Abstract
Objectives
Hip fragility fractures were regarded as one of the most severe, but recent papers report on the underestimated burden of vertebral compression fractures. This study aims to compare morbidity and mortality of hip and vertebral fragility fractures in patients treated in the same setting.
Methods
Patients aged ≥50 years with hip fracture, and those with vertebral fracture presenting to our hospital between January 2014 and January 2017 were included. Patients were evaluated 1 year after their index fracture. SF-36 scores, mortality, and institutionalization are then recorded. Patients were divided into 2 groups: hip fractures and vertebral fractures.
Results
There were 106 and 90 patients respectively evaluated in hip and vertebral fracture groups at 1 year. Patients in both groups were comparable for age, sex, comorbidities and neuropsychiatric condition (P > 0.05). At 1 year follow-up, SF-36 showed better averages in all 8 scales in hip fracture group compared to vertebral fracture group. Mortality in the hip fracture group reached 32.1% compared to 10% for the vertebral fracture group (P < 0.01). Fifteen patients were institutionalized in the hip fracture group compared to 18 patients in the vertebral fracture group (P > 0.05).
Conclusions
When comparing patients treated in the same setting, hip fracture is associated with significantly increased mortality than vertebral fracture; however, the latter is associated with more morbidity.
Keywords: Osteoporosis, Morbidity, Mortality, Vertebral fracture, Hip fracture
1. Introduction
A fragility fracture, which is a fracture sustained from a fall from standing height or less is mainly a consequence of osteoporosis [1,2]. These fractures are associated with increased morbidity and mortality in elderly patients, and place a large medical and economic burden on health care systems [[3], [4], [5]]. With the increased longevity actually recorded and expected to grow, incidence of fragility or osteoporosis related fractures will be rising steeply [6,7]. Therefore, the worldwide health and economic burden of these fractures is expected to increase accordingly [3,5,7]. The consequences of osteoporotic fractures for an individual range from chronic pain, loss of mobility, and loss of independence to institutionalization and death [8,9]. These consequences vary in impact and severity depending on the localization of the fracture. Hip fractures are usually regarded as the one of the most severe osteoporotic fractures being associated to the heaviest health burden regarding morbidity and mortality [10,11]. Patients with hip fragility fractures are expected to experience the greatest loss of their quality of life [[12], [13], [14]]. Less than 50% of patients are expected to reach their pre-injury functional status with the majority losing complete independence and being institutionalized [3,4,12,15,16]. About half of the patients report persistent pain one or more years after their hip fracture [13,14,17,18]. As for the mortality rate, hip fractures are associated with a 25–35% mortality rate at 1 year after the incident fracture, mostly due to age and comorbid diseases [[18], [19], [20], [21], [22]].
On the other hand, many recent reports state that symptomatic fragility vertebral fractures also result in marked movement limitations and affect quality of life, and especially that they are considered as the most frequent manifestation of osteoporosis [12,23,24]. They are associated with significant morbidity, and constitute an important independent risk factor for subsequent osteoporotic fractures [12,[24], [25], [26], [27]]. Pain and disability become worse with each new fracture, as does the risk of mortality [12,28]. Spinal mobility is impaired even in the absence of significant pain. Comorbidity is common, eg, kyphosis, restrictive lung disease and spinal stenosis, in particular at advanced ages, and contributes to the burden on quality of life and increased mortality [12,29,30]. Some registries reported an increased rate of 1 year mortality of 15% in men and 7% in women, related to vertebral fragility fractures [19,31]. Other prospective studies reported increased mortality related to vertebral fractures reaching 28% in long follow-up of patients with vertebral fractures requiring hospital admission [32,33].
Many medical structures around the world are conscious of this burden and are developing fracture liaising services in their premises, with the aim of capturing the fracture and making the first fracture the last [[34], [35], [36]]. There is scientific evidence supporting success of these structures in reducing morbidity and significantly reducing incidence of subsequent fracture through education and treatment [[37], [38], [39]].
In the absence of relevant studies comparing morbidity and mortality of hip and vertebral fragility fractures; and while the hip is still considered in many recent publications as the location of fragility fracture leading to the poorest health outcomes; we postulate that vertebral fragility fractures have comparable morbidity and mortality burden. We conducted this study to validate this hypothesis by comparing morbidity and mortality of hip and vertebral fragility fractures in patients treated in the same hospital through a well-established fracture liaison service.
