Abstract
Background
Specialty wards cohort hospitalised patients to improve outcomes and lower costs. When demand exceeds capacity, patients overflow and are “bedspaced” to alternate wards. Some studies have demonstrated that bedspacing among medicine service patients is associated with adverse patient-centred outcomes, however, results have been inconsistent and have primarily been performed within national health systems. The objective of this study was to assess the association of bedspacing with patient-centred outcomes among United States patients admitted to general medicine services.
Methods
We performed a retrospective cohort study of internal medicine, family medicine and geriatric service patients who were bedspaced vs cohorted for the entirety of their hospital stay within three large, urban United States hospitals (quaternary referral centre, tertiary referral centre and community hospital, with different patient demographics and case-mixes) in 2014 and 2015. We performed quantile regression to determine differences in length of stay (LOS) between bedspaced vs cohorted patients and logistic regression for in-hospital mortality and discharge to home.
Results
Among 18 802 patients in 33 wards, 6119 (33%) patients were bedspaced. Bedspaced patients had significantly longer LOS compared with cohorted patients at the 25th (0.1 days, 95% CI: 0.05 to 0.2, p=0.001), 50th (0.2 days, 95% CI: 0.1 to 0.3, p=0.003) and 75th (0.3 days, 95% CI: 0.2 to 0.5, p<0.001) percentiles; and no statistically significant differences in odds of mortality (OR=0.9, 95% CI: 0.6 to 1.3, p=0.5) or discharge to home (OR=0.9, 95% CI: 0.9 to 1.0, p=0.06) in adjusted analyses.
Conclusion
Bedspacing is associated with adverse patient-centred outcomes. Future work is needed to confirm these findings, understand mechanisms contributing to adverse outcomes and identify factors that mitigate these adverse effects in order to provide high-value, patient-centred care to hospitalised patients.
INTRODUCTION
Specialty wards (eg, internal medicine) geographically cohort (ie, centralise) hospitalised patients to improve outcomes and lower costs.1–3 When demand exceeds capacity, patients overflow and are “bedspaced” to alternate wards rather than being “cohorted”. Bedspacing has been shown to be associated with worse outcomes among several patient populations. For example, critically ill patients who “board” in emergency departments (EDs) awaiting intensive care unit (ICU) beds or are bedspaced to alternate ICUs (eg, a medical patient admitted to a surgical ICU), may experience worse clinical outcomes (eg, prolonged hospital length of stay [LOS] and increased ICU and in-hospital mortality) and care inefficiencies.4–7
Bedspaced ward patients, similar to ICU patients, may be cared for by the physicians from the home specialty ward and the nurses, therapists and case managers from the bedspaced ward. This asynchronous care team may experience lapses in communication from unfamiliarity and physical separation and the bedspaced ward staff may lack the expertise and experience required to best care for the bedspaced patients, leading to adverse patient-centred outcomes.8–10
Several studies have demonstrated that bedspacing among medicine service patients is associated with adverse patient-centred outcomes including prolonged LOS, clinical emergencies, in-hospital mortality and hospital readmissions, however, results have been inconsistent and these studies have primarily been performed outside of the United States (US) within national health systems.1–3,11–13 Therefore, our objective was to assess the association of bedspacing with patient-centred outcomes among a large population of US patients admitted to general medicine services in three diverse hospitals (ie, quaternary referral centre, tertiary referral centre and community hospital, with different patient demographics and case-mixes). We hypothesised that bedspacing would be associated with prolonged hospital LOS.
METHODS
Study design, participants and setting
We performed a retrospective cohort study of general medicine service patients. We included internal medicine, family medicine and geriatric patients who were bedspaced or cohorted for the entirety of their hospital stay within three large, urban US hospitals in 2014 and 2015 (ie, patients who switched from bedspaced to cohorted wards or vice-versa were excluded from the analysis [n=224, 1%]). We selected a heterogeneous population for our study as we were interested in general medicine services globally as our target population. We opted to include and leverage this heterogeneity in order to make the study and therefore the findings, more generalisable rather than focusing on one specific population within one hospital, as health systems are frequently assessing the overall picture when changing clinical operations. In a secondary analysis we stratified the analyses by hospital in order to assess the effects of this heterogeneity.
At the quaternary centre, all patients were admitted to internal medicine services. At the tertiary centre, approximately two-thirds of patients were admitted to internal medicine services, one-quarter to the geriatrics service and the remainder to the family medicine service during the study period. Patients are admitted to the geriatrics or family medicine services if they have geriatrics or family medicine primary care clinicians in the health system, respectively. All other patients are admitted to internal medicine services. At the community hospital, more than 98% of patients were admitted to internal medicine services (the remainder to the family medicine service) during the study period.
Data source
We included data obtained from electronic health records, extracted through the University of Pennsylvania Health System’s clinical data warehouse.
