked to the ability of synthetic marijuana to disrupt neurotransmitter pathways leading to seizures, acute coronary syndrome, and hyperemesis with sequelae that include aspiration, asphyxiation, and acute psychosis.20
METHODS OF CONSUMPTION
Marijuana is prepared from the dried flowers and leaves of the plant Cannabis sativa.21,22 The highest concentration of cannabinoids can be found in the flowers followed by the leaves.21 Cannabinoids can be consumed in several different forms: inhalation, oral, sublingual, and topical.23 In the United States, inhaled marijuana, smoking or vaporizing, is the most common form of marijuana consumption.24 Smoking involves burning marijuana leaves to release the active compounds, whereas vaporizing (“vaping”) uses a heating element to vaporize cannabinoid-containing liquids to achieve the same effect.23,25
Orally, cannabis can be consumed as edibles, tinctures (extract dissolved in ethyl alcohol), capsules, or oils.23,26 Often this route of administration results in delayed onset and prolonged duration of cannabinoids’ effects due to slow absorption via the GI system.22 These products can be in the form of baked goods (cookies, brownies, muffins, etc), candies (lollipops, gums, or chocolate), or infusions into a variety of beverages.27 Other routes of administration include sublingual (sprays and cannabis-infused strips) and transdermal (lotions and bath balms).26
THERAPEUTIC USE OF MARIJUANA
In 2017, The National Academies of Sciences, Engineering, and Medicine (NASEM) published a report summarizing current evidence-based recommendations for the therapeutic use of cannabis and the health effects of marijuana use. In this report, over 10,000 articles were reviewed and recommendations were made based on the available evidence (Table 2). The strongest evidence for the therapeutic applications of cannabis exists for the treatment of chronic pain, chemotherapy-induced nausea and vomiting (CINV), and muscle spasticity associated with multiple sclerosis.5 In addition to the comprehensive report by the NASEM, Whiting et al9 performed a systematic review and meta-analysis and was able to identify 79 randomized controlled trials (RCTs) exploring therapeutic effects of cannabinoids; again, the majority of RCTs assessed the use of cannabinoids as treatment for CINV, chronic pain, and muscle spasticity due to multiple sclerosis or paraplegia. The discussion that follows focuses on the evidence for those problems that might directly impact plastic surgery: cannabis for analgesia, postoperative nausea and vomiting (PONV), and potential adverse perioperative effects of marijuana use in surgical patients.
Table 2.
Therapeutic Use and Health Effects of Marijuana Summary5
| Clinical Application | Level of Evidence | Findings |
|---|---|---|
| Treatment of chronic pain | Conclusive or substantial | Studies demonstrated reduction in pain after cannabis administration. |
| Treatment of chemotherapy-induced nausea and vomiting | Conclusive or substantial | Most recent study concluded the similar effectiveness of cannabinoids compared with standard antiemetic regiment. |
| Treatment of patient-reported multiple sclerosis spasticity symptoms | Conclusive or substantial | Randomized controlled trials demonstrated reduced patient-reported spasticity. |
| Triggering of AMI | Limited | Retrospective cohort study and a case crossover study reported increased risk of AMI after cannabis use; however, there are several limitations with both studies. |
| Ischemic stroke | Limited | Several studies demonstrated the statistical association between cannabis and ischemic stroke, however, all with their unique limitations. |
| Treatment of cancer-associated anorexia-cachexia syndrome | Insufficient | A phase III multicenter, randomized, double-blinded, placebo-controlled trial was terminated for lack of significance difference among the treatment and control groups. |
| Improving diarrhea symptoms of irritable bowel syndrome | Insufficient | Single randomized trial failed to show any treatment effects on gastric or bowel transit time. |
| Treatment of epilepsy | Insufficient | Lack of randomized, double-blinded, controlled trials |
AMI, acute myocardial infarction.
