Abstract
Introduction
There is an increasing affinity for remote health consultations (including telephone and virtual platforms), enabling new models of accessing services to evolve. Whilst many key skills are transferable from traditional to remote consultations, there is even greater emphasis on verbal communication skills during these interactions.
Purpose
This masterclass considers the communication skills required for delivering remote health care consultations, in particular focussing on: 12 interactional features in an opening sequence of a remote call; active listening; how to offer advice using the Ask-Offer-Ask framework; and subtleties in phrasing and prosody when closing a call that may indicate a level of satisfaction (or otherwise).
Implications
In planning for digitally-enabled services to become mainstream, the differences in communication between remote and face-to-face consultations must be recognised and embraced.
Keywords: Telehealth, Remote consultation, Communication skills, Access to care, Patient preference
1. Introduction
As society becomes more digitalised, there is a strong drive in health care from clinicians, service users, commissioners, and industrial partners to use technologies that support alternatives to traditional face-to-face consultations, improve the acceptability and efficiency of services, and promote self-management. The speed of implementation accelerated rapidly with the suspension of traditional consultations due to COVID-19 (Gilbert et al., 2020), and required clinicians to deliver remote consultations, often at short notice and with little training or consideration of any differences in delivery. The purpose of this masterclass is to discuss communication skills in remote healthcare interactions.
With growing demand for health services and finite resources, digital health services are one of the fastest growing areas of health care provision, with a market potential that is expected to grow at a compound annual rate of 14% in the coming years (European Commission, 2018). This is recognised to be of global importance in the World Health Organization's recently published draft strategy for 2020–25, which advocates people-centred health systems, enabled by digital health, as one of its four strategic objectives (WHO, 2020). In the UK, the National Information Board argued the need for a different kind of health service, in which the traditional outpatient consultation will become increasingly obsolete (National Information Board, 2014), and the NHS Long Term Plan stated that digitally-enabled primary and out-patient care will be mainstream within five years (NHS, 2019). Whilst opinion may be divided about the future, it is recognised that remote consultations, using digital technologies, can offer a partial solution to these challenges (Shaw et al., 2018).
Among the alternatives to traditional consultations are telephone, text messaging, email consultations, online portals, telemedicine and telehealth. ‘Telemedicine’ has been defined as “The delivery of health care services, where distance is a critical factor, by all health care professionals using information and communication technologies for the exchange of valid information for diagnosis, treatment and prevention of disease and injuries, research and evaluation, and for the continuing education of health care providers, all in the interests of advancing the health of individuals and their communities” (WHO, 2010). This evolved into ‘telehealth’, with a broader scope that includes health promotion and disease prevention (Koch, 2006), and often involves the exchange of data between a patient at home and their clinician (Shaw et al., 2018). Then came ‘eHealth’, defined as ‘referring to health services and information delivered or enhanced through the Internet and related technologies’ (Eysenbach, 2001). Applying telehealth to the home environment has been described as ‘telehomecare’, or more recently, ‘home telehealth’ or ‘home based eHealth’ and may comprise anything from email consultations and educational programmes, to advanced sensor surveillance and clinical robots placed into patients' homes (Koch, 2006). In this article, ‘remote’ consultations will be used to cover non-face-to-face health care interactions.
High-quality evaluations of remote encounters are rare, and Table 1 summarises the evidence reviewed by Shaw et al. (2018).
Table 1.
Summary of the state of evidence for alternatives to face-to-face consultations (summarised from Shaw et al., 2018).
| Telephone |
|
| Text and email |
|
| Online portals |
|
| Telemedicine |
|
| Telehealth |
|
Within the literature, the advantages and disadvantages of remote consultations and meetings, have been reported from the perspecive of the patient, their family and the service (Table 2 ), and the environmental and technological practicalities of setting up a service have been reported elsewhere (Cottrell and Russell, 2020; Gilbert et al., 2020; Greenhalgh et al., 2018; NHS, 2019; NHSX, 2020; Wherton et al., 2020). The focus for this paper is on the communication skills needed to deliver these complex interactions.
Table 2.
Perspectives of remote consultations.
| Reported advantages | Reported disadvantages | |
|---|---|---|
| Patient and family |
|
|
| Services |
|
|
1.1. Implications
The most important determinants of a “good” consultation have been described in the literature as: i) the patient's perception of being taken seriously; ii) giving an understandable explanation of the pain; iii) applying patient-centred care; iv) reassurance; and v) being told what can be done (Lærum et al., 2006). These are all readily achievable in remote interactions.
More research is needed to determine the effectiveness and acceptability of remote consultations, including the extent of prima facie concerns that have been reported, where patients might perceive remote consultations to be a form of rationing, or a lower quality of clinical care (Ackerman et al., 2020). In primary care, video-consulting has been shown to be favoured by those who are young, technologically proficient, and more experienced in communicating online (Hammersley et al., 2019). Within physiotherapy, it was interesting to note that in the rapid implementation of a virtual clinic, the majority of patients chose a phone call rather than a video call (83.7%, n = 1359) and the reasons for this are unknown and may vary according to the situation (Gilbert et al., 2020).