Study variables
The primary exposure was bedspacing, that is, when patients should reside on specialty wards (ie, internal medicine, family medicine and geriatrics wards) but instead overflow to alternate wards in the setting of bed constraints.
The primary outcome was hospital LOS, defined as admission date/time to discharge date/time. Secondary outcomes included in-hospital mortality and discharge to home (compared with discharge to any other location) among hospital survivors.
For all analyses, we included hospital fixed effects to account for hospital-specific factors. Covariates for multivariable model adjustment were developed based on existing literature1–3,10 and included age, gender, race, ethnicity, insurance type, Elixhauser comorbidity scores, any time spent in an ICU, the Centers for Medicare and Medicaid Services (CMS) four-level severity risk adjustment (based on admitting diagnosis, demographics and comorbidities),14,15 admission diagnosis category (from International Classification of Disease-9 [ICD-9] and ICD-10 codes), daily mean number of medicine service patients by hospital during the hospitalisation, hospital admission source, season and if a hospital admission occurred during a weekend (table 1).
Table 1.
Patient and hospital characteristics and unadjusted outcomes*
| Variable | Total n=18 802 | Cohorted† n=12 683 (67%) | Bedspaced‡ n=6119 (33%) |
|---|---|---|---|
| Patient characteristics | |||
| Hospital | |||
| 1 | 6723 (36) | 5114 (40) | 1609 (26) |
| 2 | 6293 (34) | 4092 (32) | 2201 (36) |
| 3 | 5786 (31) | 3477 (27) | 2309 (38) |
| Age, median (IQR) | 60 (45–74) | 60 (45–74) | 60 (46–73) |
| Female | 10 248 (55) | 6924 (55) | 3324 (54) |
| Race | |||
| Black | 11 428 (61) | 7782 (61) | 3646 (60) |
| White | 6411 (34) | 4247 (34) | 2164 (35) |
| Other§ | 963 (5) | 654 (5) | 309 (5) |
| Latinx | 621 (3) | 380 (3) | 241 (4) |
| Insurance | |||
| Private | 7792 (41) | 5258 (42) | 2534 (41) |
| Medicare | 7772 (41) | 5328 (42) | 2444 (40) |
| Medicaid | 1798 (10) | 1179 (9) | 619 (10) |
| Other¶ | 1440 (8) | 358 (3) | 209 (3) |
| Elixhauser comorbidity score, median (IQR) | 3 (2–5) | 3 (2–5) | 3 (2–5) |
| Any time spent in an intensive care unit | 386 (2) | 274 (2) | 112 (2) |
| Centers for Medicare and Medicaid Services severity risk adjustment | |||
| Mild | 2709 (14) | 1773 (14) | 936 (15) |
| Moderate | 6895 (37) | 4714 (37) | 2181 (36) |
| Major | 7291 (39) | 4989 (39) | 2302 (38) |
| Severe | 1907 (10) | 1207 (10) | 700 (11) |
| Admission diagnosis category | |||
| Symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified | 6473 (34) | 4414 (35) | 2059 (34) |
| Diseases of the circulatory system | 1802 (10) | 1185 (9) | 617 (10) |
| Diseases of the digestive system | 1695 (9) | 1138 (9) | 557 (9) |
| Diseases of the respiratory system | 1447 (8) | 985 (8) | 462 (8) |
| Diseases of the genitourinary system | 1216 (7) | 803 (6) | 413 (7) |
| Endocrine, nutritional and metabolic diseases | 1104 (6) | 771 (6) | 333 (5) |
| Infectious diseases | 993 (5) | 654 (5) | 339 (6) |
| Other** | 4072 (22) | 2733 (22) | 1339 (22) |
| Daily mean number of medicine service patients by hospital over the index patient’s hospitalisation, median (IQR) | 72 (62–81) | 72 (62–81) | 73 (63–82) |
| Hospital admission source | |||
| Emergency department | 18 292 (97) | 12 379 (98) | 5913 (97) |
| Another acute care hospital | 433 (2) | 268 (2) | 165 (3) |
| Direct | 77 (0.4) | 36 (0.3) | 41 (0.7) |
| Season | |||
| Winter | 4444 (24) | 2935 (23) | 1509 (25) |
| Spring | 5586 (30) | 3700 (29) | 1886 (31) |
| Summer | 5542 (29) | 3646 (29) | 1896 (31) |
| Fall | 3230 (17) | 2402 (19) | 828 (14) |
| Weekend hospital admission | 4586 (24) | 2994 (24) | 1592 (26) |
| Outcomes | |||
| Hospital length of stay (days), median (IQR) | 4 (2–6) | 4 (2–6) | 4 (2–7) |
| In-hospital mortality | 123 (1) | 86 (1) | 37 (1) |
| Discharge to home among survivors | n=18 679 14 467 (78) |
n=12 597 9818 (78) |
n=6082 4649 (76) |
All values presented as n (%) except where otherwise specified.
