Abstract
Objective:
Death and morbidity associated with substance use have risen continuously over the last few decades, increasing the need for rigorous examination of promising programs. Interventions attempting to change multiple behaviors have been designed to address interconnected problems such as use of both alcohol and drugs. This meta-analysis aimed to examine the efficacy of multi-behavior interventions to curb non-medical substance use in relation to the theoretical relation among different substance use behaviors. Specifically, our synthesis aimed to estimate the optimal number of recommendations for intervention efficacy and evaluate the impact of different combinations of recommendations on intervention efficacy.
Methods:
A synthesis of multi-behavior interventions addressing non-medical substance use was conducted to measure behavioral changes between the pretest and the follow-up. These changes were then compared across different numbers of recommendations.
Results:
Sixty-nine reports and 233 effect sizes (k of conditions = 155, n = 28,295) were included. A positive linear relation was found between the number of targeted behaviors and intervention efficacy, which was stronger for drug use than alcohol use. Furthermore, recommendations on drug use worked better when paired with recommendations targeting other behaviors, whereas recommendations on alcohol use worked more independently. Lastly, multi-behavior interventions were especially efficacious when delivered by experts.
Conclusions:
Overall, our synthesis indicated that targeting multiple substances is beneficial for changing drug use outcomes, but less so for alcohol use outcomes. Therefore, in the current substance use epidemic, innovative multi-behavior programs appear to hold promise, especially to combat non-medical drug use.
Keywords: Meta-analysis, substance use, alcohol, multi-behavior interventions
The detrimental effects of non-medical substance use are well documented. According to the Centers for Disease Control, between 2006 and 2010, alcohol was responsible for an average of 88,000 deaths and 2.5 million years of potential life lost each year in the United States (Centers for Disease Control and Prevention, 2016). Deaths from illicit drug overdoses (heroin, natural and semisynthetic opioids, methadone, synthetic opioids, cocaine, etc.) in the United States are currently at a record high in both sheer numbers and prevalence per 100,000 people (Hedegaard et al., 2017). In 2015, 16.3 per 100,000 people died of a drug overdose, which represented over 2.5 times the 6.1 per 100,000 rate in 1999 (Hedegaard et al., 2017). Fortunately, many treatments and programs have been created to address non-medical substance use and addiction, including multi-behavior interventions, which are interventions geared towards changing two or more behaviors.
The efficacy of interventions aimed at reducing substance use has often been underwhelming. For example, nine prior meta-analyses estimated efficacy across populations and interventions. The sources, number of studies, critical comparisons, and effect sizes of these nine syntheses appear in Table 1. The syntheses spanned several decades with no apparent changes in efficacy, leading to the question of whether the newest generation of more complex interventions is ready to reduce substance use.
Table 1.
Summary of Prior Meta-Analyses of Substance Use Interventions.
| Title | M year | k of studies | Effect size | Comparison (& type of controls) | ||
|---|---|---|---|---|---|---|
| Prendergast, Podus, Chang, & Urada, (2002) | The effectiveness of drug abuse treatment: A meta-analysis of comparison group studies | 1980 | 78 | g = 0.34 | Drug use treatment vs. active control | |
| Prendergast, Podus, Finney, Greenwell, & Roll (2006) | Contingency management for treatment of substance misuse disorders: A meta-analysis | 1986 | 47 | g = 0.42 | Contingency management vs. control | |
| Magill & Ray (2009) | Cognitive-Behavioral Treatment with Adult Alcohol and Illicit Drug Users: A meta-analysis of randomized controlled trials | 1994 | 53 | g = 0.154 | CBT vs. active control | |
| g = 0.115 | CBT vs. active control, | |||||
| Carney & Myers, (2012) | Effectiveness of early interventions for substance using adolescents: Findings from a systematic review and meta-analysis | 2006 | 9 | g = 0.24 | Drug and alcohol treatment vs. control | |
| Blodgett, Maisel, Fuh, Wilbourne, & Finney, (2014) | How effective is continuing care for substance misuse disorders? A meta-analytic review | 1999 | 19 | g = 0.187 | Continuing care vs passive control | |
| g = 0.271 | Continuing care vs. passive control comparison | |||||
| Benishek et al., (2014) | Prize-based contingency management for the treatment of substance abusers: A meta-analysis | 2007 | 19 | d = 0.46 | Contingency management vs. active control | |
| d = 0.33 | Contingency management vs. active control | |||||
| Tanner-Smith & Risser (2016) | A meta-analysis of brief alcohol interventions for adolescents and young adults: Variability in effects across alcohol measures | NR | 190 | g = 0.25 | Brief intervention vs. passive control (adolescents) | |
| g = 0.15 | Brief intervention vs. passive control (young adults) | |||||
| Boumparis, Karyotaki, Schaub, Cuijpers, & Riper (2017) | Internet interventions for adult illicit substance misusers: A meta-analysis | 2010 | 17 | g = 0.31 | Internet interventions vs. mostly active control | |
| g = 0.22 | Internet interventions vs. mostly active control | |||||
| Sayegh, Huey, Zara, & Jhaveri (2017) | Follow-up treatment effects of contingency management and motivational interviewing on substance misuse: A meta-analysis | NR | 84 | d = 0.43 | Contingency management vs. control | |
| d = 0.06 | Contingency management vs. control | |||||
| d = 0.10 | Motivational interviewing vs. control | |||||
| d = 0.22 | Motivational interviewing vs. control | |||||
g = Hedge’s g, corrected for small sample bias. d = Cohen’s d, not corrected for small sample bias.
It is noteworthy that many of the programs included in Table 1 have addressed drug or alcohol use as relatively independent of other related behaviors or contextual factors that are likely to maintain the behavior. But in fact, research has shown that substance use often stems from a plethora of biological, psychological, and social factors, all working in tandem (Borrell-Carrió et al., 2004). Substance use is often interdependent with other disorders and behaviors. For example, a number of underlying factors that affect a person’s propensity to alcohol dependence may also lead to a propensity to tobacco dependency (Dawson, 2000; Friedman et al., 1991). Moreover, different forms of substance use are often interrelated. For example, alcohol and drug use are strongly correlated and using alcohol is often a precursor to drug use (Regier et al., 1990; Agosti, Nunes, & Levin, 2002). Relative to people who do not use alcohol, people who use alcohol are 35 times more likely to use cocaine, 17 times more likely to use sedatives, and 13 times more likely to use opioids (Helzer & Pryzbeck, 1988; Agosti, Nunes, & Levin, 2002; Stinson et al., 2005).
Recognizing the interrelation among different behaviors, cutting-edge intervention approaches often attempt to target multiple behaviors by making multiple recommendations. These interventions that attempt to change two or more behaviors are known as integrated interventions (Prochaska et al., 2008) or multi-behavior programs (Wilson et al., 2015), and can be implemented in several ways. First of all, interventions can promote multiple principal goals regarding substance use or other risks, based on knowledge of comorbid risks in the population, or programs and behaviors that the population needs. For example, an intervention tested by Haller et al. (2014) provided two main recommendations, namely to reduce alcohol use and to reduce cannabis consumption. Besides directly targeting risky behaviors, multi-behavior interventions can also address multiple behaviors that are often disrupted by the use of substances and can improve the outlook and lifestyle of people who use non-medical substances. For example, an intervention tested by Kypri and McAnally (2005) recommended increasing physical activity, increasing fruit intake, and increasing vegetable intake, besides reducing hazardous drinking. Both types of recommendations discussed above are the goals of these programs and are considered to be main recommendations.
Interventions can also promote multiple auxiliary recommendations, which are skills or behaviors that are prerequisite for recipients to implement the main recommendations. For example, the intervention tested by Deady, Mills, Teesson, & Kay-Lambkin (2016) provided three auxiliary recommendations, including to monitor drinking behaviors, to monitor thoughts, and to plan for activities, besides the main recommendation to reduce alcohol use. These recommendations concern behaviors that, if implemented, can help participants to be successful at implementing the main recommendation.
Given the demonstrated existence of clusters of harmful behaviors and the antagonistic effects between drug use and health promoting behaviors, multi-behavior programs are the most logical solution to addressing the complex problem of substance use. Before our meta-analysis, some evidence suggested that multi-behavior interventions are effective in the domain of lifestyle behaviors (Wilson et al., 2015). Although these results are auspicious, it is still unclear whether similar models will improve substance-related interventions over and above prior generations of programs, and whether these programs apply differently to drug and alcohol outcomes. Therefore, the primary purpose of this meta-analysis was to examine the efficacy of these multi-behavior interventions in the domain of substance use.
Commonly Used Recommendations and Combinations of Recommendations in Multi-Behavior Programs for Non-Medical Substance Use
Besides recommending a reduction in alcohol use and drug use, multi-behavior interventions often provide recommendations to change other related behaviors. These behaviors can range from major goals, such as maintaining a healthy lifestyle and preventing transmission of sexually transmitted infections, to ones such as seeking social support and making better use of community services. To better understand the efficacy of multi-behavior interventions in the substance use domain, it is thus crucial to first describe combinations of recommendations that are most commonly used in multi-behavior programs for non-medical substance use. Therefore, another goal of this meta-analysis was to provide this description and further investigate the efficacy of such combinations of recommendations.
Optimal Number of Recommendations to Reduce Drug and Alcohol Use: Facilitating, Independent, and Antagonistic Relations among Behaviors
Besides the type of recommendations to include, the number of recommendations to include in an intervention is also an important question to consider when aiming for the most efficacious intervention program. Whereas too few recommendations may not be stimulating enough to elicit change, an excessive number of recommendations can create burden and undermine the motivation to change (Wilson et al., 2015; Albarracín et al., 2018; Albarracín et al., 2019). Therefore, our meta-analysis also investigated the optimal number of recommendations to produce the greatest behavioral change.
The optimal number of recommendations to include in an intervention should depend on the relations among the target behaviors. Although previous research has shown a high intercorrelation among the use of multiple substances, the use of some substances may still be relatively more independent than the use of other substances. Better knowledge of the relative independence among the network of different behavior can help better predict the optimal number of recommendations targeting the use of each specific substance. To achieve this goal, in this paper, we proposed two models of relations among behaviors (see Figure 1). On the one hand, a Relative Interdependence Model represents behaviors that are causally associated. For example, a person may experience cocaine cravings each time he drinks alcohol, or not seek health care during periods of heavy drug use (Behavior A causally related with Behavior B). Therefore, alcohol use increases the probability of drug use and drug use decreases the probability of seeking health care. On the other hand, a Relative Independence Model represents behaviors that are relatively independent from each other. For example, a person may drink alcohol (Behavior A) without having a craving for cocaine (Behavior A not causally related with Behavior B) (see e.g., Livingston, Oost, Heck, & Cochran, 2015). Thus, the Relative Interdependence model should be associated with stronger correlations among these two behaviors than the relative independence model, although neither model is likely to lead to either a perfect correlation or a 0 correlation and correlations among behaviors may also occur due to other factors.
Figure 1.