1.2. Things to consider before starting
Many patients fail to get the best from their consultations because they arrive unprepared, not knowing what the consultation is about, what is likely to happen, and that they will be asked to give an account of their symptoms, concerns and medical history (Caldwell, 2019). In helping them to better prepare, it is essential to consider every aspect of communication between the service and the patient, to optimise their experience and outcome. Information sent to the patient in advance should provide details of the agreed time of the call (and if the caller ID will show as ‘withheld’), an estimate of the likely duration, and guidance about taking the call in an appropriate physical location. We have experienced patients taking calls in supermarkets, while out walking, driving, at work, or undertaking home improvements. There is an element of educating the patient that it is a health consultation and they may be asked to perform certain tasks, or if it is a video call, they may be asked to de-robe as part of the examination, as they would in a face-to-face interaction. Furthermore, it is important to explain terms carefully and not make assumptions, as patients in one study had understood the interaction was being recorded due to the word ‘video’ (Petersson et al., 2020) and this may affect uptake. Furthermore, the clinician needs to be aware of their own personal appearance, including attire (if they do not wear uniform), as well as any background behind them that will be visible to the patient on screen, to help create a professional image and favourable first impression.
With online consultations, it is important to remember the patient may be anxious, not only about their health issue, but also about using technology, and so may have logged on early to a virtual platform, to avoid feeling under pressure. It is helpful if patients have an opportunity to test their equipment and log-in process ahead of the appointment, to reduce their anxiety and any ‘digital fumbling’ at the start of the call.
1.3. Making the call
In a mixed methods study of Skype consultations in three clinical services, Greenhalgh et al. (2018) reported that the opening sequence of a video consultation was very different from that of a face-to-face interaction, due to the ‘technical phase’, which inevitably preceded the clinical talk. Ordinarily, this is the time to make a positive first impression and start building rapport, defined as a social phenomenon involving mutual attentiveness, positivity and interactional synchrony, that results in ‘good chemistry’ (Vicaria et al., 2015) and in a remote call, the technical phase adds an additional challenge. Along with compassion and empathy, rapport has been described as a cornerstone of a positive clinical encounter (Raja et al., 2015) that once lost, is hard to regain. In remote consultations (especially by telephone), it can be more difficult to build rapport with reduced non-verbal cues. From their work, Greenhalgh et al. (2018) concluded virtual consultations appeared to work best involving long-term conditions in which the patient and clinician had a pre-existing relationship and a high degree of mutual trust.
As the remote encounter starts, the patient may have been on hold for a while, had to endure piped music, and so is likely to be aware if the clinician is running even a few minutes late. In that case, it is essential for the clinician to offer an apology early, to minimise losing rapport at the outset.
Table 3 shows the start of a remote call in a musculoskeletal service, and is a composite of our telephone and online calls. It is neither perfect, nor designed to be a script, as no one size fits all however, it does include some key interactional features that will be discussed. The 12 stages of starting this remote consultation are summarised in Fig. 1 .
Table 3.
Starting the call (*can also add ‘see’ if video consultation).
| Turn | Speaker | Feature | |
|---|---|---|---|
| 1 | Patient: | Hello? | |
| 2 | Physio: | Hello. Please can I speak with Mr Stuart Evans? | Greeting |
| 3 | Patient: | Speaking. | |
| 4 | Physio: | My name's Katie Clifton. I'm a senior physiotherapist at the Woodgate Health Centre. | Introduction |
| 5 | Patient: | Oh yes, hello, I was expecting a call | |
| 6 | Physio: | Is now a good time? | Courtesy |
| 7 | Patient: | Yes, it's fine. | |
| 8 | Physio: | Can I just check that you can hear* me OK? | Equipment check |
| 9 | Patient: | Yep | |
| 10 | Physio: | And just in case we lose connection for any reason, which rarely happens, is it OK to call you back straight away on this number? | |
| 11 | Patient: | Yes, that's OK | |
| 12 | Physio: | Good. So, is this the first time you've had a physiotherapy consultation by phone? | Establish experience |
| 13 | Patient: | Yes | |
| 14 | Physio: | Well, the content will be similar to as if we were in the health centre, and just to let you know, all your information is treated confidentially and stored securely, as normal. Are happy to go ahead with this by phone? |
Reassure Consent (x 2) |
| One thing that is different, you might well hear me tapping my keyboard as I'll be making some notes as we go, to capture important things you're saying. | Signpost | ||
| So, is there anything you need to get before we start (e.g. pen and paper)? | Preparation check | ||
| 15 | Patient: | No, I'm good to go. | |
| 16 | Physio: | That's good. I just need to check a couple of details to confirm I have the correct records open: Please could you tell me your date of birth? | ID check |
| 17 | Patient: | [patient gives details] | |
| 18 | Physio: | and the first line of your address? | |
| 19 | Patient: | [patient replies] | |
| 20 | Physio: | Thank you. Right, I've seen from the referral that you've been having some problems with your left knee which I'd like to ask you about. Please do let me know if there's anything in particular you want to cover today. [Pause] |
Orient to reason for call [K + ] Agenda setting |
| 21 | Patient: | OK. Will do | |
| 22 | Physio: | So to start with, can you tell me about the problem you're having with your knee? | Key clinical question |
Fig. 1.
