Highlights
-
•
Discussed economic impact of water utilities and COVID-19 health impacts on workforce.
-
•
Presented case studies on preparedness and response to COVID-19 by utilities.
-
•
Reviewed alternate resiliency strategies for response during and after outbreaks.
Keywords: COVID-19, Pandemic, Infrastructure, Water utilities, Economic impact, Resilience
Abstract
Recent outbreaks have constantly disrupted our global economy and public health in numerous ways, impacting efficiency and prosperity across all sectors. This article focuses on the impacts of outbreaks (epidemics and pandemics) on water - wastewater utilities and water infrastructure and critically evaluates the issues underlining their impact on economic development and highlights the need for preparedness. A perspective on water infrastructure and industry-related impact on our society and economic development in the wake of the pandemic, COVID-19, is presented. Methods that could potentially institute safe, reliable, and efficient procedures for better preparedness and rapid recovery have been explored at length. The purpose of this article is therefore threefold: 1) to discuss the economic and public health impact of outbreaks on water and wastewater utilities and utility workforce; 2) to present case studies demonstrating utilities' preparedness and response to COVID-19, and 3) to review various alternatives for education and training as well as innovative processes and strategies for productivity during and after outbreaks. Strategies discussed in this article could be used as valuable tools for developing resiliency efforts, especially from the context of continuing water and wastewater utility operations and services in emergencies.
1. Introduction
At the time of writing this article, the death toll of the COVID-19 (Corona Virus Infectious Disease – 2019) outbreak has surpassed over 206,000 people in the United States with over 7.2 million active confirmed cases and over 3 million recovered cases, while the global death toll has reached 1,009,349 with over 33.7 million active confirmed cases and 23.4 million recovered cases (Dong, Du, & Gardner, 2020). The pandemic has severely disrupted our personal, professional, and social lives, affecting our economy in numerous ways due to lockdowns, border closures, and increased travel restrictions (Guerriero, Haines, & Pagano, 2020; Megahed & Ghoneim, 2020; Rumpler, Venkataraman, & Göransson, 2020; Sannigrahi, Pilla, Basu, Basu, & Molter, 2020). The global population has experienced other epidemics and pandemics over the past ten years. In view of these experiences, it is important to note that sustainable development of the human environment should account for risks from disease outbreaks so that potentially dramatic consequences for humanity can be prevented (Di Marco et al., 2020).
COVID-19 is caused by severe acute respiratory syndrome-Coronavirus 2 (SARS-CoV-2), which is remarkably similar to SARS-CoV and Middle Eastern Respiratory Syndrome virus -CoV (MERS-CoV) in terms of its structure, pathogenesis, and clinical manifestations (Petrosillo, Viceconte, Ergonul, Ippolito, & Petersen, 2020; Rockx et al., 2020) (Table 1 ). Coronaviruses are enveloped spherical viruses and about 120 nm in diameter. They belong to the family of Coronaviridae. These coronaviruses have proteins required for their proper maintenance and single-stranded ribose nucleic acid (RNA) that contains unique genetic information and distinguish each strain of virus from the other within the same family (Brian & Baric, 2005). Clinical evidence suggests that coronaviruses, such as SARS-CoV, SARS-CoV-2, and MERS-CoV, spread primarily through respiratory droplets and enter the lungs via the upper respiratory tract (Weiss & Leibowitz, 2011). The onset of infection leads to acute respiratory illness in humans and animals that are difficult to treat, depending on the severity. Viral pathogenesis begins with the virus's invasion into the host's respiratory system, followed by the association of viral surface proteins to hosts' cellular surface receptors (Weiss & Leibowitz, 2011). Upon binding, viral RNA is injected into the host cell and triggers an anti-viral immune response. If the host's immune response fails to kill the virus, the viral RNA proceeds to make several copies within the host cell. New viral particles are released while destroying the host cell, leading to acute respiratory illness and shortness of breath in infected individuals. Currently, there are no Food and Drug Administration (FDA) approved treatments for SARS-CoV-2 infections, albeit there are several candidate vaccines and anti-viral therapeutics that are in Phase I clinical trials.
Table 1.
Comparison among SARS, Swine flu, MERS and COVID-19 causing viruses, persistence in the environment and prevention and treatment methods.
| Severe Acute Respiratory Syndrome (SARS) | Swine Flu | Middle Eastern Respiratory Syndrome (MERS) | COVID-19 | |
|---|---|---|---|---|
| Year of outbreak and duration | 2002– 2004 (Wang et al., 2005) | 2009– 2010 | 2012 | 2019 - present |
| Pathogen | SARS associated - Coronavirus (CoV) or SARS-CoV | Influenza A virus - pH1N1 | MERS associated - Coronavirus (CoV) or MERS-CoV | SARS associated – Coronavirus 2 (CoV-2) or SARS-CoV-2 |
| First reported | China’s Guangdong province | California, USA | Saudi Arabia | Wuhan, China |
| Infected Cases | 8439 (Wang et al., 2005; WHO, 2003a, 2003b) | 60.8 million cases in US (CDC, 2010) | 2519 (WHO, 2018) | >33 million (Dong E et al 2020) |
| Deaths | 812 (Wang et al., 2005; WHO, 2003a, 2003b) | 151,700 to 575,400 deaths worldwide (CDC, 2010) | 866 (WHO, 2018) | >1 million (Dong E et al 2020) |
| Cases in US | 73 (WHO, 2003a, 2003b) | 12,469 deaths in US (CDC, 2010) | 2 (WHO, 2018) | >7million cases; >200,000 deaths (Dong E et al 2020) |
| Case fatality rate | 11 % (WHO, 2003a, 2003b) | 0.2 % (Hayward et al., 2014) | 34.3 % (WHO, 2015) | ∼1−3% |
| Virus incubation time | 5–14 days (WHO, 2003a, 2003b) | 2 – 7 days (Jilani, Jamil, & Siddiqui, 2019) | 5 – 10 days (WHO, 2018) | 5–14 days (Jiang, Rayner, & Luo, 2020) |
| Key symptoms | Fever, dry-cough, diarrhea, dyspnea, and hypoxia (WHO, 2003a, 2003b) | A fever, cough, sinus and ear infection, diarrhea, dyspnea and hypoxia (CDC, 2010) | Fever, dry-cough, diarrhea, dyspnea, and hypoxia (WHO, 2018) | Fever, dry-cough, diarrhea, dyspnea, and hypoxia (WHO, 2019a) |
| Clinical manifestations | Acute respiratory distress requiring ventilator support; Pneumonia; Lymphopenia (WHO, 2003a, 2003b) | Acute respiratory distress; vomiting; pain or pressure in the chest or abdomen (CDC, 2010). | Adult respiratory distress syndrome (ARDS); Pneumonia; Kidney failure (WHO, 2018) | Acute respiratory distress requiring ventilator support; Pneumonia-like illness; Lymphopenia (WHO, 2019a) |
| Sample for testing | Stool, blood, nasopharyngeal or oropharyngeal aspirate and swab, Bronchoalveolar lavage (WHO, 2003a, 2003b) | Stool, blood, nasopharyngeal or oropharyngeal aspirate and swab, Bronchoalveolar lavage (CDC, 2010) | Stool, blood, nasopharyngeal or oropharyngeal aspirate and swab, Bronchoalveolar lavage (WHO, 2018) | Stool, blood, nasopharyngeal or oropharyngeal aspirate and swab, Bronchoalveolar lavage (WHO, 2019a) |
| Diagnostic methods | RT-PCR; ELISA; Virus culture and titer assay; EM; Chest X-rays (WHO, 2003a, 2003b) | RT-PCR; ELISA; Virus culture and titer assay; EM; Chest X-rays; Rapid influenza diagnostic tests (CDC, 2010) | RT-PCR; ELISA; Virus culture and titer assay; EM; Chest X-rays (WHO, 2018) | RT-PCR; ELISA; Virus culture and titer assay; EM; Chest X-rays (WHO, 2019a) |
| Treatment identified | No vaccine; No treatment exists except supportive care (WHO, 2003a, 2003b) | 2009 H1N1 flu vaccine (FDA approved); Anti-viral drugs (CDC, 2010) | No vaccine; No treatment exists except supportive care (WHO, 2018) | No vaccine, although several candidate vaccines and drugs are undergoing testing (WHO, 2019a) |
| Prevention | Social distancing; Avoid crowded areas and close contact with sick people; Wash hands often; avoid touching the face; wear appropriate personal protective equipment (PPE); Isolate immediately when experiencing symptoms or when infected (WHO, 2003a, 2003b) | Social distancing; Avoid crowded areas and close contact with sick people; Wash hands often; avoid touching the face; wear appropriate personal protective equipment (PPE); Isolate immediately when experiencing symptoms or when infected (CDC, 2010) | Social distancing; Avoid crowded areas and close contact with sick people; Wash hands often; avoid touching the face; wear appropriate personal protective equipment (PPE); Isolate immediately when experiencing symptoms or when infected (WHO, 2018) | Social distancing; Avoid crowded areas and close contact with sick people; Wash hands often; avoid touching the face; wear appropriate personal protective equipment (PPE); Isolate immediately when experiencing symptoms or when infected (WHO, 2019a) |
| Transmission route | Close contact with infected person Moisture droplets in the air when an infected person coughs, sneezes or talks Touching objects with virus contact on it and then touching the mouth or nose. (WHO, 2003a, 2003b) | Close contact with infected person Moisture droplets in the air when an infected person coughs, sneezes or talks Touching objects with virus contact on it and then touching the mouth or nose (CDC, 2010). | Zoonotic – Can be transmitted from infected animal to humans. Person to person transmission is rare, but possible. Moisture droplets in the air when an infected person coughs, sneezes or talks (WHO, 2018) | Close contact with infected person; Moisture droplets in the air when an infected person coughs, sneezes or talks; Touching objects with virus contact on it and then touching the mouth or nose (WHO, 2019a). |
| Possible airborne and fomite transmission | Yes | Yes | Yes | Yes |
| Fecal shedding reported | Yes | Yes | Yes | Yes (Chen et al., 2020) |
| Persistence of the virus on surfaces | Virus does not persist on food. At room temperature the virus can live for an average of 4–5 days and up to 9 days. Low temperatures and high humidity are favorable for the virus to thrive for longer periods. Virus is stable in: Feces for 4 days; Urine for 1–2 days; Paper, Formica surface and plastered walls for 36 h; Plastic surfaces and stainless steel for 3 days; Glass slide for 4 days (WHO, 2003a, 2003b) |
Virus is stable on stainless steel for 2 weeks; and cloth and microfiber for 1 week (Thompson & Bennett, 2017); hands for 5 min after transfer to surfaces (Bean et al., 1982); persists on glass surfaces (Amelie Dublineau, Batejat, Pinon, Burguiere, & Manuguerra, 2011). | At room temperature the virus can live for an average of 4–5 days and up to 9 days. Low temperatures and high humidity are favorable for the virus to thrive for longer periods (WHO, 2019b). MERS-CoV is stable for several hours in the air and on environmental surfaces including fomites collected from the surroundings of infected patients (Kim et al., 2016). | Aerosolized coronavirus can remain in the air for up to 3 h. SARS-CoV-2 demonstrate relatively long viability in the air for 3 h; o copper for 4 h; on cardboard for 24 h; on plastic and stainless steel for 2–3 days. Half-life in air is similar to SARS-CoV, i.e., 2.7 h; and on steel is 13 h and on polypropylene is 16 h (van Doremalen et al., 2020). |