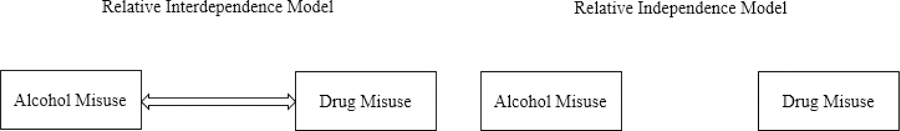
Models of Relatively Interdependent and Relatively Independent Behaviors
In the current meta-analysis, we tested our theoretical hypothesis by comparing the efficacy of multi-behavior interventions targeting alcohol use, drug use, or both. In summary, if behaviors follow the Relative Interdependence Model, such as alcohol use facilitating drug use, or drug recovery requiring a cluster of support and health care services, then an intervention should be more efficacious when it targets both alcohol use and drug use, compared to targeting drug use alone. If behaviors follow the Relative Independence Model, such as alcohol use being independent from drug use, then an intervention should be equally efficacious when it targets both alcohol use and drug use, compared to targeting alcohol use alone.
A related important question is whether adding behavioral recommendations increases efficacy in a monotonic fashion. If the behaviors contribute to positive outcomes because they are mutually facilitating, then more recommendations should be better than fewer. However, if behaviors contribute to a positive outcome but compete for resources and cause fatigue, then more recommendations should add only up to a point (Baumeister & Heatherton, 1996; Muraven et al., 1998; Vohs & Heatherton, 2000). In the domain of lifestyle (smoking, exercise, and diet), Wilson et al. (2015) showed that the improvements in efficacy resulting from adding recommendations flattened out or even decreased after 3 recommendations. However, the pattern may be different in the substance use domain. Whereas quitting smoking can make dieting more difficult, quitting alcohol can make quitting drugs easier. Likewise, protecting one’s child, completing drug treatment, maintaining drug abstinence, and complying with court orders act synergistically, so that protecting a child is generally not possible without maintaining drug abstinence, complying with court orders, and completing drug treatment. Therefore, we hypothesized that in the substance use domain, there should be a linear relation between number of recommendations and intervention efficacy, such that more recommendations generally lead to more behavioral changes.
The Current Meta-Analysis
The synthesis included 69 research reports (k of conditions = 155), which looked at the outcomes of interventions related to both alcohol and drug use. The list of the articles and its description can be found in Supplementary Table 1. We determined the change between the baseline and first follow-up and compared change across interventions with different numbers of recommendations, with passive controls coded as providing zero recommendations. The average gap between the baseline and first follow-up was two and a half weeks.
Importantly, the prior meta-analysis of multi-behavior interventions in the lifestyle domain identified several factors such as targeting a specific population and delivery format, as moderators of the effects of these multi-behavior interventions (Wilson et al., 2015). Often, targeting a specific population (e.g., specific ethnic group, vulnerable population) leads to more efficacious programs than not targeting (Ammerman et al., 2002; Ebrahim et al., 2006; Hardcastle et al., 2013), and group delivery format is associated with higher efficacy than individual delivery format (Ayala, 2006; Wright et al., 2011). Besides these features, we also coded a variety of study settings and methodological moderators that have been commonly studied in intervention research (Albarracín et al., 2005), as well as the expertise of the facilitator of the intervention as represented by professional training in health or substance use issues (Durantini et al., 2006; Amaro et al., 2007; Burton et al., 1995). We also coded whether the intervention was designed to be culturally specific or generic (Dushay et al., 2001; Fogel et al., 2015), whether the intervention made use of active (e.g., behavioral skills training) vs. passive (e.g., informational arguments) strategies (Albarracín et al., 2005; Grossbard et al., 2010), whether the intervention relied on attitudinal elements (e.g., attitudinal arguments, threat arguments; Albarracín et al., 2005; Burke et al., 2005), motivational elements (e.g., feedback, encouragement, a written contract; Jungerman et al., 2007; Latkin et al., 2009), and/or skills training (e.g., role-playing, goal setting; Albarracín et al., 2005; Calsyn et al., 2010; Kaner et al., 2013), as well as whether the intervention included biological methods (e.g., use of nicotine patches, methadone; Hanson et al., 2008; Penberthy et al., 2013). A last moderator we included was whether the intervention targeted an alcohol / drug dependent population. This moderator was added to distinguish prevention of alcohol or drug use increase from treatment in dependent populations, which are often different in efficacy and characteristics (Nemoto et al., 2002; Volkow & Li, 2005; Fischer et al., 2015). The present meta-analysis explored the influence of all these factors in the domain of substance use.
Critical to our objectives, we described the synthesized multiple-behavior interventions in terms of whether they targeted drug use, alcohol use, and any additional behaviors, such as using available community services, seeking social support, and developing behavioral skills to combat non-medical substance use. We then analyzed the impact of the number of all recommendations, as well as the number of main recommendations only, and considered this impact in the context of the types of behaviors that were combined. These analyses controlled for other factors identified as having an impact on change.
Method
Literature Search
We conducted an internet search of six research databases (EBSCO, Scopus, Web of Science, PubMed, JSTOR, and Crossref). The search terms used were as follows: intervention, health education, persuasion, recommendation, treatment, educational program, rehabilitation, counseling outcomes, treatment outcomes, treatment effectiveness evaluation, treatment compliance, health promotion, behavior change, and randomized trial. To specifically find articles related to multiple alcohol and/or drug use behaviors, we used the syntax ((alcohol or drug or substance) AND ((intervention or randomized trial)) NOT ((review or meta-analysis or campaign or cost-effectiveness or theoretical)). This search yielded a total of 2,022 articles. In an attempt to include as many pertinent articles as possible, we searched through the reference list of related meta-analyses, conference titles, and emailed the researchers who appeared most frequently in the database search, requesting any unpublished works. Article searches were performed iteratively in 2014, 2015, 2017, and 2019.
Inclusion Criteria
After finding research reports, we screened the articles with our inclusion criteria, which led to a total of 69 eligible articles (see Figure 2). The inclusion criteria were as follows:
Existence of at least two groups, including at least one multi-behavior group. To be considered eligible, all reports had to have at least two groups to allow for comparison of change across conditions. They also had to have at least one multi-behavior intervention group that provided at least one substance use recommendation.
Existence of at least one behavioral or clinical outcome. To be included, all reports had to include at least one behavioral or clinical outcome variable. For example, if a paper reported behavioral intentions only, it was excluded.
Number of recommendations available. To be included in this meta-analysis, all reports had to include information that allowed us to count the number of recommendations. Reports were excluded if the number of recommendations could not be ascertained.
Presence of sufficient statistical information. All reports that did not include enough statistical information to calculate effect sizes for change over time were excluded. Therefore, to be included, articles had to report outcome values at both baseline and at least one follow-up, or other statistics (e.g., a paired t-test) to calculate change effect sizes. Reports that only included a follow-up outcome value were excluded, due to the fact that they disallowed us to calculate effect sizes to represent change over time.
Figure 2.
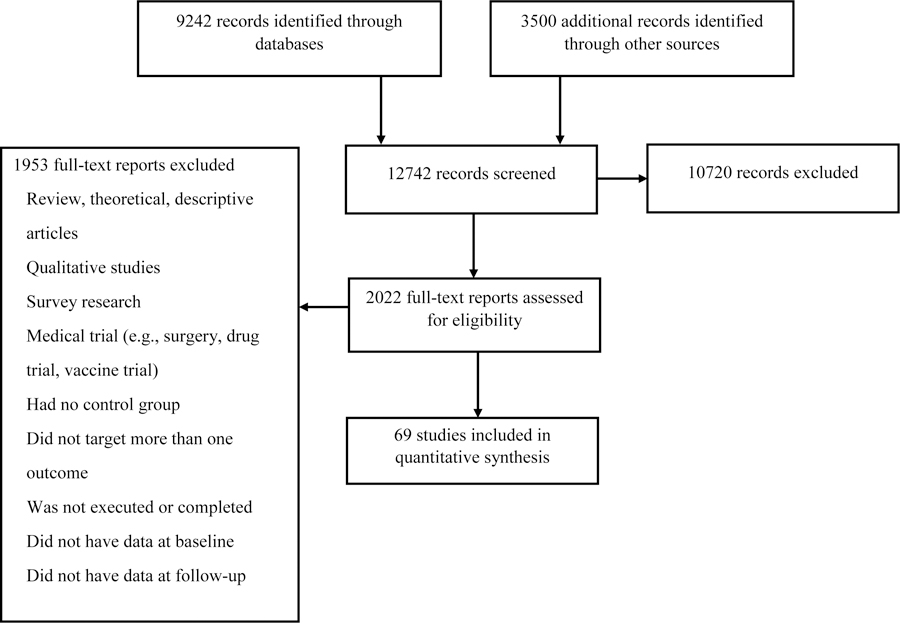
Flow of reports in this systematic review.
Measuring Change in Overall Outcomes, Drug use Outcomes, and Alcohol use Outcomes
Similar to the coding process used in Wilson et al. (2015), we recorded both behavioral and clinical intervention outcomes. The most frequent outcomes were alcohol consumption and drug consumption. The most frequent measures for alcohol consumption were the amount of alcohol consumed in a specific period (e.g., in a day, in a week), the frequency of excessive alcohol use (e.g., number of days of excessive drinking in a month), the proportion of abstinence days, and the number of drunk days. The most frequent measures for drug consumption were the amount of drug use (heroin, opioids, methadone, cocaine, crack, etc.) in a specific period (e.g., in the past week), the frequency of ecstasy use, the frequency of excessive drug use, the proportion of abstinence days, and the number of times having sex while under the influence of drugs.
Behaviors that help to reduce the risk from non-medical substance use were measured as well. These variables included adherence to medications, managing negative consequence of substance use, and counseling attendance. Clinical outcomes were measured infrequently. Clinical outcomes for alcohol use were urine test results, the number of medical conditions related to alcohol use, and diagnoses of alcohol use disorder or dependence. Clinical outcomes for substance use were urine test results, the number of drug use disorders diagnosed, and the number of dependence symptoms.
We obtained each effect size by representing the change from the pretest to the posttest (e.g., d = (Mpostest −Mpretest/SDpretest) for each of the outcome variables in a sample, including drug use outcomes, alcohol use outcomes, and any auxiliary behavioral outcomes, such as medical adherence and counseling attendance. For example, we obtained 5 effect sizes from Reback et al. (2010), including one alcohol-use outcome (i.e. percentage of people free of alcohol in a urine test), three drug-use outcomes (i.e. percentage of people free of cocaine / amphetamine / methamphetamine in a urine test), and one auxiliary outcome (i.e. intervention attendance). Importantly, the decision to analyze change over time was based on the fact that performing post-test comparisons across conditions would typically provide one or two effect sizes of the many possible comparisons across interventions with 0, 1, 2, 3, 4, 5, 6, 7, 8 recommendations, and so on. Such a situation would thus require abnormally high levels of imputation to estimate the impact of the number of recommendation count, much higher than is the norm for network meta-analysis (Lumley, 2002; Caldwell et al., 2005; Glenny et al., 2005). Thus, it seemed more appropriate to impute the correlation between measures than to model tons of differences based on the scarce data provided by the trials we synthesized.
When running analyses on drug use and alcohol use separately, we only included the outcomes that only pertained to drug use or alcohol use from each report, depending on what they reported. For example, in Reback et al. (2010), we obtained one effect size for alcohol use from the only reported alcohol-use outcome, and three effect sizes for drug use from each of the three drug-use outcomes. Outcomes that pertained only to alcohol use included alcohol consumption, sex and drinking, and managing harmful consequences of alcohol use. Outcomes that pertained only to drug use included drug consumption, exchanging drugs for sex, starting drug treatment, and sharing syringes or other equipment. In each case, effects were scored to reflect improvement. For example, a decrease in alcohol use and an increase in the percentage of a sample starting drug treatment were coded positive.