Cohorted: patients who resided on appropriate specialty wards (ie, internal medicine, family medicine and geriatrics wards).
Bedspaced: patients who overflowed to alternate wards rather than residing on appropriate specialty wards (ie, internal medicine, family medicine and geriatrics wards) in the setting of bed constraints.
Other includes: Asian, American Indian/Alaskan Native, Pacific Islander, mixed, unknown, other.
Other includes: workman’s compensation, self-pay, charity, enrolled in a study, hospice, veteran’s association, missing.
Other includes: neoplasms; diseases of the blood and blood-forming organs and certain disorders involving the immune mechanism; mental, behavioural and neurodevelopmental disorders; diseases of the nervous system; pregnancy, childbirth and the puerperium; diseases of the skin and subcutaneous tissue; diseases of the musculoskeletal system and connective tissue; congenital malformations, deformations and chromosomal abnormalities; injury, poisoning and certain other consequences of external causes; factors influencing health status and contact with health services; external causes of morbidity; multiple diagnoses. Each of these diagnoses represented <5% of the overall population and was derived from International Classification of Disease-9 (ICD-9) and ICD-10 codes.
Analyses
We first performed unadjusted analyses of bedspacing with each outcome separately. We then estimated separate multivariable regression models, adjusting for the covariates outlined above.
For our primary analysis, we performed quantile regression to determine differences in LOS between bedspaced and cohorted patients and logistic regression for in-hospital mortality and discharge to home. We used quantile regression as our primary analysis given very low rates of mortality that were equally distributed across the bedspaced and cohorted groups. Additionally, quantile regression allows for ease of interpretation by assessing LOS across the distribution of the population.
We performed a sensitivity analysis for our primary outcome using a Fine and Grey model treating death as a competing risk to estimate LOS,16 estimating a subdistribution hazard ratio (SHR) for the risk of being discharged alive (ie, a proxy for LOS as a continuous variable).
In a second sensitivity analysis, we repeated the primary analyses, excluding patients whose LOS were less than 2 days, as short stay patients may not have the opportunity to benefit from cohorting (ie, be harmed by bedspacing).
In a secondary analysis, we examined outcomes stratified by hospital in order to assess the effects of the heterogeneity of the population. In a post-hoc sensitivity analysis, we excluded patients with LOS less than 2 days and repeated the preceding analyses given the differences in outcomes between hospitals.
We performed all analyses using Stata version 16 (StataCorp LP, College Station, TX). The University of Pennsylvania Institutional Review Board approved this protocol as exempt (protocol #823944).
RESULTS
Demographics
Among 18 802 patients in 33 wards, 6119 (33%) patients were bedspaced, ranging from 24% in hospital 1 (the quaternary referral centre) to 40% in hospital 3 (the tertiary referral centre). The median age was 60 years (IQR 45–74), 10 248 (55%) patients were female and 11 428 (61%) patients were black. Most patients had private insurance (7,792 [41%]) or Medicare (7,772 [41%]) and were in the moderate (6,895 [37%]) or major (7,291 [39%]) CMS severity risk adjustment categories. The vast majority of patients (18,292 [97%]) were admitted to the hospital from the ED. Few patients (386 [2%]) spent parts of their hospitalisation in an ICU (table 1).
The median LOS was 4 days (IQR 2–6) overall, 4 days (IQR 2–6) among cohorted patients and 4 days (IQR 2–7) among bedspaced patients. 123 (1%) patients experienced in-hospital mortality, with 86 (1%) in the cohorted group and 37 (1%) in the bedspaced group. 14 467 (78%) patients were discharged to home, with 9818 (78%) in the cohorted group and 4649 (76%) in the bedspaced group.
Primary analyses
Bedspaced patients had significantly longer LOS compared with cohorted patients at the 25th, 50th and 75th percentiles in both unadjusted and adjusted models, up to 0.3 days (ie, 7 hours) (95% CI: 0.2–0.5, p<0.001) longer at the 75th percentile in the adjusted model (figure 1). Bedspaced patients had no difference in mortality compared with cohorted patients (unadjusted: OR=0.9, 95% CI: 0.6 to 1.4, p=0.8; adjusted: OR=0.9, 95% CI: 0.6 to 1.3, p=0.5). Bedspaced patients had lower odds of discharge to home compared with cohorted patients, but this did not reach statistical significance (unadjusted: OR=0.9, 95% CI: 0.9 to 1.0, p=0.1; adjusted: OR=0.9, 95% CI: 0.9 to 1.0, p=0.06, adjusted predicted probability: bedspaced 76.7% vs cohorted 77.8%).
Figure 1.
