Abstract
Background
Hypertension is one of the leading causes of disease in the world. This study is a systematic review paper, intended to provide compressive evidence on the prevalence, distribution, determinants, and burden of hypertension in Ethiopia.
Methods
A quantitative epidemiological literature review was conducted by searching different articles in different databases, including PubMed, Cochrane, and Google scholar. The search involved population-based, hospital-based, and institution-based studies on hypertension conducted in Ethiopia. All data were extracted independently by two reviewers using data collection formats. Finally, this review included 22 studies.
Results
Different studies reported varied prevalence of hypertension because of the differences in participant’s mean ages, source population, and study settings. Population-based studies revealed the prevalence of hypertension to be 9.3–30.3%, institution-based studies revealed 7–37%, whereas hospital-based studies revealed 13.2–18.8%. In studies included in this review, about 37–78% of hypertensive patients were not aware of their blood pressure condition. There was a high prevalence of hypertension in urban residents, and different factors were associated with hypertension, including being overweight, family history of hypertension, age, sex, diabetes mellitus, alcohol intake, physical inactivity, and obesity.
Conclusion and Recommendation
Hypertension was substantially prevalent in Ethiopia, which calls for the implementation of timely and appropriate strategies for the prevention and control of the disease.
Keywords: hypertension, epidemiology, prevalence, associated factors, Ethiopia
Background
Hypertension (HTN) is a chronic medical condition characterized by elevated blood pressure (BP) in the arteries. It makes the heart work harder to circulate blood through the blood vessels.1 The World Health Organization (WHO) estimated that around 62% of cardiovascular diseases (CVDs) and 49% of ischemic heart diseases are attributable to high BP in the world.2 More than a quarter of the world’s population had HTN in 2000, and by 2025, it may increase to 1.56 billion.3 One major problem with HTN is its high mortality rate. According to the global report on the epidemiology of HTN, CVDs are responsible for the largest proportion of non-communicable disease (NCD) deaths in the world (48%), and raised BP is one of the leading behavioral and physiological risk factor to which 13% of global deaths are attributed.4 The other problem is death due to complications of the disease. According to a study on causes of death in 2008, of 17 million CVD deaths every year, complications of HTN account for 9.4 million deaths. HTN is responsible for at least 45% of deaths due to heart disease and 51% of deaths due to stroke.5
Hypertension is one risk factor for NCDs in Ethiopia. A meta-analysis on the prevalence of HTN in Ethiopia found that it is increasing with an estimated prevalence of 19.6%.6 In the last few years, the lifestyle of the Ethiopian population is changing due to urbanization and demographic transition. As a result, the burden of HTN could be on the rise.7,8
This systematic review compiles the available evidence regarding the prevalence, distribution, risk factors, and magnitude of awareness about HTN among the Ethiopian adult population. It provides information on the epidemiology of the disease to develop effective prevention and control strategies.
Methods
Study Search
The search included all papers on the epidemiology of HTN, conducted in Ethiopia, and available on PubMed, Cochrane, and Google Scholar. The study included articles providing data on HTN, prevalence, incidence, determinants, and associated factors. The search of the literature used the following keywords individually or in combination: HTN, Ethiopia, prevalence, determinants, and BP. The review included articles conducted between the years 2009 and 2016. The literature review was from May 2016 to August 2016.
Study Selection
The review included community, hospital, and institution-based cross-sectional studies conducted in Ethiopia and reported epidemiology of HTN. Besides, studies were selected if they have clear objectives, methodology, and if written in the English language.
Inclusion Criteria
Included literature
That involved age group of 15 years and above
That used a cut-off value of ≥140 for systolic and ≥ 90 mmHg for diastolic BP for classifying HTN
That used self-reported antihypertensive medication use for HTN
That used BP measurement on a single visit for classifying HTN
Study Outcomes
The outcome of this systematic review was the epidemiology of HTN in Ethiopia, including prevalence, distribution, risk factors, and awareness about the disease.
Data were extracted independently by two reviewers using data collection format, which includes data on the year of publication, a region of the study, age of participants, sample size, response rate, and study design. The review included, whenever information was available, the prevalence of HTN by age, gender, awareness of condition status, and rural-urban residence.
