A 57-year-old woman with Sjögren syndrome presented with acute onset right submandibular swelling and pain with associated fever and dysphagia. She had bilateral submandibular gland tenderness with palpable stones along the ducts. There was no fluctuance or erythema. Computed tomography revealed several stones in the bilateral submandibular ducts with right-sided sialoadenitis (Fig. 1a).
Fig. 1.
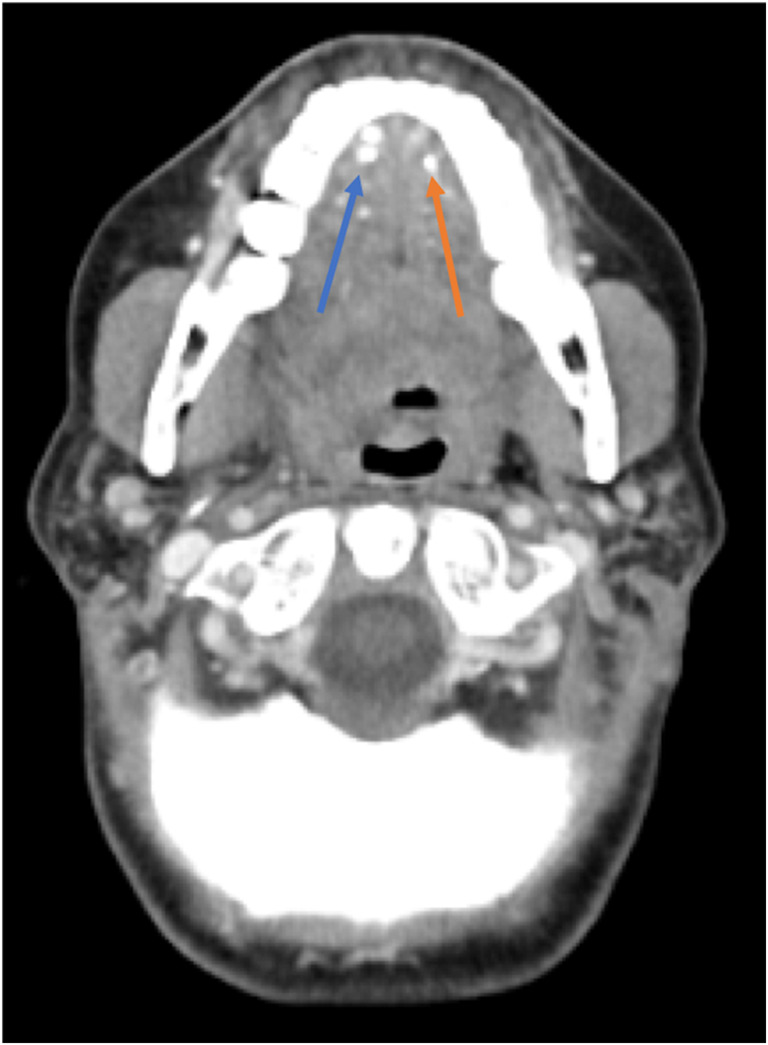

a Computed tomography with contrast revealed right submandibular sialoadenitis with at least 6 stones throughout its length (blue arrow), and left submandibular sialolithiasis without evidence of sialoadenitis (orange arrow). b Sialoliths that the patient expelled on day 4 of admission.
The differential diagnosis for painful salivary gland swelling includes stones, strictures, viral infections, and bacterial infections.1 History and physical exam are crucial for diagnosis, and can be aided with radiologic evaluation. Submandibular stones are most common due to longer duct length and salivary flow against gravity. Stones within the parotid and submandibular glands are managed similarly, and bilateral pathology does not change the treatment algorithm.2 A risk factor for secondary bacterial infections is stasis within the duct from sialolithiasis, with Staphylococcus aureus commonly responsible.1 Antistaphylococcal antibiotics are indicated for primary/secondary infection.3, 4 Sialolithiasis in patients with Sjögren syndrome is rarely reported.5, 6 As dehydration and decreased salivary production predispose patients to sialolithiasis, it follows that Sjögren syndrome may increase this risk.
The patient expelled two calculi from the right submandibular gland on day four of hospitalization (Fig. 1b). Her symptoms improved. She was discharged with 14 days of amoxicillin-clavulanate.
Compliance with Ethical Standards
Conflict of Interest
All authors have no conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Mandel L. Salivary gland disorders. Med Clin North Am. 2014;98:1407–49. doi: 10.1016/j.mcna.2014.08.008. [DOI] [PubMed] [Google Scholar]
- 2.Marchal F, Dulguerov P. Sialolithiasis management: the state of the art. Arch Otolaryngol Head Neck Surg. 2005;129:951–956. doi: 10.1001/archotol.129.9.951. [DOI] [PubMed] [Google Scholar]
- 3.Williams MF. Sialolithiasis. Otolaryngol Clin North Am. 1999;32:819–34. doi: 10.1016/S0030-6665(05)70175-4. [DOI] [PubMed] [Google Scholar]
- 4.Kurtoğlu G, Durmuşoğlu M, Ecevit MC. Submandibular sialolithiasis perforating the floor of mouth: a case report. Turk Arch Otorhinolaryngol. 2015;53:35. doi: 10.5152/tao.2014.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shimizu M, Yoshiura K, Nakayama E, et al. Multiple sialolithiasis in the parotid gland with Sjögren’s syndrome and its sonographic findings—Report of 3 cases. Oral Surg Oral Med Oral Pathol Oral Radiol. 2005;99:85–92. doi: 10.1016/j.tripleo.2004.04.014. [DOI] [PubMed] [Google Scholar]
- 6.Kraaij S, Karagozoglu KH, Kenter YA, Pijpe J, Gilijamse M, Brand HS. Systemic diseases and the risk of developing salivary stones: a case control study. Oral Surg Oral Med Oral Pathol Oral Radiol. 2015;119:539–43. doi: 10.1016/j.oooo.2015.01.010. [DOI] [PubMed] [Google Scholar]