ROLE OF CANNABINOIDS IN THE TREATMENT OF POSTOPERATIVE PAIN
The use of cannabis for the treatment of chronic pain has been widely studied, and there is a considerable body of evidence in support of cannabinoids as an effective treatment.5 Whiting et al9 showed, on average, a minimum of 30% reduction in chronic pain in the cannabinoid group compared with the placebo group. Interestingly, Bradford and Bradford28 analyzed the prescription data from Medicare Part D enrollees in states with MMLs and found a reduction of 1826 daily doses of prescription pain medication in states with MMLs. Several studies have also evaluated reasons patients seek medical marijuana. A study in 2013 surveyed 348 patients in a medical marijuana clinic in Michigan and found that 87% of those patients are seeking medical marijuana for pain relief.29 Similarly, the vast majority (94%) of medical marijuana users in Colorado reported using medical marijuana for pain relief.5
Although the evidence for the use of cannabis in the treatment of chronic pain is favorable, data on the use of cannabinoids as a postoperative analgesic are mixed. Azim et al30 explored the endocannabinoid system (Table 1), both peripherally and centrally, in patients undergoing total knee arthroplasty and found that the levels of endocannabinoid were significantly elevated in patients who developed higher postoperative pain. They concluded that the endocannabinoid system may serve as a target for the development of novel analgesics for postoperative pain.
Holdcroft et al31 conducted a dose-escalating study of oral cannabis, Cannador (Table 1), for the treatment of postoperative pain and found lower rescue analgesia requirements in the 10- and 15-mg groups. They also reported decreasing pain intensity across the escalating dose group. The study, however, was terminated due to Cannador eliciting a vasovagal response in doses of 15 mg.31 A study published in the Journal of Arthroplasty compared total hip and knee arthroplasty patients who received 5 mg of dronabinol (Table 1) twice daily postoperatively versus the control group that received standard pain regiment. They found that the mean length of hospital stay in the dronabinol group was shorter, and they also consumed less total morphine equivalent dose compared with the control group; however, neither of these achieved statistical significance.32
A meta-analysis on 3 RCTs looking at postoperative pain management using cannabis concluded that cannabis-based medications are not effective in the treatment of postoperative pain and recommended further investigation due to small sample sizes.33 An additional study published in the Canadian Journal of Anesthesiology found no significant differences in morphine equivalent dose in the group receiving synthetic THC versus the control group.34 Beaulieu35 conducted a double-blinded RCT on the use of nabilone (Table 1) for the treatment of postoperative pain. In this study, no significant differences were found in the nabilone group versus the placebo; however, patients who received higher dose of nabilone (2 mg), contrary to the original hypothesis of the article, were found to have significantly higher pain scores compared with the other groups. Buggy et al36 conducted a double-blinded RCT with 40 women undergoing hysterectomy to assess the efficacy of orally administered THC in the treatment of postoperative pain. They also found no significant effect in 5 mg of orally administered THC versus the placebo group in the treatment of postoperative pain.
ROLE OF CANNABINOIDS IN THE TREATMENT OF PONV
Cannabinoid use as an antiemetic agent for CINV has been widely studied. The NASEM concluded in their report that there is substantial evidence in support of oral cannabinoids effectiveness in the treatment of CINV.5 Smith et al37 conducted a systematic review in 2015 to assess the effectiveness of cannabis-based medications in the treatment of CINV. Twenty-three RCTs were included investigating nabilone or dronabinol with placebo or other antiemetic medications, such as metoclopramide or chlorpromazine. They concluded that cannabinoids were more effective than placebo and similar in efficacy compared with the other antiemetic agents in the treatment of CINV.37 Whiting et al9 also performed a systematic review and meta-analysis and found a greater complete response for CINV in the cannabinoid group compared with the placebo; however, this did not reach statistical significance in all studies.
PONV is a common adverse effect of anesthesia and complications after surgery. It can affect overall patient satisfaction and surgical outcomes and result in additional use of hospital resources.38 It has been hypothesized that antiemetic properties of cannabinoids can be applied to postoperative patients with nausea and vomiting, although a randomized control trial published in 2017 showed no difference in the cannabinoid and the placebo group. There were limitations to the study, specifically the dose of nabilone which was thought to be too small to have any effect.34 Another RCT conducted by Kleine-Brueggeney et al39 randomized 40 patients to receive IV THC or placebo intraoperatively. Their primary outcome was the overall incidence of PONV during 24 hours postoperatively. They failed to show a statistical significance between the THC and placebo group, and the study was terminated after the initial 40 patients due to adverse effects of confusion and sedation in the THC cohort.39 Hickernell et al32 conducted a retrospective review of patients receiving 5 mg of dronabinol twice daily after total joint arthroplasty and similarly failed to show a significant difference in the 2 groups in regard to PONV. The results were, however, limited due to the study being underpowered to determine a difference among the groups.32
ADVERSE EFFECTS OF CANNABINOIDS IN THE SURGICAL PATIENTS
Just because patients use herbal supplements to treat a variety of health conditions, it can only be assumed that they will use cannabinoids in a similar fashion. With this in mind, it is imperative for the practicing plastic surgeon to understand what effects, beneficial and otherwise, cannabinoid use will have on their patients. Although positive and negative effects of herbal supplements have been described in the literature,40 the full range of cannabinoid benefits and side effects is still unknown.
