Abstract
Background
The ultimate success of a total hip replacement lies in patients forgetting about their artificial joints during routine activities. “Forgotten Joint Score (FJS)” is emerging as an important tool in assessing outcomes of total hip arthroplasty. There has been no version of this score available in commonly spoken vernaculars in India. This study aims to formulate and validate the Hindi version of FJS in Indian population.
Methods
A total of 136 patients with a minimum follow-up of 6 months and a maximum follow-up of 18 months after total hip arthroplasty were asked to fill the translated and adapted version of FJS questionnaire, at two points of time 2 weeks apart. The Hindi version of FJS (I-FJS) was tested for reliability and responsiveness, floor and ceiling effect and validity against modified Harris Hip Score (mHHS). Construct validity was expressed as the Pearson correlation coefficient. Internal consistency was expressed as Cronbach’s alpha and test–retest reliability as the intra-class correlation coefficient (ICC).
Results
I-FJS showed excellent internal consistency with Cronbach’s alpha of 0.88. Intra-class correlation coefficient (ICC) was 0.94. I-FJS showed good correlation with m-HHS (r = 0.8, p = 0.001). The standard error of measurement was 3.6 and the smallest detectable change was 9.97. There was no floor or ceiling effect observed with I-FJS. Data from this study were insufficient to establish adequate responsiveness of I-FJS.
Conclusion
I-FJS is a valid, reliable and reproducible score for hip function in post-THA patients. It is devoid of any floor or ceiling effect. Hindi version of FJS could be an effective tool for studying hip function in the Indian population.
Keywords: Harris hip score, Forgotten Joint Score, Patient-reported outcome, Total hip arthroplasty, Functional outcomes
Introduction
Total hip arthroplasty (THA) is considered as the treatment of choice in end-stage arthritis of hip joint [1–3]. The etiology of disease of hip joint may be inflammatory, degenerative, infective, or osteonecrosis of the femoral head. THA has provided excellent results in terms of patient satisfaction and functional improvement, irrespective of the cause of arthritis. Hence, the number of THA surgeries is on an increasing trend [4].
Outcome assessment after THA can be done by objective and subjective methods. Traditionally used objective methods include range of motion, joint stability, implant survivorship and radiological assessment. However, all these assessment tools fail to include the patient’s perspective of surgical outcomes. Clinician’s judgment of outcomes and patients’ satisfaction with surgery are not always consistent with each other [3, 5–7]. Therefore, subjective assessment tools, such as clinician-reported outcome tools (CRO) and patient-reported outcome measurements (PROMs) have been developed. CROs have limitation of potential intra-observer and inter-observer variability. Most of the commonly used PROMs are based on pain and function. With the advancement in arthroplasty and a greater number of younger individuals undergoing the procedure, functional expectations from the procedure have changed over time. Thus, conventional PROMs would have a ceiling effect, potentially losing their ability to determine the difference in outcomes at a higher functional range [8, 9]. Harris Hip Score (HHS) is a commonly used CRO for the hip joint. Modified Harris Hip Score (m-HHS) is a PROM but it is not validated for native speakers of Hindi language.
Recently, Behrend et al. [10] developed a new PROM questionnaire, ‘Forgotten Joint Score’ (FJS), aiming at the patient’s ability to forget the presence of an artificial joint. Loss of awareness of the artificial joint is seen as the ultimate goal of functional improvement, resulting in maximum patient satisfaction. It represents a higher level of function, with absence of pain, and ability to perform desired tasks in daily life. FJS has been translated and validated in many languages, proving its validity and reliability [11–14]. There is no Indian version of the FJS so far. As Hindi is the most commonly spoken and understood language in India, we have validated FJS in Hindi. The purpose of this study is to formulate and validate the Hindi version of FJS (I-FJS) in the Indian population.
Materials and Methods
Study Plan
A retrospective cross-sectional study was planned in a tertiary care institute in North India after approval from the institutional review board. All patients who had undergone primary total hip arthroplasty between January 2018 and June 2019, and able to read, write and understand the Hindi language fluently were included in the study. Patients having a follow-up period of a minimum of 6 months and a maximum of 18 months from surgery were included. We included patients with avascular necrosis of femoral head, sequelae of childhood hip disorders and primary osteoarthritis of hip. However, patients with inflammatory arthritis or hip fractures needing THA were excluded from the study.
