Abstract
The study is a systematic review and meta-analysis of prospective randomised control studies and prospective cohort studies of mid-term functional outcome of total knee replacement undertaken using imageless computer navigation compared with conventional instrumented total knee replacement. The literature search strategy included a search of the electronic databases, visual scanning of reference lists, hand searching of key journals and conference proceedings, and abstracts, citations, and trial registers. In total, 440 papers were retrieved after removal of duplicates, and with further screening, 11 papers were included in the systematic review and 6 papers were considered appropriate for meta-analysis. Analysis of the data showed evidence of a modest improvement in functional outcome at mid-term follow-up with use of imageless computer navigation assistance compared with conventional instrumented total knee replacement with a total score point estimate of 3.36 confidence interval (CI) (− 0.583, 7.298), objective score point estimate of 1.45 CI (0.11, 2.799), and functional score point estimate of 2.4, CI (− 1.174, 5.977). The predominant risk of bias was from random allocation and attrition. There is evidence of a modest improvement in functional outcome with the use of imageless computer navigation assistance compared with conventional instrumented total knee replacement at mid-term follow-up.
Electronic supplementary material
The online version of this article (10.1007/s43465-020-00161-z) contains supplementary material, which is available to authorized users.
Keywords: Total knee replacement, Arthroplasty, Computer navigation, Navigation-assisted knee, Imageless navigation, MeSH terms: arthroplasty, Replacement, Knee, Navigation, Computer
Introduction
Total knee replacement is a highly successful procedure for the treatment of end-stage knee arthritis. It has achieved this by relieving the debilitating pain associated with this condition and the procedure has resulted in restoring functional independence and quality of life [1, 2].
Total knee replacement as currently performed uses manufacturer provided instrumentation that (co-opts) took cognizance of the anatomy of the patient’s knees [3]. The instrumentation enables reproducible cuts on the bone, thereby ensuring a more accurate prosthetic sizing and (implantation) and fitting.
Refinements in metallurgy and component manufacture, improvement in pre-operative management, and surgical techniques have enabled total knee replacement to evolve into a reliable and reproducible procedure with high success rate with a 95% survival at 10–15 years [4].
However, despite the successes of knee arthroplasty, there is a small but constant number of patients whose knee replacements fail early. This is partly attributed to some areas of imprecision in the performance of total knee replacement using the conventional (manual) instrumented technique [3]. Furthermore, up to 20% of patients are dissatisfied with their ‘new’ knee following total knee replacement [5].
Various studies have consistently shown that with the use of the conventional instrumented techniques, a failure to achieve a post-operative mechanical alignment within the optimal range of 0–3 degrees of valgus occurs in 10–38% of total knee replacements [6, 7].
Computer navigation, on the other hand, with its novel kinematic support has delivered improved precision of technique in knee arthroplasty surgery with subsequent reduction in the error rates observed with the conventional instrumented technique [8–10]. The question that is often asked is whether this improvement in precision will translate to improvement in functional outcome and reduction in revision rates.
The aim of this systematic review, therefore, is to assess the functional outcome of imageless computer navigation-assisted total knee replacement compared with conventional instrumented knee replacement at mid-term follow-up using prospective randomised control studies and prospective non-randomised cohort studies. Furthermore, our aims were to also assess other aspects of treatment outcome including complication rates and survival of implanted knees.
Methodology
This study is carried out according to PRISMA guidelines [11], and was limited to prospective randomised control studies and prospective cohort studies. The intervention of interest is imageless computer navigation modalities in total knee replacement. Inclusion criteria are as per the PICO format. The population is patients with end-stage knee osteoarthritis undergoing total knee replacement. Intervention is imageless computer-navigated total knee replacement and the comparator is the conventional instrumented total knee replacement. Primary outcome measure is mid-term functional outcome following total knee replacement with a minimum follow-up period of 4–5 years post-operation. Secondary outcomes reviewed included peri-operative and post-operative complications, patient satisfaction, and implant survival.
Excluded from this review were Non-English language studies, animal studies, retrospective studies, cases including femoral mal-union, cadaveric studies, case series, case reports, systematic reviews, revision surgeries, and review articles. Other types of navigation apart from imageless navigation were also excluded as are robot-assisted total knee replacement procedures. In addition, outcomes less than 4 years were equally excluded.
Search Strategy
The searches were carried out independently by authors (CA, TA, and ON) and the selected abstracts agreed by consensus. The databases searched included Medline OVID (1997–January 2015), The Cochrane database of systematic reviews and randomised control trials (1997–January 2015), EMBASE (1997–January 2015), Cochrane and DARE (Database of Abstracts of Reviews of Effectiveness), Scopus (1997–January 2015), and Web of Science (1997–January 2015).
To complement the searches, screening reference lists of relevant articles, systematic reviews, and meta-analysis and other studies were carried out on relevant papers that may have been missed by the more formalised database searches.
Search terms included MESH (Medical Subject Headings) and ‘Free text’ keywords within the title and abstract fields. Similar terms were combined with OR, while concepts were combined with AND. The search terms used included; arthritis, osteoarthritis, knee arthritis, knee osteoarthritis, arthroplasty, replacement, knee, computer-assisted surgery, computer navigation, navigation, computed, treatment outcome, and functional outcome.