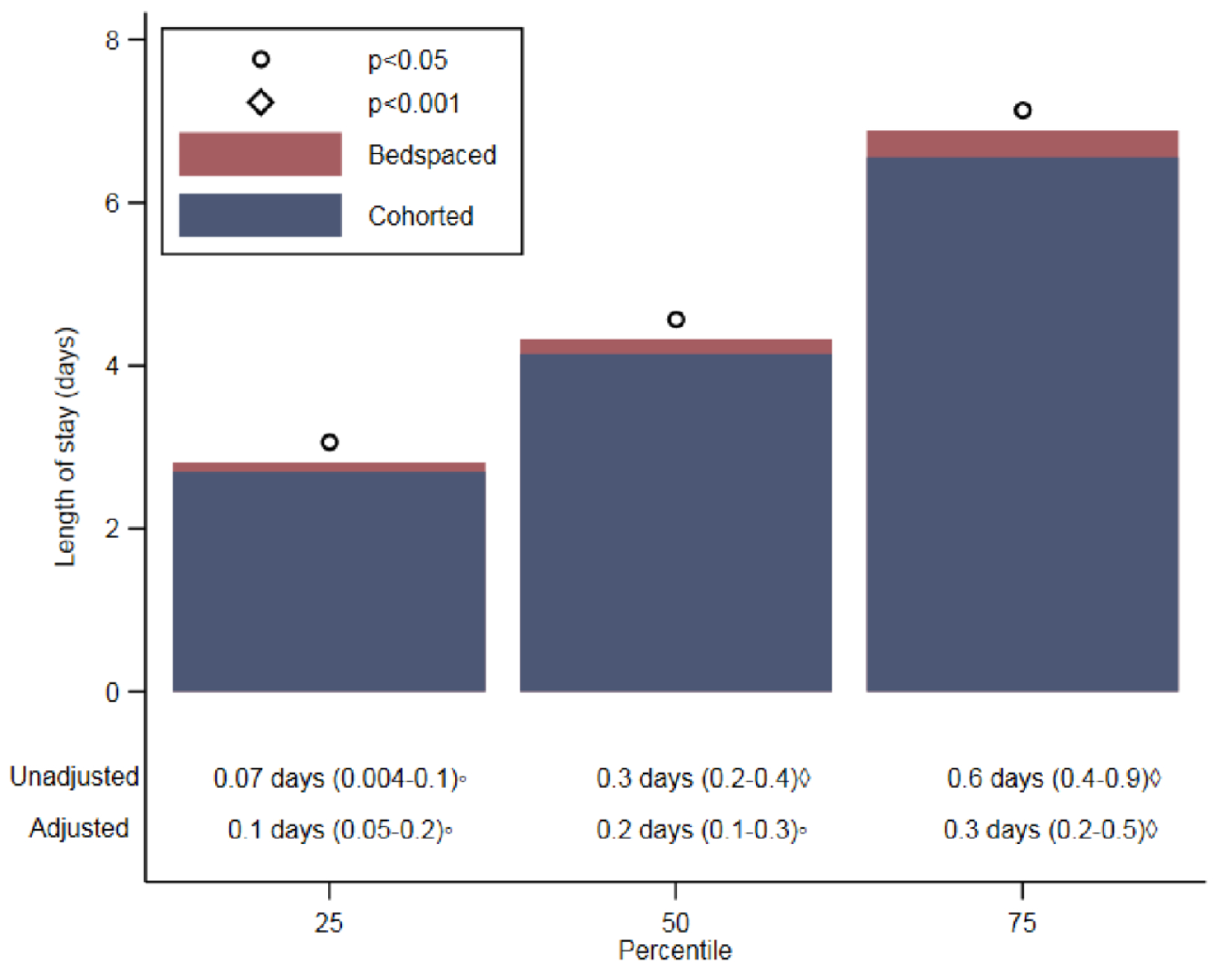
Differences in adjusted length of stay at the 25th, 50th and 75th percentiles among bedspaced* patients vs cohorted† patients‡.
*Bedspaced: patients who overflowed to alternate wards rather than residing on appropriate specialty wards (ie, internal medicine, family medicine and geriatrics wards) in the setting of bed constraints. †Cohorted: patients who resided on appropriate specialty wards (ie, internal medicine, family medicine and geriatrics wards).
‡p-values denote differences between bedspaced and cohorted patients.
Sensitivity analyses
In unadjusted analyses, bedspacing was associated with a decreased rate of discharge (SHR=0.9, 95% CI: 0.9 to 0.9, p<0.001). After adjustment for potential confounders, the SHR estimated from a Fine and Grey competing risks model was 0.9 (95% CI: 0.9 to 0.98, p=0.001), indicating that the rate of discharge was lower for bedspaced patients (suggesting longer adjusted LOS).