Results
Study Selection
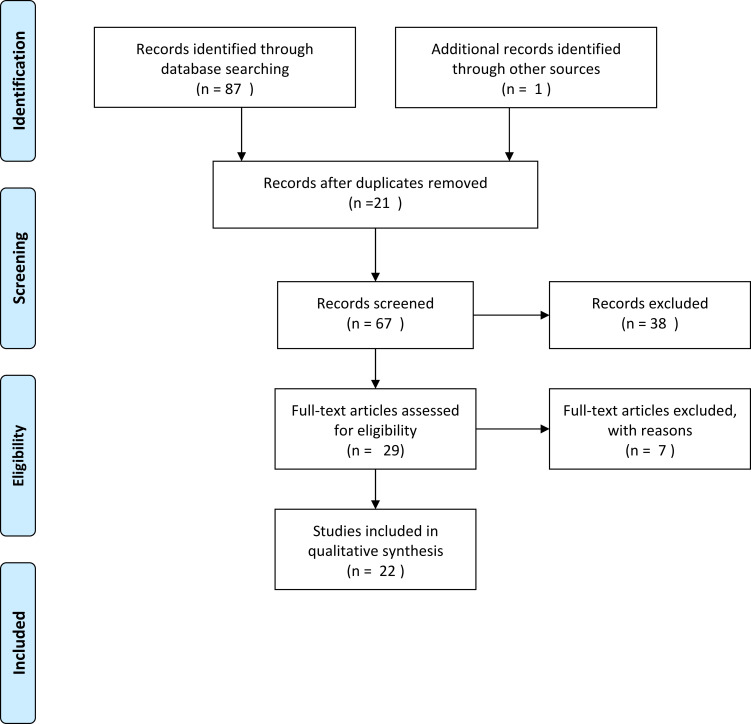
We found eighty-eight (88) studies on electronic search on PubMed, Google Scholar, and Cochrane. We rejected sixty-six (66) studies due to duplication (21 studies), title review (24), abstract review (14), and lack of relevant information (7). Finally, the systematic review included 22 articles (Figure 1).
Figure 1.
PRISMA Flow Diagram.
Notes: PRISMA figure adapted from Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group (2009). Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med 6(7): e1000097. doi:10.1371/journal.pmed1000097.42
Characteristics of the Studies
The studies described the epidemiology of HTN, such as prevalence, distribution, risk factors, and burden of the disease in Ethiopia. All are cross-sectional studies with a study population varying from 422 in Bedele/Oromia9 to 3273 in Addis Ababa10 and were conducted between the years 2009 and 2015. All included studies were done with different standardized ages and represented five regions of the country: (Amhara, Oromia, Southern Region, Tigray, and Addis Ababa). Among all, four studies included urban and rural areas.9,11–13 The rest studies included urban settings only (Table 1).
Table 1.
Summary of the Epidemiology of Hypertension in Ethiopia
| Author (Year of Publication) | The Region in the Country | Settings (Urban/Rural) | Study Base (Population Based/Hospital-Based) | Age of Subjects | Sample Size (Response Rate %) | Prevalence with Its 95% CI | Awareness | Assessed Risk Factors | Factors with Significant Association |
|---|---|---|---|---|---|---|---|---|---|
| Assefa et al, 201414 | Mekele/Tigray | Urban | Population | >18yr | 709(99.7) | 11% | - | Age, Education, Marital status, ALC, BMI | Age >41yrs, educated, OW, OB |
| Abdissa et al, 201415 | Adis Ababa | Urban | Population | >18 | 2716 | 25%(23.4–26.7) | Age, Sex, Residence | Being male, age | |
| Nshisso et al,201216 | Addis Ababa | Urban | Gov’t employee | >15 | 2153(100) | 19.1% (17.1–20.8) | 55% | Age, Sex, BMI | Age, DM |
| Tadesse & Alemu, 201417 | Gonder/Amhara | Urban | Institution based | ≥18 | 610 | 7.7% | - | Sex, Sleep, Weight, CS, Khat, ALC, BMI, PI | Being male, OW, sleep duration less than 5 hours |
| Abebe et al, 201511 | Gonder/Amhara | Urban & rural | Population | ≥35 | 2200 (97) | 27.9% (26.0, 29.8) | 59.0% | Age, FBG, ALC, OW, BMI, WS, Sex, Residence, PI | Age, ALC, FBG, OW |
| Guchiye & Enqusilasie, 201418 | Addis Ababa | Urban | Steel factory workers | ≥18 | 501 | 37.7% (0.3, 0.4) | 22.0% | Age, Sex, Marital status, FHH, Education, Income, ALC, OB, Job | Age, FHH, ALC, OB |
| Angaw et al, 201519 | Addis Ababa | Urban | Institution based | ≥18 | 655 (96) | 27.3% (23.3–31%) | - | Age, CS, ALC, Khat, FHH, BMI, SRDm | age >28 years, CS, FHH, SRDm, BMI |
| Gudina et al, 20149 | Bedele/Oromia | Urban | Population based | >15 yrs | 422(93.8) | 16.9%. | 44.8% | Age, Sex, Marital status, CS, Education, Khat, WS, ALC, PI, Salt | Age≥35, WS |
| Awoke et al, 201220 | Gondar/Amhara | Urban | Population | ≥ 35 | 679(97.6) | 28.3% (24.9–31.7) | 63% | Age, Education, Marital status, Job, SRDm, FHH, no cont. walking for 10mi/da, BMI, Vegetable eating | FHH, OB, SRDm, age≥55, no cont. walking for 10mi/da |
| Gudina et al, 201321 | Jimma/oromia | Urban & rural | Hospital-based | ≥ 15 | 774(94.83) | 13.2% (10.8–15.6) | 35.1% | Sex, FMH, BMI, Coffee, Khat, CS, OCP use, SRDm | FHH, SRDm, OW, OCP use |
| Giday et al, 201012 | Sidama zone/Southern Region | Urban & rural | Hospital/Population | 15–80 | 444/395(88.9) | 18.8% (15.1–23.1) | - | Ethnicity, DM, BMI, DM, Sex, FHH, WC, FHD | DM |
| Muluneh et al, 201213 | SW Ethiopia, Gilgel Gibe/Southern Region | Urban & rural | Population | 15–64 | 3223(81.3) | 9.3% (8.3–10.3) | 26% | Age, Sex, Residence | - |
| Helelo et al, 201322 | Durame/Southern region | Urban | Population | ≥ 31 | 518(98.6) | 22.4% (18.8–26) | 60% | Sex, Age, FHH, salt use, no cont. walking for 10mi/da, Vegetable eating, BMI | Male sex, FHH, OW, salt use, no cont. walking for 10mi/da |
| Tesfaye et al, 200910 | Addis Ababa | Urban | Population | 25–64 | 3273(88.1) | 30.3% (28.7–31.9) | 35.2% | Age, Sex, Education, BMI, PI, WS, ALC, Salt, CS, Ethnicity, Religion | Age, sex, BMI, PI, WS |
Abbreviations: ALC, alcohol; BP, blood pressure; BMI, body mass index; Cont, continuous; CS, cigaratte smoking; FHH, family history of hypertension; OW, over weight; OB, obesity (BMI>30); SRDm, self reported diabetes mellitus; WS, waist circumference; FBG, fasting blood glucose; PI, physical inactivity; OCP use, oral contraceptive use; FHD, family history of sudden death.