Adaptation of FJS in Hindi
Translation and adaptation of the FJS questionnaire was carried out following the International Quality of Life Assessment (IQOLA) guidelines [15]. Two independent bilingual health professionals and one non-health worker translated the original FJS to Hindi. The vernacular version was then back-translated to English by two different bilingual health professionals and one non-health worker. The final version was prepared based on a consensus decision of all the six members involved (Fig. 1).
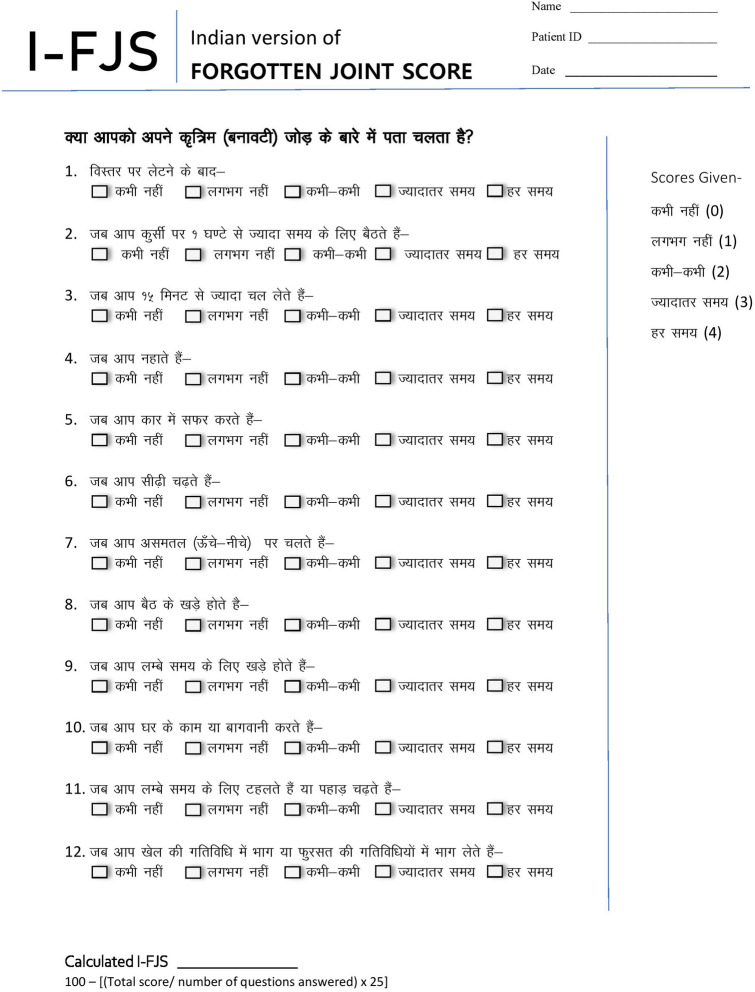
Fig. 1.
The final version of I-FJS (Indian version of Forgotten Joint Score)
Pilot Study
I-FJS was tested for comprehensibility for ease of reading and understanding, and for cultural suitability and acceptability. It was carried out by doing a pilot study in 20 patients fulfilling the inclusion criteria. The patients assessed each question on a Likert scale of 1–5 (from highly unsuitable to highly suitable). The main study was carried out after this pilot testing. Data from the pilot study were not included in the main study.
Data Acquisition
All patients fulfilling the inclusion criteria were informed about the methodology of the study and informed consent was taken. They were asked to fill the questionnaire containing I-FJS and modified Harris Hip Score (mHHS). All the scores and parameters were documented. For the assessment of test–retest reliability, patients filled the I-FJS questionnaire again, 2 weeks after the primary evaluation. If the patient could understand English, the mHHS questionnaire was administered in English; otherwise, it was translated from English to Hindi verbally by the person administering the questionnaire to the patient.
Assessment Tools Used
m-HHS: Harris Hip Score [17] is a clinician-reported outcome score having three domains: pain, function, and range of motion. The score ranges from 0 to 100 with later being the best possible outcome. We used a modified version of HHS [18], which assesses only the subjective part of the score. It is a self-administered PROM tool. Domains covered in this score are pain, function (limp, distance walked, and support) and activities (stairs, sitting, shoes, transportation). Scores range from 0 to 91, which are multiplied by 1.1 to derive the final score ranging from 0 to 100. The higher is the score better are the functional outcomes.
Hindi version of FJS: FJS, developed by Behrend et al. [10], consists of 12 questions assessing the level of awareness of the artificial joint in various activities of daily living. The score in all items is expressed as never, almost never, seldom, sometimes, and mostly and noted as 0, 1, 2, 3, and 4, respectively. The total score is transformed to a scale of 0–100, with a higher score meaning a better outcome. The adapted version of FJS (I-FJS) followed the same scoring principles.