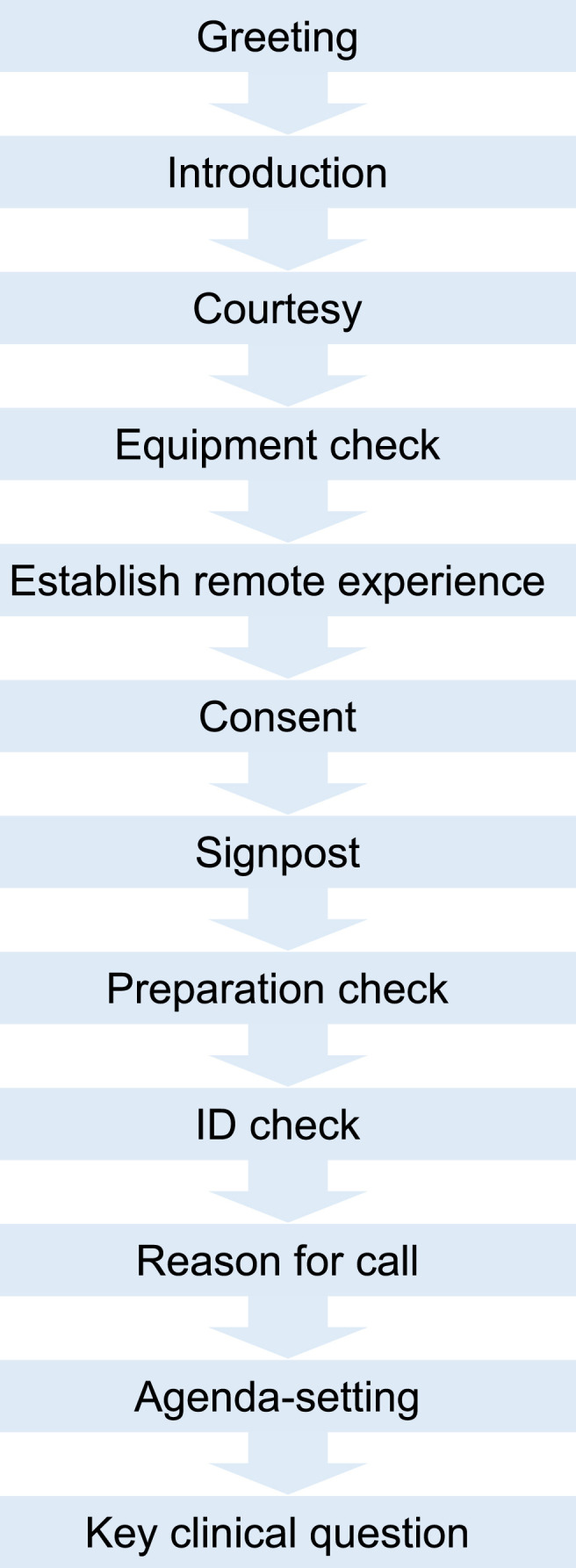
Stages for starting a remote consultation.
Greeting: In turn 2 of Table 3, the clinician identifies the intended recipient through the form of a request. Both the patient's forename and surname are used, to increase the likelihood of speaking to the correct person without making assumptions, as there may be more than one Mr Evans at the location.
Introduction: In turn 4, equally the clinician introduces herself with her forename, surname and a simplified job title. From earlier work we undertook improving patient experience, patients most wanted to know the name of their clinician AND their level of experience, or as one patient put it “Are they any good?” (Roberts, 2006). Patients are unlikely to be familiar with, or impressed by, unclear or jargonistic job titles. (For junior staff in the UK for example, introducing yourself as a ‘Qualified’ or ‘Chartered’ Physiotherapist is preferable to terms like band 5 or ‘Rotational’ Physiotherapist.)
Courtesy: In turn 6, the clinician checks if it is convenient for the patient to take the call at this time. This courtesy also gives the patient an opportunity to say if they have any time restrictions.
Equipment check: When using virtual platforms, it is important to check the patient can see and hear the caller, (turn 8). This provides an opportunity in online interactions to ask a patient to adjust their lighting, screen angle etc. and vice versa. At this point it is worth establishing what would happen if the technology fails, especially in a telephone call, so that the patient's phone is not permanently engaged as both parties try to re-establish contact, which it is easier for the clinician to initiate.
Establish remote experience: It is useful to know if this is the patient's first experience of a remote consultation (turn 12), to orient the clinician to the amount of explanation and signposting required. Moreover, it can provide an opportunity to show empathy and build rapport if the patient expresses anxiety with their IT skills.
In turn 14, the clinician indicates that the consultation will be thorough and provides assurances that the data will be treated confidentially.
Consent: With remote consultations, as it is the clinician who has made the call and the patient has not attended in person, there is not the degree of implied consent that is afforded to traditional consultations. Therefore in turn 14, the clinician seeks express consent for a remote consultation. Table 4 summarises the key consent issues.
Table 4.
Types of consent in health care consultations (1For further detail about material risk, see MDU, 2018. 2This does not cover treatments within the consultation, as express consent is required for these.).
| Type | Definition | Example of use | Example in remote consultation |
|---|---|---|---|
| Express | When a patient explicitly indicates their agreement, either verbally or in writing. This should be obtained for any procedure that requires material risk1, before the procedure starts. |
|
See turn 14: ‘Are you happy to go ahead with this by phone?’ |
| Implied | When a patient performs an action that suggests they consent. |
|
Patient removes their clothing to show their range of movement in a virtual consultation. |
Gaining express consent is necessary if any other staff may be involved in the call, for example a student. It is essential that the clinician explains who the person is, and why they may be present. Where possible, the patient's permission should be asked in advance, by the clinician alone, as the power differential in a clinician–patient relationship already makes it difficult for a patient to decline. It is essential that the patient's autonomy be respected, and they are given an opportunity to decline without prejudice, without needing to give a reason, and without feeling coerced.
Signposting: In turn 14, the clinician signposts to the patient that they may hear (or see) her using the keyboard. When a recipient hears a caller typing, they commonly assume the caller is otherwise engaged and therefore, not listening. Moreover, it can be helpful in building rapport for a clinician to feedback to a patient that what they are saying is important and worthy of recording.
Preparation check: At the end of turn 14, the clinician shows consideration by providing an opportunity for the patient to get anything they need, such as glasses, pen and paper, list of medications, or as we have found, this may include inviting a partner to join them.