Prevalence of Hypertension in Ethiopia
Despite differences in study design, and study population characteristics (eg, age and gender distributions and community residences), available evidence suggest that hypertension is a growing health problem in Ethiopia. Several studies showed the prevalence of HTN in different regions of Ethiopia. Two population-based studies conducted in Addis Ababa revealed 30.3% and 25%, respectively.10,15 Other institution-based studies conducted in Addis Ababa on government employees, steel factory workers in Akaki, and civil servants in the ministry revealed hypertension prevalence to be 19.1%, 37.7%, and 27.3%, respectively.16,18,19 Studies conducted in other regions of Ethiopia, such as in North West Ethiopia, revealed the overall prevalence of hypertension in a population-based study to be 28. 3% and 27.9% at different times,11,20 while institution based study on college students of Gondar revealed a prevalence of 7.7%.17 Another population-based study in Northern Ethiopia, Mekele town, showed 11%.14 Several studies in the southern region of Ethiopia showed different prevalence. Population-based studies conducted at Gilgel Gibe research center, which involved around 3000 participants, showed 9.3%,13 while in Durame town in the same region, and with a much lesser sample size (518) showed 22.4%.22 Two studies, conducted in the Oromia region, a population-based study in Bedele town, and a hospital-based study in Jima, showed a prevalence of HTN 16.9% and 13.2%, respectively.9,21
Regarding sex-specific differences in the prevalence of HTN, studies in Ethiopia had different outcomes. Some studies showed a higher prevalence in males, such as a study in Addis Ababa, which revealed a huge difference, where the result was 40.1% in males and 22.4% in females.18 Other studies revealed 8% difference in males vs females.15,16,17 Some studies revealed a higher prevalence of HTN among women than men, even though the difference is small. According to a study conducted in federal ministry civil servants in Addis Ababa, 28.3% of females and 26.2% of males were hypertensive.19 Other studies also found a higher prevalence of HTN in females.11,20,23 In a study done in Mekele town, however, there was no significant difference.14
In this review, there was no study conducted in rural residents only, while only four studies included both urban and rural residents together. Those studies that compared the two residents revealed a higher prevalence of HTN in urban than in rural residents.11,13 A study conducted in Addis Ababa sub-cities showed an increase in the central part of the cities than the cities alongside.15
The major problem with HTN disease is that a significant number of the populations are not aware of their health status, which calls for appropriate and timely intervention. Most individuals with high BP do not have symptoms until a complication arises to result in sudden death from a heart attack or sudden intracranial bleeding or developed severe disability such as stroke as well as heart failure. According to a study in Southwest Ethiopia, the prevalence of high BP by self-report and physical measurement was 2.6% and 9.3%, respectively.13 A study conducted in Northwest Ethiopia also revealed among all subjects with HTN, 59.7% were not aware of their HTN until the time of the survey.11 A study in Addis Ababa workers also found out from the total of hypertensive patients, around 78.3% did not know of their condition.18
Risk Factors of Hypertension
Numerous studies conducted found out the risk factors of HTN together with its prevalence. Among non-modifiable factors, age was one of the significant risk factors for being hypertensive. A study on workers of a steel factory in Addis Ababa found that those in the age group 35–44, 45–54, and those ≥55 had 6, 7, and 12 times respectively higher risk of HTN when compared with the young age group 18–24 years.18 The same was true with a study done in Addis Ababa civil servants where participants with an age group ≥48 years and 38–47 years were six and three times more likely to be hypertensive as compared to those who were in the age category of 18–27 years respectively.19 The risk of HTN increases with age, especially for those who were greater than 55 years old.20,21 The prevalence increased significantly with increasing age with an increase of 10% per decade, especially for age group >65 years, and the risk of HTN was around 20 times more compared to those under 25 years of age.15 The association of age and HTN was also claimed by a study that found that when a person got older by one year, the risk of HTN occurrence increased by 6%.11
