Abstract
Italy was the first western hotspot of the COVID-19 pandemic. In order to contain the spread of the virus, the Italian Government imposed home confinement to the entire population for almost two months. The present study is the first large-scale longitudinal report of the sleep and mental health changes during the prolonged lockdown due to the COVID-19 outbreak. We focused on the gendered vulnerability in a sample of the Italian population since cross-sectional research identified women to be more at-risk than men during this unprecedented situation.
A total of 2701 individuals (mean age ± standard deviation, 32.37 ± 11.62; range, 18–82) participated in a web-based longitudinal survey consisting of two measurements. Participants were first-time recruited on social networks and via telephone messages through a snowball sampling and tested during the third week of the lockdown period. Subsequently, a follow-up evaluation was carried out during the seventh week of restraining measures. The survey assessed sleep quality, insomnia and depression symptoms, perceived stress, and anxiety, using the following questionnaires: the Pittsburgh Sleep Quality Index, the Insomnia Severity Index, the Beck Depression Inventory-second edition, the 10-item Perceived Stress Scale, and the State-Anxiety Inventory.
Female gender showed the worst condition for all the examined dimensions in both the assessments. Nevertheless, at the follow-up women reported a reduction in insomnia and depression severity symptoms, perceived stress, and anxiety. On the other hand, male participants showed a worsening of sleep quality, insomnia symptoms, and perceived stress. Consequently, the gender prevalence gap of clinical conditions such as insomnia and depression was largely reduced under lockdown.
Our investigation pointed to a different time course of sleep and mental health between genders during the home confinement period. Women seemed to show greater long-term resilience during the lockdown. Meanwhile, the male gender emerges as the most vulnerable category to the extension of the restraining measures. Our results suggest that there is no “weaker gender” after a prolonged lockdown. Indeed, the Italian population transversely presented signs of psychological suffering and significant sleep disturbances after the protracted and stressful lockdown period due to the COVID-19 pandemic.
Keywords: COVID-19 lockdown, Gender, Longitudinal, Stress, Sleep disturbances, Mental health
Highlights
-
•
Women maintain the most severe sleep and psychological disturbances during lockdown.
-
•
Only men show a deterioration over time of sleep and psychological well-being.
-
•
Women prove a greater long-term resilience to the extension of the home confinement.
-
•
Gender gap of clinical insomnia and depression decreases after one month of lockdown.
1. Introduction
From December 2019, the new Coronavirus (SARS-CoV-2) started to spread in China. This virus led to COVID-19, an acute respiratory syndrome linked to a potentially life-threatening pneumonia disease. In a few months, the outbreak quickly spread throughout the world until it was categorized as a pandemic by the World Health Organization (World Health Organization, 2020a). Italy was the first western hotspot of COVID-19. In line with China, the Italian Government adopted extraordinary measures aimed at limiting the contagion. Since March 9, 2020, a total lockdown was imposed, which forced the entire population into home confinement. The restraining measures were extended until May 4, 2020, resulting in approximately two months of confinement. This unprecedented situation profoundly impacted the everyday life of all Italian citizens. The limitation of social interaction and the restriction of movement freedom could be linked to consistent psychological impact among the general population (Brooks et al., 2020).
Increased stress and exacerbation of depression and anxiety symptomology was reported in China as in the rest of the world during the COVID-19 pandemic (Rajkumar, 2020; Vindegaard and Benros, 2020). Moreover, in a situation where the rhythms of life were deeply altered, sleep has been proposed as one of the primary targets to be impacted, as well as a crucial mediator of mental health outcomes (Altena et al., 2020). Recent cross-sectional studies on the psychological impact of the COVID-19 pandemic focused on specific at-risk groups, such as healthcare professionals (Pappa et al., 2020), and referred to limited periods. Some studies addressed longitudinally the impact of the current situation but used pre-outbreak baselines (Pierce et al., 2020; Cellini et al., 2020; Wright et al., 2020). Therefore, the large-scale temporal impact of the restraining measures within the general population has been scarcely studied. Because of the protracted duration of the home confinement, it is fundamental to investigate the long-term consequences of this extraordinary situation. To our knowledge, this is the first study that longitudinally addresses the within-subject psychological impact of seven weeks of home confinement in the same large sample of the general population during a public pandemic catastrophe. Two thousand seven hundred one Italian citizens were tested using a web-based survey in two time periods: during the third and the seventh week of lockdown. The survey assessed sleep quality, insomnia and depression symptoms, perceived stress, and anxiety.