2. Methods
This is a retrospective monocentric study on prospectively collected data, performed in our center of practice after approval by the ethical review board of this institution (BMC-18-000414) and followed the Declaration of Helsinki. All patients agreed to participate in the study and provided written informed consent.
2.1. Subjects
All patients aged 50 years and above, presenting to the emergency department of our institution with a hip (femoral neck or intertrochanteric) fragility fracture or a vertebral compression fracture between January 2014 and January 2017 are included in this study. Patients with history of previous fragility fractures were not excluded. Patients with history of cancer and patients with chronic kidney disease were excluded, reducing the confounding effect of possible pathologic fractures. Included patients are then divided into 2 groups according to their fracture site: hip fracture group and vertebral fracture group. All in all, 225 patients were included in the study. All patients were living in their homes with their respective families before the index fracture. Eleven patients were excluded for history of cancer or chronic kidney disease. One hundred and twenty patients were included in the hip fracture group and 105 patients were included in the vertebral fracture group. There were no patients presenting with both fractures in the same setting.
2.2. Data collection
Demographic data was recorded for each patient, together with the existing comorbidities (hypertension, diabetes, dyslipidemia, coronary artery disease, chronic lung disease), and neuropsychiatric disorders at the time of presentation. Through the fracture liaison service of our hospital, patients were regularly contacted and followed-up for chemical secondary prevention, fall prevention, and rehabilitation. Patients who agreed to come to the clinics were seen at 1 year after the index fracture. The primary outcome for both groups comparison was the 8-scale Short Form (SF-36) questionnaire score at 1 year of follow-up. The 8 scales have been aggregated into 2 summary measures, which are the Physical Component Summary (PCS) score and Mental Component Summary (MCS) score, which are also calculated [40]. Secondary outcomes were mortality rate, survival analysis, and institutionalization rate at 1 year of follow-up. Institutionalization rate refers to the rate of patients transferred to a long term care medical center during follow-up after becoming dependent in his/her activities of daily living.
2.3. Statistics
Mean values of quantitative variables (age, SF-36 scores) were compared using student t-test. Proportions of dichotomic variables (sex, mortality, and institutionalization) were compared using Chi square test. The statistical analysis was performed using IBM SPSS version 23.0 (SPSS Inc. Chicago, IL, USA). P value is considered significant when it is below 0.05.
3. Results
3.1. Demographic analysis and comorbidities
In the hip fracture group, 106 of the 120 patients (88%) agreed to participate in the study. Mean age averaged 75 years (55–85). Seventy-four (70%) patients presented with at least 1 comorbidity. Ten patients (9%) had concomitant neuropsychiatric condition (3 patients with depression; 7 patients with mild cognitive impairment).
In the vertebral fracture group, there were 90 of the 105 patients (86%) who decided to take part in this work. Mean age reached 74 years (60–87). Sixty-nine (73%) patients presented with at least 1 comorbidity at the time of their index fracture. Eight patients (9%) had concomitant neuropsychiatric conditions (2 patients with dementia and 6 patients with neuropsychiatric impairment).
Both groups were comparable in regard to demographic criteria, comorbidities and concomitant neuropsychiatric conditions. Table 1 summarizes the initial group characteristics and the statistical analyses. Patients who refused to participate (14 vs 15) were also comparable for their demographic and comorbidities distribution.
Table 1.
Demographic characteristics of patients in hip fragility fracture and vertebral fragility fracture groups, together with proportion of patients with 1 or more comorbidity in both groups and that of patients with concomitant neuropsychiatric disorders. The table shows also the results of the statistical analysis comparing both groups.
| Variable | Hip fragility fracture group (n = 106) | Vertebral fragility fracture group (n = 95) | P-value |
|---|---|---|---|
| Age mean, yr | 75.32 | 74.47 | 0.090 |
| Sex, number of females (%) | 69 (65) | 71 (75) | 0.088 |
| Patients with one or more comorbidity, number (%) | 74 (70) | 69 (73) | 0.125 |
| Patients with concomitant neuropsychiatric disorder, number (%) | 10 (9) | 8 (9) | 0.545 |
3.2. Short Form (SF)-36 questionnaire
Analysis of the results of the SF-36 questionnaire filled by the 196 patients in both groups revealed higher means in hip fracture patients for all 8 scales. Statistical comparison showed a significant difference between both groups in all scales except for limitation due to physical health rubric. Table 2 shows the detailed comparison and the statistical analysis of the 8 scales between both groups.