Coding of Number of Overall and Main Recommendations
We coded the number of recommendations by counting the total number of behavioral goals, including both main and auxiliary goals. We also created a separate count of number of main recommendations for the purpose of some analyses. Main recommendations were defined as the main goals defined in an intervention which had a direct impact on clients’ quality of life, whereas auxiliary recommendations are those that can help clients to achieve the main goals of the intervention. For example, the intervention in Santa, LaRowe, Armeson, Lamb, and Hartwell (2016) was coded as providing four recommendations because the intervention encouraged participants to reduce substance use, stay clean and sober, attend treatment, and take medication for the substance use disorder. Among these recommendations, the first one was considered a main recommendation, because it directly targeted the risky behavior of substance use and was the intervention’s focus. The other three were coded as auxiliary because they were introduced to help clients to achieve the main goal of reducing non-medical substance use.
Coding of Type of Recommendations
In addition to understanding the impact of the number of recommendations, we were interested in describing the most commonly used recommendations and combinations of recommendations, and their influence on change. Therefore, for each intervention, we coded whether it included recommendations targeting alcohol use, drug use, and any other commonly targeted behaviors, including sexual behavior, lifestyle behavior, service use, support seeking, and development of behavioral skills. However, due to the small ks for each of these types of recommendations, we combined all these recommendations into the category of “other recommendations” and classified all interventions into seven categories based on whether they included recommendations targeting alcohol use, drug use, and at least one other domain: (a) neither alcohol nor drug use, (b) alcohol use only, (c) drug use only, (d) alcohol and drug use, (e) alcohol use and at least one other domain, (f) drug use and at least one other domain, and (g) drug use, alcohol use, and at least one other domain.
Coding of Exploratory Study Characteristics
Relevant characteristics of the reports, as well as the methods used in the studies, were coded by two independent raters as described in Supplementary Materials. Disagreements between coders were resolved by discussion and further examination of the reports.
Description of the report.
We coded report characteristics, including the (a) publication year, (b) first authors’ institution (e.g., college, hospital, research center), (c) first authors’ institutional area (e.g., psychology, public health, medicine), (d) source type (e.g., journal article, dissertation), (e) location of the intervention, and (f) language of the intervention.
Demographic and other participant characteristics.
We also coded characteristics of the sample, including the (a) sample size, (b) percentage of males in each group, (c) mean age, (d) percentages of participants of European, African, Latin, Asian, and Native American descent, (e) percentage of participants who completed high school and their mean years of education, (f) percentages of participants who identified as heterosexual, gay and bisexual, and (g) percentage of participants with a pre-existing health condition (e.g., HIV, heart disease).
We further coded factors related to the intervention participants. We coded reports for (a) the specific sample targeted in the intervention (e.g., college students, people who inject drugs), and recoded this variable to indicate whether the intervention targeted a population that was alcohol / drug dependent, (b) whether the intervention was targeted to an ethnic minority group, (c) whether the intervention was targeted to a specific gender group, and (d) whether the sample was self-selected, indicated by whether participation in the intervention was voluntary or whether the study conducted with a captive audience (e.g., prison inmates).
Intervention characteristics.
Finally, we coded for characteristics of the intervention programs, including (a) whether participants were randomly assigned and (b) the mean number of days between the intervention and posttest. We also coded for factors related to the implementation of these interventions. Specifically, we classified each intervention group according to (a) where participants were recruited (e.g., drug treatment facility, social service agency), and recoded this variable to describe a hospital/clinic setting vs. a non-hospital/clinic setting, (b) whether the facilitator was a professional (e.g., physician, nurse, social workers, licensed counselors) or lay community member (e.g., community leaders and peers), (c) whether the intervention was delivered in a group setting, to individuals, or a combination of the two, (d) the exposure format (e.g., radio, brochure), which was recoded as face-to-face vs. other formats, (e) the exposure setting (e.g., school, community), and (f) clinic vs. non-clinic setting. We also determined (g) whether the intervention was designed to be culturally specific or generic, (h) whether the intervention made use of active (e.g., behavioral skills training) vs. passive (e.g., informational arguments) strategies, (i) whether the intervention relied on attitudinal elements (e.g., attitudinal arguments, threat arguments), motivational elements (e.g., feedback, encouragement), or skills training elements (e.g., role-playing, goal setting), (j) whether the intervention included biological methods (e.g., use of nicotine patches, methadone), and (k) whether the intervention include a written behavioral contract.
Data Analytic Plan
To obtain effect sizes from the mean scores we subtracted the mean at posttest from the mean at pretest and divided it by the pooled standard deviation. To get effect sizes from proportions, we calculated the odds ratio and divided its natural log by 1.81 to convert it into Cohen’s d as outlined by Chinn (2000). For cases in which the proportion was equal to 0 or 1 at either posttest or pretest, we applied the correction from Sweeting, Sutton, and Lambert (2004), which involved adding 0.005 to (or subtracting 0.005 from) both pretest and posttest scores. Because the correlation between the pre-test and post-test measures is nor reported, we set this correlation constantly as r = .5. We note, however, that supplementary analyses were conducted with r = .8, as s sensitivity analysis, and all our conclusions remained the same. Hedges and Olkin’s (1985) correction factor was applied to all effect sizes to correct for small sample size bias. Reverse factors were applied to all the effect sizes so that a positive effect size always showed improvement, whereas a negative effect size showed worsening in the targeted health outcome.
For reports that included multiple outcomes or multiple measurements for one outcome (e.g., substance use, alcohol use), we kept all the effect sizes in the final analyses and used the robust variance estimate to deal with the dependency among correlated effect sizes obtained from the same study (Tanner-Smith et al., 2016).
Most data analysis was conducted using RVE (i.e. robust variance estimate) meta-regression in the statistical program R (Tanner-Smith & Tipton, 2014). R was also used to generate a funnel plot and run trim and fill analysis to gauge publication bias. Due to high levels of heterogeneity (I2 = 0.953), we used only random-effect models for all analyses. That is, the effect sizes were weighted by the inverse of their sampling variance plus a random variance component.
Results & Discussion
Description of Sample
We included 69 reports, resulting in 155 research groups and 233 effect sizes. Among the 155 research groups, 103 groups recommended multiple behaviors, 20 groups recommended a single behavior, and 22 groups did not recommend any behavior. The number of recommendations in the synthesized studies ranged from 0 to 11. When only counting the main recommendations, 87 groups included more than one main recommendation, 44 groups included one main recommendation, and 24 groups did not include any main recommendation. Of the 155 groups, 106 included outcomes on alcohol use and 86 included outcomes on drug use. The total number of participants included in this meta-analysis was 28,295.
A summary of the demographic characteristics, intervention set-up details, and participants information appears in Supplementary Table 2. As can be seen, most of the reports included in this meta-analysis were journal articles, published around 2011, and conducted in the United States. The samples included both males (56%) and females (44%), who, on average, were in their mid-thirties. On average1, 37% of participants were gay or bisexual (k = 31), 61% had completed high school (k = 80), 57% had a risk factor or health condition at baseline (k = 51), 48% were European-American (k = 121), 28% were African-American (k = 112), 86% were randomly assigned to conditions (k = 155), and 85% voluntarily participated in the interventions (k = 151). Among all interventions, 83% were delivered face-to-face (k = 126), 25% were delivered to groups (k = 136), 53% were delivered to individuals (k = 136), 87% used professional experts as facilitators (k =155), 26% targeted alcohol / drug dependent populations (k = 155), 6% targeted a specific at-risk ethnic group (k = 155), 24% targeted a specific gender (k = 148), and only 8% were described by the authors as culturally appropriate (k = 155).
Average Intervention Effect Size
Overall, there were significant improvements in the studied samples. The grand average for change over time was d = 0.42 (CI = [0.34, 0.50], p < .001, k = 233, I2 = 0.953), which was close to a medium effect2. Comparing the efficacy of multi-behavior interventions to that of previous intervention programs on substance use (Table 1), multi-behavior interventions performed better than most of the intervention programs that have been examined in the past. When separating alcohol and drug use outcomes, the average change on alcohol use outcomes over time was d = 0.31 (CI = [0.24, 0.38], p < .001, k = 118, I2 = 0.892). The average change on drug use outcomes over time was d = 0.53 (CI = [0.39, 0.67], p < .001, k = 91, I2 = 0.972). Multi-behavior interventions led to significantly more change on drug use outcomes than on alcohol use outcomes (B = 0.245, SE = 0.079, p = .002).
Optimal number of Recommendations
Our objective was to estimate the association between number of recommendations and change. To test for the linear and quadratic predictions between number of behavioral recommendations and intervention efficacy, we first ran an RVE (i.e. robust variance estimate) meta-regression analysis of overall efficacy on number of recommendations, including mean-centered linear and quadratic terms in the model. As shown in Table 2a, the linear term was significant (B = 0.073, SE = 0.016, p < .001) but the quadratic term was not (B = 0, SE = 0.007, p > .05). This pattern replicated for both alcohol use outcomes alone (Linear: B = 0.046, SE = 0.017, p < .05) and drug use outcomes alone (Linear: B = 0.085, SE = 0.025, p < .01). To better understand the effect of the main intervention recommendations, we counted only the main recommendations and reran the above regression analysis. The patterns were mostly similar to the previous analysis. For overall outcomes, the linear term was significant (B = 0.129, SE = 0.031, p < .001) but the quadratic term was not (B = 0.022, SE = 0.023, p > .05). This pattern replicated for drug-use outcomes alone (Linear: B = 0.182, SE = 0.080, p < .05) but not for alcohol-use outcomes alone (Linear: B = 0.042, SE = 0.024, p > .05).
Table 2a.
Summaries of the Meta-Regression Analysis for Change with Robust Variance Estimate (Correlation between Pre- and Post-Score Set as 0.5)
| Estimated coefficients? (Standard error) | |||
|---|---|---|---|
| Overall Outcome Change (k = 233) |
Alcohol Use Change (k = 118) |
Drug Use Change (k = 91) |
|
| All recommendations included | |||
| Recommendation number linear | 0.073 (0.016) *** | 0.046 (0.017) * | 0.085 (0.025) ** |
| Recommendation number squared | 0.000 (0.007) | −0.002 (0.003) | −0.005 (0.011) |
| Only main recommendations included | |||
| Recommendation number linear | 0.129 (0.031) *** | 0.042 (0.024) | 0.182 (0.080) * |
| Recommendation number squared | 0.022 (0.023) | 0.021 (0.026) | −0.003 (0.074) |
p < .05
p < .01
p < .001.
k is the total number of effect sizes included.
Knowing that underestimation of the pre-post correlation can lead to potential errors in estimation of the effect (Cuijpers et al., 2017), we changed the correlation between the pre and post measures from 0.5 to 0.8 and rerun the above meta-regression, as a sensitivity analysis. As shown in Table 2b, changing the correlation between the pre and post measures only changed the numerical value of the estimated effect but did not change the overall linear pattern between number of recommendation and the intervention efficacy. This pattern replicated for both alcohol and drug use outcomes and for both main and auxiliary recommendations.
Table 2b.
