Abstract
Several coronavirus disease 2019 (COVID-19) vaccines are currently in human trials. In June 2020, we surveyed 13,426 people in 19 countries to determine potential acceptance rates and factors influencing acceptance of a COVID-19 vaccine. Of these, 71.5% of participants reported that they would be very or somewhat likely to take a COVID-19 vaccine, and 48.1% reported that they would accept their employer’s recommendation to do so. Differences in acceptance rates ranged from almost 90% (in China) to less than 55% (in Russia). Respondents reporting higher levels of trust in information from government sources were more likely to accept a vaccine and take their employer’s advice to do so.
Subject terms: Health policy, Health services, Public health
Survey data from across 19 countries reveal heterogeneity in attitudes toward acceptance of a COVID-19 vaccine and suggest that trust in government is associated with vaccine confidence.
Main
The COVID-19 pandemic is expected to continue to impose enormous burdens of morbidity and mortality while severely disrupting societies and economies worldwide. Governments must be ready to ensure large-scale, equitable access and distribution of a COVID-19 vaccine if and when a safe and effective one becomes available. This will require sufficient health system capacity, as well as strategies to enhance trust in and acceptance of the vaccine and those who deliver it.
In 2015, the World Health Organization (WHO) Strategic Advisory Group of Experts on Immunization defined vaccine hesitancy as a ’delay in acceptance or refusal of vaccination despite availability of vaccination services’1, which can vary in form and intensity based on when and where it occurs and what vaccine is involved, as has been confirmed in multiple studies2,3. Concern about vaccine hesitancy is growing worldwide4; in fact, WHO identified it as one of the top ten global health threats in 2019 (https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019). In many countries, vaccine hesitancy and misinformation present substantial obstacles to achieving coverage and community immunity5,6.
Governments, public health officials and advocacy groups must be prepared to address hesitancy and build vaccine literacy so that the public will accept immunization when appropriate. Anti-vaccination activists are already campaigning in multiple countries against the need for a vaccine, with some denying the existence of COVID-19 altogether7. Misinformation spread through multiple channels could have a considerable effect on the acceptance of a COVID-19 vaccine8. The accelerated pace of vaccine development has further heightened public anxieties and could compromise acceptance9.
Governments and societies must gauge current levels of willingness to receive a potentially safe and effective COVID-19 vaccine and identify correlates of vaccine hesitancy and/or acceptance. We present findings from a survey of the likelihood of vaccine acceptance from a sample of 13,426 respondents in 19 countries.
Results
Survey respondents represented a random sample of the populations of 19 countries that comprise around 55% of the global population. Their characteristics and a summary of their responses to the survey questions are listed in Table 1. Women were 53.5% of the study population, and 63.3% of all participants earned more than $32 per day. More than a third of the respondents (36.3%) had a university degree, and 62.4% were between 25 and 54 years old.
Table 1.
Description of participants and breakdown of the two COVID-19 vaccine questions
| Overall | |
|---|---|
| n | 13,426 |
| Gender (%) | |
| Female | 7,172 (53.5) |
| Male | 6,129 (45.8) |
| Other | 94 (0.7) |
| Gapminder income level (%) | |
