Abstract
Background
Many children with autism spectrum disorder (ASD) have problem behaviors that interfere with learning and social interaction.
Methods
This randomized controlled trial compared treatment with functional communication training (FCT) to “treatment as usual” for young children with ASD (n=38, ages 21–84 months). FCT was conducted by parents with training and real-time coaching provided by behavioral consultants using telehealth.
Results
FCT treatment via telehealth achieved a mean reduction in problem behavior of 98% compared to limited behavioral improvement in children receiving “treatment as usual” during a 12-week period. Social communication and task completion also improved.
Conclusions
For children with ASD and moderate to severe behavior problems, parent-implemented FCT using telehealth significantly reduced problem behavior while ongoing interventions typically did not.
Keywords: Autism Spectrum Disorder, Problem Behavior, Functional Communication, Training, Telehealth, Children, Randomized Controlled Trial
Children with autism spectrum disorder (ASD) are at significantly high risk for developing problems with destructive and disruptive behavior (Horner, Carr, Strain, Todd, & Reed, 2002; Soke et al., 2016). These problems may take the form of many different types of behavior, with the most severe being aggression (e.g., hitting, biting, yelling), self-injury (e.g., head-banging, eye-gouging, hitting or biting self), property destruction (e.g., breaking items, throwing items), and severe noncompliance. These behaviors can severely limit a child’s opportunities to engage in positive social interactions, to benefit from therapeutic interventions, and to participate fully in daily life at home and in the community.
When behavior problems are serious enough to require treatment, several evidence-based options are available, including therapy from a behavior therapist or behavior analyst (Ahearn & Tiger, 2013), parent education or parent training (Bearss et al., 2015), or psychoactive medication (Aman et al., 2009). For behavioral treatment in ASD, applied behavior analysis (ABA) has been studied extensively, and core ABA principles (e.g., reinforcement, extinction, etc.) are critical components of many of the most widely used evidence-based interventions (Wong et al., 2015), regardless of whether the intervention focuses on skill acquisition (Dawson et al., 2010; Koegel & Koegel, 1988; Lovaas, 1987) or the direct treatment of problem behavior (Lindgren et al., 2016). Among the ABA methods used to treat problem behavior in ASD, functional communication training (FCT; Carr & Durand, 1985) is used most extensively, and prior studies have shown that FCT can successfully treat many different problem behaviors in diverse populations and across a range of environments (Lindgren et al., 2016; Reichle & Wacker, 2017; Tiger, Hanley, & Bruzek, 2008).
In practice, FCT usually begins with a functional analysis (FA; Iwata, Dorsey, Slifer, Bauman, & Richman, 1994) to identify the class of reinforcement, or “function,” that maintains problem behavior for each child (Durand & Carr, 1985; Reichle & Wacker, 2017). The social functions that are typically identified are escape (avoiding a nonpreferred activity), tangible (obtaining a desired object or activity), and attention (gaining attention from an adult or peer). After the function(s) of a problem behavior has been identified, children are taught to use alternative communication strategies (e.g., speaking, pointing to picture cards, pressing a microswitch, etc.) that result in the same reinforcer as the problem behavior (Carr, 1988). By substituting appropriate social communication in the form of mands (appropriate requests) to replace a child’s inappropriate behavior, FCT can reduce problem behavior, change the way a child interacts with family and peers, and help the child function more successfully in daily life (Reichle & Wacker, 2017). For these reasons, FA combined with FCT typically represents the preferred treatment for destructive or disruptive behavior when treatment is provided by behavioral psychologists or behavior analysts (Reichle & Wacker, 2017; Tiger et al., 2008).
Even when an effective behavioral intervention can be identified for treating problem behavior in ASD, access to intervention may be limited by geographic location, provider availability, family circumstances, or cost. To help overcome these barriers, telehealth service delivery models have been developed to improve access to behavioral services (Wacker et al., 2013b). A comparison study showed that parent-implemented FCT could be delivered via telehealth coaching with similar outcomes and at lower cost compared with having behavior therapists travel to work with children and parents in their homes (Lindgren et al., 2016). Thus, effective behavioral treatments such as FCT can be conducted via telehealth, which permits greater access for families in diverse locations and increased opportunities to provide interventions to much larger populations of children with ASD.
The current study was designed as a randomized controlled trial (RCT) to test the efficacy of FCT delivered via telehealth as a treatment for significant problem behaviors demonstrated by young children with ASD. Although several decades of high-quality single-subject research have provided an extensive evidence base for FCT (Reichle & Wacker, 2017; Tiger et al., 2008; Wong et al., 2015), FCT has not been previously tested in a randomized trial. This study was conducted using single-case designs for each participant, including multielement designs for the FA and reversal and nonconcurrent multiple baseline designs for the FCT treatment. An in-home telehealth treatment model was used to ensure reduced costs and increased access for families in any geographic location as long as they were able to connect to high-speed internet. Treatment procedures were conducted by parents under the supervision of trained behavioral consultants using methods that have been previously tested in other studies using single-subject designs (Lindgren et al., 2016; Wacker et al., 2013b). The study design included a control group for which FCT treatment was delayed for 12 weeks until after the RCT was completed. For the delayed treatment group, any children who continued to show problem behavior after the 12-week delay were provided with FCT treatment.
The hypotheses tested in the study were that (1) parents could be trained and coached via live telehealth to use FA and FCT strategies to significantly reduce problem behavior and increase social communication in their children in comparison with children receiving their “usual” ongoing interventions, (2) children would demonstrate increases in manding and task completion during and after treatment, and (3) parents would report high levels of acceptance of treatment procedures delivered via telehealth.
METHODS
Study Design
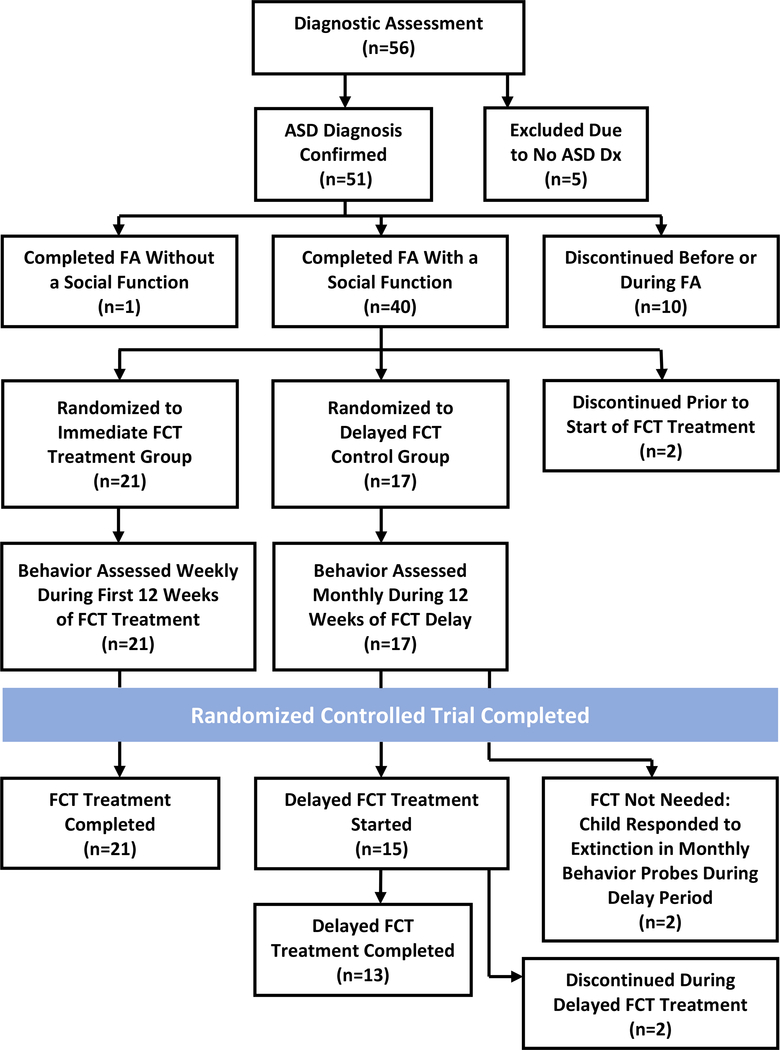
The study was designed as an RCT comparing treatment with FCT to a “waitlist control” group that received “treatment as usual” rather than FCT for the 12-week period during which the RCT was conducted. Twelve weeks was selected as an appropriate time period for group comparisons because it was long enough to allow behavior change to be seen in response to treatment (for the experimental group) while also representing a realistic waiting period (for the control group) because it was comparable to the average time that newly referred children with ASD waited for initial appointments in behavioral clinics at our medical center. After 12 weeks, the RCT phase of the study ended and all participants in the Delay (Control) group received treatment with FCT if their behavior continued to require treatment. In all cases, initial assessment using FA and subsequent treatment using FCT were conducted by parents with support from real-time telehealth coaching by a behavioral consultant (see Suess et al., 2014, and Wacker et al., 2013b, for more detailed descriptions of the type of procedures used for parent training and coaching). Figure 1 outlines the overall design of the randomized trial and shows the number of children who participated in each phase of the study.
