Abstract
Low perceived distress tolerance (DT), a trait-like individual difference factor reflecting one’s perceived ability to withstand aversive affective states, has been linked with current internalizing and substance use disorders (SUD). However, perceived DT has not been systematically evaluated as a familial, transdiagnostic vulnerability factor for internalizing and SUDs. The current study tested whether perceived DT runs in families and whether it is reduced among individuals with vs. without remitted internalizing/SUD psychopathology. Perceived DT and internalizing/SUD disorders were measured in 638 individuals (nested within 256 families). Analyses also adjusted for the effects of neuroticism to test whether DT was a specific vulnerability factor independent of temperamental negative affect. Analyses revealed that perceived DT was lower in individuals with remitted distress (i.e., major depression, generalized anxiety disorder, post-traumatic stress disorder) but not fear disorders (i.e., panic disorder, social anxiety disorder, specific phobia, obsessive-compulsive spectrum disorders) relative to healthy controls, and the effect of distress-misery disorder history remained significant when adjusting for neuroticism. Perceived DT was not significantly different among individuals with vs. without a remitted SUD disorder. There were no effects for comorbid SUD and distress-misery disorders. Finally, perceived DT was also significantly correlated within families, suggesting that it runs in families. Overall, results suggest that independent of neuroticism, low perceived DT is a familial vulnerability for distress (but not fear or substance use) disorders.
Keywords: distress tolerance, vulnerability, internalizing, externalizing, familial
Introduction
Internalizing (i.e., depression, anxiety, obsessive-compulsive [OC]-spectrum, and eating disorders; see Kotov et al., 2017, 2018 for placement of OC and eating disorders in internalizing spectrum) and substance use disorders (SUDs) are costly, co-occur at high rates, and cause substantial disability (Compton et al., 2007; Conway et al., 2006; Lewinsohn et al., 2004; Grant et al., 2005; Lai et al., 2015). The high rates of co-morbidity among internalizing and SUDs are explained in part by common genetic and environmental risk between internalizing and externalizing disorders (e.g., Pesenti-Gritti et al., 2008), which suggests the presence of common vulnerabilities that cut across these disorders. Identification of transdiagnostic vulnerabilities is therefore vital for our understanding of the etiology of internalizing/SUDs, co-morbidity within and across internalizing/SUDs, and internalizing/SUD treatment response (Shankman & Gorka, 2015).
Impaired regulation of negative affect and excessive reliance upon avoidance behavior is a common feature of both internalizing (Wilamowska et al., 2010) and SUDs (Baker et al., 2004), suggesting that individual differences in the capacity to withstand negative emotional states (i.e., distress tolerance) may confer risk for both internalizing and SUDs. Distress tolerance (DT) is typically conceptualized as a trait-like individual difference variable reflecting the actual or perceived capacity to tolerate negative emotional states (Leyro et al., 2010). Indeed, moderate temporal stability has been reported for behavioral and self-report measures of DT (Cummings et al., 2013; Kiselica et al., 2014). Self-report measures asses an individuals’ perceived capacity to tolerate emotional distress in general, whereas behavioral measures often operationalize DT as the quit latency on a distressing laboratory task (McHugh & Otto, 2011). Behavioral and self-report measures of DT are not typically correlated (e.g., Kiselica et al., 2015; McHugh et al., 2011), suggesting that they are assessing largely distinct constructs. For example, self-report measures of DT have been associated with internalizing and SUD diagnoses as well as symptom severity (e.g., Allan et al., 2015, Macatee et al., 2018), whereas behavioral measures have been linked with treatment-relevant behaviors in SUD populations (e.g., early lapse, treatment dropout, abstinence duration; Abrantes et al., 2008; Daughters et al., 2005; Reese et al., 2019; Strong et al., 2012) but less consistently with psychopathology/symptom severity (e.g., Ellis et al., 2013; Kiselica et al., 2015; Marshall-Berenz et al., 2010). Thus, given perceived DT’s trait-like nature and consistent associations with internalizing and SUDs, perceived DT may be a vulnerability factor for certain psychopathologies.
Theoretical conceptualization of DT as a vulnerability largely began with the cognitive-behavioral conceptualization and treatment of borderline personality disorder (Linehan, 1993). In this model, poor perceived DT is thought to arise from the combination of a biologically-based propensity for heightened negative emotional reactivity/delayed recovery with an emotionally-invalidating environment, ultimately resulting in the secondary negative appraisals of distress and attendant amplified avoidance urges characteristic of low perceived DT. This conceptualization suggests that perceived DT should run in families, potentially via heritability of a neurotic temperament (i.e., low threshold for and delayed recovery from negative emotional experience) and/or a shared emotionally-invalidating home environment, but the theorized familial nature of perceived DT has never been empirically tested. This is a significant limitation given its importance to a prominent theoretical conceptualization of the DT construct (Linehan, 1993), its implications for risk detection and preventive interventions, and its role as a criterion for determining whether an individual difference variable acts as a vulnerability for psychopathology (Zubin & Spring, 1977).
To determine if an individual difference variable is a vulnerability for a disorder, Zubin and Spring (1977) proposed that the vulnerability should be present (1) before, (2) during, and (3) after an episode of the disorder, and (4) the vulnerability should be familial (i.e., correlated within families) (see Kraemer et al., 1997 for a similar, but slightly different model without an explicit focus on familial vulnerabilities). It is important to note that these criteria only require that the vulnerability demonstrate relative between-subject stability over time, but allow for within-subject fluctuation (e.g., due to disorder onset/remission, treatment or pathoplastic factors; Ormel et al., 2004). Interestingly, among these four criteria, most studies have only examined whether DT is present during an episode of psychopathology (i.e., in those with a current diagnosis). Low perceived DT has been associated with the presence of multiple (if not all) internalizing disorders as well as increased symptom severity across these disorders (Allan et al., 2015; Macatee et al., 2015; Vujanovic et al., 2017).
Low perceived DT has also been prospectively associated with maintenance/increases in anxiety symptoms over one-month in non-clinical, undergraduate samples (Cougle et al., 2011; Macatee et al., 2015). However, these naturalistic studies used unselected, undergraduate samples and only followed participants for one-month, making it difficult to conclude that low DT preceded symptom development (i.e., Zubin and Spring [1997] criteria 1) given that the sampling approach did not explicitly exclude individuals with current or remitted psychopathology. Multiple treatment studies have found that improvement in DT and reduction in internalizing symptoms during treatment covary over time (Banducci et al., 2017; Boffa et al., 2018; McHugh et al., 2014), though only one of these studies assessed whether DT changed prior to symptoms changing (Boffa et al., 2018). Overall, the limitations of these longitudinal studies make it difficult to know if DT is better conceptualized as a state characteristic, malleable maintenance factor, or a trait-like vulnerability for internalizing psychopathology.