Table 2.
Detailed results and mean scores of the 8 items of the SF-36 in both groups, together with PCS and MCS components and rates of mortality and institutionalization in both groups. Results of statistical analysis of the comparison between both groups is also shown.
| Variable | Hip fragility fracture group (n = 106) | Vertebral fragility fracture group (n = 95) | P-value | |
|---|---|---|---|---|
| SF-36 | Physical functioning | 68.61 | 44.63 | P < 0.05 |
| Role limitations due to physical health | 54.17 | 49.38 | P > 0.05 | |
| General health | 75.00 | 55.00 | P < 0.05 | |
| Bodily pain | 77.86 | 57.18 | P < 0.05 | |
| Social functioning | 82.08 | 67.70 | P < 0.05 | |
| Vitality | 56.39 | 38.00 | P < 0.05 | |
| Mental health | 72.08 | 46.25 | P < 0.05 | |
| Role limitations due to emotional problems | 90.75 | 58.35 | P < 0.05 | |
| PCS | 66.91 | P < 0.05 | ||
| MCS | 73.33 | 50.58 | P < 0.05 | |
| Mortality | 34 (32%) | 10 (11%) | P < 0.05 | |
| Institutionalization | 15 (14%) | 18 (19%) | P > 0.05 | |
PCS, Physical Component Summary; MCS, Mental Component Summary.
SF-36 PCS averaged 62.54 ( ±10.35) in the hip fragility fracture group, compared to 45.75 ( ±9.4) in the vertebral fragility fracture group (P < 0.05). SF-36 MCS averaged 78.69 ( ±7.58) in the hip fragility group, compared to 55.37 ( ±8.89) in the vertebral fragility group (P < 0.05) (Table 2).
3.3. Mortality, survival analysis and institutionalization rates
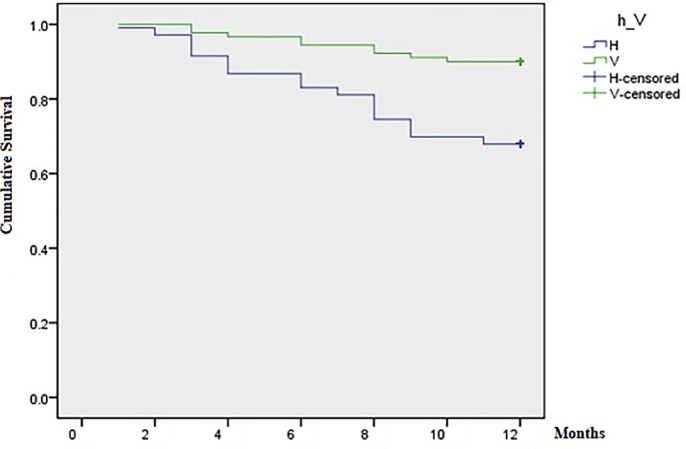
There were 34 patients who died during the first year of follow up (32%) in the hip fracture group, compared to 10 patients in the vertebral fracture group (11%) (P < 0.05). Of the 44 deaths recorded in this cohort, 30(68%) occurred after sudden cardiorespiratory arrest, 8(18%) were due to a severe sepsis from pulmonary origin, and 6(14%) were related to a severe sepsis from a urinary origin. Survival analysis yielded the Kaplan-Meier plot shown in Fig. 1. Survival in the vertebral fracture group was better than that in the hip fracture group throughout the study (P < 0.01).
Fig. 1.
Kaplan-Meier plot showing the survival analysis in both groups. The blue plot represents survival in the hip fracture group; the green plot represents survival in the vertebral fracture group. Survival in vertebral fracture group is better than that in hip fracture group throughout the study. H, hip fracture; V, vertebral fracture.
At the 1 year follow-up, 15 patients became dependent and were institutionalized in the hip fracture group (14%) compared to 18 patients in the vertebral fracture group (19%) (P > 0.05) (Table 2).