Figure 1.
Randomized controlled trial: Study design and implementation
Study Outcomes
The primary outcome for the trial was the reduction in the frequency of problem behavior shown by the child; secondary outcomes were increases in mands (appropriate requests) and the number of developmentally appropriate “work” tasks completed during sessions. The durability of treatment effects was examined by collecting the same outcome data at six months after completion of treatment. The study was designed to have at least .90 power for detection of a difference between treatment groups of 10% or more in the mean percentage of reduction in problem behavior from baseline to the completion of the RCT (using a two-tailed test at the p < .05 level). The RCT design also included intention-to-treat analysis to control for bias associated with possible differential rates of attrition between the two treatment groups.
Participants
Participants were 56 young children (ages 21–84 months; 47 male, 9 female) referred to the study based on probable ASD and significant behavior problems. Referrals to the study came from clinical staff in pediatric and psychiatric clinics within a comprehensive university-based health care system, as well as from staff at regional pediatric clinics that were part of a statewide network affiliated with the university system. After comprehensive diagnostic evaluations, 51 of the 56 enrolled children were diagnosed with ASD and referred for telehealth-delivered FA and FCT. Thirty-eight children completed the FA and were randomized to one of the two treatment groups (Immediate vs. Delay) for the RCT. Minority representation was 10% for children in the study. Parents were trained and coached to implement FA+FCT procedures, and parents also provided ratings of their acceptance of treatment. Selected summary data from 32 of the participants had been included in a previous FCT study (Lindgren et al., 2016).
Inclusion criteria were as follows: (a) age in the range of 18–84 months, (b) a confirmed diagnosis of ASD, (c) significant problem behavior that was serious enough to interfere with daily functioning, and (d) willingness of at least one parent to participate in weekly telehealth sessions and to implement study procedures as directed. Problem behaviors were identified individually for each child based on parent report and occurrence of behaviors during the FA.
Definitions of Problem Behaviors
Topographies of problem behavior included self-injurious behavior (e.g., head banging), aggression (e.g., hitting), property destruction (e.g., throwing toys), verbal outbursts (e.g., screaming), and severe noncompliance. Self-injurious behavior occurred in the forms of hand biting, head hitting, head banging, and leg hitting. Hand biting was recorded when the child’s hand crossed the plane of the mouth and the mouth closed on the hand for any length of time. Head/leg hitting was defined as when the child’s open or closed hand contacted their head/leg (or any other part of their body) with force. A child’s head contacting the floor or another hard surface (e.g., a tabletop) from a distance of at least 6 in with force resulted in head banging being recorded. Topographies of aggressive behaviors were hitting, kicking, biting, and scratching. Hitting and kicking were defined as the child’s arms or legs contacting the body of another person from a distance of at least 6 in and with force. Biting was defined as the child’s mouth closing on the body of another person for any length of time. Scratching was defined as when the child’s hand moved laterally over another’s body with force. Property destruction was recorded when a child threw an item a distance of more than 6 in, displaced furniture, or wrote on unintended surfaces (e.g., walls). Verbal outbursts were recorded when an individual engaged in vocalizations above a conversational tone for more than 3 consecutive seconds. We stopped recording verbal outbursts when the child spoke in an appropriate volume for 3 consecutive seconds. Noncompliance was recorded when a child did not begin an adult-directed task within 5 seconds. We stopped recording noncompliance when the child began completing the adult-directed task for 5 consecutive seconds.
ASD Diagnosis, Randomization, and Informed Consent
The diagnosis of ASD was confirmed by a psychologist trained in using the ADI-R (Rutter, Le Couteur, & Lord, 2003), ADOS (Lord, Rutter, DiLavore, & Risi, 1999), and diagnostic criteria from DSM-IV (American Psychiatric Association, 1994) or DSM-5 (American Psychiatric Association, 2014). Children were referred for treatment with FCT if an FA identified problem behavior that served a “social” function (i.e., the behavior was reinforced by positive or negative reinforcement in the form of access to attention, access to preferred items or activities, or escape from demands). Children who completed the FA and were assigned at random to either the Immediate or the Delay treatment group (n = 38) were included in the randomized trial (see Figure 1). Randomization was carried out using permuted blocks with stratification based on gender, age (≤ 47 months vs. ≥ 48 months), and presence or absence of intellectual disability (ID). Twenty-one children were randomized to Immediate treatment with FCT, and 17 children were randomized to the Delay (Control) group, which received “treatment as usual” for 12 weeks before starting treatment with FCT. Ongoing treatments varied for each of these children and included activities such as speech or occupational therapy, educational programming, dietary restrictions, social skills training, psychoactive medication, and/or behavior management strategies or intervention plans being used in home or school settings. Randomization was not contingent on the behavioral functions identified during the FA or on the severity of problem behavior. Research procedures were reviewed and approved by an institutional review board for the protection of human subjects. Informed consent was obtained from all individual participants included in the study, with parents or legal guardians providing consent for the participating children.
Procedures and Instruments
Diagnostic and Developmental Assessments
In addition to using the ADI-R, ADOS, and DSM-IV/DSM-5 to confirm an ASD diagnosis, the study also included developmental assessments at baseline using the Mullen Scales of Early Learning (Mullen, 1995) and the Vineland Adaptive Behavior Scale – Second Edition (Vineland-II; Sparrow, Cicchetti, & Ballo, 2005) to determine the presence or absence of ID.
Behavioral Consultation
All FA and FCT procedures were conducted by the parents of the participating children within their own homes, with coaching provided by behavioral consultants via telehealth. The consultants were behavior analysts or advanced graduate trainees with a minimum of two years of supervised work experience in behavior analysis. Weekly supervision and analysis of FA+FCT data were provided by a doctoral-level behavioral psychologist throughout the study. The teleconferencing procedures used by the behavioral consultants to provide FA and FCT coaching to parents were based on those described by Wacker et al. (2013a), Suess et al. (2014), and Lindgren et al. (2016).