When patients with LOS less than 2 days were eliminated from the analyses, results were similar to the primary analyses, however odds of discharge to home became statistically significant. Using quantile regression, bedspaced patients had significantly longer LOS compared with cohorted patients at the 25th, 50th and 75th percentiles in both unadjusted and adjusted models, up to 0.4 days (ie, 10 hours) (95% CI: 0.2 to 0.7, p<0.001) longer at the 75th percentile in the adjusted model. Bedspaced patients had no difference in mortality compared with cohorted patients (unadjusted: OR=1.0, 95% CI: 0.7 to 1.5, p=0.996; adjusted: OR=0.9, 95% CI: 0.6 to 1.5, p=0.8). Bedspaced patients had lower odds of discharge to home compared with cohorted patients (unadjusted: OR=0.9, 95% CI 0.9 to 0.99, p=0.03; adjusted: OR=0.9, 95% CI: 0.8 to 0.98, p=0.02, adjusted predicted probability: bedspaced 73.7% vs cohorted 75.4%). Using Fine and Grey competing risk models, bedspacing was associated with a decreased rate of discharge in both unadjusted (SHR=0.9, 95% CI: 0.9 to 0.9, p<0.001) and adjusted (SHR=0.9, 95% CI: 0.9 to 0.96, p<0.001) models (suggesting longer adjusted LOS).
Secondary analysis: stratification by hospital
Hospitals 1 and 2 had similar results to the pooled analyses with larger effect sizes and hospital 3 differed (table 2).
Table 2.
Secondary analysis: associations of bedspacing with patient-centred outcomes, stratified by hospital
| Hospital 1 | Hospital 2 | Hospital 3 | ||||
|---|---|---|---|---|---|---|
| Outcomes | Estimate (95% CI) | P value | Estimate (95% CI) | P value | Estimate (95% CI) | P value |
| Unadjusted analyses | ||||||
| Length of stay (days) | ||||||
| 25th percentile | 0.3 (0.2 to 0.5) | <0.001 | 0.2 (0.1 to 0.4) | <0.001 | −0.2 (−0.3 to −0.05) | 0.004 |
| 50th percentile | 0.3 (0.1 to 0.6) | 0.003 | 0.7 (0.5 to 0.9) | <0.001 | −0.2 (−0.4 to −0.05) | 0.01 |
| 75th percentile | 1.0 (0.6 to 1.4) | <0.001 | 1.2 (0.9 to 1.6) | <0.001 | −0.3 (−0.7 to 0.05) | 0.09 |
| In-hospital mortality (OR) | 1.0 (0.5 to 1.8) | 0.9 | 0.9 (0.4 to 1.9) | 0.7 | 1.0 (0.5 to 1.8) | 0.98 |
| Discharge to home (OR) | 0.9 (0.8 to 0.99) | 0.04 | 0.7 (0.6 to 0.8) | <0.001 | 1.3 (1.1 to 1.5) | <0.001 |
| Adjusted analyses* | ||||||
| Length of stay (days) | ||||||
| 25th percentile | 0.2 (0.1 to 0.4) | <0.001 | 0.3 (0.1 to 0.4) | <0.001 | −0.1 (−0.2 to 0.04) | 0.2 |
| 50th percentile | 0.4 (0.2 to 0.7) | <0.001 | 0.4 (0.2 to 0.6) | <0.001 | −0.1 (−0.3 to 0.07) | 0.3 |
| 75th percentile | 1.0 (0.7 to 1.4) | <0.001 | 0.5 (0.2 to 0.9) | 0.002 | −0.1 (−0.4 to 0.2) | 0.5 |
| In-hospital mortality (OR) | 0.9 (0.4 to 1.8) | 0.7 | 0.4 (0.2 to 1.1) | 0.07 | 1.2 (0.6 to 2.6) | 0.6 |
| Discharge to home (OR) | 0.9 (0.8 to 1.0) | 0.1 | 0.7 (0.6 to 0.8) | <0.001 | 1.2 (1.0 to 1.3) | 0.04 |
Models were adjusted for: age, gender, race, ethnicity, insurance type, Elixhauser comorbidity scores, the Centers for Medicare and Medicaid Services four-level severity risk adjustment (based on admitting diagnosis, demographics and comorbidities), admission diagnosis category (from International Classification of Disease-9 [ICD-9] and ICD-10 codes), daily mean number of medicine service patients by hospital during the hospitalisation, hospital admission source, season and if a hospital admission occurred during a weekend.
In hospital 1, bedspaced patients had significantly longer LOS compared with cohorted patients at the 25th, 50th and 75th percentiles in both unadjusted and adjusted models, up to 1 day (ie, 24 hours) (95% CI: 0.7 to 1.4, p<0.001) longer at the 75th percentile in the adjusted model. Bedspaced patients had no difference in mortality compared with cohorted patients (unadjusted: OR=1.0, 95% CI: 0.5 to 1.8, p=0.9; adjusted: OR=0.9, 95% CI: 0.4 to 1.8, p=0.7). Bedspaced patients had lower odds of discharge to home compared with cohorted patients, but this did not reach statistical significance in the adjusted model (unadjusted: OR=0.9, 95% CI: 0.8 to 0.99, p=0.04; adjusted: OR=0.9, 95% CI: 0.8 to 1.0, p=0.1, adjusted predicted probability: bedspaced 79.6% vs cohorted 81.2%).