This study aimed at investigating the changes in the above-mentioned variables during the extended lockdown, to address the hypothesis that the restraining measures could have had a cumulative negative impact on the mental health of the general population. Different from previous research works, we took into account gender differences to evaluate if men and women suffered differently from this situation. The importance of gender-disaggregated data was strongly suggested as regards COVID-19 vulnerability (Wenham et al., 2020). This is also crucial on the psychological side since the risk for psychopathology markedly differs between men and women, and women represent a high-risk category for mental health problems such as depression, anxiety, and post-traumatic stress disorder (PTSD; Malhi and Mann, 2018; World Health Organization, 2020b; Olff et al., 2007). In this view, women could suffer the COVID-19 lockdown more severely, and preliminary cross-sectional studies reported female gender to be a vulnerability factor for developing psychological symptoms during the early stage of the pandemic (Vindegaard and Benros, 2020; Mazza et al., 2020; Wang et al., 2020a; Casagrande et al., 2020; Salfi et al., 2020; Ozdin and Ozdin, 2020; Léger et al., 2020).
The present investigation has two main peculiarities. First of all, we showed the trajectories of the progress of sleep and psychological well-being within the same population during the extended lockdown period. Secondly, it is the first investigation to address the different progression of sleep disturbances and psychological symptoms for men and women. Our results are useful to identify gender-specific timing of intervention to prevent and counteract the long-term development of mental health problems during this unprecedented situation.
2. Materials and methods
2.1. Participants and procedure
7107 Italian citizens (mean age ± standard deviation, 32.38 ± 11.38; range, 18–84; 1616 men) completed a web-based survey during the third week of the home confinement (Test 1; 25–31 March 2020), the days immediately following the peak of contagion (Istituto Superiore di Sanità, 2020). The questionnaires have been disseminated through a snowball technique (i.e., respondents were encouraged to recruit other participants) on social networks and via telephone messages. Given the self-selected and non-probabilistic nature of the data collection, we could not assess the response rate, as indicated by the American Association for Public Opinion Research (AAPOR) reporting guideline. The survey assessed demographic information, sleep quality, insomnia and depression symptoms, perceived stress, and anxiety, using the following validated questionnaires (in order of presentation): the Pittsburgh Sleep Quality Index (PSQI; Curcio et al., 2013), the Insomnia Severity Index (ISI; Castronovo et al., 2016), the Beck Depression Inventory-second edition (BDI-II, Ghisi et al., 2006), the 10-item Perceived Stress Scale (PSS-10; Mondo et al., 2019), the state-anxiety subscale of the State-Trait Anxiety Inventory (STAI-X1; Spielberger et al., 1970). On average, 10 min were needed to complete the sleep questionnaires; after that participants were free to decide whether to stop after each of the three questionnaires tapping into mental health problems. This feature was implemented to avoid a false-response bias, ensuring greater reliability of the collected responses. After four weeks, the website link of the follow-up survey was provided to the participants via email address/telephone number. A total of 2701 individuals (mean age ± standard deviation, 32.37 ± 11.62; range, 18–82; 491 men) participated in the follow-up assessment (Test 2) in seven days (21–27 April 2020), completing the same questionnaires of the first measurement time. The local institutional review board at the University of L'Aquila approved the current study (protocol n. 43,066). Online informed consent was obtained from the participants. The study has been carried out according to the principles established by the Declaration of Helsinki.
2.2. Questionnaires
The survey was developed using Google Form. Sociodemographic information about age, gender, education, occupation, and geographical location was surveyed. Additionally, participants indicated if they had been subjected to forced quarantine or any relative/friend have contracted COVID-19 from the time of the first compilation (Table 1). The PSQI (Curcio et al., 2013) is a validated tool to assess sleep quality and disturbances. It consists of nineteen questions, from which a total score is calculated ranging from 0 to 21. The ISI (Castronovo et al., 2016) measures the severity of insomnia symptoms through seven questions. The score ranges from 0 to 28. The BDI-II (Ghisi et al., 2006) evaluates the symptoms of depression. It consists of 21 items, and the total score (range score, 0–63) is a valid measure of depression severity. The PSS-10 (Mondo et al., 2019) is a 10-item questionnaire evaluating thoughts and feelings of subjects referred to stressful events. The total score ranges from 0 to 50, and it is an indicator of perceived stress. The STAI-X1 (Spielberger et al., 1970) is a well-established anxiety scale included in the Cognitive Behavioural Assessment battery 2.0 (Sanavio et al., 1998). It comprises 20 items, and the total score is a valid measure of state anxiety. For all questionnaires, higher scores indicate more serious conditions. Of note, ISI and BDI-II are conceived as clinical instruments, and validated cut-off scores are available in the literature. In particular, a score >14 for ISI identifies moderate/severe insomnia. For BDI-II, a score >28 denotes severe clinical depression.