| <US$ 2 per day | 447 (3.3) |
| $2–$8 per day | 840 (6.3) |
| $8–$32 per day | 3,011 (22.4) |
| $32+ per day | 8,498 (63.3) |
| Did not answer | 630 (4.7) |
| Education level (%) | |
| Less than high school | 3,830 (28.6) |
| High school or some college | 4,692 (35.0) |
| Bachelor’s degree | 3,694 (27.6) |
| Postgraduate degree | 1,179 (8.8) |
| Age group in years (%) | |
| 18–24 | 2,057 (15.4) |
| 25–54 | 8,360 (62.4) |
| 55–64 | 1,493 (11.1) |
| 65+ | 1,485 (11.1) |
| Accept COVID-19 vaccine if generally available (%) | |
| Completely agree | 6,288 (46.8) |
| Somewhat agree | 3,316 (24.7) |
| Neutral/no opinion | 1,912 (14.2) |
| Somewhat disagree | 819 (6.1) |
| Completely disagree | 1,091 (8.1) |
| Accept COVID-19 vaccine if employer recommended it (%) | |
| Completely agree | 1,881 (14.0) |
| Somewhat agree | 4,579 (34.1) |
| Neutral/no opinion | 3,488 (26.0) |
| Somewhat disagree | 2,299 (17.1) |
| Completely disagree | 1,179 (8.8) |
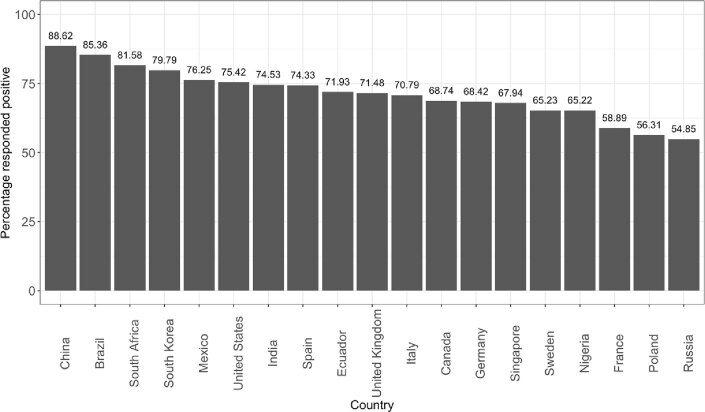
Respondents from China gave the highest proportion of positive responses (631 of 712 respondants, 88.6%) and the lowest proportion of negative responses (5 of 712, 0.7%) when asked if they would take a ‘proven, safe and effective vaccine’. Respondents from Poland reported the highest proportion of negative responses (182 of 666, 27.3%), whereas Russian respondents gave the lowest proportion of positive responses (373 of 680, 54.9%). The proportion of positive responses for all countries can be found in Extended Data Fig. 1.
Extended Data Fig. 1. ‘If a COVID-19 vaccine is proven safe and effective and is available, I will take it’.
Numbers above the bars represent the percent of respondents in each country who responded positively to the question ‘If a COVID-19 vaccine is proven safe and effective and is available, I will take it’.
When asked whether “You would accept a vaccine if it were recommended by your employer and was approved safe and effective by the government,” 14.0% (1,881 of 13,426) completely agreed, whereas 25.9% (3,478 of 13,426) somewhat or completely disagreed (Table 1). There was considerable variation by country, with China again having the highest proportion of positive responses (596 of 712, 83.7%) and the lowest proportion of negative responses (26 of 712, 3.7%). Russia had the highest proportion of negative responses (278 of 680, 40.9%) and the lowest proportion of respondents (184 of 680, 27.1%) willing to accept their employer’s recommendation (Supplementary Table 1).
Table 2 summarizes results for the 16 regressions: one set of eight univariate regressions for the positive outcomes for the two questions of interest against the four demographic variables: whether or not the respondent or a family member was sick, cases per million categorized as high/medium/low, mortality per million categorized as high/medium/low and trust in government. People aged 25–54, 55–64 and 65+ were more likely to accept the vaccine than those who were aged 18–24. This difference was strongest (odds ratio (OR) = 1.73; 95% confidence interval (CI) (1.48, 2.02)) when responses from the oldest age cohort and those from the youngest age cohort were compared (Table 2). A similar trend was observed in regard to acceptance of the vaccine if one’s employer required it, except that responses from the oldest age cohort were similar to the youngest age cohort. Gender differences were small, but the univariate association for both questions suggested that men were slightly less likely to respond positively than women, with an OR of 0.84 (95% CI (0.78, 0.91)) of men responding positively relative to women for the general question, and an OR of 0.93 (95% CI (0.87, 1.00)) for the business-related question.
Table 2.