4. Discussion
We believe that this is the first scientific work in the medical literature that compare head to head mortality and morbidity of hip and vertebral fragility fractures in patients treated in the same setting and followed by the same team of physicians, through the same fracture liaison service [37]. This is of paramount importance after increasing reports showing high mortality and morbidity burden associated with vertebral fragility fractures, approaching that of hip fragility fractures, usually viewed as the one of the most severe fragility fractures with the highest impact on the patient health [12,24,30]. Therefore, a head to head comparison of health burden associated with hip fragility fractures and vertebral fragility fractures was needed.
The primary outcome of this study showed that patients with vertebral fragility fractures performed significantly worse in 7 of the 8 items of the SF-36 functional score. In one item, the role limitations due to physical health, patients with hip fractures performed better than patients with vertebral fragility fractures, but without reaching statistical significance. These results show that vertebral fragility fractures are associated with a higher morbidity when compared to hip fragility fractures, in patients comparable for age, sex distribution, and comorbidities status, treated in the same setting.
Survival analysis revealed a 32% mortality rate in patients with hip fragility fractures at 1 year of follow-up, contrasting with an 11% mortality rate in the vertebral fracture group. These rates are concordant with the reported rates in the available medical literature [3,12,18,22,31,41]. Survival in the vertebral fracture group was better than that of the hip fracture group throughout the 12 months of the study. What is added is the fact that these rates are reported in 2 comparable groups of patients treated in the same setting, followed by the same physicians, in the same hospital, and through the same fracture liaison service. One should keep in mind that the censoring effect as follow-up is limited to 12 months; whereas mortality associated to hip fragility fractures and vertebral fragility fractures will still be impacted for the upcoming years of follow-up. Moreover, patients lost to follow-up may also affect these results; however since comparable patients are lost to follow-up in both groups, this is not expected to impact the comparison.
Finally, this study showed that the institutionalization rate is comparable between both groups of patients, showing comparable results to the study published by Benzinger et al. [16].
Increased mortality associated with hip fragility fractures is not surprising; but the significant increased morbidity at 1 year of follow-up in patients with vertebral fragility fractures compared to that of patients with hip fragility fractures was mainly unexpected. This significantly increased morbidity could be related to the vertebral fracture itself, associated with severe back pain, aggravated spinal deformity, decreased mobility, and decreased pulmonary function through pulmonary restrictive syndrome, leading to severe restriction of independence and sometimes to institutionalization [12,33,41]. Moreover, exaggerated kyphosis associated with vertebral fractures may lead also to spinal stenosis, fatigue, early satiety and weight loss, and inactivity, leading to a higher risk of deep vein thrombosis and low self-esteem with significant emotional and social problems [12,42,43]. All of these factors may account for the significantly increased morbidity associated with vertebral fractures.
One un-evaluated factor impacted mortality in patients of this study: sarcopenia. Sarcopenia is characterized by loss of muscle mass and function with aging which increases risk of disability and death [44]. This factor is of paramount importance and should be assessed and treated as it was associated with increased mortality in patients with hip fractures and in those with vertebral fragility fractures [45,46]. Good management of these patients should include focus on rich and equilibrated dietary intake, physical rehabilitation, and fall prevention.
Patients were approached through a fully functional fracture liaison service (FLS) that showed its efficacy in improving osteoporosis diagnosis, secondary prevention through instauration and follow-up of compliance to medical treatment, thereby significantly reducing the incidence of subsequent osteoporotic fractures [37]. This may impact quality of life in patients of both groups as they are regularly contacted and followed-up by the fracture liaison nurse that reminds them of the importance of physical rehabilitation and fall prevention education. Although FLS did not impact mortality in fracture patients, they had a positive impact on quality of life with clinically significant improvements of functional capacity scores [37,47,48].
However, one should not jump easily into conclusions without taking into account several limitations for this study. First, being retrospective, this study risks selection bias and incomplete data collection. However, in our center, a prospectively collected data base for all patients hospitalized for fragility fractures was created since 2012, including their regular follow-ups in the clinics. Another limitation is probably the monocentric design. Including more centers could have led to more included cases, but also to divergent practices, organization and management. This would have also increased bias related to data collections, especially since our hospital is one of the rare hospitals in the region to have a fully functional and organized FLS. Patients dropping out to follow-up at 1 year might be a limitation; however, 196 of the 225 patients were included making the dropout rate as low as 13%, equally distributed between both groups with dropping out patients having comparable characteristics (age, sex, comorbidities). Another limitation is the lack of quality of life assessment before fractures. However, we know that all patients were living in their own homes before the index fracture, and that the institutionalization rate observed at 1 year of follow-up is mainly due to the morbidity associated to the fracture and the subsequent deterioration of the quality of life. One last limitation is the higher mortality observed in the hip fragility fracture group; as death might have reached patients with highest morbidity; leaving patients with lower morbidity alive, which may account in part for the difference of morbidity observed between both study groups.