Study Selection
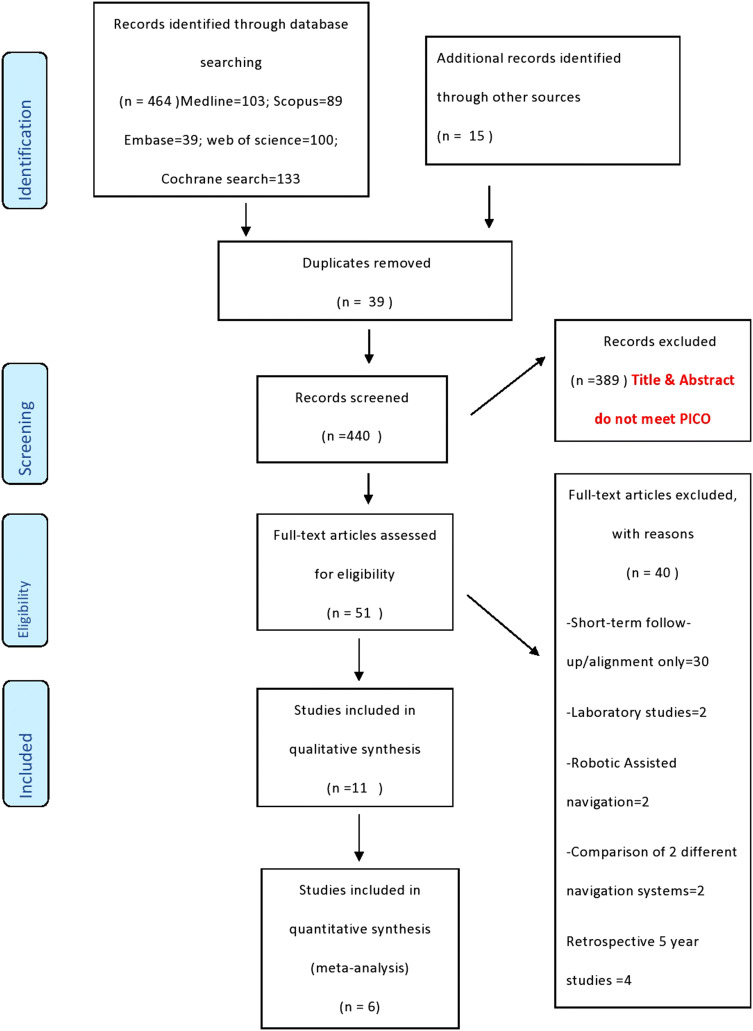
The papers were screened for eligibility by reading titles and abstracts of the studies. This was carried out independently by the three authors. Selected studies are further screened against the inclusion criteria for eligibility for inclusion in the systematic review by reading the full-text articles (Fig. 1). Those rejected at the full-text stage are noted and reasons for exclusion at this stage provided. Any disagreement was resolved by consensus. Figure 1 shows flowchart of the study selection process.
Fig. 1.
Flowchart of the study selection process
Data Extraction
Data extracted included: study characteristics including author and year of publication, type of publication, participant numbers and numbers per category, and patient demographic data including age (mean and standard deviation) and gender. The other data extracted included: the type of intervention and control, the details of intervention including type of navigation, and the duration of the surgery (Table 1). The post operative management of both groups (imageless computer navigation and conventional instrumented total knee replacement) was noted. Outcome data extracted included peri-operative complications, post-operative outcomes including range of motion, functional outcome, satisfaction rates, and revision rates. Data extraction tool was adapted from the Cochrane data extraction form and was piloted on three papers by two of the authors (CA, TA).
Table 1.
Characteristics of included studies
| Author | Year | Journal | Study design | Navigation Patient no |
Conventional Patient no |
Navigation Type of |
Implant | Follow-up duration (years) |
|---|---|---|---|---|---|---|---|---|
| Huang et al. [15] | 2012 | J Arthroplasty | RCT | 60 | 55 | Imageless infr | PFC | 5 |
| Yaffe et al. [16] | 2013 | Orthopaedics | Prospective cohort | 38 | 40 | Imageless infr | Columbus | 5 |
| Blakeney et al. [17] | 2014 | The Knee | RCT | 36 | 71 | Imageless infr | Genesis II | 4 |
| Cip et al. [18] | 2014 | J Arthroplasty | RCT | 100 | 100 | Imageless infr | Nexgen | 5 |
| Kim et al. [19] | 2012 | J Bone Joint Surg Am | RCT | 520 | 520 | Imageless infr | Nexgen,PFC | 10.8 |
| Hoffart et al. [20] | 2012 | J Bone Joint Surg Br | Prospective cohort | 98 | 97 | Imageless infr | TC-Plus | 5 |
| Thiengwittayaporn et al. [21] | 2013 | J Orthop Surg and Research | RCT | 80 | 80 | Imageless EM | Nexgen HF | 6.1 |
| Harvie et al. [22] | 2012 | J Arthroplasty | RCT | 35 | 36 | Imageless infr | Duracon | 5 |
| Hoppe et al. [23] | 2012 | Acta Orthopaedica | Prospective cohort | 55 | 31 | Infra and CT | Innex UCOR | 5 |
| Allen et al. [24] | 2014 | Int Orthopaedics | Quasi RCT | 37 | 37 | Imageless infr | LCS | 5 |
| Lutzner et al. [25] | 2013 | Knee Surg Sports Traumatol Arthrosc | RCT | 40 | 40 | Imageless infr | SCORPIO | 5 |
Imageless infr imageless infrared, imageless EM imageless electromagnetic, infra & CT infrared and CT
Study Quality and Risk of Bias
Cochrane risk of bias tool was used to rate the internal validity of the selected studies. The Cochrane risk of bias tool is grouped into five risk groupings with seven corresponding domains. The assessment of risk of bias for each domain was determined as low risk of bias, unclear risk of bias, and high risk of bias [12].