In hospital 2, bedspaced patients had significantly longer LOS compared with cohorted patients at the 25th, 50th and 75th percentiles in both unadjusted and adjusted models, up to 0.5 days (ie, 12 hours) (95% CI: 0.2 to 0.9, p=0.002) longer at the 75th percentile in the adjusted model. Bedspaced patients had no difference in mortality compared with cohorted patients (unadjusted: OR=0.9, 95% CI: 0.4 to 1.9, p=0.7; adjusted: OR=0.4, 95% CI: 0.2 to 1.1, p=0.07). Bedspaced patients had lower odds of discharge to home compared with cohorted patients (unadjusted: OR=0.7, 95% CI: 0.6 to 0.8, p<0.001; adjusted: OR=0.7, 95% CI: 0.6 to 0.8, p<0.001, adjusted predicted probability: bedspaced 76.6% vs cohorted 81.6%).
Hospital 3 did not have statistically significant differences in LOS at any quantile or in-hospital mortality between bedspaced and cohorted patients. Bedspaced patients had higher odds of discharge to home (unadjusted: OR=1.3, 95% CI: 1.1 to 1.5, p<0.001; adjusted: OR=1.2, 95% CI: 1.0 to 1.3, p=0.04, adjusted predicted probability: bedspaced 73.5% vs cohorted 71.2%).
Secondary analysis: sensitivity analysis
When patients with LOS less than 2 days were eliminated from the analyses, results were similar to the secondary analysis among hospitals 1 and 2, but the differences between bedspaced and cohorted patients were attenuated in hospital 3.
In hospital 1, bedspaced patients had significantly longer LOS compared with cohorted patients at the 25th, 50th and 75th percentiles in both unadjusted and adjusted models, up to 1 day (ie, 24 hours) (95% CI: 0.6 to 1.5, p<0.001) longer at the 75th percentile in the adjusted model. Bedspaced patients had no difference in mortality compared with cohorted patients (unadjusted: OR=0.9, 95% CI: 0.5 to 1.7, p=0.7; adjusted: OR=0.8, 95% CI: 0.4 to 1.8, p=0.6). Bedspaced patients had lower odds of discharge to home compared with cohorted patients, but this did not reach statistical significance (unadjusted: OR=0.9, 95% CI: 0.8 to 1.0, p=0.05; adjusted: OR=0.9, 95% CI: 0.8 to 1.0, p=0.1, adjusted predicted probability: bedspaced 77.5% vs cohorted 79.3%).
In hospital 2, bedspaced patients had significantly longer LOS compared with cohorted patients at the 25th, 50th and 75th percentiles in both unadjusted and adjusted models, up to 0.6 days (ie, 14 hours) (95% CI: 0.2 to 1.0, p=0.003) longer at the 75th percentile in the adjusted model. Bedspaced patients had no difference in mortality compared with cohorted patients (unadjusted: OR=0.8, 95% CI: 0.3 to 2.1, p=0.7; adjusted: OR=0.4, 95% CI: 0.2 to 1.3, p=0.1). Bedspaced patients had lower odds of discharge to home compared with cohorted patients (unadjusted: OR=0.7, 95% CI: 0.6 to 0.8, p<0.001; adjusted: OR=0.7, 95% CI: 0.6 to 0.8, p<0.001, adjusted predicted probability: bedspaced 73.9% vs cohorted 79.8%).
Hospital 3 did not have statistically significant differences in LOS at any quantile or in-hospital mortality between bedspaced and cohorted patients. Bedspaced patients had higher odds of discharge to home in unadjusted analyses (OR=1.3, 95% CI: 1.1 to 1.4, p=0.001), however adjusted odds of discharge to home were not statistically significant (OR=1.1, 95% CI: 1.0 to 1.3, p=0.1).
