Introduction
The Apple Watch (Apple Inc, Cupertino, CA) is a class II medical device that features an electrocardiogram (ECG) monitoring feature that is primarily used for the detection of atrial fibrillation.1 With the increasing availability of the Apple Watch and other consumer-grade rhythm monitoring devices, identifying the strengths and limitations of utilizing these devices in the clinical setting, particularly during an era of increasing telemedicine, is of vital importance. Here we present a case demonstrating a specific limitation of the Apple Watch in the identification of atrial tachyarrhythmias and provide a solution to resolve this issue.
Case report
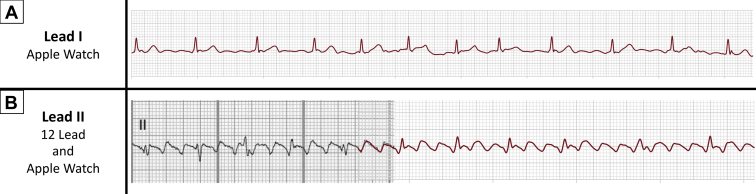
A 54-year-old woman with history of mechanical aortic valve replacement presented to the emergency department after experiencing dyspnea and being alerted to elevated heart rates by her fitness tracker. ECG revealed typical atrial flutter with variable atrioventricular conduction. She opted to undergo outpatient ablation and was discharged with rate control and continued anticoagulation. It was felt that continued home monitoring would be useful to determine if the patient had atrial fibrillation in addition to typical flutter. With permission, the authors attempted to determine if the morphology of atrial flutter could be identified in the ambulatory setting with only a consumer-grade mobile device. The standard series 5 Apple watch recording provides the equivalent of a lead I electrogram, and atrial flutter with variable atrioventricular conduction can be mistaken for atrial fibrillation (Figure 1A). Thus, an Apple watch was placed on the patient’s left thigh, and the right index finger was placed on the digital crown in order to obtain a lead II equivalent.2,3 The recording obtained via the Apple watch was then superimposed on the respective 12-lead ECG lead (Figure 1B).
Figure 1.
A: The Apple Watch (Apple Inc, Cupertino, CA) provides a lead I electrogram. In this standard configuration worn on the patient’s wrist, the patient’s atrial tachyarrhythmia appears consistent with atrial fibrillation. B: The same tachyarrhythmia is assessed using the Apple Watch in a lead II configuration by placing the watch on the patient’s thigh and placing the right index finger on the digital crown. In this configuration, the patient’s rhythm is actually identified to be typical atrial flutter with variable atrioventricular conduction. Superimposing the Apple Watch tracing over the patient’s standard lead II obtained via 12-lead demonstrates the accuracy of this method.
Discussion
While traditional event monitors and the Apple Watch allow for discovery of tachyarrhythmias, morphology identification can be difficult owing to the limited surface lead positions. This is particularly relevant in differentiating typical atrial flutter from atrial fibrillation because flutter waves are indistinct in lead I and can be mistaken for fibrillation waves. Using the equivalent of lead II described above identifies flutter wave morphology, allowing the diagnosis of typical flutter even when the atrioventricular conduction is variable. In our patient’s case, it was useful to catalog the rhythm in lead II daily to confirm she was persistently in typical flutter because patients with typical flutter may have atrial fibrillation at other times. The distinction is important in choosing an ablation strategy that could be limited to the cavotricuspid isthmus in patients with only atrial flutter vs additional pulmonary vein isolation for patients with atrial fibrillation. While up to 50% of patients with atrial flutter may develop atrial fibrillation at 5-year follow-up, an approach of a prophylactic pulmonary vein isolation in patients with only atrial flutter is controversial.4 Additionally, the ability to obtain multiple leads from hand-held consumer devices may prove useful in making accurate diagnoses in other clinical scenarios, including wide QRS complex tachycardia and coronary ischemia.5 Clinical decision-making including such data may help in reducing costs and avoiding hospitalization, especially in the current pandemic conditions. Further, these recordings can improve the quality of virtual Tele-Health visits by becoming part of the routine evaluation.
Conclusion
When utilizing consumer-grade rhythm monitoring devices in the clinical setting, it is important to identify the strengths and limitations of the particular device. Obtaining additional leads in a single-lead device allows for the accurate differentiation of atrial flutter from atrial fibrillation.
Key Teaching Points.
-
•
Atrial flutter with variable atrioventricular conduction can be mistaken for atrial fibrillation in lead I.
-
•
Handheld electrocardiography device–specific limitations in rhythm morphology identification can be overcome by obtaining additional leads.
-
•
Utilizing consumer grade devices to their fullest extent while understanding their limitations can be a useful adjunct during an era of increasing telemedicine.
Footnotes
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. The authors have no relevant financial disclosures.
References
- 1.Isakadze N., Martin S.S. How useful is the smartwatch ECG? Trends Cardiovascul Med. 2019;21:49. doi: 10.1016/j.tcm.2019.10.010. [DOI] [PubMed] [Google Scholar]
- 2.Cobos Gil M.A. Standard and Precordial Leads Obtained with an Apple Watch. Ann Intern Med. 2020;172:436–437. doi: 10.7326/M19-2018. [DOI] [PubMed] [Google Scholar]
- 3.Wilson F.N., Johnston F.D., MacLeod A.G. Electrocardiograms that represent the potential variations of a single electrode. Am Heart J. 1934;9:447–458. [Google Scholar]
- 4.Gula L.J., Skanes A.C., Klein G.J. Atrial flutter and atrial fibrillation ablation – sequential or combined? A cost-benefit and risk analysis of primary prevention pulmonary vein ablation. Heart Rhythm. 2016;13:1441–1448. doi: 10.1016/j.hrthm.2016.02.018. [DOI] [PubMed] [Google Scholar]
- 5.Drexler M., Elsner C., Gabelmann V., Gori T., Münzel T. Apple Watch detecting coronary ischaemia during chest pain episodes or an apple a day may keep myocardial infarction away. Eur Heart J. 2020;41:2224. doi: 10.1093/eurheartj/ehaa290. [DOI] [PMC free article] [PubMed] [Google Scholar]