Univariate regression outputs for vaccine acceptability questions against demographics and variables of interest
| Beta-coefficients of vaccine questions (95% CIs) | Beta-coefficients of business question (95% CIs) | |
|---|---|---|
| Age (years) | 25–54 vs 18–24, 1.12 (1.01, 1.25) | 25–54 vs 18–24, 1.22 (1.10, 1.34) |
| 55–64 vs 18–24, 1.21 (1.04, 1.40) | 55–64 vs 18–24, 1.17 (1.02, 1.33) | |
| 65+ vs 18–24, 1.73 (1.48, 2.02) | 65+ vs 18–24, 1.13 (0.99, 1.29) | |
| Sex | Male vs female, 0.84 (0.78, 0.91) | Male vs female, 0.93 (0.87, 1,00) |
| Other vs female, 0.22 (0.14, 0.33) | Other vs female, 0.68 (0.45, 1.03) | |
| Income | $2–$8 vs <$2, 1.38 (1.09, 1.74) | $2–8 vs <$2, 0.91 (0.72, 1.14) |
| $8–$32 vs <$2, 1.87 (1.53, 2.29) | $8–32 vs <$2, 1.04 (0.85, 1.27) | |
| $32+ vs <$2, 2.18 (1.79, 2.64) | $32+ vs <$2, 1.47 (1.21, 1.79) | |
| Refused vs <$2, 0.91 (0.71, 1.16) | Refused vs <$2, 0.78 (0.61, 1.00) | |
| Education | Medium vs low, 1.26 (1.15, 1.39) | Medium vs low, 1.26 (1.15, 1.37) |
| High vs low, 1.34 (1.21, 1.48) | High vs low, 1.24 (1.13, 1.36) | |
| Very high vs low, 1.45 (1.25, 1.69) | Very high vs low, 1.31 (1.15, 1.49) | |
| Myself or family sick with COVID-19 | Yes vs no, 0.97 (0.87, 1.08) | Yes vs no, 1.05 (0.96, 1.71) |
| Cases per million population | Middle vs low, 1.60 (1.46, 1.75) | Middle vs low, 1.17 (1.08, 1.27) |
| High vs low, 1.55 (1.42, 1.71) | High vs low, 0.74 (0.68, 0.80) | |
| Mortality per million population | Middle vs low, 1.38 (1.25, 1.52) | Middle vs low, 0.61 (0.56, 0.67) |
| High vs low, 1.43 (1.30, 1.56) | High vs low, 0.66 (0.61, 0.72) | |
| Trust in government | Yes vs no, 1.67 (1.54, 1.80) | Yes vs no, 4.35 (4.01, 4.72) |
People earning more than $32 per day were 2.18 (95 CI% (1.79, 2.64)) times more likely to respond positively to the general question than people earning less than $2 per day. Higher levels of education were also associated positively with vaccine acceptance on both questions. People who reported COVID-19 sickness in themselves or family members were no more likely to respond positively to the vaccine question than other respondents (OR = 0.97; 95% CI (0.87, 1.08)).
Respondents who said that they trusted their government were more likely to accept a vaccine than those who said that they did not (OR = 1.67; 95% CI (1.54, 1.80)). Moreover, if an individual trusted their government, they were more likely to respond positively to their employer’s vaccine recommendation than someone who did not (OR = 4.35; 95% CI (4.01, 4.72)) (Table 2).
Discussion
We conducted a study of potential acceptance of a COVID-19 vaccine in 13,426 randomly selected individuals across 19 countries, most with a high COVID-19 burden. Of these, 71.5% responded that they would take a vaccine if it were proven safe and effective, and 48.1% said that they would get vaccinated if their employer recommended it (Table 1). However, we observed high heterogeneity in responses between countries. Furthermore, reporting one’s willingness to get vaccinated might not be necessarily a good predictor of acceptance, as vaccine decisions are multifactorial and can change over time.
The far-from-universal willingness to accept a COVID-19 vaccine is a cause for concern. Countries where acceptance exceeded 80% tended to be Asian nations with strong trust in central governments (China, South Korea and Singapore). A relatively high tendency toward acceptance in middle-income countries, such as Brazil, India and South Africa, was also observed. Unless and until the origins of such wide variation in willingness to accept a COVID-19 vaccine is better understood and addressed, differences in vaccine coverage between countries could potentially delay global control of the pandemic and the ensuing societal and economic recovery.