| Persistence of Virus in water bodies | Surrogate SARS coronaviruses, transmissible gastroenteritis (TGEV) and mouse hepatitis virus (MHV) remained infectious in water and sewage for days to weeks (Casanova, Rutala, Weber, & Sobsey, 2009). In a study from China, SARS-CoV survived for 14 days in sewage at 4 degrees and for 2 days at 20 degrees. SARS-CoV persisted in Stools for 3 days; In urine for 17 days at 20 °C and in domestic sewage for 14 days (Wang et al., 2005) | Unclear | Unclear | Presence of SARS-CoV-2 in untreated wastewater was reported (Ahmed et al., 2020; WHO, 2020); however, it is still under investigation |
| Current scenario | No cases of SARS for over a decade (WHO, 2003a, 2003b) | Seasonal outbreaks persist (CDC, 2010) | MERS is an ongoing public health concern (WHO, 2018) | Ongoing global threat and concern due to spiking mortality rates (WHO, 2019a) |
In the last two decades, SARS-CoV and MERS-CoV epidemics have occurred from 2002 to 2004, and in 2012, respectively (Table 1). According to the World Health Organization (WHO), SARS-CoV was first reported in China's Guangdong province infecting 8439 people and killing 812 people, presenting a case fatality rate of 11 % (WHO, 2003a, 2003b). Whereas, MERS-CoV was first reported in Saudi Arabia, infecting 2519 people, and killing 866 people, presenting a case fatality rate of 34.4 % (WHO, 2015). The average incubation time for both SARS-CoV and MERS-CoV was reported to be five days in most cases (WHO, 2003a, 2003b). Common transmission routes of the viruses are via droplets that enter the air when an infected person coughs, sneezes, or talks (Annalaura, Ileana, Dasheng, & Marco, 2020). According to WHO, the high-risk individuals involve health care workers, especially those involved in procedures generating aerosols, the aged, and individuals with underlying medical conditions demonstrating immune insufficiency. The key symptoms include fever, cough, sore throat, and shortness of breath. Clinical manifestations are acute respiratory distress requiring ventilator support and pronounced lymphopenia (diminished lymphocyte counts) (WHO, 2003a, 2003b). Some of the most efficient methods to detect and quantify viral copies in blood, stools, and nasopharyngeal swabs from infected patients are polymerase chain reaction (PCR), which is a powerful molecular biology technique; virus titer determination, serology antigen and antibody assays such as enzyme-linked immunosorbent assay (ELISA) that are validated by the Center for Disease Control and Prevention (CDC).
There is growing information becoming available on the transmission potential of coronaviruses through the environment. It has been reported that these viruses are stable in feces and urine at room temperature for up to 4 days (Chen et al., 2020; Wang et al., 2005). Additional studies have reported that coronavirus can survive for 36 h on paper, Formica surface and plastered wall; 72 h on plastic surface and stainless steel; and 96 h on a glass slide (Feied, 2004; WHO, 2003a, 2003b). Necessary preventative measures to follow include practicing social distancing and wearing appropriate personal protective equipment such as face mask or face shield, goggles, gloves, and protective clothing, mainly when working in aerosol formation environments. Strict precautionary measures should be taken by personnel working in wastewater facilities because studies report that SARS-CoV is sensitive to rising temperatures. It can survive in water at 4 °C for several months and in wastewater to 4 days (Gundy, Gerba, & Pepper, 2009). This viral property raises added concerns to the public health sector as well as the wastewater plant. Furthermore, we believe it is essential to highlight coronavirus's potential transmission, especially SARS-CoV-2/COVID-19, through wastewater, especially for the personnel's safety on duty during the ongoing pandemic.
The purpose of this article is threefold: 1) to discuss the economic and public health impact of water and wastewater utilities and the utility workforce; 2) to present case studies demonstrating utilities' preparedness and response to COVID-19, and 3) review various alternatives for education and training as well as innovative processes and strategies for productivity during and after outbreaks. First, a brief background of the potential global economic impact of COVID-19 and the specific economic impact caused by water and wastewater utilities are presented. Second, the implications of the COVID-19 outbreak for water and wastewater utility workforce and preparedness and response to COVID-19 is discussed. Finally, a systematic strategy involving innovations required to enhance economic immunity to outbreaks, virus control, education and training procedures, and future preparedness is discussed in detail.
1.1. COVID-19 impact on our environment and public health
Our water sources are constantly exposed to numerous microorganisms, like bacteria, viruses, protozoa, which are sometimes known as high-risk biological pollutants depending on their pathogenic potentials. Not all microorganisms present in water sources and wastewater are pathogenic. However, a few bacteria (such as Escherichia coli, Salmonella enterica serovar Typhi, Shigella dysenteriae, Vibrio cholera, and Legionella), viruses (Enterovirus, Hepatitis virus, Rotavirus, Coronavirus, Adenovirus, and Norovirus) and protozoa (Cryptosporidium, Giardia, Entamoeba histolyticaare) are known to cause adverse health issues (Jia & Zhang, 2020). While the shutdown during the pandemic has heavily restricted travel and recreational activities, it has instilled some environmental transformations such as decreased greenhouse gas emissions, cleaner beaches, less polluted water bodies, and improved air quality and visibility. However, these transformations are ephemeral and will change with normal operations (Rumpler et al., 2020; Zambrano-Monserrate, Ruano, & Sanchez-Alcalde, 2020). Despite the beneficial environmental transformation seen during the shutdown, high volumes of solid wastes are generated by residential areas and medical facilities such as hospitals, nursing homes, and other senior-living homes where high-risk populations live. It has become a significant challenge to collect, transport, process, and dispose of the waste containing infectious materials generating from these operations.
1.2. Overview of water and wastewater treatment processes
Most of the world's population depends on groundwater sources for water supplies, which are usually protected from various environmental pollutants, and significantly under 50 % of the U.S. population relies on groundwater for their private or public drinking water supply (Gude, 2018). High-quality groundwater that is free of hardness and dissolved solids is disinfected before supplying to communities. Several physical and chemical separation processes are employed for groundwater with significant hardness (carbonate and non-carbonate hardness compounds) and surface water sources. These include chemical coagulation, flocculation, lime-softening, ion-exchange, sedimentation, and filtration, followed by disinfection. For groundwater high in dissolved solids concentration, membrane separation processes are considered. Disinfection processes may include chemical oxidants such as chlorine, hydrogen peroxide, ozone, and other oxidants, physical process such as heat and ultrasound, and electromagnetic processes such as microwave and U.V. radiation. The selection of effective disinfection process depends on the water source's characteristics and composition. Domestic or municipal wastewater treatment is mostly carried through biological means using various microorganisms capable of removing pollutants of concern. Heterotrophic, photoautotrophic, denitrifying, and anaerobic bacteria are the major players in removing carbonaceous and nitrogenous compounds from wastewater (Gude, 2015; Lofrano & Brown, 2010). Aerobic processes are common in municipal wastewater applications, while chemical and thermochemical processes may be considered industrial and specialty wastewater.
The conventional treatment scheme is classified into three stages: primary treatment; secondary biological treatment; and tertiary treatment for nutrient removal. While the secondary treatment is enforced as a minimum standard in the U.S., advanced treatment options may include filtration, disinfection, adsorption, and membrane separation processes to further remove specific inorganic and organic pollutants and microbial contaminants. Water scarcity in many regions has caused communities to consider water reuse options to protect and increase existing water sources (Gude, 2017). Due to the COVID-19 outbreak, many community water systems with water reuse options in their operating scheme are concerned about the water source's safety. The wastewater treatment process yields excess sludge that may have concentrated particles of viable and non-viable virus matter (WHO, 2020). Proper management, treatment, and disposal methods are critical to minimize contact and spread of the virus.
2. Potential for global economic impact and water-based economy
With its presence in over 195 countries, the inevitable economic impact of COVID-19 is expected to be substantial, testing local, national, and international economies. A congressional research service report notes that the global economic growth could slow down by 2% per month, causing a 13%–32% shortfall in global trade at current rates (CRS, 2020). Preliminary data show that the U.S. gross domestic product (GDP) has fallen by 4.8 % at an annual rate and several foreign investors have withdrawn their investments out of Asian economies. The International Monetary Fund (IMF) estimates that government borrowings at the global level will rise from 3.7 % of the global GDP in 2019 to 9.9 % in 2020 to sustain economic activity (IMF, 2020).
2.1. Economic impact on utilities in developed countries
The American Water Works Association (AWWA), in collaboration with the American Metropolitan Water Association (AMWA), has released a financial report concerning the potential impact of the COVID-19 pandemic on the water and wastewater industry in the United States. Both water and wastewater treatment systems play a vital role in our communities and economic development through industry operations. The study has gathered the data concerning the demands for water use and revenues at the public utilities after the COVID-19 disruption and estimated total losses that might accrue at the end of the crisis. The study finds that the aggregate financial impact of COVID-19 on water utilities will be approximately $13.9 billion, which may slow down the economic activity in other industries leading to a cumulative economic impact of $32.7 billion. This financial crisis will also lead to a reduction in up to 90,000 private-sector jobs. The actual economic impact on the water utilities would be $15 billion, including the revenue losses due to delinquent customers who face their economic crisis and deferred water tariffs. Loss of income was also attributed to the loss of revenue from commercial and industrial customers. When the economic impact that is potentially caused by the losses in wastewater treatment plants is considered, the overall economic impact of both water and wastewater utilities for the U.S. will be around $27 billion.