ID check: In turn 16, the clinician uses two short pieces of personal data to confirm that she is speaking to the intended recipient. This must be done before any health information is given about the reason for the call, to maintain confidentiality and prevent a data breach, in line with professional codes of conduct (CSP, 2019; HCPC, 2013).
Reason for the call: Having confirmed the clinician is speaking with the intended recipient, she then orientates to the reason for the call (turn 20). There are several different approaches to this, and she chooses this opportunity to display prior knowledge of the patient's symptoms, (a problem with their left knee), in what Heritage calls a more knowledgeable (K+) epistemic status (Heritage, 2012). This shows an element of preparation for the call. Sometimes instead, clinicians choose to shift the balance of power to the patient using an open question such as “How can I help?” which is an example of an epistemic K- question.
Agenda-setting: The clinician completes turn 20 with an agenda-setting item that evokes preference, helps tailor the consultation to the patient's needs and align with their expectations. It is important to give sufficient time for the patient to respond, as they may not have been asked this before in consultations.
Key clinical question: In turn 22, the key clinical question gives control to the patient, as they are invited to talk about their presenting condition. As Robinson and Heritage observed (2006), this is the only time in consultations when patients are given the opportunity to share information in their own words and according to their own agenda. Giving the patient an opportunity to direct the conversation has been shown to increase adherence to treatment (Zolnierek, and Dimatteo, 2009) and improve patient ‘satisfaction,’ (Robinson and Heritage, 2005; Heritage and Robinson, 2006). This act of delegating control is especially important in remote consultations, where rapport is impeded by reduced non-verbal cues. In this case, the clinician orients the talk towards the patient's knee symptoms, by inviting a narrative, using the open question “Can you tell me … ?” We have previously undertaken research exploring clinicians' preferences for opening encounters in consultations between physiotherapists and patients with back pain (Chester et al., 2014) and the preferred choice was the open-focussed question: “Do you want to just tell me a little bit about [problem presentation] first of all?” (See Table 5 ).
Table 5.
Results from our national survey showing the preferred phrasing of the key clinical question in initial consultations between physiotherapists and patients with low back pain (Chester et al., 2014).
| Preferences | Phrase |
|---|---|
| 1st | Do you want to just tell me a little bit about [problem presentation] first of all? |
| 2nd | I've had this referral through. Tell me what's happened. |
| 3rd | The referral says you've got [problem presentation] is this correct? |
| 4th | How can I help you today? |
| 5th | What we'll do today is just have a bit of a chat about [problem presentation], I believe it is. All right? |
| 6th | It's your [problem presentation — knee, back etc.] that you're here for is it? |
| 7th | What problem are you having at the moment? |
| 8th | Do you want to tell me your story? |
| 9th | Do you want to start off by telling me whereabouts you're getting your pain at the moment? |
| 10th | I know a little bit from the GP, when did this start? |
| 11th | How long have you had [problem presentation] for? |
Having asked the key clinical question, the clinician needs to listen to the patient's account without interruption. Langewitz et al. (2002) reported that patients take 92 s on average to explain their problem in an outpatient setting if they are not interrupted. Without non-verbal cues to help identify when a turn will end, the likelihood of overlapping or interrupting a patient during a remote consultation is increased. Interruptions can occur at any time during the encounter and by either the patient or clinician (Beckman and Frankel, 1984) and it has been reported that interruptions may lead to delays in patients expressing their concerns (Irish and Hall, 1995) and missed opportunities to gather relevant information (Marvel et al., 1999), resulting in incomplete or improper medical advice (Irish and Hall, 1995). In our work observing 15,489 turns taken during initial consultations in a primary care setting for patients with low back pain (Roberts and Burrow, 2018), we reported physiotherapists (especially female) were 7 times more likely to interrupt than patients.
Questioning styles: Throughout the interaction, the clinician needs to keep questions simple, ideally addressing a single issue. Asking closed questions, e.g.: ‘Is this your first online consultation?’ is likely to proffer a yes/no response, whilst open questions will invite patients to give a more detailed account that can ensure their agenda is addressed. Throughout history-taking, using open questions with a ‘TED’ stem, (i.e. questions that seek to ‘Tell’, ‘Explain’, or ‘Describe’), can provide rich information e.g: ‘Can you explain how your knee pain is affecting your life at the moment?’ Such questions can aid flow in the consultation, and save the clinician needing to ask multiple questions, which in turn, reduces the risk of interruptions.
Active listening: Patients often report they don't feel listened to following health care consultations and it is worth remembering that LISTEN also spells SILENT! At the end of history-taking, delegating control again to the patient, with a question like: ‘Before we go on to have a look at your knee, is there anything else that we haven't talked about that you think is important and want to raise?‘, can provide another opportunity to ensure their agenda is addressed. This recognises their issues may be multifactorial, as evidenced by the EPaC (Elicitation of Patient Concerns) study in the UK, where an analysis of 185 primary care traditional video-recordings with GPs revealed an average of 2.1 concerns were raised per 10-min scheduled appointment (Stuart et al., 2019). Seeking any additional issues at this point in the consultation may help prevent ‘door-knob concerns’, where the patient is metaphorically on their way out with their hand on the door knob, and an additional concern surfaces, often the most important one (Finset, 2016), or they leave with unmet needs. In primary care, unvoiced health concerns have been associated with worsening of symptoms, increased patient anxiety, the need for additional visits and increased burden and costs (in time and resources) both for patients and the service (Heritage et al., 2007; Stuart et al., 2019).