Although extant data indicate that low perceived DT is associated with internalizing disorders broadly, some data suggest that it may relate to certain internalizing disorders more than others. Numerous investigations of the phenotypic and genotypic structure of internalizing disorders have shown that the conditions cluster into two correlated, but separable factors: fear (e.g., panic disorder, specific phobia, social phobia, OC-spectrum) and distress-misery disorders (e.g., GAD, MDD, PTSD; Kendler et al., 2003; Krueger, 1999; Seeley et al., 2011; Shankman & Klein, 2003; Watson, 2005; Slade & Watson, 2006). Interestingly, studies have shown more robust associations between DT and distress-misery relative to fear disorders (Keough et al., 2010; Laposa et al., 2015; Macatee et al., 2016; Michel et al., 2016; Norr et al., 2013), though other work has shown that unique associations between perceived DT and fear disorders remain significant when controlling for co-occurring distress-misery psychopathology (e.g., Allan et al., 2015). Thus, whether perceived DT is more of a vulnerability factor (rather than just a characteristic) for distress-misery or fear disorders remains an open question.
Low perceived DT may not be specific to internalizing disorders as it has also been linked with current SUD diagnoses and SUD symptom severity (Allan et al., 2015; Macatee et al., 2018; Ozdel & Ekinci, 2014), though null associations have also been reported (Kiselica et al., 2015). Low perceived DT has also been prospectively associated with greater cannabis use during a self-guided quit attempt (Hasan et al., 2015) and increases in alcohol problems across a six-month period (Simons & Gaher, 2005). Further, low perceived DT and related phenomena (i.e., low confidence in ability to not use substances when distressed) have been linked to greater alcohol (Berking et al., 2011) and cannabis (Gullo et al., 2017) consumption following psychosocial treatment. Thus, as with internalizing disorders, extant cross-sectional, prospective, and treatment outcome data suggest that low perceived DT is a marker of current substance use problem severity and possibly a vulnerability factor for the course of substance use disorders. However, the absence of data on perceived DT among healthy individuals prior to SUD onset or among individuals with remitted SUDs precludes conclusions about its possible status as a vulnerability factor for SUDs.
Given the high co-morbidity among internalizing and SUDs (e.g., Compton et al., 2007), it is plausible that perceived DT is lowest among individuals with co-morbid internalizing and SUDs. However, little research has been conducted on the unique effects of internalizing and SUDs on perceived DT. Ozdel and Ekinci (2014) found that, relative to healthy controls, patients with current co-morbid SUD and internalizing disorders as well as those who only have a current SUD had significantly lower perceived DT, and the co-morbid group reported significantly lower perceived DT than the SUD-only group. These studies did not have an internalizing disorder only group – thus, leaving open the possibility that low perceived DT is primarily associated with internalizing disorders rather than co-occurrence of internalizing and SUDs specifically. In sum, at present the nature of the relationship between perceived DT and internalizing/SUD co-morbidity is unclear.
Taken together, the extant cross-sectional, prospective, and treatment outcome data suggest that low perceived DT is relevant to current internalizing (and perhaps more robustly for distress-misery relative to fear disorders) as well as SUD symptom expression. The aim of the present study is to test two criteria of familial vulnerability factors outlined by Zubin and Spring (1977). First, levels of perceived DT in adults with remitted internalizing and SUD psychopathology were compared to those in healthy controls. It was hypothesized that DT would be lower in the remitted compared to the healthy sample, consistent with DT as a vulnerability factor. Further, within the remitted internalizing group, it was hypothesized that those with remitted distress-misery disorders would differ more from healthy controls than those with remitted fear disorders will. Second, perceived DT was compared within first-degree relatives across 256 families to determine if DT is familial. In line with the expectation that perceived DT is a vulnerability factor, it was hypothesized that perceived DT would be significantly correlated within families. Finally, given the conceptual/empirical overlap between DT and neuroticism (Kiselica et al., 2015; Leyro et al., 2010) as well as evidence that neuroticism is a familial vulnerability for internalizing psychopathology (Hettema et al., 2006; Klein et al, 2009), the present study examined whether these associations are present after adjusting for the effects of neuroticism. Adjusting for neuroticism also tests that the effects on psychopathology are due to the perceived tolerability of negative affect rather than just the frequency/intensity of negative affect.
Methods
Participants
A sample of 638 adults (mean age = 28.57 [SD = 12.41], 62.8% Female) with complete diagnostic and self-reported DT information were taken from a larger study examining familial neurobiological processes across a range of internalizing and externalizing diagnoses (see Weinberg et al., 2015; Gorka et al., 2016 for additional details). Participants were nested within 256 families and included 215 sibling pairs as well as the siblings’ other first-degree biological relatives who agreed to participate in the study. The sample included healthy controls (33.6% with no lifetime history of psychopathology) as well as individuals with a wide range of psychopathologies. A Research Domain Criteria (RDoC) approach was taken to participant recruitment such that recruitment screening was agnostic to Diagnostic and Statistical Manual of Mental Disorders (DSM) diagnostic categories (beyond the exclusion criteria listed below). However, participants with elevated negative affect were oversampled to ensure that the sample was clinically relevant. Specifically, the Depression, Anxiety, and Stress Scale (Lovibond & Lovibond, 1995) was administered during the initial phone screen to ensure that the severity of internalizing symptomology within the sample was normally distributed, but also had a higher average general psychological distress score (M = 10.35, SD = 10.07) than the general population (M =8.3 , SD = 9.83; Crawford et al., 2011). Further, participants with Alcohol Use Disorder (AUD) were oversampled given the peripheral aims of the larger study (Gorka et al., 2019).
Inclusion criteria for the larger family study included being between 18 and 30 years old and having at least one full biological sibling in the same age range that was also willing to participate. Siblings were similarly recruited regardless of DSM diagnostic categories. Both siblings participated in the study. At least one additional immediate family member (i.e., mother, father, or a third sibling) was also required to be willing and able to participate in the clinical interview portion of the study only (for the main aims of the larger study regarding whether various factors run in families). Exclusion criteria included personal or family history of psychosis or mania at the time of the interview (given that psychosis and mania have been shown to be separable from internalizing and externalizing disorders; Krueger et al., 1998; Markon, 2010), major medical or neurological illness, inability to read or write English, history of serious head trauma, and left-handedness (to protect against confounds with the neurophysiological data collected for the main aims of the larger study). Advertisements (fliers, internet postings, etc.) were used to recruit participants from the community and from mental health clinics. This IRB-approved investigation was carried out in accordance with the latest version of the Helsinki declaration and all participants provided informed consent after study procedures were explained.
To test the present study’s hypotheses regarding DT in individuals with remitted psychopathology vs. those without a history of psychopathology, individuals with psychopathology were excluded, leaving n sample of 409 (nested within 216 families). To test the present study’s hypothesis regarding the familial nature of DT, only the subsample in which each family had at least two members with DT scores was utilized (N=604 nested within 222 families).
Measures
Distress Tolerance Scale (DTS; Simons & Gaher, 2005)
The DTS is a self-report questionnaire that assesses an individual’s perceived capacity to withstand negative affect. Using a 1 (“Strongly agree”) to 5 (“Strongly disagree”) likert-type scale, respondents are asked to rate how strongly they agree with each of 15 statements (e.g., “feeling distressed or upset is unbearable to me”) that assess the typical thoughts and feelings they experience while experiencing distress. Lower scores indicate worse perceived DT. The DTS has demonstrated good internal consistency and moderate temporal stability in prior studies (Kiselica et al., 2014; Macatee et al., 2015; Simons & Gaher, 2005). In the present study, the DTS demonstrated good internal consistency (α=.93; M = 53.85, SD = 13.93).