Statistics
R version 3.1.2 (2014-10-31) [13] was used for all analyses. Meta package [14] was used for R to produce the DerSimonian–Laird estimates. Global estimates and 50% and 95% confidence intervals (CI) were obtained for each analysis. Raw data for meta-analysis are in Appendix C.
Results
A search of the electronic databases revealed a total of 479 studies. Medline revealed 292 studies, Embase revealed 39 studies, Scopus revealed 89 studies, Web of Science revealed 100 studies, and Cochrane database search revealed 133 studies. Grey literature search revealed a further 15 studies. Thirty-nine (39) duplicate studies were identified and removed leaving 440 studies. Screening of these studies by titles and abstract led to the exclusion of 389 studies. The full-text articles of the remaining 51 studies were assessed by the authors with 40 studies excluded for the following reasons; 30 had short-term follow-up/alignment outcome only, 2 were laboratory studies, 2 were robotic-assisted navigation, and 4 were retrospective studies with 5-year follow-up. This left 11 papers which are the subject of this review.
The studies included involve 2206 participants with 1099 allocated to the imageless navigation-assisted total knee replacement arm and 1107 assigned to the conventional instrumented total knee replacement arm of the study. Two studies involved bilateral total knee replacement with one knee assigned to one technique and the other knee to the alternative technique of knee replacement [19, 24].
Total knee replacement was carried out in all cases allocated to the navigation arm of the study using imageless computer navigation assistance. Optical/infrared referencing was used in ten studies with a study [21] using electromagnetic referencing for the navigation.
Two studies used the navigation system for the femoral cuts only and conventional surgical procedure to conduct the tibia cuts of the knee replacement [20, 23]. In the conventional arm of the study, manufacturer supplied instruments and jigs were used according to the manufacturer’s specification. All surgical exposures were carried out identically in each arm of the study and ten studies involved standard length parapatellar exposure, and in one study [21], minimal incision surgery was utilised in both arms of their study. A total of nine different implants by different manufacturers were used in the 11 studies with 3 studies using Nexgen implant, 1 study using PFC implant, and 1 study using both PFC and Nexgen implants. A study used a standard Nexgen and a high flex Nexgen.
Outcomes
Five different functional outcome scores were used to assess knee function following total knee replacement in the 11 studies. Functional outcome was assessed using the Knee Society Score in seven studies, and the Western Ontario and McMaster Universities Osteoarthritic index (WOMAC) was used in two studies, whilst the Oxford Knee Score was used in one study as was the International Knee Society (IKS) score and the Hospital for Special Surgery knee scores (HSS). Knee Society Score (KSS) is a well-validated scoring system that has an objective (surgeon assessed) knee joint score of 100 points and a subjective (patient assessed) knee function score of 100 points. The objective knee score assesses range of knee motion, pain relief, knee alignment, and stability. The subjective function score assesses use of walking aids, walking distance, and stair climbing ability. Total score is a summation of the two scores. The higher the score, the better the outcome. A score of 80–100 excellent; 70–79 good; 60–69 Fair; Below 60 poor.
Four studies showed statistically significant improvement in functional outcome at mid-term follow-up in favour of computer-navigated total knee replacement [15, 17, 18, 20]. In three of the studies [15, 17, 18], the improved functional outcome at 5-year follow-up was correlated with improvement in coronal alignment within the optimal three degrees of varus/valgus mechanical alignment. One study [20] demonstrated improvement in functional outcome at 5-year follow-up with computer-navigated knee replacement with no difference in alignment outcome between the two arms of the study. The reason given for this finding was that differences in rotational alignment outcome between the two techniques may be responsible for the difference in functional outcome, even though this was not measured in that study.
Four studies showed no significant difference in both alignment and functional outcomes between the two techniques [16, 19, 21, 24]. All studies, however, showed a high level of accuracy in achieving implant alignment within the optimal three degrees mechanical alignment in the use of either technique. This reflects the experience of the surgeons with the use of either technique and explains the similarity in functional outcomes achieved. Three studies demonstrated improvement in radiographic alignment but no improvement in functional outcome at 5-year follow-up [22, 23, 25].
Quantitative Analysis
We present the results graphically for each of the Total Score, Objective Score, and Functional Score. Six studies [16, 18, 20, 21, 23, 25] provided total, objective, and functional score, while a seventh Havie et al. [22] had only the total score.