Summaries of the Meta-Regression Analysis for Change with Robust Variance Estimate (Correlation between Pre- and Post-Score Set as 0.8)
| Estimated coefficients β (Standard error) | |||
|---|---|---|---|
| Overall Outcome Change (k = 233) |
Alcohol Use Change (k = 118) |
Drug Use Change (k = 91) |
|
| All recommendations included | |||
| Recommendation number linear | 0.070 (0.015) *** | 0.045 (0.016) ** | 0.080 (0.025) ** |
| Recommendation number squared | 0.000 (0.007) | −0.003 (0.003) | −0.005 (0.010) |
| Only main recommendations included | |||
| Recommendation number linear | 0.125 (0.030) *** | 0.041 (0.023) | 0.177 (0.078) * |
| Recommendation number squared | 0.020 (0.022) | 0.020 (0.026) | −0.007 (0.074) |
p < .05
p < .01
p < .001.
k is the total number of effect sizes included.
To further describe an optimal number of recommendations, we calculated the mean change for each number of recommendations on all outcomes. Due to the small ks for interventions recommending 6 or more than 6 behaviors, we combined them all into one group as “6 & 6+ recommendations”. As shown in Panel A of Figure 3, the mean change steadily increased as the number of recommendations increased, with interventions recommending 6 or more than 6 recommendations bringing the largest change over time. The overall pattern of means is offered for descriptive purposes and further support the positive linear relation between number of recommendations and intervention efficacy that we formally tested in Table 2.
Figure 3.
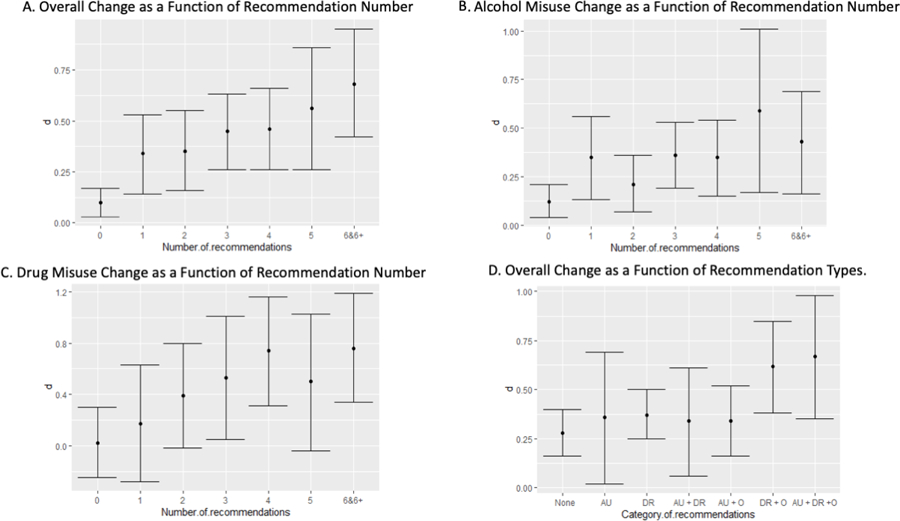
Findings for Number and Type of Recommendations. Note. AU = Alcohol Use; DR = Drug Use; O = Other Category
We then calculated the mean change for each number of recommendations for alcohol use outcomes and drug use outcomes separately. As shown in Panel B of Figure 3, the mean change for alcohol use outcomes did not change much as the number of recommendations increased beyond one, suggesting that a single recommendation might be sufficient in this case. In contrast, the mean change for drug use outcomes steadily increased as the number of recommendations increased and flattened out after 4, although the quadratic pattern was not significant (see Table 2). This pattern suggested that multiple recommendations were needed to maximize efficacy in drug interventions.
Overall, the results in Table 3 show a linear association between number of recommendations and intervention efficacy for our three measures of substance use outcomes. First, although the regression analysis shows a linear effect of number of recommendations on efficacy for alcohol use, Panel B of Figure 3 indicates little benefit in adding recommendations beyond one, suggesting that a single recommendation might be enough to change alcohol use behavior. In contrast, for drug use, recommending reducing drug use along with other behaviors is most efficacious. Regarding the number of included recommendations, intervention including four or more than four recommendations appeared to be most efficacious in changing drug use behavior. These patterns provide more support for the Relative Interdependence Model for drug use than for alcohol use.
Table 3.
Exploratory Moderator Analyses.
| Moderators | d [CI] | Estimated coefficients B (Standard error) |
k |
|---|---|---|---|
| Is the target group alcohol / drug dependent? | 0.230 (0.106) * | 233 | |
| Yes | 0.59 [0.37, 0.80] | 69 | |
| No | 0.36 [0.28, 0.43] | 164 | |
| Is the intervention delivered by experts? | 0.385 (0.106) ** | 110 | |
| Yes | 0.57 [0.33, 0.80] | 99 | |
| No | 0.18 [0.00, 0.36] | 11 | |
| Is there behavioral contract? | 0.726 (0.238) * | 233 | |
| Yes | 1.02 [0.52, 1.72] | 7 | |
| No | 0.39 [0.32, 0.47] | 226 | |
p < .05
p < .01.
k is the total number of effect sizes included.
Types of Recommendations
To better understand the impact of different types of recommendations included in the interventions and further test our hypothesized models (i.e., Relative Interdependence Modal and Relative Independence Model), we then calculated the mean change for different groups of interventions on overall outcomes based on the types of recommendations included. 3
If drug use is more dependent on alcohol use than alcohol use is on drug use, then the effects of interventions targeting both alcohol and drug use may be larger than those targeting alcohol use only. As shown in Panel D of Figure 3, however, the effects of interventions targeting both alcohol and drug use appeared to be similar to those targeting alcohol or drug use only. Still, we found that intervention efficacy was especially high when it included interventions recommending reducing both drug use and another behavior compared to only drug use. However, the efficacy of interventions recommending reducing alcohol use did not improve when paired with recommendations of other behaviors.
All in all, substance use outcomes improved more when drug recommendations were combined with at least one other recommendation, such as seeking service use and support seeking. This finding provides further support for the Relative Interdependence Model for drug use. Replicating the finding that alcohol-use outcomes changed equally in response to single- and multi-recommendation interventions, a single recommendation of alcohol use achieved roughly the same level of change as did combinations of alcohol use and other recommendations such as seeking service use or reducing drug use. This finding again supported the earlier finding (see Panels B and C at Figure 3) that alcohol use is relatively more independent from other related behaviors, compared to drug use.
Exploratory Moderator Analysis
We then conducted exploratory moderator analyses to determine whether participant or intervention characteristics were associated with efficacy. All analyses were conducted with the overall samples of conditions except for those with intervention characteristics as moderators, which pertained only to intervention groups. These analyses appear in Table 3 and showed three major significant moderators. Specifically, interventions were more efficacious when they targeted an alcohol / drug dependent population (d = 0.59, 95% CI = [0.37, 0.80], k = 69) than when they did not (d = 0.36, 95% CI = [0.28, 0.43], k = 164); when they were delivered by experts (d = 0.57, 95% CI = [0.33, 0.80], k = 99) than when they were not (d = 0.18, 95% CI = 0.00, 0.36], k = 11); and when they included a behavioral contract (d = 1.02, 95% CI = [0.52, 1.72], k = 7) than when they did not (d = 0.39, 95% CI = [0.32, 0.47], k = 226). The rest of the described moderators had no significant effect.
Testing the Linearity between Number of Recommendations and Efficacy after Controlling for Significant Moderators
We lastly tested whether number of recommendations predicted intervention efficacy above and beyond each of these predictors. Specifically, we conducted three multiple regression models, each including the number of recommendations and one of the three moderators above as the predictors. The linear term of number of recommendations was still significant after controlling for targeting drug / alcohol dependent population (B = 0.067, SE = 0.020, p < .01), expert delivery (B = 0.136, SE = 0.034, p < .001), and inclusion of behavioral contract (B = 0.067, SE = 0.020, p < .01). However, only expert delivery remained as a significant predictor after controlling for the number of recommendations included (B = 0.249, SE = 0.083, p < .05). Again, these findings confirmed the positive linear relationship between number of recommendations and intervention efficacy, showing the promising prospect of multi-behavior interventions in combating non-medical substance use.
Summary
In conclusion, our analyses revealed that multi-behavior interventions were efficacious at reducing non-medical substance use behaviors, especially for drug use behaviors. The data also suggested a linear association between the number of recommendations and change, such that the more behaviors recommended, the more efficacious the interventions were, particularly for drug use outcomes. This pattern held even after controlling for alcohol / drug dependent subpopulations, facilitators’ characteristics, and inclusion of behavioral contracts. Finally, we found strong support for the Relative Interdependence Model for drug use in relation to other behaviors, particularly seeking services that support recovery. In contrast, we found less support for the Relative Interdependence Model for alcohol use, which could be targeted more independently of other outcomes and achieve the same level of success as in combination with other outcomes.
Inclusion Bias
Finally, we assessed inclusion bias in multiple ways. First, we visually inspected the funnel plot of the effect size against the standard error (see Figure 4). If the distribution of effect sizes were unbiased, the plot should resemble a funnel, with studies with greater errors (assessed as smaller sample sizes) displaying greater variability (Sterne et al., 2006). Our plot revealed a bias suggesting that some positive effects were missing across different levels of precision. Therefore, we ran Egger’s test of asymmetry (Egger et al., 1997). For our data, the intercept for Egger’s test was 4.08 (p < .001), which suggested that there is asymmetry in the distribution of effect sizes. To address the asymmetry, we ran Duval and Tweedie’s (2000) trim and fill analysis. This method first fills in any missing effect sizes and then adds them to the analysis to recalculate an adjusted effect size corrected for observed biases (Rothstein, 2005). The trim and fill analysis (see Figure 4) added 43 studies to the right side, which moved our estimate from 0.42 (CI = [0.34, 0.50] to a new adjusted d = 0.53 (CI = [0.47, 0.60]) for the intervention groups, which remained significant. All the above analyses of bias indicated that our estimated effects were overly conservative and not affected by the usual publication bias that shows reluctance to publish negative effects. In this case, the synthesis appears to be missing positive effects.
Figure 4.
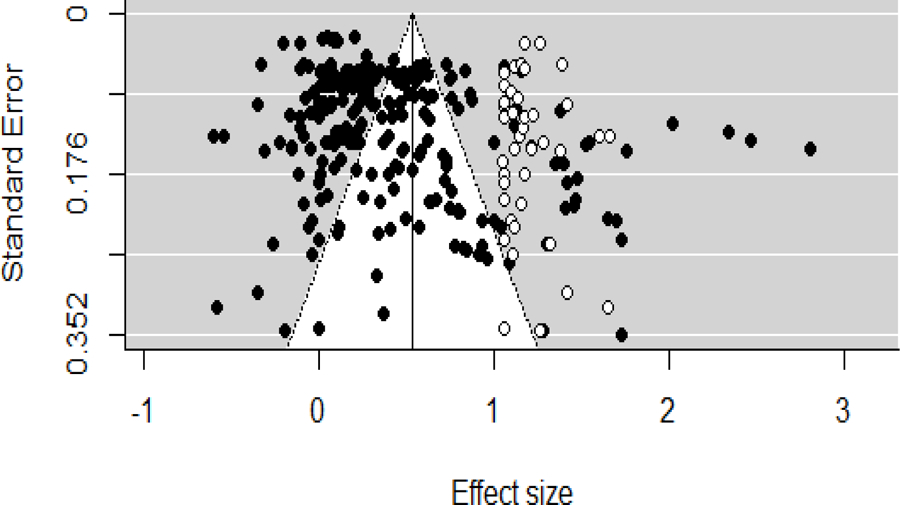
Funnel plot for inclusion bias analysis (dots added by trim and fill methods are shown in white).