Evaluation of I-FJS
The I-FJS was tested for validity, reliability, and responsiveness [19].
-
Validity
Validity estimates how well a score measures what it is supposed to measure. Criterion validity measures how well the measurement instrument relates to a gold standard. Since there is no gold standard, validity was limited to only construct validity. Construct validity is defined as the extent to which a score relates to other scores. It is measured in terms of the correlation coefficient. Correlation coefficient > 0.7 was taken as good, 0.3–0.7 as moderate and < 0.3 relates as poor. Correlation between I-FJS and m-HHS was calculated. Our hypothesis was that there would be a good correlation between the I-FJS and the mHHS.
-
Reliability
It is the extent to which the score is free from measurement error. It is expressed over three domains: internal consistency, test–retest reliability, and measurement error.-
Internal consistencyIt is defined as the extent to which individual items in a questionnaire are inter-related [19]. Cronbach’s alpha is used as the measure of internal consistency. Values between 0.7 and 0.95 are considered to be having sufficient internal consistency.
-
Test–retest reliabilityTest–retest reliability relates to the reproducibility of the score or the extent to which the score remains unchanged in the same patient on repeated measurements. The interval between repeated measurements should be long enough to exclude recall bias, but at the same time, it should be short enough to keep the clinical status unchanged. The recommended time period [19, 20] was set as a minimum of 2 weeks. Reproducibility is measured in terms of intra-class correlation (ICC). It ranges between 0 and 1.
-
Measurement error
-
ResponsivenessIt is defined as an estimate of how well a questionnaire detects clinically important change over time. It is a measure of the longitudinal validity of a construct. Terwee et al. [19] suggested a positive rating of responsiveness if the smallest detectable change is smaller than minimal important change (MIC). This study was based on a single set of data, so evaluation MIC was not possible. MIC could only be estimated in the current study according to Norman et al. [22] as half the value of standard deviation.
-
-
Floor or ceiling effect
Floor effect is defined as the inability of the score to discriminate in lower levels of the scale if more individuals could fall below the lowest possible value. Similarly, the ceiling effect is the inability to detect changes beyond the highest possible score. Floor or ceiling effect is considered to be present if more than 15% of participants achieve the lowest or the highest possible score [19].
Statistical Analysis
Continuous variables in demographic data were stated as mean standard deviation. For testing the internal consistency, Cronbach’s alpha was used. Test–retest reliability was tested using ICC from a one-way ANOVA model with random effect. ICC was classified according to Landis et al. [20]: < 0.2, poor 0.2–0.4, fair 0.4–0.6, moderate; 0.6–0.8, substantial > 0.8, almost perfect. The construct validity of the I-FJS score was checked with Pearson’s correlation coefficient. All the statistical data analysis was carried out with SPSS version 25.
Result
Translation
Forward and backward translation of FJS was carried out following guidelines provided by IQOLA. Only minor modifications were made in the questionnaire as per the cultural adaptation in our population. Question 12 in FJS asks ‘Are you aware of your artificial joint while doing your favorite sport?’ In the Indian population, perusing sports is not very common with patients seeking treatment of advance arthritic disease. Thus, the question was modified to ‘…while doing your leisure time activities?’ which seemed acceptable to all six members in the translation panel. Basing on this, the final version of I-FJS was prepared and subjected to testing in our study population. The same has been done by the previous study on FJS-12 conducted on Indian patients undergoing total knee replacements [23].
Pilot Study
In the pilot study, it was seen that all the questions were answered by most of the participants. The results of the pilot study are summarized in Table 1. The pilot study showed good cross-cultural adaption of the Hindi FJS-12.
Table 1.