Personality Inventory for DSM5-Negative Affect
The Negative Affect domain of the PID-5 (Krueger et al., 2012) was used to assess neuroticism. The PID-5 was designed to assess the personality traits of the alternative model of personality disorders in DSM-5 and is a 220-item self-report scale that measures five broad pathological personality domains (Negative Affect, Detachment, Antagonism, Disinhibition, and Psychoticism) and 25 underlying and related facets of these domains. Each PID-5 item is rated on a 4-point Likert scale ranging from 0 (very false or often false) to 3 (very true or often true). The Negative Affect domain has been shown to be strongly correlated with other measures of neuroticism (Watson et al., 2013). Three facets comprise the Negative Affect domain: Emotional Lability (e.g. “My emotions are unpredictable”), Anxiousness (e.g. “I worry about almost everything”), and Separation Insecurity (e.g. “I’d rather be in a bad relationship than be alone”). In the present study, the PID-5 Negative Affect domain demonstrated good internal consistency (α=.94; M=22.12, SD=15.31).
Structured Clinical Interview for DSM- 5 (SCID)
The SCID (First et al., 2015) is a semi-structured clinical interview used to assess whether an individual meets criteria for any diagnoses as defined by the fifth edition of the DSM. The following modules were administered in the current study: Major Depression, Alcohol Use Disorder, Substance Use Disorder, PTSD, Panic Disorder, Agoraphobia, Social Anxiety Disorder, Specific Phobia, OCD, GAD, Anorexia, Bulimia, Binge Eating Disorder, and the bipolar and psychotic screening modules. Doctoral students and bachelor’s level research assistants were trained to criterion on the SCID and supervised by a licensed clinical psychologist. Test-retest agreement was in the fair to substantial ranges for lifetime diagnoses (k’s =.46-.87) and in the fair to moderate ranges for current diagnoses (k’s =.54 -.74) with the exception of lifetime (k = .18) and current (k = .29) social anxiety disorder diagnoses, with interrater agreement in the slight range (Shankman et al., 2018; Shrout, 1998).
Data Analytic Plan
Of the 409 participants used to compare DT in individuals with vs. without a history of psychopathology, 24 did not have complete PID5-NA data. Twenty-two of these 24 participants had at least one family member with complete PID5-NA data and so the missing PID5-NA score was imputed by taking the mean of the available familial PID5-NA scores due to evidence that the PID5-NA runs in families (Katz et al., 2018). Thus, 409 participants nested within 216 families were available for the analyses without PID5-NA included as a covariate and 407 participants nested within 214 families were available for the analyses in which PID5-NA was included as a covariate.
Due to the nested structure of the data (i.e., persons nested within families), linear mixed effect models were used to test differences in DT between healthy individuals and those with a remitted internalizing and/or SUD, an analytic method that models both family-level and person-level variance. The family-level intercept was entered as a random (covariance structure: variance components) and fixed effect. History of an internalizing disorder (i.e., presence vs. absence), history of a SUD (i.e., presence vs. absence), and their interaction were entered as fixed effects. DTS score was the dependent variable. Non-significant fixed effects were removed from the model before significant effects were probed using pairwise comparisons. To determine if significant effects for DTS were attributable to neuroticism, PID5-NA score was entered as a fixed effect covariate and models were rerun to evaluate robustness.
To test whether DTS scores were correlated within families, a one-way random effects intraclass correlation coefficient (ICC) model was conducted on DTS scores utilizing all families that had at least two members with DTS data (N=604 nested within 222 families). Because families differed in the number of members with available DTS data, ICCs were computed with AgreeStat 2015.6.1 (Gwet, 2017) to handle missing data as described by Searle (1997). Of these 222 families, 18 had DTS data from both the mother and father. To determine if variability in the nature of genetic relatedness among family members contributed to our overall ICC estimate, an additional ICC model was run in which the mother or father’s DTS data was randomly selected from each of these 18 families and removed (i.e., to ensure each family only contained data from genetically-related members [all siblings or one parent+sibling(s)]) (N=586 nested within 222 families). Similarly, an additional ICC model was run using sibling data only (N=485 nested within 209 families).
Results
DT in Remitted Internalizing and SUD Psychopathology
The internalizing by SUD interaction, F(1,392.99)=0.12, p=.73, was non-significant and thus was removed from the model before main effects were examined. As expected, the main effect of internalizing disorder history on DTS scores was significant, F(1,405.64)=7.24, p=.007. Contrary to expectations, the main effect of SUD history on DTS scores, F(1,396.55)=1.52, p=.22, was non-significant. Individuals with a remitted internalizing disorder reported significantly lower DT (M=54.43, SE=1.04) relative to those without a lifetime internalizing disorder, M=58.40, SE=0.84), t(406.91)=3.07, p=.002. The internalizing disorder history main effect was no longer significant, F(1,402.86)=2.51, p=.11, after inclusion of PID5-NA as a covariate, F(1,400.81)=68.41, p<.001.
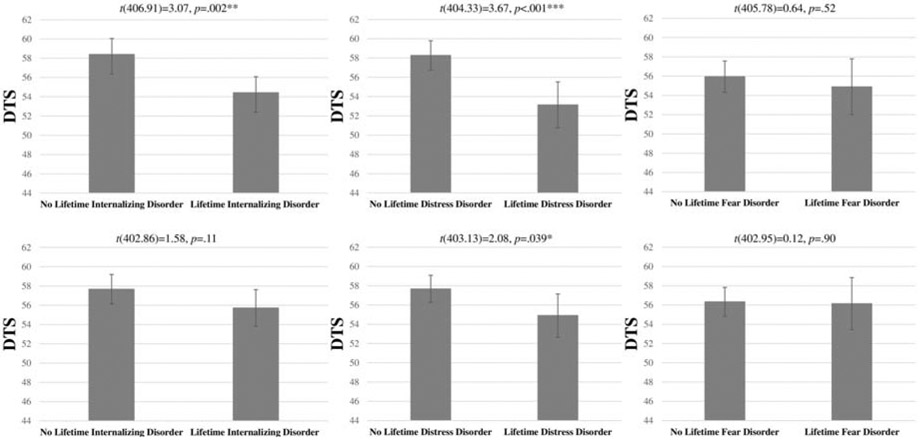
Given the heterogeneity of internalizing disorders, we examined whether the main effect of internalizing disorder history was attributable to fear and/or distress-misery disorders. Remitted distress-misery disorder (GAD, MDD, PTSD; n=113) and remitted fear disorder (Social Anxiety Disorder, Specific Phobia, Panic Disorder, OC-spectrum disorders; n=76) were entered simultaneously as dichotomous fixed effects in a mixed model predicting DTS scores. The main effect of distress-misery disorder history on DTS scores, F(1,399.98)=12.17, p=.001, was significant, whereas the main effect of fear disorder history was not, F(1,405.78)=0.41, p=.52. Individuals with a remitted distress-misery disorder reported significantly lower DT (M=53.15, SE=1.21) than those with no history of a distress-misery disorder (M=58.27, SE=0.77), t(404.33)=3.67, p<.001. Importantly, the effect of distress-misery disorder history was substantially reduced but remained significant, F(1,403.13)=4.31, p=.039, after inclusion of PID5-NA as a covariate, F(1,401.50)=65.97, p<.001 (see Figure 1).