Univariate variation among demographically defined groups was least among those with lower education and income levels. Future vaccine communication strategies should consider the level of health, scientific and general literacy in subpopulations, identify locally trusted sources of information10 and go beyond simply pronouncing that vaccines are safe and effective. Strategies to build vaccine literacy and acceptance should directly address community-specific concerns or misconceptions, address historic issues breeding distrust and be sensitive to religious or philosophical beliefs11. Researchers have identified promising interventions for building confidence and reducing vaccine hesitancy in different contexts12,13, but translating this evidence into large-scale vaccination campaigns will require particular awareness of and attention to existing public perceptions and felt needs. Engaging formal and informal opinion leaders within these communities will be key.
Additionally, we observed age-related associations with vaccine acceptance. Older people were more likely to report that they would take a vaccine, whereas respondents 25‒54 and 55‒64 years of age were more likely to accept an employer’s vaccine recommendation. This finding might reflect who was actually employed or employable at the time of the survey—an issue we did not investigate. Men in this study were less likely than women to accept vaccines in general or their employer’s recommendation to get vaccinated; however, this association was not strong. Those with a higher income were most likely to accept a vaccine than those with a lower income. These data could help governments, policymakers, health professionals and international organizations to more effectively target messaging around COVID-19 vaccination programs.
The other source of concern was a discrepancy between reported acceptance of a COVID-19 vaccine and acceptance if vaccination was mandated by one’s employer. All respondents, regardless of nationality, reported that they would be less likely to accept a COVID-19 vaccine if it were mandated by employers. This finding across all countries with both high and low reported vaccine acceptance proportions suggests that promoting voluntary acceptance is a better option for employers. It might seem easier to monitor compliance among adults in the working age group if employers required it, but this could fail if it is perceived as limiting employees’ freedom of choice or a manifestation of employers’ self-interest14.
A careful balance is required between educating the public about the necessity for universal vaccine coverage and avoiding any suggestion of coercion. Respected community-based groups and non-governmental organizations, such as the Red Cross, which is considered to be impartial, are essential to help build trust in a future COVID-19 vaccine.
Arguably, trust is an intrinsic and potentially modifiable component of successful uptake of a COVID-19 vaccine. Our findings show that trust in government is strongly associated with vaccine acceptance and can contribute to public compliance with recommended actions15. Lessons learned from previous infectious disease outbreaks and public health emergencies, including HIV, H1N1, SARS, MERS and Ebola, remind us that trusted sources of information and guidance are fundamental to disease control16. However, addressing vaccine hesitancy requires more than building trust. It is a multifactorial, complex and context-dependent endeavor that must be addressed simultaneously at global, national and sub-national levels.
Clear and consistent communication by government officials is crucial to building public confidence in vaccine progams. This includes explaining how vaccines work, as well as how they are developed, from recruitment to regulatory approval based on safety and efficacy. Effective campaigns should also aim to carefully explain a vaccine’s level of effectiveness, the time needed for protection (with multiple doses, if required) and the importance of population-wide coverage to achieve community immunity. Instilling public confidence in regulatory agency reviews of vaccine safety and effectiveness will be important. Credible and culturally informed health communication is vital in influencing positive health behaviors17,18, as has been observed with respect to encouraging people to cooperate with COVID-19 control measures. This includes preparing the public and leaders of civic, religious and fraternal organizations that are respected within various sectors of society and local communities, as well as the private sector, for a mass vaccination program with credible spokespeople, local engagement, accurate information and technological support.
This study had limitations. It must be kept in mind that all public surveys of the type reported here are snapshots taken at a point in time. This particular survey was conducted in the context of a highly dynamic and changing landscape, with daily variations in perceived disease threat and COVID-19 vaccine development itself.
In the 3 months since this survey was conducted, several highly visible events have affected COVID-19 vaccine development. A phase III trial of one of the most visible vaccine candidates was put on hold due to the report of a serious adverse event, although that hold was later lifted19. The Russian government, on the other hand, has made a vaccine available for general use on the basis of extremely limited data20. A group of former US Food and Drug Adminstration commissioners and several companies developing COVID-19 vaccines and biomedical advisory bodies have urged the US federal government to base any pending vaccine approvals on clinical data and not bend to political pressure from the incumbent US president to approve a vaccine before the US elections (https://www.washingtonpost.com/opinions/2020/09/29/former-fda-commissioners-coronavirus-vaccine-trump/).