5. Conclusions
When comparing patients treated in the same setting, by the same group of doctors and through the same fracture liaison service, comparable for demographic and health confounders except for the site of their fracture (hip fragility fracture vs vertebral fragility fracture), results are as follows: hip fragility fracture is associated with significantly more mortality then vertebral fracture; however, the latter is associated with more morbidity at 1 year following the index fracture. Both fractures are associated with comparable rates of institutionalization. Therefore, despite ongoing efforts to reduce hip fracture mortality, significant mortality is still observed even in a fracture liaison service setting. More efforts are to be invested in educating and closely following patients with vertebral fragility fractures aiming to reduce the significantly increased morbidity associated with these fractures.
Conflicts of interest
No potential conflict of interest relevant to this article was reported.
CRediT author statement
Maroun Rizkallah: Conceptualization, Methodology, Writing - original draft. Falah Bachour: Methodology, Validation, Supervision. Mirvat el Khoury: Investigation, Resources, Data curation. Amer Sebaaly: Validation, Writing - review & editing, Supervision. Boutros Finianos: Investigation, Data curation, Writing - review & editing. Rawad el Hage: Methodology, Data curation, Supervision. Ghassan Maalouf: Conceptualization, Validation, Supervision, Project administration.
Acknowledgments
ORCID. Maroun Rizkallah: 0000-0003-2592-7841. Falah Bachour: 0000-0002-7899-6448. Mirvat el Khoury: 0000-0003-0770-5284. Amer Sebaaly: 0000-0002-2785-7835. Boutros Finianos: 0000-0002-8922-6705. Rawad el Hage: 0000-0002-1690-6742. Ghassan Maalouf: 0000-0002-1069-6553.
Footnotes
Peer review under responsibility of The Korean Society of Osteoporosis.
References
- 1.Cohn M.R., Gianakos A.L., Grueter K., Rosen N., Cong G.-T., Lane J.M. Update on the comprehensive approach to fragility fractures. J Orthop Trauma. 2018;32:480–490. doi: 10.1097/BOT.0000000000001244. [DOI] [PubMed] [Google Scholar]
- 2.Mo J., Huang K., Wang X., Sheng X., Wang Q., Fang X. The sensitivity of orthopaedic surgeons to the secondary prevention of fragility fractures. J Bone Joint Surg Am. 2018;100:e153. doi: 10.2106/JBJS.17.01297. [DOI] [PubMed] [Google Scholar]
- 3.Ballane G., Cauley J.A., Luckey M.M., Fuleihan G.E.-H. Secular trends in hip fractures worldwide: opposing trends East versus West. J Bone Miner Res. 2014;29:1745–1755. doi: 10.1002/jbmr.2218. [DOI] [PubMed] [Google Scholar]
- 4.Cauley J.A., Chalhoub D., Kassem A.M., Fuleihan G.E.-H. Geographic and ethnic disparities in osteoporotic fractures. Nat Rev Endocrinol. 2014;10:338–351. doi: 10.1038/nrendo.2014.51. [DOI] [PubMed] [Google Scholar]
- 5.Rosengren B.E., Karlsson M., Petersson I., Englund M. The 21st-century landscape of adult fractures: cohort study of a complete adult regional population. J Bone Miner Res. 2015;30:535–542. doi: 10.1002/jbmr.2370. [DOI] [PubMed] [Google Scholar]
- 6.Curran D., Maravic M., Kiefer P., Tochon V., Fardellone P. Epidemiology of osteoporosis-related fractures in France: a literature review. Joint Bone Spine. 2010;77:546–551. doi: 10.1016/j.jbspin.2010.02.006. [DOI] [PubMed] [Google Scholar]
- 7.Zhou J., Qin M.-Z., Liu Q., Liu J.-P. Investigation and analysis of osteoporosis, falls, and fragility fractures in elderly people in the Beijing area: a study on the bone health status of elderly people ≥ 80 years old with life self-care. Arch Osteoporos. 2017;12:108. doi: 10.1007/s11657-017-0408-2. [DOI] [PubMed] [Google Scholar]