1.4. Offering advice
In considering offering advice to a patient, using the ‘Ask-Offer-Ask’ approach, based on the Ask-Tell-Ask framework (Barnett, 2001), can help build a two-way conversation to share health information. The first ‘ask’ establishes what information and strategies the patient is aware of e.g. ‘Can you tell me what you already know about ways you can manage your knee pain and what else you would like to know?’ Giving patients this opportunity to raise their own ideas, provides a basis to tailor and endorse activities that interest them. This collaboration strengthens self-efficacy and is reported to have positive effects on pain and physical activity engagement (Degerstedt et al., 2020), while also providing an opportunity to address any unhelpful beliefs that may exist.
A focus on ‘offering’ advice, rather than ‘giving’ or ‘telling’, is likely to be better received by the patient, to avoid psychological reactance, a term used to describe the feelings and thoughts that occur with perceptions of threat to freedom (Dorrance Hall, 2019), and can be achieved by asking ‘Would you like me to suggest some other ideas that might help you manage the pain?’ Care is required to ensure any advice offered is patient-centred and specific, and avoids vague terms such as ‘often’ and ‘frequently’.
The ‘2nd ask’ empowers patients to reflect on their understanding and consider any barriers they can identify with the advice e.g. ‘Can you tell me how you might be able to fit this in with your day and any difficulties you see with trying this?’ Giving mixed messages is common, and this second ask allows the clinician to clarify understanding and summarise the advice at the end of the consultation, so that the patient leaves the call with a clear message. This is a good time to signpost online resources and check the patient's access to these, which may involve following-up by email or text, with specific links or exercises.
As health services make better use of digital technologies, the public are consuming more digital advice and done well, this provides more opportunities for much-needed health promotion, which has been identified as inconsistent in consultations (Lowe et al., 2018). The inequity in access, or digital divide, does however, favour patients with higher digital literacy and educational attainment and clinicians need to think about how they compensate for the reduced shared activities, such as explanations using anatomical models etc., often present in traditional encounters.
1.5. Closing
Sensitively closing a remote conversation can be challenging. Early, influential work on closing conversations by Schegloff and Sacks (1973) identified the ‘closing problem’, when the usual format of turn-taking is suspended. Once both speakers have displayed a readiness to close, for example if a health professional asks a patient if they have any questions and they decline, this creates a ‘warrant’ for closing, as there is nothing further to discuss (Schegloff and Sacks, 1973). Button explored this further in a comprehensive analysis of conversational practices including ‘minimal’ and ‘drastic’ closings, where in the former, the conversation closes after a brief move is made, in contrast to a ‘dramatic’ close, where the talk re-opens and the close may not occur until much later (Button, 1987, 1991).
Soliciting whether the patient has any other concerns near the end of the consultations is a commonly-used strategy in consultations, and Robinson and Heritage (2016) showed in the US that this was understood by patients to bring the appointment to a close. Research has found that if the question is phrased ‘Is there anything else I can help you with?’ the turn design ‘anything else’ can impede patients raising additional concerns, as this is negatively polarised to prefer a ‘no response’ (Heritage et al., 2007). Meanwhile, replacing ‘anything else’ with ‘something else’ is positively polarised and favours a ‘yes’ response (Heritage et al., 2007). Furthermore, it has been found that using ‘concern-seeking’ questions to elicit patients' agendas (‘Do you have other concerns?‘) resulted in patients being more likely to volunteer a new health concern than if ‘question-seeking’ questions were used (‘Do you have other questions?‘), (Robinson et al., 2016). Other forms of closing sequences may include offering to send a patient some materials, such as an information booklet, exercise sheet etc., similar to the ‘closing offers’ described by Sacks (1992).
1.6. Evaluating the interaction
During closing sequences, patients often display a sense of gratitude for the service they have received, and clinicians need to listen carefully for any subtle displays of dissatisfaction that they may wish to try and rectify before the consultation closes. In a study of telephone calls to a cancer helpline looking at how callers convey their satisfaction or otherwise with the service provided during the call, Woods et al. focussed on endogenous indications of caller satisfaction displayed through the closing stages of calls and found that patients may display dissatisfaction by downgrading their appreciation with phrases like ‘all right then’, or using flat, unenthusiastic prosody, suggesting the patients' expectations have not (yet) been fulfilled (Woods et al., 2015).
Determining the ‘success’ of remote consultations can be difficult to gauge (Leydon et al., 2019), especially if there is no spontaneous feedback from the recipient. In a study evaluating the success of calls to three UK cancer helplines, call handlers described a successful call as one in which the caller's expressed needs have been clearly met (Leydon et al., 2019), again highlighting the importance of agenda-setting.
When evaluating clinical services, the validity and appropriateness of using the concept of ‘satisfaction’ has been questioned, as it has been shown that expressions of satisfaction do not appear to relate to actual processes of care (Avis et al., 1997). Due to the ‘serious limitations’ with the consumer model of patient satisfaction, Avis et al. suggest that qualitative approaches be used in preference to satisfaction surveys (Avis et al., 1997). Furthermore, the term ‘patient experience’ is often erroneously used interchangeably with ‘patient satisfaction’, however they are not reporting the same construct. ‘Patient experience’ seeks to determine whether something that should have happened did in fact happen (according to the patient), whereas ‘satisfaction’ seeks to determine whether a patient's expectations about their care were met. Moreover, in evaluating services, the context is key. For example, asking patients to evaluate remote consultations at a time when no face-to-face consultations were possible is likely to yield a different response to evaluating their acceptability when there is a free choice of service delivery.
2. Conclusion
Remote consultations can be seen as a way of improving access and delivery of health care. This paper considers the communication skills that clinicians need to deliver these complex interactions and focuses on 12 interactional features in an opening sequence of a telephone or video call. As alternatives are found to traditional face-to-face consultations, preparation is needed to: 1) educate patients that these consultations must take place in an appropriate physical location; and 2) support clinicians to further develop their communication skills in interactions where building rapport is impeded by reduced non-verbal cues and the technical focus at the start of the call. Therefore in scaling-up and optimising digital health services, the differences in communication between remote and face-to-face consultations must be recognised and embraced.