Total Score
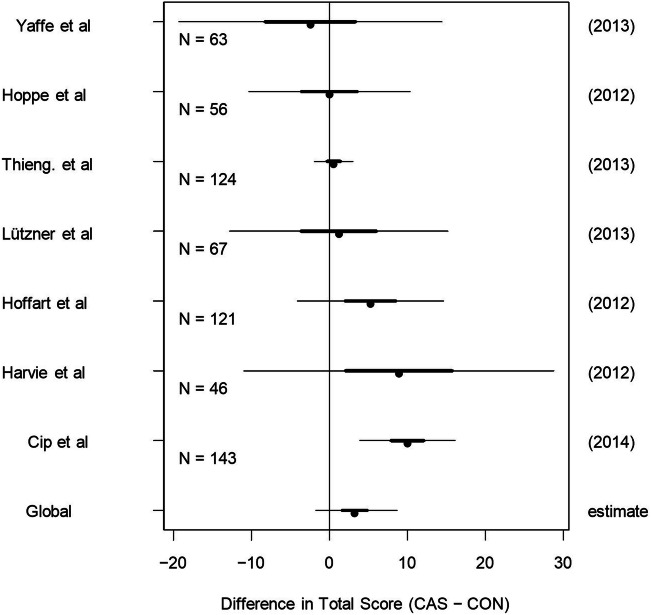
Figure 2 contains the point estimates, 50% confidence intervals (the heavy lines), and 95% confidence intervals (the thinner lines).
Fig. 2.
Point estimates with 50% and 95% confidence intervals for Total Score
For Total Score, the global estimate is 3.19 and its 95% confidence interval contains zero quite comfortably. This suggests that there is modest evidence of improvement in outcomes when computer-assisted navigation is used. Using DerSimonian–Laird random effects approach, point estimate is 1.45 with 95% confidence interval (0.11, 2.799).
Objective Score
We now perform the analysis for the Objective Score component of the Total Score (see Fig. 3). For Objective Score, the global estimate is 1.5 and its 95% confidence interval contains zero, suggesting that there is modest evidence of a small improvement in outcomes when computer-assisted navigation is used. Using DerSimonian–Laird random effects approach, point estimate is 1.45 with 95% confidence interval (0.11, 2.799).
Fig. 3.
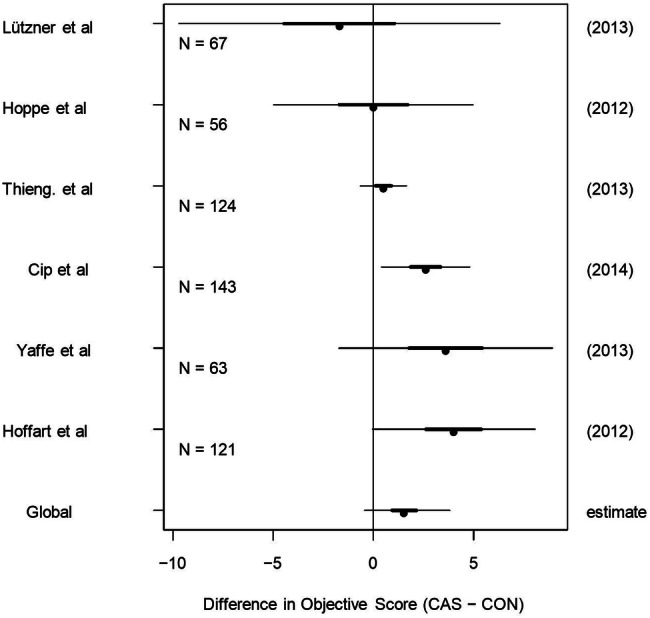
Point estimates with 50% and 95% confidence intervals for Objective Score
Functional Score
The results of running the analysis on the Functional Score component appear in Fig. 4. For Functional Score, the global estimate is 2.12 and its 95% confidence interval comfortably contains zero, suggesting that there is weak evidence of a small improvement in Functional Score when computer-assisted navigation is used. Using the DerSimonian–Laird random effects approach, the point estimate is 2.4 with 95% confidence interval (− 1.174, 5.977).
Fig. 4.
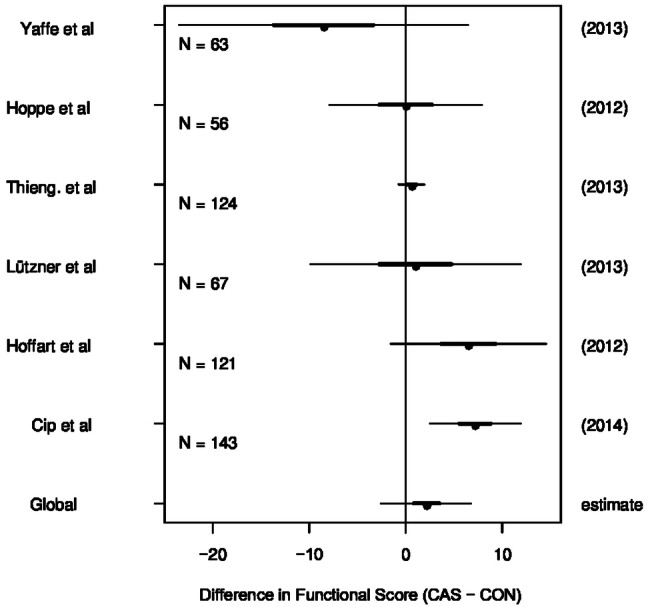
Point estimates with 50% and 95% confidence intervals for Functional Score
The summary of the primary outcome shows modest evidence of improvement in outcomes when computer-assisted navigation is used, but the size of the difference is small: Total score, point estimate 3.36 CI (− 0.583, 7.298), objective score, point estimate 1.45 CI (0.11, 2.799), and function score, point estimate 2.4, CI (− 1.174, 5.977).