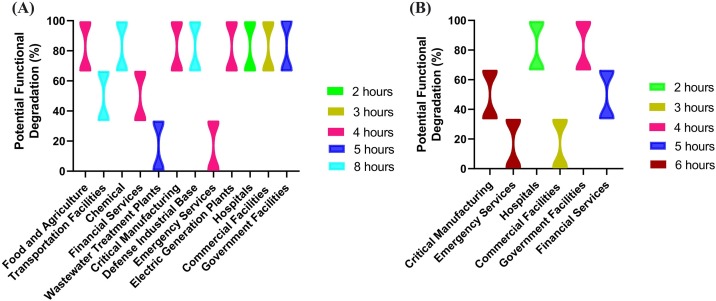
The U.S. Department of homeland security conducted a survey on 2661 sites to analyze water- and wastewater-related dependencies of 16 critical sectors in the U.S. (USDHS, 2014). These critical sectors include chemical production, commercial facilities, government facilities, hospitals, electric generation plants, emergency services, defense industrial base, financial services, food and agriculture, critical manufacturing, transportation facilities, and wastewater treatment plants. Fig. 1 A shows the critical dependencies of different sectors and how their functional capability is degraded when water services are not available. Some of the critical sectors are sensitive as their functional degradation is seen within or after two hours of water unavailability. Food, agriculture and several other sectors are severely impacted within 2−8 hours. Hospitals provide critical services and are more dependent on water supplies. Similarly, Fig. 1B shows the critical dependencies of various sectors on wastewater treatment services for their essential function. Despite this fact, there are many water utilities beyond their lifespan, with an estimated investment gap of $400 billion - $ 1 trillion to maintain the current water service (NAIC 2016). An estimated 4.8 trillion is needed over the next 20 years to maintain the water infrastructure in good standing (The Value of Water Campaign 2017). However, it should be noted that the SARS-CoV-2 so far has not led to interruptions in water or wastewater services to date.
Fig. 1.
Key dependencies of critical industrial sectors on water supplies and wastewater treatment in their facilities: (A) potential functional degradation of the critical industry due to lack of water supplies; and (B) potential functional degradation of the critical industry due to lack of wastewater treatment.
2.2. Economic impact on utilities in developing countries
In general, significant populations in developing and underdeveloped countries lack access to basic sanitation, hygiene, and safe drinking water. About 800 million people face this issue daily and spend up to 10 h only to reach unprotected water sources and collect water for consumption and other uses (Armitage & Nellums, 2020; Ray, 2020). The time spent in to get access to water causes billions of dollars of loss in economic opportunities. An estimated economic loss of $260 billion is attributed to a lack of essential water and sanitation. It is also reported that about $18.5 billion could be saved by avoiding deaths related to the lack of water and sanitation (SIWI, 2005). Lack of water for sanitation creates more significant challenges for combatting infectious diseases in developing countries. Many health advisory boards, including the World Health Organization, suggest frequent handwashing for at least 20 s as a protective measure for avoiding contact with SARS-CoV-2. However, nearly 40 % of the world's population lacks access to basic sanitation (Otto, Kuzma, Strong, & Chertock, 2020). Over 75 % of households in low-income and middle-income countries a deprived of water (Armitage & Nellums, 2020; SenGupta, 2020).
2.3. Critical insights into water economy
Conventionally water is not considered a critical element of economic development. It has always been dealt with as a separate sector, often considered a money-sink or a non-profitable endeavor. In some regions of the world, water is considered a free and abundant resource (Gude, 2016). Primary causes for significant underinvestment in water utilities are 1) poor understanding of the criticality of the water sector, 2) inadequate valuation of water services, 3) fragmented or weak support from government agencies, and 4) lack of regional collaboration over water resources and infrastructure. It should be realized that investing in a water-based economy is a wise step towards sustainable development for both developed and developing countries. For example, federal investment in water infrastructure per capita in the U.S. is about $11, similar to energy sector, transportation systems, and information systems which are $46, $136, and $251, respectively. The current national capital need is about $123 billion per year, which, if fulfilled, will potentially result in over $220 billion annual economic activity in the country, creating 1.3 million jobs over ten years. This investment would also save $94 billion a year in sales in the next ten years and as much as $402 billion a year from 2027 to 2040, which creates a missed opportunity due to the misconceptions as mentioned earlier. Similarly, an estimated benefit of $3-$34 per $1 investment is possible by improving water supplies, sanitation, and hygiene in developing countries, mainly due to increased production and productivity within economic sectors (SIWI, 2005).
3. Impacts of COVID-19 and implications for water and wastewater utility operations
In general, there is little risk for disease transmission through the urban water cycle. The risk of transmission is of orders of magnitude lower than other water and wastewater borne viruses. This section discusses the presence of transmission and implications for water and wastewater utility workforce.
3.1. SARS-CoV-2 in water and wastewater utilities
Currently, there is no evidence about the presence of SARS-CoV-2 in surface and groundwater sources, and proper treatment of these water sources renders their safe consumption and use. However, there is evidence that SARS-CoV-2 could be present in fecal matter from infected persons, and when in contact with wastewater constituents, could cause concern. Wastewater treatment facilities are continuously monitoring and tracking the possible occurrence of this virus or its genetic fingerprints at the facilities. Although the virus has shallow stability (persistence) in the environment, it can quickly be inactivated with disinfectants, especially oxidants, when compared with other non-enveloped human enteric viruses with the known waterborne transmission (La Rosa, Bonadonna, Lucentini, Kenmoe, & Suffredini, 2020; Rimoldi et al., 2020). The virus’s presence in water environments even for a short term could cause a potential threat to personnel involved in wastewater treatment operations. Recent studies have reported the virus's presence in raw wastewater but not in treated effluents indicating its inability to survive the treatment process and, therefore, the lack of potential risk (Rimoldi et al., 2020).
3.2. Implications for water and wastewater utility personnel
Current evidence partially supports the viability of SARS-CoV-2 in raw wastewater. However, it is critical to protect our wastewater utility workforce. Some areas of concern would be the possibility of 1) virus survival in airborne aerosol particles, ranging between 1 μm to several microns, and 2) surface contamination of equipment, facility, and machinery (Table 1). Aerosols of size >5 microns are of particular concern. They are known to provide virus survival environments and have a high potential for disease transmission, although this is highly dependent on virus type and environmental conditions (Cao, Noti, Blachere, Lindsley, & Beezhold, 2011; Morawska & Cao, 2020). As mentioned before, wastewater treatment plants are mostly dependent on aerobic processes. Aeration tanks are mechanically mixed by supplying coarse or diffuse bubble systems, all resulting in the potential release of aerosols that may carry the virus in them. The facilities' wastewater utility workforce is susceptible to these aerosols while carrying out regular inspection and maintenance activities. Moreover, the potential for an active virus on the surfaces of equipment, facilities, and machinery is high as the workforce enters the office areas daily. Proper precautionary measures and protocols should be followed to ensure the workforce's occupational health and required strategies are discussed later.
3.3. Economic (industry sector) dependence on water utilities
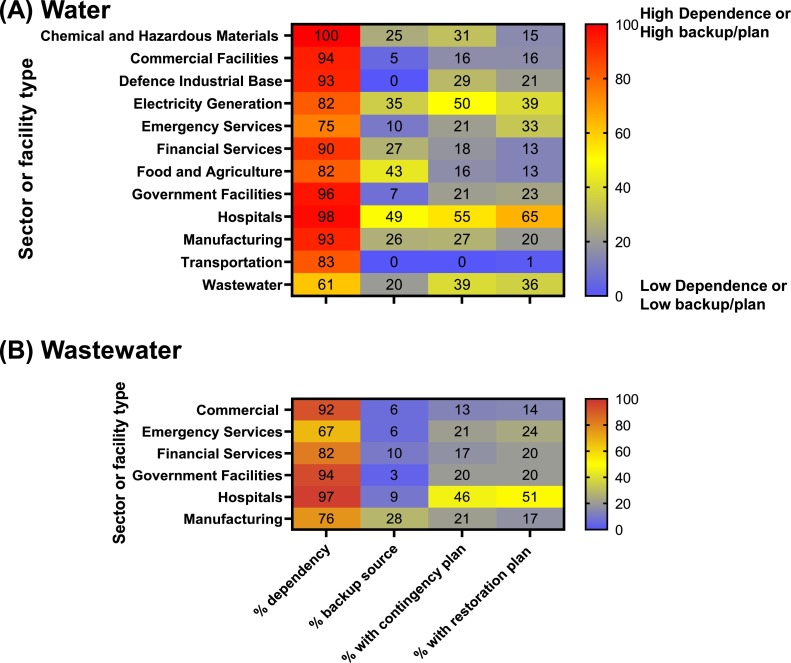
Many other industrial sectors depend upon water supplies as well as wastewater treatment services for their daily operations. It is almost impossible to carry out routine operations in some sectors such as chemical and hazardous materials production, hospitals, manufacturing, and some commercial facilities without these essential services (USDHS, 2014 and 2020, NIAC, 2016). Fig. 2 A shows the dependence of various industry sectors on water supplies in the first column from the left. Fig. 2B shows the dependency of some industrial sectors on the need for wastewater treatment and management. Fig. 2A and B also show the scales for how some of the utilities are prepared with backup water source or alternate water source for water supply or backup alternate wastewater treatment option, contingency plan, and restoration plan. Many sectors are not well prepared in these aspects in finding backup, alternate sources or contingency, and restoration plans. This situation could be alarming in the events of outbreaks leading to mandatory shutdowns causing significant economic losses.
Fig. 2.
Survey results from utility sector operators: (A) dependence on the water source, backup/alternate, contingency and restoration plan in percentages; and (B) dependence on wastewater treatment, backup/alternate, contingency, and restoration plan in percentages.