Demographic details of the patients in the study
| Parameters | Mean ± SD | Range |
|---|---|---|
| Age | 43.0 ± 15.3 years | 20–78 years |
| Sex | ||
| Male | 79 (58.3%) | |
| Female | 57 (41.7%) | |
| Side involved | ||
| Left | 54 (39.7%) | |
| Right | 82 (60.3%) | |
| Time at follow-up | ||
| 1st follow-up after surgery | 9.5 ± 1.8 months | 7–17 months |
| Interval between 1st and 2nd follow up | 28.8 ± 7.4 days | 14–42 days |
Final Study
A total of 150 patients fulfilling inclusion and exclusion criteria were enrolled for the study. Fourteen patients were lost to follow-up and were excluded from the analysis (Fig. 2). The final data of 136 patients were analyzed. Of them, 70 patients had avascular necrosis, 20 had primary osteoarthritis, 28 had post-traumatic osteoarthritis and had 18 osteoarthritis secondary to a pediatric hip disorder. The sample size was based on a recommendation that there should be at least 10 patients per question in a questionnaire [18]. The demographic data of these patients is given in Table 2. Mean time between surgery and data collection was 9.5 ± 1.8 months (range 7–17 months). The second questionnaire was completed on average 28.8 ± 7.4 days (range 14–42 days) after the first questionnaire for test–retest reliability. A total of 71 patients completed the questionnaire at 2 weeks.
Fig. 2.
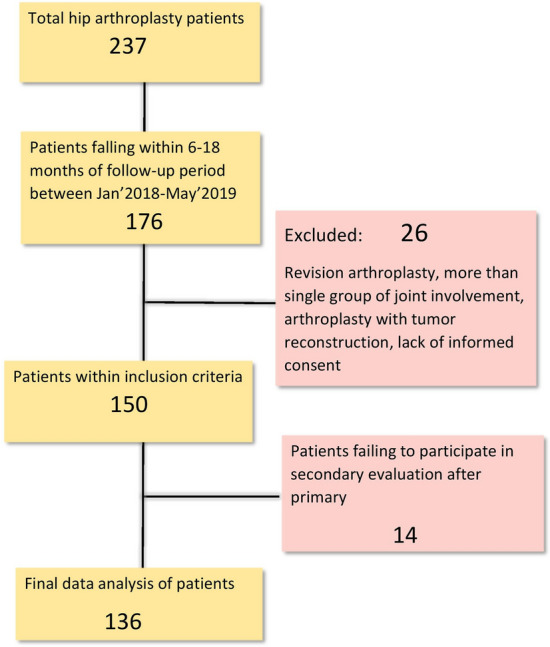
The flow chart of patient enrolment of the study
Table 2.
Hindi FJS-12 questionnaire with pilot study and final study values
| Pilot study | Final Study | ||||||
|---|---|---|---|---|---|---|---|
|
Likert Scale Mean ± Std. deviation |
I-FJS Mean ± Std. deviation |
Percent age of responses | Hindi-FJS Mean ± Std. deviation |
Percentage of responses | ||
| Q1 |
|
1.55 ± 0.60 | 1.1 ± 1.16 | 100 | 1.15 ± 0.97 | 97.6 | |
| Q2 |
|
1.35 ± 0.58 | 2.05 ± 1.23 | 100 | 1.25 ± 1.10 | 100 | |
| Q3 |
|
1.05 ± 0.22 | 1.3 ± 1.34 | 100 | 1.02 ± 1.01 | 99.2 | |
| Q4 |
|
1.8 ± 0.69 | 1.3 ± 1.21 | 100 | 1.23 ± 0.90 | 96 | |
| Q5 |
|
1.55 ± 0.60 | 2.0 ± 1.02 | 100 | 1.64 ± 0.79 | 96.8 | |
| Q6 |
|
1.05 ± 0.22 | 2.45 ± 1.05 | 100 | 2.12 ± 0.87 | 98.4 | |
| Q7 |
|
1.2 ± 0.41 | 1.9 ± 1.11 | 95 | 1.73 ± 0.86 | 94.4 | |
| Q8 |
|
1.2 ± 0.41 | 2.45 ± 0.82 | 100 | 2.25 ± 0.59 | 97.6 | |
| Q9 |
|
1.05 ± 0.23 | 2.45 ± 1.14 | 100 | 2.26 ± 1.06 | 98.4 | |
| Q10 |
|
1.6 ± 0.75 | 2.25 ± 1.06 | 95 | 2.15 ± 0.92 | 95.2 | |
| Q11 |
|
1.7 ± 0.73 | 2.35 ± 0.98 | 95 | 2.10 ± 0.78 | 94.4 | |
| Q12 |
|
1.8 ± 0.76 | 2.2 ± 1.19 | 95 | 2.21 ± 0.96 | 94.4 | |
| Total | 23.8 ± 9.49 | 97.08 | 21.16 ± 7.07 | 96.86 | |||
The average I-FJS was 55.89 ± 14.73 and m-HHS was 73.84 ± 17.60. I-FJS showed excellent internal consistency with Cronbach’s alpha of 0.88. The intraclass correlation coefficient was 0.94. The standard error of measurement was 3.6 and the smallest detectable change was 9.97. I-FJS showed a good correlation with m-HHS, with a Pearson coefficient of 0.80 (p = 0.001). Since there is no consensus on minimal important change (MIC) for FJS, MIC could only be estimated by dividing the standard deviation by two, as proposed by Norman et al. [22]. It came out to be 7.5. Thus, the smallest detectable change was higher than the minimal important change implying a lack of responsiveness of this score in this study. There was no floor or ceiling effect observed with I-FJS as no patient had the maximum or minimum achievable score.