The Secondary Outcome is as outlined below:
Technical complications including anterior femoral notching and excessive tibia resections necessitating the use of large plastic inserts were more in the computer-navigated arm of the study compared with the conventional group. These complications were thought to be due to a failure of registration, but may also reflect the learning curve in the use of computer navigation [19]. Infection rate was similar in both groups (Table 2).
Table 2.
Complication rates
| Complications included in the studies | ||
|---|---|---|
| Computer navigated group | Conventional group | |
| Total number | 1099 patients | 1107 patients |
| Infection | 4 | 3 |
| Fibrosis/stiffness | 4 | 0 |
| Technical | ||
| Femoral notching | 26 | 6 |
| Excessive tibial resection | 5 | 0 |
| Malalignment/instability | 7 | 13 |
| Loosening | 9 | 15 |
| Revision | 3 | 8 |
Risk of Bias Assessment
The assessment of bias was carried out using the Cochrane collaborations tool for assessing risk of bias [11]. A summary Table of Risk of assessment of individual studies in the review is presented below in Table 3.
Table 3.
Risk of bias table of included studies
| Study | Adequate sequence generation | Allocation concealment | Assessor blinding | Incomplete outcome data addressed | Free of selective reporting | Free of other bias |
|---|---|---|---|---|---|---|
| Huang et al. [15] | Yes | Yes | Unclear | No | Unclear | Yes |
| Yaffe et al. [16] | No | No | Yes | No | Unclear | Yes |
| Blakney et al. [17] | Yes | Yes | Yes | Yes | Unclear | Yes |
| Cip et al. [18] | Unclear | Yes | Yes | No | Unclear | Unclear |
| Kim et al. [19] | Yes | Unclear | Yes | No | Unclear | Unclear |
| Hoffart et al. [20] | No | No | Yes | Yes | Unclear | Yes |
| Thiengwittayaporn et al. [21] | Yes | Unclear | Yes | No | Unclear | Unclear |
| Harvie et al. [22] | Yes | Unclear | Yes | No | Unclear | Yes |
| Hoppe et al. [23] | No | No | Unclear | No | Unclear | Unclear |
| Allen et al. [24] | Unclear | Unclear | Yes | No | Unclear | Unclear |
| Lutzner et al. [25] | Yes | Unclear | Yes | No | Unclear | Unclear |
Whilst six studies [15, 17, 19, 21, 22, 25] demonstrated adequate randomisation, three studies, on the other hand, clearly described the method of allocation concealment [15, 17, 18]. Although, in nine studies, the blinding of the assessor was well elucidated, blinding of the surgeon was not documented in most studies. A problem with most studies was the loss to follow-up with death of the participants on account of the age group involved being the most common cause. Only two studies accounted for incomplete outcome data statistically on an intention-to-treat basis [17, 20]. In addition, five studies described the experience of the surgeon with navigation, whilst, in six studies, this was not specified.
Publication Bias
Funnel plots of all three components of the Knee Society Score are shown below in Figs. 5, 6 and 7.
Fig. 5.
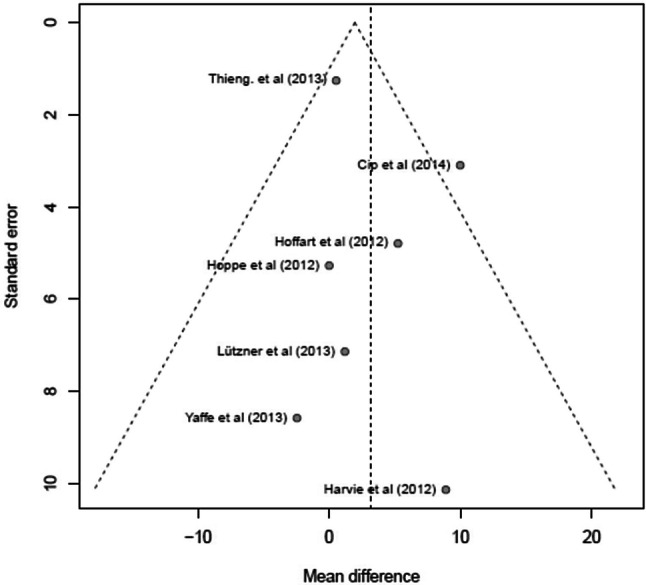
Funnel plot for Total Score Component of the Knee Society (KSS) Score
Fig. 6.
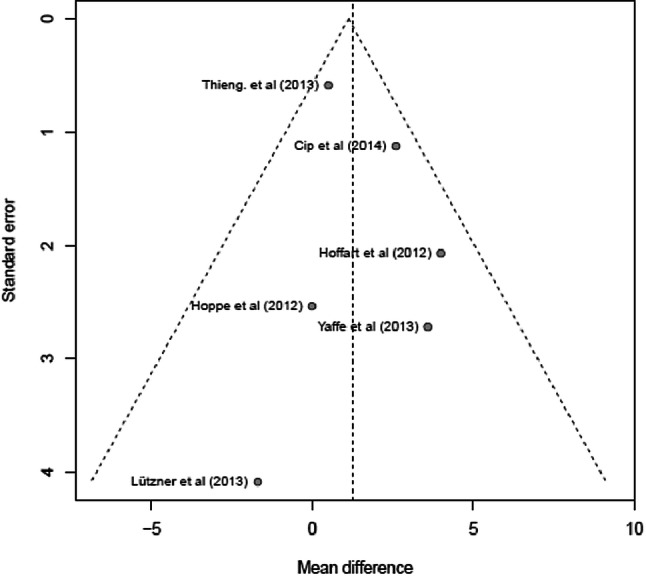
Funnel plot for the Objective Score Component of the KSS Score
Fig. 7.