- 8.Hernlund E., Svedbom A., Ivergård M., Compston J., Cooper C., Stenmark J. A report prepared in collaboration with the international osteoporosis foundation (IOF) and the European federation of pharmaceutical industry associations (EFPIA). Arch osteoporos. vol. 8. 2013. Osteoporosis in the European Union: medical management, epidemiology and economic burden; p. 136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Johnell O., Kanis J.A. An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int. 2006;17:1726–1733. doi: 10.1007/s00198-006-0172-4. [DOI] [PubMed] [Google Scholar]
- 10.Harvey N.C.W., McCloskey E.V., Mitchell P.J., Dawson-Hughes B., Pierroz D.D., Reginster J.-Y. Mind the (treatment) gap: a global perspective on current and future strategies for prevention of fragility fractures. Osteoporos Int. 2017;28:1507–1529. doi: 10.1007/s00198-016-3894-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zaheer S., LeBoff M.S., Feingold K.R., Anawalt B., Boyce A., Chrousos G. Osteoporosis: prevention and treatment [Internet] Endotext. 2000 Available from, http://www.ncbi.nlm.nih.gov/pubmed/25905299. [Google Scholar]
- 12.Sànchez-Riera L., Wilson N. Fragility fractures & their impact on older people. Best Pract Res Clin Rheumatol. 2017;31:169–191. doi: 10.1016/j.berh.2017.10.001. [DOI] [PubMed] [Google Scholar]
- 13.Morin S.N., Lix L.M., Majumdar S.R., Leslie W.D. Temporal trends in the incidence of osteoporotic fractures. Curr Osteoporos Rep. 2013;11:263–269. doi: 10.1007/s11914-013-0168-x. [DOI] [PubMed] [Google Scholar]
- 14.Dyer S.M., Crotty M., Fairhall N., Magaziner J., Beaupre L.A., Cameron I.D. A critical review of the long-term disability outcomes following hip fracture. BMC Geriatr. 2016;16:158. doi: 10.1186/s12877-016-0332-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cauley J.A. Public health impact of osteoporosis. J Gerontol A Biol Sci Med Sci. 2013;68:1243–1251. doi: 10.1093/gerona/glt093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Benzinger P., Riem S., Bauer J., Jaensch A., Becker C., Büchele G. Risk of institutionalization following fragility fractures in older people. Osteoporos Int. 2019;30:1363–1370. doi: 10.1007/s00198-019-04922-x. [DOI] [PubMed] [Google Scholar]
- 17.Ha Y.-C., Baek J.-H., Ko Y.-B., Park S.-M., Song S.-H. High mortality and poor morbidity after hip fracture in patients with previous vertebral fractures. J Bone Miner Metab. 2015;33:547–552. doi: 10.1007/s00774-014-0616-4. [DOI] [PubMed] [Google Scholar]
- 18.Sadat-Ali M., Alfaraidy M., AlHawas A., Al-Othman A.A., Al-Dakheel D.A., Tayara B.K. Morbidity and mortality after fragility hip fracture in a Saudi Arabian population: report from a single center. J Int Med Res. 2017;45:1175–1180. doi: 10.1177/0300060517706283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kang H.-Y., Yang K., Kim Y.N., Moon S., Choi W.-J., Kang D.R. Incidence and mortality of hip fracture among the elderly population in South Korea: a population-based study using the national health insurance claims data. BMC Public Health. 2010;10:230. doi: 10.1186/1471-2458-10-230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.de Bruin I.J.A., Klop C., Wyers C.E., Overbeek J.A., Geusens P.P.M.M., van den Bergh Jpw All-cause mortality with current and past use of antidepressants or benzodiazepines after major osteoporotic and hip fracture. Osteoporos Int. 2019;30:573–581. doi: 10.1007/s00198-019-04851-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Reguant F., Arnau A., Lorente J.V., Maestro L., Bosch J. Efficacy of a multidisciplinary approach on postoperative morbidity and mortality of elderly patients with hip fracture. J Clin Anesth. 2019;53:11–19. doi: 10.1016/j.jclinane.2018.09.029. [DOI] [PubMed] [Google Scholar]