Figure 1.
Distress Tolerance Scale (DTS) scores among those with vs. without a remitted internalizing (left column), distress-misery (middle column), or fear (right column) disorder are presented above. Estimated marginal means for the DTS score are presented without (top row) and with (bottom row) the Personality Inventory for the DSM-5 – Negative Affect subscale (PID5-NA) included as a covariate. *p<.05; **p<.01; ***p<.001.
Because of mixed findings on the loading of PTSD and OCD on the distress and fear factors (Forbes et al., 2011; Kotov et al., 2015; Raines et al., 2015; Slade & Watson, 2006), analyses were re-conducted without these disorders included in their respective groups; the effect of remitted distress-misery disorder remained significant, F(1,403.19)=8.69, p=.003, and the effect of remitted fear disorder remained non-significant, F(1,405.42)=1.46, p=.23. The effect of remitted distress-misery disorders became a trend after inclusion of PID5-NA as a covariate, F(1,403.54)=3.38, p=.067.
DT as Familial Vulnerability
As hypothesized, ICC analyses using all available family member data revealed that DTS scores were significantly correlated within families, ICC=.09, 95% CI [.09, ,55], p<.001. The ICC remained significant in the model that restricted family data to only siblings or sibling(s) with one parent, ICC=.08, 95% CI[.08, .49], p<.001, as well as the siblings-only model, ICC=.07, 95% CI[.07, .64], p<.001.
Discussion
The present study used several Zubin and Spring’s (1977) criteria to determine if perceived DT may be a vulnerability for internalizing and SUD psychopathology. Specifically, perceived DT was evaluated (1) in a sample of individuals without current psychopathology to determine if it is lower in individuals with remitted internalizing and substance use disorders relative to those with no history of psychopathology, and (2) within families to determine if perceived DT runs in families. Results revealed that perceived DT (1) was lower in individuals with a distress-misery but not fear or substance use disorder history relative to those with no history of psychopathology, and (2) significantly correlated within families. Further, perceived DT among individuals with a distress-misery disorder history remained lower than perceived DT in those with no history of psychopathology after adjusting for the effect of neuroticism. Together with prior studies showing inverse associations between perceived DT and current distress-misery disorder diagnoses/symptoms, the present results suggest that perceived DT may be an enduring, familial vulnerability for distress-misery disorders.
Perceived DT’s more robust association with distress-misery relative to fear disorders/symptoms has been demonstrated in some prior studies (e.g., Macatee et al., 2016), though other studies have found no significant differences between individuals with fear vs. distress-misery disorders (Allan et al., 2015) or found associations between perceived DT and specific symptom dimensions within fear disorders (e.g., obsessions in OCD; Cougle et al., 2011; Macatee et al., 2013). The present results suggest that prior findings of associations between perceived DT and current fear disorders may be attributable to co-morbid distress-misery disorders and/or state negative emotionality characteristic of active internalizing psychopathology in general. Importantly, the present study (1) ruled out that the effects for distress-misery disorder were due to comorbid lifetime fear disorders by covarying out whether the individual had a remitted fear disorder and (2) limited the influence of current symptoms on DTS ratings by excluding individuals with current psychopathology. Further, perceived DT remained lower in those with a past distress-misery diagnosis relative to individuals without any history of psychopathology after adjusting for the effect of neuroticism, suggesting that perceived tolerability of negative affect may be a vulnerability for distress-misery disorders independent of the propensity to experience frequent/intense negative affect.
Although the present results suggest that low perceived DT is an enduring characteristic of distress-misery psychopathology independent of active symptom expression, the present data cannot speak to whether low perceived DT is a pre-existing trait-like vulnerability for distress-misery disorders or an enduring scar. Another, not mutually-exclusive possibility is that low perceived DT is a pathoplastic factor in that it causally influences the expression of distress-misery disorders over time (Klein et al., 2009). In support of a pathoplastic interpretation, prior research has found that low perceived DT predicted greater maintenance/increases in worry symptoms one-month later (Macatee et al., 2015), and increases in perceived DT as a consequence of treatment predicted subsequent decreases in post-traumatic stress symptoms (Boffa et al., 2018). It is also possible that perceived DT functions as a pre-existing vulnerability for some distress-misery disorders (or some individuals), but functions as a scar or pathoplastic factor in others. Future longitudinal data examining initial onset, remission, and recurrence of distress-misery psychopathology is needed to adjudicate among these possibilities as well as identify factors that may moderate DT’s specific role.
The null association between perceived DT and remitted SUDs was unexpected. Prior findings were largely with samples with current SUD psychopathology (Allan et al., 2015; Macatee et al., 2018; Ozdel & Ekinci, 2014), suggesting that low perceived DT may be a state characteristic of an active SUD disorder as opposed to a vulnerability for SUDs. However, in the present study, remitted mild SUD, particularly mild Alcohol Use Disorder, was overrepresented in the remitted SUD subsample relative to those with a remitted moderate or severe SUD (57 out of 116), possibly limiting our ability to detect an effect if perceived DT is differentially relevant across substances and/or SUD severity. This sample bias likely reflects the larger study’s focus on oversampling individuals with elevated negative affect and, to a lesser extent, Alcohol Use Disorder. It also is important to note that the elimination of separate abuse and dependence categories in DSM-V makes it difficult to compare the present study’s finding to prior literature on perceived DT and addictive behavior which predominantly focused on substance dependence (e.g., Ozdel & Ekinci, 2014), a DSM-IV diagnosis that is most concordant with moderate to severe DSM-5 SUD (Compton et al., 2013). Future research in a remitted SUD sample with greater representation of individuals with moderate or severe SUD histories is needed to determine if perceived DT is a vulnerability for and/or scar of more severe forms of SUD psychopathology (e.g., substance dependence vs. abuse; Compton et al., 2013).
The significant correlation of perceived DT among family members suggests that perceived DT may be influenced by familial features such as shared environment (e.g., emotional invalidation; Linehan, 1993) and/or genetic factors (e.g., altered serotonergic functioning; Amstadter et al., 2012). However, the ICC point estimate was quite modest and identical to the lower-bound of the 95% CI, a circumstance that can occur when there is a small difference between 0 (i.e., the smallest possible ICC value), and the lower-bound of the 95% CI around the ICC point estimate. Thus, though the significant ICC suggests perceived DT is familial as hypothesized, the familial variance appears to be small. It is important to note that, though the ICC estimate is small, the magnitude of the ICC cannot be strictly interpreted as conventional interrater reliability since each rater is not actually rating the same target (e.g., behavior, diagnosis) but instead the target is hypothetical “family-level” DT; thus, familial variance may be underestimated using this approach. Future studies incorporating twin methodologies would be an important next step to understanding familial influences on DT. For example, twin studies have the potential to inform the relative contributions of environmental factors (e.g., distress-related learning experiences) and genetic factors on observed perceived DT scores. Given the complex interplay between genes and environment, twin designs also would be useful for informing our understanding of potential gene by environment (GxE) interactive effects on DT; for example, positive environmental influences (e.g., supportive relationships) have been shown to buffer against genetic risk for psychiatric disorders; Barr et al., 2017. This area of study would ultimately refine theoretical conceptualizations of DT, allowing for the nuance and complexity inherent in psychiatric risk.