Another non-modifiable risk factor for HTN was family history. Different studies in Ethiopia claimed that individuals with a family history of HTN to be around three times more likely to have HTN than those with no family history.18–20,22
Among behavioral characteristics, being overweight was found to be positively associated with the odds of HTN. Those who were overweight/obese/body mass index (BMI) greater or equal to 25 kg/m2 were seven times more at risk for HTN.19,17,22,21 Other studies also claimed that obesity increases the risk of increased BP by four to five times compared to a normal BMI.20,14 Another study in Gondar found out that even a one-unit increase in BMI (kg/m2) increased the risk of HTN by 7%.11 On the other hand, a study revealed a high prevalence of metabolic syndrome among hypertensive patients attending follow up at the University of Gondar Hospital.24
Studies also found a positive association between regular alcohol drinkers and HTN. The chance of developing HTN increases by two to three times in regular drinkers than non-drinkers and irregular drinkers.11,18 According to a population-based cross-sectional survey on risk factors for HTN in Gilgel Gibe’s research center, southwest Ethiopia, drinking more than or equal to 4 drinks on a single occasion increases the risk of HTN by six times than non-drinkers.23 In a study conducted in Mekele town, however, there was no association observed with alcohol drinking and HTN.14 Another behavioral risk factor, those lacking physical activity (not walking at least for 10 minutes continuously daily) were about three times more likely to be hypertensive than those who did.20,22 Other factors that were associated with HTN were salt use,22 oral contraceptive use,21 sleeping less than 5 hours per day,17 and smoking.19 Khat chewing was not significantly associated with HTN in all studies reviewed18,20,21,23 while drinking coffee had a protective effect from HTN in one study reviewed.21
The review also indicates the association between HTN and diabetes mellitus (DM) particularly, with type 2 DM. The study on civil servants in Addis Ababa showed participants who had self-reported DM to be 13.56 times more likely to be hypertensive than non-diabetics.19 Other studies reported around 2 to 4 times higher risk of HTN in diabetic individuals compared to non-diabetic individuals.12,20,21 Another study in Northwest and on 2153 Adults in Addis Ababa also showed the association of DM with HTN.11,16
The Burden of Hypertension in Ethiopia
Hypertension is becoming a burden in Ethiopia, with a high rate of hospitalization and mortality. A study on pattern and trend of medical admissions of patients with chronic NCDs in selected hospitals in Addis Ababa found that, among patients who were attending outpatient clinics, about 40% were with CVDs. The study shows that the number of cardiovascular cases, including HTN, was 20,319, and the total numbers of hypertensive patients were 8843 (43.5%).25
From 49,309 deaths eligible for verbal autopsy, NCD caused 51% of the deaths, according to burial surveillance undertaken in Addis Ababa from 2006 to 2009. The leading causes of death were CVD (24%), of which the proportions for HTN and stroke were 12% and stroke 11%, respectively. Premature deaths (defined as earlier than age 65) from NCDs were mainly due to HTN and stroke in addition to others.26 A study on causes of death in Northern Ethiopia also revealed that 36.4% of the deaths were due to NCDs. Other causes include CVDs (17.9%), cerebrovascular disease (10.1%), ischemic heart disease (3.8%), congestive heart failure (2.0%), and hypertensive diseases (2%).27 In another study in the Amhara region, 6.5% of deaths were due to CVDs, including HTN among all age-groups.28
Discussion
Hypertension is a public health problem in developing countries, including Ethiopia. Based on available records, the present study attempted to synthesize the pieces of evidence on the epidemiology of HTN. The national prevalence of HTN in Ethiopia is 19.6%,6 which is lower than studies conducted on four sub-Saharan Africa countries and Uganda that revealed 25.9%29 and 26.4% prevalence, respectively.30