- 22.Katsoulis M., Benetou V., Karapetyan T., Feskanich D., Grodstein F., Pettersson-Kymmer U. Excess mortality after hip fracture in elderly persons from Europe and the USA: the CHANCES project. J Intern Med. 2017;281:300–310. doi: 10.1111/joim.12586. [DOI] [PubMed] [Google Scholar]
- 23.Ong T., Kantachuvesiri P., Sahota O., Gladman J.R.F. Characteristics and outcomes of hospitalised patients with vertebral fragility fractures: a systematic review. Age Ageing. 2018;47:17–25. doi: 10.1093/ageing/afx079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gerdhem P. Osteoporosis and fragility fractures: vertebral fractures. Best Pract Res Clin Rheumatol. 2013;27:743–755. doi: 10.1016/j.berh.2014.01.002. [DOI] [PubMed] [Google Scholar]
- 25.Bleibler F., Rapp K., Jaensch A., Becker C., König H.-H. Expected lifetime numbers and costs of fractures in postmenopausal women with and without osteoporosis in Germany: a discrete event simulation model. BMC Health Serv Res. 2014;14:284. doi: 10.1186/1472-6963-14-284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nazrun A.S., Tzar M.N., Mokhtar S.A., Mohamed I.N. A systematic review of the outcomes of osteoporotic fracture patients after hospital discharge: morbidity, subsequent fractures, and mortality. Ther Clin Risk Manag. 2014;10:937–948. doi: 10.2147/TCRM.S72456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sebaaly A., Rizkallah M., Bachour F., Atallah F., Moreau P.E., Maalouf G. Percutaneous cement augmentation for osteoporotic vertebral fractures. EFORT open Rev. 2017;2:293–299. doi: 10.1302/2058-5241.2.160057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kim T.-Y., Jang S., Park C.-M., Lee A., Lee Y.-K., Kim H.-Y. Trends of incidence, mortality, and future projection of spinal fractures in Korea using nationwide claims data. J Korean Med Sci. 2016;31:801–805. doi: 10.3346/jkms.2016.31.5.801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Alexandru D., So W. Evaluation and management of vertebral compression fractures. Perm J. 2012;16:46–51. doi: 10.7812/tpp/12-037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schupfner R., Stoevelaar H. The appropriate management of osteoporotic vertebral compression Fractures : a single Institute evaluation using the VCF monitor. Acta Orthop Belg. 2017;83:506–511. [PubMed] [Google Scholar]
- 31.Lee Y.-K., Jang S., Jang S., Lee H.J., Park C., Ha Y.-C. Mortality after vertebral fracture in Korea: analysis of the national claim registry. Osteoporos Int. 2012;23:1859–1865. doi: 10.1007/s00198-011-1833-5. [DOI] [PubMed] [Google Scholar]
- 32.Kado D.M., Browner W.S., Palermo L., Nevitt M.C., Genant H.K., Cummings S.R. Vertebral fractures and mortality in older women: a prospective study. Study of Osteoporotic Fractures Research Group. Arch Intern Med. 1999;159:1215–1220. doi: 10.1001/archinte.159.11.1215. [DOI] [PubMed] [Google Scholar]
- 33.Kanis J.A., Oden A., Johnell O., De Laet C., Jonsson B. Excess mortality after hospitalisation for vertebral fracture. Osteoporos Int. 2004;15:108–112. doi: 10.1007/s00198-003-1516-y. [DOI] [PubMed] [Google Scholar]
- 34.Rizkallah M., Sebaaly A., Maalouf G., Khoury M., Bachour F. Commentary: where are we from the Implementation of fragility fracture guidelines in Lebanon? J Yoga Phys Ther. 2016;6 http://www.omicsonline.org/open-access/commentary-where-are-we-from-the-implementation-of-fragility-fractureguidelines-in-lebanon-2157-7595-1000244.php?aid=75049 [Google Scholar]
- 35.Briot K. Fracture liaison services. Curr Opin Rheumatol. 2017;29:416–421. doi: 10.1097/BOR.0000000000000401. [DOI] [PubMed] [Google Scholar]