With respect to clinical implications, significantly reduced perceived DT among individuals with remitted distress-misery psychopathology relative to healthy controls suggests that perceived DT may be a relevant target for interventions aimed at preventing relapse. Mindfulness-based cognitive therapy appears to be effective in preventing relapse among remitted patients with a history of multiple depressive episodes (Piet & Hougaard, 2011), and increases in perceived DT may be a relevant indicator of treatment response (though see Segal et al., 2019 for evidence that perceived DT increases are unrelated to depressive relapse risk). Future research should investigate the clinical relevance of perceived DT fluctuation in patients with remitted distress-misery psychopathology.
The present study had several limitations. First, risk of Type I error inflation and insufficient power prevented examination of individual disorders within the fear, distress, and SUD groups. Second, there was considerable variability in number of respondents per family which likely contributed to the ICC’s wide 95% CI. Third, the disproportionate representation of mild SUD in the remitted SUD group makes the null effects difficult to interpret given the lack of correspondence between mild SUD in DSM-5 and substance dependence in DSM-IV (Compton et al., 2013). Fourth, the present study focused on perceived DT rather than behaviorally-assessed DT which may have influenced the null SUD findings given the established sensitivity of behaviorally-assessed DT to clinically-relevant behaviors in SUD populations (Abrantes et al., 2008; Daughters et al., 2005; Reese et al., 2019; Strong et al., 2012). Finally, only one measure of perceived DT was utilized which may have impacted the null effects observed for remitted fear psychopathology (e.g., sensitivity to anxiety specifically may be more relevant to fear disorders).
Overall, the present study’s results suggest that perceived DT may be a familial vulnerability for or scar of distress-misery but not fear or SUD psychopathology, though the null findings for SUD psychopathology should be interpreted cautiously given the generally low SUD severity in the sample. Further, the modest amount of familial variance suggests that perceived DT is substantially influenced by the non-shared environment. Future longitudinal research is warranted to determine the role of perceived DT in initial onset, remission, and recurrence of distress-misery disorders.
Table 1.
Remitted Diagnoses in Internalizing Only, SUD Only, and Co-morbid Sub-groups
| Remitted Internalizing Only (n=93) (%) |
Remitted SUD Only (n=50) (%) |
Remitted Internalizing + SUD (n=66) (%) |
|
|---|---|---|---|
|
Lifetime Diagnosis | |||
|
Mood/Anxiety Dx | |||
| MDD | 55.9 | 0 | 69.7 |
| PTSD | 4.3 | 0 | 12.1 |
| GAD | 8.6 | 0 | 18.2 |
| SAD | 21.5 | 0 | 16.7 |
| PD | 7.5 | 0 | 7.6 |
| SP | 21.5 | 0 | 7.6 |
|
OC-Spectrum Dx | |||
| OCD | 6.5 | 0 | 3 |
| Trichotilloman | |||
| ia | 0 | 0 | 4.5 |
| Excoriation | 3.2 | 0 | 1.5 |
| BDD | 3.2 | 0 | 3 |
| Eating Dx | |||
| AN | 5.4 | 0 | 6.1 |
| BN | 0 | 0 | 3 |
| BED | 0 | 0 | 1.5 |
|
Substance Use Dx | |||
| Alcohol UD | 0 | 82 | 77.3 |
| Cannabis UD | 0 | 46 | 40.9 |
| Stimulant UD | 0 | 4 | 15.2 |
| Sedative UD | 0 | 0 | 1.5 |
| PCP UD | 0 | 0 | 1.5 |
| Hallucinogen | |||
| UD | 0 | 4 | 3 |
| Other UD | 0 | 0 | 1.5 |
Note. Dx=Diagnosis; MDD=Major depressive disorder; PTSD=Post-traumatic stress disorder; GAD=Generalized anxiety disorder; SAD=Social anxiety disorder; PD=Panic disorder; SP=Specific phobia; OC-spectrum=Obsessive-compulsive spectrum; OCD=Obsessive-compulsive disorder; BDD=Body dysmorphic disorder; AN=Anorexia nervosa; BN=Bulimia nervosa; BED=Binge-eating disorder; SUD=Substance Use Disorder; UD = use disorder.
Table 2.
Remitted SUDs in the sub-group with lifetime SUD(s) of mild severity only vs. the subgroup with lifetime moderate/severe SUD(s)
| Remitted Mild SUD (n=57) |
Remitted Moderate/Severe SUD (n=59) | ||
|---|---|---|---|
| Lifetime Diagnosis | Mild (%) | Any Severity (Mild, Moderate, or Severe) (%) | Moderate/Severe (%) |
| Alcohol UD | 78.9 | 79.7 | 64.4 |
| Cannabis UD | 29.8 | 55.9 | 47.4 |
| Stimulants UD | 3.5 | 16.9 | 13.6 |
| Sedatives UD | 0 | 1.7 | 0 |
| PCP UD | 0 | 1.7 | 1.7 |
| Hallucinogens UD | 0 | 6.8 | 5.1 |
| Other UD | 1.8 | 0 | 0 |
Note. SUD=Substance Use Disorder; Dx=Diagnosis; UD=Use disorder; PCP=Phencyclidine.
Highlights.