Ethical approval
Not applicable.
Funding
This research did not receive specific funding from agencies in the public, commercial or not-for-profit sectors.
Declaration of competing interest
Neither author has any interests to disclose.
Biographies
Lisa Roberts: is a clinical academic with a joint role as Clinical Professor of Musculoskeletal Health at the University of Southampton and Consultant Physiotherapist at University Hospital Southampton NHS Foundation Trust. Her research interests include: improving communication in consultations; shared decision-making; psychologically-informed practice, promoting independence using web-based technologies; (and evaluating consultant roles). She has published multiple papers in this area, been an invited speaker at many national and international conferences and led workshops in optimising communication in clinical consultations.
Lisa Osborn-Jenkins: is a Specialist Musculoskeletal Physiotherapist in complex musculoskeletal presentations and persistent pain. Her clinical roles are within NHS secondary care specialist services but have also included working in a First Contact Practitioner role and private practice. As a National Institute for Health Research pre-doctoral clinical academic awardee, her primary area of research explores advice-giving practice in physiotherapy and among other musculoskeletal practitioners. She has presented at national and international conferences, delivered workshops in this area, and worked alongside the Chartered Society of Physiotherapy exploring musculoskeletal health advice available to the public
References
- Ackerman S.L., Gleason N., Shipman S.A. Comparing patients' experiences with electronic and traditional consultation: results from a multisite survey. J. Gen. Intern. Med. 2020;35(4):1135–1142. doi: 10.1007/s11606-020-05703-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Avis M., Bond M., Arthur A. Questioning patient satisfaction: an empirical investigation in two outpatient clinics. Soc. Sci. Med. 1997;44(1):85–92. [Google Scholar]
- Barnett P.B. Rapport and the hospitalist. AJM. 2001;111(9B):31S–35S. doi: 10.1016/s0002-9343(01)00967-6. [DOI] [PubMed] [Google Scholar]
- Beckman H.B., Frankel R.M. The effect of physician behaviour on the collection of data. Ann. Intern. Med. 1984;101(5):692–696. doi: 10.7326/0003-4819-101-5-692. [DOI] [PubMed] [Google Scholar]
- Button G. In: Talk and Social Organisation. Button G., Lee J., editors. Multilingual Matters Ltd; Philadelphia: 1987. Moving out of closings; pp. 101–151. [Google Scholar]
- Button G. In: Talk and Social Structure. Boden D., Zimmerman D.H., editors. Polity Press; Cambridge: 1991. Conversation-in-a-Series; pp. 251–277. [Google Scholar]
- Caffery L.J., Farjian M., Smith A.C. Telehealth interventions for reducing waiting lists and waiting times for specialist outpatient services: a scoping review. J. Telemed. Telecare. 2016;22(8):504–512. doi: 10.1177/1357633X16670495. [DOI] [PubMed] [Google Scholar]
- Caldwell G. The process of clinical consultation is crucial to patient outcomes and safety: 10 quality indicators. Clin. Med. 2019;19(6):503–506. doi: 10.7861/clinmed.2019-0263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chartered Society of Physiotherapy Code of Members' professional values and behavior. 2019. https://www.csp.org.uk/publications/code-members-professional-values-behaviour
- Chester E.C., Robinson N.C., Roberts L.C. Opening clinical encounters in an adult musculoskeletal setting. Man. Ther. 2014;19(4):306–310. doi: 10.1016/j.math.2014.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cottrell M.A., Russell T.G. Telehealth for musculoskeletal physiotherapy. Musculoskelet. Sci. Pract. 2020;48:102193. doi: 10.1016/j.msksp.2020.102193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Degerstedt A., Alinaghizadeh H., Thorstensson C., Olsson C. High self-efficacy - a predictor of reduced pain and higher levels of physical activity among patients with osteoarthritis: an observational study. BMC Muscoskel. Disord. 2020;21:380. doi: 10.1186/s12891-020-03407-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dorrance Hall E. 2019. Why We Hate People Telling Us what to Do.https://www.psychologytoday.com/gb/blog/conscious-communication/201906/why-we-hate-people-telling-us-what-do [Google Scholar]
- European Commission . Publications Office of the European Union; Luxembourg: 2018. Market Study on Telemedicine.https://ec.europa.eu/health/sites/health/files/ehealth/docs/2018_provision_marketstudy_telemedicine_en.pdf [Google Scholar]
- Eysenbach G. What is e-health? J. Med. Internet Res. 2001;3(2) doi: 10.2196/jmir.3.2.e20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finset A. When patients have more than one concern. Patient Educ. Counsel. 2016;99(5):671. doi: 10.1016/j.pec.2016.03.016. [DOI] [PubMed] [Google Scholar]