To address some of these issues, The U.S. Congress has introduced new requirements called "Risk and Resilience Assessments" and "Emergency Response Plans" for all drinking water utilities that serve more than 3300 people. Different deadlines were suggested requiring large utilities to respond to these new requirements as a priority. The risk and resilience assessment should include natural hazards and malevolent acts, water facility infrastructure resilience, including all equipment, tanks and pipelines, monitoring practices, financial systems, chemical and material handling, operation, and maintenance systems. An emergency plan should include strategies to improve resilience, plans, and procedures to respond to natural hazards, actions, and equipment to respond, including cybersecurity (United States Environmental Protection Agency (USEPA, 2019). However, it should be noted that both the risk and resilience assessment and emergency response plan do not cover outbreaks such as an epidemic or a pandemic indicating a greater need for consideration and inclusion in policies and regulations.
4. Preparedness and response to COVID-19 by Utilities
Water and wastewater utilities around the world respond to emergencies in different ways. Emergency preparedness is a critical component of the operational portfolio for most water utilities (Sowby, 2020). Some utilities have elaborated procedures in place and are prepared to respond to outbreaks while others cannot afford to have or develop procedures for various reasons. The following sections discuss the preparedness and response strategies by water utilities in China, Hong Kong, Italy, the United Kingdom (UK), and the U.S. (GWI 2020).
4.1. Water utilities in China
In China, the Shanghai Chengtou Holding company is a large water utility responsible for water and wastewater services to more than 23 million people. This utility maintained the continuity of service and managed the risks of viral contamination from sewage aerosols in operations. When the coronavirus outbreak was at the most intense stage in China in February, the administration took stricter shifts to make each office and plant have only one staff at work at a time. The cleaning staff disinfected the plants and the surfaces of equipment and facilities several times a day. Raw materials such as chemicals and materials have been stocked up for near-future use. Measures taken between water and wastewater systems were different. The operators in water treatment plants wore regular site uniforms, while those who work for wastewater systems wore full protection suits. Frequent body temperature testing was done, including entering the facilities each time and wearing face masks at work. The workforce was encouraged to take shifts to ensure isolation and separation were maintained at best. The utility paid more attention to monitoring fecal coliforms in the effluents in wastewater treatment systems and increased the monitoring frequency. Utilities worked hard to improve the disinfection processes by taking additional measures. For example, plants that applied ultraviolet (UV) technologies previously, an additional barrier such as chlorination was included. Similarly, for plants that used chlorination for disinfection, the dosage of sodium hypochlorite was increased.
4.2. Water utilities in Hong Kong
The Hong Kong, water supplies department serves more than 7 million people with drinking water. This utility was well prepared for the outbreak due to the previous experience. Hong Kong had encountered SARS in 2003, providing some previous experience to this utility. A contingency plan was prepared to deal with emergency and epidemics after SARS, MERS, and influenza but had not been used. However, this plan served as a useful reference as COVID-19 presented similar challenges as MERS and SARS. This utility also developed a business continuity plan during the times of influenza. These contingency or continuity plans kept them well prepared to react and respond to COVID-19. Hong Kong is a highly populated city with high chances of disease outbreaks. The utilities followed the advice of the health department to ensure that the workforce was protected, for example, the staff who felt unwell were advised to stay at home. Body temperature checks were made mandatory at home and as they entered the workspace (office). Infrared thermometer equipment was used to measure body temperatures. Staggered hours of operations allowed them to avoid peak hours of transportation by allowing early or late operations. Lunch hours were also staggered. Social distancing was highlighted to avoid being infected or minimize the chance of being infected, resulting in the efficient management of businesses using technology and information systems (Sun & Zhai, 2020). The utility expects to enhance automation, remote control, and home office professional capability to address future emergencies and disease outbreaks based on this experience.
4.3. Water utilities in Italy
Gruppo HERA is the primary (second largest) water utility in Italy, where the outbreak was significant with numerous COVID-19 related deaths. This utility serves more than 3.6 million people in Bologna and neighboring regions. The utility continuously engaged in committee meetings to determine the most appropriate solutions. This process has allowed them to perform essential services while reducing the risk for the workforce. The main concern was about the possible quarantines of entire groups of workers dedicated to essential services such as those involved in remote control of networks and plants. The utility also ensured a good network and plant security level with third parties and their personnel with a service delivery level that brings the least possible inconveniences to end-users. The utility has reduced the organization's level of risk over the years, ensuring that services were resilient in the face of main breaks and plant outages and duplicating control and management systems as part of a disaster recovery plan. A SARS-CoV-2 virus presented unexpected conditions and the utility had to overcome these challenges based on previous emergency plans. Some of the lessons learned and required actions were:
-
1
To look for new ways of working with other organizations,
-
2
To work on workforce management systems and to strengthen the remote-control system,
-
3
To minimize contractors' obligations to strengthen the supply chain for critical materials and services, and
-
4
To develop remote working as a standard working model for the staff in the future.
4.4. Water utilities in the United Kingdom
In the U.K., Anglian Water serves more than 6 million people in England's East. This utility closely followed the instructions from an established pandemic plan. The plan is based on risk in terms of probability and likelihood of flu pandemic and has driven an internal risk planning. The risk plan considers a scenario wherein an excess of twenty percent of the workforce may not be available as a core element of utility's resilience and business contingency plan for several years. The plan includes teams that understand the criticality of roles of the workforce within those teams. A team and a combination perspective are utilized to maintain absence for 48 h to over a month. By understanding the nature and roles of teams enable them to enact a contingency planning. Before the outbreak could strike, the teams exercised teleworking to test the network capacity and capability as a means of preparedness. This "game" exercise provides opportunities for the workforce to develop ideas and discuss any concerns. This exercise also allowed for more feedback that could be helpful for a real emergency.
4.5. Water utilities in the United States
The Los Angeles Department of Water and Power in California, with over 10,000 employees, serves 4 million people drinking water. This utility has a fully vertically integrated utility structure where staff work together while maintaining proper social distancing. With a significant number of international staff, some on vacation, or attending other social events, the challenge has transitioned beyond the workplace to the workforce's personal lives, potentially carrying the disease to the workplace. This utility staff manages both water and power systems and proximity with other staff in many field locations. Employee safety has been the top priority. The utility considers business continuity from a finance perspective when it is mostly dependent on its customers' cash flow. Revenues are critical to pay for the staff while being sensitive to what has been happening on the customer base. People who work in the travel industry may have been severely impacted, forcing the utility to consider beyond the business and customer relationships. Plans are under development considering these facts while being sensitive to the issues caused by the outbreak.
As discussed above, the approaches taken by utilities are diverse as the challenges are multi-faceted. There are no best or worst practices as this is a learning process for many utilities. However, some utilities have increased the treatment process robustness by including additional barriers (such as additional disinfection), enhanced workforce safety and wellness. Some utilities have constantly engaged the community about the upcoming challenges and ensured network safety and plant security levels. Previous pandemic experiences have helped some utilities in UK and Hong Kong to be better prepared for this pandemic. Some utilities had to deal with the financial challenges due the inability of customers to pay bills. Community engagement and contingency planning can be identified as two critical steps in managing operations during outbreaks. A significant portion of utilities across the world currently do not have any resiliency and emergency response planning. For example, a survey involving 1388 water utilities revealed that about 51.5 % of the water utilities in the US have fully implemented planning while 38.9 % of the water utilities are currently implementing or in progress, and 9.6 % of the utilities identified as interested in a plan (AWWA, 2020). This is a critical requirement for utilities considering recent trends of epidemics and pandemics.
4.6. Common challenges faced by the utilities
The outbreak of COVID-19 has undoubtedly posed a great challenge for the water utility sector around the world. Living through this process can have some positive and long-lasting impacts on our society. It provides opportunities for collaboration, teamwork, and flexible work patterns at utilities. It will help speed up automation and smart digital systems and spread engagement in co-learning activities between utilities. Some of the common challenges faced by the utilities are mainly related to maintaining recommended social distancing. Some utilities in certain regions share resources and staff (workforce) by mutual agreements as a part of resource management and contingency plan to address this issue. Frequent handwashing is highly encouraged as a practice to enable the safety of employees. State and local agencies and administrators hold weekly webinars with updates of water utilities' operations and services. Keeping up with the major vendors was necessary to ensure that they could supply all the chemicals the utility needs to maintain water treatment and water systems upgrades and repairs. Staggering work schedules have helped in separating employees into teams. Temperature measurements were also widely implemented to monitor the health of employees. 24/7 emergency response service teams were available for the safety of all employees.
5. Near-future efforts to prepare for outbreaks
There are many opportunities to gain experience and knowledge developed from lessons learned during the COVID-19 pandemic, leading to discoveries and innovation in various aspects of water and wastewater utility operations and services. The following sections discuss efforts that utilities can implement to prepare for future outbreaks.
5.1. Wastewater facilities as disease surveillance observatory and repository models
Wastewater treatment facilities can be used as microbial (virus) observatories for disease surveillance and testing the presence of SARS-CoV-2 in the influents (Sims & Kasprzyk-Hordern, 2020). This can serve as a key to estimate the general health status and determine any hotspots for preventive measures. Numerous scientists and research groups are currently investigating the origin, transmission, and clinical therapies for addressing the COVID-19, and datasets are being generated (Guo et al., 2020). Research should be continued to develop ways through which the methods commonly used for sampling and concentration of enteric, non-enveloped viruses from water environments can be successfully adapted (La Rosa et al., 2020).
Wastewater based epidemiology is being increasingly recognized as a complementary approach for infectious disease surveillance and early warning system for disease outbreaks (Daughton, 2020; Orive, Lertxundi, & Barcelo, 2020; Sims & Kasprzyk-Hordern, 2020). The presence of virus (viable and non-viable particles) can be quantified by targeting virus functional or structural motifs in wastewater (Daughton, 2020). Detection methods such as qPCR, RT-PCR, ELISA, and the most probable number (MPN) method can be employed to quantify the virus's presence. Well established quality analysis (Q.A.) and quality control (Q.C.) methods/procedures should be followed to account for sensitivity, error analysis and to ensure uniformity across the datasets from different research groups to facilitate further the process of validating and developing procedures. In some cases, the analysis could be hindered by detection limits. As the population and demographics (customer profiles) vary for each utility, monitoring and tracking is essential to establish temporal and spatial patterns. The location and time of sample collection and the wastewater strength and stage of treatment will be critical in understanding the outcomes. Normalization of data is essential for ranking community-wide infection rates to develop better-informed intervention measures and prevent emergencies. This quantification also allows the estimation of chemical requirements and resource needs at utilities. Care must be taken as reporting average log reductions of pathogens could also lead to extensive misrepresentation and misunderstanding of both data and results (Schmidt, Anderson, & Emelko, 2020). SARS-CoV-2 provides numerous opportunities to learn, discover, and collaborate with other scientists to better understand the preparedness and response schemes from local, regional, and national settings. Wastewater utilities can develop sample repositories nationwide to conveniently derive information on the occurrence and identification of SARS-CoV-2 and their persistence and propensity to withstand degradation processes. The virus may develop resistance to oxidation and other removal processes. This information can be shared among the utility sector stakeholders to better understand the virus's prevalence in different wastewaters to protect the environment and society.
