Achieving endoscopic biliary access in the setting of altered GI anatomy poses notable technical challenges. Although percutaneous drainage remains a viable alternative, endoscopic approaches are generally preferred by patients because of improvements in quality of life. Roux-en-Y hepaticojejunostomy (RYHJ) biliary reconstruction during liver transplantation is one such example of altered GI anatomy not generally amenable to biliary interventions using conventional endoscopic techniques. We describe a case demonstrating a successful endoscopic approach to achieve biliary access and treat biliary cast syndrome in a patient with a right lobe liver transplant with RYHJ reconstruction.
A 59-year-old man with primary sclerosing cholangitis complicated by cirrhosis underwent a right lobe living donor liver transplant with RYHJ biliary reconstruction. He subsequently presented with biliary obstruction. An MRI study on posttransplant day 10 identified a hepaticojejunostomy stricture and infected biloma requiring percutaneous transhepatic biliary drain placement. Percutaneous cholangiogram 8 weeks later revealed resolution, and the percutaneous transhepatic biliary drain was removed. Shortly thereafter, the patient developed fatigue, fevers, and abnormal liver chemistry results consistent with cholangitis.
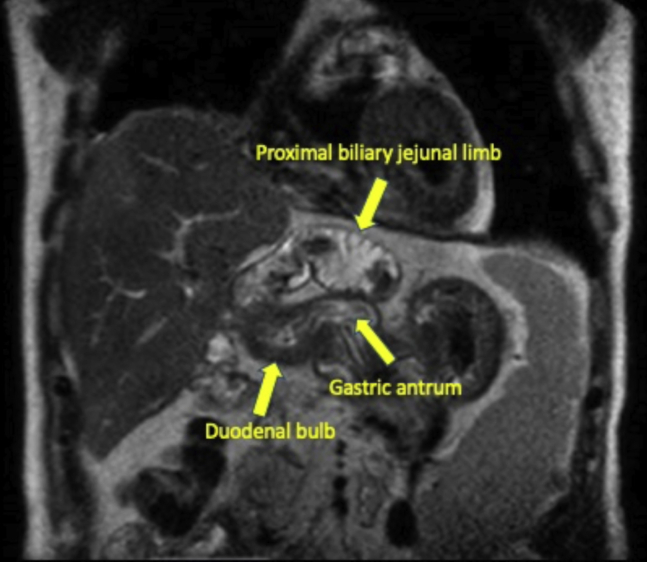
The patient declined repeat percutaneous intervention. Identification of the hepaticojejunostomy to allow for subsequent endoscopic retrograde cholangiography was attempted using a pediatric colonoscope. The jejunojejunal anastomosis could not be identified, and this approach was aborted (Video 1, available online at www.VideoGIE.org). An enteroscope was not used given difficulty in biliary interventions with this type of endoscope and the need for multiple interventions. Multidisciplinary review of the recent MRI scan revealed the proximal biliary jejunal limb in close proximity to the gastric antrum and duodenal bulb (Fig. 1), potentially allowing for EUS-guided access to the biliary anastomosis. The risks and options were discussed with the patient, who elected to proceed with an EUS approach.
Figure 1.
MRI revealed the proximal biliary jejunal limb in close proximity to the gastric antrum and duodenal bulb.
The linear-array echoendoscope was advanced to the gastric antrum, and the proximal aspect of the jejunal biliary limb was identified. After administration of intravenous antibiotics, a 19-gauge EUS-FNA needle was used to puncture the small bowel (Fig. 2) and bile was aspirated, confirming endoscopic location near the hepaticojejunostomy. A large volume of dilute contrast and methylene blue was injected into the biliary limb (Fig. 3). After adequate distension of the biliary limb, a 15- × 10-mm cautery-enhanced lumen-apposing metal stent (LAMS) was advanced into the jejunal biliary limb under endosonographic and fluoroscopic guidance.