Regarding rural vs urban prevalence of HTN in Ethiopia, studies revealed a higher prevalence in urban areas than in rural areas. Different studies outside Ethiopia also showed urbanization to be a higher risk factor for HTN. A study in 4 sub-Saharan countries showed a higher prevalence in urban areas, which ranges from 20–25% and 7% in rural areas.29 Another study in Uganda also reveals a higher prevalence in urban areas.30 The difference in lifestyles of the population in urban areas like lack of physical activity, increased intake of an unhealthy diet, smoking, and increased stress could be the cause for the increased prevalence. The increased prevalence; could also be because of the increased use of motorized transport and occupation such as trade and office work.10
Concerning awareness of BP status, most of the studies in this review revealed that about 37%20 to 78%18 of hypertensive patients were not aware of their BP status. The reason could be because most individuals with high BP do not have symptoms until a complication arises, which may result in sudden death from a heart attack or sudden intracranial bleeding or severe disability such as stroke as well as heart failure.9 The other possible reason could be the low level of screening done in the country. This finding is in line with a study, in Nairobi Kenya,31 in 4 sub-Saharan countries (Uganda, in school teachers in South Africa and Tanzania, in nurses in Nigeria),29 and in Malaysia (50%).32 According to a systematic review conducted on awareness of HTN in Africa, the levels of awareness, treatment, and control varied widely from country to country, with the lowest levels found in rural communities in Nigeria (8%), Uganda (10%), and Gabon (9%). Studies that considered the elderly subjects showed the highest awareness rates (81% in urban elderly populations of Tunisia). On the other hand, a large multinational Epidemiological Trial of HTN in North Africa (ETHNA) that included 27,296 subjects revealed an awareness rate of 71% among hypertensive patients.33
Regarding risk factors for HTN from the non-modifiable risk factors, all studies included in this review revealed a significant association of age with HTN.18,20,21,23 The reason could be because of the biological effect of increased arterial resistance due to arterial thickening and stiffness as one gets older.11,34 This finding is in line with studies conducted in Malaysia, Uganda, India, and Afghanistan.30,32,35,36
In this systematic review, seven studies revealed a positive association of DM with HTN, especially with type two DM.11,12,16,19,20,21 A study in Afghanistan36 and in four sub-Saharan African countries (Uganda, South African and Tanzania, and Nigeria)29 showed a similar result. This positive association is because DM is commonly associated with obesity, which increases blood cholesterol and triglyceride levels, and lowers high-density lipoprotein levels.19 It also leads to vasculature complications, including atherosclerosis, which is known to contribute to various other disorders, including stroke, small and large vesicle disease, and coronary heart disease.16 Another reason could be because both DM and HTN share common risk factors or because the two conditions may cause each other.20 DM and HTN also share common pathways such as the sympathetic nervous system, renin-angiotensin-aldosterone system, oxidative stress, adipokines, and insulin resistance. These pathways interact and influence each other and may even cause a vicious cycle. HTN and DM are both results of the metabolic syndrome. They may, therefore, develop one after the other in the same individual.37 The effect of DM on the kidney could also play a role.1
Almost all studies in this systematic review found that being overweight to be significantly associated with high BP.14,20–23 A study in sub-Saharan Africa29 and Afghanistan36 showed similar results. The increased risk of HTN is because of the increased glucose, cholesterol, triglycerides, insulin, and reduced HDL in obese individuals.2,19
From other behavioral risk factors, the review found a positive association between alcohol and HTN in 3 studies reviewed. A study in rural Delhi, India, showed a similar result.38 Alcohol may increase BP by a different mechanism, such as by increasing: the sympathetic nervous system, cortisol, renin, calcium, angiotensin II, norepinephrine, and decreasing baroreceptor response.39 Drinking alcohol is also known to reduce the anti-hypertensive effect of medications.1