Several adverse effects of cannabinoids and anesthesia have been described in the literature. Due to the presence of CB1 receptors on vascular endothelium, activation of CB1 can lead to vasodilation and increase in heart rate leading to increased cardiac output and increased myocardial oxygen demand.5,12,41,42 Increased heart rate associated with atropine and epinephrine administration can be potentiated by cannabinoids.41 This can be concerning due to the potential of interference with anesthetics agents and physiologic data intraoperatively.
The data on chronic marijuana users are mixed: Moon et al43 found that chronic marijuana users have higher rates of heart disease, stroke, and coronary artery disease, although in general, the evidence supporting increased incidence of cardiac events in these patients is limited.5 Nonetheless, some authors suggest that surgery should not be performed if the patient has used cannabinoids within 72 hours of surgery because of this potential.44,45
A study published in the European Journal of Anesthesiology found that for chronic cannabinoid users, significantly larger amount of opioids were used to manage pain postoperatively compared with the nonuser group.46 Liu et al47 also reported increased postoperative pain and poor quality of sleep in the chronic cannabinoids users undergoing orthopedic surgery. In a prospective, randomized, single-blinded study, chronic cannabis users were found to require higher doses of propofol to achieve the desired level of anesthesia.12,48
WOUND HEALING APPLICATION
A lesser-known application of cannabinoids may be present in the area of wound healing. Cannabinoids have been implicated in regulation of fibroblast function, which play a pivotal role in wound healing. They are also involved in long-term wound healing by regulating the further differentiation of epidermal keratinocytes.49 HU-210, a structural analog of THC, has been proven to have an inhibitory effect on cellular proliferation, thereby increasing the anti-inflammatory properties of the wound.50 Further studies of these effects could result in topical wound healing adjuncts.
STATE OF MARIJUANA LEGALIZATION
Legislation regarding marijuana use may be classified into 3 categories of policy: MMLs, decriminalization, and legalization. MMLs protect patients from criminal prosecution for the use of marijuana for specific medical conditions. Decriminalization refers to policies that protect persons from criminal prosecution for possession of marijuana for personal use or nonmonetary distribution. However, in states with decriminalization laws, an individual in possession of marijuana may still receive a fine and subsequent charge on their criminal record. Legalization completely removes criminal and monetary penalties of any kind for recreational use, possession, and distribution of marijuana.51
Although marijuana continues to be illegal at the federal level,52 protections provided by MMLs in states with existing policies differ widely. These policies can restrict who may prescribe medical marijuana, what medical conditions it can be prescribed for, and how patients may obtain medical marijuana.51,53 For instance, in Colorado, patients may obtain medical marijuana from a local dispensary or home cultivation. However, in Wisconsin, the sale and distribution of medical marijuana remain illegal and patients must obtain the prescribed medical marijuana from out-of-state.2,53,54 State MMLs may also restrict the components present in the cannabis plant (THC and CBD) for medical marijuana use. For example, some states do not allow the use of products containing THC, whereas others may have no restrictions or low THC-to-CBD ratio requirements.51
RECOMMENDATIONS FOR THE PRACTICING PLASTIC SURGEON
Despite the presence of numerous studies that support therapeutic applications of marijuana and its associated compounds, there continues to be a lack of literature in regard to the use of cannabinoids in plastic surgery. Based on the evidence reviewed, there are 3 recommendations for the practicing plastic surgeons because they evaluate and manage patients who may be using marijuana for therapeutic or recreational reasons.
Pain Control
The literature supports the use of cannabinoids in the treatment of chronic pain, but data supporting its application for perioperative pain are lacking. This paucity of data calls for further research for the use of cannabinoids in acute pain, more specifically postoperative pain. It is important, however, to understand the need for increased analgesia to control postoperative pain in chronic marijuana users. Postoperative pain is a unique entity requiring a multimodal approach. Inflammatory components may be treated with anti-inflammatory medications. Cannabinoid research regarding efficacy in postoperative pain with direct correlation to specific types of pain will help provide more insight into how to best use this product.
Postoperative Nausea and Vomiting
The literature supports the use of cannabinoids in the treatment of CINV, but data supporting its application for treating nausea and vomiting associated with surgery are lacking. Being able to utilize known benefits of cannabinoids as a single agent is a promising area of research. Further research is required for conclusive application of cannabinoids in PONV.