Functional Analysis
With assistance from telehealth coaching by behavioral consultants, parents conducted the FA procedures within a multielement single-case design based on methods described by Iwata et al. (1994). Each FA session was 5 minutes in duration and was digitally recorded for later coding/scoring by independent data collectors; three to five sessions were typically completed during each 60-minute telehealth visit. The FA sessions were conducted using procedures described by Harding, Wacker, Berg, Lee, & Dolezal (2009). One social function (i.e., escape, tangible, or attention) was evaluated per session. The parent intermittently instructed the child to complete tasks (e.g., “Put the block in the bucket.”) during an escape session, restricted the child’s access to a preferred toy during a tangible session, and restricted parent attention to the child during an attention session. Reinforcement (i.e., providing a break from the task, access to the preferred toy, or access to the parent’s attention) was delivered to the child when problem behavior occurred. A “free play” (control) condition was also provided to give the child noncontingent access to preferred items and attention without any restrictions or task demands. The child’s response during these FA sessions was used to determine the conditions that were functioning to reinforce the child’s problem behavior.
Functional Communication Training
After completing the FA, children in the trial were randomized to either the Immediate treatment group or the Delay treatment group. Baseline sessions for both groups were based on either the identified FA condition that maintained problem behavior or on extinction (i.e., ignoring problem behavior). Extinction was the most common baseline condition conducted prior to starting FCT (and was used with 76% of participants) because it allowed for evaluation of the occurrence of problem behavior in the absence of reinforcement; this condition also helped to determine if additional treatment components (other than extinction) were needed to decrease the occurrence of problem behavior. In some cases, extinction can produce increases in the intensity or rate of problem behavior; for this reason, some parents chose instead to use the results of the FA as the baseline. This decision was acceptable to the investigators because the use of FA as baseline is common in the ABA literature (Fuhrman, Fisher, & Greer, 2016). Regardless of the baseline procedure used, an average of 2.76 5-min sessions (range: 1–9 sessions) were conducted with each participant. Most baseline sessions were conducted across 1 to 2 weekly visits (M = 1.8 visits; range: 1–5).
After FCT treatment began, each weekly telehealth visit was approximately 60 minutes in duration; each individual session within a 60-minute visit lasted 5 minutes and was recorded for later data coding/scoring. To facilitate communication during FCT, a word/picture card or microswitch (with recorded voice output) was paired with any pre-existing mand. Appropriate requests were reinforced by the parent, and the occurrence of problem behavior was ignored (placed on extinction) or resulted in the parent providing guided compliance. An individualized FCT treatment plan was developed based on the results of the FA. For example, if the FA identified problem behavior that functioned to escape task demands, then the FCT treatment plan focused on teaching the child to request breaks appropriately after complying with instructions to complete a task. (Table 1 provides brief descriptions of the FCT procedures used to treat problem behavior maintained by escape or tangible functions.) A typical task demand was initiated by placing a small amount of developmentally appropriate “work” in front of the child and asking the child to complete the task (e.g., point to two pictures in a book). As soon as the task was completed, a word/picture card or microswitch was placed in front of the child, and the child was given a prompt to request a break. The choice of break activities was matched to a preference assessment (Roane, Vollmer, Ringdahl, & Marcus, 1998). Problem behavior resulted in continuation of the task or re-presentation of the task if the behavior occurred during a break. Parents were asked to practice FCT procedures for at least 10–15 minutes each day at home. (The treatment procedures were based on those described by Wacker, Harding, & Berg, 2011; Wacker et al., 2013b, provide additional description of how these procedures can be implemented via telehealth.)
Table 1.
Description of FCT Treatment Sessions Targeting Problem Behavior Maintained by Escape or Tangible Functions
| FCT Escape: Steps Completed by Parent and Child |
| 1 Child played with preferred items for approximately 30 seconds. |
| 2 Parent instructed the child to complete a developmentally appropriate task that was identified in the FA as resulting in problem behavior. |
| 3 Parent instruction to complete the task continued until the child completed the task. |
| 4 Parent prompted the child to request a break from the task by presenting a picture card or microswitch following completion of the task. |
| 5 Child requested a break by touching the microswitch or card and was allowed to play with preferred items for approximately two minutes. |
| 6 Child was directed to complete a new task in response to problem behavior that occurred during play. |
| 7 Steps 2 through 6 were repeated until the end of the treatment session. |
| FCT Tangible: Steps Completed by Parent and Child |
| 1 Child played with a high preferred tangible item for approximately 30 seconds. |
| 2 Parent restricted the child's access (for a specified amount of time) to the high preferred tangible item that was identified in the FA as resulting in problem behavior. |
| 3 Child was given access to a low preferred tangible item with which to play while waiting for access to the high preferred tangible item. |
| 4 Parent prompted the child to request access to the high preferred tangible item by presenting a picture card or microswitch following the specified amount of wait time. |
| 5 Child requested access to the high preferred tangible item by touching the microswitch or card and was allowed to play with the high preferred tangible item for approximately two minutes. |
| 6 Child was restricted from accessing the high preferred tangible item in response to problem behavior that occurred during play. |
| 7 Steps 2 through 6 were repeated until the end of the treatment session. |
Note. FCT = Functional Communication Training; FA = Functional Analysis
To make direct comparisons between the Immediate and Delay groups, the percentage of problem behavior for Immediate participants was assessed at the completion of 12 weeks of treatment sessions, even if FCT treatment was not yet complete at that point. On average, treatment was completed in nine weekly visits (range: 3–20 weeks) for children in the Immediate group, which meant that many children in the Immediate group had completed FCT by the end of the randomized trial. Treatment was planned to be continued for up to 25 weeks or until (a) at least an 80% reduction from baseline occurred for problem behavior over three consecutive FCT sessions, (b) the child complied with at least 80% of task requests, and (c) the child made requests independently at appropriate times.
Delay Group Procedures During RCT
During the 12-week RCT, the children in the Delay (Control) group did not begin FCT treatment, but they continued to receive all the supports and interventions that had been provided to them prior to enrollment in the study. While families waited to begin FCT treatment until after completion of the randomized trial, behavioral consultants coached parents to conduct two to three 5-min sessions during behavior monitoring visits that were conducted each month via telehealth. During these monthly visits, parents conducted extinction sessions to determine whether problem behavior was continuing to occur. For comparison with the Immediate treatment group as part of the RCT, the percentage of 6-sec intervals showing problem behavior for the Delay (Control) group at baseline was again assessed at the completion of 12 weeks of waiting to begin FCT treatment. If the assessment at 12 weeks demonstrated continuing problem behaviors, treatment with FCT was initiated at that time.
Treatment Acceptability
After treatment had ended, parents completed a 7-point scale to rate the acceptability of FCT treatment by using the first item of the Treatment Acceptability Rating Form-Revised (TARF-R; Reimers, Wacker, & Cooper, 1991). This item asked the parent “How acceptable do you find the treatment to be regarding your concerns about your child?” Responses to this question are highly correlated with the overall score on the full TARF-R.
Quantitative Analyses
Single-Subject Analyses
Data for all participants were collected within single-subject designs (multielement designs for the FA data and nonconcurrent multiple baseline across participants plus reversal designs for the FCT data), and observation sessions were recorded and scored for each FA and FCT visit. Each 5-min session was divided into 50 6-sec intervals, and problem behavior was coded if present in each interval. Interobserver agreement was obtained for 30% of sessions and averaged greater than 95% agreement.
Experimental Group vs. Control Group Comparisons
For the randomized trial, the percentage of 6-sec intervals with problem behavior in each session was recorded at baseline and at 12 weeks after the start of treatment for the Immediate (Experimental) group or at the end of the 12-week waiting period for the Delay (Control) group. In addition, behavioral observation data were scored at the end of FCT treatment for all subjects and then monitored again at 6 months after the completion of treatment. The overall percentage reduction in problem behavior was determined by computing the percentage of 6-sec intervals that included problem behavior at baseline minus the percentage of intervals with problem behavior at the end of FCT; that difference was then divided by the percentage of intervals with problem behavior at baseline and multiplied by 100. Similar data on increases in manding and task completion were analyzed to evaluate changes in positive behaviors involving communication and cooperation.
