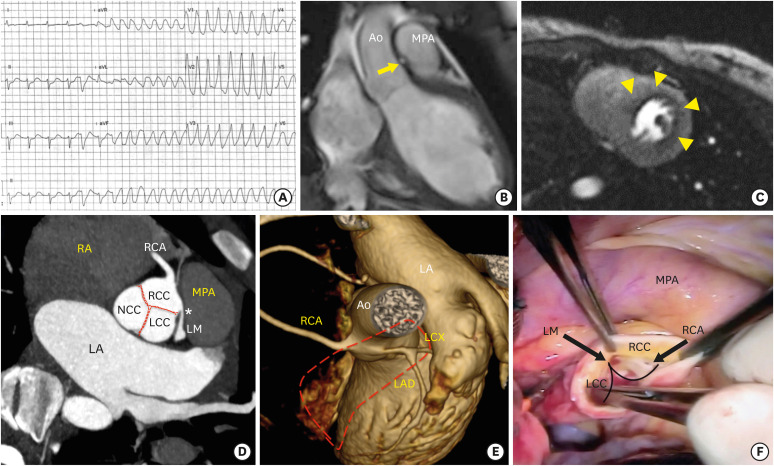
A 14-year-old girl with unremarkable medical history was brought to our hospital owing to a brief episode of a sudden loss of consciousness during the cheerleading practice without preceding chest pain or palpitation. Upon arrival, she was oriented and cooperative. The initial rhythm on electrocardiogram was sinus tachycardia with nonspecific ST-segment depression in lead II, III and aVF, which suddenly turned to ventricular tachycardia (Figure 1A) followed by ventricular fibrillation causing cardiac arrest. She was defibrillated immediately with the return of spontaneous circulation in less than 3 minutes. A transthoracic echocardiogram showed normal left ventricular systolic function without wall motion abnormality. The aortic cusps appeared normal. The patient subsequently underwent cardiovascular magnetic resonance (CMR) to evaluate structural heart disease and myocardial ischemia. Notably, the coronal view of cine image demonstrated an abnormal tubular structure interposing between the aortic root and main pulmonary artery (arrow, Figure 1B, Movie 1). Shot axis view of adenosine stress perfusion image revealed a large area of inducible perfusion defect at anteroseptal, anterior and lateral walls, in the distribution of left main artery (LM) territory (arrows, Figure 1C). Based on all CMR findings, the anomalous origin of left coronary artery causing myocardial ischemia was suspected. The coronary computed tomography angiography demonstrated the origin of LM artery arising from right coronary cusp (RCC), coursing between the aortic root and pulmonary artery (Figure 1D and E). Pressure effect from the aorta and pulmonary artery to LM caused acute angle at the ostium (asterisk, Figure 1D) resulting in luminal narrowing. These confirmed the diagnosis of the inter-arterial type of anomalous LM arising from RCC caused malignant arrhythmia, hence the coronary angiography was deemed unnecessary in order to avoid further radiation exposure. Intraoperative findings revealed the right coronary artery normally originated from RCC while the LM abnormally arose from RCC (arrows, Figure 1F). She underwent the relocation of LM to left coronary cusp with uneventful postoperative follow-up.
Figure 1. (A) The initial electrocardiogram revealed sinus rhythm, which suddenly turned to ventricular tachycardia. (B) The coronal view of cine cardiovascular magnetic resonance image demonstrated an abnormal tubular structure (arrow) interposing between the aortic root and MPA. (C) Shot axis view of adenosine stress perfusion image revealed a large area of inducible perfusion defect (arrows) in the distribution of LM territory. (D) The coronary computed tomography angiography showed the origin of LM arising from RCC with acute angle at the ostium (asterisk) coursing between the Ao and pulmonary artery (E). (F) Intraoperative finding revealed the LM abnormally arose from RCC. Ao: aorta, LA: left atrium, LAD: left anterior descending artery, LCC: left coronary cusp, LCX: left circumflex artery, LM: left main coronary artery, MPA: main pulmonary artery, NCC: non-coronary cusp, RA: right atrium, RCA: right coronary artery, RCC: right coronary cusp. Dashed line represents the cutaway MPA.
Inter-arterial type is the most common form of an anomalous coronary artery from opposite sinus that associates with sudden cardiac death in adolescence.1),2) This case highlights an important role of multimodality imaging by providing a complete anatomic description and functional assessment before contemplating the surgical strategy.
Footnotes
Conflict of Interest: The authors have no financial conflicts of interest.
SUPPLEMENTARY MATERIAL
The coronal view of cine cardiovascular magnetic resonance image demonstrate an abnormal tubular structure interposing between the great vessels.
References
- 1.Cheezum MK, Ghoshhajra B, Bittencourt MS, et al. Anomalous origin of the coronary artery arising from the opposite sinus: prevalence and outcomes in patients undergoing coronary CTA. Eur Heart J Cardiovasc Imaging. 2017;18:224–235. doi: 10.1093/ehjci/jev323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Finocchiaro G, Behr ER, Tanzarella G, et al. Anomalous coronary artery origin and sudden cardiac death: clinical and pathological insights from a national pathology registry. JACC Clin Electrophysiol. 2019;5:516–522. doi: 10.1016/j.jacep.2018.11.015. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The coronal view of cine cardiovascular magnetic resonance image demonstrate an abnormal tubular structure interposing between the great vessels.