Perioperative Consideration
Because cannabinoid receptors are located in vascular endothelium, cannabinoid use has a spectrum of potential consequences, from cardiac events to perfusion of local flaps, to the vascular physiology associated with free tissue transfer. Accordingly, a thorough history of marijuana use, including routes of consumption, frequency, and duration of use, should be a standard part of history taking during the preoperative visit. Side effects of marijuana, especially in chronic users, must be considered in the surgical patients.
CONCLUSIONS
As the cultural and political forces begin to move toward widespread acceptance and the use of cannabis and cannabis-related products, it is important that plastic surgeons maintain a working knowledge of cannabis and its effects, both therapeutic and nontherapeutic. Recreational use of marijuana will increase as its legalization becomes more widespread in the coming months and years. As for therapeutic use of cannabis, there are some applications where its utility is well-supported by quality data. However, for most issues impacting the typical plastic surgery patient, the data are scarce and require further development. It is important that plastic surgeons stay abreast of future studies and critically evaluate the implications it may have for their patients.
Supplementary Material
Footnotes
Published online 29 May 2020.
Presented as an abstract for ePoster at the Plastic Surgery Research Council 2020 Annual Meeting, May 28-31, 2020, Toronto, Ontario, Canada.
Disclosure: The authors have no financial interest to declare in relation to the content of this article.
Related Digital Media are available in the full-text version of the article on www.PRSGlobalOpen.com.
REFERENCES
- 1.Pew Research Center. U.S. public opinion on legalizing marijuana, 1969-2018. 2019. Available at https://www.pewresearch.org/fact-tank/2019/06/26/facts-about-marijuana/ft_19-06-26_marijuana_us-public-opinion-on-legalizing-marijuana-1969-2018/. Accessed September 30, 2019.
- 2.National Conference of State Legislatures. State medical marijuana laws. Available at http://www.ncsl.org/research/health/state-medical-marijuana-laws.aspx. Accessed September 16, 2019.
- 3.Substance Abuse and Mental Health Services Administration. Key substance use and mental health indicators in the United States: results from the 2018 National Survey on Drug Use and Health. 2019. HHS Publication No. PEP19-5068, NSDUH Series H-54. Available at https://www.samhsa.gov/data/. Accessed September 16, 2019.
- 4.World Health Organization. Management of substance abuse: cannabis. Available at https://www.who.int/substance_abuse/facts/cannabis/en/. Accessed September 16, 2019.
- 5.National Academies of Sciences, Engineering and Medicine The Health Effects of Cannabis and Cannabinoids: the Current State of Evidence and Recommendations for Research. 2017Washington, D.C. [PubMed] [Google Scholar]
- 6.Huestis MA.Human cannabinoid pharmacokinetics. Chem Biodivers. 2007;4:1770–1804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.NIDA. Marijuana. National Institute on Drug Abuse website. Available at: https://www.drugabuse.gov/publications/research-reports/marijuana. Accessed October 25, 2019.
- 8.Pertwee RG.Cannabinoid pharmacology: the first 66 years. Br J Pharmacol. 2006;147suppl 1163–167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Whiting PF, Wolff RF, Deshpande S, et al. Cannabinoids for medical use: a systematic review and meta-analysis. JAMA. 2015;313:2456–2473. [DOI] [PubMed] [Google Scholar]
- 10.Rahn EJ, Hohmann AG.Cannabinoids as pharmacotherapies for neuropathic pain: from the bench to the bedside. Neurotherapeutics. 2009;6:713–737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bakshi C, Barrett AM.Impact of recreational and medicinal marijuana on surgical patients: a review. Am J Surg. 2019;217:783–786. [DOI] [PubMed] [Google Scholar]
- 12.Bryson EO, Frost EAM.The perioperative implications of tobacco, marijuana, and other inhaled toxins. Int Anesthesiol Clin. 2011;49:103–118. [DOI] [PubMed] [Google Scholar]
- 13.Grotenhermen F.Pharmacokinetics and pharmacodynamics of cannabinoids. Clin Pharmacokinet. 2003;42:327–360. [DOI] [PubMed] [Google Scholar]
- 14.Marcu JP, Schechter JB.Preedy V.Molecular pharmacology of CB1 and CB2 cannabinoid receptors. In: Neuropathology of Drug Addictions and Substance Misuse 2016:1Elsevier Inc; 713–721. [Google Scholar]
- 15.Thomas A, Baillie GL, Phillips AM, et al. Cannabidiol displays unexpectedly high potency as an antagonist of CB1 and CB2 receptor agonists in vitro. Br J Pharmacol. 2007;150:613–623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Svíženská I, Dubový P, Šulcová A.Cannabinoid receptors 1 and 2 (CB1 and CB2), their distribution, ligands and functional involvement in nervous system structures—a short review. Pharmacol Biochem Behav. 2008;90:501–511. [DOI] [PubMed] [Google Scholar]
- 17.Hermanns-Clausen M, Kithinji J, Spehl M, et al. Adverse effects after the use of JWH-210—a case series from the EU Spice II plus project. Drug Test Anal. 2016;8:1030–1038. [DOI] [PubMed] [Google Scholar]
- 18.Mills B, Yepes A, Nugent K.Synthetic cannabinoids. Am J Med Sci. 2015;350:59–62. [DOI] [PubMed] [Google Scholar]
- 19.Kutner M.Synthetic Marijuana deaths tripled this year. 2015. Available at https://www.newsweek.com/synthetic-marijuana-deaths-tripled-year-342453. Accessed November 13, 2019.