5.2. Innovative and multi-barrier processes for pathogen reduction
Bacteria present in wastewater operations can eliminate the virus in the biological treatment process. However, not all processes can eradicate the virus from wastewater. Therefore, multi-barrier innovative processes can be developed to ensure the removal of viruses from effluents. These could include photoautotrophic algal wastewater treatment systems. A recent study has shown that this system can outperform other activated sludge systems and membrane bioreactor systems (Delanka-Pedige, Munasinghe-Arachchige, Zhang, & Nirmalakhandan, 2020). While log reduction values for membrane bioreactors were higher for Enterovirus and Norovirus, this system can provide a low-energy alternative through inherent reductions of bacteria and viruses.
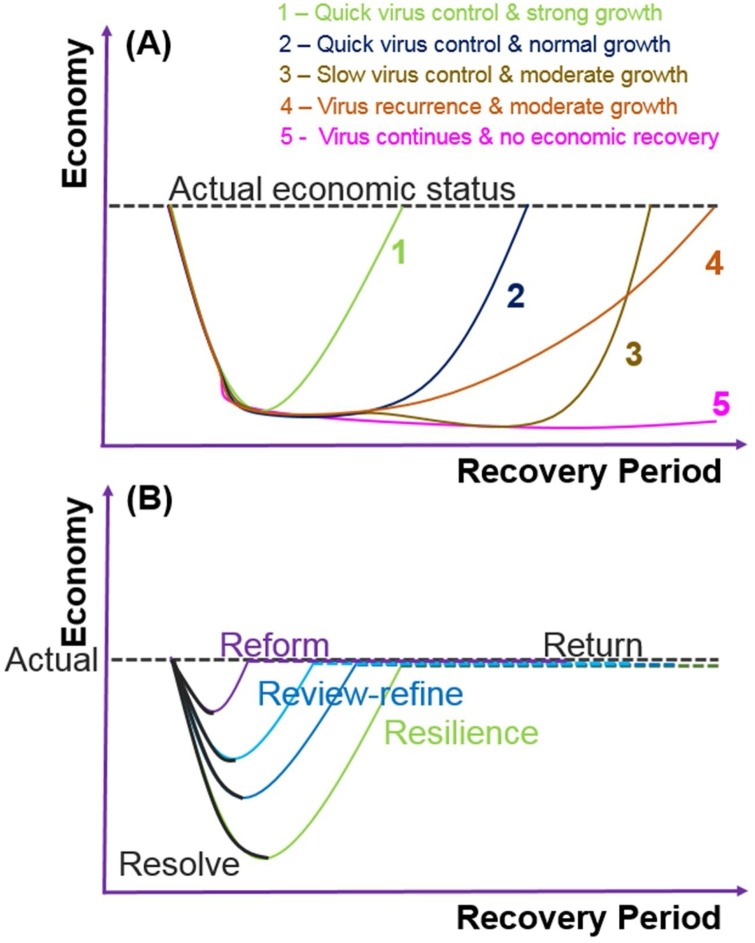
5.3. Findings ways to build financial immunity at the utility level
Several economic “recovery and rebound” scenarios can be envisioned to account for the dynamic behavior of virus control and economic growth in the communities served by the utilities. In general, the economic impact is experienced at a regional or national, or even international levels. The recovery period for economic growth depends on how quickly the virus is controlled, and infected persons are isolated while making efforts to boost the economy by not compromising workforce efficiency. Fig. 3 A shows five different scenarios that could potentially be observed in some regions or countries of the world. The global economy, however, depends on how individual regions can minimize their epidemic impacts. Common scenarios may include: 1) quick virus control – strong economic growth; 2) quick virus control – moderate economic growth; 3) slow virus control – moderate economic growth; 4) virus recurrence – moderate economic growth; and 5) virus continues - no significant economic recovery.
Fig. 3.
(A) Dynamics and possible scenarios of economic impact affected by the presence and control of virus (COVID-19 pandemic), and (B) A future strategy to develop a resilient economy learning from epidemic impacts.
Some of the critical features for building economic immunity are based on resiliency principles (McAndrew, 2019). Fig. 3B shows a future strategy to prepare for an economic downturn and develop a resiliency plan based on water utilities (Juan-García et al., 2017; USEPA, 2015). This strategy involves the following essential steps: resolve or resist (accept and absorb the damage and account for losses); resilience (take action immediately to recover losses by following pre-determined contingency and/or emergency plans and operational guidelines, speed up and increase efficiencies to rebuild the economy); return (restore post-pandemic normal operations); revisit (review and refine strategies followed in resilience stage to evaluate and identify best operational guidelines and procedures); and reform (develop a robust and optimum financial and operational model based on data-driven contingency and emergency frameworks considering extreme and unexpected outbreaks) (Rahman, 2020). A similar approach can be followed to control disease outbreaks.
As discussed earlier, the inability to pay for the utility bills by the customers could result in serious financial challenges for the utilities to carry on their critical operations. In addition, government interventions (such as social distancing and others) during the outbreaks may influence the economic impact in both positive and negative ways, directly and indirectly (Ashraf, 2020). Most of the utilities are publicly owned and non-profit privately-owned. Many state and local governments implement some sort of economic regulation on these utilities (Warner, Zhang, & Rivas, 2020). Therefore, local, state and federal governments should volunteer to support the utilities in financial matters so that water utilities can continue to provide essential services during the times of economic downturn. On the other hand, utilities should understand the economic burdens of the customers and make efforts to provide some flexibility in paying their bills (Retzlaff, 2020).
6. Education, management, and system-level approaches
Education and community outreach are critical to propagate the importance of adequately preparing and responding to outbreaks. Public outreach and essential workforce safety are the two crucial factors in these critical times.
6.1. Education and training
The utility workforce is at a higher risk of contracting the infection by possible environmental transmission. Special educational training on COVID-19 awareness should be provided. Information on practicing protective measures during an infectious outbreak can be effectively disseminated via various platforms such as social media, internet and radio, and television programs. One promising technique for effective education and training of the future workforce is to utilize technologies like virtual reality and other platforms based on artificial intelligence to provide real-life learning experiences. These tools provide lessons for preparedness and response by simulating a virtual scenario (Singh et al., 2020). A virtual reality platform is advantageous in many aspects of normal functioning. It is also suitable for remote applications involving planning, treatment, and controlling infections by bringing awareness of the disease. Especially during emergency shutdowns, virtual interactive platforms provide telemedicine opportunities where doctors can consult with patients and provide medical prescriptions. There are many unknowns about the SARS-CoV-2 virus and associated disease currently. This might provide misinformation (false information, unintentional) and disinformation (deliberately misleading information). For this reason, it is advised that the public are informed correctly (Nature, 2020). Education and communication efforts should fight against any misinformation and disinformation attempts as communities work towards resilience. Right educational and communication platforms empower citizens to discern what is real and what is not. Communities must be involved in research and development efforts to gain their trust. Public engagement enhanced with transparency is the key to ultimate success.
6.2. Essential workers and their health risks
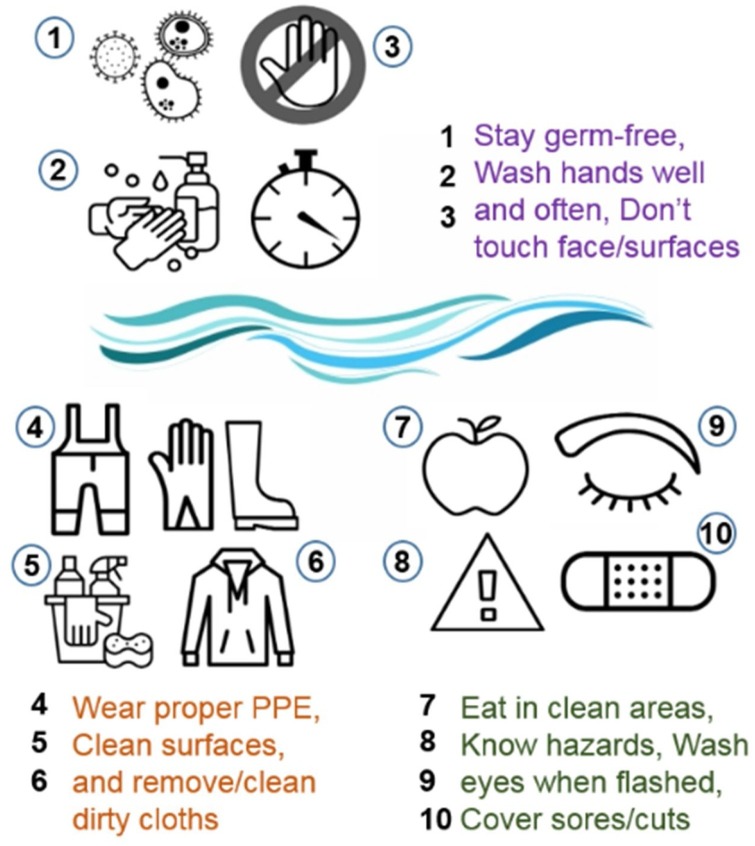
The United States Environmental Protection Agency (USEPA) urged administrators across the states that all water and wastewater workers and service providers in the water sector are considered essential workers by state authorities when enacting restrictions to curb the spread of COVID-19. The U.S. Department of homeland security (USDHS) released a guidance document for essential water infrastructure workforce to respond to the pandemic, which defines explicitly personnel that is directly involved in operations of water authorities, community water systems, wastewater treatment facilities, repair and maintenance of water and wastewater conveyances, sample collection, equipment monitoring, water distribution, and testing, wastewater collection facilities, technical support of SCADA (supervisory control and data acquisition) control systems, chemical and equipment suppliers and personal protection, and infrastructure support through digital systems in both water and wastewater treatment operations. Some basic operational guidelines and preventive practices are recommended for the essential workforce at the water and wastewater treatment facilities, summarized in Fig. 4 (WEF, 2020).