Discussion
Awareness of a joint reflects disunity between the affected joint and the self [24]. Following surgery, patients may have pain, functional impairment, stiffness or numbness, which may lead to a subconscious perception of separation of the joint from a patient’s own-self. This feeling may bring in a sense of insecurity, particularly in more demanding activities such as descending stairs, going downhill, or kneeling [25]. On the contrary, a patient with perfect outcomes may feel unaware of an artificial joint inside the body. This can be considered as the ultimate goal of joint replacement surgery. This ‘unity’ of the joint and the body may not be present in the early postoperative period. That is why a minimum postoperative period of six months was taken as an inclusion criterion in this study.
For a patient to ‘forget’ about its artificial joint, there should be an acceptable range of pain-free motion with stability in all degrees of freedom of the joint. FJS assesses all these parameters and is, thus, apt in quantifying patients’ subjective feelings. There are equally weighted 12 questions concerning awareness of the joint in routine activities. This study was conducted to investigate the validity of FJS in the Indian population after its adaptation into the native language (I-FJS). The Indian version of FJS proved its validity and reliability. Traditional tools used in hip surgery are HHS and Oxford hip score. They are evaluated in the English language as none of the available scores has been adequately validated in Hindi. This questions the accuracy of the measurement of functional outcomes in patients from this country. PROMs are self-filled questionnaire and, thus, should be in the native language.
Excellent test–retest reliability was observed, with ICC of 0.94 which is consistent with other studies [13, 26]. Excellent construct validity of I-FJS was seen, making it a viable tool for clinical use and research. FJS has also been validated by different authors in other populations. Klouche et al. [26] found similar results on comparing FJS with m-HHS (r = 0.7). Matsumoto et al. [12] also found a good correlation (r = 0.7) of FJS with the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) and the Japanese Orthopaedic Association Hip Disease Evaluation Questionnaire. Klouche et al. [26] developed and validated a French version of FJS and found it to be valid and comparable to the English version. No floor or ceiling effects were seen. It correlated strongly with the HHS and Oxford Hip Score. High internal consistency and reproducibility were seen. Hamilton et al. [14] validated the English version of FJS for the population in the United Kingdom. A high correlation with the Oxford hip score was seen. High internal consistency and reliability were seen, with a low ceiling effect. Larsson et al. [13] also found a lower ceiling effect with FJS as compared to Oxford Hip Score. FJS had high internal consistency and reproducibility.
With an increasing number of patients undergoing joint replacement surgery, the bar of patient satisfaction is rising higher. Performance in higher range of patient satisfaction is an important limitation of conventional PROMs [27]. Behrend et al. [10] observed no floor or ceiling effect with FJS. No floor or ceiling effect was observed with I-FJS too. Thus, it is capable of differentiating better between patients with excellent outcomes and those with good but not excellent outcomes.
The average time period at which our patients were subjected to the questionnaire was 9.5 1.8 months after the surgery, in contrast to other studies that have taken the questionnaire at a minimum follow-up of 12-month [10, 28]. FJS is very sensitive to change between 6 and 12 months after the surgery [29]. Our FJS values were slightly lower than other studies in literature as patients with lesser postoperative duration are expected to have a lower score.
Data on the responsiveness of FJS are lacking and some other authors have also shown that MIC in FJS was smaller than the smallest detectable change [30, 31]. Giesinger et al. [32] found MIC to range between 20.8 and 25.6 within the first 12 months postoperatively in cases of total knee arthroplasty. There is no existing gold standard for the calculation of MIC [15, 33]. In the current study, no external anchor was used for estimation of MIC; so, it was estimated using distribution-based method. It came out to be 7.5 as per Norman et al. [22].
Cultural differences do exist and are important to be considered when a PROM is being adapted to for an ethnicity. We found that the question about the sporting activity was not relevant during the pilot study. Thus, it was changed to leisure activity. Similar findings were seen by Theinpont et al. [28] in the Turkish population. A study on the UK population showed that about 48% of the patients failed to answer this question [34].