- 20.Kelly BF, Nappe TM. Cannabinoid Toxicity. 2019 Available at http://www.ncbi.nlm.nih.gov/pubmed/29489164. Accessed December 2, 2019. [PubMed]
- 21.Adams IB, Martin BR.Cannabis: pharmacology and toxicology in animals and humans. Addiction. 1996;91:1585–1614. [PubMed] [Google Scholar]
- 22.Kumar RN, Chambers WA, Pertwee RG.Pharmacological actions and therapeutic uses of cannabis and cannabinoids. Anaesthesia. 2001;56:1059–1068. [DOI] [PubMed] [Google Scholar]
- 23.Spindle TR, Bonn-Miller MO, Vandrey R.Changing landscape of cannabis: novel products, formulations, and methods of administration. Curr Opin Psychol. 2019;30:98–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hindocha C, Freeman TP, Ferris JA, et al. No smoke without tobacco: a global overview of cannabis and tobacco routes of administration and their association with intention to quit. Front Psychiatry. 2016;7:104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Varlet V, Concha-Lozano N, Berthet A, et al. Drug vaping applied to cannabis: is “cannavaping” a therapeutic alternative to marijuana? Sci Rep. 2016;6:25599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Russell C, Rueda S, Room R, et al. Routes of administration for cannabis use—basic prevalence and related health outcomes: a scoping review and synthesis. Int J Drug Policy. 2018;52:87–96. [DOI] [PubMed] [Google Scholar]
- 27.Lamy FR, Daniulaityte R, Sheth A, et al. “Those edibles hit hard”: exploration of twitter data on cannabis edibles in the U.S. Drug Alcohol Depend. 2016;164:64–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bradford AC, Bradford WD.Medical marijuana laws reduce prescription medication use in Medicare part D. Health Aff (Millwood). 2016;35:1230–1236. [DOI] [PubMed] [Google Scholar]
- 29.Ilgen MA, Bohnert K, Kleinberg F, et al. Characteristics of adults seeking medical marijuana certification. Drug Alcohol Depend. 2013;132:654–659. [DOI] [PubMed] [Google Scholar]
- 30.Azim S, Nicholson J, Rebecchi MJ, et al. Endocannabinoids and acute pain after total knee arthroplasty. Pain. 2015;156:341–347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Holdcroft A, Maze M, Doré C, et al. A multicenter dose-escalation study of the analgesic and adverse effects of an oral cannabis extract (Cannador) for postoperative pain management. Anesthesiology. 2006;104:1040–1046. [DOI] [PubMed] [Google Scholar]
- 32.Hickernell TR, Lakra A, Berg A, et al. Should cannabinoids be added to multimodal pain regimens after total hip and knee arthroplasty? J Arthroplasty. 2018;33:3637–3641. [DOI] [PubMed] [Google Scholar]
- 33.Aviram J, Samuelly-Leichtag G.Efficacy of cannabis-based medicines for pain management: a systematic review and meta-analysis of randomized controlled trials. Pain Physician. 2017;20:E755–E796. [PubMed] [Google Scholar]
- 34.Levin DN, Dulberg Z, Chan AW, et al. A randomized-controlled trial of nabilone for the prevention of acute postoperative nausea and vomiting in elective surgery. Can J Anaesth. 2017;64:385–395. [DOI] [PubMed] [Google Scholar]
- 35.Beaulieu P.Effects of nabilone, a synthetic cannabinoid, on postoperative pain. Can J Anaesth. 2006;53:769–775. [DOI] [PubMed] [Google Scholar]
- 36.Buggy DJ, Toogood L, Maric S, et al. Lack of analgesic efficacy of oral δ-9-tetrahydrocannabinol in postoperative pain. Pain. 2003;106:169–172. [DOI] [PubMed] [Google Scholar]