In the context of these developments that post-date our survey, subsequent national surveys in the United States and elsewhere have suggested strongly that public hesitancy to a COVID-19 vaccine is now greater than that which we report here (https://www.kff.org/coronavirus-covid-19/press-release/poll-most-americans-worry-political-pressure-will-lead-to-premature-approval-of-a-covid-19-vaccine-half-say-they-would-not-get-a-free-vaccine-approved-before-election-day/). This can only intensify the vaccine communications challenges discussed above.
In most of the 19 countries surveyed in our study, current levels of willingness to accept a COVID-19 vaccine are insufficient to meet the requirements for community immunity. To build increased trust among the general population, the elements that define and build trust must be understood and interventions crafted accordingly. It is increasingly clear that transparent, evidence-informed policy and clear, accurate communication will be required of all relevant stakeholders. The ongoing pandemic provides the public health community with an important opportunity to build vaccine literacy and confidence to support the uptake of a potential COVID-19 vaccine, as well as to bolster overall immunization programs for all vaccine-preventable diseases.
Methods
We analyzed two questions from the COVID-SCORE study pertaining to COVID-19 vaccine acceptance21. In that survey, participants responded to a total of 22 items, including two related to vaccine uptake, one related to trust in pandemic information sources and standard demographic questions regarding age, gender, level of education and household income (Supplementary Table 1).
Study participants
Participants were recruited by Consensus Strategies through multiple international online panel providers for each country to avoid coverage bias: Dynata provided 7,423 respondents across all 19 countries; Opinion Access provided 3,293 respondents from 14 countries; Survey Monkey provided 1,941 responses from 12 countries; and Amazon MTurk provided 762 respondents from eight countries. Respondents’ identities were verified using IP addresses and mobile phone numbers to ensure that each participant was real and unique upon initial registration. Participants were recruited for the panels via a variety of methods, including online, telephone and direct mail solicitation. Sampling was random and is described in detail elsewhere21.
This study was approved by Emerson College, USA (institutional review board protocol no. 20–023-F-E-6/12), with an expiration date of June 11, 2021. The online questionnaire was administered by Emerson College to gather information from respondents after obtaining their written, informed consent about the survey and this project. No personally identifiable information was collected or stored.
Data collection
Survey data were collected from June 16 to June 20, 2020, from an online panel of 13,426 respondents aged 18 years or older from 19 countries from among the top 35 countries affected by the pandemic in terms of cases per million population, ranging between 619 and 773 participants per country. To ensure regional representation, we selected the next most affected country from regions not represented on the top 35 list: Brazil, Canada, China, Ecuador, France, Germany, India, Italy, Mexico, Nigeria, Poland, Russia, Singapore, South Africa, South Korea, Spain, Sweden, the United Kingdom and the United States22.
The more general vaccine-related question was, ‘If a COVID-19 vaccine is proven safe and effective and is available to me, I will take it’. Respondents were also asked to register their level of agreement with a second statement: ‘I would follow my employer’s recommendation to get a COVID-19 vaccine once the government has approved it as safe and effective’. Responses were recorded on a five-point Likert scale (‘completely disagree’, ‘somewhat disagree’, ‘neutral/no opinion’, ‘somewhat agree’ and ‘completely agree’). We examined the demographic breakdown of the responses to these questions. Data for age and income were collected through open-text fields. Age was coded into age categories: 18–24, 25–54, 55–64 and 65 years or older. Where respondents provided income information, the levels were categorized as ‘<(US)$2 per day’, ‘$2–$8 per day’, ‘$8–$32 per day’ and ‘$32+ per day’. Education levels were categorized as less than high school (low), high school or some college (medium), bachelor’s degree (high) and postgraduate degree (very high). Gender was defined as male, female or other. We also collected information on whether the respondent or a family member had been sick with COVID-19 and COVID-19 cases and deaths per million population at the country level22. For cases per million population and mortality per million population, we categorized the continuous values into categories of low, medium and high. For cases per million population, low was defined as fewer than 2,000 cases per million population; medium was defined as between 2,000 and 4,000 cases per million population; and high was defined as more than 4,000 cases per million population. For mortality per million population, low was defined as fewer than 200 deaths per million population; medium was defined as between 200 and 400 deaths per million population; and high was defined as more than 400 deaths per million population.