Lack of physical activity, not walking at least for 10 minutes continuously daily, was significantly associated with HTN,20,22 which is in line with a study conducted in Kenya.31 The reduced physical activity led to an increased obesity rate, which leads to adverse metabolic effects on BP, cholesterol, triglycerides, and insulin resistance.2 Physical activity reduces BP because of its direct lowering effect and also its effect on other metabolic factors, such as increased HDL cholesterol, improved glucose metabolism, and reduced body fat.1,2
Another risk factor for HTN is a family history of HTN. The possible mechanism for the correlation is the increased sodium reabsorption, genetic mutations in sodium transport, in kallikrein excretion, uric acid excretion, insulin secretion, in high-density LDL sub-fractions, fat pattern index, oxidative stress, and BMI.40 Increased salt intake is also associated with raised BP. The mechanism involved includes water retention, microvascular remodeling, change in vascular resistance.41 The possible reason for the link between smoking and HTN could be because of increased inflammation and stiffness caused by cigarettes.19
Limitation of the Review
This review did not attempt to synthesize trends in the prevalence of HTN because; the studies reviewed included different populations and age groups. On the other hand, variations in BP measurement methodology, age-range, and study site made it difficult for comparison of the studies.
Conclusions
As the available evidence showed, it is clear that HTN is a public health problem in Ethiopia, mainly in urban areas. Levels of prevalence, distribution, and mortality are ominously high, suggesting that increased complications of the disease such as stroke, heart failure, and renal failure will likely occur in the years to come. Besides, the level of awareness about the disease is low, suggesting a future increase in complications of the disease. The review identified both modified and non-modified risk factors for HTN. There is a pressing need to control the disease, especially by focusing on modifiable risk factors such as healthy lifestyles, physical activity, and reduced alcohol consumption. Other measures include improving other behavioral risk factors as a means of primary prevention and increasing awareness about HTN through public education.
Acknowledgments
The authors are thankful to all individuals who were involved in the research.
Funding Statement
This study received no support from a funding agency.
Abbreviations
BP, blood pressure; CVD, cardiovascular disease; DM, diabetes mellitus; HTN, hypertension; NCD, noncommunicable disease; WHO, World Health Organization.
Data Sharing Statement
The literature analyzed in the current study are available from online data sources by using the references listed.
Ethics Approval and Consent to Participate
Not applicable
Consent for Publication
Not applicable
Author Contributions
All authors contributed to data analysis, drafting or revising the article, have agreed on the journal to which the article will be submitted, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no competing interests for this work.
References
- 1.World Health Organization. International Society of Hypertension Guidelines for the management of hypertension. J Hypertension. 1999;17:151–183. [PubMed] [Google Scholar]
- 2.World Health Report. Reducing Risks, Promoting Healthy Life. 2002; Available from ttp://www.who.int/whr/2002/en. Accessed September28, 2020.
- 3.World Health Organization. Global status report on Noncommunicable diseases. 2014; Available from https://www.who.int/nmh/publications/ncd-status-report-2014/en/. Accessed September28, 2020.
- 4.World Health Organization. Epidemiology of hypertension. JAPI. 2013;61:12–13. [Google Scholar]
- 5.World Health Organization. Causes of Death. Geneva; 2008. Available from https://www.who.int/gho/mortality_burden_disease/causes_death_2008/en/. Accessed September28, 2020. [Google Scholar]
- 6.Kibret KT, Mesfin YM. Prevalence of hypertension in Ethiopia: a systematic meta-analysis. Public Health Rev. 2015;36(14). doi: 10.1186/s40985-015-0014-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.ICAP. Strengthening chronic disease services in Ethiopia. Lessons Learned from HIV/AIDS program implementation. 2010:11–17. Accessed from: https://www.ghdonline.org/uploads/ICAP_HIV-NCD_report_Feb2011.pdf. Accessed September28, 2020.