- Gilbert A.W., Billany J.C.T., Adam R., Martin L., Tobin R., Bagdai S., Galvin N., Allain A., Davies L., Bateson J. Rapid implementation of virtual clinics due to COVID-19: report and early evaluation of a quality improvement initiative. BMJ Open Quality. 2020;9 doi: 10.1136/bmjoq-2020-000985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenhalgh T., Shaw S., Wherton J., Vijayaraghavan S., Morris J., Bhattacharya S., Hanson P., Campbell-Richards D., Ramoutar S., Collard A., Hodkinson I. Real-world implementation of video outpatient consultations at macro, meso, and micro levels: mixed-method study. J. Med. Internet Res. 2018;20(4):e150. doi: 10.2196/jmir.9897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greis C., Meier Zürcher C., Djamei V., Moser A., Lautenschlager S., Navarini A.A. Unmet digital health service needs in dermatology patients. J. Dermatol. Treat. 2018;29(7):643–647. doi: 10.1080/09546634.2018.1441488. [DOI] [PubMed] [Google Scholar]
- Hammersley V., Donaghy E., Parker R., McNeilly H., Atherton H., Bikker A., Campbell J., McKinstry B. Comparing the content and quality of video, telephone, and face-to-face consultations: a nonrandomised, quasi-experimental, exploratory study in UK primary care. Br. J. Gen. Pract. 2019;69(686):e595–e604. doi: 10.3399/bjgp19X704573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Health and Care Professions Council . 2013. The Standards of Proficiency for Physiotherapists.https://www.hcpc-uk.org/standards/standards-of-proficiency/physiotherapists/ [Google Scholar]
- Heritage J., Robinson J.D. The structure of patients' presenting concerns: physicians' opening questions. Health Commun. 2006;19(2):89–102. doi: 10.1207/s15327027hc1902_1. [DOI] [PubMed] [Google Scholar]
- Heritage J. Epistemics in action: action formation and territories of knowledge. Res. Lang. Soc. Interact. 2012;45:1–29. [Google Scholar]
- Heritage J., Robinson J.D., Elliott M.N., Beckett M., Wilkes M. Reducing patients' unmet concerns in primary care: the difference one word can make. J. Gen. Intern. Med. 2007;22(10):1429–1433. doi: 10.1007/s11606-007-0279-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Irish J.T., Hall J.A. Interruptive patterns in medical visits: the effects of role, status and gender. Soc. Sci. Med. 1995;41(6):873–881. doi: 10.1016/0277-9536(94)00399-e. [DOI] [PubMed] [Google Scholar]
- Jones G., Brennan V., Jacques R., Wood H., Dixon S., Radley S. Evaluating the impact of a 'virtual clinic' on patient experience, personal and provider costs of care in urinary incontinence: a randomised controlled trial. PloS One. 2018;13(1) doi: 10.1371/journal.pone.0189174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koch S. Home telehealth – current state and future trends. Int. J. Med. Inf. 2006;75(8):565–576. doi: 10.1016/j.ijmedinf.2005.09.002. [DOI] [PubMed] [Google Scholar]
- Lærum E., Indahl A., Sture Skouen J. What is ‘the good back consultation’? A combined qualitative and quantitative study of chronic low back pain patients' interaction with and perceptions of consultations with specialists. J. Rehabil. Med. 2006;38:255–262. doi: 10.1080/16501970600613461. [DOI] [PubMed] [Google Scholar]
- Landow S.M., Mateus A., Korgavkar K., Nightingale D., Weinstock M.A. Teledermatology: key factors associated with reducing face-to-face dermatology visits. J. Am. Acad. Dermatol. 2014;71(3):570–576. doi: 10.1016/j.jaad.2014.02.021. [DOI] [PubMed] [Google Scholar]
- Langewitz W., Denz M., Keller A., Kiss A., Rütimann S., Wössmer B. Spontaneous talking time at start of consultation in outpatient clinic: cohort study. BMJ. 2002;325(7366):682–683. doi: 10.1136/bmj.325.7366.682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leydon G.M., Halls A., Ekberg K., Latter S., Stuart B., Moynihan C., Salmon P., Danquah L., Brindle L., Howe S., Woods C.J., Little P. Specialist call handlers' perspectives on providing help on a cancer helpline: a qualitative interview study. Eur. J. Canc. Care. 2019;28(5) doi: 10.1111/ecc.13081. [DOI] [PubMed] [Google Scholar]
- Lowe A., Littlewood C., McLean S. Understanding physical activity promotion in physiotherapy practice: a qualitative study. Musculoskelet. Sci. Pract. 2018;35:1–7. doi: 10.1016/j.msksp.2018.01.009. [DOI] [PubMed] [Google Scholar]
- Marvel M.K., Epstein R.M., Flowers K., Beckman H.B. Soliciting the patient's agenda: have we improved? J. Am. Med. Assoc. 1999;281(3):283–287. doi: 10.1001/jama.281.3.283. [DOI] [PubMed] [Google Scholar]
- Medical Defence Union Montgomery and informed consent. 2018. https://www.themdu.com/guidance-and-advice/guides/montgomery-and-informed-consent
- National Information Board . The Stationery Office; London: 2014. Personalised Health and Care 2020. Using Data and Technology to Transform Outcomes for Patients and Citizens.https://www.gov.uk/government/publications/personalised-health-and-care-2020 [Google Scholar]
- Nhs The NHS long term plan. 2019. https://www.longtermplan.nhs.uk/
- NHSX . 2020. COVID-19 Information Governance Advice for Staff Working in Health and Care Organisations.https://www.nhsx.nhs.uk/covid-19-response/data-and-information-governance/information-governance/covid-19-information-governance-advice-health-and-care-professionals/ [Google Scholar]