Given the existing criticism of the above methods as lacking a statistical model and proper evaluation (McShane et al., 2016), we then applied the selection methods to further assess and adjust for publication biases relating to the statistical significance of effect sizes. Selection methods assume that the probability of publication depends on the p-value of its effect size. In other words, different p-values tend to have different chances of getting published and therefore being included in a meta-analysis (Hedges & Vevea, 1996; Vevea & Woods, 2005). Given that our dataset showed an untraditional bias against positive effects, we run a two-tailed sensitivity analysis for our dataset. Assuming a moderate two-tailed selection bias, the adjusted effect dropped to 0.39, which is a 0.03 reduction from the original effect size. Assuming a severe two-tailed selection bias, the adjusted effect turned into 0.36, which is a 0.06 reduction from the original effect size. These sensitivity analyses did suggest some potential bias, but the bias should have very little impact on our estimated effect sizes.
Altogether, the distribution of effect sizes in our meta-analysis was asymmetric. However, the asymmetry does not suggest exclusion of negative or non-significant effects. Instead, the asymmetry indicates that positive effects might be missing, which would then lead to overly conservative estimates of the efficacy of multi-behavior interventions. The sensitivity analyses also showed that, even assuming a severe bias, the observed effect remains significant. All in all, the observed bias is most likely due to the heterogeneity in the current dataset created by different methodological variables and unlikely to nullify our conclusions.
Conclusions
Overview of Findings
Given the rising rates of alcohol-related deaths and drug overdoses in the United States, understanding intervention efficacy in this domain is critical. Our study is the first to describe the body of evidence on multiple-behavior interventions for substance use. The majority of multi behavior programs analyzed in the current meta-analysis involved 2 or 3 recommendations targeting more than one behavioral domain, either alcohol use plus drug use, alcohol use plus one other domain (e.g. lifestyle, sexual behavior, service use), or drug use plus one other domain.
Our study showed that multi-behavior interventions were overall effective in reducing non-medical substance use, more so for drug use than for alcohol use. Our results also showed a general positive linear relation between number of recommendations and overall change, which was stronger for drug use outcomes and weaker for alcohol use outcomes. Regarding the type of included recommendations, we found that inclusion of recommendations for other behaviors increases the efficacy of drug use interventions but does not seem to improve the efficacy of alcohol use interventions. Altogether, these findings supported the notion that drug use often accompanies alcohol use (i.e., Relative Interdependence Model; see Figure 1), whereas alcohol use is more independent from drug use and other related behaviors (i.e., Relative Independence Model, see Figure 1). All in all, although the heterogeneity of the data caution against broad generalizations, multi-behavior interventions seemed better for drug use, whereas single-behavior interventions might be sufficient for alcohol use.
It is important to note that this linear pattern is different from the curvilinear pattern found by Wilson et al. (2015) in the lifestyle domain, suggesting that the optimal number of recommendations to be included in intervention programs differs across domains. Although three recommendations might be sufficient to change lifestyle related behaviors (e.g. exercising, smoking) and single recommendation might be sufficient to decrease alcohol use, more recommendations are necessary to reduce drug use. These findings surrounding the domain-specific optimal number of recommendations have important implications for the design of future intervention programs. Based on our findings, alcohol use can be treated as a relatively independent problem and an alcohol intervention program can simply target the alcohol use behavior itself (i.e. aiming to reduce the amount of alcohol consumed in the target population). In contrast, intervention programs to curb non-medical drug use need to consider the interconnections among the drug use behaviors and other related behaviors. For example, these interventions may benefit from determining all the substances that a patient is currently using and all the relevant behaviors that are leading to or relevant to the use of a specific substance (e.g., lack of social support, limited access to drug treatment program). Interventions may also benefit from including recommendations targeting all of these relevant behaviors, instead of just drug use. Accordingly, when reassessing patient behavior at a follow-up point, the interventionists should not limit the assessment to just drug use but instead measure the related behaviors and a more holistic improvement.
Lastly, our exploratory moderator analyses found participant and intervention characteristics that moderate the efficacy of interventions. Specifically, interventions were more efficacious when targeting an alcohol / drug dependent population, being delivered by experts, and including a behavioral contract. Number of recommendations still remained as a significant predictor after controlling for each of these predictors, but only expert delivery remained as a significant predictor after controlling for the number of recommendations. These results, if supported by further evidence from randomized controlled trials, may also provide important guideline for future interventions. For example, future intervention programs may invest more resources in the training of the facilitators to ensure their expertise in delivering the interventions.
Limitations and Future Work
There are a few limitations to be noted for the current meta-analysis. First of all, although we included both behavioral and clinical outcomes, most of the outcome measurements included in the current meta-analyses were behavioral (roughly 90 percent), due to the fact that most studies in the substance use domain rely solely on behavioral outcomes. Since most of the behavioral outcomes are measured through self-report, various problems can rise, such as social desirability bias and participants’ lack of knowledge about health behaviors (Newell et al., 1999). To enhance the generalizability of the current findings, future research should examine the impact of multi-behavior programs on clinical outcomes.
Next, although the intervention programs included in our synthesis covered a wide range of number of recommendations (i.e., 0–11), they did not assess all possible numbers of recommendations. Past research suggests that related behavioral recommendations might compete for resources and lead to a fatigue effect (Baumeister & Heatherton, 1996; Muraven et al., 1998; Vohs & Heatherton, 2000). Although this fatigue effect does not seem to appear in our studies with up to 11 recommendations, a higher number of recommendations could still be problematic. Therefore, future research should replicate the current meta-analytic study findings by examining future multi-behavioral interventions with more than 11 recommendations to determine the effect of higher numbers of recommendations.
Lastly, there are conflicting opinions on use of effect sizes that reflect change over time as posed to treatment-control conditions, although those apply primarily to the use of pre-post designs without controls (Cuijpers et al., 2017). Despite the validity of these arguments, we believe that the problem at hand required the chosen effect size. In addition, our findings were robust to changes in the estimated correlation between the pre- and post- measures from 0.5 to 0.8 as a sensitivity analysis. The additional analyses showed that any uncertainty about this correlation could influence the point estimation of the effect but is very unlikely to alter the primary conclusions from our study. Secondly, although it is true that it is hard to separate the intervention effect from the effect coming from natural processes, we are always comparing across conditions rather than relying on a single effect.
Closing Remarks
Designing more efficacious intervention programs is key to halting the current substance use crisis. This meta-analysis found a general positive linear relation between the number of recommendations and change, which was stronger for drug use programs than for alcohol use programs. This result ensures that multi-behavior interventions are promising methods to combat the current drug use epidemic and may be an effective solution through widespread implementation. Our analyses also showed that drug use interventions appeared to be more efficacious when also targeting other related behaviors, whereas alcohol use interventions can be efficacious enough when only targeting alcohol use itself. Additionally, this meta-analysis identified multiple moderators that can influence the efficacy of this particular type of promising intervention in the substance use domain. To maximize change, interventions should be delivered by experts, which imply the necessity of greater funding in the area of behavioral health and more training of health professionals. Lastly, the efficacy of multi-behavior programs seemed robust to differences in contexts and target populations, which makes the findings generalizable. Altogether, although more work still need to be done to reach confident conclusions about the optimal number and type of recommendations, our meta-analysis contributes to our understanding of multi-behavior programs in the substance use domain and has actionable implications for the development and implementation of future intervention programs, as well as policy surrounding them.
Supplementary Material
Acknowledgments
This research was supported by Grant R01 MH094241 (Dolores Albarracn) from the National Institute of Health.
Footnotes
The protocol of this research is described at: https://osf.io/gy2w7.
This research was presented at the Ninetieth Annual Meeting of Midwestern Psychological Association, Chicago, IL, 2018 by Wenhao Dai.
We have no known conflict of interest to disclose.
k referred to the number of conditions in which relevant information was reported. For example, only 22 groups reported percentage of gay or bisexual man, and 56% was the average percentage among these 22 groups.
According to Cohen’s tradition (Chen et al., 2010), d = 0.2 is considered a small effect, d = 0.5 is considered a moderate effect, d = 0.8 is considered a large effect. Therefore, the effect we found in the current meta is close to a moderate effect.
Due to the low power and low statistical efficiency, we were unable to examine the efficacy of different recommendations combinations on alcohol and drug use outcomes separately.