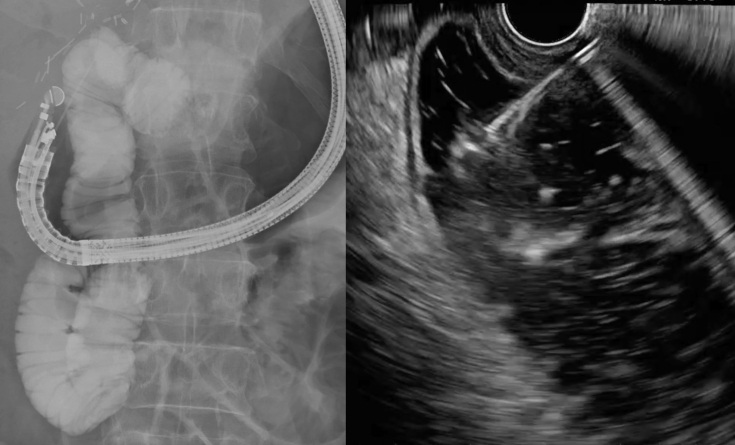
Figure 2.
A 19-gauge EUS-FNA needle was used to puncture the small bowel.
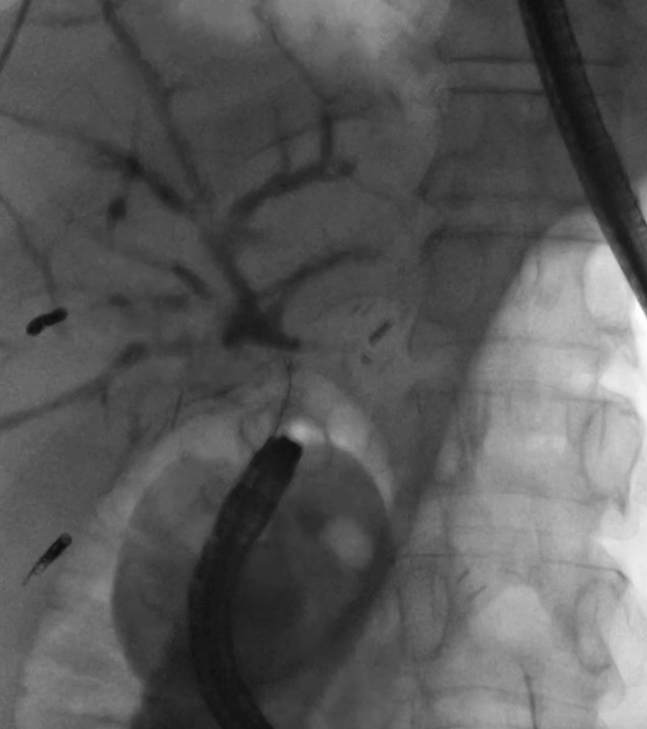
Figure 3.
A large volume of dilute contrast and methylene blue was injected into the biliary limb.
After deployment of the proximal flange in the gastric antrum, there was reflux of bile and blue-tinged fluid into the gastric lumen (Fig. 4). Next, a long wire was advanced into the jejunal limb. The LAMS was successfully balloon dilated to 13.5 mm under endoscopic and fluoroscopic guidance (Video 1). The echoendoscope was exchanged for a standard gastroscope. The gastroscope was passed into the biliary jejunal limb via the LAMS, and the strictured hepaticojejunostomy was identified within 2 cm of the anastomosis (Fig. 5). The biliary tree was accessed using an angled guidewire and dual-lumen catheter.