Table 1.
Demographic and COVID-related characteristics of the sample participating in both the measurements (Test 1: 25–31 March 2020; Test 2: 21–27 April 2020).
| No. (%) |
|||
|---|---|---|---|
| Overall sample (N=2701) | Men (N=491) | Women (N=2210) | |
| Demographic variables | |||
| Age | |||
| 18–30 years | 1617 (59.9) | 280 (57.0) | 1337 (60.5) |
| 31–50 years | 783 (29.0) | 137 (27.9) | 646 (29.2) |
| > 50 years | 301 (11.1) | 74 (15.1) | 227 (10.3) |
| Education | |||
| Until middle school | 36 (1.3) | 10 (2.0) | 26 (1.2) |
| High school | 851 (31.5) | 182 (37.1) | 669 (30.3) |
| Graduated | 1814 (67.2) | 299 (60.9) | 1515 (68.5) |
| Occupation | |||
| Unemployed | 231 (8.6) | 36 (7.3) | 195 (8.8) |
| Employed | 1545 (57.2) | 299 (60.9) | 1246 (56.4) |
| Student | 925 (34.2) | 156 (31.8) | 769 (34.8) |
| Geographical location | |||
| Northern Italya | 991 (36.7) | 175 (35.6) | 816 (36.9) |
| Central Italyb | 800 (29.6) | 144 (29.3) | 656 (29.7) |
| Southern Italyc | 910 (33.7) | 172 (35.0) | 738 (33.4) |
| COVID-related information | |||
| COVID-19 infection | |||
| Yes | 7 (0.3) | 1 (0.2) | 6 (0.3) |
| No | 2673 (99.0) | 484 (98.6) | 2189 (99.0) |
| No response | 21 (0.8) | 6 (1.2) | 15 (0.7) |
| Forced Quarantine | |||
| Yes | 97 (3.6) | 17 (3.5) | 80 (3.6) |
| No | 2601 (96.3) | 474 (96.5) | 2127 (96.2) |
| No response | 3 (0.1) | 0 (0) | 3 (0.1) |
| Relative/friend with COVID-19 | |||
| Yes | 600 (22.2) | 97 (19.8) | 503 (22.8) |
| No | 2085 (77.2) | 391 (79.6) | 1694 (76.7) |
| No response | 16 (0.6) | 3 (0.6) | 13 (0.6) |
Northern Italy: Aosta Valley, Emilia Romagna, Friuli-Venezia Giulia, Liguria, Lombardy, Piedmont, Trentino-Alto Adige, and Veneto.
Central Italy: Lazio, Marche, Tuscany, and Umbria.
Southern Italy: Abruzzo, Apulia, Basilicata, Calabria, Campania, Molise, Sardinia, and Sicily.
2.3. Statistical analysis
We carried out several preliminary analyses to assess the robustness and reliability of the data. To control for potential selection bias of the follow-up respondents based on the examined variables (PSQI, ISI, BDI-II, PSS-10, STAI-X1), we performed mixed-model analyses on the questionnaire scores of all participants who took the Test 1, using “Test 2 participation” (yes, no), “gender” (man, woman) and their interaction as predictors. Neither significant effect of “Test 2 participation” nor an interaction between the two predictors has been highlighted by the analyses (all P > 0.10). Additionally, because of the facultative nature of the last three questionnaires tapping into mental health problems, we performed the Little's MCAR test on these variables, which showed that missing questionnaires occurred completely at random, both at Test 1 (χ2 = 1.78, P = 0.63) and Test 2 (χ2 = 3.64, P = 0.30).
To evaluate the changes between Test 1 and Test 2, the questionnaire scores (PSQI, ISI, BDI-II, PSS-10, STAI-X1) were submitted to mixed model analyses with a random intercept per participant, to account for the correlation of questionnaire scores within each subject and intraindividual variability. The main models included “time” (Test 1, Test 2), “gender” (man, woman), and their interaction as predictors. Explorative analyses taking into account the interaction between “gender”, “time”, and the other demographic and COVID-related variables did not yield any significant effect (all P > 0.10). Therefore, the other demographic factors were collapsed and are not reported in the results. Analyses were performed using the “lme4” R package (Bates et al., 2015) weighting the estimates according to the gender prevalence within the Italian population. Models were fitted using REML, and P-values were obtained using the Satterthwaite approximation. Bonferroni post hoc tests were computed using the “emmeans” R package (Lenth et al., 2020). Statistical significance was set at P < 0.05, and all tests were 2-tailed. To check for potential biases due to the unbalanced gender composition of the sample, a randomized female sample corresponding to an equal number of male participants (n = 491) was extracted from the overall follow-up sample using SPSS v.22 (IBM Corp, Armonk, NY, USA). Then, the mixed model analyses applied to the total sample were replicated, confirming the outcomes of the main models.