Low perceived distress tolerance (DT) is associated with current psychopathology
It is unknown if DT is a state marker or familial vulnerability for psychopathology
DT was measured in individuals varying in remitted disorders nested in families
DT was significantly correlated within families
DT was lower in those with a remitted distress disorder vs. healthy controls
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Abrantes AM, Strong DR, Lejuez CW, Kahler CW, Carpenter LL, Price LH, … & Brown RA (2008). The role of negative affect in risk for early lapse among low distress tolerance smokers. Addictive Behaviors, 33(11), 1394–1401. doi: 10.1016/j.addbeh.2008.06.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allan NP, Macatee RJ, Norr AM, Raines AM, & Schmidt NB (2015). Relations between common and specific factors of anxiety sensitivity and distress tolerance and fear, distress, and alcohol and substance use disorders. Journal of Anxiety Disorders, 33, 81–89. doi: 10.1016/j.janxdis.2015.05.002 [DOI] [PubMed] [Google Scholar]
- Amstadter AB, Daughters SB, MacPherson L, Reynolds EK, Danielson CK, Wang F, … & Lejuez CW (2012). Genetic associations with performance on a behavioral measure of distress intolerance. Journal of Psychiatric Research, 46(1), 87–94. doi: 10.1016/j.jpsychires.2011.09.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker TB, Piper ME, McCarthy DE, Majeskie MR, & Fiore MC (2004). Addiction motivation reformulated: an affective processing model of negative reinforcement. Psychological Review, 111(1), 33–51. [DOI] [PubMed] [Google Scholar]
- Banducci AN, Connolly KM, Vujanovic AA, Alvarez J, & Bonn-Miller MO (2017). The impact of changes in distress tolerance on PTSD symptom severity post-treatment among veterans in residential trauma treatment. Journal of Anxiety Disorders, 47, 99–105. doi: 10.1016/j.janxdis.2017.01.004 [DOI] [PubMed] [Google Scholar]
- Barr PB, Salvatore JE, Maes HH, Korhonen T, Latvala A, Aliev F, … & Dick DM (2017). Social relationships moderate genetic influences on heavy drinking in young adulthood. Journal of Studies on Alcohol and Drugs, 78(6), 817–826. doi: 10.15288/jsad.2017.78.817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berking M, Margraf M, Ebert D, Wupperman P, Hofmann SG, & Junghanns K (2011). Deficits in emotion-regulation skills predict alcohol use during and after cognitive–behavioral therapy for alcohol dependence. Journal of Consulting and Clinical Psychology, 79(3), 307–318. doi: 10.1037/a0023421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boffa JW, Short NA, Gibby BA, Stentz LA, & Schmidt NB (2018). Distress tolerance as a mechanism of PTSD symptom change: Evidence for mediation in a treatment-seeking sample. Psychiatry Research, 267, 400–408. doi: 10.1016/j.psychres.2018.03.085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compton WM, Dawson DA, Goldstein RB, & Grant BF (2013). Crosswalk between DSM-IV dependence and DSM-5 substance use disorders for opioids, cannabis, cocaine and alcohol. Drug and Alcohol Dependence, 132(1-2), 387–390. doi: 10.1016/j.drugalcdep.2013.02.036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compton WM, Thomas YF, Stinson FS, & Grant BF (2007). Prevalence, correlates, disability, and comorbidity of DSM-IV drug abuse and dependence in the United States: results from the national epidemiologic survey on alcohol and related conditions. Archives of General Psychiatry, 64(5), 566–576. doi: 10.1001/archpsyc.64.5.566 [DOI] [PubMed] [Google Scholar]
- Conway KP, Compton W, Stinson FS, & Grant BF (2006). Lifetime comorbidity of DSM-IV mood and anxiety disorders and specific drug use disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Clinical Psychiatry, 67(2), 247–257. doi: 10.4088/JCP.v67n0211 [DOI] [PubMed] [Google Scholar]
- Cougle JR, Timpano KR, Fitch KE, & Hawkins KA (2011). Distress tolerance and obsessions: An integrative analysis. Depression and Anxiety, 28(10), 906–914. doi: 10.1002/da.20846 [DOI] [PubMed] [Google Scholar]
- Crawford J, Cayley C, Lovibond PF, Wilson PH, & Hartley C (2011). Percentile norms and accompanying interval estimates from an Australian general adult population sample for self-report mood scales (BAI, BDI, CRSD, CES-D, DASS, DASS-21, STAI-X, STAI-Y, SRDS, and SRAS). Australian Psychologist, 46(1), 3–14. doi: 10.1111/j.1742-9544.2010.00003.x [DOI] [Google Scholar]
- Cummings JR, Bornovalova MA, Ojanen T, Hunt E, MacPherson L, & Lejuez C (2013). Time doesn’t change everything: The longitudinal course of distress tolerance and its relationship with externalizing and internalizing symptoms during early adolescence. Journal of Abnormal Child Psychology, 41(5), 735–748. doi: 10.1007/s10802-012-9704-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daughters SB, Lejuez CW, Bornovalova MA, Kahler CW, Strong DR, & Brown RA (2005). Distress tolerance as a predictor of early treatment dropout in a residential substance abuse treatment facility. Journal of Abnormal Psychology, 114(4), 729–734. doi: 10.1037/0021-843X.114.4.729 [DOI] [PubMed] [Google Scholar]
- Ellis AJ, Vanderlind WM, & Beevers CG (2013). Enhanced anger reactivity and reduced distress tolerance in major depressive disorder. Cognitive Therapy and Research, 37(3), 498–509. doi: 10.1007/s10608-012-9494-z [DOI] [Google Scholar]
- First MB, Williams JBW, Karg RS, & Spitzer RL (2015). Structured clinical interview for DSM-5—research version (SCID-5 for DSM-5, research version; SCID-5-RV). Arlington, VA: American Psychiatric Association, 1–94. [Google Scholar]
- Forbes D, Lockwood E, Elhai JD, Creamer M, O'Donnell M, Bryant R, … & Silove D (2011). An examination of the structure of posttraumatic stress disorder in relation to the anxiety and depressive disorders. Journal of Affective Disorders, 132(1-2), 165–172. doi: 10.1016/j.jad.2011.02.011 [DOI] [PubMed] [Google Scholar]
- Gorka SM, Hee D, Lieberman L, Mittal VA, Phan KL, & Shankman SA (2016). Reactivity to uncertain threat as a familial vulnerability factor for alcohol use disorder. Psychological Medicine, 46(16), 3349–3358. doi: 10.1017/S0033291716002415 [DOI] [PubMed] [Google Scholar]
- Gorka SM, Lieberman L, Kreutzer KA, Carrillo V, Weinberg A, & Shankman SA (2019). Error-related neural activity and alcohol use disorder: Differences from risk to remission. Progress in Neuropsychopharmacology & Biological Psychiatry, 92, 271–278. doi: 10.1016/j.pnpbp.2019.01.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Hasin DS, Stinson FS, Dawson DA, Ruan WJ, Goldstein RB, … & Huang B, (2005). Prevalence, correlates, co-morbidity, and comparative disability of DSM-IV generalized anxiety disorder in the USA: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Psychological Medicine, 35(12), 1747–1759. doi: 10.1017/S0033291705006069 [DOI] [PubMed] [Google Scholar]
- Gullo MJ, Matveeva M, Feeney GF, Young RM, & Connor JP (2017). Social cognitive predictors of treatment outcome in cannabis dependence. Drug and Alcohol Dependence, 170, 74–81. doi: 10.1016/j.drugalcdep.2016.10.030 [DOI] [PubMed] [Google Scholar]