Analysis
We analyzed the distribution of the responses against the different questions for the entire dataset and further examined differences by country. We calculated results for two sets of univariate regressions: one for each of the two questions related to vaccines. We used logistic regression, defining the outcome as 1 if a respondent answered ‘completely agree’ or ‘somewhat agree’ and 0 for any other response. The independent demographic variables included age, gender, income and education. We also examined the relationship between the two regression outcomes and whether someone in the respondent’s family had been sick with COVID-19, as well as existing country-by-country data on COVID-19 cases per million population, COVID-19 mortality per million population and whether a respondent reported that they trusted pandemic information from their government (yes or no).
Reporting Summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Online content
Any methods, additional references, Nature Research reporting summaries, source data, extended data, supplementary information, acknowledgements, peer review information; details of author contributions and competing interests; and statements of data and code availability are available at 10.1038/s41591-020-1124-9.
Supplementary information
Supplementary Table 1
Acknowledgements
Funding was provided by the City University of New York Graduate School of Public Health and Health Policy Foundation, Bocconi University, J. Fielding, the United States Council for International Business Foundation and K. Rabin. Consensus Strategies was the funding recipient. J.V.L. acknowledges support to ISGlobal from the Spanish Ministry of Science, Innovation and Universities through the ‘Centro de Excelencia Severo Ochoa 2019–2023’ Programme (CEX2018-000806-S) and from the Government of Catalonia through the CERCA Programme.
Extended data
Author contributions
S.C.R., J.V.L. and A.E.M. conceived the study. S.K. collected the data. A.P. was responsible for the coding of the analyses. A.P., A.E.M. and J.V.L. analyzed the data. J.V.L., A.P., K.R. and A.E.M. wrote the first draft of the paper. J.V.L., A.E.M., A.P., K.R., S.C.R., L.O.G. and H.L. edited and approved the final manuscript.
Data availability
All data used in this analysis can be found at https://osf.io/kzq69/.
Code availability
All code to reproduce this analysis can be found at https://osf.io/kzq69/.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Change history
2/15/2021
A Correction to this paper has been published: 10.1038/s41591-020-01226-0
Extended data
is available for this paper at 10.1038/s41591-020-1124-9.
Supplementary information
is available for this paper at 10.1038/s41591-020-1124-9.
References
- 1.MacDonald NE. & SAGE Working Group on Vaccine Hesitancy. Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015;33:4161–4164. doi: 10.1016/j.vaccine.2015.04.036. [DOI] [PubMed] [Google Scholar]
- 2.Karafillakis E, Larson HJ. & ADVANCE Consortium. The benefit of the doubt or doubts over benefits? A systematic literature review of perceived risks of vaccines in European populations. Vaccine. 2017;35:4840–4850. doi: 10.1016/j.vaccine.2017.07.061. [DOI] [PubMed] [Google Scholar]
- 3.Cobos Muñoz D, Monzón Llamas L, Bosch-Capblanch X. Exposing concerns about vaccination in low- and middle-income countries: a systematic review. Int. J. Public Health. 2015;60:767–780. doi: 10.1007/s00038-015-0715-6. [DOI] [PubMed] [Google Scholar]
- 4.European Parliament. European Parliament resolution of 19 April 2018 on vaccine hesitancy and drop in vaccination rates in Europe (2017/2951 RSP). https://www.europarl.europa.eu/doceo/document/TA-8-2018-0188_EN.pdf (2018).