Fig. 4.
Summary of basic personal and preventive guidelines provided for essential workers at water and wastewater treatment facilities.
The risk of exposure presents a significant challenge for the utility workforce to accomplish their daily tasks in the water and wastewater sectors (Switzer, Wang, & Hirschvogel, 2020). There are several critical areas of operations in collection systems. These occur at lift stations, inspection and O & M activities, line cleaning, man-hole maintenance, spill response, and pipeline repairs and maintenance (WEF, 2020). Sample collection, field instrumentation and calibration, and grit/sludge/biosolids handling and management are also potential activities. These activities involve exposure routes through contact, splash, abrasion or puncture, and respiration. Recommended PPE for minimizing the contact will include gloves, boots, coverall, safety glasses, face shield or goggles, Tyvek suits to avoid full-body contact, N95 respirator, surgical or dust mask. Workforce shortage is a critical barrier. For managing workforce needs effectively, utilities may consider establishing mutual aid agreements to share staff and equipment in times of emergency response. This response mechanism can be coordinated by municipal utility associations (Switzer et al., 2020).
6.3. Preliminary planning and implementation
Developing immunity is the key, which can be achieved by developing antibodies. This may not necessarily involve extensive scale testing, tracking, and monitoring. However, many of these face enormous challenges like accuracy, data management, adherence to regulatory policies and the methods followed under various sensitivity issues. Meanwhile, some preliminary preventive measures can be implemented to gain control overspread. These include: 1) social distancing, 2) travel restrictions, 3) testing, tracking and targeted quarantine, and 4) personal protective equipment and cleaning. Distancing has some positive impact, but it is not always feasible or possible in high population areas. Travel restrictions have some positive impact, but the resurgence of new cases sometimes nullified these due to imported cases. Testing, tracking, and targeted quarantine (i.e., isolation) have also yielded some positive results. For example, in India, this method has been implemented with comprehensive early testing and isolation. However, the impact of contact tracing on transmission in high-prevalence settings is currently unproven. Personal protective equipment (PPE) and cleaning of surfaces, and frequent handwashing are essential basic techniques that must be followed. The use of surgical masks is a practical protective option, since the virus may remain viable for hours to days on surfaces and hours in the air. Cleaning surfaces with disinfecting liquids is the best practice for prevention. Widespread access to accurate antibody tests is not yet possible, and currently, there is no evidence about the extent to which exposure to the virus confers long-term immunity.
The virus's mobility and transmission rates should be understood as quickly as possible because they depend on each country's emergency strategies. For example, in South Korea, the transmission rate was significantly low due to robust testing and tracking rather than reducing mobility (e.g., closure of public spaces, lockdowns, closure of schools). In certain countries like Norway, the transmission rate is naturally low due to geographical and environmental factors, which may slow down the spread, despite limited control measures. Mobility reduction may not have a significant impact on the transmission reduction rate. A large population was already infected in some regions before lockdown measures were enforced, making transmission more challenging to control even after lockdowns such as in Italy and some parts of the U.S. Some countries like India are following testing, tracking and isolation by zoning.
7. During and post pandemic responses
While the scientific community works fiercely to invent solutions such as vaccines and other medical alternatives to immunize populations and treat the disease, it is still critical for businesses and other industrial facilities to continue their routine operations to combat the economic downfall. In these circumstances, care must be taken, and contingency or emergency protocols should be followed to recommission buildings and systems that were idle for prolonged periods.
7.1. Recommissioning during or after pandemic
Guidelines are available from AWWA, USEPA, and WEF for restarting operations after the lockdown periods. These include: (i) examining the capacity and structural integrity of water and wastewater infrastructure including pipelines, pumps, flow devices, and other equipment; (ii) inspecting stagnant waters in closed enclosures; (iii) identifying damages caused by chemical corrosion or microbiological fouling and scaling; then (iv) flushing with cold and then hot waters to clear debris and potential layers of biological matter and scaling; followed by (v) dosing a very high concentration of disinfectants to destroy the presence of potential pathogens including viruses. Office safety measures include humidity level checks in buildings, HVAC (heating, ventilation, and air-conditioning) system checks (inspection and calibration, if necessary), odor detection, and filter checks (CDC, 2020). Stagnant waters can increase the risk of growth and spread of Legionella and other biofilm-forming bacteria at ambient temperatures. Proper protocols should be followed to flush and eliminate the biofilms. Detailed information related to considerations for large building re-openings after extended stagnation is presented elsewhere (Proctor et al., 2020).
7.2. Point of use systems for remote locations
Water and wastewater treatment processes have been advanced significantly in recent decades. These advanced processes are still not affordable by many small communities around the world. In many residential and commercial buildings, especially remote settings, water systems can be left unused for prolonged periods. Along with proper precautionary methods, the point-of-use systems that provide improved water safety should be used. These point-of-use systems can be specialty filters or chemical reagents introduced into potable water before consumption and uses involving contact with skin.
7.3. Water safety and security in temporary settings
Water safety and security remain fundamental concerns in many developing countries, especially (SenGupta, 2020) for settlements, refugee areas, and emergency settings. Although significant scientific and technological advancements have been made worldwide, there are still large populations in Africa, Asia, and South America that lack access to water and sanitation necessities. The populations in these informal settings are at greatest risk, and they should be given a priority when allocating regional resources (Armitage & Nellums, 2020). The term 'WASH' i.e., Water, Sanitation, and Hygiene should be educated to the communities to develop an awareness of sanitation's importance. Resources should be directed to help these communities fight against diseases. Awareness of the community's response to combat the spread will vary depending on various factors such as the stage of the outbreak, available resources, and preparedness of the community, socioeconomic status and cultural differences (Ferrante & Fearnside, 2020; Lau, Chan, & Ng, 2020).
7.4. Develop modeling tools for estimating potential impacts
The first COVID-19 virus study reported by Ahmed and coworkers (Ahmed et al., 2020) included both sampling and simulation studies to estimate the number of infected individuals. They first tested virus RNA concentrations in wastewater and used these concentrations to estimate the total number of infected individuals in the catchment using Monte Carlo simulations. The model estimation agreed well with actual reported cases. Modeling can also help to predict mortality rate and transmission or effective as well as the productive number estimations. The SARS-CoV-2 mortality rate was initially estimated at 3.4 % in March 2020 based on the data reported in China (Guo et al., 2020). However, the Center for Disease Control and Prevention (CDC) estimates a mortality rate of 0.4 % based on five scenarios in the U.S. toward the end of May 2020 (CDC, 2020). An adequate reproductive number is another parameter that can be used to understand the intensity of outbreaks. Rt (effective reproduction rate) is calculated as a function of time and is the actual average number of secondary cases per primary case. The median Rt values for the first ten days of the COVID-19 epidemic were 2.90 and 2.83 for Spain and Italy, respectively, while the Latin American Rt estimations for Central and South American countries were higher in Ecuador (3.95), Panama (3.95), and Brazil (3.95). The lowest Rt was in Peru (2.36). All Latin American countries had Rt greater than 2 (Ochoa, Sanchez, Peñaloza, Motta, & Méndez-Fandiño, 2020). It should be noted that the Rt values change over time, depending on the length and intensity of outbreaks, geographical and regional socioeconomic backgrounds.
7.5. Specific measures and planning for water utility operations
Workforce safety is the top priority. Response to outbreaks by utilities should include the following components: 1) workforce safety protocols, 2) office and field infrastructure updates and 3) outbreak preparedness and response plans. Workforce safety protocols will include communication, education and training, availability of clean PPE and protocols for cleaning, materials, supplies for safety actions, and continuous testing and monitoring of staff and physical assessment and temperature measurements. Communication and training should be done in small groups to be more effective with specific details related to safety and occupational health in emergency times and those listed in Fig. 4. Office and field infrastructure should be updated with the following features:
-
1
Updated equipment and machinery
-
2
Proper ventilation in office, storage areas, and plant facilities
-
3
Work-from-home professional capacity
-
4
Online-monitoring capability with automation and data control optimization capacities
-
5
Staggered work schedules and staggered workforce schemes
Outbreak preparedness and response plans should include established and ongoing revisions of cybersecurity plan, contingency plan, resiliency plan for natural disasters and outbreaks, and risk plan for uncertainty in operations and extreme weather or third-party related events, including bioterrorism. Outbreak preparedness and response plans should consider both near-term and long-term scenarios by paying close attention to the uncertainty on an ongoing basis to review, revise, refine, and reform the plans necessary to respond, as discussed in Fig. 3. Table 2 shows the effectiveness of various approaches before, during, and after disease outbreaks for water utility operations in terms of workforce safety and process efficiency. It also highlights, administrative, engineering, preventive controls applicable in different scenarios.
Table 2.