- Gwet K (2017). AgreeStat for Windows: A Software for Analyzing the Extent of Agreement among Raters with MS Excel (Version 2015.6.1). Available from http://www.agreestat.com/ [Google Scholar]
- Hasan NS, Babson KA, Banducci AN, & Bonn-Miller MO (2015). The prospective effects of perceived and laboratory indices of distress tolerance on cannabis use following a self-guided quit attempt. Psychology of Addictive Behaviors, 29(4), 933–940. doi: 10.1037/adb0000132 [DOI] [PubMed] [Google Scholar]
- Hasin DS, O’Brien CP, Auriacombe M, Borges G, Bucholz K, Budney A, … & Schuckit M (2013). DSM-5 criteria for substance use disorders: recommendations and rationale. American Journal of Psychiatry, 170(8), 834–851. doi: 10.1176/appi.ajp.2013.12060782 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hettema JM, Neale MC, Myers JM, Prescott CA, & Kendler KS (2006). A population-based twin study of the relationship between neuroticism and internalizing disorders. American Journal of Psychiatry, 163(5), 857–864. doi: 10.1176/ajp.2006.163.5.857. [DOI] [PubMed] [Google Scholar]
- Katz AC, Hee D, Hooker CI, & Shankman SA (2018). A Family Study of the DSM-5 Section III Personality Pathology Model Using the Personality Inventory for the DSM-5 (PID-5). Journal of Personality Disorders, 32(6), 753–765. doi: 10.1521/pedi_2017_31_323 [DOI] [PubMed] [Google Scholar]
- Kendler KS, Prescott CA, Myers J, & Neale MC (2003). The structure of genetic and environmental risk factors for common psychiatric and substance use disorders in men and women. Archives of General Psychiatry, 60(9), 929–937. doi: 10.1001/archpsyc.60.9.929 [DOI] [PubMed] [Google Scholar]
- Keough ME, Riccardi CJ, Timpano KR, Mitchell MA, & Schmidt NB (2010). Anxiety symptomatology: The association with distress tolerance and anxiety sensitivity. Behavior Therapy, 41(4), 567–574. doi: 10.1016/j.beth.2010.04.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiselica AM, Rojas E, Bornovalova MA, & Dube C (2015). The nomological network of self-reported distress tolerance. Assessment, 22(6), 715–729. doi: 10.1177/1073191114559407 [DOI] [PubMed] [Google Scholar]
- Kiselica AM, Webber T, & Bornovalova MA (2014). Stability and change in distress tolerance and its prospective relationship with borderline personality features: A short-term longitudinal study. Personality Disorders: Theory, Research, and Treatment, 5(3), 247–256. doi: 10.1037/per0000076 [DOI] [PubMed] [Google Scholar]
- Klein DN, Durbin CE, & Shankman SA (2009). Depression and personality In Gotlib IH & Hammen CL (Eds.), Handbook of Depression, 2ndEd (pp. 93–112). New York: Guilford Press. [Google Scholar]
- Klein DN, Shankman SA, Lewinsohn PM, Rhode P, & Seeley JR (2004). Family study of chronic depression in a community sample of young adults. American Journal of Psychiatry, 161, 646–653. doi: 10.1176/appi.ajp.161.4.646 [DOI] [PubMed] [Google Scholar]
- Kotov R, Krueger RF, Watson D, Achenbach TM, Althoff RR, Bagby RM, … & Eaton NR (2017). The Hierarchical Taxonomy of Psychopathology (HiTOP): a dimensional alternative to traditional nosologies. Journal of Abnormal Psychology, 126(4), 454–477. doi: 10.1037/abn0000258 [DOI] [PubMed] [Google Scholar]
- Kotov R, Krueger RF, & Watson D (2018). A paradigm shift in psychiatric classification: the Hierarchical Taxonomy Of Psychopathology (HiTOP). World Psychiatry, 17(1), 24–25. doi: 10.1002/wps.20478 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotov R, Perlman G, Gámez W, & Watson D (2015). The structure and short-term stability of the emotional disorders: a dimensional approach. Psychological Medicine, 45(8), 1687–1698. doi: 10.1017/S0033291714002815 [DOI] [PubMed] [Google Scholar]
- Kraemer HC, Kazdin AE, Offord DR, Kessler RC, Jensen PS, & Kupfer DJ (1997). Coming to terms with the terms of risk. Archives of General Psychiatry, 54(4), 337–343. doi: 10.1001/archpsyc.1997.01830160065009 [DOI] [PubMed] [Google Scholar]
- Krueger RF (1999). The structure of common mental disorders. Archives of General Psychiatry, 56(10), 921–926. doi: 10.1001/archpsyc.56.10.921 [DOI] [PubMed] [Google Scholar]
- Krueger RF, Caspi A, Moffitt TE, & Silva PA (1998). The structure and stability of common mental disorders (DSM-III-R): a longitudinal-epidemiological study. Journal of Abnormal Psychology, 107(2), 216–227. doi: 10.1037/0021-843X.107.2.216 [DOI] [PubMed] [Google Scholar]
- Krueger RF, Derringer J, Markon KE, Watson D, & Skodol AE (2012). Initial construction of a maladaptive personality trait model and inventory for DSM-5. Psychological Medicine, 42(9), 1879–1890. doi: 10.1017/S0033291711002674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai HMX, Cleary M, Sitharthan T, & Hunt GE (2015). Prevalence of comorbid substance use, anxiety and mood disorders in epidemiological surveys, 1990–2014: a systematic review and meta-analysis. Drug and Alcohol Dependence, 154, 1–13. doi: 10.1016/j.drugalcdep.2015.05.031 [DOI] [PubMed] [Google Scholar]
- Laposa JM, Collimore KC, Hawley LL, & Rector NA (2015). Distress tolerance in OCD and anxiety disorders, and its relationship with anxiety sensitivity and intolerance of uncertainty. Journal of Anxiety Disorders, 33, 8–14. doi: 10.1016/j.janxdis.2015.04.003 [DOI] [PubMed] [Google Scholar]
- Leyro TM, Zvolensky MJ, & Bernstein A (2010). Distress tolerance and psychopathological symptoms and disorders: a review of the empirical literature among adults. Psychological Bulletin, 136(4), 576–600. doi: 10.1037/a0019712 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linehan MM (1993). Cognitive behavioural treatment of borderline personality disorder. New York: Guilford. [Google Scholar]
- Lovibond PF, & Lovibond SH (1995). The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behaviour Research and Therapy, 33(3), 335–343. doi: 10.1016/0005-7967(94)00075-U [DOI] [PubMed] [Google Scholar]
- Macatee RJ, Albanese BJ, Allan NP, Schmidt NB, & Cougle JR (2016). Distress intolerance as a moderator of the relationship between daily stressors and affective symptoms: Tests of incremental and prospective relationships. Journal of Affective Disorders, 206, 125–132. doi: 10.1016/j.jad.2016.07.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macatee RJ, Capron DW, Guthrie W, Schmidt NB, & Cougle JR (2015). Distress tolerance and pathological worry: tests of incremental and prospective relationships. Behavior Therapy, 46(4), 449–462. doi: 10.1016/j.beth.2015.03.003 [DOI] [PubMed] [Google Scholar]
- Macatee RJ, Capron DW, Schmidt NB, & Cougle JR (2013). An examination of low distress tolerance and life stressors as factors underlying obsessions. Journal of Psychiatric Research, 47(10), 1462–1468. doi: 10.1016/j.jpsychires.2013.06.019 [DOI] [PubMed] [Google Scholar]
- Macatee RJ, Albanese BJ, Crane NA, Okey SA, Cougle JR, & Schmidt NB (2018). Distress intolerance moderation of neurophysiological markers of response inhibition after induced stress: Relations with cannabis use disorder. Psychology of Addictive Behaviors, 32(8), 944–955. doi: 10.1037/adb0000418 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Markon KE (2010). Modeling psychopathology structure: a symptom-level analysis of Axis I and II disorders. Psychological Medicine, 40(2), 273–288. doi: 10.1017/S0033291709990183 [DOI] [PubMed] [Google Scholar]