One important limitation of this study is that only postoperative evaluation of FJS and mHHS was made. The preoperative evaluation was not performed. Nor post-operative evaluations were made at different points of time. With this data, we could only estimate MIC as half the value of standard deviation. Responsiveness was found to be lacking. Lack of data collection at wide intervals has also restricted us from calculating the effect size of the score, standardized response mean or the area under the curve. Future studies should estimate the MIC values of I-FJS. Another limitation of the study is that the second questionnaire was completed on average 28.8 days instead of the target of 2 weeks. Timely follow-up assessment though ideal is sometimes not possible. It is possible that the clinical condition of the patient might have changed in those 4 weeks.
Conclusion
I-FJS is a valid, reliable and reproducible score for hip function. It is devoid of any floor or ceiling effect. Responsiveness of FJS could not be found in this study. But with good validity and reliability established, the Hindi version of FJS could be an effective tool for studying hip function in the Indian population.
Funding
There was no funding source.
Compliance with Ethical Standards
Conflict of interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical review committee statement
The institutional ethics committee approved the study (AIIMS/IEC/18/146). Each author certifies that he or she has no commercial associations (e.g., consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article. The study was conducted in All India Institute of Medical Sciences, Rishikesh, India.
Informed consent
For this type of study informed consent is not required.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Siddharth S. Sethy, Email: Sekhar.ciddharth@gmail.com
Tarun Goyal, Email: goyal.tarun@gmail.com.
Souvik Paul, Email: 1990.souvik@gmail.com.
S. Lakshmana Das, Email: sekarldas@gmail.com.
Arghya Kundu Choudhury, Email: arghyakunduchoudhury@gmail.com.
Roop Bhushan Kalia, Email: roopkalia2003@yahoo.com.
References
- 1.Baker PN, van der Meulen JH, Lewsey J, Gregg PJ. National Joint Registry for England and Wales. The role of pain and function in determining patient satisfaction after total knee replacement: Data from the National Joint Registry for England and Wales. The Journal of Bone and Joint Surgery. 2007;89(7):893–900. doi: 10.1302/0301-620X.89B7.19091. [DOI] [PubMed] [Google Scholar]
- 2.Hamilton DF, Lane JV, Gaston P, Patton JT, MacDonald D, Simpson AHRW, et al. What determines patient satisfaction with surgery? A prospective cohort study of 4709 patients following total joint replacement. British Medical Journal Open. 2013;3(4):e002525. doi: 10.1136/bmjopen-2012-002525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bullens PH, van Loon CJ, de Waal Malefijt MC, Laan RF, Veth RP. Patient satisfaction after total knee arthroplasty: A comparison between subjective and objective outcome assessments. Journal of Arthroplasty. 2001;16(6):740–747. doi: 10.1054/arth.2001.23922. [DOI] [PubMed] [Google Scholar]
- 4.Pachore JA, Vaidya SV, Thakkar CJ, Bhalodia HKP, Wakankar HM. ISHKS joint registry: A preliminary report. Indian Journal of Orthopaedics. 2013;47(5):505–509. doi: 10.4103/0019-5413.118208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Minator Sajjadi M, Keyhani S, Kazemi SM, Hanafizadeh B, Ebrahimpour A, Banasiri M. Patient satisfaction following total knee arthroplasty: Comparison of short-term results in rheumatoid arthritis and osteoarthritis. Archives of Bone and Joint Surgery. 2019;7(1):61–66. [PMC free article] [PubMed] [Google Scholar]
- 6.Suda AJ, Seeger JB, Bitsch RG, Krueger M, Clarius M. Are patients’ expectations of hip and knee arthroplasty fulfilled? A prospective study of 130 patients. Orthopedics. 2010;33(2):76–80. doi: 10.3928/01477447-20100104-07. [DOI] [PubMed] [Google Scholar]