- 8.Central Statistical Agency (CSA). Ethiopia Demographic and Health Survey. Addis Ababa.: Central Statistical Authority; 2011:1–22. [Google Scholar]
- 9.Gudina EK, Bonsa F, Hajito KW. Prevalence of hypertension and associated factors in Bedele town, southwest Ethiopia. Ethiop J Health Sci. 2014;24(1):21–26. doi: 10.4314/ejhs.v24i1.3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tesfaye F, Byass P, Wall S. Population-based prevalence of high blood pressure among adults in Addis Ababa: uncovering a silent epidemic. BMC Cardiovasc Disord. 2009;9:39. doi: 10.1186/1471-2261-9-39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Abebe SM, Berhane Y, Worku A, Getachew A. Prevalence and associated factors of hypertension: a crossectional community based study in northwest ethiopia. PLoS One. 2015;10(4):1–11. doi: 10.1371/journal.pone.0125210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Giday A, Wolde M, Yihdego D. Hypertension, obesity and central obesity in diabetics and non-diabetics in Southern Ethiopia. Ethiop J Health Dev. 2010;24(2):145–147. doi: 10.4314/ejhd.v24i2.62964 [DOI] [Google Scholar]
- 13.Muluneh AT, Haileamlak A, Tessema F, Alemseged F, Woldemichael K, Asefa M. Population-based survey of chronic non-communicable diseases at Gilgel gibe field research center, southwest Ethiopia. Ethiop J Health Sci. 2012;22(5):7–18. [PMC free article] [PubMed] [Google Scholar]
- 14.Assefa BZ, Haftu BG, Alemayehu BK. Prevalence and associated factors of hypertension among adult population in Mekelle City, Northern Ethiopia. IJIPSR. 2014;2(3):653–668. [Google Scholar]
- 15.Abdissa SG, Feleke Y, Awol M. Prevalence of hypertension and pre-hypertension in Addis Ababa, Ethiopia: a survey done in recognition of World Hypertension Day, 2014. Ethiop J Health Dev. 2015;29(1):22–30. [Google Scholar]
- 16.Nshisso LD, Reesea A, Gelayea B, Lemma S, Berhane Y, Williamsa MA. Prevalence of hypertension and diabetes among Ethiopian adults diabetes. Metab Syndr. 2012;6(1):36–41. doi: 10.1016/j.dsx.2012.05.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tadesse T, Alemu H. Hypertension and associated factors among university students in Gondar, Ethiopia: a cross-sectional study. BMC Public Health. 2014;14:937. doi: 10.1186/1471-2458-14-937 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Guchiye B, Enquselasie F. Prevalence and Associated Factors of Hypertension Among Workers of Steel Factories. Akaki, Addis Ababa; 2014. Available from: http://localhost:80/xmlui/handle/123456789/6935. Accessed September28, 2020. [Google Scholar]
- 19.Angaw K, Dadi AF, Alene KA. Prevalence of hypertension among federal ministry civil servants in Addis Ababa, Ethiopia: a call for a workplace-screening program. BMC Cardiovasc Disord. 2015;15(76). doi: 10.1186/s12872-015-0062-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Awoke A, Awoke T, Alemu S, Megabiaw B. Prevalence and associated factors of hypertension among adults in Gondar, Northwest Ethiopia: a community based cross-sectional study. BMC Cardiovasc Disord. 2012;12(113):1–6. doi: 10.1186/1471-2261-12-113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gudina EK, Michael Y, Assegid S. Prevalence of hypertension and its risk factors in southwest Ethiopia: a hospital-based cross-sectional survey. Integr Blood Press Control. 2013;6:111–117. doi: 10.2147/IBPC.S47298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Helelo TP, Gelaw YA, Adane AA. Prevalence and associated factors of hypertension among adults in Durame. PLoS One. 2014;9(11):1–9 e112790. doi: 10.1371/journal.pone.0112790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Birlew T, Alemseged F. Risk factors for hypertension among adults. An analysis of survey data on chronic non-communicable disease at Gilgel gibe field research center, southwest Ethiopia. Sci J Public Health. 2015;3(2):281–290. doi: 10.11648/j.sjph.20150302.29 [DOI] [Google Scholar]
- 24.Tachebele B, Molla A, Zelalem A, Nebiyu M. Metabolic syndrome among hypertensive patients at University of Gondar Hospital, North West Ethiopia: a cross-sectional study. BMC Cardiovasc Disord. 2014;14(177). doi: 10.1186/1471-2261-14-177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bekele A, Teklie H, Tadesse M, et al. Pattern and trend of medical admissions of patients of chronic non-communicable diseases in selected hospitals in addis Ababa, Ethiopia. (Asrjets). 2015;13(1):34–48. [Google Scholar]