Finally, the prevalence of moderate/severe insomnia and severe depression were computed according to the validated cut-off scores. Subsequently, logistic regression analyses were performed to evaluate the difference between genders of the prevalence of insomnia and depression clinical conditions at the two measurement times.
3. Results
The follow-up measurement was characterized by higher scores in all the questionnaires, except for the PSQI. Specifically, the “time” factor was significant for ISI (B = −0.33, t2825.60 = −2.86, P = 0.004), BDI-II (B = −0.37, t2300.62 = −2.23, P = 0.026), PSS-10 (B = −0.83, t2772.82 = −4.37, P < 0.001), and STAI-X1 (B = −1.40, t2378.21 = −5.93, P < 0.001), while PSQI did not (B = 0.04, t2669.22 = 0.48, P = 0.63).
Gender was significant in all the analyses, showing higher mean scores of women in all the examined dimensions (PSQI: B = −1.90, t5105.86 = −8.33, P < 0.001; ISI: B = −2.69, t5397.85 = −8.04, P < 0.001; BDI-II: B = −4.72, t4390.48 = −8.22, P < 0.001; PSS-10: B = −7.35, t4059.06 = −15.20, P < 0.001; STAI-X1: B = −5.06, t4337.02 = −7.48, P < 0.001).
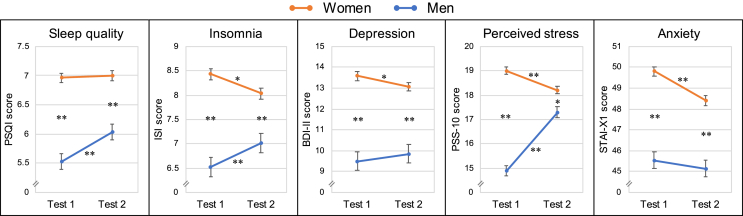
Finally, all the mixed model analyses highlighted significant interactions between “time” and “gender” factors (PSQI: B = 0.47, t2649.43 = 3.99, P < 0.001; ISI: B = 0.82, t2825.60 = 4.86, P < 0.001; BDI-II: B = 0.74, t2288.67 = 2.97, P = 0.003; PSS-10: B = 3.24, t2769.66 = 11.47, P < 0.001; STAI-X1: B = 0.86, t2360.38 = 2.45, P = 0.014). Interaction plots and post hoc results are reported in Fig. 1.
Fig. 1.
Interaction between “time” and “gender” factors for the PSQI (sleep quality), ISI (insomnia), BDI-II (depression), PSS-10 (perceived stress), and STAI-X1 (anxiety) questionnaires. Mean (and standard error) of questionnaires scores in the two assessments (Test 1: 25–31 March 2020; Test 2: 21–27 April 2020) for men (in blue) and women (in orange). Bonferroni post hoc results are reported with asterisks (*P < 0.05; **P < 0.001).
Post hoc comparisons showed that, after four weeks of home confinement, male participants exhibited an increment in PSQI, ISI, and PSS-10 scores (all P < 0.001). On the other hand, women reported a reduction in insomnia and depression symptoms, perceived stress, and anxiety (P = 0.025; P = 0.045; P < 0.001; P < 0.001, respectively). Notwithstanding this, in both the measurement occasions, female participants reported significantly higher scores on all the variables (PSS-10 at Test 2: P = 0.005; all the other P < 0.001).