References
- Agosti V, Nunes E, & Levin F (2002). Rates of psychiatric comorbidity among U.S. residents with lifetime cannabis dependence. American Journal of Drug and Alcohol Abuse, 28(4), 643–652. 10.1081/ADA-120015873 [DOI] [PubMed] [Google Scholar]
- Aharonovich E, Stohl M, Cannizzaro D, & Hasin D (2017). HealthCall delivered via smartphone to reduce co-occurring drug and alcohol use in HIV-infected adults: A randomized pilot trial. Journal of Substance Abuse Treatment. 10.1016/j.jsat.2017.09.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Albarracín D, Gillette JC, Earl AN, Glasman LR, Durantini MR, & Ho MH (2005). A test of major assumptions about behavior change: A comprehensive look at the effects of passive and active HIV-prevention interventions since the beginning of the epidemic. Psychological Bulletin, 131(6), 856–897. 10.1037/0033-2909.131.6.856 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Albarracín D, Sunderrajan A, & Dai W (2018). Action, inaction, and actionability: Definitions and implications for communications and interventions to change behaviors. In Nebraska Symposium on Motivation (Vol. 65, pp. 75–99). 10.1007/978-3-319-96920-6_3 [DOI] [Google Scholar]
- Albarracín D, Sunderrajan A, Dai W, & White BX (2019). The social creation of action and inaction: From concepts to goals to behaviors. In Advances in Experimental Social Psychology. 10.1016/bs.aesp.2019.04.001 [DOI] [Google Scholar]
- Amaro H, Larson MJ, Zhang A, Acevedo A, Dai J, & Marsumoro A (2007). Effects of trauma intervention on HIV sexual risk behaviors among women with co-occurring disorders in substance abuse treatment. Journal of Community Psychology. 10.1002/jcop.20188 [DOI] [Google Scholar]
- Ammerman AS, Lindquist CH, Lohr KN, & Hersey J (2002). The efficacy of behavioral interventions to modify dietary fat and fruit and vegetable intake: A review of the evidence. Preventive Medicine. 10.1006/pmed.2002.1028 [DOI] [PubMed] [Google Scholar]
- Arnaud N, Diestelkamp S, Wartberg L, Sack PM, Daubmann A, & Thomasius R (2017). Short- to Midterm Effectiveness of a Brief Motivational Intervention to Reduce Alcohol Use and Related Problems for Alcohol Intoxicated Children and Adolescents in Pediatric Emergency Departments: A Randomized Controlled Trial. Academic Emergency Medicine. 10.1111/acem.13126 [DOI] [PubMed] [Google Scholar]
- Avants SK, Margolin A, Usubiaga MH, & Doebrick C (2004). Targeting HIV-related outcomes with intravenous drug users maintained on methadone: A randomized clinical trial of a harm reduction group therapy. Journal of Substance Abuse Treatment. 10.1016/S0740-5472(03)00159-4 [DOI] [PubMed] [Google Scholar]
- Ayala GX (2006). An experimental evaluation of a group- versus computer-based intervention to improve food portion size estimation skills. Health Education Research. 10.1093/her/cyh049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bachanas P, Kidder D, Medley A, Pals SL, Carpenter D, Howard A, Antelman G, DeLuca N, Muhenje O, Sheriff M, Somi G, Katuta F, Cherutich P, & Moore J (2016). Delivering Prevention Interventions to People Living with HIV in Clinical Care Settings: Results of a Cluster Randomized Trial in Kenya, Namibia, and Tanzania. AIDS and Behavior. 10.1007/s10461-016-1349-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baumeister RF, & Heatherton TF (1996). Self-Regulation Failure: An Overview. Psychological Inquiry. 10.1207/s15327965pli0701_1 [DOI] [Google Scholar]
- Benishek LA, Dugosh KL, Kirby KC, Matejkowski J, Clements NT, Seymour BL, & Festinger DS (2014). Prize-based contingency management for the treatment of substance abusers: A meta-analysis. In Addiction (Vol. 109, Issue 9, pp. 1426–1436). 10.1111/add.12589 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blodgett JC, Maisel NC, Fuh IL, Wilbourne PL, & Finney JW (2014). How effective is continuing care for substance use disorders? A meta-analytic review. Journal of Substance Abuse Treatment, 46(2), 87–97. 10.1016/j.jsat.2013.08.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borrell-Carrió F, Suchman AL, & Epstein RM (2004). The biopsychosocial model 25 years later: principles, practice, and scientific inquiry. Annals of Family Medicine, 2(6), 576–582. 10.1370/afm.245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boumparis N, Karyotaki E, Schaub MP, Cuijpers P, & Riper H (2017). Internet interventions for adult illicit substance users: a meta-analysis. In Addiction (Vol. 112, Issue 9, pp. 1521–1532). 10.1111/add.13819 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyer CB, Shafer MA, & Tschann JM (1997). Evaluation of a knowledge- and cognitive-behavioral skills-building intervention to prevent STDs and HIV infection in high school students. Adolescence. [PubMed] [Google Scholar]
- Brendryen H, Johansen A, Duckert F, & Nesvåg S (2017). A Pilot Randomized Controlled Trial of an Internet-Based Alcohol Intervention in a Workplace Setting. International Journal of Behavioral Medicine. 10.1007/s12529-017-9665-0 [DOI] [PubMed] [Google Scholar]
- Burke V, Beilin LJ, Cutt HE, Mansour J, Wilson A, & Mori TA (2005). Effects of a lifestyle programme on ambulatory blood pressure and drug dosage in treated hypertensive patients: A randomized controlled trial. Journal of Hypertension. 10.1097/01.hjh.0000170388.61579.4f [DOI] [PubMed] [Google Scholar]
- Burton LC, Paglia MJ, German PS, Shapiro S, & Damiano AM (1995). The effect among older persons of a general preventive visit on three health behaviors: Smoking, excessive alcohol drinking, and sedentary lifestyle. Preventive Medicine. 10.1006/pmed.1995.1078 [DOI] [PubMed] [Google Scholar]
- Caldwell DM, Ades AE, & Higgins JPT (2005). Simultaneous comparison of multiple treatments: Combining direct and indirect evidence. In British Medical Journal. 10.1136/bmj.331.7521.897 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calsyn DA, Crits-Christoph P, Hatch-Maillette MA, Doyle SR, Song YS, Coyer S, & Pelta S (2010). Reducing sex under the influence of drugs or alcohol for patients in substance abuse treatment. Addiction. 10.1111/j.1360-0443.2009.02812.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carney T, & Myers B (2012). Effectiveness of early interventions for substance-using adolescents: Findings from a systematic review and meta-analysis. In Substance Abuse: Treatment, Prevention, and Policy (Vol. 7). 10.1186/1747-597X-7-25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carrico AW, Nation A, Gómez W, Dilworth SE, Johnson MO, Moskowitz JT, Rose CD, & Sundberg J (2015). Pilot Trial of an Expressive Writing Intervention with HIV-Positive Methamphetamine-Using Men Who Have Sex with Men. In Psychology of Addictive Behaviors. 10.1037/adb0000031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen H, Cohen P, & Chen S (2010). How big is a big odds ratio? Interpreting the magnitudes of odds ratios in epidemiological studies. Communications in Statistics: Simulation and Computation. 10.1080/03610911003650383 [DOI] [Google Scholar]
- Chinn S (2000). A simple method for converting an odds ratio to effect size for use in meta-analysis. Statistics in Medicine, 19(22), 3127–3131. [DOI] [PubMed] [Google Scholar]
- Choo EK, Zlotnick C, Strong DR, Squires DD, Tapé C, & Mello MJ (2016). BSAFER: A Web-based intervention for drug use and intimate partner violence demonstrates feasibility and acceptability among women in the emergency department. Substance Abuse. 10.1080/08897077.2015.1134755 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuijpers P, Weitz E, Cristea IA, & Twisk J (2017). Pre-post effect sizes should be avoided in meta-analyses. Epidemiology and Psychiatric Sciences. 10.1017/S2045796016000809 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dakof GA, Cohen JB, Henderson CE, Duarte E, Boustani M, Blackburn A, Venzer E, & Hawes S (2010). A randomized pilot study of the Engaging Moms Program for family drug court. Journal of Substance Abuse Treatment. 10.1016/j.jsat.2010.01.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson DA (2000). Drinking as a risk factor for sustained smoking. Drug and Alcohol Dependence, 59(3), 235–249. 10.1016/S0376-8716(99)00130-1 [DOI] [PubMed] [Google Scholar]
- Deady M, Mills KL, Teesson M, & Kay-Lambkin F (2016). An online intervention for co-occurring depression and problematic alcohol use in young people: Primary outcomes from a randomized controlled trial. Journal of Medical Internet Research. 10.2196/jmir.5178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doumas DM, Esp S, Flay B, & Bond L (2017). A randomized controlled trial testing the efficacy of a brief online alcohol intervention for high school seniors. Journal of Studies on Alcohol and Drugs. 10.15288/jsad.2017.78.706 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doumas DM, Workman C, Smith D, & Navarro A (2011). Reducing high-risk drinking in mandated college students: Evaluation of two personalized normative feedback interventions. Journal of Substance Abuse Treatment. 10.1016/j.jsat.2010.12.006 [DOI] [PubMed] [Google Scholar]
- Durantini MR, Albarracin D, Mitchell AL, Earl AN, & Gillette JC (2006). Conceptualizing the influence of social agents of behavior change: A meta-analysis of the effectiveness of HIV-prevention interventionists for different groups. Psychological Bulletin, 132(2), 212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dushay RA, Singer M, Weeks MR, Rohena L, & Gruber R (2001). Lowering HIV risk among ethnic minority drug users: Comparing culturally targeted intervention to a standard intervention. American Journal of Drug and Alcohol Abuse. 10.1081/ADA-100104515 [DOI] [PubMed] [Google Scholar]
- Duval S, & Tweedie R (2000). Trim and fill: a simple funnel- plot–based method of testing and adjusting for publication bias in meta-analysis. Biometrics, 56(2), 455–463. 10.1111/j.0006-341x.2000.00455.x [DOI] [PubMed] [Google Scholar]
- Ebrahim S, Beswick A, Burke M, & Davey Smith G (2006). Multiple risk factor interventions for primary prevention of coronary heart disease. In Cochrane Database of Systematic Reviews. 10.1002/14651858.cd001561.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egger M, Davey Smith G, Schneider M, Minder C, Mulrow C, Egger M, Smith GD, Eysenck H, Egger M, Zellweger-Zähner T, Schneider M, Junker C, Lengeler C, Antes G, Egger M, Smith GD, Light R, Pillemer D, Villar J, … Olkin I (1997). Bias in meta-analysis detected by a simple, graphical test. British Medical Journal (Clinical Research Ed.), 315(7109), 629–634. 10.1136/bmj.315.7109.629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fischer B, Blanken P, Da Silveira D, Gallassi A, Goldner EM, Rehm J, Tyndall M, & Wood E (2015). Effectiveness of secondary prevention and treatment interventions for crack-cocaine abuse: A comprehensive narrative overview of English-language studies. In International Journal of Drug Policy. 10.1016/j.drugpo.2015.01.002 [DOI] [PubMed] [Google Scholar]
- Fogel CI, Crandell JL, Neevel AM, Parker SD, Carry M, White BL, Fasula AM, Herbst JH, & Gelaude DJ (2015). Efficacy of an adapted HIV and sexually transmitted infection prevention intervention for incarcerated women: A randomized controlled trial. American Journal of Public Health. 10.2105/AJPH.2014.302105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman GD, Tekawa I, Klatsky AL, Sidney S, & Armstrong MA (1991). Alcohol drinking and cigarette smoking: an exploration of the association in middle-aged men and women. Drug and Alcohol Dependence, 27(3), 283–290. 10.1016/0376-8716(91)90011-M [DOI] [PubMed] [Google Scholar]
- Fromme K, & Corbin W (2004). Prevention of heavy drinking and associated negative consequences among mandated and voluntary college students. Journal of Consulting and Clinical Psychology. 10.1037/0022-006X.72.6.1038 [DOI] [PubMed] [Google Scholar]
- Glenny AM, Altman DG, Song F, Sakarovitch C, Deeks JJ, D’Amico R, Bradburn M, & Eastwood AJ (2005). Indirect comparisons of competing interventions. In Health Technology Assessment. 10.3310/hta9260 [DOI] [PubMed] [Google Scholar]