- Petersson N.B., Jørgensen A.L., Danbjørg D.B., Dieperink K.B. Video-consulted rounds with caregivers: the experience of patients with cancer. Eur. J. Oncol. Nurs. 2020;46:101763. doi: 10.1016/j.ejon.2020.101763. [DOI] [PubMed] [Google Scholar]
- Raja S., Hasnain M., Vadakumchery T., Hamad J., Shah R., Hoersch M. Identifying elements of patient-centered care in underserved populations: a qualitative study of patient perspectives. PloS One. 2015;10(5) doi: 10.1371/journal.pone.0126708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richardson B.R., Truter P., Blumke R., Russell T.G. Physiotherapy assessment and diagnosis of musculoskeletal disorders of the knee via telerehabilitation. J. Telemed. Telecare. 2017;23(1):88–95. doi: 10.1177/1357633X15627237. [DOI] [PubMed] [Google Scholar]
- Roberts L. First impressions: an information leaflet for patients attending a musculoskeletal out-patient department. Physiotherapy. 2006;92:179–186. [Google Scholar]
- Roberts L.C., Burrow F.A. Interruption and rapport disruption: measuring the prevalence and nature of verbal interruptions during back pain consultations. J. Commun. Healthc. 2018 doi: 10.1080/17538068.2018.1449289. [DOI] [Google Scholar]
- Robinson J.D., Heritage J. The structure of patients' presenting concerns: the completion relevance of current symptoms. Soc. Sci. Med. 2005;61(2):481–493. doi: 10.1016/j.socscimed.2004.12.004. [DOI] [PubMed] [Google Scholar]
- Robinson J.D., Heritage J. Physiciansʼ opening questions and patientsʼ satisfaction. Patient Educ. Counsel. 2006;60:279–285. doi: 10.1016/j.pec.2005.11.009. [DOI] [PubMed] [Google Scholar]
- Robinson J.D., Tate A., Heritage J. Agenda-setting revisited: when and how do primary-care physicians solicit patients' additional concerns? Patient Educ. Counsel. 2016;99(5):718–723. doi: 10.1016/j.pec.2015.12.009. [DOI] [PubMed] [Google Scholar]
- Robinson J.D., Heritage J. How patients understand physicians' solicitations of additional concerns: implications for up-front agenda setting in primary care. Health Commun. 2016;31(4):434–444. doi: 10.1080/10410236.2014.960060. [DOI] [PubMed] [Google Scholar]
- Sacks H. vol. I. Basil Blackwell; Oxford: 1992. (Lectures on Conversation). [Google Scholar]
- Schegloff E.A., Sacks H. Opening up closings. Semiotica. 1973;7:289–327. [Google Scholar]
- Shaw S., Wherton J., Vijayaraghavan S., Morris J., Bhattacharya S., Hanson P., Campbell-Richards D., Ramoutar S., Collard A., Hodkinson I., Greenhalgh T. vol. 6. NIHR Journals Library; Health Services and Delivery Research; Southampton (UK): 2018. (Advantages and Limitations of Virtual Online Consultations in a NHS Acute Trust: the VOCAL Mixed-Methods Study). 21. [DOI] [PubMed] [Google Scholar]
- Stuart B., Leydon G., Woods C., Gennery E., Elsey C., Summers R., Stevenson F., Chew-Graham C., Barnes R., Drew P., Moore M., Little P. The elicitation and management of multiple health concerns in GP consultations. Patient Educ. Counsel. 2019;102(4):687–693. doi: 10.1016/j.pec.2018.11.009. [DOI] [PubMed] [Google Scholar]
- van Eck C.F. Web-based follow-up after total joint arthroplasty proves to be cost-effective, but is it safe? Commentary on an article by Jacquelyn Marsh, PhD, et al: "Economic Evaluation of Web-Based Compared with In-Person Follow-Up after Total Joint Arthroplasty". J. Bone Joint Surg. Am. 2014;vol. 96 doi: 10.2106/JBJS.N.00829. 22. [DOI] [PubMed] [Google Scholar]
- Vestergaard L.V., Østervang C., Danbjørg D.B., Dieperink K.B. Video-based patient rounds for caregivers of patients with cancer. Oncol. Nurs. Forum. 2019;46(4):485–492. doi: 10.1188/19.ONF.485-492. [DOI] [PubMed] [Google Scholar]
- Vicaria I.M., Bernieri F.J., Isaacowitz D.M. Perceptions of rapport across the life span: gaze patterns and judgment accuracy. Psychol. Aging. 2015;30(2):396–406. doi: 10.1037/pag0000019. [DOI] [PubMed] [Google Scholar]
- Wherton J., Shaw S., Papoutsi C., Seuren L., Greenhalgh T. Guidance on the introduction and use of video consultations during COVID-19: important lessons from qualitative research. BMJ Leader. 2020 doi: 10.1136/leader-2020-000262. [DOI] [Google Scholar]
- Whited J.D. Teledermatology. Current status and future directions. Am. J. Clin. Dermatol. 2001;2(2):59–64. doi: 10.2165/00128071-200102020-00001. [DOI] [PubMed] [Google Scholar]
- Woods C.J., Drew P., Leydon G.M. Closing calls to a cancer helpline: expressions of caller satisfaction. Patient Educ. Counsel. 2015;98(8):943–953. doi: 10.1016/j.pec.2015.04.015. [DOI] [PubMed] [Google Scholar]
- World Health Organization . vol. 9. WHO Press; Switzerland: 2010. https://www.who.int/goe/publications/goe_telemedicine_2010.pdf (Telemedicine: Opportunities and Developments in Member States: Report on the Second Global Survey on eHealth 2009). [Google Scholar]
- World Health Organization Draft global strategy on digital health 2020-2015. 2020. https://www.who.int/docs/default-source/documents/gs4dhdaa2a9f352b0445bafbc79ca799dce4d.pdf?sfvrsn=f112ede5_50 [DOI] [PMC free article] [PubMed]
- Zolnierek K.B., Dimatteo M.R. Physician communication and patient adherence to treatment: a meta-analysis. Med. Care. 2009;47:832–834. doi: 10.1097/MLR.0b013e31819a5acc. [DOI] [PMC free article] [PubMed] [Google Scholar]