The Immediate and Delay groups were compared using a linear mixed model for repeated measures, with Time as the within-subjects factor and Treatment Group as the between-subjects factor. The primary outcome for the 12-week randomized trial was the percentage of intervals that showed problem behavior during each 5-min treatment session when baseline behavior was compared with behavior at 12 weeks for the two treatment groups. From the fitted statistical model, an estimate of the mean change (with 95% CI) within group was obtained and tested with the p-value adjusted by the Bonferroni method. When assumptions of the linear mixed model were not fully met, alternative statistical methods were also used to validate the findings. Results of the trial were reported using strategies adapted from the guidelines in the CONSORT (Consolidated Standards of Reporting Trials) 2010 statement (Schulz, Altman, Moher, & the CONSORT Group, 2010).
RESULTS
Behavioral Outcomes During the Randomized Controlled Trial
Sample Characteristics and Functional Analysis
All children in both the Immediate (Experimental) and the Delay (Control) treatment groups completed the randomized trial after first completing the FA. Table 2 includes the FA results and background information on the participants.
Table 2.
Characteristics of ASD Children in Randomized Trial of FCT Treatment Via Telehealth
| Immediate FCT Treatment | Delay FCT Treatment | ||
|---|---|---|---|
| Variables | (Experimental Group) | (Control Group) | Significance |
| (n = 21) | (n = 17) | ||
| Age: Mean (SD) in months | 49.71 (16.97) | 55.29 (17.01) | p = 0.321 |
| Range in months | 29 – 83 | 21 - 84 | |
| Gender: Female : Male | 3 F : 18 M | 3 F : 14 M | p = 0.672 |
| Intellectual Disability: n (%) | 13 (62%) | 11 (65%) | p = 0.863 |
| Social Function Identified: n (% of children in group) | |||
| Escape | 13 (62%) | 9 (53%) | p = 0.743 |
| Tangible | 20 (95%) | 15 (88%) | p = 0.577 |
| Attention | 1 (5%) | 2 (12%) | p = 0.577 |
Note. Children often showed more than one social function. Comparisons between treatment groups were based on ANOVA for continuous variables and Chi-Square (or Fisherȧs Exact Test for small cell sizes) for categorical variables
The two treatment groups did not differ significantly on age, gender, presence of ID, or type of function identified during the FA. All participants showed at least one social function, and most had more than one. The most common functions overall were Tangible in 92% of participants and Escape in 58%; the frequency of an Attention function was very low (8%). These FA results are comparable to other studies of young children with ASD, for whom Escape and Tangible functions are the most common (Wacker et al., 2013a). No children in the study had an Attention function without also having at least one other social function.
Primary Behavioral Outcomes
Table 3 shows the mean percentage of 6-sec intervals (per 5-min observation session) during which the child showed problem behavior at baseline and at the end of the randomized trial 12 weeks later. Because all participants in both treatment groups completed the RCT while following the protocol to which they were randomized, the intention-to-treat analysis did not differ from a per protocol analysis.
Table 3.
Behavioral Outcomes for FCT Treatment During Randomized Controlled Trial
| Immediate FCT Treatment | Delay FCT Treatment | ||||
|---|---|---|---|---|---|
| Outcome Variables | (Experimental Group) | (Control Group) | Significance | ||
| (n = 21) | (n = 17) | ||||
| Baseline | 12 Weeks | Baseline | 12 Weeks | ||
| Percentage of Intervals with Problem Behavior in Each 5-Min Session: | |||||
| Mean | 24.81 | 0.35 | 26.75 | 26.70 | F = 23.14 |
| (SD) | (15.44) | (0.75) | (16.30) | (17.33) | p < 0.0001 |
Note. Significance was based on a linear mixed model for repeated measures, with Time (Baseline vs. 12 Weeks) as the within-subjects factor and Treatment Group (Immediate vs. Delay) as the between-subjects factor. The Time x Group interaction was highly significant. However, because the linear mixed model did not meet the assumption of normality, an additional analysis was conducted after transforming the data to a single change score (Baseline minus 12-Week value) for each subject. These change scores met the assumption of normality, and a t-test comparing the mean change scores for each treatment group confirmed the highly significant difference between groups during the RCT (t = 4.83, p < 0.0001).
Children in the Immediate group obtained a mean baseline score of 24.81 (SD = 15.44) and a mean score of 0.35 (SD = 0.75) after 12 weeks of FCT. Children in the Delay group obtained a mean Baseline score of 26.75 (SD = 16.30) and a mean 12-week score of 26.70 (SD = 17.33), indicating minimal overall improvement in behavior as a result of the passage of time or response to existing interventions for these children. A basic way to summarize these results is to note that children in both groups showed problem behavior about 25–27% of the time during baseline sessions, but that FCT treatment reduced problem behavior to less than 1% of the time when measured during observation sessions at the end of the RCT. Simply waiting for behavior to get better over time did not result in improvement for most children.
As expected, the results of the linear mixed model analysis showed a highly significant Time by Group interaction (F = 23.14, p < 0.0001) as the group of children receiving treatment with FCT improved significantly compared to baseline but the control group did not. The Immediate group showed a mean reduction in problem behavior of −24.46 (95% CI: −32.56, −16.36; p < 0.0001), while the Delay (Control) group showed a mean reduction of −0.05 (95% CI: −9.49, 9.40; p > 0.99). Although most of the assumptions of a linear mixed model were met in undertaking this analysis, the assumption of normality was not. As can be seen in Table 3, FCT treatment for the Immediate group not only reduced the mean problem behavior score significantly at 12 weeks, but the variance was also reduced dramatically as a result of uniformly significant reductions in problem behavior for children in that group. Even though linear mixed models tend to be quite robust in the face of violations to assumptions, we conducted an additional analysis after transforming the data to a single “change score” (baseline score minus 12-week score) for each subject. These change scores met the assumption of normality, and a T-test comparing the mean change scores for each treatment group confirmed the highly significant difference between the two groups during the RCT (t = 4.83, p < 0.0001).
Effect Size
The effect size of the RCT results was calculated as the standardized mean difference between the Immediate (experimental) and Delay (control) groups. A change score for each child was calculated as the change in the frequency of behavior problems at baseline compared to the frequency of behavior problems at the end of the 12-week RCT. Specifically, the effect size was calculated as the mean change score of the experimental group (24.46) minus the mean change score of the control group (0.05), which was then divided by the pooled standard deviation for the entire sample (15.51). Thus, the behavior change observed in response to FCT treatment during the randomized trial corresponded to an effect size of 1.57.
Clinical Significance
Although all 21 of the children in the Immediate group showed improved behavior, only two of 17 children in the Delay group improved while waiting to begin treatment. The proportion of children achieving at least an 80% reduction of problem behavior during the RCT was significantly higher in the Immediate treatment group than in the control group (100% vs. 12% respectively; p < 0.0001, two-tailed Fisher’s exact test). The two children in the Delay group who showed improved behavior appeared to respond well to the extinction procedures that were a component of the monthly assessment probes conducted during the waiting period. Because these children responded to extinction (which discontinued reinforcement for problem behavior and constituted “planned ignoring,” as described by Lerman and Iwata, 1996), they did not require initiation of the full FCT treatment package after the waiting period ended.