- 5.Larson HJ, Jarrett C, Eckersberger E, Smith DMD, Paterson P. Understanding vaccine hesitancy around vaccines and vaccination from a global perspective: a systematic review of published literature, 2007-2012. Vaccine. 2014;32:2150–2159. doi: 10.1016/j.vaccine.2014.01.081. [DOI] [PubMed] [Google Scholar]
- 6.Lane S, MacDonald NE, Marti M, Dumolard L. Vaccine hesitancy around the globe: analysis of three years of WHO/UNICEF Joint Reporting Form data—2015–2017. Vaccine. 2018;36:3861–3867. doi: 10.1016/j.vaccine.2018.03.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Enserink, M. & Cohen, J. Fact-checking Judy Mikovits, the controversial virologist attacking Anthony Fauci in a viral conspiracy video. Sciencehttps://www.sciencemag.org/news/2020/05/fact-checking-judy-mikovits-controversial-virologist-attacking-anthony-fauci-viral (2020).
- 8.Cornwall W. Officials gird for a war on vaccine misinformation. Science. 2020;369:14–19. doi: 10.1126/science.369.6499.14. [DOI] [PubMed] [Google Scholar]
- 9.Fadda M, Albanese E, Suggs LS. When a COVID-19 vaccine is ready, will we all be ready for it? Int. J. Public Health. 2020;65:711–712. doi: 10.1007/s00038-020-01404-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Larson HJ, et al. Measuring trust in vaccination: a systematic review. Hum. Vaccines Immunother. 2018;14:1599–1609. doi: 10.1080/21645515.2018.1459252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Biasio LR. Vaccine hesitancy and health literacy. Hum. Vaccines Immunother. 2017;13:701–702. doi: 10.1080/21645515.2016.1243633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Thomson A, Vallée-Tourangeau G, Suggs LS. Strategies to increase vaccine acceptance and uptake: from behavioral insights to context-specific, culturally-appropriate, evidence-based communications and interventions. Vaccine. 2018;36:6457–6458. doi: 10.1016/j.vaccine.2018.08.031. [DOI] [PubMed] [Google Scholar]
- 13.European Centre for Disease Prevention and Control. Catalogue of interventions addressing vaccine hesitancy. https://www.ecdc.europa.eu/sites/portal/files/documents/Catalogue-interventions-vaccine-hesitancy.pdf (2017).
- 14.Lugo NR. Will carrots or sticks raise influenza immunization rates of health care personnel? Am. J. Infect. Control. 2007;35:1–6. doi: 10.1016/j.ajic.2006.10.004. [DOI] [PubMed] [Google Scholar]
- 15.Hovland CI, Weiss W. The influence of source credibility on communication effectiveness. Public Opin. Q. 1951;15:635. doi: 10.1086/266350. [DOI] [Google Scholar]
- 16.Siegrist M, Zingg A. The role of public trust during pandemics: implications for crisis communication. Eur. Psychol. 2014;19:23–32. doi: 10.1027/1016-9040/a000169. [DOI] [Google Scholar]
- 17.Quinn SC, et al. Exploring communication, trust in government, and vaccination intention later in the 2009 H1N1 pandemic: results of a national survey. Biosecurity Bioterrorism. 2013;11:96–106. doi: 10.1089/bsp.2012.0048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shore DA. Communicating in times of uncertainty: the need for trust. J. Health Commun. 2003;8:13–14. doi: 10.1080/713851977. [DOI] [PubMed] [Google Scholar]
- 19.Mahase E. Covid-19: Oxford researchers halt vaccine trial while adverse reaction is investigated. BMJ. 2020;370:m3525. doi: 10.1136/bmj.m3525. [DOI] [PubMed] [Google Scholar]
- 20.Burki, T. K. The Russian vaccine for COVID-19. Lancet Respir. Med. 10.1016/S2213-2600(20)30402-1 (2020). [DOI] [PMC free article] [PubMed]
- 21.Lazarus JV, et al. COVID-SCORE: a global survey to assess public perceptions of government responses to COVID-19 (COVID-SCORE-10) PLoS ONE. 2020;15:e0240011. doi: 10.1371/journal.pone.0240011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Johns Hopkins Coronavirus Resource Center. COVID-19 dashboard. https://coronavirus.jhu.edu/map.html (2020).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table 1
Data Availability Statement
All data used in this analysis can be found at https://osf.io/kzq69/.
All code to reproduce this analysis can be found at https://osf.io/kzq69/.