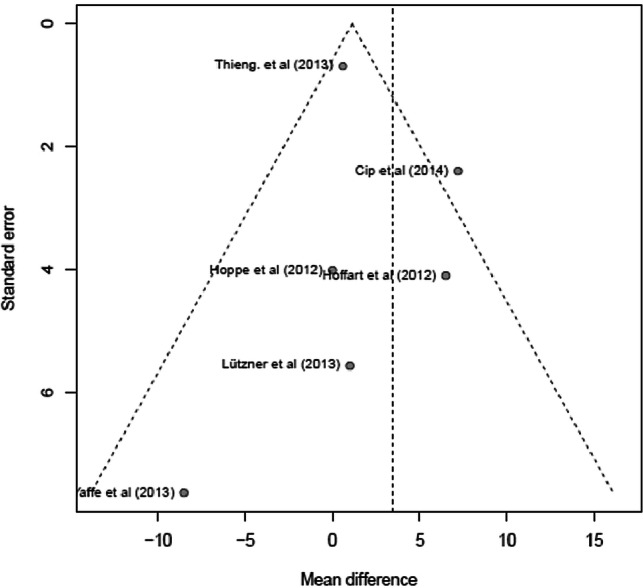
Funnel plot for the Function Score Component of the KSS Score
The vertical dotted line is the estimate of the global mean from the random effects model with the horizontal axis representing the confidence interval of the estimate. Publication bias is indicated by an absence of points at the lower quadrant of the plot.
The funnel plot shows the study by Cip et al. [18] as an outlier with other studies within the funnel plot. There are only seven studies included in the analysis and so interpretation is subjective. There was, however, no evidence of publication bias.
The funnel plot for the knee (Objective) score did not show any evidence of publication bias. The numbers of included studies, however, are small making for subjective interpretation.
The funnel plot shows an outlier in the study by Cip et al. [18]. There were no studies in the lower right quadrant suggesting some evidence of publication bias with some asymmetry in the distribution of the studies. There were only seven studies included in the analysis and so interpretation is subjective.
Discussion
Summary of Evidence
The result of analysis showed modest evidence of improvement, however, small in functional outcome, when total knee replacement was performed using computer navigation assistance compared with the conventional instrumented surgery. The improvement is noted in the total scores, the objective knee, and the function subscales of the knee society scores.
Blinded outcome assessment was the norm in all studies and the randomised studies were in the high quality studies with adequate randomisation, although most studies did not clearly specify how allocations were concealed. Many of the studies noted the experience of their surgeons, an important variable that can increase the risk of bias. Only two studies indicated that patients were blinded, but did not provide the details of how this was carried out. There were four prospective cohort studies which apart from the risk of bias due to study design had low risk of bias on other parameters. Loss to follow-up was a major factor in most studies with death of participants an important cause; there was no attempt to account for loss to follow-up in the recruitment process or by intention-to-treat analysis.
A complication that seemed higher with computer navigation-assisted knee replacement group was stiffness and arthrofibrosis. This may be because the use of this procedure resulted in longer operating time and more trauma to the soft tissues. It could also be due to the placement of pins in the quadriceps tendon/muscle away from the surgical wound, resulting in quadriceps adhesion and peri-articular soft-tissue trauma.
Study Findings in Relation to Current Literature
Recent well-conducted meta-analysis has shown that computer navigation assistance in the conduct of total knee replacement results in more precise placement of the implant compared with conventionally replaced knee [8, 10]. This is particularly true when lower limb mechanical axis within the optimal three degrees varus/valgus is assessed. This parameter has been shown in various studies to be associated with improved survival with values outside this range associated with failure [6, 26, 27].
There is, however, controversy regarding whether the improved limb alignment and implant position obtained using imageless navigation assistance results in improvement in functional outcome. A recent meta-analysis of solely randomised control trials comparing computer navigation-assisted total knee replacement and conventional knee replacement demonstrated statistically significant improvement in functional outcome in favour of computer navigation group at 2-year follow-up [8]. The explanation given by Rebal et al. [8] for the positive result in favour of navigation was their inclusion of only well randomised control trials and other stringent inclusion/exclusion criteria. Previous meta-analyses have been unable to demonstrate any such improvement with the use of navigation assistance [9, 28, 29].
In the present study, a mid-term review and meta-analysis with 4–5-year follow-up data was able to demonstrate modest evidence of small improvement in functional outcome in favour of computer navigation-assisted knee replacement. This is consonant with the results of other studies that demonstrated improved outcomes with computer-assisted navigation [8, 30]. There is also evidence from the Australian arthroplasty registry of reduced risk of revision in younger patients (under 65 years) by more than one-third when computer navigation assistance is used in total knee arthroplasty compared to conventionally instrumented total knee replacement [4].