Various stages of workforce activities, application of protective measures, and their effectiveness before, during and after outbreak.
| Strategy | Specific measure | Activity |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| During Outbreak |
|||||||||
| Before outbreak | Pre-entry | Travel to work | At water utility | At wastewater facility | Common spaces | Post-infection | After Outbreak | ||
| Avoid | Work from home | ✓ | ✓ | ||||||
| Online-monitoring capability with automation and data control optimization capacities | ✓ | ✓ | ✓ | ✓ | ✓ | ||||
| Educate | Communication | ✓ | ✓ | ✓ | ✓ | ✓ | |||
| Engineering Controls | Test and isolate | ✓ | ✓ | ✓ | ✓ | ✓ | |||
| Upgrade equipment | ✓ | ✓ | ✓ | ||||||
| Clean and disinfect | ✓ | ✓ | ✓ | ✓ | ✓ | ||||
| Separate in space and time | ✓ | ✓ | ✓ | ✓ | ✓ | ||||
| Temperature measurements | ✓ | ✓ | ✓ | ✓ | ✓ | ||||
| Administrative Controls | Drive safe behavior norms | ✓ | ✓ | ✓ | ✓ | ✓ | |||
| Increase awareness | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |||
| Insure and respond | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |||
| Update facilities | ✓ | ✓ | ✓ | ✓ | |||||
| Protect Personnel | Use protective equipment | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| Frequent handwashing | ✓ | ✓ | ✓ | ✓ | ✓ | ||||
| Preparedness and Response | Cyber security plan | ✓ | ✓ | ✓ | ✓ | ||||
| Contingency plan | ✓ | ✓ | ✓ | ✓ | |||||
| Resiliency plan | ✓ | ✓ | ✓ | ✓ | |||||
| Risk plan for uncertainty | ✓ | ✓ | ✓ | ✓ | ✓ | ||||
8. Concluding remarks
As the global pandemic COVID-19 accelerates, extreme measures were taken to take control over its spread. Current practices to manage the crisis include taking shifts, cleaning/disinfection public areas, wearing PPE when necessary and staggering work schedules and workforce which are all identified as essential measures for containing the virus. Water utilities should keep track of the water quality for potential pathogenic material and formulate required chemical treatment and disinfection process schemes. It is also critical for wastewater utilities to provide the workforce with with proper PPE and full suits in the field, especially while working around aeration tanks and other biological treatment units. Tightened monitoring and control of fecal coliforms and residual chlorines are also crucial during this period. Contingency, preparedness, and response and resiliency plans should be established if not available and must be improved continuously as a precaution to unexpected events. Utilities should collaborate among peers and academic and research partners to share the findings and develop better-informed solutions. Wastewater-based epidemiology should be considered to implement community-wide monitoring and tracking in order to respond to the outbreaks quickly and efficiently. Protocols should be developed to normalize research findings from various researchers. Evidence-based knowledge should be promoted to support risk analysis.
Although significant investments are being placed in water and wastewater treatment sectors of many developing countries, technologies that enable efficient removal of biological pollutants are still not available for many communities in all countries. Populations that depend on untreated surface water are at most risk of contracting the disease from various microorganisms, including viruses. Therefore, investments in the water sector (water and wastewater utilities) should be considered as derivatives of economic growth in these regions to promote public health and prosperity.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
VGG acknowledges the support received from the Kelly Gene Cook, Sr. Endowed Chair in the civil and environmental engineering department at Mississippi State University. This research was supported in part by the USDA-NIFA (US Department of Agriculture) Competitive Research Grant 2020-67019-30772 to Dr. Gude and his team. He also acknowledges the support received from The United States Geological Survey (USGS) and Mississippi Water Resources Research Institute (MWRRI) under two different research grants and the support received from The United States Environmental Protection Agency (USEPA) under four different research grants. Any opinions, findings, and conclusions or recommendations expressed in this material are those of the authors and do not necessarily reflect the views of the USDA, USGS, MWRRI, or USEPA.
References
- Ahmed W., Angel N., Edson J., Bibby K., Bivins A., O’Brien J.W. First confirmed detection of SARS-CoV-2 in untreated wastewater in Australia: A proof of concept for the wastewater surveillance of COVID-19 in the community. The Science of the Total Environment. 2020;(April (18)) doi: 10.1016/j.scitotenv.2020.138764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Annalaura C., Ileana F., Dasheng L., Marco V. Making waves: Coronavirus detection, presence and persistence in the water environment: State of the art and knowledge needs for public health. Water Research. 2020;(May (5)) doi: 10.1016/j.watres.2020.115907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armitage R., Nellums L.B. Water, climate change, and COVID-19: Prioritising those in water-stressed settings. The Lancet Planetary Health. 2020;4(5):e175. doi: 10.1016/S2542-5196(20)30084-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ashraf B.N. Economic impact of government interventions during the COVID-19 pandemic: International evidence from financial markets. Journal of Behavioral and Experimental Finance. 2020;27(September (1)) doi: 10.1016/j.jbef.2020.100371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- AWWA . American Water Works Association; 2020. State of the water industry, annual industry report. awwa.org/SOTWI. [Google Scholar]
- Bean B., Moore B.M., Sterner B., Peterson L.R., Gerding D.N., Balfour H.H., Jr. Survival of influenza viruses on environmental surfaces. The Journal of Infectious Diseases. 1982;146(1):47–51. doi: 10.1093/infdis/146.1.47. July 1. [DOI] [PubMed] [Google Scholar]
- Brian D.A., Baric R.S. Springer; Berlin, Heidelberg: 2005. Coronavirus genome structure and replication. InCoronavirus replication and reverse genetics; pp. 1–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cao G., Noti J.D., Blachere F.M., Lindsley W.G., Beezhold D.H. Development of an improved methodology to detect infectious airborne influenza virus using the NIOSH bioaerosol sampler. Journal of Environmental Monitoring. 2011;13(12):3321–3328. doi: 10.1039/c1em10607d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casanova L., Rutala W.A., Weber D.J., Sobsey M.D. Survival of surrogate coronaviruses in water. Water Research. 2009;43(7):1893–1898. doi: 10.1016/j.watres.2009.02.002. Apr 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CDC 2010. https://www.cdc.gov/h1n1flu/qa.htm (Accessed online on May 31st 2020).
- CDC . 2020. Guidance for reopening buildings after prolonged shutdown or reduced operation.https://www.cdc.gov/coronavirus/2019-ncov/php/building-water-system.html [Google Scholar]
- Chen Y., Chen L., Deng Q., Zhang G., Wu K., Ni L. The presence of SARS‐CoV‐2 RNA in the feces of COVID‐19 patients. Journal of Medical Virology. 2020 doi: 10.1002/jmv.25825. [DOI] [PubMed] [Google Scholar]
- CRS . 2020. Global economic effects of COVID-19. Congressional research service document. R46270. [Google Scholar]
- Daughton C. The international imperative to rapidly and inexpensively monitor community-wide Covid-19 infection status and trends. The Science of the Total Environment. 2020;(March (23)) doi: 10.1016/j.scitotenv.2020.138149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delanka-Pedige H.M., Munasinghe-Arachchige S.P., Zhang Y., Nirmalakhandan N. Bacteria and virus reduction in secondary treatment: Potential for minimizing post disinfectant demand. Water Research. 2020;(April (11)) doi: 10.1016/j.watres.2020.115802. [DOI] [PubMed] [Google Scholar]
- Di Marco M., Baker M.L., Daszak P., De Barro P., Eskew E.A., Godde C.M. Opinion: Sustainable development must account for pandemic risk. Proceedings of the National Academy of Sciences. 2020;117(8):3888–3892. doi: 10.1073/pnas.2001655117. Feb 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong E., Du H., Gardner L. An interactive web-based dashboard to track COVID-19 in real time. The Lancet Infectious Diseases. 2020;20(5):533–534. doi: 10.1016/S1473-3099(20)30120-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dublineau A., Batejat C., Pinon A., Burguiere A.M., Manuguerra J.C. Persistence of the 2009 pandemic influenza A (H1N1) virus in water and on non-porous surface. PloS One. 2011;6(11) doi: 10.1371/journal.pone.0028043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feied C. 2004. Novel Antimicrobial Surface Coatings and the Potential for Reduced Fomite Transmission of SARS and Other Pathogens. [Google Scholar]
- Ferrante L., Fearnside P.M. Protect indigenous peoples from COVID-19. Science. 2020;368(6488):251. doi: 10.1126/science.abc0073. [DOI] [PubMed] [Google Scholar]
- Gude V.G. Desalination and sustainability–an appraisal and current perspective. Water Research. 2016;89(February (1)):87–106. doi: 10.1016/j.watres.2015.11.012. [DOI] [PubMed] [Google Scholar]
- Gude V.G. Desalination and water reuse to address global water scarcity. Reviews in Environmental Science and Biotechnology. 2017;16(4):591–609. Dec 1. [Google Scholar]
- Gude V.G. Desalination of deep groundwater aquifers for freshwater supplies–Challenges and strategies. Groundwater for Sustainable Development. 2018;6(March (1)):87–92. [Google Scholar]
- Gude V.G. Energy and water autarky of wastewater treatment and power generation systems. Renewable and Sustainable Energy Reviews. 2015;45(May (1)):52–68. [Google Scholar]
- Guerriero C., Haines A., Pagano M. Health and sustainability in post-pandemic economic policies. Nature Sustainability. 2020;(June (8)):1–3. doi: 10.1038/s41893-020-0575-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gundy P.M., Gerba C.P., Pepper I.L. Survival of coronaviruses in water and wastewater. Food and Environmental Virology. 2009;1(1):10. Mar 1. [Google Scholar]
- Guo Y.R., Cao Q.D., Hong Z.S., Tan Y.Y., Chen S.D., Jin H.J. The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak–an update on the status. Military Medical Research. 2020;7(December (1)) doi: 10.1186/s40779-020-00240-0. 1-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayward A.C., Fragaszy E.B., Bermingham A., Wang L., Copas A., Edmunds W.J. Comparative community burden and severity of seasonal and pandemic influenza: Results of the Flu Watch cohort study. The Lancet Respiratory Medicine. 2014;2(6):445–454. doi: 10.1016/S2213-2600(14)70034-7. Jun 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- IMF . International Monetary Fund; 2020. Fiscal monitor. April 14, 2020, p. 2. [Google Scholar]
- Jia S., Zhang X. InHigh-risk pollutants in wastewater. Elsevier; 2020. Biological HRPs in wastewater; pp. 41–78. Jan 1. [Google Scholar]
- Jiang X., Rayner S., Luo M.H. Does SARS‐CoV‐2 has a longer incubation period than SARS and MERS? Journal of Medical Virology. 2020;92(May (5)):476–478. doi: 10.1002/jmv.25708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jilani T.N., Jamil R.T., Siddiqui A.H. StatPearls Publishing; 2019. H1N1 influenza (Swine flu). InStatPearls [Internet] Jun 9. [Google Scholar]