- 37.Smith LA, Azariah F, Lavender VT, et al. Cannabinoids for nausea and vomiting in adults with cancer receiving chemotherapy. Cochrane Database Syst Rev. 2015;2015:CD009464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jewer JK, Wong MJ, Bird SJ, et al. Supplemental peri-operative intravenous crystalloids for postoperative nausea and vomiting: an abridged Cochrane systematic review. Anaesthesia. 2020;75:254–265. [DOI] [PubMed] [Google Scholar]
- 39.Kleine-Brueggeney M, Greif R, Brenneisen R, et al. Intravenous delta-9-tetrahydrocannabinol to prevent postoperative nausea and vomiting: a randomized controlled trial. Anesth Analg. 2015;121:1157–1164. [DOI] [PubMed] [Google Scholar]
- 40.Broughton G, II, Crosby MA, Coleman J, et al. Use of herbal supplements and vitamins in plastic surgery: a practical review. Plast Reconstr Surg. 2007;119:48e–66e. [DOI] [PubMed] [Google Scholar]
- 41.Beaconsfield P, Ginsburg J, Rainsbury R.Marihuana smoking. Cardiovascular effects in man and possible mechanisms. N Engl J Med. 1972;287:209–212. [DOI] [PubMed] [Google Scholar]
- 42.Benowitz NL, Jones RT.Cardiovascular and metabolic considerations in prolonged cannabinoid administration in man. J Clin Pharmacol. 1981;21:214S–223S. [DOI] [PubMed] [Google Scholar]
- 43.Moon AS, Smith W, Mullen S, et al. Marijuana use and mortality following orthopedic surgical procedures. Subst Abus. 2019;40:378–382. [DOI] [PubMed] [Google Scholar]
- 44.Huson HB, Granados TM, Rasko Y.Surgical considerations of marijuana use in elective procedures. Heliyon. 2018;4:e00779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Gregg JM, Campbell RL, Levin KJ, et al. Cardiovascular effects of cannabinol during oral surgery. Anesth Analg. 1976;55:203–213. [DOI] [PubMed] [Google Scholar]
- 46.Jamal N, Korman J, Musing M, et al. Effects of pre-operative recreational smoked cannabis use on opioid consumption following inflammatory bowel disease surgery: a historical cohort study. Eur J Anaesthesiol. 2019;36:705–706. [DOI] [PubMed] [Google Scholar]
- 47.Liu CW, Bhatia A, Buzon-Tan A, et al. Weeding out the problem: the impact of preoperative cannabinoid use on pain in the perioperative period. Anesth Analg. 2019;129:874–881. [DOI] [PubMed] [Google Scholar]
- 48.Flisberg P, Paech MJ, Shah T, et al. Induction dose of propofol in patients using cannabis. Eur J Anaesthesiol. 2009;26:192–195. [DOI] [PubMed] [Google Scholar]
- 49.Tóth KF, Ádám D, Bíró T, et al. Cannabinoid signaling in the skin: therapeutic potential of the “c(ut)annabinoid” system. Molecules. 2019;24:E918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Palmieri B, Laurino C, Vadalà M.A therapeutic effect of cbd-enriched ointment in inflammatory skin diseases and cutaneous scars. Clin Ter. 2019;170:e93–e99. [DOI] [PubMed] [Google Scholar]
- 51.Pacula RL, Smart R.Medical marijuana and marijuana legalization. Annu Rev Clin Psychol. 2017;13:397–419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Annas GJ.Reefer madness--the federal response to California’s medical-marijuana law. N Engl J Med. 1997;337:435–439. [DOI] [PubMed] [Google Scholar]
- 53.Pacula RL, Hunt P, Boustead A.Words can be deceiving: a review of variation among legally effective medical marijuana laws in the United States. J Drug Policy Anal. 2014;7:1–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Legislative Reference Bureau. Marijuana laws and Wisconsin. Wisconsin Briefs. 2015. Retrieved from https://docs.legis.wisconsin.gov/2015/related/proposals/sb789. Accessed May 20, 2020.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