It is, therefore, likely that the younger arthroplasty patients would benefit the most from computer navigation-assisted knee replacement as the improvement in functional outcome and significant reduction in risk of revision is most beneficial in an age group with historic poor functional outcomes and survival [31]. We, therefore, recommend routine use of imageless computer navigation assistance when undertaking total knee replacement in young patients under 65 years of age.
Study and Outcome-Level Limitations
The study is a mixture of randomised and cohort studies. Better designed studies, preferably prospective randomised studies adequately powered to adjust for attrition due to death of participants on follow-up, with appropriate blinding of patient and outcome assessors will provide definitive answers with respect to the role of this new technology in total knee replacement surgery. Data for this study were extracted a few years ago, and although, to the best of our knowledge, there has not been additions to the literature that will substantially alter the conclusion to warrant a redraft, we perceive that it may well constitute another limitation of this review. Finally, a further limitation of this paper is the exclusion of Non-English literature.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Author contributions
All the authors (CA, ON, and TA) contributed to the literature search and selection of the review papers. CA and TA contributed to data extraction. CA and ON contributed to writing the paper. CA, ON, and TA contributed to proof reading the paper. We confirm that all authors have read and approved the manuscript, and agreed to its submission.
Funding
No funds were received in support of this study.
Compliance with Ethical Standards
Conflict of interest
The authors declare no conflict of interest.
Ethical standard statement
This article does not contain any studies with human or animal subjects performed by any of the authors.
Informed consent
For this type of study informed consent is not required.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Charles Ayekoloye, Email: olufunkeropo@aol.com.
Osondu Nwangwu, Email: osjayh21@yahoo.com.
Temitope Alonge, Email: temitopealonge@gmail.com.
References
- 1.Pradhan NR, Gambhir A, Porter ML. Survivorship analysis of 3234 primary knee arthroplasties implanted over a 26-year period: a study of eight different implant designs. The Knee. 2006;13:7–11. doi: 10.1016/j.knee.2005.06.004. [DOI] [PubMed] [Google Scholar]
- 2.Robertsson O, Dunbar M, Pehrsson T, Knutson K, Lidgren L. Patient satisfaction after knee arthroplasty: A report on 27,372 knees operated on between 1981 and 1995 in Sweden. Acta Orthopaedica Scandinavica. 2000;71:262–267. doi: 10.1080/000164700317411852. [DOI] [PubMed] [Google Scholar]
- 3.Shakespeare D. Conventional instruments in total knee replacement: What should we do with them? The Knee. 2006;13:1–6. doi: 10.1016/j.knee.2005.06.002. [DOI] [PubMed] [Google Scholar]
- 4.Australian Orthopaedic Association National Joint Replacement Registry (AOANJRR) Hip, Knee and Shoulder Arthroplasty: 2018 Annual Report. Adelaide: AOA; 2018. [Google Scholar]
- 5.Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KD. Patient satisfaction after total knee arthroplasty: Who is satisfied and who is not? Clinical Orthopaedics and Related Research. 2010;468:57–63. doi: 10.1007/s11999-009-1119-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mason JB, Fehring TK, Estok R, Banel D, Fahrbach K. Meta-analysis of alignment outcomes in computer-assisted total knee arthroplasty surgery. Journal of Arthroplasty. 2007;22:1097–1106. doi: 10.1016/j.arth.2007.08.001. [DOI] [PubMed] [Google Scholar]
- 7.Blakeney WG, Khan RJ, Wall SJ. Computer- assisted techniques versus conventional guides for comparing component alignment in total knee arthroplasty: A randomised control trial. Journal of Bone and Joint Surgery. American Volume. 2011;93:1377–1384. doi: 10.2106/JBJS.I.01321. [DOI] [PubMed] [Google Scholar]
- 8.Rebal BA, Babatunde OM, Lee JH, Geller JA, Patrick DA, Jr, Macaulay W. Imageless computer navigation in total knee arthroplasty provides superior short-term functional outcomes: A meta-Analysis. Journal of Arthroplasty. 2014;29:938–944. doi: 10.1016/j.arth.2013.09.018. [DOI] [PubMed] [Google Scholar]
- 9.Burnett RS, Barrack RL. Computer-assisted Total Knee Arthroplasty is currently of no proven clinical benefit: A systematic review. Clinical Orthopaedics and Related Research. 2013;471(1):264–276. doi: 10.1007/s11999-012-2528-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hetaimish BM, Khan MM, Simunovic N, Al-Harbi HH, Bhandari M, Zalzal PK. Meta-analysis of navigation vs conventional total knee arthroplasty. Journal of Arthroplasty. 2012;27:1177–1182. doi: 10.1016/j.arth.2011.12.028. [DOI] [PubMed] [Google Scholar]
- 11.Schulz KF, Altman DG, Moher D, for the CONSORT Group CONSORT 2010 Statement: updated guidelines for reporting parallel group randomised trials. BMC Medicine. 2010;8:18. doi: 10.1186/1741-7015-8-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Higgins JPT, Altman DG, Gotzsche PC, Juni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Core Team R. R: A language and environment for statistical computing. Vienna: R Foundation for Statistical Computing; 2013. [Google Scholar]
- 14.Guido Schwarzer. meta: General Package for Meta-Analysis, 2015. R package version 4.1–0.