- Go VF, Frangakis C, Minh N Le, Latkin C, Ha TV, Mo TT, Sripaipan T, Davis WW, Zelaya C, Vu PT, Celentano DD, & Quan VM (2015). Efficacy of a Multi-level Intervention to Reduce Injecting and Sexual Risk Behaviors among HIV-Infected People Who Inject Drugs in Vietnam: A Four-Arm Randomized Controlled Trial. PLoS ONE. 10.1371/journal.pone.0125909 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grossbard JR, Mastroleo NR, Kilmer JR, Lee CM, Turrisi R, Larimer ME, & Ray A (2010). Substance use patterns among first-year college students: Secondary effects of a combined alcohol intervention. Journal of Substance Abuse Treatment. 10.1016/j.jsat.2010.07.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hadley W, Brown LK, Barker D, Warren J, Weddington P, Fortune T, & Juzang I (2016). Work It Out Together: Preliminary Efficacy of a Parent and Adolescent DVD and Workbook Intervention on Adolescent Sexual and Substance Use Attitudes and Parenting Behaviors. AIDS and Behavior. 10.1007/s10461-016-1418-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haller DM, Meynard A, Lefebvre D, Ukoumunne OC, Narring F, & Broers B (2014). Effectiveness of training family physicians to deliver a brief intervention to address excessive substance use among young patients: A cluster randomized controlled trial. CMAJ. 10.1503/cmaj.131301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanson T, Alessi SM, & Petry NM (2008). Contingency management reduces drug-related human immunodeficiency virus risk behaviors in cocaine-abusing methadone patients. Addiction. 10.1111/j.1360-0443.2008.02216.x [DOI] [PubMed] [Google Scholar]
- Hardcastle SJ, Taylor AH, Bailey MP, Harley RA, & Hagger MS (2013). Effectiveness of a motivational interviewing intervention on weight loss, physical activity and cardiovascular disease risk factors: A randomised controlled trial with a 12-month post-intervention follow-up. International Journal of Behavioral Nutrition and Physical Activity. 10.1186/1479-5868-10-40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hedegaard H, Warner M, & Miniño AM (2017). Drug Overdose Deaths in the United States, 1999–2015. NCHS Data Brief, 2010(273), 1–8. https://www.cdc.gov/nchs/data/databriefs/db273.pdf [PubMed] [Google Scholar]
- Hedges LV, & Olkin I (1985). Statistical methods for meta-analysis. Phytochemistry, 72(13), 369 10.1016/j.phytochem.2011.03.026 [DOI] [Google Scholar]
- Hedges LV, & Vevea JL (1996). Estimating Effect Size under Publication Bias: Small Sample Properties and Robustness of a Random Effects Selection Model. Journal of Educational and Behavioral Statistics. 10.3102/10769986021004299 [DOI] [Google Scholar]
- Helzer JE, & Pryzbeck TR (1988). The co-occurrence of alcoholism with other psychiatric disorders in the general population and its impact on treatment. Journal of Studies on Alcohol, 49(3), 219–224. 10.15288/jsa.1988.49.219 [DOI] [PubMed] [Google Scholar]
- Hershberger SL, Wood MM, & Fisher DG (2003). A cognitive-behavioral intervention to reduce HIV risk behaviors in crack and injection drug users. AIDS and Behavior. 10.1023/A:1025487501743 [DOI] [PubMed] [Google Scholar]
- Hien DA, Wells EA, Jiang H, Suarez-Morales L, Campbell ANC, Cohen LR, Miele GM, Killeen T, Brigham GS, Zhang Y, Hansen C, Hodgkins C, Hatch-Maillette M, Brown C, Kulaga A, Kristman-Valente A, Chu M, Sage R, Robinson JA, … Nunes EV (2009). Multisite Randomized Trial of Behavioral Interventions for Women With Co-Occurring PTSD and Substance Use Disorders. Journal of Consulting and Clinical Psychology. 10.1037/a0016227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ingersoll KS, Farrell-Carnahan L, Cohen-Filipic J, Heckman CJ, Ceperich SD, Hettema J, & Marzani-Nissen G (2011). A pilot randomized clinical trial of two medication adherence and drug use interventions for HIV+ crack cocaine users. Drug and Alcohol Dependence. 10.1016/j.drugalcdep.2010.12.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones A, McGrath E, Robinson E, Houben K, Nederkoorn C, & Field M (2018). A Randomized Controlled Trial of Inhibitory Control Training for the Reduction of Alcohol Consumption in Problem Drinkers. Journal of Consulting and Clinical Psychology. 10.1037/ccp0000312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jungerman FS, Andreoni S, & Laranjeira R (2007). Short term impact of same intensity but different duration interventions for cannabis users. Drug and Alcohol Dependence. 10.1016/j.drugalcdep.2007.02.019 [DOI] [PubMed] [Google Scholar]
- Kaner E, Bland M, Cassidy P, Coulton S, Dale V, Deluca P, Gilvarry E, Godfrey C, Heather N, Myles J, Newbury-Birch D, Oyefeso A, Parrott S, Perryman K, Phillips T, Shepherd J, & Drummond C (2013). Effectiveness of screening and brief alcohol intervention in primary care (SIPS trial): Pragmatic cluster randomised controlled trial. In BMJ (Online). 10.1136/bmj.e8501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kulesza M, Apperson M, Larimer ME, & Copeland AL (2010). Brief alcohol intervention for college drinkers: How brief is? Addictive Behaviors. 10.1016/j.addbeh.2010.03.011 [DOI] [PubMed] [Google Scholar]
- Kypri K, & McAnally HM (2005). Randomized controlled trial of a web-based primary care intervention for multiple health risk behaviors. Preventive Medicine. 10.1016/j.ypmed.2005.07.010 [DOI] [PubMed] [Google Scholar]
- Latkin CA, Donnell D, Metzger D, Sherman S, Aramrattna A, Davis-Vogel A, Quan VM, Gandham S, Vongchak T, Perdue T, & Celentano DD (2009). The efficacy of a network intervention to reduce HIV risk behaviors among drug users and risk partners in Chiang Mai, Thailand and Philadelphia, USA. Social Science and Medicine. 10.1016/j.socscimed.2008.11.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leeman RF, Corbin WR, Nogueira C, Krishnan-Sarin S, Potenza MN, & O’Malley SS (2013). A human alcohol self-administration paradigm to model individual differences in impaired control over alcohol use. Experimental and Clinical Psychopharmacology. 10.1037/a0033438 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Letourneau EJ, McCart MR, Sheidow AJ, & Mauro PM (2017). First Evaluation of a Contingency Management Intervention Addressing Adolescent Substance Use and Sexual Risk Behaviors: Risk Reduction Therapy for Adolescents. Journal of Substance Abuse Treatment. 10.1016/j.jsat.2016.08.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis CF, Rivera AV, Crawford ND, DeCuir J, & Amesty S (2015). Pharmacy-randomized intervention delivering HIV prevention services during the syringe sale to people who inject drugs in New York City. Drug and Alcohol Dependence. 10.1016/j.drugalcdep.2015.06.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Litt MD, Kadden RM, & Kabela-Cormier E (2009). Individualized assessment and treatment program for alcohol dependence: Results of an initial study to train coping skills. Addiction. 10.1111/j.1360-0443.2009.02693.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Livingston NA, Oost KM, Heck NC, & Cochran BN (2015). The Role of Personality in Predicting Drug and Alcohol Use among Sexual Minorities. In Psychology of Addictive Behaviors (Vol. 29, Issue 2, pp. 414–419). 10.1037/adb0000034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lumley T (2002). Network meta-analysis for indirect treatment comparisons. Statistics in Medicine. 10.1002/sim.1201 [DOI] [PubMed] [Google Scholar]
- Magill M, & Ray L (2009). Cognitive-behavioral treatment with adult alcohol and illicit drug users: a meta-analysis of randomized controlled trials. Journal of Studies on Alcohol and Drugs, 70(4), 516–527. http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=2696292&tool=pmcentrez&rendertype=abstract%5Cnhttp://www.ncbi.nlm.nih.gov/pmc/articles/pmc2696292/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martín J, Sabugal GM, Rubio R, Sainz-Maza M, Blanco JM, Alonso JL, & Domínguez J (2001). Outcomes of a health education intervention in a sample of patients infected by HIV, most of them injection drug users: Possibilities and limitations. AIDS Care-Psychological and Socio-Medical Aspects of AIDS/HIV. 10.1080/09540120120057996 [DOI] [PubMed] [Google Scholar]
- McCusker J, Bigelow C, Frost R, Garfield F, Hindin R, Vickers-Lahti M, & Lewis B (1997). The effects of planned duration of residential drug abuse treatment on recovery and HIV risk behavior. American Journal of Public Health. 10.2105/AJPH.87.10.1637 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMahon RC, Malow RM, Jennings TE, & Gomez CJ (2001). Effects of a cognitive-behavioral HIV prevention intervention among HIV negative male substance abusers in VA residential treatment. AIDS Education and Prevention. 10.1521/aeap.13.1.91.18921 [DOI] [PubMed] [Google Scholar]
- McShane BB, Böckenholt U, & Hansen KT (2016). Adjusting for Publication Bias in Meta-Analysis: An Evaluation of Selection Methods and Some Cautionary Notes. Perspectives on Psychological Science. 10.1177/1745691616662243 [DOI] [PubMed] [Google Scholar]
- Meade CS, Drabkin AS, Hansen NB, Wilson PA, Kochman A, & Sikkema KJ (2010). Reductions in alcohol and cocaine use following a group coping intervention for HIV-positive adults with childhood sexual abuse histories. Addiction. 10.1111/j.1360-0443.2010.03075.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monti PM, Mastroleo NR, Barnett NP, Colby SM, Kahler CW, & Operario D (2016). Brief Motivational Intervention to Reduce Alcohol and HIV/Sexual Risk Behavior in Emergency Department Patients: A Randomized Controlled Trial. Journal of Consulting and Clinical Psychology. 10.1037/ccp0000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mouttapa M, Watson D, McCuller W, Reiber C, & Tsai W (2009). Substance Use and HIV Prevention for Youth in Correctional Facilities. Journal of Correctional Education. [Google Scholar]
- Muraven M, Tice DM, & Baumeister RF (1998). Self-Control as Limited Resource: Regulatory Depletion Patterns. Journal of Personality and Social Psychology. 10.1037/0022-3514.74.3.774 [DOI] [PubMed] [Google Scholar]
- Murphy JG, Duchnick JJ, Vuchinich RE, Davison JW, Karg RS, Olson AM, Smith AF, & Coffey TT (2001). Relative efficacy of a brief motivational intervention for college student drinkers. Psychology of Addictive Behaviors. 10.1037/0893-164X.15.4.373 [DOI] [PubMed] [Google Scholar]
- Nemoto T, Operario D, & Soma T (2002). Risk behaviors of Filipino methamphetamine users in San Francisco: Implications for prevention and treatment of drug use and HIV. Public Health Reports. [PMC free article] [PubMed] [Google Scholar]
- Newell S. a, Girgis a, Sanson-Fisher RW, & Savolainen NJ (1999). The accuracy of self-reported health behaviors and risk factors relating to cancer and cardiovascular disease in the general population: a critical review. American Journal of Preventive Medicine, 17(3), 211–229. [DOI] [PubMed] [Google Scholar]
- O’Farrell TJ, Schumm JA, Dunlap LJ, & Murphy MM (2016). A randomized clinical trial of group versus standard behavioral couples therapy plus individually based treatment for patients with alcohol dependence. Journal of Consulting and Clinical Psychology. 10.1037/ccp0000089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parsons JT, Lelutiu-Weinberger C, Botsko M, & Golub SA (2014). A randomized controlled trial utilizing motivational interviewing to reduce HIV risk and drug use in young gay and bisexual men. Journal of Consulting and Clinical Psychology. 10.1037/a0035311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penberthy JK, Hook JN, Hettema J, Farrell-Carnahan L, & Ingersoll K (2013). Depressive symptoms moderate treatment response to brief intervention for prevention of alcohol exposed pregnancy. Journal of Substance Abuse Treatment. 10.1016/j.jsat.2013.05.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perry CL, Komro KA, Veblen-Mortenson S, Bosma LM, Farbakhsh K, Munson KA, Stigler MH, & Lytle LA (2003). A randomized controlled trial of the middle and junior high school D.A.R.E. and D.A.R.E. Plus programs. Archives of Pediatrics and Adolescent Medicine. 10.1001/archpedi.157.2.178 [DOI] [PubMed] [Google Scholar]