- 7.Noble PC, Conditt MA, Cook KF, Mathis KB. The John Insall Award: Patient expectations affect satisfaction with total knee arthroplasty. Clinical Orthopaedics and Related Research. 2006;452:35–43. doi: 10.1097/01.blo.0000238825.63648.1e. [DOI] [PubMed] [Google Scholar]
- 8.Marx RG, Jones EC, Atwan NC, Closkey RF, Salvati EA, Sculco TP. Measuring improvement following total hip and knee arthroplasty using patient-based measures of outcome. Journal of Bone and Joint Surgery. American Volume. 2005;87(9):1999–2005. doi: 10.2106/JBJS.D.02286. [DOI] [PubMed] [Google Scholar]
- 9.Na S-E, Ha C-W, Lee C-H. A new high-flexion knee scoring system to eliminate the ceiling effect. Clinical Orthopaedics and Related Research. 2012;470(2):584–593. doi: 10.1007/s11999-011-2203-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Behrend H, Giesinger K, Giesinger JM, Kuster MS. The “forgotten joint” as the ultimate goal in joint arthroplasty: Validation of a new patient-reported outcome measure. Journal of Arthroplasty. 2012;27(3):430–436. doi: 10.1016/j.arth.2011.06.035. [DOI] [PubMed] [Google Scholar]
- 11.Klouche S, Giesinger JM, Sariali EH. Translation, cross-cultural adaption and validation of the French version of the Forgotten Joint Score in total hip arthroplasty. Orthopaedics & Traumatology: Surgery & Research. 2018;104(5):657–661. doi: 10.1016/j.otsr.2018.04.010. [DOI] [PubMed] [Google Scholar]
- 12.Matsumoto M, Baba T, Homma Y, Kobayashi H, Ochi H, Yuasa T, Behrend H, Kaneko K. Validation study of the Forgotten Joint Score-12 as a universal patient-reported outcome measure. European Journal of Orthopaedic Surgery & Traumatology. 2015;25(7):1141–1145. doi: 10.1007/s00590-015-1660-z. [DOI] [PubMed] [Google Scholar]
- 13.Larsson A, Rolfson O, Kärrholm J. Evaluation of Forgotten Joint Score in total hip arthroplasty with Oxford Hip Score as reference standard. Acta Orthopaedica. 2019;90(3):253–257. doi: 10.1080/17453674.2019.1599252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hamilton DF, Loth FL, Giesinger JM, Giesinger K, MacDonald DJ, Patton JT, Simpson AH, Howie CR. Validation of the English language Forgotten Joint Score-12 as an outcome measure for total hip and knee arthroplasty in a British population. The Bone & Joint Journal. 2017;99(2):218–224. doi: 10.1302/0301-620X.99B2.BJJ-2016-0606.R1. [DOI] [PubMed] [Google Scholar]
- 15.Bullinger M, Alonso J, Apolone G, Leplège A, Sullivan M, Wood-Dauphinee S, et al. Translating health status questionnaires and evaluating their quality: The IQOLA Project approach. International Quality of Life Assessment. Journal of Clinical Epidemiology. 1998;51(11):913–923. doi: 10.1016/s0895-4356(98)00082-1. [DOI] [PubMed] [Google Scholar]
- 16.Mokkink LB, Terwee CB, Knol DL, Stratford PW, Alonso J, Patrick DL, et al. Protocol of the COSMIN study: COnsensus-based Standards for the selection of health Measurement INstruments. BMC Medical Research Methodology. 2006;24(6):2. doi: 10.1186/1471-2288-6-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: Treatment by mold arthroplasty. An end-result study using a new method of result evaluation. Journal of Bone and Joint Surgery. 1969;51(4):737–755. doi: 10.2106/00004623-196951040-00012. [DOI] [PubMed] [Google Scholar]
- 18.Sharma S, Shah R, Draviraj KP, Bhamra MS. Use of telephone interviews to follow up patients after total hip replacement. Journal of Telemedicine and Telecare. 2005;11(4):211–214. doi: 10.1258/1357633054068883. [DOI] [PubMed] [Google Scholar]
- 19.Terwee CB, Bot SDM, de Boer MR, van der Windt DAWM, Knol DL, Dekker J, et al. Quality criteria were proposed for measurement properties of health status questionnaires. Journal of Clinical Epidemiology. 2007;60(1):34–42. doi: 10.1016/j.jclinepi.2006.03.012. [DOI] [PubMed] [Google Scholar]
- 20.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–174. doi: 10.2307/2529310. [DOI] [PubMed] [Google Scholar]
- 21.Lu W-S, Wang C-H, Lin J-H, Sheu C-F, Hsieh C-L. The minimal detectable change of the simplified stroke rehabilitation assessment of movement measure. Journal of Rehabilitation Medicine. 2008;40(8):615–619. doi: 10.2340/16501977-0230. [DOI] [PubMed] [Google Scholar]