DISCUSSION
Bedspacing is associated with increased hospital LOS and lower odds of discharge to home, which are associated with patient stress, discomfort and complication risks (eg, hospital-acquired infections, venous thromboembolic events, delirium and functional decline).17–19 These are novel findings among medicine wards as most prior studies have not demonstrated associations between bedspacing and LOS and have not investigated discharge to home as an outcome.1,2,11 Conversely, several studies have demonstrated associations between bedspacing and in-hospital mortality, which our study did not replicate.1,2 The differences in our findings may be due to a larger sample size, the differences between US hospitals and national health systems outside of the US and shorter LOS with higher post-acute care utilisation in the US compared with other countries.20,21
Although the effect size for prolonged LOS is small overall, we found that bedspaced patients experience 5% longer LOS than their cohorted counterparts across all percentiles investigated, which is potentially clinically meaningful. First, as LOS increases, the prolonged amount of time a patient spends in the hospital becomes clinically significant. And second, hospital administrators across the US have adopted “pre-noon discharges” as a metric to improve patient flow and throughput from the ED, making the difference between an 8AM and a 2PM discharge potentially consequential for hospital operations.22,23 Additionally, in the analysis stratified by hospital, bedspaced patients in the quaternary referral centre experienced 1 day longer LOS compared with their cohorted counterparts in the 75th percentile of LOS which has potentially large patient-centred and hospital operations implications.
Prolonged LOS raises fiscal costs and creates opportunity costs for future patients by limiting access to acute care beds. Additionally, although the effect size is small overall, cohorting patients could have yielded an additional 70 patients discharged to home in this study. As Medicare and other US payers seek to reduce variability and eliminate low-value care, cohorting may provide a simple yet highly impactful strategy: if extrapolated to the entire Medicare population, billions of dollars could be saved and thousands of patients could be discharged back to their homes each year. Future trials of cohorting strategies are needed to assess outcomes and possible unintended consequences (eg, longer ED boarding times and unutilized beds).
Additionally, the full benefit of geographic cohorting may not be represented by our findings, as only 60% to 76% of medicine service patients per hospital were cohorted. It is possible that the detrimental effects of bedspacing could also impact outcomes of cohorted patients when medicine ward staff care for more than a quarter of non-medicine service patients, potentially detracting care time from cohorted patients. Therefore, the effect size may be larger than our observed findings if cohorted patients composed a greater magnitude of the ward population.
The analyses stratified by hospital demonstrated that hospitals 1 and 2 (the quaternary referral centre and the community hospital, respectively) had similar results to the pooled analysis. Hospital 3 (the tertiary referral centre), the hospital with the most bedspacing, demonstrated no statistically significant differences in LOS or in-hospital mortality between bedspaced and cohorted patients, but was associated with increased odds of discharge to home – a signal in the opposite direction from the pooled analysis. These findings may be explained by the large numbers of observation patients in hospital 3 which we were not able to distinguish from inpatients. Observation patients occupy beds diffusely throughout the hospital, potentially explaining the higher proportion of bedspacing noted in hospital 3. Hospital LOS for observation patients is quite short (typically less than 24 hours), biasing LOS results towards the null hypothesis. By definition,24 all observation patients are discharged to home as they do not qualify for post-acute care facilities, including skilled nursing or acute rehabilitation facilities, which may explain the increased odds of discharge to home demonstrated in hospital 3. In our post-hoc sensitivity analysis, the association of bedspacing with increased odds of discharge to home was attenuated when patients with LOS less than 2 days were excluded from the analyses, supporting our hypothesis as outlined above.
This study has several important limitations. First, heterogeneous populations make residual confounding likely despite clustering by centre; adjusting for patient-, service- and hospital-level variables including patient severity of illness and admission diagnosis; performing analyses stratified by hospital; and excluding short-stay patients. Second, despite studying a diverse, multicenter population, all centres were urban academic hospitals in Philadelphia, Pennsylvania, US. Finally, although the data are several years old, hospital-wide capacity strain continues to increase over time, so we would expect the results with more current data to be consistent with our findings and to potentially demonstrate a larger effect size given increasing capacity strain. Indeed, our findings have influenced bed allocation plans for a new hospital within our health system.
In summary, bedspacing is associated with adverse patient-centred outcomes in the study hospitals. Future work is needed to determine if these associations exist in other health systems, to understand mechanisms underlying bedspacing contributing to adverse outcomes and to identify factors that mitigate these adverse effects in order to provide high-value, patient-centred care to hospitalised patients.
Funding
This study was funded by National Institute on Aging (K23 AG045338), Agency for Healthcare Research and Quality (K12 HS026372-01) and National Heart, Lung, and Blood Institute (F32 HL139107-01, K23 HL146894-01 and R00 HL141678).
Footnotes
Competing interests None declared.
Patient consent for publication Not required.
Provenance and peer review Not commissioned; externally peer reviewed.
Data availability statement No data are available.
Preliminary results of this work were presented as abstracts at the Society of Hospital Medicine and Society of General Internal Medicine International Conferences 2019.