Manding
Comparisons were also made between treatment groups based on the frequency of manding at the end of the 12-week randomized trial. Manding was coded by observers as a percentage of the opportunities to mand. Children in the Immediate group obtained a mean baseline score of 14.76% (SD = 24.08) and a score of 97.22% (SD = 11.19) after 12 weeks of FCT. Children in the Delay group obtained a mean Baseline score of 16.99% (SD = 32.02) and a 12-week score of 28.25% (SD = 40.10), indicating a non-significant increase in manding as a result of the continuation of existing intervention strategies for the Delay group. There was a highly significant Time by Group interaction (F = 75.12, p < 0.0001) as the group of children receiving FCT treatment showed significantly increased manding compared to baseline but the control group did not. The Immediate group showed a mean increase in manding of 83.10 (95% CI: 70.07, 96.14; p < 0.0001), while the Delay group showed a mean increase of 11.25 (95% CI: −4.34, 26.84; p > 0.99).
Task Completion
Data were also obtained for the percentage of tasks completed by the 15 children in the Immediate group whose FCT treatment program included a task completion component. (These data were not consistently available during the randomized trial for the children in the Delay group because they were not yet receiving FCT.) The mean percentage of tasks completed by children in the Immediate group at baseline was 40.89 (SD = 38.94), which improved to 99.85 (SD = 0.58) after 12 weeks of FCT (t = 5.83, p < 0.0001).
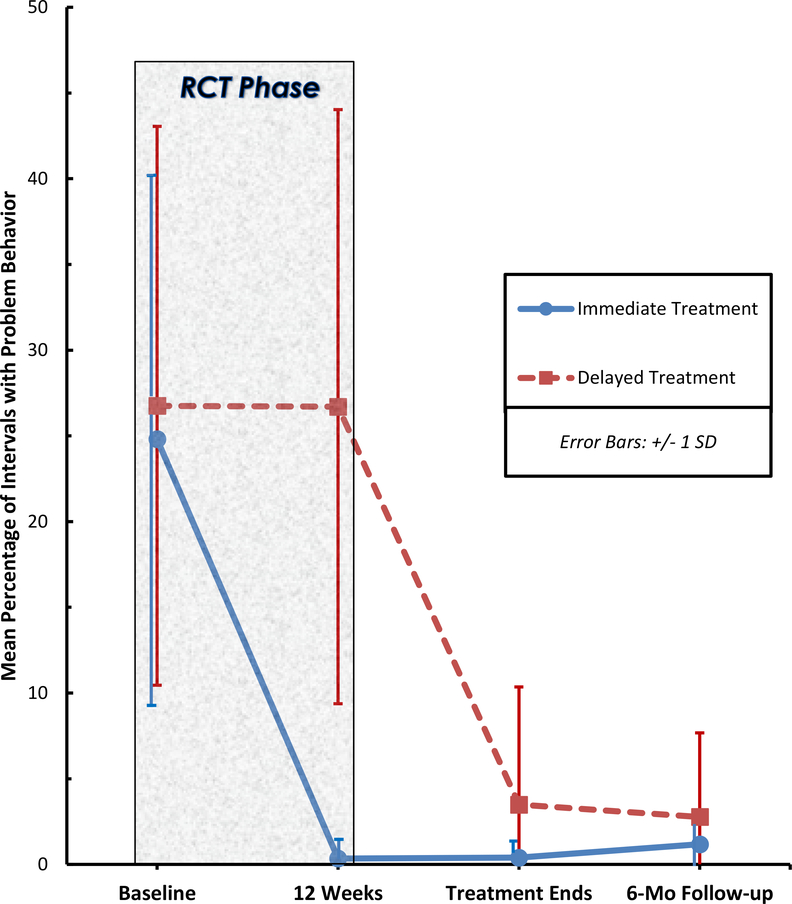
Behavioral Outcomes After Completion of the Randomized Controlled Trial
Figure 2 displays the behavior changes achieved by the children in the two treatment groups, both during and after completion of the RCT phase of the study. (To increase visibility in Figure 2, the SD error bars are offset slightly to the left for the Immediate treatment group whenever the distributions of behavior scores overlap with scores for the Delay group.) For children in the Delay group, treatment with FCT was provided after completion of the randomized trial.
Figure 2.
Randomized controlled trial: Behavioral outcomes
By the end of treatment, the percentage of problem behavior in the Delay group (M = 3.49; SD = 6.87) approached the low levels achieved by the children in the Immediate treatment group after FCT had been completed (M = .40; SD = 0.73). The small between-group difference after treatment was not statistically significant but did approach significance (p = 0.083).
Two of the children in the Delay group who started FCT treatment after the RCT ended did not complete treatment as planned. One of these children moved out of state and did not maintain contact with the study, and the other child showed significant behavior problems that did not respond to social contingencies, could not be managed by the parents at home, and required a referral for out-of-home residential placement. All of the remaining 13 children in the Delay group achieved at least an 80% reduction in problem behavior after completion of FCT treatment. Comparing behavior at baseline to behavior after completion of treatment, the Immediate group showed a mean reduction in problem behavior of 98.48% (SD = 2.99). Although the Delay (Control) group participants showed no average improvement in problem behavior during the initial 12-week waiting period, they were able to achieve a mean reduction in problem behavior of 95.83% (SD = 6.30) after completing FCT treatment. For all children completing treatment, there was not a significant mean difference in behavior change between the Immediate and Delay groups (p = 0.176). The positive outcomes in the Delay group following treatment thus represented a replication of the results obtained in the Immediate group.
Twenty-four of the children who completed FCT treatment were able to be contacted six months later to obtain follow-up data to assess the sustained effects of behavioral treatment. Only small, non-significant increases in problem behavior were detected in the Immediate group at follow-up (M = 1.18; SD = 3.07), and the percentages of problem behavior were only slightly higher in the Delay group (M = 2.77; SD = 4.91), with the difference not being significant (p = 0.338). Overall, occurrences of problem behavior were low in both groups at follow-up.
Parental Acceptance of Behavioral Telehealth Procedures
At the completion of FCT, parents were asked to judge how acceptable the treatment was with regard to their concerns about their child. Using the 7-point rating scale on the primary item from the TARF-R (Reimers et al., 1991), parents were generally positive about the treatment they had received. The mean score reported after FCT for parents in both treatment groups was 6.30 (SD = .95), which indicated a high level of acceptance of the behavioral procedures that had been taught to the parents via telehealth.
DISCUSSION
Summary of Findings
Previous research has demonstrated that parents can be trained and coached live via telehealth to conduct FA and FCT to reduce problem behavior in young children with autism (Lindgren et al., 2016; Wacker et al., 2013b). However, prior FCT studies have not conducted between-group comparisons in which children were randomly assigned to experimental and control groups. The current randomized controlled trial examined treatment group comparisons that supported the three hypotheses established at the initiation of the study: (1) that FCT treatment would decrease problem behavior, (2) that FCT would increase manding and task completion, and (3) that FCT treatment via telehealth would be highly acceptable to parents. Specifically, the trial demonstrated that treatment with FCT via in-home telehealth was able to achieve a mean reduction in problem behavior of 98% compared to no overall improvement in behavior in a group of children who received “treatment as usual” during the trial. The effect size for behavior change was 1.57. Significant increases in the production of mands and the completion of tasks assigned by parents were also observed after FCT. Treatment acceptability was high based on parent ratings, with results comparable to studies using in-home therapists (Lindgren et al., 2016; Wacker et al., 1998), and discontinuation of treatment by families was infrequent. This research demonstrates that parents can successfully use FA+FCT to treat moderate to severe behavior problems displayed by their child with ASD and can do so even when all parent coaching, behavioral assessment, and treatment procedures are conducted via real-time telehealth.