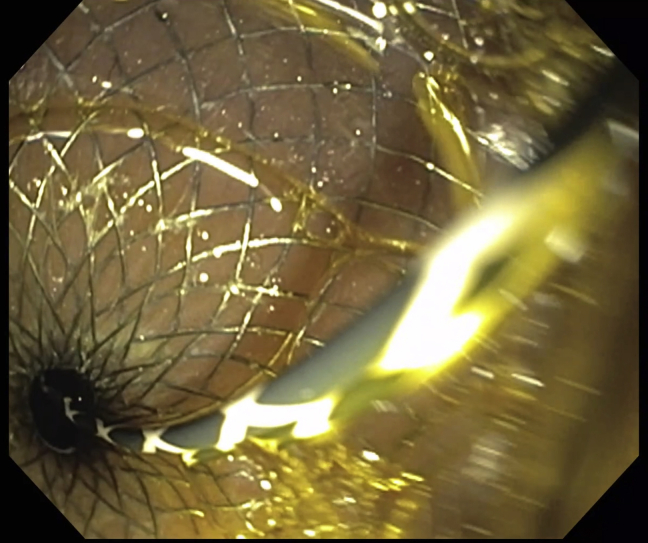
Figure 4.
After deployment of the proximal flange in the gastric antrum, there was reflux of bile and blue-tinged fluid into the gastric lumen.
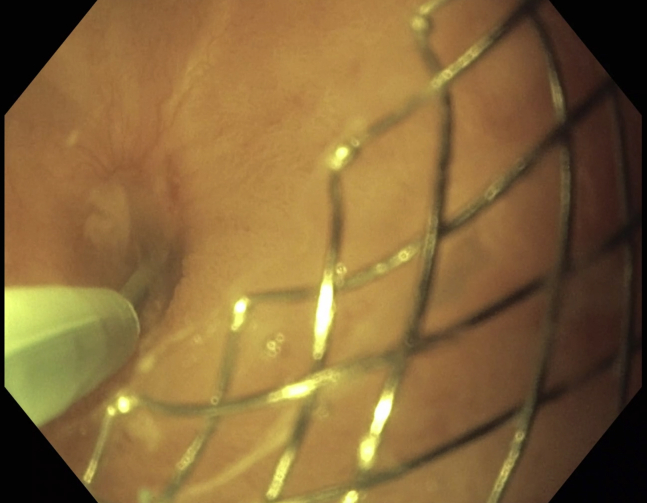
Figure 5.
The gastroscope was passed into the biliary jejunal limb via the lumen-apposing metal stent, and the strictured hepaticojejunostomy was identified within 2 cm of the anastomosis.
A cholangiogram was performed and revealed choledocholithiasis (Fig. 6). The strictured hepaticojejunostomy was successfully balloon dilated and a 7F × 7-cm stent was placed across the stricture (Fig. 7, fluoroscopic image). The patient was discharged home after the procedure but developed mild cholangitis necessitating oral antibiotics. The patient underwent 3 additional procedures, which included balloon dilation of the anastomosis, balloon sweeps, and stent placement, until significant improvement was noted. The final cholangiogram demonstrated significant improvement (Fig. 8). Therefore, a stent-free trial was attempted, and the patient has done well to date.
Figure 6.
A cholangiogram revealed choledocholithiasis.
Figure 7.
The strictured hepaticojejunostomy was stented with a 7F × 7-cm stent.
Figure 8.
The final cholangiogram demonstrated significant improvement.
In conclusion, patients who undergo liver transplant with Roux-en-Y biliary reconstruction present a significant endoscopic challenge when biliary access is required. Our case demonstrates that an EUS-guided approach can be a powerful tool to create a luminal anastomosis to serve as a conduit to facilitate biliary intervention when conventional procedures are unsuccessful or undesirable.
Disclosure
Dr Law is a consultant for Olympus America. All other authors disclosed no financial relationships.
Supplementary data
EUS-guided gastrojejunal anastomosis to facilitate endoscopic retrograde cholangiography in a patient with a right lobe liver transplant and Roux-en-Y anatomy.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
EUS-guided gastrojejunal anastomosis to facilitate endoscopic retrograde cholangiography in a patient with a right lobe liver transplant and Roux-en-Y anatomy.