- 26.Misganaw A, Mariam DH, Araya T. The double mortality burden among adults in Addis, Ethiopia, 2006–2009. Prev Chronic Dis. 2012;9:E84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Melaku YA, Sahle BW, Tesfaye FH, Bezabih AM, Aregay A, Abera SF. Causes of death among adults in northern Ethiopia: evidence from verbal autopsy data in health and demographic surveillance system. PLoS One. 2014;9(9):e106781. doi: 10.1371/journal.pone.0106781 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fantahun M, Degu G. Burden of diseases in Amhara region, Ethiopia. Ethiop Med J. 2004;42:165–172. [PubMed] [Google Scholar]
- 29.Guwatudde D, Nankya-Mutyoba J, Kalyesubula R, Laurence C, Adebamowo C, Ajayi Bajunirwe F. The burden of hypertension in sub-Saharan Africa: a four-country cross-sectional study. BMC Public Health. 2015;15:1211. doi: 10.1186/s12889-015-2546-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Guwatudde D, Mutungi G, Wesonga R, Kajjura R, Kasule H, Muwonge J. The epidemiology of hypertension in Uganda: findings from the national non- communicable diseases risk factor survey. PLoS One. 2015;10(9):e0138991. doi: 10.1371/journal.pone.0138991 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Olack B, Wabwire-Mangen F, Smeeth L, Montgomery JM, Kiwanuka N, Breiman RF. Risk factors of hypertension among adults aged 35-64 years living in an urban slum Nairobi, Kenya. BMC Public Health. 2015;15:1251. doi: 10.1186/s12889-015-2610-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tee SR, Teoh XY, Rahman WA, et al. The prevalence of hypertension and its associated risk factors in two rural communities in Penang, Malaysia. IeJSME. 2010;4(2):27–40. [Google Scholar]
- 33.Kayima J, Kayima J, Wanyenze RK, Katamba A, Leontsini E, Nuwaha F. Hypertension awareness, treatment and control in Africa: a systematic review. BMC Cardiovasc Disord. 2013;13:54. doi: 10.1186/1471-2261-154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kotcher T. Harrison’s Principles of internal medicine In: Athonys F, Eugene B, Dennis K. editors. Hypertensive Vascular Disease. Vol. 2, 17th USA: McGraw-Hill Companies;2008:1549–1562 [Google Scholar]
- 35.Mahmood SE, Prakash D, Srivastava JP, Zaidi ZH, Bhardwaj P. Prevalence of hypertension amongst adult patients attending out patient department of urban health training centre, Department of Community Medicine, Era’s Lucknow Medical College and Hospital, Lucknow. J Clin Diagn Res. 2013;7(4):652–656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Saeed KMI. Prevalence of hypertension and associated factors in Jalalabad City, Nangarhar Province, Afghanistan. Central Asian J Global Health. 2015;4(1):2166–7403. doi: 10.5195/CAJGH.2015.134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cheung BMY, Chao L. Diabetes and Hypertension: is there a common metabolic pathway. Curr Atheroscler Rep. 14(2):160–166. doi: 10.1007/s11883-012-0227-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kishore J, Gupta N, Kohli Kumar C. Prevalence of hypertension and determination of its risk factors in rural Delhi. Int J Hypertens. 2016;Article ID 7962595:6. doi: 10.1155/2016/7962595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Husain K, Ansari RA, Ferder L. Alchohol-induced hypertension: mechanism and prevention. World J Cardiol. 2014;6(5):245–252. doi: 10.4330/wjc.v6.i5.245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ranasinghe P, Cooray DN, Jayawardena R, Katulanda P. The influence of family history of hypertension on disease prevalence and associated metabolic risk factors among Sri Lankan adults. BMC Public Health. 2015;15:576. doi: 10.1186/s12889-015-1927-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Grillo A, Salvi L, Coruzzi P, Salvi P, Parati G. Sodium intake, and hypertension. Nutrients. 2019;11(9):1970. doi: 10.3390/nu11091970 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group (2009). Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med 6(7): e1000097. doi: 10.1371/journal.pmed1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]