Randomized Controlled Trials vs. Single-Case Designs
Research using single-subject designs has established FCT as the most commonly delivered behavioral treatment for severe problem behavior emitted by children with autism (Tiger et al., 2008), but the absence of randomized controlled trials of FCT is notable. Although the group designs used in RCTs are often considered the “gold standard” in establishing causal relationships between interventions and outcomes, single-case designs have focused on evaluating the effects of interventions for individual subjects and maintaining strong internal validity in behavioral research (Byiers, Reichle, & Symons, 2012; Kazdin, 2010; Smith, 2012). For behavior analysts, single-case research has long been considered to offer significant clinical advantages over group designs because treatment strategies can be modified in real-time based on each subject’s response to treatment. By using single-case methods to enhance internal validity, combined with a randomized group design that enhances external validity, the current study is a hybrid design that possesses unique strengths and minimizes threats to validity. The study provides strong evidence for the positive behavioral effects of FA+FCT in young children with ASD, as well as highlighting the practical advantages of delivering FCT via telehealth. The relatively limited use of RCTs by behavior analysts in past studies of ASD interventions is gradually changing, at least partially in response to the priority given to RCTs by funders of intervention programs and insurers reimbursing for clinical care (Smith, 2012). The results of the current RCT should help solidify the status of FA+FCT as an established treatment methodology for problem behaviors in children with ASD.
RCTs of Behavioral Telehealth for ASD
In the area of telehealth services for children with autism, only one randomized trial of any kind was reported in the literature reviewed by Knutsen et al. (2016), and that trial (Ruble, McGrew, Toland, Dalrymple, & Jung, 2013) evaluated an intervention focused on teacher training rather than FCT. A later review of parent-mediated intervention training delivered remotely for children with ASD (Parsons, Cordier, Vaz, & Lee, 2017) identified only one RCT that included both parents and children as participants; that study compared delivery of Project ImPACT by parents who were self-directed versus those who received therapist assistance (Ingersoll, Wainer, Berger, Pickard, & Bonter, 2016). At present, the current study is not only the first randomized controlled trial of FCT to be reported, but it is also the first randomized FCT trial conducted entirely via telehealth.
Real-Life Impact
To provide a practical perspective on the impact of the behavior changes obtained through FCT treatment in the current study, the outcomes achieved can be considered within the context of approximately 13 hours of waking time each day for a typical child with ASD in this age range (Humphreys et al., 2014). If the mean rate of problem behavior observed before treatment (approximately 26%) is extrapolated to a full day, the average participating child would be expected to show more than three hours per day of problem behavior. However, if treatment with FCT produces reductions in targeted problem behavior that are comparable to those obtained in the current study, a child’s problem behavior could be reduced to an average of less than three minutes per day. This potential for significant reductions in problem behavior could make it easier for children with ASD to benefit from the range of educational and health care services they often require. In addition, improvements in making communicative requests and completing tasks were important outcomes achieved in the study, and growth in these skills could have a highly positive impact on performance in therapeutic activities and skill-acquisition programs.
Potential Limitations
There are several potential limitations that must be recognized when considering the findings of this study. The study sample size was modest, although the very high rate of treatment success and the low rate of behavioral improvement without treatment made the results of the RCT clearly significant, both statistically and clinically. Because the parents and behavioral consultants knew when they were engaged in FCT treatment, they could not be completely blinded to group assignment. However, behavioral outcomes were assessed using direct observation data that were coded by independent observers and checked for reliability rather than relying on subjective rating scales or global clinical impressions by clinicians or parents to assess treatment progress. Although questions could be raised regarding the use of parents as behavior therapists with their own children, the findings reported by Suess et al. (2014) demonstrated that parents can conduct FCT procedures with reasonable fidelity even without constant coaching from a behavior analyst. The decision to use weekly FCT coaching sessions in our study can also be questioned, given that more frequent sessions might be able to produce positive outcomes more quickly. However, even with only weekly sessions, parents are coached to use FCT strategies throughout the week, which should increase treatment intensity significantly. This issue has been explored through other research that supports the positive effects of one hour per week of therapy for children with ASD (Vismara, Colombi, & Rogers, 2009).
The study included children with significant behavior problems as identified by parents and clinicians, but a fixed cut-off score on a rating scale or global measure of behavior was not used to define severity or determine inclusion in the study. Behavioral targets for intervention were established based on each parent’s identification of the primary behavior problems encountered at home as well as consideration of the behaviors observed during the FA. Individualizing behavioral targets increased ecologic validity but also meant that the specific targets were not identical for all participants. Although the use of direct observation of behavior minimized potential bias from parental report on behavior rating scales, the use of broad-band behavior scales such as the Home Situations Questionnaire – ASD (Chowdhury et al., 2016) or subscales of the Aberrant Behavior Checklist (Aman et al., 2009) could be important in identifying and tracking problem behaviors in settings and situations that were not specific targets of FCT treatment.
Because we were not able to obtain follow-up data at 6 months post-treatment for all families, we could not be certain that families without long-term follow-up had the same level of positive behavioral outcomes as other families. We did not compare behavioral interventions to treatment with psychoactive medication although treatment was successful for nearly all children regardless of whether or not they were receiving medication during the study period. Intellectual abilities of children in the study ranged from severe ID to above average ability, and no children were excluded based on limited vocal communication or level of IQ. FA+FCT treatment was successful across all IQ ranges for the young children who participated in the study.
Recommendations for Future Research
There is an expanding literature on telehealth service delivery for ASD interventions (Heitzman-Powell, Buzhardt, Rusinko, & Miller, 2013; Knutsen et al., 2016; Machalicek et al., 2016, 2010; Vismara, Young, & Rogers, 2012; Vismara, Young, Stahmer, Griffith, & Rogers, 2009; Wainer & Ingersoll, 2015), and future research on ABA telehealth will need to determine when to provide treatment and at what level of intensity. These timing and dose issues, as discussed by Lindgren et al. (2016), warrant careful study, as will issues such as the interaction of ABA treatment with other therapies, effects on family stress, prevention of the resurgence of problem behavior when a child’s appropriate requests are ignored, and the development of strategies to ensure treatment generalization across home and community settings. An ongoing multi-state collaborative study is currently comparing treatment outcomes of a standard FA+FCT package to a more streamlined, “pragmatic” version of the same intervention to try to identify an even more cost-effective way to deliver ABA treatment to families via telehealth (Lindgren and Wacker, 2015).
In addition to research that refines FA+FCT treatment methodology and increases access to ABA-based treatment packages through telehealth, it is important to continue to develop a range of other parent-mediated strategies for improving behavior in young children with ASD. These efforts will give families choices in the types of intervention provided so that treatment can be matched to the specific needs of both parents and children. For example, RCTs have been completed for Parent-Child Interaction Therapy (Ginn, Clionsky, & Eyberg, 2017), Project ImPACT (Ingersoll et al., 2016), Pivotal Response Treatment (Gengoux et al., 2019), and other structured forms of “parent training” (Bearss et al., 2015). All of these treatment approaches have produced positive behavioral effects for children with ASD, although the results differ in terms of the types of behavior change and the extent of that change. Systematic reviews and meta-analyses have summarized several of these studies and have also identified other research that supports the validity and importance of parent-implemented ASD interventions to reduce problem behavior (Postorino et al., 2017; Tarver et al., 2019). Several of these interventions have even shown promise for remote delivery via telehealth (Bearss et al., 2018; Wainer & Ingersoll, 2015). Future studies that combine broad-based parent training with FA+FCT may be able to achieve both targeted behavior change through FCT and broader generalization of treatment effects to a wider range of environments.