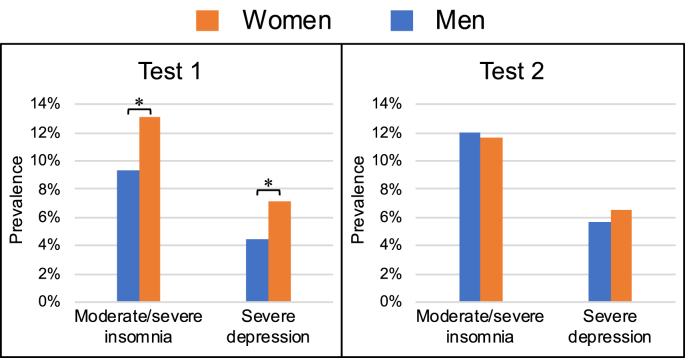
Logistic regression analyses of data reported in Fig. 2, revealed a higher female prevalence of moderate/severe insomnia and severe depression at Test 1 (moderate/severe insomnia: 13.12% vs. 9.37%, odd ratio (OR) = 0.68, P = 0.023; severe depression: 7.20% vs. 4.47%, OR = 0.60, P = 0.049). The gap in gender prevalence was no longer present at Test 2 both for moderate/severe insomnia (women: 11.63%, men: 12.02%; OR = 1.04, P = 0.81) and severe depression (women: 6.50%, men: 5.71%; OR = 0.87, P = 0.56). Indeed, men tended to worsen their condition during the lockdown (moderate/severe insomnia: +2.65%; severe depression: +1.24%), while women tended to improve it (moderate/severe insomnia: -1.49%; severe depression: -0.70%). Further analyses of the modifications of the clinical status by gender confirmed that the changes from Test 1 to Test 2 differed according to the gender (moderate/severe insomnia: χ2 = 6.49, P = 0.04, severe depression: χ2 = 9.16, P = 0.01; respectively).
Fig. 2.
Prevalence rates of men (in blue) and women (in orange) reporting moderate to severe insomnia and severe depression at the two assessments (Test 1: 25–31 March 2020; Test 2: 21–27 April 2020). Logistic regression significance is reported with asterisks (*P < 0.05).
4. Discussion
Our longitudinal study showed a different time course of sleep disturbances and mental health problems in men and women during the COVID-19 pandemic in Italy.
Women had consistently higher scores than men on sleep and mental health scales, especially at the beginning of the lockdown period. It should be noted that this is not a peculiarity of this extraordinary period. Previous research showed that women score is higher on PSQI in a wide range of countries and cultures (Curcio et al., 2013; Wong and Fielding, 2011; Hinz et al., 2017) and the female population typically has the highest prevalence of insomnia symptoms (Zhang and Wing, 2006). The prevalence of depression and anxiety is also higher for women (Malhi and Mann, 2018; World Health Organization, 2020b). Furthermore, women are marked by higher stress perception and have an increased likelihood of developing PTSD symptoms (Olff et al., 2007). Consequently, our results are in line with the literature of the pre-outbreak period.
However, the prolonged period of home confinement reduced the gender gap in two important ways. On one hand, women seemed to be more resilient than men, in the long run, exhibiting a slight trend toward improvement of insomnia, depression, anxiety, and distress at the end of the seven weeks covered by the present research. On the other hand, men showed an exacerbation of insomnia symptoms and a deterioration of sleep quality during the lockdown. Furthermore, male participants reported a substantial increment of perceived stress at the end of the study. In addition, although women reported a higher prevalence of clinical conditions such as insomnia and depression in the first part of the lockdown, the gender gap was narrowed after four weeks.
A recent study (Wang et al., 2020b) evaluated stress, anxiety, and depression in two samples of the general Chinese population that was assessed four weeks apart during the COVID-19 outbreak. No significant changes were reported at the overall-sample level. However, gender differences were not taken into account, participants were not forced into home confinement, and the study used a cross-sectional design. All these factors could explain the inconsistencies with our results.
The differential trend of mental health indicators in women and men during the long confinement period was peculiar and unexpected. Of note, the difference among gender trajectories was confirmed controlling for the other demographic variables such as age, education, and occupation. Because none of the variables collected in the present study could explain this effect, we believe that dispositional or sociocultural gender differences interacted with the extended period of restraining measures.
Men and women respond to stress differently, at both physiological and behavioral levels. According to an evolutionary perspective, the primary response aimed at reducing stress in men is a ‘fight-or-flight’ reaction, whereas women are likely to adopt a ‘tend-and-befriend’ one (Taylor et al., 2000). These patterns are supported by neuroendocrine and behavioral evidence (Verma et al., 2011). In this view, the dispositional stress response of women may have proven to be more appropriate when dealing with the current challenging time since the importance of community support and prosocial behaviors has been repeatedly emphasized to cope with the forced home confinement situation (Holmes et al., 2020; Courtet et al., 2020; Centers for Disease Control and Prevention, 2020).
From a sociocultural perspective, our results could reflect deep-rooted differences in gender roles within western societies. Particularly in Italy, women have traditionally held a prominent position in the domestic environment compared to men. The gendered time course of the impact of prolonged lockdown might be explained because the extended home confinement period largely compromised each individual's public life, preserving and emphasizing the domestic one at the same time.