- Marshall-Berenz EC, Vujanovic AA, Bonn-Miller MO, Bernstein A, & Zvolensky MJ (2010). Multimethod study of distress tolerance and PTSD symptom severity in a trauma-exposed community sample. Journal of Traumatic Stress, 23(5), 623–630. doi: 10.1002/jts.20568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McHugh RK, Daughters SB, Lejuez CW, Murray HW, Hearon BA, Gorka SM, & Otto MW (2011). Shared variance among self-report and behavioral measures of distress intolerance. Cognitive Therapy and Research, 35(3), 266–275. doi: 10.1007/s10608-010-9295-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McHugh RK, Kertz SJ, Weiss RB, Baskin-Sommers AR, Hearon BA, & Bjorgvinsson T (2014). Changes in distress intolerance and treatment outcome in a partial hospital setting. Behavior Therapy, 45(2), 232–240. doi: 10.1016/j.beth.2013.11.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McHugh RK, & Otto MW (2011). Domain-general and domain-specific strategies for the assessment of distress intolerance. Psychology of Addictive Behaviors, 25(4), 745–749. doi: 10.1037/a0025094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michel NM, Rowa K, Young L, & McCabe RE (2016). Emotional distress tolerance across anxiety disorders. Journal of Anxiety Disorders, 40, 94–103. doi: 10.1016/j.janxdis.2016.04.009 [DOI] [PubMed] [Google Scholar]
- Norr AM, Oglesby ME, Capron DW, Raines AM, Korte KJ, & Schmidt NB (2013). Evaluating the unique contribution of intolerance of uncertainty relative to other cognitive vulnerability factors in anxiety psychopathology. Journal of Affective Disorders, 151(1), 136–142. doi: 10.1016/j.jad.2013.05.063Get [DOI] [PubMed] [Google Scholar]
- Ormel J, Oldehinkel AJ, & Vollebergh W (2004). Vulnerability before, during, and after a major depressive episode: a 3-wave population-based study. Archives of General Psychiatry, 61(10), 990–996. doi: 10.1001/archpsyc.61.10.990 [DOI] [PubMed] [Google Scholar]
- Özdel K, & Ekinci S (2014). Distress intolerance in substance dependent patients. Comprehensive Psychiatry, 55(4), 960–965. doi: 10.1016/j.comppsych.2013.12.012 [DOI] [PubMed] [Google Scholar]
- Pesenti-Gritti P, Spatola CA, Fagnani C, Ogliari A, Patriarca V, Stazi MA, & Battaglia M (2008). The co-occurrence between internalizing and externalizing behaviors. European Child & Adolescent Psychiatry, 17(2), 82–92. doi: 10.1007/s00787-007-0639-7 [DOI] [PubMed] [Google Scholar]
- Raines AM, Allan NP, Oglesby ME, Short NA, & Schmidt NB (2015). Examination of the relations between obsessive–compulsive symptom dimensions and fear and distress disorder symptoms. Journal of Affective Disorders, 183, 253–257. doi: 10.1016/j.jad.2015.05.013 [DOI] [PubMed] [Google Scholar]
- Reese ED, Conway CC, Anand D, Bauer DJ, & Daughters SB (2019). Distress tolerance trajectories following substance use treatment. Journal of Consulting and Clinical psychology, 87(7), 645–656. doi: 10.1037/ccp0000403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seeley JR, Kosty DB, Farmer RF, & Lewinsohn PM (2011). The modeling of internalizing disorders on the basis of patterns of lifetime comorbidity: associations with psychosocial functioning and psychiatric disorders among first-degree relatives. Journal of Abnormal Psychology, 120(2), 308–321. doi: 10.1037/a0022621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shankman SA, Funkhouser CJ, Klein DN, Davila J, Lerner D, & Hee D (2018). Reliability and validity of severity dimensions of psychopathology assessed using the Structured Clinical Interview for DSM-5 (SCID). International Journal of Methods in Psychiatric Research, 27(1), e1590. doi: 10.1002/mpr.1590 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shankman SA, & Gorka SM (2015). Psychopathology research in the RDoC era: Unanswered questions and the importance of the psychophysiological unit of analysis. International Journal of Psychophysiology, 98, 330–337. doi: 10.1016/j.ijpsycho.2015.01.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shankman SA, & Klein DN (2003). The relation between depression and anxiety: an evaluation of the tripartite, approach-withdrawal and valence-arousal models. Clinical Psychology Review, 23(4), 605–637. doi: 0.1016/S0272-7358(03)00038-2 [DOI] [PubMed] [Google Scholar]
- Shrout PE (1998). Measurement reliability and agreement in psychiatry. Statistical Methods in Medical Research, 7(3), 301–317. doi: 10.1177/096228029800700306 [DOI] [PubMed] [Google Scholar]
- Simons JS, & Gaher RM (2005). The Distress Tolerance Scale: Development and validation of a self-report measure. Motivation and Emotion, 29(2), 83–102. doi: 10.1007/s11031-005-7955-3 [DOI] [Google Scholar]
- Slade TIM, & Watson D (2006). The structure of common DSM-IV and ICD-10 mental disorders in the Australian general population. Psychological Medicine, 36(11), 1593–1600. doi: 10.1017/S0033291706008452 [DOI] [PubMed] [Google Scholar]
- Strong DR, Brown RA, Sims M, Herman DS, Anderson BJ, & Stein MD (2012). Persistence during stress-challenge associated with lapse to opioid use during buprenorphine treatment. Journal of Addiction Medicine, 6(3), 219–225. doi: 10.1097/ADM.0b013e31825d927f [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vujanovic AA, Dutcher CD, & Berenz EC (2017). Multimodal examination of distress tolerance and posttraumatic stress disorder symptoms in acute-care psychiatric inpatients. Journal of Anxiety Disorders, 48, 45–53. doi: 10.1016/j.janxdis.2016.08.005 [DOI] [PubMed] [Google Scholar]
- Watson D (2005). Rethinking the mood and anxiety disorders: a quantitative hierarchical model for DSM-V. Journal of Abnormal Psychology, 114(4), 522–536. doi: 10.1037/0021-843X.114.4.522 [DOI] [PubMed] [Google Scholar]
- Wilamowska ZA, Thompson-Hollands J, Fairholme CP, Ellard KK, Farchione TJ, & Barlow DH (2010). Conceptual background, development, and preliminary data from the unified protocol for transdiagnostic treatment of emotional disorders. Depression and Anxiety, 27(10), 882–890. doi: 10.1002/da.20735 [DOI] [PubMed] [Google Scholar]
- Watson D, Stasik SM, Ro E, & Clark LA (2013). Integrating normal and pathological personality: Relating the DSM-5 trait-dimensional model to general traits of personality. Assessment, 20(3), 312–326. doi: 10.1177/1073191113485810 [DOI] [PubMed] [Google Scholar]
- Weinberg A, Liu H, Hajcak G, & Shankman SA (2015). Blunted neural response to rewards as a vulnerability factor for depression: Results from a family study. Journal of Abnormal Psychology, 124(4), 878–889. doi: 10.1037/abn0000081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zubin J, & Spring B (1977). Vulnerability: a new view of schizophrenia. Journal of Abnormal Psychology, 86(2), 103–126. doi: 10.1037/0021-843X.86.2.103 [DOI] [PubMed] [Google Scholar]