The traditional, conservative recommendation following a successful randomized trial of modest size is to suggest the need to complete a similar but larger trial in real-world settings and across multiple sites. In view of the current results, this recommendation must be weighed against the fact that large behavioral trials are extremely costly and there is already a large body of high-quality single-subject research supporting the use of FA and FCT with children with ASD and other developmental disabilities. Given the acceptance of FA+FCT as a “best practice” for treating severe problem behavior (Reichle & Wacker, 2017; Tiger et al., 2008) and the existing evidence for the feasibility and cost-effectiveness of completing FA+FCT via telehealth (Lindgren et al., 2016), our recommendation would be to move quickly to implement ABA telehealth strategies clinically while at the same time carefully initiating controlled trials to test the best procedures for achieving optimal behavioral outcomes at reasonable cost. We would urge caution about designing future studies that compare an “active” behavioral intervention against “treatment as usual.” Instead, we would recommend that all families receive a potentially useful intervention from the start of the study, which should optimize family engagement and acceptance of the treatments provided. Although many conceptual and practical research questions remain, the positive results of the current randomized trial should strengthen efforts to provide research-based behavioral treatment to young children with ASD.
Acknowledgements
This research was supported by grant R40 MC22644 from the Maternal and Child Health Bureau of the Health Resources and Services Administration and by grant R01 MH104363 from the National Institute of Mental Health of the National Institutes of Health. The authors have no other financial relationships or conflicts of interest related to this research to disclose.
We are grateful for the important contributions provided by the research assistants who helped to ensure successful completion of the study. We greatly appreciate the biostatistical consultation provided by Bridget Zimmerman, who designed the randomization process and assisted with the data analysis. We owe a special debt of gratitude to the families who opened their homes and lives to us.
Footnotes
Conflict of Interest: The authors declare they have no conflict of interest. (Complete information regarding grant funding from the U.S. Health Resources and Services Administration and the National Institute of Mental Health is included in a separate section of this submission.)
Compliance with Ethical Standards
Ethical Approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent: Informed consent was obtained from all individual participants included in the study.
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
REFERENCES
- Ahearn WH & Tiger JH (2013). Behavioral approaches to the treatment of autism In Madden G (Editor), APA Handbook of Behavior Analysis. Volume 2: Translating Principles into Practice, American Psychological Association, Washington D.C., pp 301–327. [Google Scholar]
- Aman MG, Mcdougle CJ, Scahill L, Handen B, Arnold LE, Johnson C, …Wagner A (2009). Medication and parent training in children with pervasive developmental disorders and serious behavior problems: Results from a randomized clinical trial. Journal of the American Academy of Child and Adolescent Psychiatry, 48(12), 1143–1154. doi: 10.1097/CHI.0b013e3181bfd669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. (1994). Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington, DC: American Psychiatric Association. [Google Scholar]
- American Psychiatric Association. (2014). Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington, DC: American Psychiatric Association. [Google Scholar]
- Bearss K, Burrell TL, Challa SA, Postorino V, Gillespie SE, Crooks C, & Scahill L (2018). Feasibility of parent training via telehealth for children with autism spectrum disorder and disruptive behavior: A demonstration pilot. Journal of Autism and Developmental Disorders, 48, 1020–1030. doi: 10.1007/s10803-017-3363-2. [DOI] [PubMed] [Google Scholar]
- Bearss K, Johnson C, Smith T, Lecavalier L, Swiezy N, Aman M, …Scahill L (2015). Effect of parent training vs parent education on behavioral problems in children with autism spectrum disorder; A randomized clinical trial. JAMA, 313(15), 1524–1533. doi: 10.1001/jama.2015.3150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byiers BJ, Reichle J, & Symons FJ (2012). Single-subject experimental design for evidence-based practice. American Journal of Speech-Language Pathology, 21(4), 397–414. doi: 10.1044/10580360(2012/11-0036). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carr EG (1988). Functional equivalence as a mechanism of response generalization In Horner R, Koegel R, & Dunlap G, (Eds.), Generalization and Maintenance: Lifestyle Changes in Applied Settings. Baltimore, MD: Paul H. Brookes. [Google Scholar]
- Carr EG, & Durand VM (1985). Reducing behavior problems through functional communication training. Journal of Applied Behavior Analysis, 18, 111–126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chowdhury M, Aman MG, Lecavalier L, Smith T, Johnson C, Swiezy N, … Scahill L (2016). Factor structure and psychometric properties of the revised Home Situations Questionnaire for autism spectrum disorder. Autism, 20(5), 528–537. doi: 10.1177/1362361315593941. [DOI] [PubMed] [Google Scholar]
- Dawson G, Rogers S, Munson J, Smith M, Winter J, Greenson J, …Varley J (2010). Randomized, controlled trial of an intervention for toddlers with autism: The Early Start Denver Model. Pediatrics, 125(1), e17–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durand VM, & Carr EG (1985). Self-injurious behavior: Motivating conditions and guidelines for treatment. School Psychology Review, 14, 171–176. [Google Scholar]
- Fuhrman AM, Fisher WW, & Greer BD (2016). A preliminary investigation on improving functional communication training by mitigating resurgence of destructive behavior. Journal of Applied Behavior Analysis, 49, 884–899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ginn NC, Clionsky LN, Eyberg SM (2017). Child-directed interaction training for young children with autism spectrum disorders: Parent and child outcomes. Journal of Clinical Child and Adolescent Psychology, 46(1), 101–109. doi: 10.1080/15374416.2015.1015135. [DOI] [PubMed] [Google Scholar]
- Gengoux GW, Abrams DA, Schuck R, Millan ME, Libove R, Ardel CM, … Hardan AY (2019). A pivotal response treatment package for children with autism spectrum disorder: An RCT. Pediatrics, 144(3), e20190178. doi: 10.1542/peds.2019-0178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harding JW, Wacker DP, Berg WK, Lee JF, & Dolezal D (2009). Conducting functional communication training in home settings: A case study and recommendations for practitioners. Behavior Analysis in Practice, 2, 21–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heitzman-Powell LS, Buzhardt J, Rusinko L, & Miller T (2013). Formative evaluation of an ABA outreach program for parents of children with autism in remote areas. Focus on Autism and Other Developmental Disabilities, 20, 1–16. [Google Scholar]
- Horner RH, Carr EG, Strain PS, Todd AW, & Reed HK (2002). Problem behavior interventions for young children with autism: A research synthesis. Journal of Autism and Developmental Disorders, 32(5), 423–446. [DOI] [PubMed] [Google Scholar]
- Humphreys JS, Gringras P, Blair PS, Scott N, Henderson J, Fleming PJ, & Emond AM (2014). Sleep patterns in children with autistic spectrum disorders: A prospective cohort study. Archives of Disease in Childhood, 99(2), 114–118. doi: 10.1136/archdischild2013-304083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ingersoll B, Wainer AL, Berger NI, Pickard KE, & Bonter N (2016). Comparison of a self-directed and therapist-assisted telehealth parent-mediated intervention for children with ASD: A pilot RCT. Journal of Autism and Developmental Disorders, 46(7), 2275–2284. doi: 10.1007/s10803-016-2755-z. [DOI] [PubMed] [Google Scholar]
- Iwata BA, Dorsey MF, Slifer KJ, Bauman KE, & Richman GS (1994). Toward a functional analysis of self-injury. Journal of Applied Behavior Analysis, 27, 197–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kazdin AE (2010). Single-case research designs: Methods for clinical and applied settings. 2nd ed. New York, NY: Oxford University Press. [Google Scholar]
- Knutsen J, Wolfe A, Burke BL, Hepburn S, Lindgren S, & Coury D (2016). A systematic review of telemedicine in autism spectrum disorders. Review Journal of Autism and Developmental Disorders, 3(4), 330–344. doi: 10.1007/s40489-016-0086-9. [DOI] [Google Scholar]
- Koegel RL, & Koegel LK (1988). Generalized responsivity and pivotal behavior In Horner R, Koegel R, & Dunlap G (Eds), Generalization and Maintenance: Lifestyle Changes in Applied Settings. Baltimore, MD: Paul H. Brookes. [Google Scholar]
- Lerman DC, & Iwata BA (1996). Developing a technology for the use of operant extinction in clinic settings: An examination of basic and applied research. Journal of Applied Behavior Analysis, 29, 345–382. doi: 10.1901/jaba.1996.29-345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindgren S, & Wacker D (2015) Comparing behavioral assessments using telehealth for children with autism. U.S. Department of Health and Human Services, National Institutes of Health, National Institute of Mental Health. Grant R01MH104363.