Another possible interpretation is that men might manifest the psychological impact of the lockdown only after a prolonged period. On the other hand, women may have been the first to suffer the consequences of the home confinement situation because of their front-line role in the family care typical of Italian society. Consequently, women might have already reached the peak of psychological distress during the first days of the lockdown, subsequently adapting better to this extraordinary situation.
A final consideration refers directly to the gendered vulnerability to COVID-19. In Italy, as in the rest of the world, the progress of contagion was accompanied by the awareness of a higher prevalence of hospitalizations and deaths among men (Global Health 5050, 2020). This information was widely disseminated by the media during the period from the first to the second measurement time of our study and may have evoked a more danger in the male population, putatively contributing to explain our pattern of results.
Our findings are inconsistent with a general framework that predicts female gender to be a vulnerability factor tout court (Vindegaard and Benros, 2020; Mazza et al., 2020; Wang et al., 2020a; Casagrande et al., 2020; Ozdin and Ozdin, 2020; Léger et al., 2020). A crucial point to stress is that, to date, studies based on a single measurement could be elusive concerning the actual psychological suffering of men. The well-known difference between genders in all the examined dimensions could lead to focus the psychological support on women. Instead, our investigation suggests that there is no “weaker gender” under lockdown and, sooner or later, both men and women can be strongly affected by this unprecedented situation.
Furthermore, our investigation did not confirm recent cross-sectional studies highlighting occupation or age as vulnerability factors (Casagrande et al., 2020; Cellini et al., 2020; Marelli et al., 2020). Because this is a longitudinal study, we investigated the presence of predictors which explained the changes over time in the examined variables. This peculiarity can explain the inconsistencies with the current literature based on a single measurement. Although the number of infections in Italy is declining at the moment, with a consequent relaxation of the restraining measures, our results could be of particular interest to the countries around the world where the contagion is ongoing, and home confinement measures still are an integral part of everyday life. The second wave of infections is also feared at the end of the summer or during the fall (Horton, 2020), and a further period of home confinement cannot be excluded.
The present findings could help to identify the timing for therapeutic interventions aimed at boosting coping skills and resilience and protecting the psychological well-being, counteracting the risk of developing mental health problems among the general population. In particular, our investigation highlights two crucial points. First of all, it confirms the urgency to predispose immediate psychological support focused on women since the beginning of the lockdown. Secondly, the present findings suggest that, with the advancement of the weeks, it is essential to shift the attention to men, who seem to be the primary category to suffer from the cumulative effects of the prolonged restraining measures during the COVID-19 pandemic. The sleep dimension emerges as the most affected by the lockdown extension among the male population. In this view, our results suggest predisposing specific sleep-focused interventions. This could be particularly important when considering the contribution of sleep disturbances in the development of mental health problems (Freeman et al., 2017).
Finally, our investigation confirms the assumption that the governments should keep the lockdown as short as possible and avoid an overly precautionary approach (Brooks et al., 2020) to limit long-term psychological consequences, especially on male citizens.
To our knowledge, this is the first study reporting large-scale longitudinal changes of sleep disturbances and the risk of mental health deterioration among the same population under home-confinement. However, some limitations need to be reported. The main one is the impossibility of determining the sampling bias in Test 1 because of the sampling technique. We can not exclude that the present study inadvertently attracted individuals reporting the most serious conditions as regards the examined dimensions. Nevertheless, this bias would be expected at the overall sample level, putatively not affecting the gendered trajectories here highlighted. Secondly, it should be acknowledged that the composition of the experimental sample is substantially unbalanced towards the female gender. Finally, our results were obtained in an Italian sample. Deep-rooted social gender inequities mark Italian society. Further longitudinal investigations could confirm our pattern of results within other populations.
Formatting of funding sources
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
CRediT authorship contribution statement
Federico Salfi: Conceptualization, Methodology, Investigation, Data curation, Formal analysis, Writing - original draft, Writing - review & editing. Marco Lauriola: Formal analysis, Writing - review & editing. Giulia Amicucci: Investigation, Writing - review & editing. Domenico Corigliano: Investigation, Writing - review & editing. Lorenzo Viselli: Investigation, Writing - review & editing. Daniela Tempesta: Writing - review & editing. Michele Ferrara: Conceptualization, Methodology, Supervision, Writing - review & editing.
Declaration of competing interest
The authors declare that they have no known competing financial interests that could have appeared to influence the work reported in this paper.