- 15.Huang NFR, Dowsey MM, Eric EE, Stoney JD, Babazadeh S, Choong PF. Coronal alignment correlates with outcome after total knee arthroplasty: Five- year follow-up of a randomised controlled trial. Journal of Arthroplasty. 2012;27:1737–1741. doi: 10.1016/j.arth.2012.03.058. [DOI] [PubMed] [Google Scholar]
- 16.Yaffe M, Chan P, Goyal N, Luo M, Cayo M, Stulberg SD. Computer-assisted versus manual TKA: Outcomes at 5-year follow-up. Orthopaedics. 2013;36:e629–e632. doi: 10.3928/01477447-20130426-26. [DOI] [PubMed] [Google Scholar]
- 17.Blakeney WG, Khan RJK, Palmar JL. Functional outcome following total knee arthroplasty: A randomised trial comparing computer-assisted surgery with conventional techniques. The Knee. 2014;21:364–368. doi: 10.1016/j.knee.2013.04.001. [DOI] [PubMed] [Google Scholar]
- 18.Cip J, Widemschek M, Luegmair M, Sheinkop MB, Benesch T. Conventaional versus computer-assisted technique for total knee arthroplasty: A minimum of 5-year follow-up of 200 patients in a prospective randomized comparative trial. Journal of Arthroplasty. 2014;29:1795–1802. doi: 10.1016/j.arth.2014.04.037. [DOI] [PubMed] [Google Scholar]
- 19.Kim YH, Park JW, Kim JS. Computer-navigated versus conventional total knee arthroplasty a prospective randomized trial. Journal of Bone and Joint Surgery. American Volume. 2012;94:2017–2024. doi: 10.2106/JBJS.L.00142. [DOI] [PubMed] [Google Scholar]
- 20.Hoffart HE, Langenstein E, Vasak N. A prospective study comparing the functional outcome of computer-assisted and conventional total knee replacement. Journal of Bone and Joint Surgery. British Volume. 2012;94:194–199. doi: 10.1302/0301-620X.94B2.27454. [DOI] [PubMed] [Google Scholar]
- 21.Thiengwittayaporn S, Kanjanapiboonwong A, Junsee D. Midterm outcomes of electromagnetic computer-assisted navigation in minimally invasive total knee arthroplasty. Journal of Orthopaedic Surgery and Research. 2013;8(1):37. doi: 10.1186/1749-799X-8-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Harvie P, Sloan K, Beaver RJ. Computer navigation vs conventional total knee arthroplasty: Five-year functional results of a prospective randomized trial. Journal of Arthroplasty. 2012;27:667–672. doi: 10.1016/j.arth.2011.08.009. [DOI] [PubMed] [Google Scholar]
- 23.Hoppe S, Mainzer JD, Frauchiger L, Ballmer PM, Hess R, Zumstein MA. More accurate component alignment in navigated total knee arthroplasty has no clinical benefit at 5-year follow-up. Acta Orthopaedica. 2012;83:629–633. doi: 10.3109/17453674.2012.747923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Allen CL, Hooper GJ, Oram BJ, Wells JE. Does computer-assisted total knee arthroplasty improve component position and patient function. International Orthopaedics. 2014;38:251–257. doi: 10.1007/s00264-013-1996-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lutzner J, Dexel J, Kirschner S. No difference between computer-assisted and conventional total knee arthroplasty: Five year result of a prospective randomised study. Knee Surgery, Sports Traumatology, Arthroscopy. 2013;21:2241–2247. doi: 10.1007/s00167-013-2608-7. [DOI] [PubMed] [Google Scholar]
- 26.Ritter MA, Davis KE, Meding JB, Pierson JL, Berend ME, Malinzak RA. The effect of alignment and BMI on failure of total knee replacement. Journal of Bone and Joint Surgery. American Volume. 2011;93:1588–1596. doi: 10.2106/JBJS.J.00772. [DOI] [PubMed] [Google Scholar]
- 27.Jeffrey RS, Morris RW, Denham RA. Coronal alignment after total knee replacement. Journal of Bone and Joint Surgery. British Volume. 1991;73:709–714. doi: 10.1302/0301-620X.73B5.1894655. [DOI] [PubMed] [Google Scholar]
- 28.Y.-H., Kim, J.-W., Park, J.-S. Kim. Computer-navigated versus conventional total knee arthroplasty: A prospective randomized trial. The Journal of Bone and Joint Surgery (Aamerican), 2012. [DOI] [PubMed]
- 29.Xie C, Liu K, Xiao L, Tang R. Clinical outcomes after computer-assisted versus conventional total knee arthroplasty. Orthopaedics. 2012;35(5):e647–e653. doi: 10.3928/01477447-20120426-17. [DOI] [PubMed] [Google Scholar]
- 30.Lehnen K, Giesinger K, Warschkow R, Porter M, Koch E, Kuster MS. Clinical outcome using a ligament referencing technique in CAS versus conventional technique. Knee Surgery, Sports Traumatology, Arthroscopy. 2011;19:887–892. doi: 10.1007/s00167-010-1264-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Parvizi J, Nunley RM, Berend KR, et al. High level of residual symptoms in young patients after total knee arthroplasty. Clinical Orthopaedics and Related Research. 2014;472(1):133–137. doi: 10.1007/s11999-013-3229-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.