- Prado G, Cordova D, Huang S, Estrada Y, Rosen A, Bacio GA, Leon Jimenez G, Pantin H, Brown CH, Velazquez MR, Villamar J, Freitas D, Tapia MI, & McCollister K (2012). The efficacy of Familias Unidas on drug and alcohol outcomes for Hispanic delinquent youth: Main effects and interaction effects by parental stress and social support. Drug and Alcohol Dependence. 10.1016/j.drugalcdep.2012.06.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prendergast ML, Podus D, Chang E, & Urada D (2002). The effectiveness of drug abuse treatment: A meta-analysis of comparison group studies. Drug and Alcohol Dependence, 67(1), 53–72. 10.1016/S0376-8716(02)00014-5 [DOI] [PubMed] [Google Scholar]
- Prendergast M, Podus D, Finney J, Greenwell L, & Roll J (2006). Contingency management for treatment of substance use disorders: A meta-analysis. In Addiction (Vol. 101, Issue 11, pp. 1546–1560). 10.1111/j.1360-0443.2006.01581.x [DOI] [PubMed] [Google Scholar]
- Prevention C for D. C. and. (2016). Fact Sheets - Alcohol Use and Your Health. [Google Scholar]
- Prochaska JJ, Spring B, & Nigg CR (2008). Multiple health behavior change research: An introduction and overview. In Preventive Medicine (Vol. 46, Issue 3, pp. 181–188). 10.1016/j.ypmed.2008.02.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Purcell DW, Latka MH, Metsch LR, Latkin CA, Gómez CA, Mizuno Y, Arnsten JH, Wilkinson JD, Knight KR, Knowlton AR, Santibanez S, Tobin KE, Dawson Rose C, Valverde EE, Gourevitch MN, Eldred L, & Borkowf CB (n.d.). Results From a Randomized Controlled Trial of a Peer-Mentoring Intervention to Reduce HIV Transmission and Increase Access to Care and Adherence to HIV Medications Among HIV-Seropositive Injection Drug Users. [DOI] [PubMed] [Google Scholar]
- Reback CJ, Peck JA, Dierst-Davies R, Nuno M, Kamien JB, & Amass L (2010). Contingency management among homeless, out-of-treatment men who have sex with men. Journal of Substance Abuse Treatment. 10.1016/j.jsat.2010.06.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Regier DA, Farmer ME, Rae DS, Locke BZ, Keith SJ, Judd LL, & Goodwin FK (1990). Comorbidity of Mental Disorders With Alcohol and Other Drug Abuse: Results From the Epidemiologic Catchment Area (ECA) Study. JAMA: The Journal of the American Medical Association, 264(19), 2511–2518. 10.1001/jama.1990.03450190043026 [DOI] [PubMed] [Google Scholar]
- Robles RR, Reyes JC, Colón HM, Sahai H, Marrero CA, Matos TD, Calderón JM, & Shepard EW (2004). Effects of combined counseling and case management to reduce HIV risk behaviors among Hispanic drug injectors in Puerto Rico: A randomized controlled study. Journal of Substance Abuse Treatment. 10.1016/j.jsat.2004.06.004 [DOI] [PubMed] [Google Scholar]
- Rongkavilit C, Naar-King S, Wang B, Panthong A, Bunupuradah T, Parsons JT, Phonphithak S, Koken JA, Saengcharnchai P, & Phanuphak P (2013). Motivational interviewing targeting risk behaviors for youth living with HIV in Thailand. AIDS and Behavior. 10.1007/s10461-013-0407-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothstein HR (2005). Publication Bias in Prevention, Assessment and Adjustments. In Assessment. 10.1002/0470870168 [DOI] [Google Scholar]
- Saitz R, Cheng DM, Winter M, Kim TW, Meli SM, Allensworth-Davies D, Lloyd-Travaglini CA, & Samet JH (2013). Chronic care management for dependence on alcohol and other drugs: The AHEAD randomized trial. JAMA - Journal of the American Medical Association. 10.1001/jama.2013.277609 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sakane N, Kotani K, Takahashi K, Sano Y, Tsuzaki K, Okazaki K, Sato J, Suzuki S, Morita S, Oshima Y, Izumi K, Kato M, Ishizuka N, Noda M, & Kuzuya H (2015). Effects of telephone-delivered lifestyle support on the development of diabetes in participants at high risk of type 2 diabetes: J-DOIT1, a pragmatic cluster randomised trial. BMJ Open. 10.1136/bmjopen-2014-007316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samet JH, Raj A, Cheng DM, Blokhina E, Bridden C, Chaisson CE, Walley AY, Palfai TP, Quinn EK, Zvartau E, Lioznov D, & Krupitsky E (2015). HERMITAGE-a randomized controlled trial to reduce sexually transmitted infections and HIV risk behaviors among HIV-infected Russian drinkers. Addiction. 10.1111/add.12716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santa Ana EJ, LaRowe SD, Armeson K, Lamb KE, & Hartwell K (2016). Impact of group motivational interviewing on enhancing treatment engagement for homeless Veterans with nicotine dependence and other substance use disorders: A pilot investigation. American Journal on Addictions. 10.1111/ajad.12426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santos GM, Coffin PO, Vittinghoff E, DeMicco E, Das M, Matheson T, Raiford JL, Carry M, Colfax G, Herbst JH, & Dilley JW (2014). Substance use and drinking outcomes in Personalized Cognitive Counseling randomized trial for episodic substance-using men who have sex with men. Drug and Alcohol Dependence. 10.1016/j.drugalcdep.2014.02.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Satre DD, Leibowitz A, Sterling SA, Lu Y, Travis A, & Weisner C (2016). A Randomized Clinical Trial of Motivational Interviewing to Reduce Alcohol and Drug Use among Patients with Depression. Journal of Consulting and Clinical Psychology. 10.1037/ccp0000096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sayegh CS, Huey SJ, Zara EJ, & Jhaveri K (2017). Follow-up treatment effects of contingency management and motivational interviewing on substance use: A meta-analysis. Psychology of Addictive Behaviors, 31(4), 403–414. 10.1037/adb0000277 [DOI] [PubMed] [Google Scholar]
- Lawrence JS St., Jefferson KW, Alleyne E, & Brasfield TL (1995). Comparison of education versus behavioral skills training interventions in lowering sexual HIV-risk behavior of substance-dependent adolescents. Journal of Consulting and Clinical Psychology. 10.1037/0022-006x.63.1.154 [DOI] [PubMed] [Google Scholar]
- Sterne JAC, Becker BJ, & Egger M (2006). The Funnel Plot. In Publication Bias in Meta-Analysis: Prevention, Assessment and Adjustments (pp. 73–98). 10.1002/0470870168.ch5 [DOI] [Google Scholar]
- Stinson FS, Grant BF, Dawson DA, Ruan WJ, Huang B, & Saha T (2005). Comorbidity between DSM-IV alcohol and specific drug use disorders in the United States: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. In Drug and Alcohol Dependence (Vol. 80, Issue 1, pp. 105–116). 10.1016/j.drugalcdep.2005.03.009 [DOI] [PubMed] [Google Scholar]
- Sunderrajan A (n.d.). No Magic Bullet or Complex Solutions to a Complex Problem: A Meta-Analysis of the Efficacy of Integrated Interventions on Change in Behavioral and Clinical Outcomes Related to HIV. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Surratt HL, & Inciardi JA (2010). An effective HIV risk-reduction protocol for drug-using female sex workers. Journal of Prevention and Intervention in the Community. 10.1080/10852351003640732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sweeting MJ, Sutton AJ, & Lambert PC (2004). What to add to nothing? Use and avoidance of continuity corrections in meta-analysis of sparse data. Statistics in Medicine, 23(9), 1351–1375. 10.1002/sim.1761 [DOI] [PubMed] [Google Scholar]
- Tanner-Smith EE, & Risser MD (2016). A meta-analysis of brief alcohol interventions for adolescents and young adults: variability in effects across alcohol measures. The American Journal of Drug and Alcohol Abuse, 42(2), 140–151. 10.3109/00952990.2015.1136638 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanner-Smith EE, & Tipton E (2014). Robust variance estimation with dependent effect sizes: Practical considerations including a software tutorial in Stata and SPSS. Research Synthesis Methods. 10.1002/jrsm.1091 [DOI] [PubMed] [Google Scholar]
- Tanner-Smith EE, Tipton E, & Polanin JR (2016). Handling Complex Meta-analytic Data Structures Using Robust Variance Estimates: a Tutorial in R. Journal of Developmental and Life-Course Criminology. 10.1007/s40865-016-0026-5 [DOI] [Google Scholar]
- Tucker JS, D’Amico EJ, Ewing BA, Miles JNV, & Pedersen ER (2017). A group-based motivational interviewing brief intervention to reduce substance use and sexual risk behavior among homeless young adults. Journal of Substance Abuse Treatment. 10.1016/j.jsat.2017.02.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vevea JL, & Woods CM (2005). Publication bias in research synthesis: Sensitivity analysis using a priori weight functions. Psychological Methods. 10.1037/1082-989X.10.4.428 [DOI] [PubMed] [Google Scholar]
- Vohs KD, & Heatherton TF (2000). Self-Regulatory Failure: A Resource-Depletion Approach. Psychological Science. 10.1111/1467-9280.00250 [DOI] [PubMed] [Google Scholar]
- Volkow ND, & Li TK (2005). Drugs and alcohol: Treating and preventing abuse, addiction and their medical consequences. In Pharmacology and Therapeutics. 10.1016/j.pharmthera.2005.06.021 [DOI] [PubMed] [Google Scholar]
- Wechsberg WM, Luseno WK, Lam WKK, Parry CDH, & Morojele NK (2006). Substance use, sexual risk, and violence: HIV prevention intervention with sex workers in pretoria. AIDS and Behavior. 10.1007/s10461-005-9036-8 [DOI] [PubMed] [Google Scholar]
- Wechsberg WM, Zule WA, El-Bassel N, Doherty IA, Minnis AM, Novak SD, Myers B, & Carney T (2016). The male factor: Outcomes from a cluster randomized field experiment with a couples-based HIV prevention intervention in a South African township. Drug and Alcohol Dependence. 10.1016/j.drugalcdep.2016.02.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wernette GT, Plegue M, Kahler CW, Sen A, & Zlotnick C (2018). A Pilot Randomized Controlled Trial of a Computer-Delivered Brief Intervention for Substance Use and Risky Sex during Pregnancy. Journal of Women’s Health. 10.1089/jwh.2017.6408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams EC, Lapham G, Achtmeyer CE, Volpp B, Kivlahan DR, & Bradley KA (2010). Use of an electronic clinical reminder for brief alcohol counseling is associated with resolution of unhealthy alcohol use at follow-up screening. Journal of General Internal Medicine. 10.1007/s11606-009-1100-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson K, Senay I, Durantini M, Sánchez F, Hennessy M, Spring B, & Albarracín D (2015). When it comes to lifestyle recommendations, more is sometimes less: A meta-analysis of theoretical assumptions underlying the effectiveness of interventions promoting multiple behavior domain change. Psychological Bulletin, 141(2), 474–509. 10.1037/a0038295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woolf SH, Krist AH, Johnson RE, Wilson DB, Rothemich SF, Norman GJ, & Devers KJ (2006). A practice-sponsored web site to help patients pursue healthy behaviors: An ACORN study. Annals of Family Medicine. 10.1370/afm.522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright JL, Sherriff JL, Dhaliwal SS, & Mamo JCL (2011). Tailored, iterative, printed dietary feedback is as effective as group education in improving dietary behaviours: Results from a randomised control trial in middle-aged adults with cardiovascular risk factors. International Journal of Behavioral Nutrition and Physical Activity. 10.1186/1479-5868-8-43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yonkers KA, Forray A, Howell HB, Gotman N, Kershaw T, Rounsaville BJ, & Carroll KM (2012). Motivational enhancement therapy coupled with cognitive behavioral therapy versus brief advice: A randomized trial for treatment of hazardous substance use in pregnancy and after delivery. General Hospital Psychiatry. 10.1016/j.genhosppsych.2012.06.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zule WA, Costenbader EC, Coomes CM, & Wechsberg WM (2009). Effects of a hepatitis C virus educational intervention or a motivational intervention on alcohol use, injection drug use, and sexual risk behaviors among injection drug users. American Journal of Public Health. 10.2105/AJPH.2007.126854 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