References
- Altena E., Baglioni C., Espie C.A. Dealing with sleep problems during home confinement due to the COVID‐19 outbreak: practical recommendations from a task force of the European CBT‐I Academy. J. Sleep Res. 2020 doi: 10.1111/jsr.13052. [DOI] [PubMed] [Google Scholar]
- Bates D., Mächler M., Bolker B.M., Walker S.C. Fitting linear mixed-effects models using lme4. J. Stat. Software. 2015;67:1–48. doi: 10.18637/jss.v067.i01. [DOI] [Google Scholar]
- Brooks S.K., Webster R.K., Smith L.E. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395:912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casagrande M., Favieri F., Tambelli R., Forte G. The enemy who sealed the world: effects quarantine due to the COVID-19 on sleep quality, anxiety, and psychological distress in the Italian population. Sleep Med. 2020 doi: 10.1016/j.sleep.2020.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castronovo V., Galbiati A., Marelli S. Validation study of the Italian version of the insomnia severity index (ISI) Neurol. Sci. 2016;37:1517–1524. doi: 10.1007/s10072-016-2620-z. [DOI] [PubMed] [Google Scholar]
- Cellini N., Canale N., Mioni G., Costa S. Changes in sleep pattern, sense of time and digital media use during COVID‐19 lockdown in Italy. J. Sleep Res. 2020 doi: 10.1111/jsr.13074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention Coping with stress. 2020. https://www.cdc.gov/coronavirus/2019-ncov/daily-life-coping/managing-stress-anxiety.html
- Courtet P., Olié E., Debien C., Vaiva G. Keep socially (but not physically) connected and carry on: preventing suicide in the age of COVID-19. J. Clin. Psychiatr. 2020;81:20com13370. doi: 10.4088/JCP.20com13370. [DOI] [PubMed] [Google Scholar]
- Curcio G., Tempesta D., Scarlata S. Validity of the Italian version of the pittsburgh sleep quality index (PSQI) Neurol. Sci. 2013;34:511–519. doi: 10.1007/s10072-012-1085-y. [DOI] [PubMed] [Google Scholar]
- Freeman D., Sheaves B., Goodwin G.M. The effects of improving sleep on mental health (OASIS): a randomised controlled trial with mediation analysis. Lancet Psychiatry. 2017;4:749–758. doi: 10.1016/S2215-0366(17)30328-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghisi M., Flebus G., Montano A., Sanavio E., Sica C. Giunti Editore; Firenze, IT: 2006. Beck Depression Inventory-II: Edizione Italiana. [Google Scholar]
- Global Health 5050 COVID-19 sex-disaggregated data tracker. 2020. https://globalhealth5050.org/covid19/sex-disaggregated-data-tracker/
- Hinz A., Glaesmer H., Brähler E. Sleep quality in the general population: psychometric properties of the Pittsburgh Sleep Quality Index, derived from a German community sample of 9284 people. Sleep Med. 2017;30:57–63. doi: 10.1016/j.sleep.2016.03.008. [DOI] [PubMed] [Google Scholar]
- Holmes E.A., O'Connor R.C., Perry V.H. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet. 2020;7:547–560. doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horton R. Offline: the second wave. Lancet. 2020;395:1960. doi: 10.1016/S0140-6736(20)31451-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Istituto Superiore di Sanità Dati della Sorveglianza integrata COVID-19 in italia. 2020. https://www.epicentro.iss.it/coronavirus/sars-cov-2-dashboard
- Léger D., Beck F., Fressard L., Verger P., Peretti-Watel P., Coconel Group Poor sleep associated with overuse of media during the COVID-19 lockdown. Sleep. 2020 doi: 10.1093/sleep/zsaa125. zsaa125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lenth R., Singmann H., Love J., Buerkner P., Herve M. Package “emmeans”: estimated marginal means, aka least-squares means. R package version 1.3.0. 2020. https://cran.r-project.org/web/packages/emmeans/emmeans.pdf
- Malhi G.S., Mann J.J. Depression. Lancet. 2018;392:2299–2312. doi: 10.1016/S0140-6736(18)31948-2. [DOI] [PubMed] [Google Scholar]
- Marelli S., Castelnuovo A., Somma A. Impact of COVID-19 lockdown on sleep quality in university students and administration staff. J. Neurol. 2020 doi: 10.1007/s00415-020-10056-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazza C., Ricci E., Biondi S. A nationwide survey of psychological distress among Italian people during the COVID-19 Pandemic: immediate psychological responses and associated factors. Int. J. Environ. Res. Publ. Health. 2020;17(9):3165. doi: 10.3390/ijerph17093165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mondo M., Sechi C., Cabras C. Psychometric evaluation of three versions of the Italian perceived stress scale. Curr. Psychol. 2019 doi: 10.1007/s12144-019-0132-8. [DOI] [Google Scholar]