- 36.Shipman K.E., Doyle A., Arden H., Jones T., Gittoes N.J. Development of fracture liaison services: what have we learned? Injury. 2017;48 doi: 10.1016/j.injury.2017.08.030. Suppl 7:S4–9. [DOI] [PubMed] [Google Scholar]
- 37.Bachour F., Rizkallah M., Sebaaly A., Barakat A., Razzouk H., El Hage R. Fracture liaison service: report on the first successful experience from the Middle East. Arch Osteoporos. 2017;12:79. doi: 10.1007/s11657-017-0372-x. [DOI] [PubMed] [Google Scholar]
- 38.Andreasen C., Solberg L.B., Basso T., Borgen T.T., Dahl C., Wisløff T. Effect of a fracture liaison service on the rate of subsequent fracture among patients with a fragility fracture in the Norwegian capture the fracture Initiative (NoFRACT): a trial protocol. JAMA Netw open. 2018;1 doi: 10.1001/jamanetworkopen.2018.5701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wasfie T., Jackson A., Brock C., Galovska S., McCullough J.R., Burgess J.A. Does a fracture liaison service program minimize recurrent fragility fractures in the elderly with osteoporotic vertebral compression fractures? Am J Surg. 2019;217:557–560. doi: 10.1016/j.amjsurg.2018.09.027. [DOI] [PubMed] [Google Scholar]
- 40.Zhou K.N., Zhang M., Wu Q., Ji Z.H., Zhang X.M., Zhuang G.H. 4. Reliability, validity and sensitivity of the Chinese (simple) Short Form 36 health survey version 2 (SF-36v2) in patients with chronic hepatitis B. J Viral Hepat. 2013;20:e47–e55. doi: 10.1111/jvh.12030. [DOI] [PubMed] [Google Scholar]
- 41.Ballane G., Cauley J.A., Luckey M.M., El-Hajj Fuleihan G. Worldwide prevalence and incidence of osteoporotic vertebral fractures. Osteoporos Int. 2017;28:1531–1542. doi: 10.1007/s00198-017-3909-3. [DOI] [PubMed] [Google Scholar]
- 42.Svensson H.K., Olsson L.-E., Hansson T., Karlsson J., Hansson-Olofsson E. The effects of person-centered or other supportive interventions in older women with osteoporotic vertebral compression fractures-a systematic review of the literature. Osteoporos Int. 2017;28:2521–2540. doi: 10.1007/s00198-017-4099-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kammerlander C., Zegg M., Schmid R., Gosch M., Luger T.J., Blauth M. Fragility fractures requiring special consideration: vertebral fractures. Clin Geriatr Med. 2014;30:361–372. doi: 10.1016/j.cger.2014.01.011. [DOI] [PubMed] [Google Scholar]
- 44.Cruz-Jentoft A.J., Baeyens J.P., Bauer J.M., Boirie Y., Cederholm T., Landi F. Sarcopenia: European consensus on definition and diagnosis: report of the European working group on sarcopenia in older people. Age Ageing. 2010;39:412–423. doi: 10.1093/ageing/afq034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kim Y.K., Yi S.R., Lee Y.H., Kwon J., Jang S.I., Park S.H. Effect of sarcopenia on postoperative mortality in osteoporotic hip fracture patients. J Bone Metab. 2018;25:227. doi: 10.11005/jbm.2018.25.4.227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bayram S., Akgül T., Adıyaman A.E., Karalar Ş., Dölen D., Aydoseli A. Effect of sarcopenia on mortality after percutaneous vertebral augmentation treatment for osteoporotic vertebral compression fractures in elderly patients: a retrospective cohort study. World Neurosurg. 2020 doi: 10.1016/j.wneu.2020.02.121. 138:e354–60. [DOI] [PubMed] [Google Scholar]
- 47.Senay A., Perreault S., Delisle J., Morin S.N., Fernandes J.C. Performance of a fracture liaison service in an orthopaedic setting. J Bone Joint Surg Am. 2020;102:486–494. doi: 10.2106/JBJS.19.00185. [DOI] [PubMed] [Google Scholar]
- 48.Singh S., Whitehurst D.G., Funnell L., Scott V., MacDonald V., Leung P.-M. Breaking the cycle of recurrent fracture: implementing the first fracture liaison service (FLS) in British Columbia, Canada. Arch Osteoporos. 2019;14:116. doi: 10.1007/s11657-019-0662-6. [DOI] [PubMed] [Google Scholar]