- Juan-García P., Butler D., Comas J., Darch G., Sweetapple C., Thornton A. Resilience theory incorporated into urban wastewater systems management. State of the art. Water Research. 2017;1(15):149–161. doi: 10.1016/j.watres.2017.02.047. May 15. [DOI] [PubMed] [Google Scholar]
- Kim S.H., Chang S.Y., Sung M., Park J.H., Bin Kim S.H., Lee H. Extensive viable Middle East respiratory syndrome (MERS) coronavirus contamination in air and surrounding environment in MERS isolation wards. Reviews of Infectious Diseases. 2016;63(3):363–369. doi: 10.1093/cid/ciw239. Aug 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- La Rosa G., Bonadonna L., Lucentini L., Kenmoe S., Suffredini E. Coronavirus in water environments: Occurrence, persistence and concentration methods-A scoping review. Water Research. 2020;(April (28)) doi: 10.1016/j.watres.2020.115899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lau B.H., Chan C.L., Ng S.M. Resilience of Hong Kong people in the COVID-19 pandemic: Lessons learned from a survey at the peak of the pandemic in Spring 2020. Asia Pacific Journal of Social Work and Development. 2020:1–10. [Google Scholar]
- Lofrano G., Brown J. Wastewater management through the ages: A history of mankind. The Science of the Total Environment. 2010;408(22):5254–5264. doi: 10.1016/j.scitotenv.2010.07.062. Oct 15. [DOI] [PubMed] [Google Scholar]
- McAndrew B. Resilience of UK water and wastewater systems: Why we need to get wise before we get smart. InREA Symposium on Resilience Engineering Embracing Resilience. 2019 May 24. [Google Scholar]
- Megahed N.A., Ghoneim E.M. Antivirus-built environment: Lessons learned from Covid-19 pandemic. Sustainable Cities and Society. 2020:102350. doi: 10.1016/j.scs.2020.102350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morawska L., Cao J. Airborne transmission of SARS-CoV-2: The world should face the reality. Environment International. 2020;(April (10)) doi: 10.1016/j.envint.2020.105730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Infrastructure Advisory Council (NIAC) 2016. Water sector resilience final report and recommendations. Accessed online on August 20, 2020. [Google Scholar]
- Nature Coronavirus misinformation needs engagement. Nature. 2020;581(7809):355–356. doi: 10.1038/d41586-020-01550-y. [DOI] [PubMed] [Google Scholar]
- Ochoa Y.C., Sanchez D.E., Peñaloza M., Motta H.F., Méndez-Fandiño Y.R. Effective reproductive number estimation for initial stage of COVID-19 pandemic in Latin American Countries. International Journal of Infectious Diseases. 2020;(April (30)) doi: 10.1016/j.ijid.2020.04.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orive G., Lertxundi U., Barcelo D. Early SARS-CoV-2 outbreak detection by sewage-based epidemiology. The Science of the Total Environment. 2020;(May (8)) doi: 10.1016/j.scitotenv.2020.139298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Otto B., Kuzma S., Strong C., Chertock M. Water Resources Institute; 2020. Combating the coronavirus without clean water.https://www.wri.org/blog/2020/04/coronavirus-water-scarcity-hand-washing [Google Scholar]
- Petrosillo N., Viceconte G., Ergonul O., Ippolito G., Petersen E. COVID-19, SARS and MERS: Are they closely related? Clinical Microbiology and Infection. 2020;(March (28)) doi: 10.1016/j.cmi.2020.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Proctor C.R., Rhoads W.J., Keane T., Salehi M., Hamilton K., Pieper K.J. 2020. Considerations for large building water quality after extended stagnation. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahman M.A. Data-driven dynamic clustering framework for mitigating the adverse economic impact of Covid-19 lockdown practices. Sustainable Cities and Society. 2020:102372. doi: 10.1016/j.scs.2020.102372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ray I. Viewpoint| Handwashing and COVID-19: Simple, right there…? World Development. 2020:105086. doi: 10.1016/j.worlddev.2020.105086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Retzlaff K.J. Water utility communications can build trust during the COVID‐19 pandemic. Journal-American Water Works Association. 2020;112(August (8)):24. doi: 10.1002/awwa.1553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rimoldi S.G., Stefani F., Gigantiello A., Polesello S., Comandatore F., Mileto D. Presence and vitality of SARS-CoV-2 virus in wastewaters and rivers. medRxiv. 2020;(January (1)) doi: 10.1016/j.scitotenv.2020.140911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rockx B., Kuiken T., Herfst S., Bestebroer T., Lamers M.M., Munnink B.B. Comparative pathogenesis of COVID-19, MERS, and SARS in a nonhuman primate model. Science. 2020;(April (17)) doi: 10.1126/science.abb7314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rumpler R., Venkataraman S., Göransson P. An observation of the impact of CoViD-19 recommendation measures monitored through urban noise levels in central Stockholm, Sweden. Sustainable cities and society. 2020;(September (3)) doi: 10.1016/j.scs.2020.102469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sannigrahi S., Pilla F., Basu B., Basu A.S., Molter A. Examining the association between socio-demographic composition and COVID-19 fatalities in the European region using spatial regression approach. Sustainable Cities and Society. 2020:102418. doi: 10.1016/j.scs.2020.102418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmidt P.J., Anderson W.B., Emelko M.B. Describing water treatment process performance: Why average log-reduction can be a misleading statistic. Water Research. 2020;(March (9)) doi: 10.1016/j.watres.2020.115702. [DOI] [PubMed] [Google Scholar]
- SenGupta A.K. COVID-19 and unsafe water: A tale of two enemies. Environmental Engineering Science. 2020;37:393–394. [Google Scholar]
- Sims N., Kasprzyk-Hordern B. Future perspectives of wastewater-based epidemiology: Monitoring infectious disease spread and resistance to the community level. Environment International. 2020;(April (4)) doi: 10.1016/j.envint.2020.105689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh R.P., Javaid M., Kataria R., Tyagi M., Haleem A., Suman R. Significant applications of virtual reality for COVID-19 pandemic. Diabetes and Metabolic Syndrome Clinical Research and Reviews. 2020;(May (12)) doi: 10.1016/j.dsx.2020.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SIWI . 2005. Stockholm International Water Institute: Making water a part of economic development. [Google Scholar]
- Sowby R.B. Emergency preparedness after COVID-19: A review of policy statements for the US water sector. Utilities Policy. 2020:101058. doi: 10.1016/j.jup.2020.101058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun C., Zhai Z. The efficacy of social distance and ventilation effectiveness in preventing COVID-19 transmission. Sustainable Cities and Society. 2020;62(November (1)) doi: 10.1016/j.scs.2020.102390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Switzer D., Wang W., Hirschvogel L. Municipal utilities and COVID-19: Challenges, responses, and collaboration. The American Review of Public Administration. 2020;50(August (6-7)):577–583. [Google Scholar]
- The Value of Water Campaign . 2017. The economic benefits of investing in water infrastructure.www.thevalueofwater.org [Google Scholar]
- Thompson K.A., Bennett A.M. Persistence of influenza on surfaces. The Journal of Hospital Infection. 2017;95(2):194–199. doi: 10.1016/j.jhin.2016.12.003. Feb 1. [DOI] [PubMed] [Google Scholar]
- USDHS . National Protection and Programs Directorate; 2014. Sector resilience report: Water and wastewater systems. [Google Scholar]
- USDHS . 2020. Advisory memorandum on identification of essential critical infrastructure workers during covid-19 response. [Google Scholar]
- USEPA . 2015. Systems measures of water distribution system resilience. EPA 600/R-14/383. [Google Scholar]
- USEPA . 2019. Risk and Resilience Assessment and emergency response plans. Office of Water(4608T) EPA-817-F-19-004, May 2019. [Google Scholar]
- van Doremalen N., Bushmaker T., Morris D.H., Holbrook M.G., Gamble A., Williamson B.N. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. The New England Journal of Medicine. 2020;382(16):1564–1567. doi: 10.1056/NEJMc2004973. Apr 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang X.W., Li J.S., Jin M., Zhen B., Kong Q.X., Song N. Study on the resistance of severe acute respiratory syndrome-associated coronavirus. Journal of Virological Methods. 2005;126(1–2):171–177. doi: 10.1016/j.jviromet.2005.02.005. Jun 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warner M.E., Zhang X., Rivas M.G. Which states and cities protect residents from water shutoffs in the COVID-19 pandemic? Utilities Policy. 2020;(September (21)) doi: 10.1016/j.jup.2020.101118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WEF . Wter Environment Federation; 2020. Protecting wastewater professionals from Covid-19 and other biological hazards. [Google Scholar]
- Weiss S.R., Leibowitz J.L. Vol. 81. Academic Press; 2011. Coronavirus pathogenesis; pp. 85–164. (Advances in virus research). Jan 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO . World Health Organization; 2015. Middle East respiratory syndrome coronavirus (MERS-CoV)https://www.who.int/emergencies/mers-cov/en/ 2015. [Google Scholar]
- WHO . World Health Organization; 2018. World Health Organization. Investigation of cases of human infection with Middle East respiratory syndrome coronavirus (MERS-CoV): Interim guidance. 2018. [Google Scholar]
- WHO . 2020. Water, sanitation, hygiene, and waste management for SARS-CoV-2, the virus that causes COVID-19 Interim guidance. 29 July 2020. Accessed online on August 4, 2020. [Google Scholar]
- WHO . World Health Organization; 2003. World Health Organization. Consensus document on the epidemiology of severe acute respiratory syndrome (SARS) 2003. [Google Scholar]
- WHO . World Health Organization; Geneva, Switzerland: 2003. World Health Organization. First data on stability and resistance of SARS coronavirus compiled by members of WHO laboratory network. http://www. who. int/csr/sars/survival_2003_05_04/en/index. html. 2003. [Google Scholar]
- WHO 2019a. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/question-and-answers-hub/q-a-detail/q-a-coronaviruses (Accessed online on May 31st 2020).
- WHO . 2019. Draft MERS-CoV Surface sampling of MERS-CoV in health care settings: A practical “how to” protocol for health care and public health professionals. June 2019. [Google Scholar]
- Zambrano-Monserrate M.A., Ruano M.A., Sanchez-Alcalde L. Indirect effects of COVID-19 on the environment. The Science of the Total Environment. 2020;(April (20)) doi: 10.1016/j.scitotenv.2020.138813. [DOI] [PMC free article] [PubMed] [Google Scholar]
Further reading
- Wang J., Shen J., Ye D., Yan X., Zhang Y., Yang W. Disinfection technology of hospital wastes and wastewater: Suggestions for disinfection strategy during coronavirus Disease 2019 (COVID-19) pandemic in China. Environmental Pollution. 2020;(April (24)) doi: 10.1016/j.envpol.2020.114665. [DOI] [PMC free article] [PubMed] [Google Scholar]