- Lindgren S, Wacker D, Suess A, Schieltz K, Pelzel K, Kopelman T, …Waldron D (2016). Telehealth and autism: Treating challenging behavior at lower cost. Pediatrics, 137(S2), S167–S175: e201528510. doi: 10.1542/peds.2015-28510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lord C, Rutter M, DiLavore PC, & Risi S (1999). Autism Diagnostic Observation Schedule (ADOS). Los Angeles, CA: Western Psychological Services. [Google Scholar]
- Lovaas OI (1987). Behavioral treatment and normal educational and intellectual functioning in young autistic children. Journal of Consulting and Clinical Psychology, 55: 3–9. [DOI] [PubMed] [Google Scholar]
- Machalicek W, Lequia J, Pinkelman S, Knowles C, Raulston T, Davis T, & Alresheed F (2016). Behavioral telehealth consultation with families of children with autism spectrum disorder. Behavioral Interventions, 31, 223–250. doi: 10.1002/bin.1450. [DOI] [Google Scholar]
- Machalicek W, O’Reilly MF, Rispoli M, Davis T, Lang R, Hetlinger Franco J, & Chan JM (2010). Training teachers to assess the challenging behaviors of students with autism using video tele-conferencing. Education and Training in Autism and Developmental Disabilities, 45, 203–215. [Google Scholar]
- Mullen E (1995). Mullen Scales of Early Learning. Bloomington, MN: Pearson Assessments. [Google Scholar]
- Parsons D, Cordier R, Vaz S, & Lee HC (2017). Parent-mediated intervention training delivered remotely for children with autism spectrum disorder living outside of urban areas: Systematic review. Journal of Medical Internet Research, 19 (8), e198. doi: 10.2196/jmir.6651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Postorino V, Sharp WG, McCracken CE, Bearss K, Burrell TL, Evans AN, & Scahill L (2017). A systematic review and meta-analysis of parent training for disruptive behavior in children with autism spectrum disorder. Clinical Child and Family Psychology Review, 20, 391–402. doi: 10.1007/s10567-017-0237-2. [DOI] [PubMed] [Google Scholar]
- Reichle J, & Wacker D (2017). Functional communication training for problem behavior. New York: Guilford Press. [Google Scholar]
- Reimers T, Wacker D, & Cooper L (1991). Evaluation of the acceptability of treatments for children’s behavioral difficulties: Ratings by parents receiving services in an outpatient clinic. Child & Family Behavior Therapy,13, 53–71. [Google Scholar]
- Roane H, Vollmer T, Ringdahl J, & Marcus B (1998). Evaluation of a brief stimulus preference assessment. Journal of Applied Behavior Analysis, 31, 605–620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruble LA, McGrew JH, Toland MD, Dalrymple NJ, & Jung LA (2013). A randomized controlled trial of COMPASS web-based and face-to-face teacher coaching in autism. Journal of Consulting and Clinical Psychology, 81(3), 566–572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rutter M, Le Couteur A, Lord C (2003). Autism Diagnostic Interview-Revised (ADI-R). Los Angeles, CA: Western Psychological Services. [Google Scholar]
- Schulz KF, Altman DG, Moher D, & CONSORT Group. (2010). CONSORT 2010 statement: Updated guidelines for reporting parallel group randomised trials. British Medical Journal, 340, c332. doi: 10.1136/bmj.c332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith T (2012). Evolution of research on interventions for individuals with autism spectrum disorder: Implications for behavior analysts. The Behavior Analyst, 35(1), 101–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soke GN, Rosenberg SA, Hamman RF, Fingerlin T, Robinson C, Carpenter L, …DiGuiseppi C (2016). Journal of Autism and Developmental Disorders, 46(11), 3607–3614. doi: 10.1007/s10803-016-2879-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sparrow SS, Cicchetti DV, & Ballo DA (2005). Vineland Adaptive Behavior Scales – Second Edition (Vineland-II). Bloomington, MN: Pearson Assessments. [Google Scholar]
- Suess AN, Romani PW, Wacker DP, Dyson SM, Kuhle JL, Lee JF, …Waldron DB (2014). Evaluating the treatment fidelity of parents who conduct in-home functional communication training with coaching via telehealth. Journal of Behavioral Education, 23(1), 34–59. [Google Scholar]
- Tarver J, Palmer M, Webb S, Scott S, Slonims V, Simonoff E, & Charman T (2019). Child and parent outcomes following parent interventions for child emotional and behavioral problems in autism spectrum disorders: A systematic review and meta-analysis. Autism, 23(7), 1630–1644. doi: 10.1177/1362361319830042. [DOI] [PubMed] [Google Scholar]
- Tiger JH, Hanley GP, & Bruzek J (2008). Functional communication training: A review and practical guide. Behavior Analysis in Practice, 1, 16–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vismara LA, Colombi C, & Rogers SJ (2009). Can one hour per week of therapy lead to lasting changes in young children with autism? Autism, 13, 93–115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vismara LA, Young GS, & Rogers SJ (2012). Telehealth for expanding the reach of early autism training to parents. Autism Research and Treatment, 2012, 121878. doi: 10.1155/2012/121878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vismara LA, Young G, Stahmer A, Griffith E, & Rogers S (2009). Dissemination of evidence-based practice: Can we train therapists from a distance? Journal of Autism and Developmental Disorders, 39(12), 1636–1651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wacker DP, Berg WK, Harding JW, Derby KM, Asmus JM, & Healy A (1998). Evaluation and long-term treatment of aberrant behavior displayed by young children with disabilities. Journal of Developmental and Behavioral Pediatrics, 19, 260–266. [DOI] [PubMed] [Google Scholar]
- Wacker DP, Harding JW, & Berg WK, (2011). An evaluation of persistence of treatment effects during long-term treatment of destructive behavior. Journal of the Experimental Analysis of Behavior, 96, 261–282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wacker DP, Lee JF, Padilla Dalmau YC, Kopelman TG, Lindgren SD, Kuhle J, …Waldron DB (2013a). Conducting functional analyses of problem behavior via telehealth. Journal of Applied Behavior Analysis, 46, 31–46. doi: 10.1002/jaba.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wacker DP, Lee JF, Padilla Dalmau YC, Kopelman TG, Lindgren SD, Kuhle J, …Waldron DB (2013b). Conducting functional communication training via telehealth to reduce the problem behavior of young children with autism. Journal of Developmental and Physical Disabilities, 25(1), 35–48. doi: 10.1007/s10882-012-9314-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wainer AL, & Ingersoll BR (2015). Increasing access to an ASD imitation intervention via a telehealth parent training program. Journal of Autism and Developmental Disorders, 45(12), 3877–90. doi: 10.1007/s10803-014-2186-7. [DOI] [PubMed] [Google Scholar]
- Wong C, Odom SL, Hume KA, Cox AW, Fettig A, & Kucharczyk S, … Schultz TR (2015). Evidence-based practices for children, youth, and young adults with autism spectrum disorder: A comprehensive review. Journal of Autism and Developmental Disorders, 45(7), 1951–66. doi: 10.1007/s10803-014-2351-z. [DOI] [PubMed] [Google Scholar]