- Olff M., Langeland W., Draijer N., Gersons B.P.R. Gender differences in posttraumatic stress disorder. Psychol. Bull. 2007;133:183–204. doi: 10.1037/0033-2909.133.2.183. [DOI] [PubMed] [Google Scholar]
- Ozdin S., Ozdin S.B. Levels and predictors of anxiety, depression and health anxiety during COVID-19 pandemic in Turkish society: the importance of gender. Int. J. Soc. Psychiatr. 2020 doi: 10.1177/0020764020927051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pappa S., Ntella V., Giannakas T., Giannakoulis V.G., Papoutsi E., Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav. Immun. 2020 doi: 10.1016/j.bbi.2020.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pierce M., Hope H., Ford T. Mental health before and during the COVID-19 pandemic: a longitudinal probability sample survey of the UK population. Lancet. 2020 doi: 10.1016/S2215-0366(20)30308-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rajkumar R.P. COVID-19 and mental health: a review of the existing literature. Asian J Psychiatr. 2020;52:102066. doi: 10.1016/j.ajp.2020.102066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salfi F., Amicucci G., Cascioli J. The impact of home confinement due to COVID-19 pandemic on sleep quality and insomnia symptoms among the Italian population. J. Sleep Res. 2020;29(S1):73–74. doi: 10.1111/jsr.13181. [DOI] [Google Scholar]
- Sanavio E., Bertolotti G., Michelin P., Vidotto G., Zotti A.M. Organizzazioni Speciali; Firenze, IT: 1998. CBA 2.0 – Cognitive Behavioural Assessment 2.0 - Scale Primarie: Manuale. [Google Scholar]
- Spielberger C.D., Gorsuch R.L., Lushene R.E. Consulting Psychologist Press; Palo Alto, CA: 1970. The State-Trait Anxiety Inventory (STAI) Test Manual for Form X. (tr. it.: Lazzari R, Pancheri P. S.T.A.I. Questionario di autovalutazione dell’ansia di stato e di tratto. Firenze, IT: Organizzazioni Speciali, 1980) [Google Scholar]
- Taylor S.E., Klein L.C., Lewis B.P., Gruenewald T.L., Gurung R.A.R., Updegraff J.A. Biobehavioral responses to stress in females: tend-and-befriend, not fight-or-flight. Psychol. Rev. 2000;107:411–429. doi: 10.1037/0033-295X.107.3.411. [DOI] [PubMed] [Google Scholar]
- Verma R., Balhara Y.P.S., Gupta C.S. Gender differences in stress response: role of developmental and biological determinants. Ind. Psychiatr. J. 2011;20:4–10. doi: 10.4103/0972-6748.98407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vindegaard N., Benros M.E. COVID-19 pandemic and mental health consequences: systematic review of the current evidence. Brain Behav. Immun. 2020 doi: 10.1016/j.bbi.2020.05.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X. Immediate psychological responses and associated factors during the initial stage of the 2019 Coronavirus Disease (COVID-19) epidemic among the general Population in China. Int. J. Environ. Res. Publ. Health. 2020;17(5):1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav. Immun. 2020;87:40–48. doi: 10.1016/j.bbi.2020.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wenham C., Smith J., Morgan R. COVID-19: the gendered impacts of the outbreak. Lancet. 2020;395:846–848. doi: 10.1016/S0140-6736(20)30526-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong W.S., Fielding R. Prevalence of insomnia among Chinese adults in Hong Kong: a population-based study. J. Sleep Res. 2011;20:117–126. doi: 10.1111/j.1365-2869.2010.00822.x. [DOI] [PubMed] [Google Scholar]
- World Health Organization Coronavirus disease (COVID-2019) situation reports. 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports/
- World Health Organization Gender and women's mental health. 2020. https://www.who.int/mental_health/prevention/genderwomen/en/
- Wright K.P., Linton S.K., Withrow D. Sleep in university students prior to and during COVID-19 stay-at-home orders. Curr. Biol. 2020;30(14):PR797–R79810. doi: 10.1016/j.cub.2020.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang B., Wing Y.K. Sex differences in insomnia: a meta-analysis. Sleep. 2006;29:85–93. doi: 10.1093/sleep/29.1.85. [DOI] [PubMed] [Google Scholar]