- 22.Norman GR, Sloan JA, Wyrwich KW. Interpretation of changes in health-related quality of life: The remarkable universality of half a standard deviation. Medical Care. 2003;41(5):582–592. doi: 10.1097/01.MLR.0000062554.74615.4C. [DOI] [PubMed] [Google Scholar]
- 23.Goyal T., Sethy S.S, Paul S., Choudhury A.K., Das S.L. (2020). Good validity and reliability of forgotten joint score-12 in total knee arthroplasty in Hindi language for Indian population. Knee Surg Sports Traumatol Arthrosc. 10.1007/s00167-020-06124-z. [DOI] [PubMed]
- 24.Hudak PL, McKeever PD, Wright JG. Understanding the meaning of satisfaction with treatment outcome. Medical Care. 2004;42(8):718–725. doi: 10.1097/01.mlr.0000132398.11342.a8. [DOI] [PubMed] [Google Scholar]
- 25.Loth FL, Liebensteiner MC, Giesinger JM, Giesinger K, Bliem HR, Holzner B. What makes patients aware of their artificial knee joint? BMC Musculoskeletal Disorder. 2018;19(1):5. doi: 10.1186/s12891-017-1923-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Klouche S, Giesinger JM, Sariali EH. Translation, cross-cultural adaption and validation of the French version of the Forgotten Joint Score in total hip arthroplasty. Orthopaedics & Traumatology: Surgery and Research. 2018;104(5):657–661. doi: 10.1016/j.otsr.2018.04.010. [DOI] [PubMed] [Google Scholar]
- 27.Hossain FS, Konan S, Patel S, Rodriguez-Merchan EC, Haddad FS. The assessment of outcome after total knee arthroplasty: Are we there yet? The Bone & Joint Journal. 2015;97(1):3–9. doi: 10.1302/0301-620X.97B1.34434. [DOI] [PubMed] [Google Scholar]
- 28.Thienpont E, Vanden Berghe A, Schwab PE, Forthomme JP, Cornu O. Joint awareness in osteoarthritis of the hip and knee evaluated with the “Forgotten Joint” Score before and after joint replacement. Knee Surgery, Sports Traumatology, Arthroscopy. 2016;24(10):3346–3351. doi: 10.1007/s00167-015-3970-4. [DOI] [PubMed] [Google Scholar]
- 29.Hamilton DF, Giesinger JM, MacDonald DJ, Simpson AH, Howie CR, Giesinger K. Responsiveness and ceiling effects of the Forgotten Joint Score-12 following total hip arthroplasty. Bone & Joint Research. 2016;5(3):87–91. doi: 10.1302/2046-3758.53.2000480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Baumann F, Ernstberger T, Loibl M, Zeman F, Nerlich M, Tibesku C. Validation of the German Forgotten Joint Score (G-FJS) according to the COSMIN checklist: Does a reduction in joint awareness indicate clinical improvement after arthroplasty of the knee? Archives of Orthopaedic and Trauma Surgery. 2016;136(2):257–264. doi: 10.1007/s00402-015-2372-x. [DOI] [PubMed] [Google Scholar]
- 31.Heijbel S, Naili JE, Hedin A, W-Dahl A, Nilsson KG, Hedström M. The Forgotten Joint Score-12 in Swedish patients undergoing knee arthroplasty: A validation study with the Knee Injury and Osteoarthritis Outcome Score (KOOS) as comparator. Acta Orthopaedica. 2020;91(1):88–93. doi: 10.1080/17453674.2019.1689327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Giesinger K, Hamilton DF, Jost B, Holzner B, Giesinger JM. Comparative responsiveness of outcome measures for total knee arthroplasty. Osteoarthritis and Cartilage. 2014;22:184–189. doi: 10.1016/j.joca.2013.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tubach F, Ravaud P, Martin-Mola E, Awada H, Bellamy N, Bombardier C, et al. Minimum clinically important improvement and patient acceptable symptom state in pain and function in rheumatoid arthritis, ankylosing spondylitis, chronic back pain, hand osteoarthritis, and hip and knee osteoarthritis: Results from a prospective multinational study. Arthritis Care & Research. 2012;64(11):1699–1707. doi: 10.1002/acr.21747. [DOI] [PubMed] [Google Scholar]
- 34.Robinson PG, Rankin CS, Lavery J, Anthony I, Blyth M, Jones B. The validity and reliability of the modified forgotten joint score. Journal of Orthopaedics. 2018;15(2):480–485. doi: 10.1016/j.jor.2018.03.029. [DOI] [PMC free article] [PubMed] [Google Scholar]