REFERENCES
- 1.Bai AD, Srivastava S, Tomlinson GA, et al. Mortality of hospitalised internal medicine patients bedspaced to non-internal medicine inpatient units: retrospective cohort study. BMJ Qual Saf 2018;27:11–20. [DOI] [PubMed] [Google Scholar]
- 2.La Regina M, Guarneri F, Romano E, et al. What quality and safety of care for patients admitted to clinically inappropriate wards: a systematic review. J Gen Intern Med 2019;34:1314–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stylianou N, Fackrell R, Vasilakis C. Are medical outliers associated with worse patient outcomes? A retrospective study within a regional NHS Hospital using routine data. BMJ Open 2017;7:e015676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chalfin DB, Trzeciak S, Likourezos A, et al. Impact of delayed transfer of critically ill patients from the emergency department to the intensive care unit. Crit Care Med 2007;35:1477–83. [DOI] [PubMed] [Google Scholar]
- 5.Singer AJ, Thode HC, Viccellio P, et al. The association between length of emergency department boarding and mortality. Acad Emerg Med 2011;18:1324–9. [DOI] [PubMed] [Google Scholar]
- 6.Vishnupriya K, Falade O, Workneh A, et al. Does sepsis treatment differ between primary and overflow intensive care units? J Hosp Med 2012;7:600–5. [DOI] [PubMed] [Google Scholar]
- 7.Pascual JL, Blank NW, Holena DN, et al. There’s no place like home: boarding surgical ICU patients in other ICUs and the effect of distances from the home unit. J Trauma Acute Care Surg 2014;76:1096–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Goulding L, Adamson J, Watt I, et al. Patient safety in patients who occupy beds on clinically inappropriate wards: a qualitative interview study with NHS staff. BMJ Qual Saf 2012;21:218–24. [DOI] [PubMed] [Google Scholar]
- 9.Goulding L, Adamson J, Watt I, et al. Lost in hospital: a qualitative interview study that explores the perceptions of NHS inpatients who spent time on clinically inappropriate hospital wards. Health Expect 2015;18:982–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Song H, Tucker AL, Graue R, et al. Capacity pooling in hospitals: the hidden consequences of Off-Service placement. Manage Sci 2019.
- 11.Liu J, Griesman J, Nisenbaum R, et al. Quality of care of hospitalized internal medicine patients bedspaced to non-internal medicine inpatient units. PLoS One 2014;9:e106763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Santamaria JD, Tobin AE, Anstey MH, et al. Do outlier inpatients experience more emergency calls in hospital? an observational cohort study. Med J Aust 2014;200:45–8. [DOI] [PubMed] [Google Scholar]
- 13.Perimal-Lewis L, Li JY, Hakendorf PH, et al. Relationship between in-hospital location and outcomes of care in patients of a large general medical service. Intern Med J 2013;43:712–6. [DOI] [PubMed] [Google Scholar]
- 14.Centers for Medicare & Medicaid Services. Prospective payment systems. Available: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/ProspMedicareFeeSvcPmtGen/index.html [Accessed 26 Sep 2018].
- 15.Vizient I 2016 risk adjustment methodology 2016.
- 16.Fine JP, Gray RJ. A proportional hazards model for the Subdistribution of a competing risk. J Am Stat Assoc 1999;94:496–509. [Google Scholar]
- 17.Fleischmann KE, Goldman L, Young B, et al. Association between cardiac and noncardiac complications in patients undergoing noncardiac surgery: outcomes and effects on length of stay. Am J Med 2003;115:515–20. [DOI] [PubMed] [Google Scholar]
- 18.Lilly CM, Cody S, Zhao H, et al. Hospital mortality, length of stay, and preventable complications among critically ill patients before and after tele-ICU reengineering of critical care processes. JAMA 2011;305:2175–83. [DOI] [PubMed] [Google Scholar]
- 19.Allman RM, Goode PS, Burst N, et al. Pressure ulcers, hospital complications, and disease severity: impact on hospital costs and length of stay. Adv Wound Care 1999;12:22–30. [PubMed] [Google Scholar]
- 20.Wunsch H, Angus DC, Harrison DA, et al. Variation in critical care services across North America and Western Europe. Crit Care Med 2008;36:2787–8. [DOI] [PubMed] [Google Scholar]
- 21.Wunsch H, Hill AD, Scales DC, et al. Comparison of care patterns and rehospitalizations for mechanically ventilated patients in New York and Ontario. Ann Am Thorac Soc 2019;16:463–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wertheimer B, Jacobs REA, Bailey M, et al. Discharge before noon: an achievable Hospital goal. J Hosp Med 2014;9:210–4. [DOI] [PubMed] [Google Scholar]
- 23.Wertheimer B, Jacobs REA, Iturrate E, et al. Discharge before noon: effect on throughput and sustainability. J Hosp Med 2015;10:664–9. [DOI] [PubMed] [Google Scholar]
- 24.Services CfMM. Fact Sheet: Two-Midnight Rule. Hospitals, Quality, Billing & Payments, 2015. Available: https://www.cms.gov/newsroom/fact-sheets/fact-sheet-two-midnight-rule-0 [Accessed 3 Jan 2020].


